Activity-Based Therapy for Mobility, Function and Quality of Life after Spinal Cord Injuries—A Mixed-Methods Case Series
Abstract
:1. Introduction
2. Materials and Methods
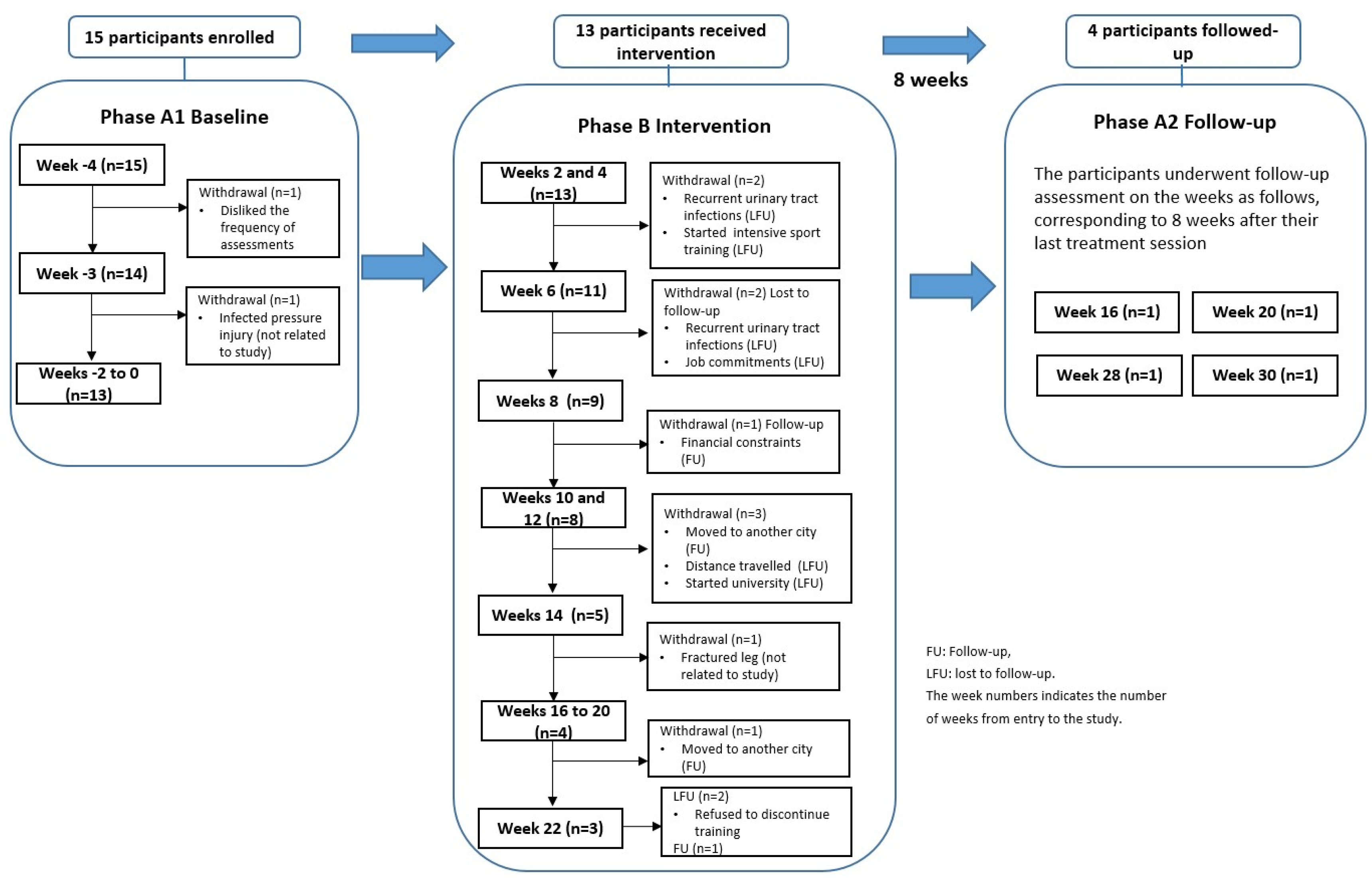
2.1. Study Design
2.2. Participants
2.3. ABT Program
2.4. Outcome Measures
2.5. Interviews
2.6. Data Analysis
2.7. Qualitative Analysis
3. Results
3.1. Participants
3.2. Sitting Balance
3.3. Mobility
3.4. Quality of Life
3.5. Secondary Outcomes
3.6. Retention and Adherence
3.7. Maintenance of Effects
3.8. Adverse Events
3.9. Participants’ Perceptions and Experiences
3.9.1. Theme 1: The Impact That My Disability Has in My Life Has Decreased (Sense of Life as before)
“The improvement is just unbelievable. So, for me, that’s the best thing about it, and the bad thing about it is I can’t do it more times than I do. I really enjoy it.”(P8)
“Before I wouldn’t have gone out of the golf club, now I go out to the golf course and walk around a bit, and even around the restaurant after having dinner and a few drinks and staying around rather than just not doing any social activities at all.”(P5)
“It’s not just the functional benefits. It’s the psychological and emotional positives that come out of it. Feeling more confident and feeling better, having more independence. I think that’s what most people want to gain after they’ve had an injury.”(P2)
“I’m eating with whatever utensils I have. I can actually remove them from my lap to the table without any assistance... I can grab the remote, work the remote from the shelf in my room onto my lap to access the TV if I want…I found eating most types of food that I’ve had trouble with beforehand have been a lot easier, like holding something like a burger.”(P1)
3.9.2. Theme 2: The Program Is Different from (Superior to) Usual Rehabilitation
“For me, is all about getting out of my chair. When you are in the chair you are mainly just restricted to doing weights, maybe a bit of trunk. When you get out of the chair at least you can stretch your whole body. You use everything. You try different exercises. You not only work out what you have but just test out and try and work out things that are weaker or that you don’t have.”(P2)
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Key Elements of Multimodal ABT
