Abstract
Social support is an important determinant of a carer’s mental health. In recent decades, despite many studies reporting on the relationship between social support and depressive symptoms in informal caregivers of adult and older dependents, there are no systematic reviews synthesizing the available evidence. The purpose of the present study was to perform a systematic review and meta-analysis on the relationship between social support and depressive symptoms in informal caregivers of adults and older dependent people. We searched PubMed, CINAHL (EBSCO), PsycINFO (ProQuest), and Scopus, up to 15 January 2023 for studies. We applied no date or language limits to our search. A random-effects model was used to pool effect estimates. The included studies were also independently assessed for quality. Publication bias was evaluated by funnel plots, Egger’s regression test, and the Trim and Fill method. Ninety-three studies were included in the review, reporting on a total of 15,431 informal caregivers. We found a moderate negative association between perceived social support and caregiver depressive symptoms (78 studies; r = −0.35, 95% CI = −0.39, −0.31; low heterogeneity and low risk of publications bias) and a small negative association between received social support and caregiver self-reported depressive symptoms (12 studies; r = −0.14, 95% CI = −0.20, −0.07; low heterogeneity and low risk of publications bias). Our results indicate that social support is a clinically relevant construct for carer well-being and an important protective factor for depressive symptoms in informal caregivers of adult and older dependents.
1. Introduction
According to the World Health Organization (WHO), one in six people experience some form of disability, which represents 16% of the world’s population [1]. In Europe, over 135 million people currently live with some form of disability associated with a chronic disease that causes dependency, a figure that is expected to increase due to the increased longevity of populations [1].
In this context, the main source of care for people living with dependency is usually support provided by family members [2]. Informal care is defined as the support and care offered by relatives, friends, or other people providing unpaid care to dependents in their immediate social network [3]. Providing unpaid care has a series of negative consequences on the physical and psychological health of informal caregivers, as well as in the social and economic spheres. The most frequent consequences are experiencing emotional distress, higher levels of subjective caregiver overload, and clinically significant anxiety and depression [4]. It is currently estimated that depression is one of the most frequent adverse consequences of providing care, being present in more than 42% of informal caregivers [5], with rates up to 40.2% in informal carers of people surviving stroke [6] and 33.9% in carers of people living with Alzheimer’s disease [7].
Several factors have been found to be associated with the presence of depressive symptoms in family caregivers, including social support. Social support is considered to play an important role in maintaining a sense of well-being for carers [8] defined as “the existence or availability of people we can trust, people who let us know that they care about us, value us, and love us” [8]. Social support can positively influence the physical and mental health of informal caregivers, contributing as a protector or buffer against stressors. It has been classified according to its purpose into specific dimensions: emotional (emotional support), instrumental (task help), and informational (information) [8]. Another classification evident in the literature is that between perceived or received social support. The first relates to the assessment of the availability of support when needed and its adequacy and/or quality, while received support is associated with the nature and frequency of specific support transactions [8].
Several theoretical models have been put forward to explain the effects of social support on mental health outcomes [9,10]. One of these includes the stress and coping models derived from the transactional stress theory of Lazarus and Folkman [9]. In this theory, stress is defined as the result of the interaction between the person and their environment, where when the latter is perceived as threatening or overwhelming in relation to the resources available to the individual, it can endanger well-being. Transactional stress theory defines social support as a variable that influences the stress appraisal process thereby directly or indirectly influencing the experience of stress; as a result, access to or lack of social support in specific but similar situations can differentially impact individuals [7]. In line with these models, Cohen and Wills [10] have argued that social support could play a key role in how individuals perceive stress, with provision to and access to certain resources making individuals perceive a current situation as less stressful.
Several empirical studies have shown that social support may have a protective effect on the onset of depressive symptoms in informal caregivers of dependent adults and older people [11,12,13]. However, the level of evidence of this protective effect remains unclear [14], with no systematic reviews consistently analysing the relationship between social support and depressive symptoms in informal caregivers. This may have important implications for carers’ emotional health, as it remains unknown which types of social support interventions may be most effective in promoting positive mental health outcomes for carers. There is also currently limited knowledge on how specific factors such as type of social support (perceived vs. received), cause of caregiving dependency, and methodological quality of studies affect the association between social support and carer depressive symptoms.
Therefore, the purpose of this review was to systematically summarize and synthesize the evidence by providing an average effect estimate of the relationship between social support and depressive symptoms in informal caregivers of dependent adults and older people. The secondary objective was to rate the quality of the evidence. The research questions that guided this systematic review were:
- Is high perceived social support associated with fewer depressive symptoms?
- Is high received social support associated with fewer depressive symptoms?
2. Materials and Methods
2.1. Design
A quantitative systematic review with meta-analysis was conducted following the recommendations of PRISMA [15] and the Cochrane Handbook [16] and registered with PROSPERO [17] (id: CRD42023405918).
2.2. Search Strategy
We carried out a systematic search up to 15 January 2023 in the following databases: PubMed, CINAHL, PsycINFO, and Scopus; details of the search strategy are presented in Table 1. No time or language filters were used (Table S1). For example, the search string used in PubMed was: ((Depression[mj] OR ((Depress*[tiab]) NOT MEDLINE[sb])) AND (Caregivers[mj] OR ((Caregiv*[tiab] OR Care giv*[tiab] OR Carer*[tiab]) NOT MEDLINE[sb])) AND (Social support[mh:noexp] OR ((social network[tiab] OR informal support[tiab] OR received support[tiab] OR perceived support[tiab]) NOT MEDLINE[sb]))) NOT (clinical trial[pt] OR randomized clinical trial[tiab] OR randomized controlled trial[tiab] OR qualitative study OR qualitative research).
2.3. Eligibility Criteria
To carry out the selection of studies, the following inclusion criteria were established: (1) original studies, (2) reporting on the relationship between social support and depressive symptoms, (3) in informal caregivers aged 18 years of age or over, (4) of adult and older dependents, (5) that presented adequate statistical data to assess the magnitude of the association or size of the effect.
2.4. Data Extraction and Synthesis
Two review authors (BGS and RdPC) extracted data independently in a standardised way. This included: the first author and year of publication, sample (type of sampling and sample size), type of design, type of social support (perceived or received, both global and separate dimensions), type of social support scale used, depressive symptoms scale, chronic condition of the care recipient and size of the association or effect. The measures of association or effect used were the correlation coefficient or another measure that could be transformed into a correlation coefficient. The conversion of other effect measures to correlation coefficients was carried out by the statistical software used.
2.5. Ratings of Quality Assessment
For the evaluation of the methodological quality of the included studies, we followed the recommendations of the Cochrane Handbook in regards to rating specific areas of quality as opposed to using overall scores for each study. Thus, we carried out the evaluation of methodological quality by assessing selection, classification, and confounding biases based on criteria proposed by Viswanathan et al. [18] and Boyle [19] which were: (1) type of sampling (use of probability sampling or not; selection bias); (2) validity and reliability of measurements used (content validity and internal consistency of the questionnaires in the target population or similar; classification bias); this criterion was mandatory for a study to be included in the meta-analysis; (3) control for confounding (control for at least one measure of caregiver objective burden) and (4) for longitudinal studies, attrition rate (follow-up rate of 80% of the original population participating in the study; selection bias).
With respect to confounders, objective burden was considered necessary due to its association with depressive symptoms [20], and included functional ability, cognitive impairment, and behavioural problems [21]. Because these measures are interrelated [22], we considered as adequate studies controlling for at least one of the previous measures of objective burden. When statistical adjustment was performed, we considered confounding bias to be absent if the variation in the point estimate was less than 10%. Two review authors independently assessed study quality (BGS and RdPC).
2.6. Certainty Assessment
Based on the recommendations of the Grading of Recommendations Assessment Development and Evaluation (GRADE) guidelines [23], we assessed the quality of evidence by rating the methodological quality of the included studies (see previous paragraph), which included inconsistency (heterogeneity), imprecision and publication bias. Inconsistency refers to the variation of the effect estimates having excluded the main causes of this variation (e.g., sampling bias), allowing us to investigate heterogeneity. Imprecision allows us to study the effects of sample size, through the amplitude of confidence intervals, sample size, and number of events. Publication bias enabled us to assess whether there is a high probability of unreported studies, mainly due to the absence of effects, or not including all relevant outcome variables.
Assessment of inconsistency and publication bias are described below. We assessed imprecision by evaluating the number of studies included in each meta-analysis (small: <5 studies, medium: 5–10 studies, and adequate: >10 studies) and the average sample size (low: <100 participants, intermediate: 100–300 participants, and high: >300 participants) [24].
2.7. Analyses
A random-effects model was used in the meta-analysis to allow generalization of the findings to any caregiving population of adult and older dependents, as recommended by Cooper et al. [25].
For the heterogeneity analysis, the Q-test was used, alongside the degree of inconsistency (I2) of Higgins et al. [26]. The Q-test indicates heterogeneity when the p-value is greater than 0.1. The degree of inconsistency (I2) is the proportion of the variability observed in the effect of the intervention (between studies) that is due to heterogeneity between studies and not to chance. It comprises values between 0% (no heterogeneity) and 100% (maximum heterogeneity), with values of 25% indicative of little heterogeneity; 50% as moderate, and 75% as high [26]. Following the recommendations of Guyatt et al. [27], we used several methods to assess publication bias. These methods were funnel plot evaluation, the Egger’s test [28], and the Trim and Fill method [29]. The Egger test is the regression of the funnel plot measuring whether the slope of the regression is equal (there is no publication bias) or different (there is) from 0, with a p-value greater than 0.1 indicative of a low risk of publication bias [28]. Following the recommendations of the Cochrane Handbook [16], the Egger test was only assessed in meta-analyses with at least 10 included studies. The Trim and Fill method calculates the estimated effect after correcting for possible asymmetry in the funnel plot by eliminating small studies that cause asymmetry and imputing the missing studies necessary [29]. Thus, by comparing the value of the combined effect with that estimated by the Trim and Fill method, we can estimate whether there is no publication bias (previous values are the same) or if there is an influence on the combined effect.
