Prospective Evaluation of Children with Robin Sequence following Tübingen Palatal Plate Therapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
- (1)
- Group of children with RS: successful TPP therapy initiated after birth;
- (2)
- Control group: no congenital malformation or chromosomal aberration;
- (3)
- Born between 1 January 2008 and 31 December 2012.
- (1)
- Missing parental consent or participant’s assent;
- (2)
- Group of children with RS: not treated with the TPP or receiving additional invasive treatments (i.e., tracheostomy);
- (3)
- Control group: craniofacial malformation, obstructive sleep apnea and other syndromes.
2.3. Instruments
2.4. Statistical Data Analysis
3. Results
3.1. Characteristics of the Study Participants
3.2. Orthodontic History
3.3. Facial Soft Tissue Analysis of 2D Images
3.4. Digital Casts Analysis
3.5. Skeletal Cephalometric Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Robin, P. A fall of the base of the tongue considered as a new cause of nasopharyngeal respiratory impairment: Pierre Robin sequence, a translation. 1923. Plast. Reconstr. Surg. 1994, 93, 1301–1303. [Google Scholar] [PubMed]
- Vatlach, S.; Maas, C.; Poets, C.F. Birth prevalence and initial treatment of Robin sequence in Germany: A prospective epidemiologic study. Orphanet J. Rare Dis. 2014, 9, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Printzlau, A.; Andersen, M. Pierre Robin sequence in Denmark: A retrospective population-based epidemiological study. Cleft Palate Craniofac. J. 2004, 41, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Côté, A.; Fanous, A.; Almajed, A.; Lacroix, Y. Pierre Robin sequence: Review of diagnostic and treatment challenges. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 451–464. [Google Scholar] [CrossRef] [PubMed]
- Santoro, M.; Coi, A.; Barišić, I.; Pierini, A.; Addor, M.C.; Baldacci, S.; Ballardini, E.; Boban, L.; Braz, P.; Cavero-Carbonell, C.; et al. Epidemiology of Pierre-Robin sequence in Europe: A population-based EUROCAT study. Paediatr. Perinat. Epidemiol. 2021, 35, 530–539. [Google Scholar] [CrossRef]
- Evans, K.N.; Sie, K.C.; Hopper, R.A.; Glass, R.P.; Hing, A.V.; Cunningham, M.L. Robin sequence: From diagnosis to development of an effective management plan. Pediatrics 2011, 127, 936–948. [Google Scholar] [CrossRef] [Green Version]
- van Lieshout, M.J.; Joosten, K.F.; Mathijssen, I.M.; Koudstaal, M.J.; Hoeve, H.L.; van der Schroeff, M.P.; Wolvius, E.B. Robin sequence: A European survey on current practice patterns. J. Cranio Maxillofac. Surg. 2015, 43, 1626–1631. [Google Scholar] [CrossRef]
