Myocardial Bridging: Review on the Role of Coronary Computed Tomography Angiography
Abstract
:1. Introduction
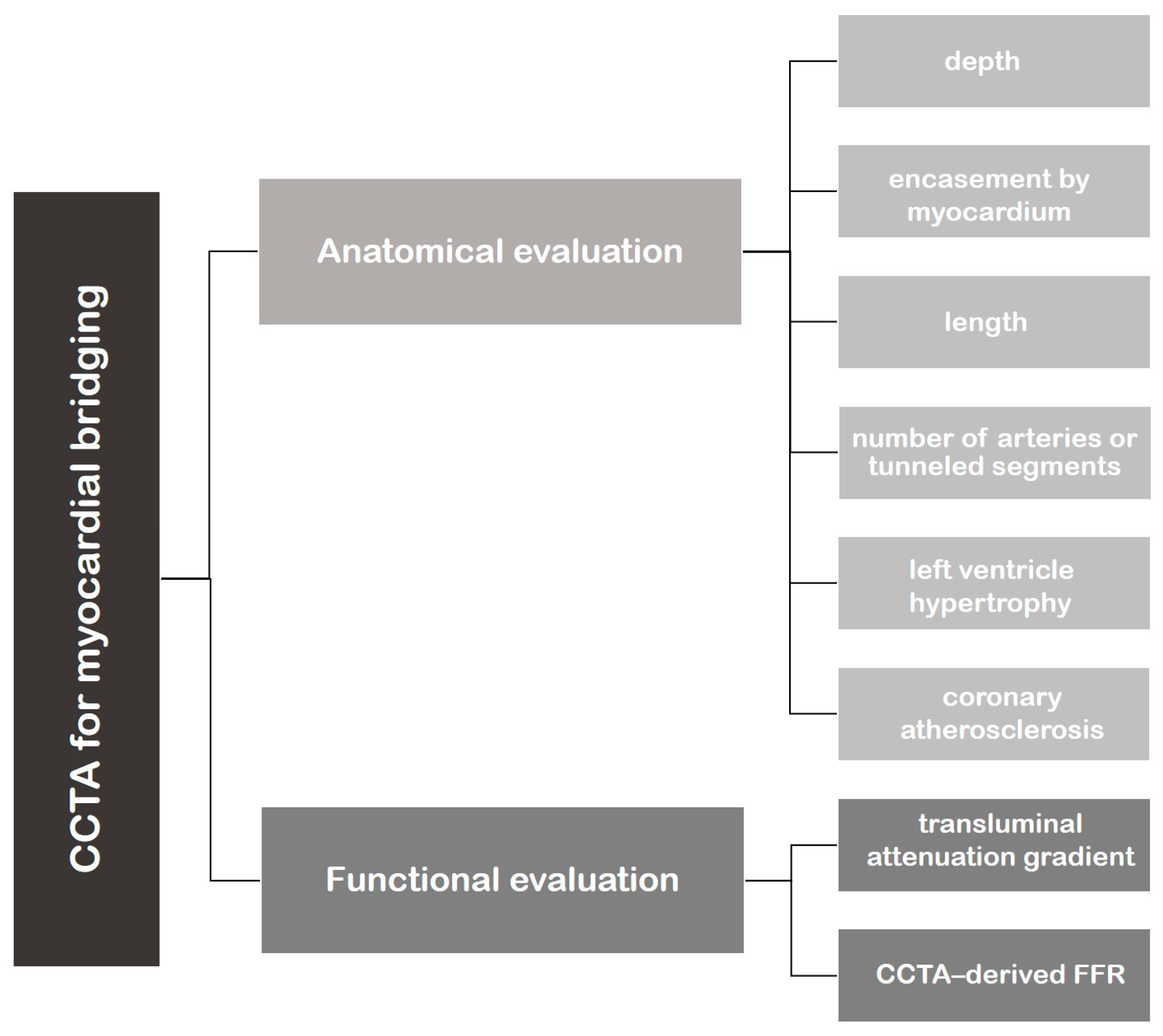
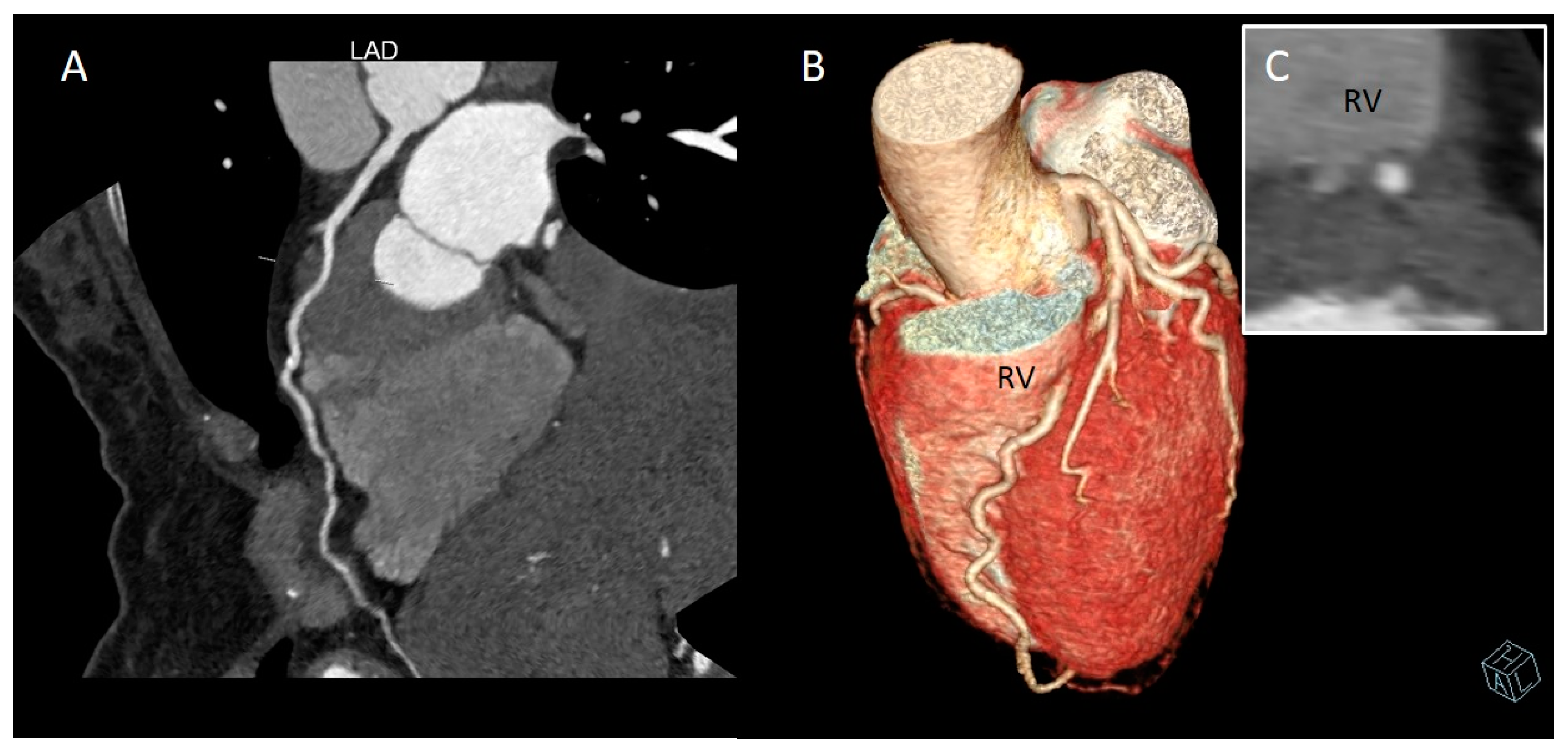
2. CCTA Imaging Protocol
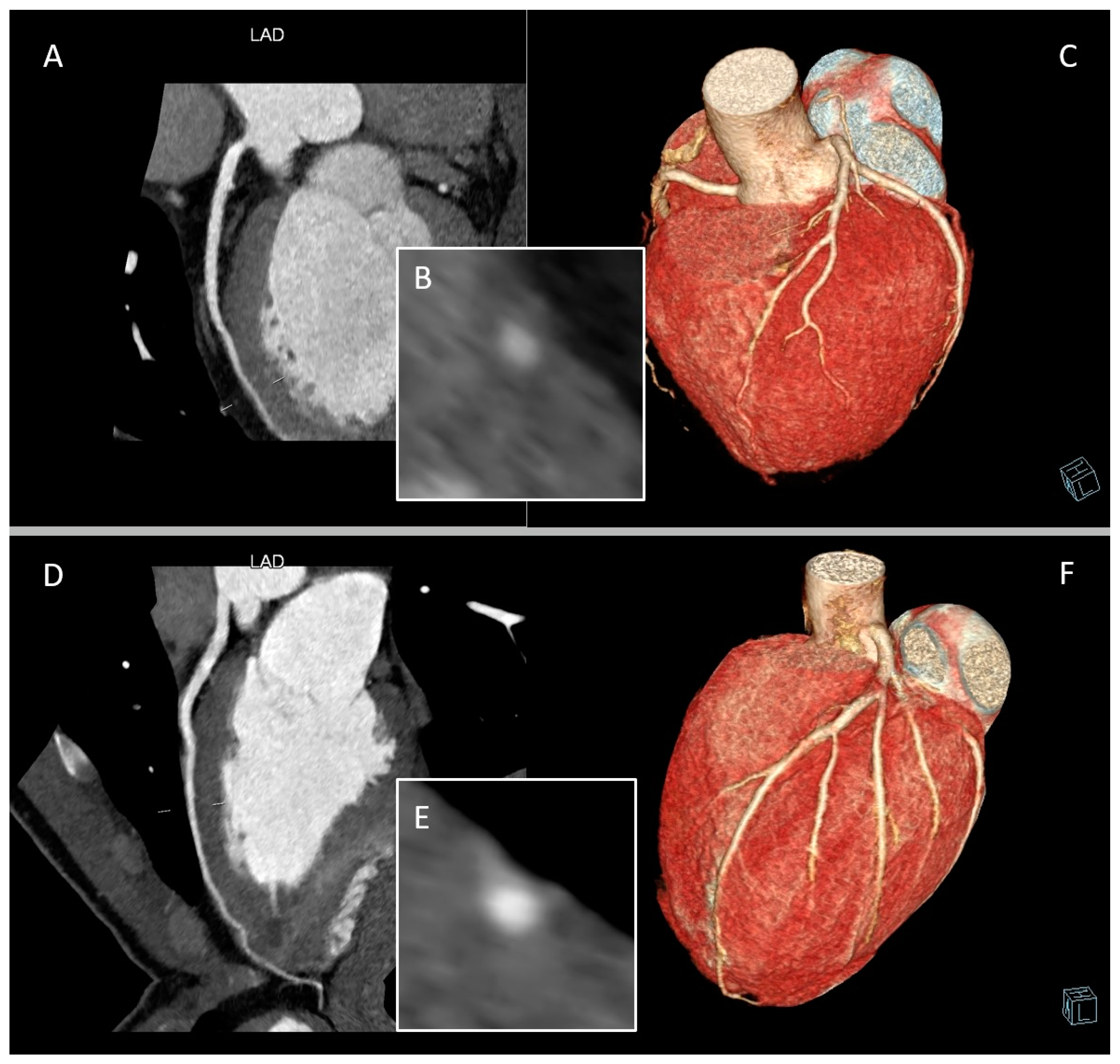
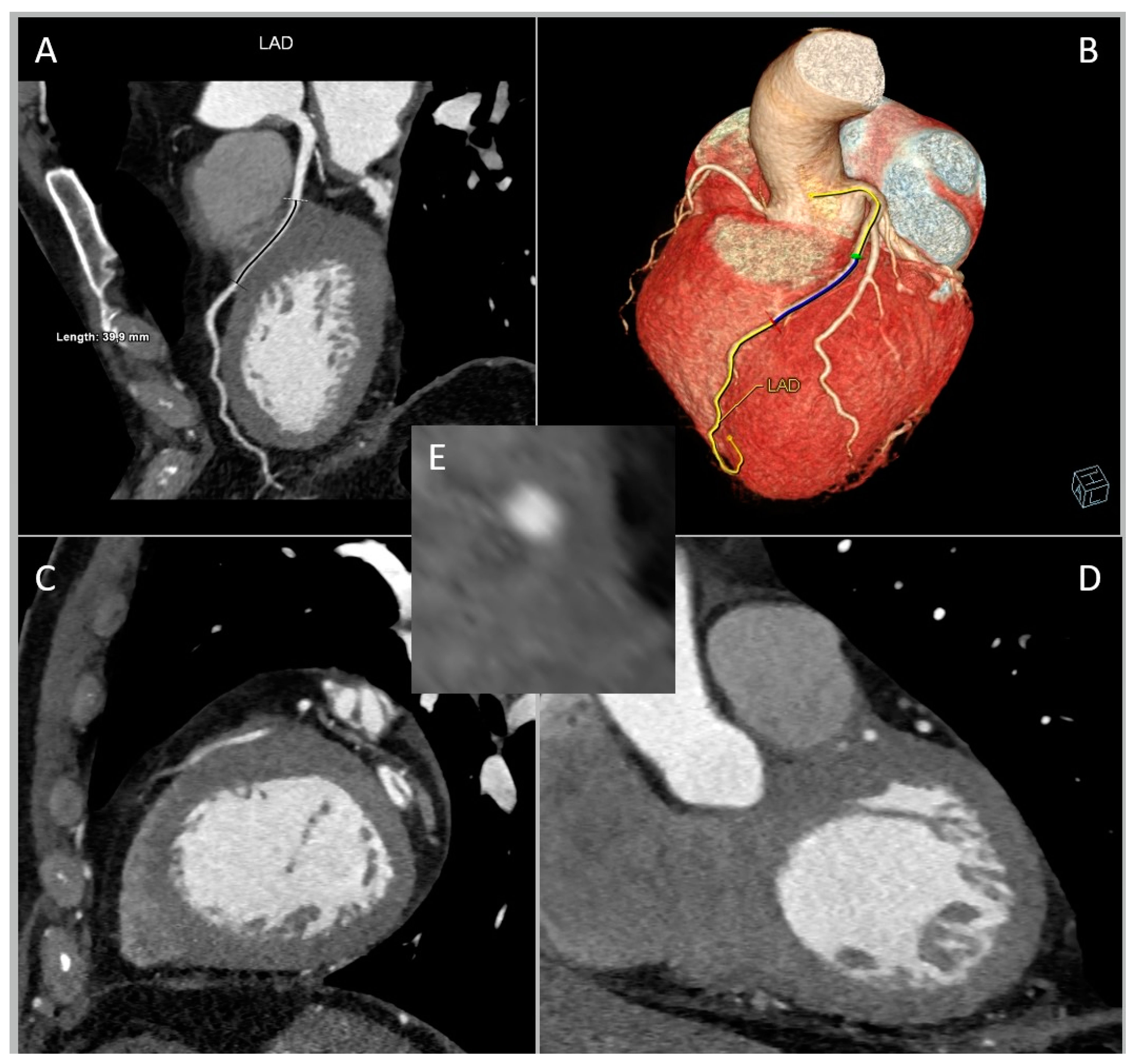
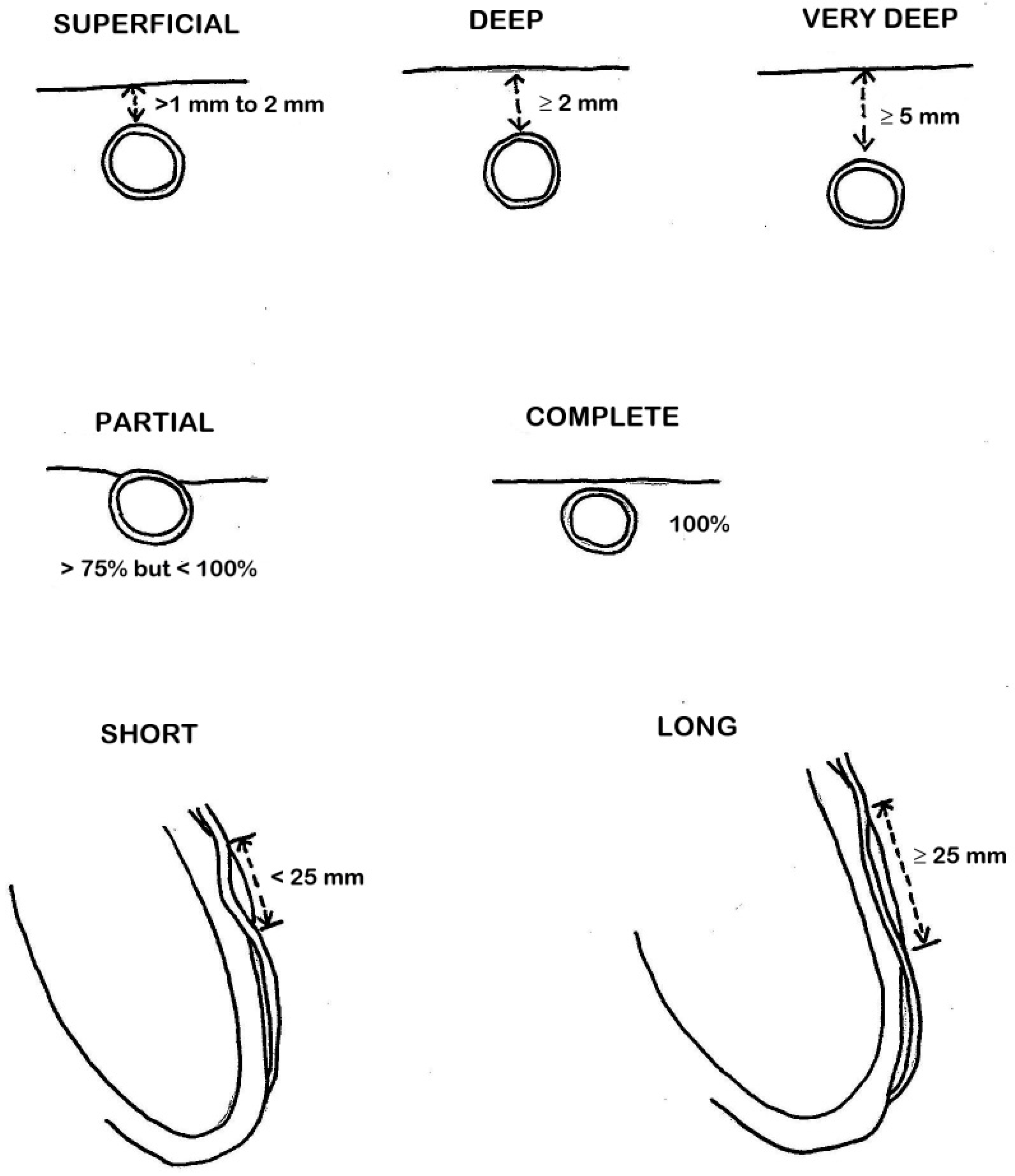
3. Role of CCTA: Anatomical Evaluation
4. Role of CCTA: Functional Evaluation
5. Discussion
6. Future Directions
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alegria, J.R.; Herrmann, J.; Holmes, D.R., Jr.; Lerman, A.; Rihal, C.S. Myocardial bridging. Eur. Heart J. 2005, 26, 1159–1168. [Google Scholar] [CrossRef] [PubMed]
- Reyman, H. Dissertatio de vasis cordis propriis. Diss. Ina. 1737, 2, 359–378. [Google Scholar]
- Geiringer, E. The mural coronary. Am. Heart J. 1951, 41, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Mohlenkamp, S.; Hort, W.; Ge, J.; Erbel, R. Update on myocardial bridging. Circulation 2002, 106, 2616–2622. [Google Scholar] [CrossRef]
- Çullu, N.; Yeniçeri, I.; Özdemir, M.Y.; Altun, I.; Doğan, E. Evaluation of the morphological and clinical features of left anterior descending myocardial bridging with multi-detector computed tomography. Kardiochir Torakochirurgia Pol. 2021, 18, 87–91. [Google Scholar] [CrossRef]
- Hashikata, T.; Kameda, R.; Ako, J. Clinical Implication and Optimal Management of Myocardial Bridging: Role of Cardiovascular Imaging. Interv. Cardiol. Clin. 2023, 12, 281–288. [Google Scholar] [CrossRef]
- Kantarci, M.; Duran, C.; Durur, I.; Alper, F.; Onbas, O.; Gulbaran, M.; Okur, A. Detection of Myocardial Bridging with ECG-Gated MDCT and Multiplanar Reconstruction. Am. J. Roentgenol. 2006, 186 (Suppl. S2), S391–S394. [Google Scholar] [CrossRef]
- Kawawa, Y.; Ishikawa, Y.; Gomi, T.; Nagamoto, M.; Terada, H.; Ishii, T.; Kohda, E. Detection of myocardial bridge and evaluation of its anatomical properties by coronary multislice spiral computed tomography. Eur. J. Radiol. 2007, 61, 130–138. [Google Scholar] [CrossRef]
- Leschka, S.; Koepfli, P.; Husmann, L.; Plass, A.; Vachenauer, R.; Gaemperli, O.; Schepis, T.; Genoni, M.; Marincek, B.; Eberli, F.R.; et al. Myocardial bridging: Depiction rate and morphology at CT coronary angiography—Comparison with conventional coronary angiography. Radiology 2008, 246, 754–762. [Google Scholar] [CrossRef]