We conducted a sensitivity analysis to investigate the robustness of our findings. We used the leave-one-out method by eliminating one study at a time and analysing the remaining k-1 studies each time. Subgroup analyses were performed to analyse the robustness of our findings and the possible effect of moderators on the combined effect estimate. We selected the following moderators: type of study design (cross-sectional vs. longitudinal), quality criteria (selection bias, classification bias, and confounding), and chronic condition of the care recipient (frail older people, dementia, cancer, mental health disorder, and stroke). In addition, we conducted meta-regressions to analyse the possible moderating effect of caregiver age (mean) and caregiver gender (% female).
All analyses were performed using the Comprehensive Meta-analysis program 3.3 (Biostat, Englewood, NJ, USA).

Table 1.
Description of studies included in the review.
Table 1.
Description of studies included in the review.
| Study (Author-Year) Country | N | Mean Age (SD) and Range | Percentage of Female (%) | Design | Recipients of Care | Type of Social Support | Measure of Social Support ** | Measuring Depressive Symptoms ** |
|---|---|---|---|---|---|---|---|---|
| Aggar 2010 [30] Australia | 93 | 65.8 (13.6) 37–95 | 59.1 | Cross-sectional | Frail older people | Perceived (global) | CRA | HADS |
| Ali 2016 [31] Pakistan | 90 | 34.9 (8.9) 20–45 | 84.4 | Cross-sectional | Stroke | Perceived (global) | MSPSS | DASS-42 |
| Amorin 2009 [32] Portugal | 46 | 35 (N/A) N/A | 80.4 | Cross-sectional | Cancer | Perceived (emotional) | ESSS | EADS-21 |
| Ar 2017 [33] Turkey | 190 | 51.4 (8.7) 26–77 | 89.5 | Cross-sectional | Dementia | Perceived (global) | MSPSS | BDI |
| Arevalo-Flechas 2014 [34] United States | 202 | 64.7(8.9) 47–83 * | 76.4 | Cross-sectional | Dementia | Perceived (global) | PRQ-85 | HADS |
| Asti 2006 [35] Turkey | 130 | 43.9 (8.52) 27–61 * | 81.5 | Cross-sectional | Dialysis | Perceived (global) | PSS | BDI |
| Au 2009 [36] China | 134 | 54.5 (13.2) 28–81 | 74.6 | Cross-sectional | Dementia | Perceived (global, emotional, and instrumental) | MSSS | CES-D |
| Azevedo 2017 [37] Brazil | 115 | 68 (N/A) 59–76 | 64.3 | Cross-sectional | Palliative care | Perceived (global) | MOS-SS | CES-D |
| Baillie 1988 [38] United States | 87 | 52.5 (13.9) 22–91 | 76 | Cross-sectional | Frail older people | Perceived (emotional) | Ad hoc | POMS |
| Ballard 1995 [39] United Kingdom | 109 | 64.3 (13.5) 37–91 * | 80.7 | Cross-sectional | Dementia | Perceived (global) | Ad hoc | Cornell |
| Bambara 2014 [40] United States | 42 | 51.6 (9.8) 32–71 * | 90.5 | Cross-sectional | Multiple sclerosis | Perceived (global) | SSSI | PHQ-9 |
| Bergman 1992 [41] United States | 94 | 70.2 (8.9) 52–88 * | 69.2 | Cross-sectional | Dementia | Perceived (global) | PRQ-85 | CES-D |
| Biggati 2011 [42] United States | 78 | 51.2 (12.6) 26–76 * | 0 | Cross-sectional | Cancer | Perceived (global) | ISEL | CES-D |
| Bonsu 2019 [43] Africa | 100 | 33.2 (8.9) 15–51 * | 79 | Cross-sectional | Severe burns injuries | Perceived (global) | MSPSS | BDI |
| Burgeois 1996 [44] United States | 100 | 71.9 (7.3) 57–87 * | 55 | Cross-sectional | Dementia | Perceived (global) | ISEL | CES-D |
| Burton 2008 [45] United States | 50 | 72.4 (10.2) 52–93 * | 80 | Cross-sectional | Palliative care | Perceived (global) | Ad hoc | CES-D |
| Butler 2001 [46] United States | 62 | 58 (N/A) 31–81 | 75.8 | Cross-sectional | Frail older people | Perceived (global) | Ad hoc | CES-D |
| Cabral 2014 [47] Portugal | 104 | 52 (N/A) 22–77 | 62.5 | Cross-sectional | Mental health | Perceived (global) | ESSS | EADS-21 |
| Calvete 2011 [48] Spain | 223 | 49.9 (12.6) 20–77 | 72.2 | Cross-sectional | Traumatic brain injury | Perceived (global, emotional, instrumental) | FNQ | CES-D |
| Cardenas 2014 [49] United States | 264 | 57.5 (13) 21.5–84 * | 100 | Cross-sectional | Dementia | Perceived (global) | ISSB | CES-D |
| Chai 2018 [50] Asia | 165 | 45 (14.6) 16–74 * | 54.4 | Cross-sectional | Mental health | Perceived (global) | MSPSS | QIDS-SR 16 |
| Chou 2010 [51] China | 350 | 66.6 (7.7) 55–87 | 44.9 | Cross-sectional | Intellectual disability | Perceived (global) | SSS | CES-D |
| Chow 2012 [52] China | 158 | 75.6 (6.8) 55–90 | 61.4 | Cross-sectional | Frail older people | Perceived (global) | SSSQ | GDS |
| Clyburn 2000 [53] Canada | 613 | 58.8 (13.5) 32–86 * | 71 | Cross-sectional | Dementia | Received (global) | Ad hoc | CES-D |
| Crespo 2005 [54] Spain | 108 | 57.2 (11.5) 34–78 * | 82.2 | Cross-sectional | Frail older people | Received and perceived (global) | SSSQ | BDI |
| Cumming 2008 [55] Australia | 116 | 66.9 (13.3) 32–92 | 71 | Cross-sectional | Stroke | Perceived (global) | MOS-SS | IDA Scale |
| Decker 1989 [56] United States | 67 | 55.9 (N/A) 17–75 | 88 | Cross-sectional | Spinal cord injury | Perceived (global) | Ad hoc | CES-D |
| Del Pino Casado 2022 [57] Spain | 81 | 57.6 (12.5) 28–89 | 87.3 | Longitudinal (repeated measures) | Frail older people | Perceived (global) | Duke-UNC | Goldberg |
| Durkin 2010 [58] United States | 130 | 63.4 (15) 20–87 | 84 | Longitudinal (repeated measures) | Frail older people | Perceived (global) | ISEL | CES-D |
| Faber 2005 [59] United States | 310 | 38.9 (7.3) 22–62 | 100 | Cross-sectional | Cancer | Perceived (global) | ISEL | CES-D |
| Gibson 2013 [60] United States | 1218 | 62.2 (13.2) 36–89 * | 82 | Cross-sectional | Dementia | Received (global) | K & B-C | CES-D |
| Giovannetti 2015 [61] Italy | 129 | 52.8 (13.1) 27–79* | 68.2 | Cross-sectional | Disorders of consciousness | Perceived (global) | MOS-SS | BDI-II |
| Grant 2000 [62] United States | 52 | 53.7 (16) 22–81 | 82.7 | Cross-sectional | Stroke | Perceived (global, emotional, instrumental) | ISEL | CES-D |
| Grant 2001 [63] United States | 40 | 53.3 (N/A) 22–81 | 85 | Cross-sectional | Stroke | Perceived (global) | ISEL | CES-D |
| Graven 2020 [64] United States | 530 | 41.4 (10.4) 21–62 * | 49.1 | Cross-sectional | Heart failure | Perceived (global) | ISEL | CES-D |
| Haley 1987 [65] United States | 54 | 56.1 (16.3) 20–87 | 80 | Cross-sectional | Dementia | Perceived (global) | HDLS | BDI |
| Han 2014 [66] China | 301 | 46.7 (14) 19–75 * | 63 | Cross-sectional | Cancer | Perceived (global) | MSPSS | CESD-10 |
| Harwood 2000 [67] United States | 64 | 63.8 (14.9) 27–90 | 70 | Cross-sectional | Dementia | Perceived (global) | PESS | CES-D |
| Hasson-Ohayon 2010 [68] Israel | 150 | 56.2 (11) 34–78 * | 100 | Cross-sectional | Cancer | Received (global) | CPASS | BSI |
| Hobbs 1997 [69] United States | 100 | 65.6 (8.12) 55–86 | 100 | Cross-sectional | Mental health | Perceived (global) | PESS | CES-D |
| Hwang 2011 [70] United States | 35 | 51.7 (12.9) 18–71 | 60 | Cross-sectional | Pulmonary hypertension | Perceived (global) | MOS-SS | PHQ-9 |
| Jeong 2017 [71] Korea | 39 | 45 (12.8) 19–71 * | 72.2 | Cross-sectional | Cancer | Perceived (global) | Duke-UNC | HADS |
| Khusaifan 2017 [72] Saudi Arabia | 122 | N/A | 78.7 | Cross-sectional | Dementia | Perceived (global) | MSPSS | HDRS |
| Kiral 2017 [73] Turkey | 141 | 59.7 (12.7) 32–85 * | 77 | Cross-sectional | Dementia | Perceived (global) | MSPSS | BDI |
| Koerner 2010 [74] United States | 61 | 56.7(13.2) 30–83 * | 73 | Cross-sectional | Frail older people | Perceived (global) | Walen & Lanchman | HSC |
| Kruithof 2016 [75] Netherlands | 183 | 62.5 (10.9) 41–84 * | 78.7 | Longitudinal (repeated measures) | Stroke | Received (global) | SSL-12-I | HADS |
