Long-Term Health-Related Quality of Life (QOL) after Paediatric Spinal Deformity Surgery and Comparison with the General Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Questionnaires
2.2. Statistical Analysis
3. Results
- A.
- Patients with AIS
- B.
- Patients with congenital scoliosis
- C.
- Patients with syndromic/secondary scoliosis
- D.
- Patients with Scheuermann kyphosis
- E.
- Patients with low-grade isthmic spondylolisthesis
- F.
- Patients with high-grade dysplastic spondylolisthesis
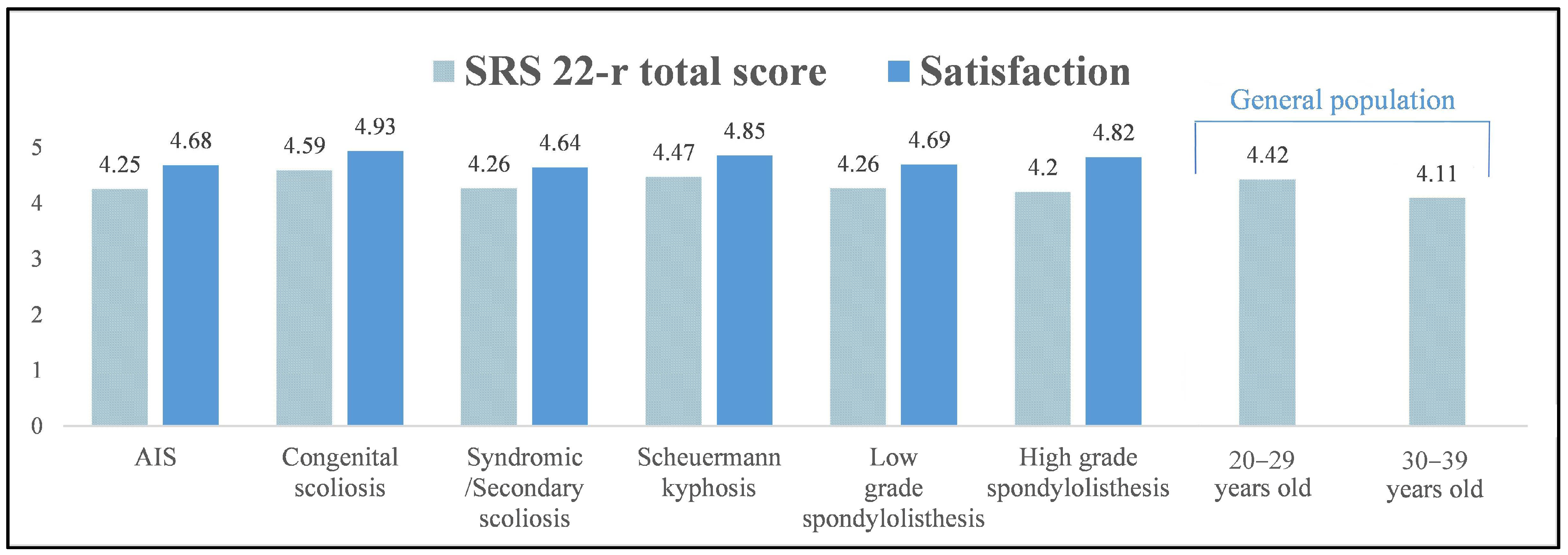
3.1. Comparison of QOL among Different Spinal Conditions
3.2. Comparison of QOL between Patients with Spinal Conditions and the General Population
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weinstein, S.; Dolan, L.; Cheng, J.; Danielsson, A.; Morcuende, J. Adolescent idiopathic scoliosis. Lancet 2008, 371, 1527–1537. [Google Scholar] [CrossRef] [PubMed]
- Asher, M.; Lai, S.M.; Burton, D.; Manna, B. The influence of spine and trunk defoirity on preoperative idiopathic scoliosis patients’ health-related quality of life questionnaire responses. Spine 2004, 29, 861–868. [Google Scholar] [CrossRef] [PubMed]
- Glassman, S.; Berven, S.; Bridwell, K.; Horton, W.; Dimar, J. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 2005, 30, 682–688. [Google Scholar] [CrossRef]
- Leidi, N.K.; Revicki, D.A.; Geneste, B. Recommendations for evaluating the validity of quality of life claims for labeling and promotion. Value Health 1999, 2, 113–127. [Google Scholar] [CrossRef] [PubMed]
- Akazawa, T.; Kotani, T.; Sakuma, T.; Iijima, Y.; Torii, Y.; Ueno, J.; Umehara, T.; Iinuma, M.; Yoshida, A.; Tomochika, K.; et al. Health-related quality of life of patients with adolescent idiopathic scoliosis at least 40 years after surgery. Spine 2023, 48, 501–506. [Google Scholar] [CrossRef]
- Danielsson, A.J.; Nachemson, A.L. Back pain and function 23 years after fusion for adolescent idiopathic scoliosis: A case-control study-part II. Spine 2003, 28, E373–E383. [Google Scholar] [CrossRef]
- Simony, A.; Hansen, E.J.; Carreon, L.Y.; Christensen, S.B.; Andersen, M.O. Health-related quality-of-life in adolescent idiopathic scoliosis patients 25 years after treatment. Scoliosis 2015, 10, 22. [Google Scholar] [CrossRef]
- Iida, T.; Suzuki, N.; Kono, K.; Ohyama, Y.; Imura, J.; Ato, A.; Ozeki, S.; Nohara, Y. Minimum 20 years long-term clinical outcome after spinal fusion and instrumentation for scoliosis: Comparison of the SRS-22 patient questionnaire with that in nonscoliosis group. Spine 2015, 40, E922–E928. [Google Scholar] [CrossRef]
- Darnis, A.; Grobost, P.; Roussouly, P. Very long-term clinical and radiographic outcomes after posterior spinal fusion with pedicular screws for thoracic adolescent idiopathic scoliosis. Spine Deform. 2021, 9, 441–449. [Google Scholar] [CrossRef]
