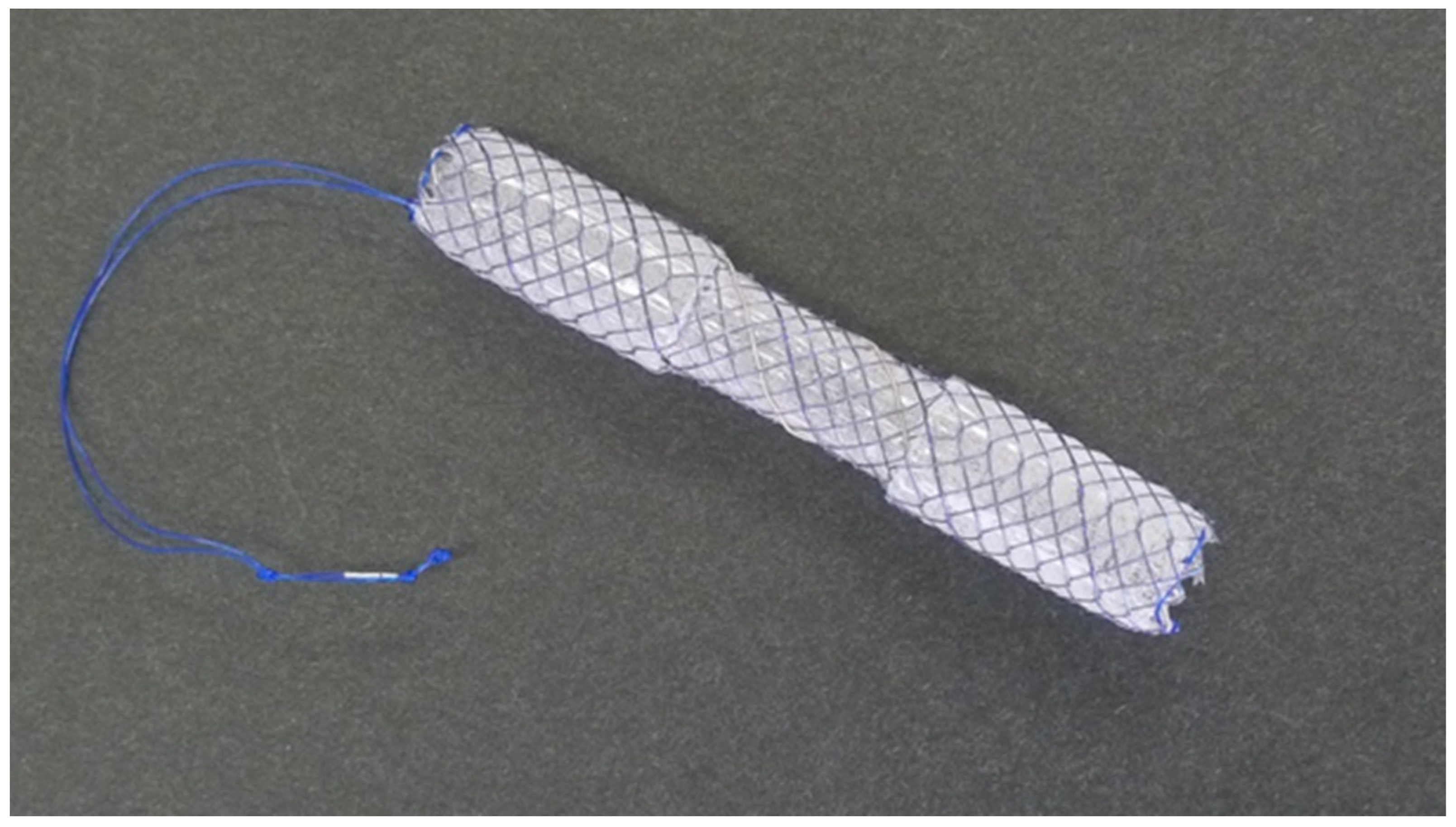
Usefulness of Intraductal Placement of a Dumbbell-Shaped Fully Covered Self-Expandable Metal Stent for Post-Cholecystectomy Bile Leaks
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Procedures
2.3. Follow-Up
2.4. Outcome Measures and Definitions
2.5. Statistics
3. Results
3.1. Flowchart and Characteristics of the Study Patients
3.2. Outcomes
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rustagi, T.; Aslanian, H.R. Endoscopic management of biliary leaks after laparoscopic cholecystectomy. J. Clin. Gastroenterol. 2014, 48, 674–678. [Google Scholar] [CrossRef]
- Fatima, J.; Barton, J.G.; Grotz, T.E.; Geng, Z.; Harmsen, W.S.; Huebner, M.; Baron, T.H.; Kendrick, M.L.; Donohue, J.H.; Que, F.G.; et al. Is there a role for endoscopic therapy as a definitive treatment for post-laparoscopic bile duct injuries? J. Am. Coll. Surg. 2010, 211, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Llach, J.; Bordas, J.M.; Elizalde, J.I.; Enrico, C.; Ginès, A.; Pellisé, M.; Mondelo, F.; Piqué, J.M. Sphincterotomy in the treatment of biliary leakage. Hepatogastroenterology 2002, 49, 1496–1498. [Google Scholar]
- Sandha, G.S.; Bourke, M.J.; Haber, G.B.; Kortan, P.P. Endoscopic therapy for bile leak based on a new classification: Results in 207 patients. Gastrointest. Endosc. 2004, 60, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Marks, J.M.; Ponsky, J.L.; Shillingstad, R.B.; Singh, J. Biliary stenting is more effective than sphincterotomy in the resolution of biliary leaks. Surg. Endosc. 1998, 12, 327–330. [Google Scholar] [CrossRef] [PubMed]
- Shah, J.N. Endoscopic treatment of bile leaks: Current standards and recent innovations. Gastrointest. Endosc. 2007, 65, 1069–1072. [Google Scholar] [CrossRef]
- Aksoz, K.; Unsal, B.; Yoruk, G.; Buyrac, Z.; Haciyanli, M.; Akpinar, Z.; Alper, E. Endoscopic sphincterotomy alone in the management of low-grade biliary leaks due to cholecystectomy. Dig. Endosc. 2009, 21, 158–161. [Google Scholar] [CrossRef] [PubMed]
- Mavrogiannis, C.; Liatsos, C.; Papanikolaou, I.S.; Karagiannis, S.; Galanis, P.; Romanos, A. Biliary stenting alone versus biliary stenting plus sphincterotomy for the treatment of post-laparoscopic cholecystectomy biliary leaks: A prospective randomized study. Eur. J. Gastroenterol. Hepatol. 2006, 18, 405–409. [Google Scholar] [CrossRef]
- Katsinelos, P.; Kountouras, J.; Paroutoglou, G.; Chatzimavroudis, G.; Germanidis, G.; Zavos, C.; Pilpilidis, I.; Paikos, D.; Papaziogas, B. A comparative study of 10-Fr vs. 7-Fr straight plastic stents in the treatment of postcholecystectomy bile leak. Surg. Endosc. 2008, 22, 101–106. [Google Scholar] [CrossRef]
- Singh, V.; Singh, G.; Verma, G.R.; Gupta, R. Endoscopic management of postcholecystectomy biliary leakage. Hepatobiliary Pancreat. Dis. Int. 2010, 9, 409–413. [Google Scholar] [PubMed]
- Fasoulas, K.; Zavos, C.; Chatzimavroudis, G.; Trakateli, C.; Vasiliadis, T.; Ioannidis, A.; Kountouras, J.; Katsinelos, P. Eleven-year experience on the endoscopic treatment of post-cholecystectomy bile leaks. Ann. Gastroenterol. 2011, 24, 200–205. [Google Scholar]