- Paes, E.C.; Bittermann, G.K.P.; Bittermann, D.; Muradin, M.M.; Van Hogezand, R.; Etty, E.; van der Molen, A.B.M.; Kon, M.; Breugem, C.C. Long-Term Results of Mandibular Distraction Osteogenesis with a Resorbable Device in Infants with Robin Sequence: Effects on Developing Molars and Mandibular Growth. Plast. Reconstr. Surg. 2016, 137, 375e–385e. [Google Scholar] [CrossRef]
- Buchenau, W.; Urschitz, M.S.; Sautermeister, J.; Bacher, M.; Herberts, T.; Arand, J.; Poets, C.F. A randomized clinical trial of a new orthodontic appliance to improve upper airway obstruction in infants with Pierre Robin sequence. J. Pediatr. 2007, 151, 145–149. [Google Scholar] [CrossRef]
- Poets, C.F.; Maas, C.; Buchenau, W.; Arand, J.; Vierzig, A.; Braumann, B.; Müller-Hagedorn, S. Multicenter study on the effectiveness of the pre-epiglottic baton plate for airway obstruction and feeding problems in Robin sequence. Orphanet J. Rare Dis. 2017, 12, 46. [Google Scholar] [CrossRef]
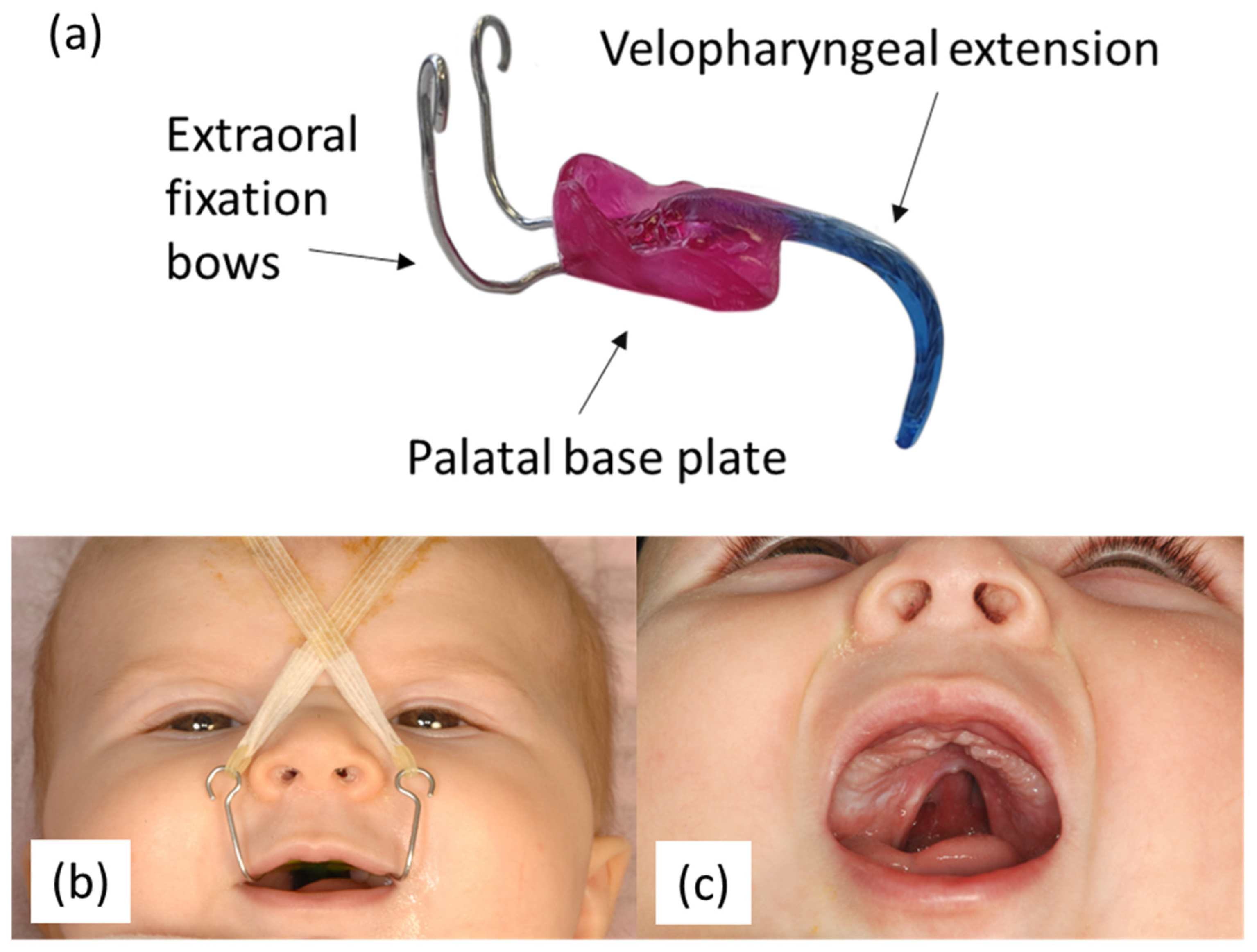
- Wiechers, C.; Arand, J.; Koos, B.; Poets, C.F. Evidence and practical aspects of treatment with the Tübingen palatal plate. Semin. Fetal Neonatal Med. 2021, 26, 101281. [Google Scholar] [CrossRef]
- Poets, C.F.; Koos, B.; Reinert, S.; Wiechers, C. The Tübingen palatal plate approach to Robin sequence: Summary of current evidence. J. Cranio Maxillofac. Surg. 2019, 47, 1699–1705. [Google Scholar] [CrossRef] [PubMed]
- Poets, C.F.; Wiechers, C.; Koos, B.; Muzaffar, A.R.; Gozal, D. Pierre Robin and breathing: What to do and when? Pediatr. Pulmonol. 2022, 57, 1887–1896. [Google Scholar] [CrossRef] [PubMed]
- Wiechers, C.; Iffländer, R.; Gerdes, R.; Ciuffolotti, M.; Arand, J.; Weise, C.; Peters, K.; Grandke, B.; Reinert, S.; Koos, B.; et al. Retrospective study on growth in infants with isolated Robin sequence treated with the Tuebingen Palate Plate. Orphanet J. Rare Dis. 2021, 16, 338. [Google Scholar] [CrossRef]
- Bacher, M.; Sautermeister, J.; Urschitz, M.S.; Buchenau, W.; Arand, J.; Poets, C.F. An Oral Appliance with Velar Extension for Treatment of Obstructive Sleep Apnea in Infants with Pierre Robin Sequence. Cleft Palate Craniofac. J. 2011, 48, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Weise, C.; Frank, K.; Wiechers, C.; Weise, H.; Reinert, S.; Koos, B.; Xepapadeas, A.B. Intraoral scanning of neonates and infants with craniofacial disorders: Feasibility, scanning duration, and clinical experience. Eur. J. Orthod. 2022, 44, 279–286. [Google Scholar] [CrossRef]
- Aretxabaleta, M.; Xepapadeas, A.B.; Poets, C.F.; Koos, B.; Spintzyk, S. Fracture Load of an Orthodontic Appliance for Robin Sequence Treatment in a Digital Workflow. Materials 2021, 14, 344. [Google Scholar] [CrossRef]
