Coronary Event Risk Test (CERT) as a Risk Predictor for the 10-Year Clinical Outcome of Patients with Peripheral Artery Disease
Abstract
:1. Introduction
2. Methods
2.1. Study Subjects
2.2. Clinical and Laboratory Analyses
2.3. Statistical Analyses
2.4. Ethics Approval and Consent Statements
3. Results
3.1. Follow-Up
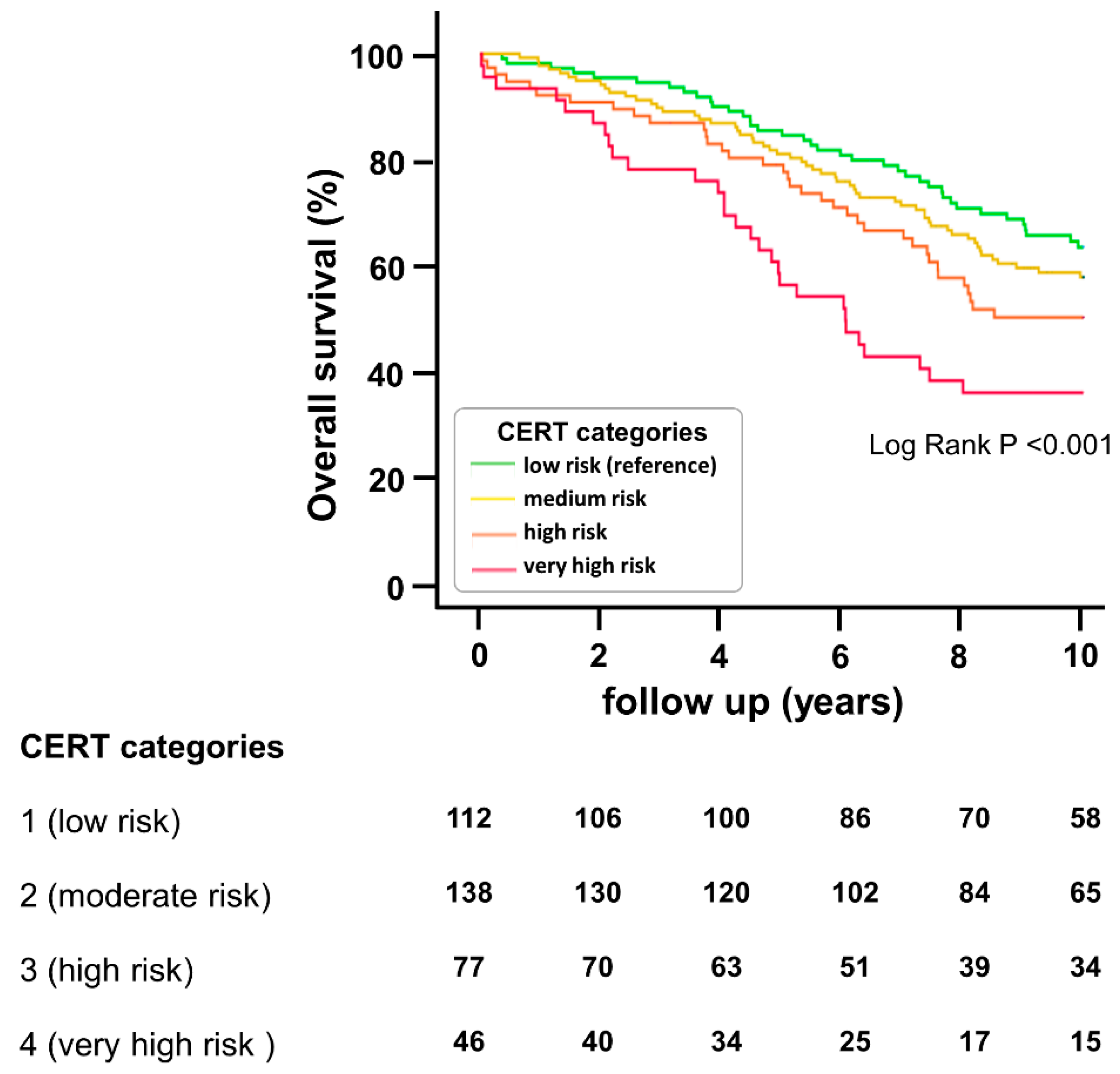
3.2. CERT Categories Predict Overall Mortality
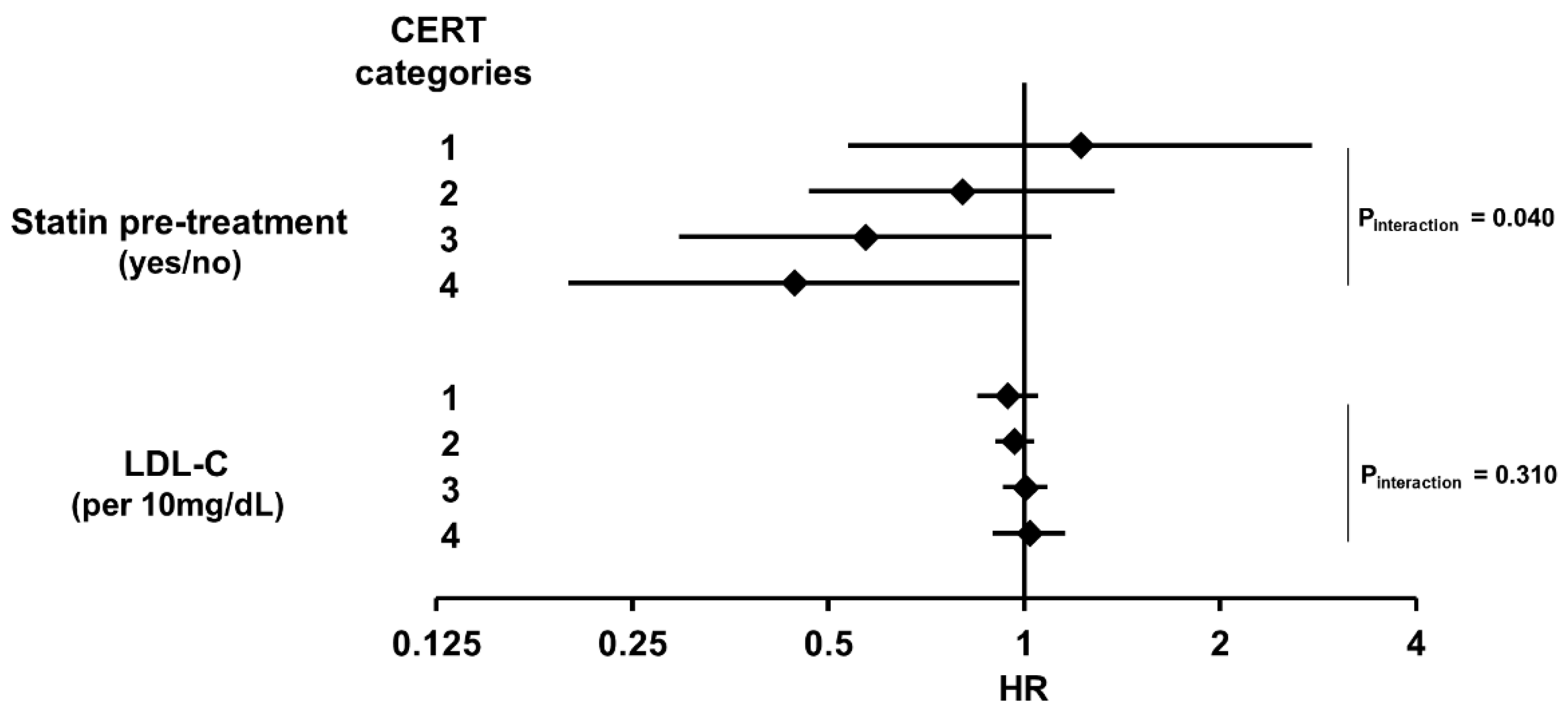
3.3. Statin Effect Is Stronger in Higher-Risk Groups
4. Discussion
4.1. Main Findings
4.2. Ceramides as Risk Predictors
4.3. Ceramides as Treatment Targets
4.4. Summary of Clinical Consequences
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CAD | Coronary artery disease |
| CERT | Coronary event risk test |
| CKD | Chronic kidney disease |
| CVD | Cardiovascular disease |
| HR | Hazard ratio |
| LC-MS/MS | Liquid chromatography-tandem mass spectrometry |
| LDL | Low-density lipoprotein |
| MACE | Major adverse cardiovascular events |
| T2DM | Type 2 diabetes mellitus |
| PAD | Peripheral artery disease |
References
- Weitz, J.I.; Byrne, J.; Clagett, G.P.; Farkouh, M.E.; Porter, J.M.; Sackett, D.L.; Strandness, D.E.; Taylor, L.M. Diagnosis and Treatment of Chronic Arterial Insufficiency of the Lower Extremities: A Critical Review. Circulation 1996, 94, 3026–3049. [Google Scholar] [CrossRef] [PubMed]
- Criqui, M.H. Peripheral Arterial Disease—Epidemiological Aspects. Vasc. Med. 2001, 6, 3–7. [Google Scholar] [CrossRef] [PubMed]
- CAPRIE Steering Committee A Randomised, Blinded, Trial of Clopidogrel versus Aspirin in Patients at Risk of Ischaemic Events (CAPRIE). Lancet 1996, 348, 1329–1339. [CrossRef]
- Steg, P.G.; Bhatt, D.L.; Wilson, P.W.F.; D’Agostino, R.; Ohman, E.M.; Röther, J.; Liau, C.-S.; Hirsch, A.T.; Mas, J.-L.; Ikeda, Y.; et al. One-Year Cardiovascular Event Rates in Outpatients with Atherothrombosis. JAMA 2007, 297, 1197–1206. [Google Scholar] [CrossRef]
- Welten, G.M.; Schouten, O.; Hoeks, S.E.; Chonchol, M.; Vidakovic, R.; van Domburg, R.T.; Bax, J.J.; van Sambeek, M.R.H.M.; Poldermans, D. Long-Term Prognosis of Patients with Peripheral Arterial Disease: A Comparison in Patients with Coronary Artery Disease. J. Am. Coll. Cardiol 2008, 51, 1588–1596. [Google Scholar] [CrossRef] [PubMed]