- Benli, I.T.; Ates, B.; Akalin, S.; Citak, M.; Kaya, A.; Alanay, A. Minimum 10 years follow-up surgical results of adolescent idiopathic scoliosis patients treated with TSRH instrumentation. Eur. Spine J. 2007, 16, 381–391. [Google Scholar] [CrossRef]
- Helenius, I.; Remes, V.; Lamnberg, T.; Schlenzka, D.; Poussa, M. Long-term health-related quality of life after surgery for adolescent idiopathic scoliosis and spondylolisthesis. J. Bone Jt. Surg. Am. 2008, 90, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Tsirikos, A.I.; Wordie, S.J. Population-based normative data for the Scoliosis Research Society 22r, EQ-5D, and VAS questionnaires among individuals aged 20 to 69 years. Bone Jt. Open 2022, 3, 130–134. [Google Scholar] [CrossRef]
- Asher, M.; Lai, S.M.; Burton, D.; Manna, B. The reliability and concurrent validity of the SRS-22 patient questionnaire for idiopathic scoliosis. Spine 2003, 28, 63–69. [Google Scholar] [CrossRef]
- McKean, G.M.; Tsirikos, A.I. Quality of life in children and adolescents undergoing spinal deformity surgery. J. Back. Musculoskelet. Rehabil. 2017, 30, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Diarbakerli, E.; Grauers, A.; Gerdhem, P. Population-based normative data for the Scoliosis Research Society 22r questionnaire in adolescents and adults, including a comparison with EQ-5D. Eur. Spine J. 2017, 26, 1631–1637. [Google Scholar] [CrossRef] [PubMed]
- EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Rabin, R.; de Charro, F. EQ-5D: A measure of health status from the EuroQol Group. Ann. Med. 2001, 33, 337–343. [Google Scholar] [CrossRef]
- Dolan, P. Modelling valuations for EuroQol health states. Med. Care 1997, 35, 1095–1108. [Google Scholar] [CrossRef]
- Boonstra, A.M.; Schiphordt Preuper, H.R.; Reneman, M.; Posthumus, J.B.; Stewart, R.E. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 2008, 31, 165–169. [Google Scholar] [CrossRef]
- Tsirikos, A.I.; Sud, A.; McGurk, S.M. Radiographic and functional outcome of posterolateral lumbosacral fusion for low grade isthmic spondylolisthesis in children and adolescents. Bone Jt. J. 2016, 98, 88–96. [Google Scholar] [CrossRef]
- Schlösser, T.P.C.; Garrido, E.; Tsirikos, A.I.; McMaster, M.J. Health-related quality of life and sagittal balance at two to 25 years after posterior transfixation for high-grade dysplastic spondylolisthesis. Bone Jt. Open 2021, 2, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Asher, M.A.; Burton, D.C. Adolescent idiopathic scoliosis: Natural history and long term treatment effects. Scoliosis 2006, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, S.L.; Dolan, L.A.; Spratt, K.F.; Peterson, K.K.; Spoonamore, M.J.; Ponseti, I.V. Health and function of patients with untreated idiopathic scoliosis: A 50-year natural history study. JAMA 2003, 289, 559–567. [Google Scholar] [CrossRef]