- Xepapadeas, A.B.; Weise, C.; Frank, K.; Spintzyk, S.; Poets, C.F.; Wiechers, C.; Arand, J.; Koos, B. Technical note on introducing a digital workflow for newborns with craniofacial anomalies based on intraoral scans—Part II: 3D printed Tübingen palatal plate prototype for newborns with Robin sequence. BMC Oral Health 2020, 20, 171. [Google Scholar] [CrossRef]
- Purnell, C.A.; Janes, L.E.; Klosowiak, J.L.; Gosain, A.K. Mandibular Catch-Up Growth in Pierre Robin Sequence: A Systematic Review. Cleft Palate-Craniofac. J. 2019, 56, 168–176. [Google Scholar] [CrossRef]
- Hotz, M.; Gnoinski, W. Clefts of the secondary palate associated with the “Pierre Robin syndrome”. Management by early maxillary orthopaedics. Swed. Dent. J. Suppl. 1982, 15, 89–98. [Google Scholar]
- Pruzansky, S.; Richmond, J.B. Growth of mandible in infants with micrognathia; clinical implications. AMA Am. J. Dis. Child. 1954, 88, 29–42. [Google Scholar] [PubMed]
- Pruzansky, S. Not all dwarfed mandibles are alike. Birth Defects 1969, 5, 120–129. [Google Scholar]
- Daskalogiannakis, J.; Ross, R.B.; Tompson, B.D. The mandibular catch-up growth controversy in Pierre Robin sequence. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 280–285. [Google Scholar] [CrossRef]
- Rogers, G.; Lim, A.A.; Mulliken, J.B.; Padwa, B.L. Effect of a Syndromic Diagnosis on Mandibular Size and Sagittal Position in Robin Sequence. J. Oral Maxillofac. Surg. 2009, 67, 2323–2331. [Google Scholar] [CrossRef] [PubMed]
- Mackay, D.R. Controversies in the Diagnosis and Management of the Robin Sequence. J. Craniofac. Surg. 2011, 22, 415–420. [Google Scholar] [CrossRef]
- Suri, S.; Ross, R.B.; Tompson, B.D. Craniofacial morphology and adolescent facial growth in Pierre Robin sequence. Am. J. Orthod Dentofac. Orthop. 2010, 137, 763–774. [Google Scholar] [CrossRef]
- Laitinen, S.H.; Ranta, R.E. Cephalometric measurements in patients with Pierre Robin syndrome and isolated cleft palate. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1992, 26, 177–183. [Google Scholar] [CrossRef]
- Hermann, N.V.; Darvann, T.A.; Ersbøll, B.K.; Kreiborg, S. Short mandible—A possible risk factor for cleft palate with/without a cleft lip. Orthod. Craniofac. Res. 2014, 17, 106–114. [Google Scholar] [CrossRef]
- Hermann, N.V.; Kreiborg, S.; Darvann, T.A.; Jensen, B.L.; Dahl, E.; Bolund, S. Early Craniofacial Morphology and Growth in Children with Unoperated Isolated Cleft Palate. Cleft Palate Craniofac. J. 2002, 39, 604–622. [Google Scholar] [CrossRef]
- Matsuda, A.; Suda, N.; Motohashi, N.; Tsuji, M.; Ohyama, K. Skeletal characteristics and treatment outcome of five patients with Robin sequence. Angle Orthod. 2006, 76, 898–908. [Google Scholar] [CrossRef]