- Kim, P.J.; Hur, G.; Kim, S.Y.; Namgung, J.; Hong, S.W.; Kim, Y.H.; Lee, W.R. Frequency of myocardial bridges and dynamic compression of epicardial coronary arteries: A comparison between computed tomography and invasive coronary angiography. Circulation 2009, 119, 1408–1416. [Google Scholar] [CrossRef]
- Kramer, J.R.; Kitazume, H.; Proudfit, W.L.; Sones, F. Clinical significance of isolated coronary bridges: Benign and frequent condition involving the left anterior descending artery. Am. Heart J. 1982, 103, 283–288. [Google Scholar] [CrossRef]
- Mouratidis, B.; E Lomas, F.; McGill, D. Thallium-201 myocardial SPECT in myocardial bridging. J. Nucl. Med. 1995, 36, 1031–1033. [Google Scholar] [PubMed]
- Souibri, K.; Grollier, G. Infarction Due to Myocardial Bridging. N. Engl. J. Med. 2005, 353, 1147. [Google Scholar] [CrossRef] [PubMed]
- Cottin, Y.; Laurent, G.; Gabrielle, F.; André, F.; Baudoin, N.; Blettery, B.; David, M.; Wolf, J.E. Acute myocardial infarction related to myocardial bridging. Eur. Heart J. 1995, 16, 2002–2003. [Google Scholar] [CrossRef] [PubMed]
- Zeina, A.R.; Shefer, A.; Sharif, D.; Rosenschein, U.; Barmeir, E. Acute myocardial infarction in a young woman with normal coronary arteries and myocardial bridging. Br. J. Radiol. 2008, 81, e141–e144. [Google Scholar] [CrossRef] [PubMed]
- Takamura, K.; Fujimoto, S.; Nanjo, S.; Nakanishi, R.; Hisatake, S.; Namiki, A.; Ishikawa, Y.; Ishii, T.; Yamazaki, J. Anatomical Characteristics of Myocardial Bridge in Patients With Myocardial Infarction by Multi-Detector Computed Tomography. Circ. J. 2011, 75, 642–648. [Google Scholar] [CrossRef]
- Matta, A.; Nader, V.; Canitrot, R.; Delmas, C.; Bouisset, F.; Lhermusier, T.; Blanco, S.; Campelo-Parada, F.; Elbaz, M.; Carrie, D.; et al. Myocardial bridging is significantly associated to myocardial infarction with non-obstructive coronary arteries. Eur. Heart J. Acute Cardiovasc. Care 2022, 11, 501–507. [Google Scholar] [CrossRef]
- Faruqui, A.M.; Maloy, W.C.; Felner, J.M.; Schlant, R.C.; Logan, W.D.; Symbas, P. Symptomatic myocardial bridging of coronary artery. Am. J. Cardiol. 1978, 41, 1305–1310. [Google Scholar] [CrossRef]
- Gow, R.M. Myocardial bridging: Does it cause sudden death? Card. Electrophysiol. Rev. 2002, 6, 112–114. [Google Scholar] [CrossRef]
- Nakanishi, R.; Rajani, R.; Ishikawa, Y.; Ishii, T.; Berman, D.S. Myocardial bridging on coronary CTA: An innocent bystander or a culprit in myocardial infarction? J. Cardiovasc. Comput. Tomogr. 2012, 6, 3–13. [Google Scholar] [CrossRef]