- Kim, K.H.; Kim, T.N. Endoscopic management of bile leakage after cholecystectomy: A single-center experience for 12 years. Clin. Endosc. 2014, 47, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Canena, J.; Horta, D.; Coimbra, J.; Meireles, L.; Russo, P.; Marques, I.; Ricardo, L.; Rodrigues, C.; Capela, T.; Carvalho, D.; et al. Outcomes of endoscopic management of primary and refractory postcholecystectomy biliary leaks in a multicentre review of 178 patients. BMC Gastroenterol. 2015, 15, 105. [Google Scholar] [CrossRef] [PubMed]
- Yachimski, P.; Orr, J.K.; Gamboa, A. Endoscopic plastic stent therapy for bile leaks following total vs subtotal cholecystectomy. Endosc. Int. Open 2020, 8, E1895–E1899. [Google Scholar] [CrossRef] [PubMed]
- Celik, M.; Yilmaz, H.; Kilic, M.C.; Soykan, M.; Akbudak, I.H.; Ozban, M.; Yilmaz, M. Efficacy and safety of endoscopic retrograde cholangiopancreatography with endoscopic sphincterotomy and biliary stenting in post-operative bile leaks. Ulus. Travma Acil Cerrahi Derg. 2023, 29, 904–908. [Google Scholar]
- Juza, R.M.; Pauli, E.M. Endoscopic Management of Acute Biliopancreatic Disorders. J. Gastrointest. Surg. 2019, 23, 1055–1068. [Google Scholar] [CrossRef]
- Sultan, A.M.; Elnakeeb, A.M.; Elshobary, M.M.; El-Geidi, A.A.; Salah, T.; El-Hanafy, E.A.; Atif, E.; Hamdy, E.; Elebiedy, G.K. Management of post-cholecystectomy biliary fistula according to type of cholecystectomy. Endosc. Int. Open 2015, 3, E91–E98. [Google Scholar] [CrossRef] [PubMed]
- Ljubicic, N.; Biscanin, A.; Pavic, T.; Nikolic, M.; Budimir, I.; Mijic, A.; Duzel, A. Biliary leakage after urgent cholecystectomy: Optimization of endoscopic treatment. World J. Gastrointest. Endosc. 2015, 7, 547–554. [Google Scholar] [CrossRef]
- Kahaleh, M.; Sundaram, V.; Condron, S.L.; De La Rue, S.A.; Hall, J.D.; Tokar, J.; Friel, C.M.; Foley, E.F.; Adams, R.B.; Yeaton, P. Temporary placement of covered self-expandable metallic stents in patients with biliary leak: Midterm evaluation of a pilot study. Gastrointest. Endosc. 2007, 66, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.Y.; Ellen, K.; Berg, C.L.; Schmitt, T.M.; Kahaleh, M. Fully covered self-expandable metallic stents in the management of complex biliary leaks: Preliminary data—A case series. Endoscopy 2009, 41, 781–786. [Google Scholar] [CrossRef] [PubMed]
- Baron, T.H. Covered self-expandable metal stents for benign biliary tract diseases. Curr. Opin. Gastroenterol. 2011, 27, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.C.; Kim, J.H.; Yoo, B.M.; Lim, S.G.; Kim, J.H.; Kim, W.H.; Kim, M.W. Temporary placement of a newly designed, fully covered, self-expandable metal stent for refractory bile leaks. Gut Liver 2011, 5, 96–99. [Google Scholar] [CrossRef] [PubMed]
- Akbar, A.; Irani, S.; Baron, T.H.; Topazian, M.; Petersen, B.T.; Gostout, C.J.; Levy, M.J.; Gan, I.; Gluck, M.; Ross, A.; et al. Use of covered self-expandable metal stents for endoscopic management of benign biliary disease not related to stricture (with video). Gastrointest. Endosc. 2012, 76, 196–201. [Google Scholar] [CrossRef]