- Isma, N.; Barani, J.; Mattiasson, I.; Lindblad, B.; Gottsäter, A. Lipid-Lowering Therapy Is Related to Inflammatory Markers and 3-Year Mortality in Patients With Critical Limb Ischemia. Angiology 2008, 59, 542–548. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, A.T.; Haskal, Z.J.; Hertzer, N.R.; Bakal, C.W.; Creager, M.A.; Halperin, J.L.; Hiratzka, L.F.; Murphy, W.R.C.; Olin, J.W.; Puschett, J.B.; et al. ACC/AHA 2005 Practice Guidelines for the Management of Patients with Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic). Circulation 2006, 113, e463–e654. [Google Scholar] [CrossRef]
- Leiherer, A.; Muendlein, A.; Brandtner, E.M.; Saely, C.H.; Ramadani, H.; Vonbank, A.; Mader, A.; Dopheide, J.F.; Jylhä, A.; Lääperi, M.; et al. Lipid Profiles of Patients with Manifest Coronary versus Peripheral Atherosclerosis—Is There a Difference? J. Intern. Med. 2021, 290, 1249–1263. [Google Scholar] [CrossRef]
- Canals, D.; Salamone, S.; Hannun, Y.A. Visualizing Bioactive Ceramides. Chem. Phys. Lipids 2018, 216, 142–151. [Google Scholar] [CrossRef]
- Bikman, B.T.; Summers, S.A. Ceramides as Modulators of Cellular and Whole-Body Metabolism. J. Clin. Investig. 2011, 121, 4222–4230. [Google Scholar] [CrossRef]
- Schissel, S.L.; Tweedie-Hardman, J.; Rapp, J.H.; Graham, G.; Williams, K.J.; Tabas, I. Rabbit Aorta and Human Atherosclerotic Lesions Hydrolyze the Sphingomyelin of Retained Low-Density Lipoprotein: Proposed Role for Arterial-Wall Sphingomyelinase in Subendothelial Retention and Aggregation of Atherogenic Lipoproteins. J. Clin. Investig. 1996, 98, 1455–1464. [Google Scholar] [CrossRef]
- Hilvo, M.; Simolin, H.; Metso, J.; Ruuth, M.; Öörni, K.; Jauhiainen, M.; Laaksonen, R.; Baruch, A. PCSK9 Inhibition Alters the Lipidome of Plasma and Lipoprotein Fractions. Atherosclerosis 2018, 269, 159–165. [Google Scholar] [CrossRef]