- Narula, J.; Chandrashekhar, Y.; Ahmadi, A.; Abbara, S.; Berman, D.S.; Blankstein, R.; Leipsic, J.; Newby, D.; Nicol, E.D.; Nieman, K.; et al. SCCT 2021 Expert Consensus Document on Coronary Computed Tomographic Angiography: A Report of the Society of Cardiovascular Computed Tomography. J. Cardiovasc. Comput. Tomogr. 2021, 15, 192–217. [Google Scholar] [CrossRef] [PubMed]
- Abbara, S.; Blanke, P.; Maroules, C.D.; Cheezum, M.; Choi, A.D.; Han, B.K.; Marwan, M.; Naoum, C.; Norgaard, B.L.; Rubinshtein, R.; et al. SCCT guidelines for the performance and acquisition of coronary computed tomographic angiography: A report of the society of Cardiovascular Computed Tomography Guidelines Committee: Endorsed by the North American Society for Cardiovascular Imaging (NASCI). J. Cardiovasc. Comput. Tomogr. 2016, 10, 435–449. [Google Scholar] [CrossRef] [PubMed]
- de Graaf, F.; Schuijf, J.; Delgado, V.; van Velzen, J.; Kroft, L.; de Roos, A.; Jukema, J.; van der Wall, E.; Bax, J. Clinical Application of CT Coronary Angiography: State of the Art. Heart Lung Circ. 2010, 19, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Gould, K.L.; Johnson, N.P. Myocardial Bridges: Lessons in Clinical Coronary Pathophysiology. JACC Cardiovasc. Imaging 2015, 8, 705–709. [Google Scholar] [CrossRef]
- Ishikawa, Y.; Akasaka, Y.; Suzuki, K.; Fujiwara, M.; Ogawa, T.; Yamazaki, K.; Niino, H.; Tanaka, M.; Ogata, K.; Morinaga, S.; et al. Anatomic properties of myocardial bridge predisposing to myocardial infarction. Circulation 2009, 120, 376–383. [Google Scholar] [CrossRef]
- Corban, M.T.; Hung, O.Y.; Eshtehardi, P.; Rasoul-Arzrumly, E.; McDaniel, M.; Mekonnen, G.; Timmins, L.H.; Lutz, J.; Guyton, R.A.; Samady, H. Myocardial bridging: Contemporary understanding of pathophysiology with implications for diagnostic and therapeutic strategies. J. Am. Coll. Cardiol. 2014, 63, 2346–2355. [Google Scholar] [CrossRef]
- A Truong, Q.; Ptaszek, L.M.; Charipar, E.M.; Taylor, C.; Fontes, J.D.; Kriegel, M.; Irlbeck, T.; Toepker, M.; Schlett, C.L.; Bamberg, F.; et al. Performance of electrocardiographic criteria for left ventricular hypertrophy as compared with cardiac computed tomography: From the Rule Out Myocardial Infarction Using Computer Assisted Tomography trial. J. Hypertens. 2010, 28, 1959–1967. [Google Scholar] [CrossRef]