- Farshad, M.; Kutschke, L.; Laux, C.J.; Kabelitz, M.; Schupbach, R.; Böni, T.; Jentzsch, T. Extreme long-term outcome of operatively versus conservatively treated patients with adolescent idiopathic scoliosis. Eur. Spine J. 2020, 29, 2084–2090. [Google Scholar] [CrossRef] [PubMed]
- Lenke, L.G.; Bridwell, K.H.; Baldus, C.; Blanke, K.; Schoenecker, P.L. Cotrel-Dubousset instrumentation for adolescent idiopathic scoliosis. J. Bone Jt. Surg. 1992, 74, 1056–1067. [Google Scholar] [CrossRef]
- Bjerkreim, I.; Steen, H.; Brox, J.I. Idiopathic scoliosis treated with Cotrel-Dubousset instrumentation: Evaluation 10 years after surgery. Spine 2007, 32, 2103–2110. [Google Scholar] [CrossRef]
- Takayama, K.; Nakamura, H.; Matsuda, H. Low back pain in patients treated surgically for scoliosis: Longer than sixteen-year follow up. Spine 2009, 34, 2198–2204. [Google Scholar] [CrossRef]
- Kibsgard, T.; Brox, J.I.; Reikeras, O. Physical and mental health in young adults operated on for idiopathic scoliosis. J. Orthop. Sci. 2004, 9, 360–363. [Google Scholar] [CrossRef]
- Green, D.W.; Lawhorne, T.W.I.I.I.; Widmann, R.F.; Kepler, C.K.; Ahern, C.; Mintz, D.N.; Rawlins, B.A.; Burke, S.W.; Boachie-Adjei, O. Long-term magnetic resonance imaging follow-up demonstrates minimal transitional level lumbar disc degeneration after posterior spine fusion for adolescent idiopathic scoliosis. Spine 2011, 36, 1948–1954. [Google Scholar] [CrossRef]



| Diagnosis | Secondary Scoliosis | Syndromic Scoliosis |
|---|---|---|
| Congenital cardiac disease | 21 | - |
| Syringomyelia | 18 | - |
| Chiari I malformation/syringomyelia | 26 | - |
| Chiari I malformation | 7 | - |
| Congenital cardiac disease, Chiari I malformation/syringomyelia | 1 | - |
| Spinal cord tethering | 1 | - |
| Marfan syndrome | - | 4 |
| Neurofibromatosis type I | - | 4 |
| Di George syndrome | - | 2 |
| Osteogenesis imperfecta (OI) | - | 2 |
| Klippel–Trenaunay–Weber syndrome | - | 2 |
| Turner syndrome | - | 2 |
| Undiagnosed syndrome | - | 2 |
| Asperger’s syndrome | - | 1 |
| Ehlers–Danlos syndrome | - | 1 |
| Chromosome abnormality | - | 2 |
| Coffin–Siris syndrome | - | 1 |
| Dandy–Walker syndrome | - | 1 |
| Opitz G syndrome | - | 1 |
| Intraspinal tumour | 2 | - |
| Pilocytic astrocytoma | 1 | - |
| AIS Group | Function | Pain | Self-Image | Mental Health | Satisfaction | Total Score |
|---|---|---|---|---|---|---|
| Preoperative (993 patients) | 4.04 (range: 1.8–5) | 3.86 (range: 1.4–5) | 3.16 (range: 2–5) | 3.84 (range: 1.4–5) | - | 3.7 (range: 1.95–5) |
| 6 months postoperative (993 patients) | 3.81 (range: 1.8–5) | 4.24 (range: 1.4–5) | 4.25 (range: 2–5) | 4.1 (range: 1.4–5) | 4.77 (range: 1.5–5) | 4.15 (range: 1.09–5) |
| 12 months postoperative (993 patients) | 4.29 (range: 2.6–5) | 4.42 (range: 1.4–5) | 4.28 (range: 2–5) | 4.23 (range: 1–5) | 4.81 (range: 2.5–5) | 4.35 (range: 2.41–5) |