- Tarasov, K.; Ekroos, K.; Suoniemi, M.; Kauhanen, D.; Sylvänne, T.; Hurme, R.; Gouni-Berthold, I.; Berthold, H.K.; Kleber, M.E.; Laaksonen, R.; et al. Molecular Lipids Identify Cardiovascular Risk and Are Efficiently Lowered by Simvastatin and PCSK9 Deficiency. J. Clin. Endocrinol. Metab. 2014, 99, e45–e52. [Google Scholar] [CrossRef]
- Mundra, P.A.; Barlow, C.K.; Nestel, P.J.; Barnes, E.H.; Kirby, A.; Thompson, P.; Sullivan, D.R.; Alshehry, Z.H.; Mellett, N.A.; Huynh, K.; et al. Large-Scale Plasma Lipidomic Profiling Identifies Lipids That Predict Cardiovascular Events in Secondary Prevention. JCI Insight 2018, 3, e121326. [Google Scholar] [CrossRef]
- Tippetts, T.S.; Holland, W.L.; Summers, S.A. The Ceramide Ratio: A Predictor of Cardiometabolic Risk. J. Lipid Res. 2018, 59, 1549–1550. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.M.; Suoniemi, M.; Kardys, I.; Vihervaara, T.; de Boer, S.P.M.; Akkerhuis, K.M.; Sysi-Aho, M.; Ekroos, K.; Garcia-Garcia, H.M.; Oemrawsingh, R.M.; et al. Plasma Concentrations of Molecular Lipid Species in Relation to Coronary Plaque Characteristics and Cardiovascular Outcome: Results of the ATHEROREMO-IVUS Study. Atherosclerosis 2015, 243, 560–566. [Google Scholar] [CrossRef] [PubMed]
- Hilvo, M.; Meikle, P.J.; Pedersen, E.R.; Tell, G.S.; Dhar, I.; Brenner, H.; Schöttker, B.; Lääperi, M.; Kauhanen, D.; Koistinen, K.M.; et al. Development and Validation of a Ceramide- and Phospholipid-Based Cardiovascular Risk Estimation Score for Coronary Artery Disease Patients. Eur. Heart J. 2019, 41, 371–380. [Google Scholar] [CrossRef]
- Hazarika, S.; Annex, B.H. Biomarkers and Genetics in Peripheral Artery Disease. Clin. Chem. 2017, 63, 236–244. [Google Scholar] [CrossRef]
- Rutherford, R.B.; Baker, J.D.; Ernst, C.; Johnston, K.W.; Porter, J.M.; Ahn, S.; Jones, D.N. Recommended Standards for Reports Dealing with Lower Extremity Ischemia: Revised Version. J. Vasc. Surg. 1997, 26, 517–538. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Zimmet, P.Z. Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications. Part 1: Diagnosis and Classification of Diabetes Mellitus. Provisional Report of a WHO Consultation. Diabet. Med. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- Kidney Disease Outcomes Quality Initiative. KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Diabetes and Chronic Kidney Disease. Am. J. Kidney Dis. 2007, 49, S12–S154. [Google Scholar] [CrossRef]