- Ge, J.; Jeremias, A.; Rupp, A.; Abels, M.; Baumgart, D.; Liu, F.; Haude, M.; Görge, G.; Von Birgelen, C.; Sack, S.; et al. New signs characteristic of myocardial bridging demonstrated by intracoronary ultrasound and Doppler. Eur. Heart J. 1999, 20, 1707–1716. [Google Scholar] [CrossRef]
- Wu, S.; Liu, W.; Zhou, Y. Spontaneous coronary artery dissection in the presence of myocardial bridge causing myocardial infarction: An insight into mechanism. Int. J. Cardiol. 2016, 206, 77–78. [Google Scholar] [CrossRef]
- Verhagen, S.N.; Rutten, A.; Meijs, M.F.; Isgum, I.; Cramer, M.J.; van der Graaf, Y.; Visseren, F.L. Relationship between myocardial bridges and reduced coronary atherosclerosis in patients with angina pectoris. Int. J. Cardiol. 2013, 167, 883–888. [Google Scholar] [CrossRef]
- Nishimiya, K.; Matsumoto, Y.; Wang, H.; Piao, Z.; Ohyama, K.; Uzuka, H.; Hao, K.; Tsuburaya, R.; Takahashi, J.; Ito, K.; et al. Absence of adventitial vasa vasorum formation at the coronary segment with myocardial bridge—An optical coherence tomography study. Int. J. Cardiol. 2018, 250, 275–277. [Google Scholar] [CrossRef] [PubMed]
- Alsoufi, B. Do not miss the bridge. J. Thorac. Cardiovasc. Surg. 2018, 156, 1627–1628. [Google Scholar] [CrossRef]
- White, S.J.; Hayes, E.M.; Lehoux, S.; Jeremy, J.Y.; Horrevoets, A.J.; Newby, A.C. Characterization of the differential response of endothelial cells exposed to normal and elevated laminar shear stress. J. Cell. Physiol. 2011, 226, 2841–2848. [Google Scholar] [CrossRef]
- Bourassa, M.G.; Butnaru, A.; Lespérance, J.; Tardif, J.-C. Symptomatic myocardial bridges: Overview of ischemic mechanisms and current diagnostic and treatment strategies. J. Am. Coll. Cardiol. 2003, 41, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Koo, H.J.; Yang, D.H.; Kim, Y.-H.; Kang, J.-W.; Kang, S.-J.; Kweon, J.; Kim, H.J.; Lim, T.-H. CT-based myocardial ischemia evaluation: Quantitative angiography, transluminal attenuation gradient, myocardial perfusion, and CT-derived fractional flow reserve. Int. J. Cardiovasc. Imaging 2015, 32 (Suppl. S1), 1–19. [Google Scholar] [CrossRef] [PubMed]
- Stuijfzand, W.J.; Danad, I.; Raijmakers, P.G.; Marcu, C.B.; Heymans, M.W.; van Kuijk, C.C.; van Rossum, A.C.; Nieman, K.; Min, J.K.; Leipsic, J.; et al. Additional Value of Transluminal Attenuation Gradient in CT Angiography to Predict Hemodynamic Significance of Coronary Artery Stenosis. JACC Cardiovasc. Imaging 2014, 7, 374–386. [Google Scholar] [CrossRef]