- Figueroa, A.A.; Glupker, T.J.; Fitz, M.G.; BeGole, E.A. Mandible, tongue, and airway in Pierre Robin sequence: A longitudinal cephalometric study. Cleft Palate Craniofac. J. 1991, 28, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Krimmel, M.; Kluba, S.; Breidt, M.; Bacher, M.; Müller-Hagedorn, S.; Dietz, K.; Bülthoff, H.; Reinert, S. Three-Dimensional Assessment of Facial Development in Children with Unilateral Cleft Lip with and without Alveolar Cleft. J. Craniofac. Surg. 2013, 24, 313–316. [Google Scholar] [CrossRef] [PubMed]
- Angle, E.H. Classification of malocclusion. Dent. Cosm. 1899, 41, 350–357. [Google Scholar]
- American Board of Orthodontics. Photograph Requirements. Available online: https://ntiiiby.americanboardortho.com/media/krgfhpdg/example-photos-radiographs.pdf (accessed on 1 November 2022).
- van der Haven, I.; Mulder, J.W.; van der Wal, K.G.; Hage, J.J.; de Lange-de Klerk, E.S.; Haumann, T.J. The jaw index: New guide defining micrognathia in newborns. Cleft Palate Craniofac. J. 1997, 34, 240–241. [Google Scholar] [CrossRef] [PubMed]
- Rakosi, T.J.I. Kieferorthopädie Diagnostik; Georg Thieme Verlag: Stuttgart, Germany, 1989. [Google Scholar]
- Ricketts, R.M. Divine proportion in facial esthetics. Clin. Plast. Surg. 1982, 9, 401–422. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, A.M. Röntgenstatik; Urban & Schwarzenberg: München, Germany, 1958. [Google Scholar]
- Moyers, R.E. Handbook of Orthodontics, 4th ed.; Year Book Medical Publishers: Chicago, IL, USA, 1988. [Google Scholar]
- Harth, G. Biometrische Untersuchungen Über die Dimensionen des Normalgebisses in Verschiedenen Lebensaltern: Intramaxilläre Beziehgn. Dtsch. Mschr. Zahnheilk. 1930, 48, 1537–1563. [Google Scholar]
- Rose, E.; Thissen, U.; Otten, J.-E.; Jonas, I. Cephalometric Assessment of the Posterior Airway Space in Patients with Cleft Palate after Palatoplasty. Cleft Palate Craniofacial J. 2003, 40, 498–503. [Google Scholar] [CrossRef] [PubMed]
- Segner, D.; Hasund, A. Individualisierte Kephalometrie, 4th ed.; unveränd. Aufl.; Segner: Hamburg, Germany, 2003. [Google Scholar]
- Fischer-Brandies, H.; Stahl, A.N.F. Kieferorthopädische Technik: Mit Hinweisen auf Indikation und Klinik; Georg Thieme Verlag: Stuttgart, Germany, 1990. [Google Scholar]
- Müller-Hagedorn, S.; Koos, B. Das pädiatrische obstruktive Schlafapnoesyndrom. Somnologie 2016, 20, 297–308. [Google Scholar] [CrossRef]
- Ozawa, T.O.; Lorenzoni, D.C.; de Oliveira, L.G.F.; Da Filho, O.G.S. Facial Profile Evaluation of Isolated Pierre Robin Sequence. Cleft Palate Craniofac. J. 2012, 49, 546–552. [Google Scholar] [CrossRef]
- Suri, S.; Ross, R.B.; Tompson, B.D. Mandibular morphology and growth with and without hypodontia in subjects with Pierre Robin sequence. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 37–46. [Google Scholar] [CrossRef]