| Kusku 2009 [76] Turkey | 51 | 42.2 (11.1) 20–64 * | 84.3 | Cross-sectional | Cancer | Perceived (global) | MSPSS | BDI |
| Lakey 2002 [77] United States | 100 | 49 (N/A) N/A | 100 | Cross-sectional | Dementia | Perceived (emotional) | QRI | CES-D |
| Lee 2003 [78] China | 69 | 53 (14.4) 23–82 | 84 | Cross-sectional | Dementia | Perceived (global) | PRQ-85 | CES-D |
| Leibach 2013 [79] United States | 81 | 43.4 (15.3) 13–74 * | 66.7 | Cross-sectional | Multiple sclerosis | Perceived (global) | ISEL | PHQ-9 |
| Li 1997 [80] United States | 252 | 65.4 (8.3) 49–82 * | 100 | Cross-sectional | Frail older people | Received (global, emotional, instrumental) | Ad hoc | CES-D |
| Li 2019 [81] China | 557 | 57 (6.7) 44–70 * | 47.2 | Cross-sectional | Frail older people | Perceived (global) | MSPSS | CES-D |
| Losada 2010 [82] Spain | 334 | 58.6 (12.9) 28–85 | 77.8 | Cross-sectional | Dementia | Received (global) | PSQ | CES-D |
| Luchsinger 2015 [83] United States | 139 | 59.3 (10.4) 39–80 * | 85.7 | Cross-sectional | Dementia | Perceived (global) | SSNL | GDS |
| Majerovitz 2007 [84] United States | 103 | 56 (N/A) N/A | 74 | Cross-sectional | People living in nursing homes | Perceived (global) | SSSQ | CES-D |
| MaloneBeach 1995 [85] United States | 57 | 58.3 (11.1) 22–83 | 100 | Cross-sectional | Dementia | Received (global, emotional, instrumental) | Ad hoc | CES-D |
| Manso Martínez 2013 [86] Spain | 88 | 56.6 (12.2) 32–81 * | 84.1 | Cross-sectional | Frail older people | Perceived (global) | Duke-UNC | HADS |
| Moral Serrano 2003 [87] Spain | 215 | 55.3 (14.6) 26–85 * | 87 | Cross-sectional | Older people hospitalized at home | Perceived (global) | Duke-UNC | Goldberg |
| Neri 2012 [88] Brazil | 176 | 71.8 (4.9) 68–90 | 70.7 | Cross-sectional | Frail older people | Perceived (global) | ISEL | GDS |
| Nuwamanya 2023 [11] Africa | 336 | 39.2 (11.5) 16–62 * | 60.4 | Cross-sectional | Cancer | Perceived (global) | MSPSS | PHQ-9 |
| Pagel 1987 [89] United States | 68 | 65 (9) 35–85 | 63.2 | Cross-sectional | Dementia | Perceived (global) | GSS | BDI |
| Pagnini 2010 [90] Italy | 40 | 55.6 (12.3) 51–80 * | 70 | Cross-sectional | Amyotrophic lateral sclerosis | Perceived (global) | MG-SS | BDI-II |
| Pearce 2006 [91] United States | 162 | 51 (13.3) 24–78 * | 73 | Cross-sectional | Terminal cancer | Perceived (global) | ISEL | DSM-IV |
| Raad 2020 [14] United States | 558 | 46.1 (14.1) 18–74 * | 58 | Cross-sectional | Traumatic brain injury | Perceived (global) | TBI-CareQOL | TBI-CareQOL |
| Rapp 1998 [92] United States | 65 | 61.3 (14.4) 33–90 * | 76.8 | Cross-sectional | Dementia | Perceived (global) | MOS-SS | CES-D |
| Rauktis 1995 [93] United States | 106 | 59 (N/A) 30–84 | 86 | Cross-sectional | Mental health | Perceived (global) | PSI | CES-D |
| Rivera 1991 [94] Africa | 165 | 58.6 (10.9) 30–85 | 100 | Cross-sectional | Frail older people | Perceived (global) | ASSIS | SADS |
| Riverra–Navarro 2018 [95] Spain | 326 | 60.1 (14.5) 31–89 * | 67.2 | Cross-sectional | Dementia | Perceived (global) | Duke-UNC | HADS |
| Robinson 1989 [96] United States | 78 | 65 (N/A) 47–85 | 100 | Cross-sectional | Dementia | Received (global) | ISSB | CES-D |
| Robinson 1994 [97] United States | 40 | 65 (N/A) 52–80 | 100 | Cross-sectional | Dementia | Perceived and Received (global) | GSS/SNL | CES-D |
| Rodakowski 2013 [98] United States | 173 | 53 (15) 23–83 * | 76 | Cross-sectional | Spinal cord injury | Received | REACH trial | CES-D |
| Rodi 2015 [99] United States, United Kingdom and Australia | 87 | N/A (N/A) 18–74 | 86.2 | Cross-sectional | Cancer | Perceived (global) | MOS-SS | BDI-II |
| Sahin 2012 [100] Turkey | 60 | 54.7 (N/A) N/A | 18 | Cross-sectional | Cancer | Perceived (global) | PSS-Fa | BDI |
| Sandoval 2019 [101] Chile | 377 | 51.7 (15.4) 15–87 | 85.1 | Cross-sectional | Frail older people | Perceived (global) | Duke-UNC | CES-D |
| Schulz 1991 [102] United States | 172 | 57.8 (N/A) N/A | 18 | Repeated measures with cross-sectional correlations | Dementia | Perceived (global) | ISEL | CES-D |
| Schumacher 1993 [103] United States | 75 | 43.8 (14.7) 18–75 | 51 | Cross-sectional | Cancer | Perceived (global) | Ad hoc | POMS |
| Schwarz 2000 [104] United States | 100 | 64.7 (13.4) 29–88 | 74 | Repeated measures with cross-sectional correlations | Frail older people | Received (global) | MISSB | CES-D |
| Scicolone 2018 [105] United States | 249 | 64.3 (11.1) 30–89 | 92.5 | Cross-sectional | Frail older people | Perceived (global) | MOS-SS | CES-D |
| Serrani 2014 [106] Argentina | 100 | 48.2 (3.4) 51–55 * | 91 | Cross-sectional | Greater | Perceived (global) | Duke-UNC | CES-D |
| Serrano-Ortega 2017 [107] Spain | 177 | 58.5 (12.9) 20–89 | 88 | Longitudinal (repeated measures) | Frail older people | Perceived (global) | Duke-UNC | Goldberg |
| Shaughnessy 2011 [108] Canada | 30 | 73.7 (6.9) 57–86 | 63.3 | Cross-sectional | Dementia | Perceived (global) | MOS-SS | CES-D |
| Shukri 2020 [109] Malaysia | 340 | 46 (15.2) 20–70 | 54.4 | Cross-sectional | Hemodialysis | Perceived (global) | MSPSS | HADS |
| Speer 1993 [110] United States | 26 | 67.3 (N/A) N/A | 15 | Cross-sectional | Parkinson | Perceived (emotional) | ISEL | GDS |
| Steffen 2002 [111] United States | 145 | 60.2 (13.3) 33.6–86.8 * | 80 | Cross-sectional | Dementia | Perceived (global) | PSS | BDI |
| Stevens 2013 [112] Mexico | 90 | 47.12 (12.7) 22–73 * | 92 | Cross-sectional | Traumatic brain injury | Perceived (global, emotional, instrumental) | ISEL | PHQ-9 |
| Tay 2022 [12] United States | 98 | 58.9 (14.24) 27–87 | 72.6 | Cross-sectional | Palliative care | Perceived (global) | MOS-SS | HADS |
| Tang 2015 [113] United States | 91 | 67 (12.2) 43–92 * | 70 | Cross-sectional | Dementia | Perceived (global) | ISEL | BDI-II |
| Thielemann 2001 [114] United States | 164 | 61.9 (10.8) 31–81 | 60 | Cross-sectional | Cancer | Perceived (global) | ISEL | CES-D |
| Verez Cotelo 2015 [115] Spain | 25 | 55 (12.8) 39–87 | 80 | Cross-sectional | Dementia | Perceived (global) | Duke-UNC | BDI-II |
| Yen 2006 [116] China | 55 | 54.3 (14.7) 20–83 | 70.9 | Cross-sectional | Mental health | Perceived (global) | Ad hoc | CES-D |
| Yoon 2003 [117] Korea | 311 | 56.1 (15.6) 24–92 | 81 | Cross-sectional | Frail older people | Received (global, emotional, instrumental) | PRQ-2000 | SDS |
| Yun 2023 [118] Korea | 396 | 80.7 (5.7) 69–96 | 57.6 | Cross-sectional | Frail older people | Perceived (global) | Ad hoc | SGDS-K |
| Zhong 2020 [13] China | 567 | 80.6 (8.8) 63–98 * | 54.2 | Cross-sectional | Frail older people | Perceived (global) | MSPSS | CES-D |
Abbreviations: SD: standard deviation; *: ranges are estimated as ±2 standard deviations; N/A: not available; **: abbreviations of the scales used are shown in back matter part.
3. Results
3.1. Description of Search Results
Our search yielded a total of 3436 results. After eliminating duplicates, 3389 results were reviewed by title and abstract. Of these, 3151 were eliminated for not being relevant, with a total of 238 full-texts being reviewed. After further screening, 85 articles were rejected as not relevant, with a total of 57 studies being excluded with specific reasons and 3 classified as redundant. Our final number of included studies was 93 [11,12,13,14,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118] (Figure 1).
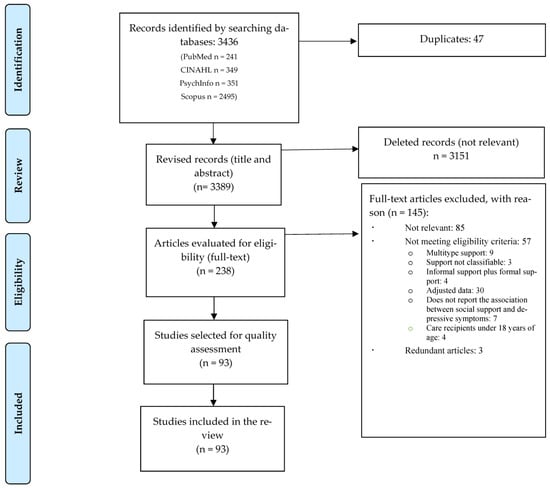
Figure 1.
PRISMA flow diagram of the review process.