- Active-assisted exercises: Performed on a plinth or mat in supine, prone or side-lying position. The therapist assisted the lower-limb movements through different ranges of motion, and when possible provided resistance. Participants were encouraged to attempt and visualise actively assisting or resisting the movement performed.
- Resistance training for upper and/or lower limbs: Used when a participant demonstrated voluntary motor control and consisted of concentric and eccentric exercises against gravity or adding external resistance, such as weights or resistance bands.
- Load bearing: Consists of activities on hands or elbows and/or feet or knees in contact with the ground, with some percentage of body weight supported through the extremities. While on hands and knees or in the kneeling position, the participant is encouraged to perform upper- and lower-body movements, in order to enhance trunk and pelvic control. Crawling and locomotion in the kneeling position were also performed.
- Standing with or without standing frames: Participants stand with the assistance of a frame and are encouraged to perform trunk and arm movements, or if able, to raise themselves into a standing position to load the lower extremities, using the parallel bars, and perform lower-limb movements, until fatigue.
- Partial body weight using antigravity board: Participants complete active and/or active-assisted squat exercises (unilateral or bilateral) while partially loading their lower extremities. Participants also perform exercises for postural control in a seated position with partial body weight borne through their lower limbs.
- Leg ergometry: Using a stationary exercise bicycle, the participants are seated with trunk support provided by a therapist, if necessary, and attempt to pedal the bike under his/her own power. If unable to do so, manual external assistance is provided to complete the movement.
- Electrically stimulated leg ergometry: While seated in their wheelchair or in a chair with back support, the gluteus maximus, hamstrings, quadriceps, triceps surae and tibialis anterior could be electrically stimulated by surface electrodes, according to the participant’s needs to produce a cycling movement. Leg ergometry could also be conducted in a standing position with electrodes on the gluteus maximus, hamstrings, gastrocnemius, quadriceps and the tibialis anterior muscle groups with body-weight support and assistance of a robotic stepping device that simulates gait movements.