| 24 months postoperative (993 patients) | 4.43 (range: 2.4–5) | 4.51 (range: 2.2–5) | 4.32 (range: 1.2–5) | 4.2 (range: 1.4–5) | 4.78 (range: 2–5) | 4.4 (range: 1.95–5) |
| 5–10 years postoperative (560 patients) | 4.39 (range: 1.2–5) | 4.45 (range: 1.2–5) | 4.32 (range: 1–5) | 4.01 (range: 1–5) | 4.77 (range: 1–5) | 4.44 (range: 1.55–4.95) |
| >10 years postoperative (220 patients) | 4.29 (range: 2–5) | 4.35 (range: 1.2–5) | 4.21 (range: 2–5) | 3.99 (range: 1.8–5) | 4.68 (range: 3–5) | 4.25 (range: 2.18–5) |
| Congenital Scoliosis Group | Function | Pain | Self-Image | Mental Health | Satisfaction | Total Score |
|---|---|---|---|---|---|---|
| Preoperative (80 patients) | 3.98 (range: 2.4–4.8) | 3.94 (range: 1.8–5) | 3.22 (range: 1.6–4.6) | 3.98 (range: 1.2–5) | - | 3.77 (range: 1.75–4.6) |
| 6 months postoperative (80 patients) | 3.67 (range: 1.6–4.8) | 4.23 (range: 2.8–5) | 3.91 (range: 2.6–4.8) | 4.28 (range: 2.2–5) | 4.77 (range: 3–5) | 4.09 (range: 2.55–4.68) |
| 12 months postoperative (80 patients) | 3.98 (range: 2.4–4.8) | 4.37 (range: 2.8–5) | 4.08 (range: 2–5) | 4.11 (range: 2–5) | 4.86 (range: 3–5) | 4.2 (range: 2.36–4.77) |
| 24 months postoperative (80 patients) | 4.39 (range: 3.4–4.8) | 4.46 (range: 2.6–5) | 4.08 (range: 2.4–5) | 4.16 (range: 1.8–5) | 4.64 (range: 2–5) | 4.31 (range: 3–5) |
| 5–10 years postoperative (65 patients) | 4.39 (range: 3.8–4.8) | 4.68 (range: 3.4–5) | 4.24 (range: 2.4–5) | 4.4 (range: 2.6–5) | 4.75 (range: 2.5–5) | 4.46 (range: 3.36–4.95) |
| >10 years postoperative (45 patients) | 4.49 (range: 4–5) | 4.63 (range: 3.8–5) | 4.62 (range: 3.75–5) | 4.49 (range: 3–5) | 4.93 (range: 4.5–5) | 4.59 (range: 4.18–4.91) |
| Syndromic and Secondary Scoliosis Group | Function | Pain | Self-Image | Mental Health | Satisfaction | Total Score |
|---|---|---|---|---|---|---|
| Preoperative (102 patients) | 3.97 (range: 3–4.8) | 3.79 (range: 1.8–5) | 2.99 (range: 1–5) | 3.61 (range: 1–5) | - | 3.58 (range: 2.09–4.6) |
| 6 months postoperative (102 patients) | 3.64 (range: 2–5) | 4.22 (range: 2.2–5) | 4.11 (range: 3–5) | 3.97 (range: 2.6–5) | 4.78 (range: 4–5) | 4.06 (range: 3.27–4.91) |
| 12 months postoperative (102 patients) | 4.22 (range: 2.97–5) | 4.5 (range: 3–5) | 4.33 (range: 1.6–5) | 4.26 (range: 1.6–5) | 4.81 (range: 3.5–5) | 4.37 (range: 2.91–5) |
| 24 months postoperative (102 patients) | 4.47 (range: 3.2–5) | 4.67 (range: 3.6–5) | 4.41 (range: 2.8–5) | 4.34 (range: 1.8–5) | 4.85 (range: 3.5–5) | 4.51 (range: 3.49–4.95) |
| 5–10 years postoperative (72 patients) | 4.34 (range: 3–5) | 4.53 (range: 3.4–5) | 4.44 (range: 3.4–5) | 4.32 (range: 2.8–5) | 4.8 (range: 2.5–5) | 4.44 (range: 3.73–4.95) |
| >10 years postoperative (36 patients) | 4.17 (range: 2.6–4.8) | 4.11 (range: 3.2–5) | 4.31 (range: 3.6–5) | 4.29 (range: 3.4–5) | 4.64 (range: 4–5) | 4.26 (range: 3.36–4.77) |