- Laitinen, S.H.; Heliövaara, A.; Ranta, R.E. Craniofacial morphology in young adults with the Pierre Robin sequence and isolated cleft palate. Acta Odontol. Scand. 1997, 55, 223–228. [Google Scholar] [CrossRef]
- Enlow, D.H. A morphogenetic analysis of facial growth. Am. J. Orthod. 1966, 52, 283–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Enlow, D.H. Facial Growth, 3rd ed.; Saunders: Philadelphia, PA, USA, 1990. [Google Scholar]
- Limbrock, G.J.; Castillo-Morales, R.; Hoyer, H.; Stöver, B.; Onufer, C.N. The Castillo-Morales approach to orofacial pathology in Down syndrome. Int. J. Orofac. Myol. 1993, 19, 30–37. [Google Scholar] [CrossRef]
- Paladini, D.; Morra, T.; Teodoro, A.; Lamberti, A.; Tremolaterra, F.; Martinelli, P. Objective diagnosis of micrognathia in the fetus: The jaw index. Obstet. Gynecol. 1999, 93, 382–386. [Google Scholar] [CrossRef]
- Mermans, J.F.; Ghasemi, S.M.; Lissenberg-Witte, B.I.; Don Griot, J.P.W. The Reproducibility of the Jaw Index in the Measurement of Healthy Newborns. Cleft Palate Craniofac. J. 2020, 57, 574–580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vegter, F.; Hage, J.J.; Mulder, J.W. Pierre Robin syndrome: Mandibular growth during the first year of life. Ann. Plast. Surg. 1999, 42, 154–157. [Google Scholar]
- Wiechers, C.; Buchenau, W.; Arand, J.; Oertel, A.F.; Peters, K.; Müller-Hagedorn, S.; Koos, B.; Poets, C.F. Mandibular growth in infants with Robin sequence treated with the Tübingen palatal plate. Head Face Med. 2019, 15, 17. [Google Scholar] [CrossRef]
- Eriksen, J.; Hermann, N.V.; Darvann, T.A.; Kreiborg, S. Early postnatal development of the mandible in children with isolated cleft palate and children with nonsyndromic Robin sequence. Cleft Palate Craniofac. J. 2006, 43, 160–167. [Google Scholar] [CrossRef]
- Murage, K.P.; Costa, M.A.; Friel, M.T.; Havlik, R.J.; Tholpady, S.S.; Flores, R.L. Complications Associated with Neonatal Mandibular Distraction Osteogenesis in the Treatment of Robin Sequence. J. Craniofac. Surg. 2014, 25, 383–387. [Google Scholar] [CrossRef]
- Ow, A.; Cheung, L.K. Skeletal Stability and Complications of Bilateral Sagittal Split Osteotomies and Mandibular Distraction Osteogenesis: An Evidence-Based Review. J. Oral Maxillofac. Surg. 2009, 67, 2344–2353. [Google Scholar] [CrossRef]
- Salzmann, J.A. Orthodontics in Daily Practice; J.B. Lippincott & Co.: Philadelphia, PA, USA, 1974. [Google Scholar]

| 1 | Orthodontic anamnesis examination |
|
| 2 | Jaw Index [35] |
|
| 3 | 2D facial profile analysis with photostat lateral images |
|
| 4 | Dental digital casts analysis | |
| 5 | Cephalometric measurements |