- Canena, J.; Liberato, M.; Meireles, L.; Marques, I.; Romao, C.; Coutinho, A.P.; Neves, B.C.; Veiga, P.M. A non-randomized study in consecutive patients with postcholecystectomy refractory biliary leaks who were managed endoscopically with the use of multiple plastic stents or fully covered self-expandable metal stents (with videos). Gastrointest. Endosc. 2015, 82, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Irani, S.; Baron, T.H.; Law, R.; Akbar, A.; Ross, A.S.; Gluck, M.; Gan, I.; Kozarek, R.A. Endoscopic treatment of nonstricture-related benign biliary diseases using covered self-expandable metal stents. Endoscopy 2015, 47, 315–321. [Google Scholar] [CrossRef]
- Moon, J.H.; Choi, H.J.; Koo, H.C.; Han, S.H.; Lee, T.H.; Cho, Y.D.; Park, S.H.; Kim, S.J. Feasibility of placing a modified fully covered self-expandable metal stent above the papilla to minimize stent-induced bile duct injury in patients with refractory benign biliary strictures (with videos). Gastrointest. Endosc. 2012, 75, 1080–1085. [Google Scholar] [CrossRef]
- Koch, M.; Garden, O.J.; Padbury, R.; Rahbari, N.N.; Adam, R.; Capussotti, L.; Fan, S.T.; Yokoyama, Y.; Crawford, M.; Makuuchi, M.; et al. Bile leakage after hepatobiliary and pancreatic surgery: A definition and grading of severity by the International Study Group of Liver Surgery. Surgery 2011, 149, 680–688. [Google Scholar] [CrossRef]
- Cotton, P.B.; Eisen, G.M.; Aabakken, L.; Baron, T.H.; Hutter, M.M.; Jacobson, B.C.; Mergener, K.; Nemcek, A., Jr.; Petersen, B.T.; Petrini, J.L.; et al. A lexicon for endoscopic adverse events: Report of an ASGE workshop. Gastrointest. Endosc. 2010, 71, 446–454. [Google Scholar] [CrossRef]
- Lam, R.; Muniraj, T. Fully covered metal biliary stents: A review of the literature. World J. Gastroenterol. 2021, 27, 6357–6373. [Google Scholar] [CrossRef]
- Vlaemynck, K.; Lahousse, L.; Vanlander, A.; Piessevaux, H.; Hindryckx, P. Endoscopic management of biliary leaks: A systematic review with meta-analysis. Endoscopy 2019, 51, 1074–1081. [Google Scholar] [CrossRef]
- Irani, S.; Baron, T.H.; Akbar, A.; Lin, O.S.; Gluck, M.; Gan, I.; Ross, A.S.; Petersen, B.T.; Topazian, M.; Kozarek, R.A. Endoscopic treatment of benign biliary strictures using covered self-expandable metal stents (CSEMS). Dig. Dis. Sci. 2014, 59, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Kawakubo, K.; Isayama, H.; Nakai, Y.; Togawa, O.; Sasahira, N.; Kogure, H.; Sasaki, T.; Matsubara, S.; Yamamoto, N.; Hirano, K.; et al. Risk factors for pancreatitis following transpapillary self-expandable metal stent placement. Surg. Endosc. 2012, 26, 771–776. [Google Scholar] [CrossRef] [PubMed]