- Steigner, M.L.; Mitsouras, D.; Whitmore, A.G.; Otero, H.J.; Wang, C.; Buckley, O.; Levit, N.A.; Hussain, A.Z.; Cai, T.; Mather, R.T.; et al. Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ. Cardiovasc. Imaging 2010, 3, 179–186. [Google Scholar] [CrossRef]
- Choi, J.-H.; Min, J.K.; Labounty, T.M.; Lin, F.Y.; Mendoza, D.D.; Shin, D.H.; Ariaratnam, N.S.; Koduru, S.; Granada, J.F.; Gerber, T.C.; et al. Intracoronary Transluminal Attenuation Gradient in Coronary CT Angiography for Determining Coronary Artery Stenosis. JACC Cardiovasc. Imaging 2011, 4, 1149–1157. [Google Scholar] [CrossRef]
- Yu, M.; Zhang, Y.; Li, Y.; Li, M.; Li, W.; Zhang, J. Assessment of Myocardial Bridge by Cardiac CT: Intracoronary Transluminal Attenuation Gradient Derived from Diastolic Phase Predicts Systolic Compression. Korean J. Radiol. 2017, 18, 655–663. [Google Scholar] [CrossRef]
- Yoon, Y.E.; Choi, J.-H.; Kim, J.-H.; Park, K.-W.; Doh, J.-H.; Kim, Y.-J.; Koo, B.-K.; Min, J.K.; Erglis, A.; Gwon, H.-C.; et al. Noninvasive diagnosis of ischemia-causing coronary stenosis using CT angiography: Diagnostic value of transluminal attenuation gradient and fractional flow reserve computed from coronary CT angiography compared to invasively measured fractional flow reserve. JACC Cardiovasc. Imaging 2012, 5, 1088–1096. [Google Scholar]
- Zhou, F.; Wang, Y.N.; Schoepf, U.J.; Tesche, C.; Tang, C.X.; Zhou, C.S.; Xu, L.; Hou, Y.; Zheng, M.W.; Yan, J.; et al. Diagnostic Performance of Machine Learning Based CT-FFR in Detecting Ischemia in Myocardial Bridging and Concomitant Proximal Atherosclerotic Disease. Can. J. Cardiol. 2019, 35, 1523–1533. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Dai, X.; Yu, L.; Lu, Z.; Shen, C.; Tao, X.; Zhang, J. Hemodynamic Change of Coronary Atherosclerotic Plaque After Statin Treatment: A Serial Follow-Up Study by Computed Tomography-Derived Fractional Flow Reserve. J. Am. Heart Assoc. 2020, 9, e015772. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Yu, L.; Dai, X.; Zhang, J. CT Fractional Flow Reserve for the Diagnosis of Myocardial Bridging-Related Ischemia: A Study Using Dynamic CT Myocardial Perfusion Imaging as a Reference Standard. Korean J. Radiol. 2021, 22, 1964–1973. [Google Scholar] [CrossRef]