| Measurement | Children with RSs | Healthy Controls | Difference | Chi2 | Prob > Chi² |
|---|---|---|---|---|---|
| % | % | Healthy—RS | |||
| Mentalis muscle activity | [n = 17] | [n = 19] | 3.18 | 0.07 | |
| Normal balanced | 64.7 | 89.5 | 24.8 | ||
| Hyperactive | 35.3 | 10.5 | −24.8 | ||
| Lip position | [n = 14] | [n = 19] | 2.89 | 0.09 | |
| Competent | 85.7 | 100.0 | 14.3 | ||
| Incompetent | 14.3 | 00.0 | −14.3 | ||
| Posture | [n = 14] | [n = 19] | 0.06 | 0.80 | |
| Physiological | 13.3 | 10.5 | −2.8 | ||
| Hypotonic | 86.7 | 89.5 | 2.8 | ||
| Habits | [n = 13] | [n = 19] | 0.88 | 0.35 | |
| Yes | 30.8 | 52.6 | 21.9 | ||
| No | 69.2 | 47.4 | −21.9 | ||
| Stage of dentition | [n = 15] | [n = 19] | 2.41 | 0.49 | |
| Mixed early | 26.7 | 21.0 | −5.6 | ||
| Rest period | 13.3 | 36.8 | 23.5 | ||
| Mixed late | 53.3 | 36.8 | −16.5 | ||
| Early permanent | 06.7 | 05.3 | −1.4 | ||
| Angle Occlusion left-side | [n = 15] | [n = 20] | 1.52 | 0.68 | |
| Class I | 28.6 | 45.0 | 16.4 | ||
| Class II | 57.1 | 50.0 | 7.1 | ||
| Class III | 14.3 | 5.0 | −9.3 | ||
| Angle Occlusion right-side | [n = 15] | [n = 20] | 0.22 | 0.97 | |
| Class I | 38.5 | 40.0 | 1.5 | ||
| Class II | 53.8 | 55.0 | 1.2 | ||
| Class III | 7.7 | 5.0 | −2.7 | ||
| Midline shift | [n = 17] | [n = 20] | |||
| Upper—dental | 0.08 | 0.77 | |||
| Matching to the midline | 40.5 | 45.9 | 5.4 | ||
| Deviation < 5mm | 5.4 | 8.1 | 2.7 | ||
| Deviation > 5mm | 0.0 | 0.0 | 0.0 | ||
| Lower—dental | 1.35 | 0.51 | |||
| Coincident | 18.9 | 27.0 | 8.1 | ||
| Deviation < 5mm | 24.2 | 27.0 | 2.8 | ||
| Deviation > 5mm | 2.7 | 0.0 | −2.7 | ||
| Lower—mandibular | 0.11 | 0.74 | |||
| Coincident | 85.7 | 89.5 | 3.7 | ||
| Deviation < 5mm | 14.3 | 10.5 | −3.8 | ||
| Deviation > 5mm | 0.00 | 0.0 | 0.0 | ||
| Phoniation | [n = 14] | [n = 19] | 2.20 | 0.33 | |
| Normal | 85.7 | 84.2 | −1.5 | ||
| Interdental | 14.3 | 05.3 | 61.0 | ||
| Nasal | 00.0 | 10.5 | −10.5 | ||
| Airway exam tonsils | [n = 14] | [n = 19] | 1.44 | 0.49 | |
| Normal | 60.0 | 57.9 | −2.1 | ||
| Small | 6.7 | 0.0 | −6.7 | ||
| Enlarged | 33.3 | 42.1 | 8.8 | ||
| Swallowing patterns | [n = 14] | [n = 19] | 0.03 | 0.85 | |
| Somatic | 71.4 | 68.4 | −3.0 | ||
| Visceral | 28.6 | 31.6 | 3.0 | ||
| Tongue position | [n = 14] | [n = 19] | 0.11 | 0.75 | |
| Regular | 78.6 | 73.7 | −4.9 | ||
| Deep | 21.4 | 26.32 | 4.9 | ||
| TMJ Check | [n = 19] | [n = 19] | 7.13 | <0.01 * | |
| Conspicuous | 31.6 | 00.0 | −31.6 | ||
| Inconspicuous | 68.4 | 100.0 | 31.6 | ||
| Breathing | [n = 15] | [n = 19] | 5.99 | 0.05 | |
| Nose breathing | 60.0 | 73.7 | |||
| Mouth breathing | 13.3 | 26.3 | |||
| Snoring | 26.7 | 0.0 | |||
| Median (range) | Median (range) | p-value | |||