| Scheuermann Kyphosis Group | Function | Pain | Self-Image | Mental Health | Satisfaction | Total Score |
|---|---|---|---|---|---|---|
| Preoperative (105 patients) | 3.81 (range: 1.75–5) | 3.5 (range: 1.2–5) | 2.82 (range: 1–5) | 3.54 (range: 1.4–5) | - | 3.44 (range: 1.88–4.9) |
| 6 months postoperative (105 patients) | 3.56 (range: 1.8–5) | 4.23 (range: 2.4–5) | 4.24 (range: 3–5) | 3.94 (range: 2.4–5) | 4.84 (range: 4–5) | 4.07 (range: 3.18–4.95 |
| 12 months postoperative (105 patients) | 4.13 (range: 2.8–5) | 4.43 (range: 2.6–5) | 4.35 (range: 3–5) | 4.16 (range: 2.8–5) | 4.8 (range: 3–5) | 4.31 (range: 3.32–5) |
| 24 months postoperative (105 patients) | 4.27 (range: 2.8–5) | 4.52 (range: 2.4–5) | 4.41 (range: 2.4–5) | 4.2 (range: 2–5) | 4.82 (range: 3–5) | 4.39 (range: 2.95–5) |
| 5–10 years postoperative (82 patients) | 4.46 (range: 2.2–5) | 4.56 (range: 2.6–5) | 4.6 (range: 3.4–5) | 4.21 (range: 2–5) | 4.92 (range: 4–5) | 4.5 (range: 3.09–5) |
| >10 years postoperative (69 patients) | 4.51 (range: 3.2–5) | 4.5 (range: 3–5) | 4.47 (range: 1.6–5) | 4.27 (range: 2.2–5) | 4.85 (range: 3.5–5) | 4.47 (range: 2.59–5) |
| Low-Grade Spondylolisthesis Group | Function | Pain | Self-Image | Mental Health | Satisfaction | Total Score |
|---|---|---|---|---|---|---|
| Preoperative (40 patients) | 3.30 (range: 2.2–4.6) | 3 (range: 2–4.6) | 3.4 (range: 2.4–4.2) | 3.73 (range: 1.6–4.8) | - | 3.31 (range: 2.25–4.45) |
| 6 months postoperative (40 patients) | 3.85 (range: 2.4–5) | 4.04 (range: 1.8–5) | 4.09 (range: 2.4–5) | 3.95 (range: 3.2–5) | 4.89 (range: 3.5–5) | 4.06 (range: 2.55–5) |
| 12 months postoperative (40 patients) | 4.21 (range: 2.6–5) | 4.03 (range: 2–5) | 4.17 (range: 3.2–5) | 3.83 (range: 1.4–5) | 4.75 (range: 3.5–5) | 4.12 (range: 2.86–5) |
| 24 months postoperative (40 patients) | 4.25 (range: 2.4–5) | 4.19 (range: 1–5) | 4.18 (range: 2.6–5) | 4.19 (range: 2–5) | 4.68 (range: 4–5) | 4.24 (range: 2.35–5) |
| 5–10 years postoperative (35 patients) | 4.09 (range: 1.8–5) | 4.28 (range: 2–5) | 4.26 (range: 2.4–5) | 4.02 (range: 2–5) | 4.72 (range: 4.5–5) | 4.21 (range: 2.68–4.86) |
| >10 years postoperative (30 patients) | 4.28 (range: 2.8–5) | 4.37 (range: 2–5) | 4.14 (range: 3–5) | 4.09 (range: 2.4–5) | 4.69 (range: 4–5) | 4.26 (range: 2.91–4.86) |
| High-Grade Spondylolisthesis Group | Function | Pain | Self-Image | Mental Health | Satisfaction | Total Score |
|---|---|---|---|---|---|---|
| Preoperative (34 patients) | 3.49 (range: 1.8–4.4) | 3.23 (range: 1.6–4.2) | 3.51 (range: 2–4.5) | 4.03 (range: 2.4–5) | - | 3.57 (range: 2.3–4.5) |
| 6 months postoperative (34 patients) | 4.25 (range: 3.7–4.6) | 4.32 (range: 3.5–4.7) | 4.18 (range: 3–4.4) | 4.1 (range: 3.1–4.8) | 4.6 (range: 4–5) | 4.23 (range: 2.85–5) |