- Laaksonen, R.; Ekroos, K.; Sysi-Aho, M.; Hilvo, M.; Vihervaara, T.; Kauhanen, D.; Suoniemi, M.; Hurme, R.; März, W.; Scharnagl, H.; et al. Plasma Ceramides Predict Cardiovascular Death in Patients with Stable Coronary Artery Disease and Acute Coronary Syndromes beyond LDL-Cholesterol. Eur. Heart J. 2016, 37, 1967–1976. [Google Scholar] [CrossRef]
- Kinoshita, M.; Matsumori, N. Inimitable Impacts of Ceramides on Lipid Rafts Formed in Artificial and Natural Cell Membranes. Membranes 2022, 12, 727. [Google Scholar] [CrossRef] [PubMed]
- Hannun, Y.A.; Obeid, L.M. Sphingolipids and Their Metabolism in Physiology and Disease. Nat. Rev. Mol. Cell Biol. 2018, 19, 175–191. [Google Scholar] [CrossRef]
- Park, T.S.; Hu, Y.; Noh, H.L.; Drosatos, K.; Okajima, K.; Buchanan, J.; Tuinei, J.; Homma, S.; Jiang, X.C.; Abel, E.D.; et al. Ceramide Is a Cardiotoxin in Lipotoxic Cardiomyopathy. J. Lipid Res. 2008, 49, 2101–2112. [Google Scholar] [CrossRef]
- Bharath, L.P.; Ruan, T.; Li, Y.; Ravindran, A.; Wan, X.; Nhan, J.K.; Walker, M.L.; Deeter, L.; Goodrich, R.; Johnson, E.; et al. Ceramide-Initiated Protein Phosphatase 2A Activation Contributes to Arterial Dysfunction In Vivo. Diabetes 2015, 64, 3914–3926. [Google Scholar] [CrossRef] [PubMed]
- Mehra, V.C.; Jackson, E.; Zhang, X.M.; Jiang, X.C.; Dobrucki, L.W.; Yu, J.; Bernatchez, P.; Sinusas, A.J.; Shulman, G.I.; Sessa, W.C.; et al. Ceramide-Activated Phosphatase Mediates Fatty Acid-Induced Endothelial VEGF Resistance and Impaired Angiogenesis. Am. J. Pathol. 2014, 184, 1562–1576. [Google Scholar] [CrossRef] [PubMed]
- Byrne, P.; Cullinan, J.; Smith, S.M. Statins for Primary Prevention of Cardiovascular Disease. BMJ 2019, 367, l5674. [Google Scholar] [CrossRef]
- Navarese, E.P.; Robinson, J.G.; Kowalewski, M.; Kołodziejczak, M.; Andreotti, F.; Bliden, K.; Tantry, U.; Kubica, J.; Raggi, P.; Gurbel, P.A. Association between Baseline LDL-C Level and Total and Cardiovascular Mortality after LDL-C Lowering a Systematic Review and Meta-Analysis. JAMA 2018, 319, 1566–1579. [Google Scholar] [CrossRef]