3.2. Description of Study Characteristics
As shown in Table 1, most of the studies included in the review, were cross-sectional, except for 6 studies which were longitudinal repeated measures (of which, two had cross-sectional correlations). Eighty-six percent of samples were non-probabilistic (n = 80). There was a total of 15,431 participants, with a minimum sample size of 17 and a maximum sample size of 691. The weighted average age of caregivers was 56.6 years, while the % of women was 74.6%. The year of publication ranged from 1987 to 2023.
The most frequent chronic condition of care recipients was dementia (n = 26), followed by frailty (n = 21), cancer (n = 14), mental health condition (n = 5) and stroke (n = 5). Most studies measured levels of social support, with the Multidimensional Scale of Perceived Social Support (MSPSS) (perceived social support), and depressive symptoms using the Center for Epidemiological Studies (CES-D) scale.
3.3. Quality Assessment
Table 2 shows quality ratings of the included studies. All but thirteen studies used non-probability samples and twenty-one studies controlled for confounding. The majority of studies had no classification bias. All longitudinal studies, except one, reported attrition rates.

Table 2.
Quality assessment of included studies.
3.4. Results of the Different Meta-Analyses
We were able to meta-analyse both the relationship of depressive symptoms with perceived social support and received social support. The results of the different meta-analyses are shown in Table 3.

Table 3.
Findings of the meta-analyses on the relationship between social support and depressive symptoms.
3.4.1. Perceived Social Support
Seventy-eight studies reported on the relationship between global perceived social support and depressive symptoms; pooling studies showed a negative statistically significant association of a medium size effect (r = −0.35; confidence interval [CI] = −0.39; −0.31; N = 11.835; N average = 151.7; Figure 2). All but one study reported a negative direction and all but nine reported a negative statistical association. The results were consistent (I2 = 0.0; p-value for the Q test = 0.99), accurate, and robust (maximum percentage variation of the combined effect [% max] for sensitivity analysis eliminating one study at a time: = 5.7%). The funnel plot (Figure 3) appeared somewhat asymmetrical, with a small tendency for smaller studies to have larger effect sizes. The Egger test showed low risk of publication bias (p = 0.19) but the Trim & Fill test corrected the combined effect by 14.3% downwards.
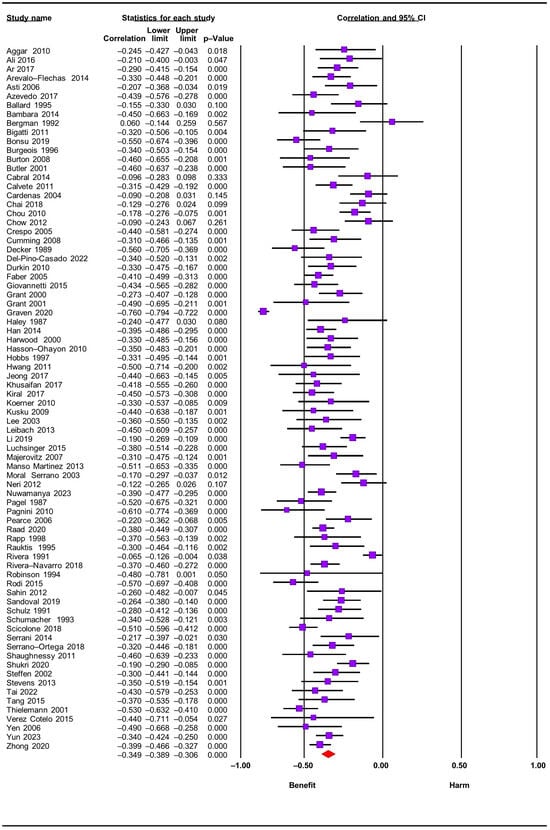
Figure 2.
Forest plot for perceived social support and depressive symptoms [11,12,13,14,30,31,33,34,35,37,39,40,41,42,43,44,45,46,47,48,49,50,51,52,54,55,56,57,58,59,61,62,63,64,65,66,67,68,69,70,71,72,73,74,76,78,79,81,83,84,86,87,88,89,90,91,92,93,94,95,97,99,100,101,102,103,105,106,107,108,109,111,113,114,115,116,118].
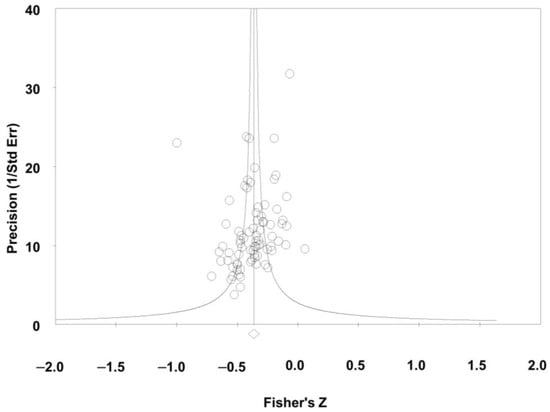
Figure 3.
Funnel plot for perceived social support and depressive symptoms.
After subgroup analyses, we found no statistically significant differences in effect sizes when taking into account type of study design (cross-sectional vs. longitudinal), type of chronic condition of the care recipient (frail older people, dementia, cancer, mental health disorder, and stroke) and study quality criteria (selection bias, classification, and confounding). Forest plots for subgroup analyses are shown in Figure S1. In addition, meta-regressions showed no variations of the combined effect due to caregiver mean age and % of females (p-values of 0.21 and 0.72, respectively). Scatterplots are shown in Supplementary Figures (Figure S2).
Regarding the dimensions of perceived social support, we found studies reporting on emotional and instrumental dimensions. Seven studies analysed the relationship between perceived emotional social support and depressive symptoms; meta-analysis showed a negative medium-size effect (r = −0.35; CI = −0.45; −0.25; N = 624; N mean = 89.1) with low heterogeneity overall (I2 = 19.1). The funnel plot appeared asymmetric, but the Trim and Fill method (corrected combined effect did not vary from the original) showed no publication bias.
Finally, three studies evaluated the relationship between instrumental perceived social support and depressive symptoms, with a negative and medium-sized association (r = −0.35; CI = −0.44; −0.26; N = 365; N average = 121.7), and no heterogeneity present (I2 = 0.0). We were unable to assess risk of publication bias due to the small number of included studies.
3.4.2. Received Social Support
Twelve studies examined the relationship between global received social support and depressive symptoms; meta-analysis showed a negative statistical association of a small magnitude overall (r = −0.14; CI = −0.20; −0.07; N = 3470; N average = 289.2; Figure 4). All but two studies reported a negative direction and seven of the twelve studies reported a negative statistical association. Results showed overall low heterogeneity (I2 = 13.8; p-value for the Q test: 0.31) and were accurate and moderately robust (% max for sensitivity analysis eliminating one study at a time: 12.9%). Meta-regressions showed no variations of the combined effect due to caregiver mean age and % of females (p-value of 0.18 and 0.90, respectively). Scatterplots are shown in Supplementary Figures (Figure S2). The funnel plot (Figure 5) seemed somewhat asymmetric, although the Egger test showed no evidence of publication bias (p = 0.48), with the Trim & Fill test correcting the combined effect only by 7.1% downwards.

Figure 4.
Forest plot for received social support and depressive symptoms [36,53,60,75,80,82,85,96,97,98,104,117].
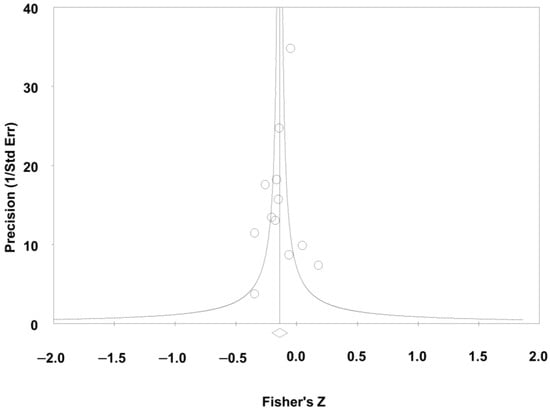
Figure 5.
Funnel plot for received social support and depressive symptoms.
Regarding the dimension of perceived social support, we found three studies reporting on emotionally received social support and three on instrumental support; meta-analysis indicated similar findings to global received social support (for emotional support: r = −0.15; CI = −0.23; −0.07; N = 620; N mean = 206.7; for instrumental: r = −0.14; CI = −0.26; −0.02; N = 620; N mean = 206.7).
4. Discussion
In the present work, we report on the first systematic review and meta-analysis of the relationship between social support and depressive symptoms of informal caregivers. We found that higher levels of depressive symptoms in informal caregivers of adult and older dependents are associated with lower levels of social support, both perceived and received dimensions. To our knowledge, our review is the first to systematically analyse this association, reporting on the global literature to date. An important strength of our review is that we report on a large number of studies overall, including data from diverse populations, with additional sensitivity and subgroup analyses allowing us to assess the effect of the quality of the evidence.
In relation to perceived social support, our results coincide with those of other reviews highlighting the possible protective effect of perceived social support on depressive symptoms in caregivers of children and adolescents with autism [119], in the general population [120], and healthy older people [121]. Our results are in line with reviews conducted in informal caregivers of dependent adults and older people reporting on the relationship between perceived social support and other mental health consequences of provision of care such as subjective caregiver burden [122] and anxiety symptoms [123]. Previous reviews [119,120,121], investigating the possible protective effect of perceived social support on depressive symptoms in populations other than those investigated in our review, also show similar findings.
The relationship between high levels of perceived social support and lower symptoms of depression could be explained under the prism of several different theories [9,10]. According to Lazarus and Folkman [9], in stressful situations, people carry out an assessment of both the possible repercussions of a situation and their ability to cope with the stressor. When these evaluations are negative, stress proliferates. In the caregiving context, if perceptions of social support are perceived as adequate, this may predispose carers to be more likely to cognitively assess the caregiving situation as benign and therefore perceive stressors as less threatening. This may in turn enhance confidence and self-efficacy in undertaking caregiving duties and positively influence mental health outcomes for carers.