- Zhou, F.; Tang, C.X.; Schoepf, U.J.; Tesche, C.; Bauer, M.J.; Jacobs, B.E.; Zhou, C.S.; Yan, J.; Lu, M.J.; Lu, G.M.; et al. Fractional flow reserve derived from CCTA may have a prognostic role in myocardial bridging. Eur. Radiol. 2019, 29, 3017–3026. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Tang, C.X.; Schoepf, U.J.; Tesche, C.; Rollins, J.D.; Liu, H.; Zhou, C.S.; Yan, J.; Lu, M.J.; Lu, G.M.; et al. Machine Learning Using CT-FFR Predicts Proximal Atherosclerotic Plaque Formation Associated with LAD Myocardial Bridging. JACC Cardiovasc. Imaging 2019, 12 Pt 1, 1591–1593. [Google Scholar] [CrossRef] [PubMed]
- Hostiuc, S.; Negoi, I.; Rusu, M.C.; Hostiuc, M. Myocardial Bridging: A Meta-Analysis of Prevalence. J. Forensic Sci. 2018, 63, 1176–1185. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.G.; E Trotter, S.; Konig, B.; Decourt, L.V.; Fox, K.; Olsen, E.G. Myocardial bridges: Morphological and functional aspects. Br. Heart J. 1991, 66, 364–367. [Google Scholar] [CrossRef]
- Jodocy, D.; Aglan, I.; Friedrich, G.; Mallouhi, A.; Pachinger, O.; Jaschke, W.; Feuchtner, G.M. Left anterior descending coronary artery myocardial bridging by multislice computed tomography: Correlation with clinical findings. Eur. J. Radiol. 2010, 73, 89–95. [Google Scholar] [CrossRef]
- Liu, G.; Qu, Y.; Chen, X.; Liao, M.; Hu, H.; Cao, Y.; Tian, Z. Measurements of myocardial bridges on computed tomography predict presence of clinical symptoms and outcomes of adverse heart events: A retrospective study in a large population from China. Acta Radiol. 2016, 58, 1068–1076. [Google Scholar] [CrossRef]
- Sternheim, D.; Power, D.A.; Samtani, R.; Kini, A.; Fuster, V.; Sharma, S. Myocardial Bridging: Diagnosis, Functional Assessment, and Management: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 78, 2196–2212. [Google Scholar] [CrossRef]
- Tarantini, G.; Migliore, F.; Cademartiri, F.; Fraccaro, C.; Iliceto, S. Left Anterior Descending Artery Myocardial Bridging: A Clinical Approach. J. Am. Coll. Cardiol. 2016, 68, 2887–2899. [Google Scholar] [CrossRef] [PubMed]
- Bockeria, L.A.; Sukhanov, S.G.; Orekhova, E.N.; Shatakhyan, M.P.; Korotayev, D.A.; Sternik, L. Results of Coronary Artery Bypass Grafting in Myocardial Bridging of Left Anterior Descending Artery. J. Card. Surg. 2013, 28, 218–221. [Google Scholar] [CrossRef]