- Kohli-Lynch, C.N.; Bellows, B.K.; Thanassoulis, G.; Zhang, Y.; Pletcher, M.J.; Vittinghoff, E.; Pencina, M.J.; Kazi, D.; Sniderman, A.D.; Moran, A.E. Cost-Effectiveness of Low-Density Lipoprotein Cholesterol Level-Guided Statin Treatment in Patients with Borderline Cardiovascular Risk. JAMA Cardiol. 2019, 4, 969–977. [Google Scholar] [CrossRef]
- Ridker, P.M.; Bhatt, D.L.; Pradhan, A.D.; Glynn, R.J.; MacFadyen, J.G.; Nissen, S.E. Inflammation and Cholesterol as Predictors of Cardiovascular Events among Patients Receiving Statin Therapy: A Collaborative Analysis of Three Randomised Trials. Lancet 2023, 401, 1293–1301. [Google Scholar] [CrossRef]
- Johannesen, C.D.L.; Langsted, A.; Mortensen, M.B.; Nordestgaard, B.G. Association between Low Density Lipoprotein and All Cause and Cause Specific Mortality in Denmark: Prospective Cohort Study. BMJ 2020, 371, m4266. [Google Scholar] [CrossRef] [PubMed]
- Abdelhafiz, A.H.; Loo, B.E.; Hensey, N.; Bailey, C.; Sinclair, A. The U-Shaped Relationship of Traditional Cardiovascular Risk Factors and Adverse Outcomes in Later Life. Aging Dis. 2012, 3, 454–464. [Google Scholar] [PubMed]
- Summers, S.A. Could Ceramides Become the New Cholesterol? Cell Metab. 2018, 27, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Tippetts, T.S.; Holland, W.L.; Summers, S.A. Cholesterol—The Devil You Know; Ceramide—The Devil You Don’t. Trends Pharmacol. Sci. 2021, 42, 1082–1095. [Google Scholar] [CrossRef]
- Norris, G.H.; Blesso, C.N. Dietary and Endogenous Sphingolipid Metabolism in Chronic Inflammation. Nutrients 2017, 9, 1180. [Google Scholar] [CrossRef]
- Luukkonen, P.K.; Sädevirta, S.; Zhou, Y.; Kayser, B.; Ali, A.; Ahonen, L.; Lallukka, S.; Pelloux, V.; Gaggini, M.; Jian, C.; et al. Saturated Fat Is More Metabolically Harmful for the Human Liver Than Unsaturated Fat or Simple Sugars. Diabetes Care 2018, 41, 1732–1739. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.D.; Toledo, E.; Hruby, A.; Rosner, B.A.; Willett, W.C.; Sun, Q.; Razquin, C.; Zheng, Y.; Ruiz-Canela, M.; Guasch-Ferré, M.; et al. Plasma Ceramides, Mediterranean Diet, and Incident Cardiovascular Disease in the PREDIMED Trial. Circulation 2017, 135, 2028–2040. [Google Scholar] [CrossRef]