Cohen and Wills [10,124] argued that social support may exert its effect at two different points in the causal sequence, linking stress to its consequences. On one hand, the perception that others can provide necessary support could lead to appraising a situation as less stressful. On the other hand, the support a person receives may lessen the influence of stress by facilitating problem-solving (providing a solution to the problem or reducing the perceived importance of the problem), providing a distraction from the distressing situation, or facilitating healthy behaviours. Therefore, when levels of social support are generally perceived as adequate, carer stress situations or associated stressors may appear as less threatening. This may therefore explain how high levels of social support can reduce levels of emotional distress such as depressive symptoms.
Our results reporting on the relationship between perceived social support and depressive symptoms are robust, based on sufficient levels of evidence overall. For example, we found adequate precision, and consistency, with no statistically significant differences between the combined effect of studies with good versus low quality. There were also no statistically significant differences between the different groups of recipients of care, and although there was evidence of risk of publication bias, the combined effect corrected by the Trim and Fill method varied little from the original combined effect.
Our results therefore have important clinical implications as they indicate that levels of perceived social support by informal caregivers may be an important marker of depressive symptoms. Investing therefore in the development and provision of interventions promoting and strengthening perceived social support for families may prevent or alleviate carer depressive symptoms. For example, social support group interventions may improve carer well-being by reducing loneliness, and caregiver burden or enhance the perceived effectiveness of how carers manage caregiving tasks [125].
Our results on the relationship between received social support and depressive symptoms are moderately robust with sufficient levels of evidence overall since there was adequate precision, low inconsistency and, although publication bias was present, this risk had little effect on the final results. Due to the small number of included studies, however, we were not able to perform subgroup analyses.
Interestingly as in previous reviews [122,123], we found that the effect of received social support on depressive symptoms was overall small, suggesting that the central role of social support on the onset and development of depressive symptoms in informal caregivers may be specific to perceived rather than received levels of social support, similar to previous reviews [122,123].
Our results therefore support the hypothesis that perceived and received levels of social support are different constructs with different effects on stress proliferation [126]. For example, several studies have shown that the effect of received support on stress proliferation is smaller compared to that of perceived social support [127,128]. Our study expands knowledge on caregiver depressive symptoms by demonstrating how different types of social support contribute to the experience of depressive affect. The findings from this work can therefore inform interventions that target specific areas of support for family carers and those that aim to reduce the risk of mild symptoms of depression developing into clinical psychopathology. Our results may also provide valuable insights for policymakers, clinicians, and researchers as they point towards the value of implementing social support interventions as preventive mental health strategies for carers. Future studies should assess how different dimensions of social support impact caregivers’ mental health and investigate how cultural or contextual factors might influence the relationship between social support and depressive symptoms. Future work should also examine how other social parameters such as social recognition may be influencing the association between social support and carer depressive symptoms.
Limitations
Our study has several limitations. Most studies included in our review employed a cross-sectional design and used non-probability samples. Cross-sectional designs are limited in informing causality relationships. However, given our subgroup analyses showed that this did not affect our results we are relatively confident that our reported effect estimates are close to the true effect estimate. In the case of received social support, subgroup analyses could not be carried out due to the small number of studies; this means that the effect of type of design, study quality, or cause of care-recipient dependency on the relationship between received social support and depressive symptoms remains unknown. It was also not possible to control for several confounders such as a prior history of depression or analyse the effect of objective caregiver burden for received social support. Finally, the longitudinal studies included in this review did not report analyses controlling for possible reverse causality. The existence of reverse causality would imply that depressive symptoms could influence perceptions of social support. Future longitudinal studies therefore are necessary to examine the effect of reverse causality, which will increase our confidence in the estimated effect sizes.
5. Conclusions
Despite the above limitations, we are able to reach important clinical conclusions about levels of social support in informal caregivers of dependent adults and older people: (1) perceived social support and received social support are different constructs that differentially influence depressive symptoms in informal caregivers, (2) perceived social support is an important protective factor for high levels of depressive symptoms reported by informal carers, (3) the relationship between perceived social support and depressive symptoms does not vary substantially across the different types of care dependency and (4) the effect of perceived social support on depressive symptoms appears to be clinically relevant.
Our results overall strengthen the use of social support as a marker of clinically significant depressive symptoms for informal carers. They also support the development and wider provision of interventions promoting and strengthening perceived social support to prevent or alleviate depressive symptoms in informal caregivers.
Further longitudinal studies analysing the possible effect of reverse causality between social support and depressive symptoms are needed to increase our understanding of the effect of social support on caregivers’ mental health.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12206468/s1, Table S1: Summary of the search strategy used in the databases. Figure S1: Forest plots for subgroup analyses. Figure S2: Scatterplots for meta-regressions.
Author Contributions
Conceptualization, R.d.-P.-C., B.G.-S., V.O. and C.L.-M.; methodology, R.d.-P.-C. and B.G.-S.; validation, B.G.-S. and R.d.-P.-C.; formal analysis, R.d.-P.-C. and B.G.-S.; data curation, B.G.-S. and R.d.-P.-C.; writing—original draft preparation, R.d.-P.-C., B.G.-S., V.O. and C.L.-M.; writing—review and editing, R.d.-P.-C., B.G.-S., V.O. and C.L.-M.; supervision, R.d.-P.-C.; project administration, R.d.-P.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
Among the papers included in the review were a study by del-Pino-Casado R and López-Martínez C and the doctoral dissertation of a doctoral student of del-Pino-Casado R (Serrano-Ortega 2017 [107]) that complied with the established criteria. There is no other conflict of interest.
Abbreviations
| Abbreviations of Measures of: | |
| Social Support | |
| ASSIS | Arizona Social Support Interview Schedule |
| CRA | Caregiver Reaction Assessment |
| CPASS | Cancer Perceived Agent of Support Questionnaire |
| Duke-UNC | Duke-UNC functional social support questionnaire |
| ESSS | Satisfaction with Social Support Scale |
| FNQ | Family Needs Questionnaire |
| GSS | Global Satisfaction Scale |
| HDLS | Health and Daily Living Form |
| ISEL | Interpersonal Support Evaluation List |
| ISSB | Inventory of Socially Supportive Behavior |
| K & B-C | Krause and Borawski-Clark Scale |
| MG-SS | McGill Quality of Life- Social Support |
| MISSB | Modified Inventory of Social Support Behaviors |
| MOS-SS | Medical Outcome Study- Social Support Survey |
| MSPSS | Multidimensional Scale of Perceived Social Support |
| MSSS | Mac-Arthur Social Support Scale |
| NSIS | Negative Social Interaction |
| PESS | Pearling Expressive Support Scale |
| PRQ-85 | Personal Resource Questionnaire |
| PSI | Positive Social Interactions |
| PSS | Perceived Social Support Scale |
| PSQ | Psychosocial Support Questionnaire |
| QRI | Quality of Relationships Inventory |
| SOCSUP | Total Social Support Scale Score |
| SNL | Social Network List |
| SSL | Social Support List |
| SSNL | Stokes’ Social Network List |
| SSSQ | Sarason’s Social Support Questionnaire |
| SSRS | Social Support Rating Scale |
| SSS | Social Support Scale |
| SSSI | Social Stress and Social Interview |
| TBI-CareQOL | The Traumatic Injury Quality of Life |
| Walen & Lanchman | Walen & Lanchman Questionnaire |
| Depression | |
| BDI | Beck Depression Inventory |
| BSI | Brief Symptom Inventory |
| CES-D | The Center for Epidemiological Studies—Depression Scale |
| Cornell | Cornell Depression scale |
| DASS-42 | Depression Anxiety and Stress Scale |
| DSM-IV | Mayor Depressive Disorder and Anxiety Disorder Diagnoses by the Structured Clinical Interview. |
| EADS-21 | Escalas de Ansiedad, Depresión y Estrés [Anxiety, Depression and Stress Scales] |
| GDS | Global Deterioration Scale |
| GHQ | General Health Questionnaire |
| HADS | Hospital Anxiety and Depression Scale |
| HDRS | Hamilton Depression Rating Scale |
| HSC | Hopkins Symptom Checklist |
| IDA Scale | Irritability, Depression, and Anxiety Scale |
| PHQ-9 | Patient Health Questionnaire |
| POMS | Profile of Mood States |
| QIDS-SR 16 | Quick Inventory of Depressive Symptomatology |
| SCL-90 | Symptom Checklist |
| SDS | Self-Rating Depression Scale |
| SQD | Square Depression Scale |
| TBI-CareQOL | The Traumatic Injury Quality of Life |
References
- World Health Organization (WHO). Disability. Available online: https://www.who.int/es/news-room/fact-sheets/detail/disability-and-health (accessed on 1 March 2023).