- Maeda, K.; Schnittger, I.; Murphy, D.J.; Tremmel, J.A.; Boyd, J.H.; Peng, L.; Okada, K.; Pargaonkar, V.S.; Hanley, F.L.; Mitchell, R.S.; et al. Surgical unroofing of hemodynamically significant myocardial bridges in a pediatric population. J. Thorac. Cardiovasc. Surg. 2018, 156, 1618–1626. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.-Z.; Zhu, G.-Y.; Zhang, Y.; Bai, L.-J.; Wang, Z. Myocardial Bridge Bypass Graft: A Novel Surgical Procedure for Extensive Myocardial Bridges. Ann. Thorac. Surg. 2021, 112, e115–e117. [Google Scholar] [CrossRef] [PubMed]
- Hashikata, T.; Honda, Y.; Wang, H.; Pargaonkar, V.S.; Nishi, T.; Hollak, M.B.; Rogers, I.S.; Nieman, K.; Yock, P.G.; Fitzgerald, P.J.; et al. Impact of Diastolic Vessel Restriction on Quality of Life in Symptomatic Myocardial Bridging Patients Treated With Surgical Unroofing: Preoperative Assessments with Intravascular Ultrasound and Coronary Computed Tomography Angiography. Circ. Cardiovasc. Interv. 2021, 14, e011062. [Google Scholar] [CrossRef] [PubMed]
- Konen, E.; Goitein, O.; Sternik, L.; Eshet, Y.; Shemesh, J.; Di Segni, E. The Prevalence and Anatomical Patterns of Intramuscular Coronary Arteries: A Coronary Computed Tomography Angiographic Study. J. Am. Coll. Cardiol. 2007, 49, 587–593. [Google Scholar] [CrossRef]
- Tsujita, K.; Maehara, A.; Mintz, G.S.; Doi, H.; Kubo, T.; Castellanos, C.; Liu, J.; Yang, J.; Oviedo, C.; Franklin-Bond, T.; et al. Comparison of Angiographic and Intravascular Ultrasonic Detection of Myocardial Bridging of the Left Anterior Descending Coronary Artery. Am. J. Cardiol. 2008, 102, 1608–1613. [Google Scholar] [CrossRef]
- D’amario, D.; Ciliberti, G.; Restivo, A.; Laborante, R.; Migliaro, S.; Canonico, F.; Sangiorgi, G.M.; Tebaldi, M.; Porto, I.; Andreini, D.; et al. Myocardial bridge evaluation towards personalized medicine: Study design and preliminary results of the RIALTO registry. Eur. Heart J. Suppl. 2022, 24, H48–H56. [Google Scholar] [CrossRef] [PubMed]
- Tarantini, G.; Barioli, A.; Fovino, L.N.; Fraccaro, C.; Masiero, G.; Iliceto, S.; Napodano, M. Unmasking Myocardial Bridge–Related Ischemia by Intracoronary Functional Evaluation. Circ. Cardiovasc. Interv. 2018, 11, e006247. [Google Scholar] [CrossRef]
- Aleksandric, S.B.; Djordjevic-Dikic, A.D.; Dobric, M.R.; Giga, V.L.; Soldatovic, I.A.; Vukcevic, V.; Tomasevic, M.V.; Stojkovic, S.M.; Orlic, D.N.; Saponjski, J.D.; et al. Functional Assessment of Myocardial Bridging with Conventional and Diastolic Fractional Flow Reserve: Vasodilator Versus Inotropic Provocation. J. Am. Heart Assoc. 2021, 10, e020597. [Google Scholar] [CrossRef]