- Mathews, A.T.; Famodu, O.A.; Olfert, M.D.; Murray, P.J.; Cuff, C.F.; Downes, M.T.; Haughey, N.J.; Colby, S.E.; Chantler, P.D.; Olfert, I.M.; et al. Efficacy of Nutritional Interventions to Lower Circulating Ceramides in Young Adults: FRUVEDomic Pilot Study. Physiol. Rep. 2017, 5, e13329. [Google Scholar] [CrossRef]
- Kitatani, K.; Idkowiak-Baldys, J.; Hannun, Y.A. The Sphingolipid Salvage Pathway in Ceramide Metabolism and Signaling. Cell Signal 2008, 20, 1010–1018. [Google Scholar] [CrossRef]
- Hannun, Y.A.; Obeid, L.M. Principles of Bioactive Lipid Signalling: Lessons from Sphingolipids. Nat. Rev. Mol. Cell Biol. 2008, 9, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Ng, T.W.K.; Ooi, E.M.M.; Watts, G.F.; Chan, D.C.; Weir, J.M.; Meikle, P.J.; Barrett, P.H.R. Dose-Dependent Effects of Rosuvastatin on the Plasma Sphingolipidome and Phospholipidome in the Metabolic Syndrome. J. Clin. Endocrinol. Metab. 2014, 99, E2335–E2340. [Google Scholar] [CrossRef] [PubMed]
- Crea, F.; Niccoli, G. Ezetimibe and Plaque Regression: Cholesterol Lowering or Pleiotropic Effects? J. Am. Coll. Cardiol. 2015, 66, 508–510. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.B.; Fink, C.S.; Trautwein, E.A.; Ntanios, F.Y. β-Sitosterol Stimulates Ceramide Metabolism in Differentiated Caco2 Cells. J. Nutr. Biochem. 2005, 16, 650–655. [Google Scholar] [CrossRef]
- Croyal, M.; Kaabia, Z.; León, L.; Ramin-Mangata, S.; Baty, T.; Fall, F.; Billon-Crossouard, S.; Aguesse, A.; Hollstein, T.; Sullivan, D.R.; et al. Fenofibrate Decreases Plasma Ceramide in Type 2 Diabetes Patients: A Novel Marker of CVD? Diabetes Metab. 2018, 44, 143–149. [Google Scholar] [CrossRef]
- Das Pradhan, A.; Glynn, R.J.; Fruchart, J.-C.; MacFadyen, J.G.; Zaharris, E.S.; Everett, B.M.; Campbell, S.E.; Oshima, R.; Amarenco, P.; Blom, D.J.; et al. Triglyceride Lowering with Pemafibrate to Reduce Cardiovascular Risk. N. Engl. J. Med 2022, 387, 1923–1934. [Google Scholar] [CrossRef]