- Fujisawa, R.; Colombo, F. The Long-Term Care Workforce: Overview and Strategies to Adapt Supply to a Growing Demand; OECD Health Working Papers, No. 44; OECD Publishing: Paris, France, 2009. [Google Scholar] [CrossRef]
- Suarez Cuba, M.Á. Identificación y utilidad de las herramientas para evaluar el apoyo social al paciente y al cuidador informal. Revista Médica La Paz 2011, 17, 60–67. [Google Scholar]
- Zhang, B.; Lv, X.; Qiao, M.; Liu, D. The Full Mediating Role of Loneliness on the Relationship Between Social Support and Depression Among Rural Family Caregivers of Persons with Severe Mental Illness. Front. Public Health 2021, 9, 729147. [Google Scholar] [CrossRef]
- Geng, H.; Chuang, D.; Yang, F.; Yang, Y.; Liu, W.; Liu, L.; Tian, H. Prevalence and determinants of depression in caregivers of cancer patients: A systematic review and meta-analysis. Medicine 2018, 97, 39. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Jiang, Y. A Meta-analytic Study of Predictors for Informal Caregiver Burden in Patients with Stroke. J. Stroke Cerebrovasc. Dis. 2018, 27, 3636–3646. [Google Scholar] [CrossRef]
- Sallim, A.B.; Sayampanathan, A.A.; Cuttilan, A.; Chun-Man Ho, R. Prevalence of Mental Health Disorders Among Caregivers of Patients with Alzheimer Disease. J. Am. Med. Dir. Assoc. 2015, 16, 1034–1041. [Google Scholar] [CrossRef]
- Gottlieb, B.H.; Bergen, A.E. Social support concepts and measures. J. Psychosom. Res. 2010, 69, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal and Coping; Springer: New York, NY, USA, 1985. [Google Scholar]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef] [PubMed]
- Nuwamanya, S.; Nkola, R.; Najjuka, S.M.; Nabulo, H.; Al-Mamun, F.; Mamun, M.A.; Kaggwa, M.M. Depression in Ugandan caregivers of cancer patients: The role of coping strategies and social support. Ptiñizadas Sychooncol. 2023, 32, 113–124. [Google Scholar] [CrossRef]
- Tay, D.L.; Iacob, E.; Reblin, M.; Cloyes, K.G.; Jones, M.; Hebdon, M.C.T.; Mooney, K.; Beck, A.C.; Ellington, L. What contextual factors account for anxiety and depressed mood in hospice family caregivers? Psychooncology 2022, 31, 316–325. [Google Scholar] [CrossRef]
- Zhong, Y.; Wang, J.; Nicholas, S. Social support and depressive symptoms among family caregivers of older people with disabilities in four provinces of urban China: The mediating role of caregiver burden. BMC Geriatr. 2020, 20, 3. [Google Scholar] [CrossRef]
- Raad, J.H.; Tulsky, D.S.; Lange, R.T.; Brickell, T.A.; Sander, A.M.; Hanks, R.A.; French, L.; Miner, J.A.; Kisala, P.A.; Carlozzi, N.E. Establishing the Factor Structure of a Health-Related Quality of Life Measurement System for Caregivers of Persons Living with Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2020, 101, 1220–1232. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. La declaración PRISMA para informar revisiones sistemáticas y metanálisis de estudios que evalúan intervenciones de atención médica: Explicación y elaboración. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thomas, J. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Wiley Blackwell & Sons: Hoboken, NJ, USA, 2020. [Google Scholar]
- Booth, A.; Clarke, M.; Dooley, G.; Ghersi, D.; Moher, D.; Petticrew, M. The nuts and bolts of PROSPERO: An international prospective register of systematic reviews. Syst. Rev. 2012, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Viswanathan, M.; Berkman, N.D.; Dryden, D.M.; Hartling, L. Assessing Risk of Bias and Confounding in Observational Studies of Interventions or Exposures: Further Development of the RTI Item Bank; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2013. [Google Scholar]
- Boyle, M.H. Guidelines for evaluating prevalence studies. BMJ Ment. Health 1998, 1, 37–39. [Google Scholar] [CrossRef]
- Van der Lee, J.; Bakker, T.J.; Duivenvoorden, H.J.; Dröes, R. Multivariate models of subjective caregiver burden in dementia: A systematic review. Ageing Res. Rev. 2014, 15, 76–93. [Google Scholar] [CrossRef] [PubMed]
- Aneshensel, C.S.; Pearlin, L.I.; Mullan, J.T.; Zarit, S.H.; Whitlatch, C.J. Perfiles en el Cuidado; Prensa Académica: San Diego, CA, USA, 1995. [Google Scholar]
- Pinquart, M.; Sörensen, S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2003, 58, 112–128. [Google Scholar] [CrossRef]
- Atkins, D.; Best, D.; Briss, P.A.; Eccles, M.; Falck-Ytter, Y.; Flottorp, S.; Guyatt, G.H.; Harbour, R.T.; Haugh, M.C.; Henry, D.; et al. Grading quality of evidence and strength of recommendations. BMJ 2004, 328, 1490–1494. [Google Scholar] [CrossRef]
- Meader, N.; King, K.; Llewellyn, A.; Norman, G.; Brown, J.; Rodgers, M.; Moe-Byrne, T.; Higgins, J.P.; Sowden, A.; Stewart, G. A checklist designed to aid consistency and reproducibility of GRADE assessments: Development and pilot validation. Syst. Rev. 2014, 3, 82. [Google Scholar] [CrossRef]
- Cooper, H.; Hedges, L.V.; Valentine, J.C. The Handbook of Research Synthesis and Meta-Analysis; Russell Sage Foundation: New York, NY, USA, 2019. [Google Scholar]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ Br. Med. J. 2003, 327, 557. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Montori, V.; Vist, G.; Kunz, R.; Brozek, J.; Alonso-Coello, P.; Djulbegovic, B.; Atkins, D.; Falck-Ytter, Y.; et al. GRADE guidelines: 5. Rating the quality of evidence—Publication bias. J. Clin. Epidemiol. 2011, 64, 1277–1282. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Aggar, C.; Ronaldson, S.; Cameron, I.D. Reactions to caregiving of frail, older persons predict depression. Int. J. Ment. Health Nurs. 2010, 19, 409–415. [Google Scholar] [CrossRef]
- Ali, N.; Kausar, R. Social Support and Coping as Predictors of Psychological Distress in Family Caregivers of Stroke Patients. Pak. J. Psychol. Res. 2016, 31, 587–608. [Google Scholar]
- Amorim, L.; Pereira, M.G. Optimismo, suporte social e morbilidade psicológica em filhos adultos de doentes oncológicos. Psicol. Saúde E Doenças 2009, 10, 83–98. [Google Scholar]
- Ar, Y. Predictors of Depression, Anxiety, Grief and Growth among Turkish Offspring as Caregivers of Parents with Alzheimer’s Disease: A Multi-Method Study; Middle East Technical University: Ankara, Turkey, 2017. [Google Scholar]
- Arévalo-Flechas, L.; Acton, G.I.; Escamilla, M.N.; Bonner, P.L.; Lewis, S. Latino Alzheimer’s caregivers: What is important to them? J. Manag. Psychol. 2014, 29, 661–684. [Google Scholar] [CrossRef]
- Asti, T.; Kara, M.; Ipek, G.; Erci, B. The experiences of loneliness, depression, and social support of Turkish patients with continuous ambulatory peritoneal dialysis and their caregivers. J. Clin. Nurs. 2006, 15, 490–497. [Google Scholar] [CrossRef]
- Au, A.; Lau, K.M.; Koo, S.; Cheung, G.; Pan, P.C.; Wong, M.K. The effects of informal social support on depressive symptoms and life satisfaction in dementia caregivers in Hong Kong. East Asian Arch. Psychiatry 2009, 19, 57. [Google Scholar]
- Azevedo, C.; Pessalacia, J.D.R.; Mata, L.R.F.d.; Zoboli, E.L.C.P.; Pereira, M.d.G. Las interfaces entre apoyo social, calidad de vida y depresión en usuarios elegibles para cuidados paliativos. Rev. Esc. Enferm. USP 2017, 51, e03245. [Google Scholar]
- Baillie, V.; Norbeck, J.S.; Barnes, L.E. Stress, social support, and psychological distress of family caregivers of the elderly. Nurs. Res. 1988, 37, 217–222. [Google Scholar] [CrossRef]
- Ballard, C.G.; Saad, K.; Coope, B.; Graham, C.; Gahir, M.; Wilcock, G.K.; Oyebode, F. The aetiology of depression in the carers of dementia sufferers. J. Affect. Disord. 1995, 35, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Bambara, J.K.; Turner, A.P.; Williams, R.M.; Haselkorn, J.K. Social support and depressive symptoms among caregivers of veterans with multiple sclerosis. Rehabil. Psychol. 2014, 59, 230. [Google Scholar] [CrossRef]
- Bergman, B.F. Loneliness, Depression, and Social Support among Caregivers of Spouses with Alzheimer’s Disease: The Home versus the Nursing Home Care Experience; University of Nebraska Medical Center: Omaha, NE, USA, 1992. [Google Scholar]
- Bigatti, S.M.; Wagner, C.D.; Lydon-Lam, J.R.; Steiner, J.L.; Miller, K.D. Depression in husbands of breast cancer patients: Relationships to coping and social support. Support. Care Cancer 2011, 19, 455–466. [Google Scholar] [CrossRef]
- Bonsu, K.; Kugbey, N.; Ayanore, M.A.; Atefoe, E.A. Mediation effects of depression and anxiety on social support and quality of life among caregivers of persons with severe burns injury. BMC Res. Notes 2019, 12, 772. [Google Scholar] [CrossRef] [PubMed]
- Bourgeois, M.S.; Beach, S.; Schulz, R.; Burgio, L.D. When primary and secondary caregivers disagree: Predictors and psychosocial consequences. Psychol. Aging 1996, 11, 527. [Google Scholar] [CrossRef] [PubMed]
- Burton, A.M.; Haley, W.E.; Small, B.J.; Finley, M.R.; Dillinger-Vasille, M.; Schonwetter, R. Predictors of well-being in bereaved former hospice caregivers: The role of caregiving stressors, appraisals, and social resources. Palliat. Support. Care 2008, 6, 149–158. [Google Scholar] [CrossRef]
- Butler, S.S.; Turner, W.; Kaye, L.W.; Ruffin, L.; Downey, R. Depression and caregiver burden among rural elder caregivers. J. Gerontol. Soc. Work 2005, 46, 7–63. [Google Scholar] [CrossRef]