| Overjet (mm) | 4 (2–10) [n = 17] | 3 (0–9) [n = 20] | 0.01 * | ||
| Overbite (mm) | 4.25 (2–6) [n = 16] | 3 (−3–6) [n = 19] | 0.07 | ||
| Mouth opening distance incisors (mm) | 36 (28–51) [n = 16] | 44 (36–55) [n = 12] | 0.01 * | ||
| Jaw Index | 4.15 (1.87–9.55) [n = 16] | 2.98 (0–8.96) [n = 20] | 0.02 * | ||
| Measurement | Children with RS [n = 21] | Healthy Controls [n = 22] | p-Value |
|---|---|---|---|
| Median (range) | Median (range) | ||
| Profile angle (SnPog’-Pn [10°]) | 23 (14–29) | 11.00 (9–23) | <0.001 * |
| Facial convexity angle (Gl’-Sn-Pog’ [167.0 ± 5.4°]) | 157 (149–173) | 159.00 (149–170) | 0.01 * |
| Merrifield z-angle (71.8°) | 62.1 (42–82.3) | 71.30 (60.4–84.4) | <0.001 * |
| Nasolabialangle (Cotg-Sn-Ls [106.5°]) | 112.6 (100–132.3) | 114.5 (102.7–138.4) | 0.90 |
| Angle of the lowerface (Sn-Tra-Me’ [44.8 ± 3.1°]) | 39.6 (28.8–48.9) | 35.8 (31.7–39.5) | 0.01 * |
| Angle of the midface (N’-Tra-Sn [28.2 ± 2.6°]) | 27.1 (21.5–31.5) | 25.5 (19.6–30) | 0.01 * |
| Relation between higher/lower face (Tri-NR/NL:NR/NL-f-Me [161.80%]) | 157.5 147.1–211.8) | 168.3 (147.3–193.2) | 0.26 |
| Relation between mid-/lowerface (f-Gl-Sub: Sub-f-Me [100%]) | 100 (84–147) | 100 (90–110) | 0.86 |
| Relation between length and width of the face (TH-F-Me: WR-WL [161.80%]) | 155.5 (145.8–175.9) | 162.55 (146.4–182.5) | 0.14 |
| Chin angle (GoL-f-Me-GoR [66%]) | 111 (98–131) | 111 (97–124) | 0.97 |
| Measurement | Children with RS [n = 21] | Healthy Controls [n = 22] | p-Value |
|---|---|---|---|
| Median (range) | Median (range) | ||
| Moyers analysis | |||
| Si LJ (mm) | 22.9 (20.3–24.2) | 23.2 (19.3–25.7) | 0.32 |
| SI UJ (mm) | 30.00 (22.9–34) | 30.2 (25.7–35.6) | 0.85 |
| Tonn Index UJ/LJ (%) | 72.5 (69–80) | 76 (66–90) | 0.03 * |
| Discrepancy Z1Q (mm) | −0.35 (−6.3–2.4) | −0.2 (−20.8–3.9) | 0.65 |
| Discrepancy Z2Q (mm) | 0 (−3.4–4.2) | 0.2 (−2.4–2.3) | 0.39 |
| Discrepancy Z4Q (mm) | 0.5 (−5.2–2.5) | 0.6 (−7.5–3.4) | 0.53 |
| Discrepancy Z3Q (mm) | −0.95 (−11–3.5) | 0.55 (−0.8–2.31) | 0.19 |
| Harth analysis | |||
| AAWUJ (mm) | 36 (32–40) | 36 (32–40) | 0.53 |
| AAWLJ (mm) | 35 (31–39) | 36 (31–47) | 0.57 |
| PAWUJ (mm) | 48 (42–55) | 46 (35–51) | 0.01 * |
| PAWLJ (mm) | 48 (36–55) | 49 (42–56) | 0.36 |
| Measurement | Children with RS [n = 11] | Healthy Controls [n = 6] |
|---|---|---|
| Median (range) | Median (range) | |
| PAS (mm) | ||
| Maxilla plane (20 mm) | 12.5 (6.2–18.4) | 17.05 (9.2–22.3) |
| Occlusal plane (9 mm) | 8 (3–14) | 7.5 (6–10) |
| Mandibular plane (13 mm) | 11 (4–12) | 9 (5–13) |
| Hasund analysis | ||
| SNA (82 ± 3°) | 77 (70.6–82.4) | 80.5 (76.6–82.3) |
| SNB (80 ± 3°) | 73.8 (63–80.7) | 75.9 (67.3–79) |
| ANB (2.0 ± 2°) | 4.8 (1–8.7) | 4.9 (1.4–9.7) |