- Song, J.-H.; Kim, G.-T.; Park, K.-H.; Park, W.-J.; Park, T.-S. Bioactive Sphingolipids as Major Regulators of Coronary Artery Disease. Biomol. Ther. 2021, 29, 373–383. [Google Scholar] [CrossRef]
- Yin, D.; Matsumura, M.; Rundback, J.; Yoho, J.A.; Witzenbichler, B.; Stone, G.W.; Mintz, G.S.; Maehara, A. Comparison of Plaque Morphology between Peripheral and Coronary Artery Disease (from the CLARITY and ADAPT-DES IVUS Substudies). Coron. Artery Dis 2017, 28, 369–375. [Google Scholar] [CrossRef]
- Eurostat Mortality and Life Expectancy Statistics—Statistics Explained. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Mortality_and_life_expectancy_statistics (accessed on 30 March 2023).
| Total Cohort (n = 379) | Category 1 (Low Risk, n = 116) | Category 2 (Moderate Risk, n = 140) | Category 3 (High Risk, n = 77) | Category 4 (Very High Risk, n = 46) | p-Value | |
|---|---|---|---|---|---|---|
| Age, years | 67 [60–74] | 65 [57–74] | 67 [60–74] | 70 [64–75] | 71 [62–76] | 0.007 |
| Male sex, % (n) | 72 (273) | 73 (85) | 75 (105) | 73 (56) | 59 (27) | 0.127 |
| Current smokers, % (n) | 31 (89) | 34 (24) | 29 (32) | 30 (20) | 33 (13) | 0.793 |
| Ever smokers, % (n) | 84 (317) | 82 (95) | 85 (119) | 84 (65) | 83 (38) | 0.815 |
| Body mass index, kg/m2 | 26 [24–30] | 26 [24–30] | 26 [24–30] | 27 [24–30] | 26 [23–31] | 0.670 |
| Creatinine, mg/dL | 0.90 [0.77–1.05] | 0.90 [0.79–1.00] | 0.87 [0.77–1.00] | 0.90 [0.70–1.15] | 0.95 [0.72–1.26] | 0.166 |
| Hypertension, % (n) | 94 (356) | 93 (108) | 97 (136) | 88 (68) | 96 (44) | 0.698 |
| T2DM, % (n) | 40 (150) | 38 (44) | 34 (47) | 43 (33) | 57 (26) | 0.033 |
| CKD % (n) | 20 (75) | 16 (18) | 15 (21) | 25 (19) | 37 (17) | 0.001 |
| LDL-cholesterol, mg/dL | 102 [81–125] | 96 [83–119] | 105 [81–126] | 111 [79–149] | 92 [76–114] | 0.716 |
| Statin use at baseline, % (n) | 70 (266) | 78 (91) | 66 (92) | 62 (48) | 76 (35) | 0.247 |
| Rutherford score | 2 [1–3] | 2 [1–3] | 1 [0–3] | 3 [1–3] | 3 [1–4] | 0.006 |
| Ankle–brachial index | 1.0 [0.8–1.2] | 1.0 [0.9–1.2] | 1.0 [0.9–1.2] | 1.0 [0.8–1.1] | 0.9 [0.7–1.1] | 0.047 |
| Overall Mortality | Cardiovascular Mortality | MACE | |||||