- Cabral, L.; Duarte, J.; Ferreira, M.; dos Santos, C. Anxiety, stress and depression in family caregivers of the mentally ill. Aten. Primaria 2014, 46, 176–179. [Google Scholar] [CrossRef]
- Calvete, E.; de Arroyabe, E.L. Depression and grief in Spanish family caregivers of people with traumatic brain injury: The roles of social support and coping. Brain Inj. 2012, 26, 834–843. [Google Scholar] [CrossRef]
- Cardenas, V. The Relationship between Social Support and Depression among Latina and Caucasian Dementia Caregivers. Ph.D. Thesis, Pacific Graduate School of Psychology, Palo Alto, CA, USA, 2004. [Google Scholar]
- Chai, Y.C.; Mahadevan, R.; Ng, C.G.; Chan, L.F.; Md Dai, F. Caregiver depression: The contributing role of depression in patients, stigma, social support and religiosity. Int. J. Soc. Psychiatry 2018, 64, 578–588. [Google Scholar] [CrossRef]
- Chou, Y.C.; Pu, C.; Fu, L.; Kröger, T. Depressive symptoms in older female carers of adults with intellectual disabilities. J. Intellect. Disabil. Res. 2010, 12, 1031–1044. [Google Scholar] [CrossRef] [PubMed]
- Chow, E.O.; Ho, H.C. The relationship between psychological resources, social resources, and depression: Results from older spousal caregivers in Hong Kong. Aging Ment. Health 2012, 16, 1016–1027. [Google Scholar] [CrossRef] [PubMed]
- Clyburn, L.D.; Stones, M.J.; Hadjistavropoulos, T.; Tuokko, H. Predicting caregiver burden and depression in Alzheimer’s disease. J. Gerontol. B Psychol. Sci. Soc. Sci. 2000, 55, S2–S13. [Google Scholar] [PubMed]
- Crespo-López, M.; López-Martínez, J. Estrés y estado emocional en cuidadores de familiares mayores con y sin demencia. Rev. Esp. Geriatr. Gerontol. 2005, 40, 55–61. [Google Scholar] [CrossRef]
- Cumming, T.B.; Cadilhac, D.A.; Rubin, G.; Crafti, N.; Pearce, D.C. Psychological distress and social support in informal caregivers of stroke survivors. Brain Impair. 2008, 9, 152–160. [Google Scholar] [CrossRef]
- Decker, S.D.; Schultz, R.; Wood, D. Determinants of well-being in primary caregivers of spinal cord injured persons. Rehabil. Nurs. 1989, 14, 6–8. [Google Scholar] [CrossRef]
- Del-Pino-Casado, R.; López-Martínez, C.; Frías Osuna, A.; Orgeta, V. The relationship between perceived social support and psychological distress in carers of older relatives: A longitudinal cross-lagged analysis. J. Affect. Disord. 2022, 297, 401–406. [Google Scholar] [CrossRef]
- Durkin, D.W. Changes in Emotional Well-Being and Self-Perceived Physical Health over Time among African American and White Male Caregivers of Older Adults; The University of Alabama: Tuscaloosa, AL, USA, 2010. [Google Scholar]
- Faber, K.E. The Impact of Being a Caregiver to a Parent with Cancer: Daughters’ Correlates and Predictors of Coping; Teachers College, Columbia University: New York, NY, USA, 2005. [Google Scholar]
- Gibson, B.E. A Methodological Journey to Examine the Stress Process among Dementia Caregivers from Three Ethnoracial Groups: Caucasian, African American, and Hispanic; The University of North Carolina at Greensboro: Greensboro, NC, USA, 2003. [Google Scholar]
- Giovannetti, A.M.; Covelli, V.; Sattin, D.; Leonardi, M. Caregivers of patients with disorder of consciousness: Burden, quality of life and social support. Acta Neurol. Scand. 2015, 132, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Grant, J.S.; Bartolucci, A.A.; Elliot, T.R.; Giger, J.N. Sociodemographic, physical, and psychosocial characteristics of depressed and non-depressed family caregivers of stroke survivors. Brain Inj. 2000, 14, 1089–1100. [Google Scholar] [PubMed]
- Grant, J.S.; Elliott, T.R.; Giger, J.N.; Bartolucci, A.A. Social problem-solving abilities, social support, and adjustment among family caregivers of individuals with a stroke. Rehabil. Psychol. 2001, 46, 44. [Google Scholar] [CrossRef]
- Graven, L.J.; Azuero, A.; Abbott, L.; Grant, J.S. Psychosocial factors related to adverse outcomes in heart failure caregivers: A structural equation modeling analysis. J. Cardiovasc. Nurs. 2020, 35, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Haley, W.E.; Levine, E.G.; Brown, S.L.; Bartolucci, A.A. Stress, appraisal, coping, and social support as predictors of adaptational outcome among dementia caregivers. Psychol. Aging 1987, 2, 323. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Hu, D.; Liu, Y.; Lu, C.; Luo, Z.; Zhao, J.; Lopez, V.; Mao, J. Coping styles and social support among depressed Chinese family caregivers of patients with esophageal cancer. Eur. J. Oncol. Nurs. 2014, 18, 571–577. [Google Scholar] [CrossRef] [PubMed]
- Harwood, D.G.; Ownby, R.L.; Burnett, K.; Barker, W.W.; Duara, R. Predictors of appraisal and psychological well-being in Alzheimer’s disease family caregivers. J. Clin. Geropsychol. 2000, 6, 279–297. [Google Scholar] [CrossRef]
- Hasson-Ohayon, I.; Goldzweig, G.; Braun, M.; Galinsky, D. Women with advanced breast cancer and their spouses: Diversity of support and psychological distress. Psychooncology 2010, 19, 1195–1204. [Google Scholar] [CrossRef]
- Hobbs, T.R. Depression in the caregiving mothers of adult schizophrenics: A test of the resource deterioration model. Community Ment. Health J. 1997, 33, 387–399. [Google Scholar] [CrossRef]
- Hwang, B.; Howie-Esquivel, J.; Fleischmann, K.E.; Stotts, N.A.; Dracup, K. Family caregiving in pulmonary arterial hypertension. Heart Lung 2012, 41, 26–34. [Google Scholar] [CrossRef]
- Jeong, A.; An, J.Y. The moderating role of social support on depression and anxiety for gastric cancer patients and their family caregivers. PLoS ONE 2017, 12, e0189808. [Google Scholar] [CrossRef]
- Khusaifan, S.J.; El Keshky, M.E.S. Social support as a mediator variable of the relationship between depression and life satisfaction in a sample of Saudi caregivers of patients with Alzheimer’s disease. Int. Psychogeriatr. 2017, 29, 239–248. [Google Scholar] [CrossRef]
- Kiral, K.; Yetim, Ü.; Özge, A.; Aydin, A. The relationships between coping strategies, social support and depression: An investigation among Turkish care-givers of patients with dementia. Ageing Soc. 2017, 37, 167–187. [Google Scholar] [CrossRef]
- Koerner, S.S.; Shirai, Y.; Kenyon, D.B. Sociocontextual circumstances in daily stress reactivity among caregivers for elder relatives. J. Gerontol. B Psychol. Sci. Soc. Sci. 2010, 65, 561–572. [Google Scholar] [CrossRef] [PubMed]
- Kruithof, W.J.; Post, M.W.M.; van Mierlo, M.L.; van den Bos, G.A.M.; de Man-van Ginkel, J.M.; Visser-Meily, J.M.A. Caregiver burden and emotional problems in partners of stroke patients at two months and one year post-stroke: Determinants and prediction. Patient Educ. Couns. 2016, 99, 1632–1640. [Google Scholar] [CrossRef] [PubMed]
- Kuscu, M.K.; Dural, U.; Onen, P.; Yaşa, Y.; Yayla, M.; Basaran, G.; Turhal, s.; Bekiroğlu, N. The association between individual attachment patterns, the perceived social support, and the psychological well-being of Turkish informal caregivers. Psycho-Oncol. 2009, 18, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Lakey, B.; Adams, K.; Neely, L.; Rhodes, G.; Lutz, C.J.; Sielky, K. Perceived support and low emotional distress: The role of enacted support, dyad similarity, and provider personality. Pers. Soc. Psychol. Bull. 2002, 28, 1546–1555. [Google Scholar] [CrossRef]
- Lee, H.J.; Seo, J.M.; Ahn, S.H. The role of social support in the relationship between stress and depression among family caregivers of older adults with dementia. J. Korean Acad. Nurs. 2003, 33, 713–721. [Google Scholar] [CrossRef]
- Leibach, G. Examining the Relations Between the Mental Health and Physical Health of Caregivers of MS in a Mexican Sample. Master’s Thesis, Virginia Commonwealth University, Richmond, VA, USA, 2013. [Google Scholar]
- Li, L.W.; Seltzer, M.M.; Greenberg, J.S. Social support and depressive symptoms: Differential patterns in wife and daughter caregivers. J. Gerontol. B Psychol. Sci. Soc. Sci. 1997, 52, S200–S211. [Google Scholar] [CrossRef]
- Li, M.; Mao, W.; Chi, I.; Lou, V.W. Geographical proximity and depressive symptoms among adult child caregivers: Social support as a moderator. Aging Ment. Health 2019, 23, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Losada, A.; Márquez-González, M.; Knight, B.G.; Yanguas, J.; Sayegh, P.; Romero-Moreno, R. Psychosocial factors and caregivers’ distress: Effects of familism and dysfunctional thoughts. Aging Ment. Health 2010, 14, 193–202. [Google Scholar] [CrossRef]
- Luchsinger, J.A.; Tipiani, D.; Torres-Patiño, G.; Silver, S.; Eimicke, J.P.; Ramirez, M.; Teresi, J.; Mittelman, M. Characteristics and mental health of Hispanic dementia caregivers in New York City. Am. J. Alzheimer’s Dis. Other Dement. 2015, 30, 584–590. [Google Scholar] [CrossRef]
- Majerovitz, S. Predictors of burden and depression among nursing home family caregivers. Aging Ment. Health 2007, 11, 323–329. [Google Scholar] [CrossRef]
- Malone Beach, E.E.; Zarit, S.H. Dimensions of social support and social conflict as predictors of caregiver depression. Int. Psychogeriatr. 1995, 7, 25–38. [Google Scholar] [CrossRef]
- Manso Martínez, M.E.; Sánchez López, M.d.P.; Cuéllar Flores, I. Salud y sobrecarga percibida en personas cuidadoras familiares de una zona rural. Clin Salud 2013, 24, 37–45. [Google Scholar] [CrossRef][Green Version]