| Indiv. ANB | 3.3 (1.4–7.4) | 4.1 (0.9–6.8) |
| SN-Pg (82 ± 3°) | 68.8 (62.4–77.9) | 77.4 (66.6–79.8) |
| NS-Ba (130 ± 6°) | 128.7 (113.3–135.38) | 127.3 (122.1–139.2) |
| Ar-Go-Gn (126 ± 10°) | 131.6 (118–142.4) | 126.9 (120.3–143.8) |
| Holdaway angle (9.2°) | 15.9 (5.8–24.7) | 15.2 (6.7–24.1) |
| Interincisal angle 1-1 (131 ± 6°) | 144.2 (125.2–161.7) | 129.7 (116.4–140.7) |
| Nasolabial angle (109.8°) | 103.1 (94–121.5) | 106.7 (97.5–124.1) |
| OK1-NA (22.0 ± 3°) | 15.8 (6.3–26.1) | 19 (13.4–39.1) |
| UK1-NB (25.0 ± 3°) | 15.2 (5.2–29.5) | 23.6 (14.7–29.8) |
| OK1O-NA (4.0 ± 2 mm) | 0.7 (−3.6–4) | 1 (−2.1–4.6) |
| UK1O-NB (4.0 ± 2 mm) | 0.6 (−1.6–7) | 5.3 (0.3–6.8) |
| ML-NSL (32.0 ± 6°) | 37.9 (20.9–69.1) | 33.1 (25.3–48.7) |
| NL-NSL (8.5 ± 3°) | 14.5 (6.1–22.1) | 6.4 (4.2–19.7) |
| ML-NL (23.5 ± 3°) | 23.9 (14.8–50.4) | 26.5 (16.1–38) |
| Hasund Index (N-Sp’/Sp’-Gn [80.1%]) | 78.3 (69.9–84.8) | 81.2 (65.9–89.3) |
| Tübingen analysis | ||
| Wits appraisal (-0.3 ± 0.3 mm) | 0.9 (−4.7–5.6) | 2.6 (−0.6–4) |
| Mandibulary length (Go-Pog’ [75.7 mm]) | 69.9 (51.4–78.9) | 76.9 (74.7–83.7) |
| Posterior mandibular body height (Go-Cond’ [54.2 mm]) | 51.3 (41.9–63.5) | 52.2 (44.8–56) |
| Maxillary length (Spp-A’ [63.4 mm]) | 62.05 (51.7–70.4) | 63.4 (61.7–69.2) |
| S-Go: N-Me (63,5 ± 1.5%) | 62.1 (39.1–71.5) | 64.8 (52.7–73.1) |
| NSpP: SpPMe (79.5%) | 78 (70.1–83.7) | 81.15 (67–88.4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Effert, J.; Uhlig, S.; Wiechers, C.; Quante, M.; Poets, C.F.; Schulz, M.C.; Reinert, S.; Krimmel, M.; Koos, B.; Weise, C. Prospective Evaluation of Children with Robin Sequence following Tübingen Palatal Plate Therapy. J. Clin. Med. 2023, 12, 448. https://doi.org/10.3390/jcm12020448
Effert J, Uhlig S, Wiechers C, Quante M, Poets CF, Schulz MC, Reinert S, Krimmel M, Koos B, Weise C. Prospective Evaluation of Children with Robin Sequence following Tübingen Palatal Plate Therapy. Journal of Clinical Medicine. 2023; 12(2):448. https://doi.org/10.3390/jcm12020448
Chicago/Turabian StyleEffert, Josephine, Simone Uhlig, Cornelia Wiechers, Mirja Quante, Christian F. Poets, Matthias C. Schulz, Siegmar Reinert, Michael Krimmel, Bernd Koos, and Christina Weise. 2023. "Prospective Evaluation of Children with Robin Sequence following Tübingen Palatal Plate Therapy" Journal of Clinical Medicine 12, no. 2: 448. https://doi.org/10.3390/jcm12020448
APA StyleEffert, J., Uhlig, S., Wiechers, C., Quante, M., Poets, C. F., Schulz, M. C., Reinert, S., Krimmel, M., Koos, B., & Weise, C. (2023). Prospective Evaluation of Children with Robin Sequence following Tübingen Palatal Plate Therapy. Journal of Clinical Medicine, 12(2), 448. https://doi.org/10.3390/jcm12020448