|---|---|---|---|---|---|---|---|
| HR [IQR] | p | HR [IQR] | p | HR [IQR] | p | ||
| CERT categories (4 steps) | Model 1 | 1.351 [1.157–1.578] | <0.001 | 1.427 [1.123–1.812] | 0.004 | 1.255 [1.062–1.482] | 0.008 |
| Model 2 | 1.259 [1.074–1.476] | 0.005 | 1.349 [1.055–1.726] | 0.017 | 1.225 [1.033–1.452] | 0.020 | |
| Model 3 | 1.265 [1.079–1.484] | 0.004 | 1.360 [1.062–1.741] | 0.015 | 1.221 [1.026–1.452] | 0.024 | |
| Model 4 | 1.215 [1.035–1.427] | 0.017 | 1.304 [1.018–1.670] | 0.035 | 1.167 [0.981–1.388] | 0.081 | |
| CERT (13 steps) | Model 1 | 1.089 [1.040–1.140] | <0.001 | 1.124 [1.046–1.207] | 0.001 | 1.062 [1.010–1.117] | 0.019 |
| Model 2 | 1.067 [1.019–1.118] | 0.006 | 1.105 [1.027–1.188] | 0.007 | 1.065 [1.013–1.119] | 0.014 | |
| Model 3 | 1.068 [1.019–1.120] | 0.006 | 1.105 [1.027–1.188] | 0.008 | 1.062 [1.010–1.117] | 0.019 | |
| Model 4 | 1.055 [1.007–1.106] | 0.024 | 1.090 [1.014–1.172] | 0.020 | 1.049 [0.998–1.103] | 0.061 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leiherer, A.; Muendlein, A.; Saely, C.H.; Geiger, K.; Brandtner, E.-M.; Heinzle, C.; Gaenger, S.; Mink, S.; Laaksonen, R.; Fraunberger, P.; et al. Coronary Event Risk Test (CERT) as a Risk Predictor for the 10-Year Clinical Outcome of Patients with Peripheral Artery Disease. J. Clin. Med. 2023, 12, 6151. https://doi.org/10.3390/jcm12196151
Leiherer A, Muendlein A, Saely CH, Geiger K, Brandtner E-M, Heinzle C, Gaenger S, Mink S, Laaksonen R, Fraunberger P, et al. Coronary Event Risk Test (CERT) as a Risk Predictor for the 10-Year Clinical Outcome of Patients with Peripheral Artery Disease. Journal of Clinical Medicine. 2023; 12(19):6151. https://doi.org/10.3390/jcm12196151
Chicago/Turabian StyleLeiherer, Andreas, Axel Muendlein, Christoph H. Saely, Kathrin Geiger, Eva-Maria Brandtner, Christine Heinzle, Stella Gaenger, Sylvia Mink, Reijo Laaksonen, Peter Fraunberger, and et al. 2023. "Coronary Event Risk Test (CERT) as a Risk Predictor for the 10-Year Clinical Outcome of Patients with Peripheral Artery Disease" Journal of Clinical Medicine 12, no. 19: 6151. https://doi.org/10.3390/jcm12196151