- Moral Serrano, M.; Juan Ortega, J.; López Matoses, M.J.; Pellicer Magraner, P. Perfil y riesgo de morbilidad psíquica en cuidadores de pacientes ingresados en su domicilio. Aten. Primaria 2003, 32, 77–83. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Neri, A.L.; Yassuda, M.S.; Fortes-Burgos, A.C.G.; Mantovani, E.P.; Arbex, F.S.; Torres, S.V.d.S.; Perracini, M.R.; Guariento, M.E. Relationships between gender, age, family conditions, physical and mental health, and social isolation of elderly caregivers. Int. Psychogeriatr. 2012, 24, 472–483. [Google Scholar] [CrossRef]
- Pagel, M.; Becker, J. Depressive thinking and depression: Relations with personality and social resources. J. Personal. Soc. Psychol. 1987, 52, 1043. [Google Scholar] [CrossRef]
- Pagnini, F.; Rossi, G.; Lunetta, C.; Banfi, P.; Castelnuovo, G.; Corbo, M.; Molinari, E. Burden, depression, and anxiety in caregivers of people with amyotrophic lateral sclerosis. Psychol. Health Med. 2010, 15, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Pearce, M.J.; Singer, J.L.; Prigerson, H.G. Religious coping among caregivers of terminally ill cancer patients: Main effects and psychosocial mediators. J. Health Psychol. 2006, 11, 743–759. [Google Scholar] [CrossRef]
- Rapp, S.R.; Shumaker, S.; Schmidt, S.; Naughton, M.; Anderson, R. Social resourcefulness: Its relationship to social support and wellbeing among caregivers of dementia victims. Aging Ment. Health 1998, 2, 40–48. [Google Scholar] [CrossRef]
- Rauktis, M.E.; Koeske, G.F.; Tereshko, O. Negative social interactions, distress, and depression among those caring for a seriously and persistently mentally III relative. Am. J. Community Psychol. 1995, 23, 279–299. [Google Scholar] [CrossRef]
- Rivera, P.A.; Rose, J.M.; Futterman, A.; Lovett, S.B.; Gallagher-Thompson, D. Dimensions of perceived social support in clinically depressed and nondepressed female caregivers. Psychol. Aging 1991, 6, 232. [Google Scholar] [CrossRef]
- Rivera-Navarro, J.; Sepúlveda, R.; Contador, I.; Fernández-Calvo, B.; Ramos, F.; Tola-Arribas, M.Á.; Goñi, M. Detection of maltreatment of people with dementia in Spain: Usefulness of the Caregiver Abuse Screen (CASE). Eur. J. Ageing 2018, 15, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Robinson, K.M. Predictors of depression among wife caregivers. Nurs. Res. 1989, 38, 359–363. [Google Scholar] [CrossRef]
- Robinson, K.M.; Kaye, J. The relationship between spiritual perspective, social support, and depression in caregiving and noncaregiving wives. Sch. Inq. Nurs. Pract. 1994, 8, 375–389. [Google Scholar]
- Rodakowski, J.; Skidmore, E.R.; Rogers, J.C.; Schulz, R. Does social support impact depression in caregivers of adults ageing with spinal cord injuries? Clin. Rehabil. 2013, 27, 565–575. [Google Scholar] [CrossRef]
- Rodi, N. Understanding Posttraumatic Stress Symptoms in Caregivers and Relatives of Adults Surviving Cancer; Hofstra University: Hempstead, NY, USA, 2015. [Google Scholar]
- Sahin, Z.A.; Tan, M. Loneliness, depression, and social support of patients with cancer and their caregivers. Clin. J. Oncol. Nurs. 2012, 16, 2. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sandoval, F.; Tamiya, N.; Lloyd-Sherlock, P.; Noguchi, H. The relationship between perceived social support and depressive symptoms in informal caregivers of community-dwelling older persons in Chile. Psychogeriatrics 2019, 19, 547–556. [Google Scholar] [CrossRef]
- Schulz, R.; Williamson, G.M. A 2-year longitudinal study of depression among Alzheimer’s caregivers. Psychol. Aging 1991, 6, 569. [Google Scholar] [CrossRef]
- Schumacher, K.L.; Dodd, M.J.; Paul, S.M. The stress process in family caregivers of persons receiving chemotherapy. Res. Nurs. Health 1993, 16, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, K.A.; Roberts, B.L. Social support and strain of family caregivers of older adults. Holist. Nurs. Pract. 2000, 14, 77–90. [Google Scholar] [CrossRef]
- Scicolone, M.A. Examining Pathways of the Caregiver Burden-Health Relationship in Family Caregivers of Elderly Veterans: The Importance of Caregiver Self-Efficacy and Social Support; The University of Alabama: Tuscaloosa, AL, USA, 2018. [Google Scholar]
- Serrani, D. Influencia de apoyo social y uso de servicios de salud sobre la depresión en cuidadores de adultos mayores en zona rural. Rev. Chil. Salud Pública 2014, 18, 61–71. [Google Scholar] [CrossRef]
- Serrano-Ortega, N. Afrontamiento, Sobrecarga Subjetiva y Ansiedad y Síntomas Depresivos en Personas Cuidadoras de Familiares Mayores Dependientes. Ph.D. Thesis, University of Jaén, Jaén, Spain, 2017. [Google Scholar]
- Shaughnessy, V. The Impact of Mild Cognitive Impairment on Spouses: A Multi-Modal Investigation; York University: Toronto, ON, Canada, 2011. [Google Scholar]
- Shukri, M.; Mustofai, M.A.; Md Yasin, M.A.S.; Tuan Hadi, T.S. Burden, quality of life, anxiety, and depressive symptoms among caregivers of hemodialysis patients: The role of social support. Int. J. Psychiatry Med. 2020, 55, 397–407. [Google Scholar] [CrossRef]
- Speer, D.C. Predicting Parkinson’s Disease patient and caregiver adjustment: Preliminary findings. Behav. Health Aging 1993, 3, 139–146. [Google Scholar]
- Steffen, A.M.; McKibbin, C.; Zeiss, A.M.; Gallagher-Thompson, D.; Bandura, A. The revised scale for caregiving self-efficacy: Reliability and validity studies. J. Gerontol. B Psychol. Sci. Soc. Sci. 2002, 57, 74–86. [Google Scholar] [CrossRef] [PubMed]
- Stevens, L.F.; Perrin, P.B.; Gulin, S.B.; Rogers, H.L.; Cabrera, T.V.; Jiménez-Maldonado, M.; Arango-Lasprilla, J.C. Examining the influence of three types of social support on the mental health of Mexican caregivers of individuals with traumatic brain injury. Am. J. Phys. Med. Rehabil. 2013, 92, 959–967. [Google Scholar] [CrossRef]
- Tang, F.; Jang, H.; Lingler, J.; Tamres, L.K.; Erlen, J.A. Stressors and caregivers’ depression: Multiple mediators of self-efficacy, social support, and problem-solving skill. Soc. Work Health Care 2015, 54, 651–668. [Google Scholar] [CrossRef]
- Thielemann, P.A. Coping Style and Social Support Effects on Depression in Spousal Caregivers of Patients with Advanced Lung Cancer; University of South Florida: Tampa, FL, USA, 2001. [Google Scholar]
- Verez Cotelo, N.; Andrés Rodríguez, N.F.; Fornos Pérez, J.A.; Andrés Iglesias, J.C.; Ríos Lago, M. Burden and associated pathologies in family caregivers of Alzheimer’s disease patients in Spain. Pharm. Pract. 2015, 13, 2. [Google Scholar] [CrossRef]
- Yen, W.; Lundeen, S. The association between meaning of caregiving, perceived social support and level of depression of Taiwanese caregivers of mentally ill patients. Int. J. Psychiatr. Nurs. Res. 2006, 12, 1378–1392. [Google Scholar] [PubMed]
- Yoon, H. Factors associated with family caregivers’ burden and depression in Korea. Int. J. Aging Hum. Dev. 2003, 57, 291–311. [Google Scholar] [CrossRef]
- Yun, S. Application of the Sociocultural Stress and Coping Model on Spousal Caregivers of Korean Older Adults; University of Colorado Springs: Colorado Springs, CO, USA, 2023. [Google Scholar]
- Schiller, V.F.; Dorstyn, D.S.; Taylor, A.M. The Protective Role of Social Support Sources and Types Against Depression in Caregivers: A Meta-Analysis. J. Autism Dev. Disord. 2021, 51, 1304–1315. [Google Scholar] [CrossRef]
- Santini, Z.I.; Koyanagi, T.; Tyrovolas, S.; Mason, C.; Haro, J.M. The association between social relationships and depression: A systematic review. J. Affect. Disord. 2015, 175, 53–65. [Google Scholar] [CrossRef]
- Tengku Mohd, T.A.M.; Yunus, R.M.; Hairi, F.; Hairi, N.N.; Choo, W.Y. Social support and depression among community dwelling older adults in Asia: A systematic review. BMJ Open 2019, 9, e026667. [Google Scholar] [CrossRef] [PubMed]
- Del-Pino-Casado, R.; Frias-Osuna, A.; Palomino-Moral, P.A.; Ruzafa-Martinez, M.; Ramos-Morcillo, A.J. Social support and subjective burden in caregivers of adults and older adults: A meta-analysis. PLoS ONE 2018, 13, e0189874. [Google Scholar] [CrossRef]
- Priego-Cubero, E.; Orgeta, V.; López-Martínez, C.; del-Pino-Casado, R. The Relationship between Social Support and Anxiety Symptoms in Informal Carers: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 1244. [Google Scholar] [CrossRef]
- Cohen, S.; Gottlieb, B.H.; Underwood, L.G. (Eds.) Social relationships and health. In Social Support Measurement and Intervention: A Guide for Health and Social Scientists; Oxford University Press: New York, NY, USA, 2000; pp. 3–25. [Google Scholar]
- Dam, A.E.; de Vugt, M.E.; Klinkenberg, I.P.; Verhey, F.R.; van Boxtel, M.P. A systematic review of social support interventions for caregivers of people with dementia: Are they doing what they promise? Maturitas 2016, 85, 117–130. [Google Scholar] [CrossRef]
- Rui, J.R.; Guo, J. Differentiating the stress buffering functions of perceived versus received social support. Curr. Psychol. 2022, 42, 13432–13442. [Google Scholar] [CrossRef]
- Grey, I.; Arora, T.; Thomas, J.; Saneh, T.; Tohme, P.; Abi-Habib, R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. 2020, 293, 113452. [Google Scholar] [CrossRef] [PubMed]
- Uchino, B.N. Understanding the links between social support and physical health: A life-span perspective with emphasis on the separability of perceived and received support. Perspect. Psychol. Sci. 2009, 4, 236–255. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).