| 12 months postoperative (34 patients) | 4.4 (range: 4.2–5) | 4.43 (range: 3.8–4.65) | 4.32 (range: 3.5–4.7) | 4.26 (range: 3.6–5) | 4.75 (range: 4–5) | 4.52 (range: 3.24–5) |
| 24 months postoperative (34 patients) | 4.64 (range: 4.33–5) | 4.57 (range: 3.8–5) | 4.58 (range: 3.8–5) | 4.35 (range: 3.6–5) | 4.94 (range: 4–5) | 4.57 (range: 4.23–4.91) |
| 5–10 years postoperative (32 patients) | 4.13 (range: 2.2–5) | 4.04 (range: 2.2–5) | 3.91 (range: 2–5) | 3.95 (range: 2.2–5) | 4.36 (range: 4–5) | 4.04 (range: 2.14–4.82) |
| >10 years postoperative (28 patients) | 4.19 (range: 2.4–5) | 4.23 (range: 2–5) | 4.08 (range: 1.6–5) | 4.05 (range: 1.6–5) | 4.82 (range: 4–5) | 4.2 (range: 2.27–4.91) |
| AIS | Congenital Scoliosis | Syndromic and Secondary Scoliosis | Scheuermann Kyphosis | Spondylolisthesis | ||
|---|---|---|---|---|---|---|
| High Grade | Low Grade | |||||
| (993 patients) | (80 patients) | (102 patients) | (105 patients) | (34 patients) | (40 patients) | |
| Preoperative | 3.7 (range: 1.95–5) | 3.77 (range: 1.75–4.6) | 3.58 (range: 2.09–4.6) | 3.44 (range: 1.88–4.9) | 3.57 (range: 2.3–4.5) | 3.31 (range: 2.25–4.45) |
| 6 months postoperative | 4.15 (range: 1.09–5) | 4.09 (range: 2.55–4.68) | 4.06 (range: 3.27–4.91) | 4.07 (range: 3.18–4.95) | 4.23 (range: 2.85–5) | 4.06 (range: 2.55–5) |
| 12 months postoperative | 4.35 (range: 2.41–5) | 4.2 (range: 2.36–4.77) | 4.37 (range: 2.91–5) | 4.31 (range: 3.32–5) | 4.52 (range: 3.24–5) | 4.12 (range: 2.86–5) |
| 24 months postoperative | 4.4 (range: 1.95–5) | 4.31 (range: 3–5) | 4.51 (range: 3.45–4.95) | 4.39 (range: 2.95–5) | 4.57 (range: 4.23–4.91) | 4.24 (range: 2.35–5) |
| 5–10 years postoperative | 4.34 (range: 1.55–4.95) | 4.46 (range: 3.36–4.95) | 4.44 (range: 3.73–4.95) | 4.5 (range: 3.09–5) | 4.04 (range: 2.14–4.82) | 4.21 (range: 2.68–4.86) |
| >10 years postoperative | 4.25 (range: 2.18–5.00) | 4.59 (range: 4.18–4.91) | 4.26 (range: 3.36–4.77) | 4.47 (range: 2.59–5) | 4.2 (range: 2.27–4.91) | 4.26 (range: 2.91–4.86) |
| AIS | Congenital Scoliosis | Syndromic and Secondary Scoliosis | Scheuermann Kyphosis | Spondylolisthesis | General Population | |||
|---|---|---|---|---|---|---|---|---|
| High Grade | Low Grade | 20–29 Years Old | 30–39 Years Old | |||||
| (220 patients) | (45 patients) | (36 patients) | (69 patients) | (28 patients) | (30 patients) | (183 people) | (115 people) | |
| Mean age (years) | 29.5 (range: 23.5–37) | 28.3 (range: 20–35) | 30.2 (range: 28–33) | 30.1 (range: 25–34) | 37 (range: 25–55) | 27.1 (range: 21.1–33) | 25 (range: 20–29) | 34 (range: 30–39) |
| Function | 4.29 (range: 2–5) | 4.49 (range: 4–5) | 4.17 (range: 2.6–4.8) | 4.51 (range: 3.2–5) | 4.19 (range: 2.4–5) | 4.28 (range: 2.8–5) | 4.51 (range: 2–5) | 4.23 (range: 2.6–5) |