- Forsdahl, S.H.; Rogers, I.S.; Schnittger, I.; Tanaka, S.; Kimura, T.; Pargaonkar, V.S.; Chan, F.P.; Fleischmann, D.; Tremmel, J.A.; Becker, H.-C. Myocardial Bridges on Coronary Computed Tomography Angiography―Correlation with Intravascular Ultrasound and Fractional Flow Reserve. Circ. J. 2017, 81, 1894–1900. [Google Scholar] [CrossRef]
- Podolec, J.; Wiewiórka, Ł.; Siudak, Z.; Malinowski, K.; Dudek, D.; Gackowski, A.; Żmudka, K.; Legutko, J. Prevalence and clinical presentation of myocardial bridge on the basis of the National Polish Percutaneous Interventions Registry and the Classification of Rare Cardiovascular Diseases. Kardiol. Polska 2018, 77, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Tremmel, J.A.; Yamada, R.; Rogers, I.S.; Yong, C.M.; Turcott, R.; McConnell, M.V.; Dash, R.; Schnittger, I. A Novel Stress Echocardiography Pattern for Myocardial Bridge with Invasive Structural and Hemodynamic Correlation. J. Am. Heart Assoc. 2013, 2, e000097. [Google Scholar] [CrossRef] [PubMed]
- Pargaonkar, V.S.; Rogers, I.S.; Su, J.; Forsdahl, S.H.; Kameda, R.; Schreiber, D.; Chan, F.P.; Becker, H.-C.; Fleischmann, D.; Tremmel, J.A.; et al. Accuracy of a novel stress echocardiography pattern for myocardial bridging in patients with angina and no obstructive coronary artery disease—A retrospective and prospective cohort study. Int. J. Cardiol. 2020, 311, 107–113. [Google Scholar] [CrossRef] [PubMed]
- D’Amario, D.; Borovac, J.A.; Crea, F. Coronary microvascular dysfunction in heart failure with preserved ejection fraction: Not the end but the end of the beginning. Eur. J. Heart Fail. 2021, 23, 773–775. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rovera, C.; Moretti, C.; Bisanti, F.; De Zan, G.; Guglielmo, M. Myocardial Bridging: Review on the Role of Coronary Computed Tomography Angiography. J. Clin. Med. 2023, 12, 5949. https://doi.org/10.3390/jcm12185949
Rovera C, Moretti C, Bisanti F, De Zan G, Guglielmo M. Myocardial Bridging: Review on the Role of Coronary Computed Tomography Angiography. Journal of Clinical Medicine. 2023; 12(18):5949. https://doi.org/10.3390/jcm12185949
Chicago/Turabian StyleRovera, Chiara, Claudio Moretti, Francesca Bisanti, Giulia De Zan, and Marco Guglielmo. 2023. "Myocardial Bridging: Review on the Role of Coronary Computed Tomography Angiography" Journal of Clinical Medicine 12, no. 18: 5949. https://doi.org/10.3390/jcm12185949