- Takeda, T.; Sasaki, T.; Mie, T.; Furukawa, T.; Kanata, R.; Kasuga, A.; Matsuyama, M.; Ozaka, M.; Sasahira, N. Novel risk factors for recurrent biliary obstruction and pancreatitis after metallic stent placement in pancreatic cancer. Endosc. Int. Open 2020, 8, E1603–E1610. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, K.; Nakai, Y.; Mizuno, S.; Sato, T.; Noguchi, K.; Kanai, S.; Suzuki, T.; Hakuta, R.; Ishigaki, K.; Saito, K.; et al. Endoscopic Bridge-and-Seal of Bile Leaks Using a Fully Covered Self-Expandable Metallic Stent above the Papilla. J. Clin. Med. 2022, 11, 6019. [Google Scholar] [CrossRef]
- Rainio, M.; Lindstrom, O.; Udd, M.; Haapamaki, C.; Nordin, A.; Kylanpaa, L. Endoscopic Therapy of Biliary Injury After Cholecystectomy. Dig. Dis. Sci. 2018, 63, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Murata, J.; Shigekawa, M.; Ishii, S.; Suda, T.; Ikezawa, K.; Hirao, M.; Matsumoto, K.; Kegasawa, T.; Iwahashi, K.; Iio, S.; et al. Efficacy and associated factors of endoscopic transpapillary drainage for postoperative biliary leakage. DEN Open 2024, 4, e281. [Google Scholar] [CrossRef]


| Age | 73.5 (51–87) |
| Sex, male | 2 (33) |
| ASA-PS | 2.5 (2–4) |
| CCI | 6 (2–7) |
| Primary disease, AC/GBS | 3 (50)/3 (50) |
| Type of surgery, laparoscopic/open | 4 (67)/2 (33) |
| Site of leak, cystic duct stump/common bile duct | 5 (83)/1 (17) |
| Severity of leak, low-grade/high-grade | 3 (50)/3 (50) |
| Timing of intervention, primary/conversion from ENBD | 3 (50)/3 (50) |
| Time from surgery to ERCP, days | 10 (3–34) |
| Length of D-SEMS, 50 mm/60 mm | 4 (67)/2 (33) |
| Diameter of D-SEMS, 10 mm/8 mm | 5 (83)/1 (17) |
| Technical success | 6 (100) |
| Clinical success | 5 (83) |
| Time to the clinical success, days | 5 (3–24) |
| Early adverse events (mild pancreatitis) | 1 (17) |
| Late adverse events (stent–stone complex) | 1 (17) |
| D-SEMS indwelling period, days | 61 (42–606) |
| Follow-up period after index ERCP, days | 761 (161–1392) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakagawa, K.; Matsubara, S.; Suda, K.; Otsuka, T.; Oka, M.; Nagoshi, S. Usefulness of Intraductal Placement of a Dumbbell-Shaped Fully Covered Self-Expandable Metal Stent for Post-Cholecystectomy Bile Leaks. J. Clin. Med. 2023, 12, 6530. https://doi.org/10.3390/jcm12206530
Nakagawa K, Matsubara S, Suda K, Otsuka T, Oka M, Nagoshi S. Usefulness of Intraductal Placement of a Dumbbell-Shaped Fully Covered Self-Expandable Metal Stent for Post-Cholecystectomy Bile Leaks. Journal of Clinical Medicine. 2023; 12(20):6530. https://doi.org/10.3390/jcm12206530
Chicago/Turabian StyleNakagawa, Keito, Saburo Matsubara, Kentaro Suda, Takeshi Otsuka, Masashi Oka, and Sumiko Nagoshi. 2023. "Usefulness of Intraductal Placement of a Dumbbell-Shaped Fully Covered Self-Expandable Metal Stent for Post-Cholecystectomy Bile Leaks" Journal of Clinical Medicine 12, no. 20: 6530. https://doi.org/10.3390/jcm12206530
APA StyleNakagawa, K., Matsubara, S., Suda, K., Otsuka, T., Oka, M., & Nagoshi, S. (2023). Usefulness of Intraductal Placement of a Dumbbell-Shaped Fully Covered Self-Expandable Metal Stent for Post-Cholecystectomy Bile Leaks. Journal of Clinical Medicine, 12(20), 6530. https://doi.org/10.3390/jcm12206530