| Pain | 4.35 (range: 1.2–5) | 4.63 (range: 3.8–5) | 4.11 (range: 3.2–5) | 4.50 (range: 3–5) | 4.23 (range: 2–5) | 4.37 (range: 2–5) | 4.58 (range: 1.8–5) | 4.3 (range: 1.6–5) |
| Self-image | 4.21 (range: 2–5) | 4.62 (range: 3.75–5) | 4.31 (range: 3.6–5) | 4.47 (range: 1.6–5) | 4.08 (range: 1.6–5) | 4.14 (range: 3–5) | 4.37 (range: 1.8–5) | 4.04 (range: 2.4–5) |
| Mental health | 3.99 (range: 1.8–5) | 4.49 (range: 3–5) | 4.29 (range: 3.4–5) | 4.27 (range: 2.2–5) | 4.05 (range: 1.6–5) | 4.09 (range: 2.4–5) | 4.22 (range: 2.4–5.6) | 3.87 (range: 2–5) |
| Total score | 4.25 (range: 2.18–5) | 4.59 (range: 4.18–4.91) | 4.26 (range: 3.36–4.77) | 4.47 (range: 2.59–5) | 4.2 (range: 2.27–4.91) | 4.26 (range: 2.91–4.86) | 4.42 (range: 2.42–5) | 4.11 (range: 2.47–4.89) |
| AIS | Congenital Scoliosis | Syndromic and Secondary Scoliosis | Scheuermann Kyphosis | Spondylolisthesis | General Population | |||
|---|---|---|---|---|---|---|---|---|
| High Grade | Low Grade | 20–29 Years Old | 30–39 Years Old | |||||
| (220 patients) | (45 patients) | (36 patients) | (69 patients) | (28 patients) | (30 patients) | (183 people) | (115 people) | |
| Mean age (years) | 29.5 (range: 23.5–37) | 28.3 (range: 20–35) | 30.2 (range: 28–33) | 30.1 (range: 25–34) | 37 (range: 25–55) | 27.1 (range: 21.1–33) | 25 (range: 20–29) | 34 (range: 30–39) |
| EQ-5D VAS | 83.64 (range: 70–100) | 87.7 (range: 70–99) | 83.2 (range: 30–90) | 87.69 (range: 60–100) | 82.6 (range: 40–95) | 83.4 (range: 40–99) | 86 (range: 25–100) | 83 (range: 40–100) |
| EQ-5D index | 0.83 (range: 0.13–1) | 0.91 (range: 0.8–1) | 0.84 (range: 0.18–1) | 0.89 (range: 0.1–1) | 0.81 (range: 0.1–1) | 0.83 (range: 0.16–1) | 0.91 (range: 0.06–1) | 0.85 (range: 0–1) |
| VAS back pain | 1.62 (range: 0–9) | 0.75 (range: 0–3) | 1.69 (range: 0–9.2) | 0.61 (range: 0–2.7) | 1.82 (range: 0–6) | 1.74 (range: 0–6) | 1.12 (range: 0–8) | 1.7 (range: 0–8) |
| VAS leg pain | 0.9 (range: 0–9) | 0.3 (range: 0–3) | 1.1 (range: 0–8) | 0.57 (range: 0–6) | 1.8 (range: 0–8) | 1.75 (range: 0–6) | 0.75 (range: 0–9) | 1.32 (range: 0–10) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsirikos, A.I.; García-Martínez, S. Long-Term Health-Related Quality of Life (QOL) after Paediatric Spinal Deformity Surgery and Comparison with the General Population. J. Clin. Med. 2023, 12, 7142. https://doi.org/10.3390/jcm12227142
Tsirikos AI, García-Martínez S. Long-Term Health-Related Quality of Life (QOL) after Paediatric Spinal Deformity Surgery and Comparison with the General Population. Journal of Clinical Medicine. 2023; 12(22):7142. https://doi.org/10.3390/jcm12227142
Chicago/Turabian StyleTsirikos, Athanasios I., and Silvia García-Martínez. 2023. "Long-Term Health-Related Quality of Life (QOL) after Paediatric Spinal Deformity Surgery and Comparison with the General Population" Journal of Clinical Medicine 12, no. 22: 7142. https://doi.org/10.3390/jcm12227142