- Gait training or supported ambulation: Involves different forms of gait training, including body-weight-supported treadmill training with or without FES or manual external assistance, overground training with a frame with or without manual external assistance, or treadmill training without support, according to participants’ locomotor capability. These activities sometimes required assistance from up to four therapists, depending on the participant’s ability to control their trunk and lower limbs.
- Vibration training: The aim of this intervention is to promote sensory input putatively to alter muscle spindle sensitivity to stretch and modulate reflex alpha motoneuron activation of muscle contractions. Exercises are performed with the feet in contact with an oscillatory platform in either a seated or standing position.
- Task-specific training: According to the participant’s goals and abilities, this involves bed mobility, transfers, balance in sitting or standing, walking mobility and postural changes.
Appendix B. Semi-Structured Interview
- (1)
- Tell me about your experiences during the period that you were in the ABT program?
- -
- I want to know the good things and the things that weren’t good as well.
- (2)
- Tell me about the benefits (changes) that you’ve got from the program?
- -
- Physically/Functionally?
- -
- Socially?
- -
- Emotionally/Psychologically/Well being?
- -
- Family/carers?
- (3)
- What is your opinion about the program? Could you tell me on a scale from 0–10 your opinion about the program, being 0: really bad and 10: really great.
- (4)
- What are your feelings about the program? How do you feel about it?
- (5)
- Tell me about the logistics during the period that you were in the program?
- -
- Time
- -
- Transport
- (6)
- Is there anything else that you would like to tell me?
Appendix C
| Outcome | Model | AIC | BIC |
|---|---|---|---|
| QoL | Random Intercept | 475.8 | 476.9 |
| Random Intercept + Slope | 477.8 | 479.5 | |
| MRMI | Random Intercept | 325.3 | 326.4 |
| Random Intercept + Slope | * | * | |
| SRD | Random Intercept | −154.3 | −153.2 |
| Random Intercept + Slope | * | * |
Appendix D. Secondary Outcomes
| Outcome Measure | Baseline Mean ± SD | Post-Intervention Mean ± SD | Change Score Mean ± SD | 95% CI | t Value | p-Value | Effect Sizes (Cohen’s d) |
|---|---|---|---|---|---|---|---|
| SCIM | 46.7 ± 24.7 | 48.9 ± 25.9 | 2.2 ± 3.2 | 0.3 to 4.2 | 2.52 | 0.027 * | 0.09 (very small) |
| CIQ | 16.5 ± 3.9 | 18.2 ± 4.6 | 1.7 ± 2.3 | 0.3 to 3.1 | 2.62 | 0.023 * | 0.41 (small) |
| SWLS | 18.3 ± 4.9 | 20.3 ± 7.5 | 2 ± 4.1 | −0.5 to 4.4 | 1.78 | 0.101 | - |
Appendix E. Changes at Follow-Up
| Outcome Measures | Baseline | Post-Intervention | % Change from Baseline to Post-Intervention | Follow-Up | % Change from Post-Intervention to Follow-Up |
|---|---|---|---|---|---|
| Participant1 | |||||
| QoLI | 23.3 ± 0.8 | 26.9 | 16 | 27.2 | 1 |
| MRMI | 6.8 ± 0.4 | 9.0 | 32 | 9.0 | 0 |
| SRD | 1.1 ± 0.0 | 1.2 | 10 | 1.2 | 1 |
| SCIM | 26.0 | 27.0 | 4 | 30 | 11 |
| CIQ | 14.5 | 15.8 | 9 | 18.6 | 18 |
| SWLS | 24.0 | 28.0 | 17 | 24.0 | −14 |
| Participant 2 | |||||
| QoLI | 23.3 ± 1.0 | 22.8 | −2 | 21.3 | −7 |
| MRMI | 7.6 ± 0.6 | 9.0 | 18 | 9.0 | 0 |
| SRD | 0.8 ± 0.1 | 1.0 | 23 | 0.9 | −4 |
| SCIM | 25.0 | 28.0 | 12 | 30.0 | 7 |
| CIQ | 22.0 | 22.0 | 0 | 22.0 | 0 |
| SWLS | 19.0 | 23.0 | 21 | 17.0 | 26 |
| Participant 5 | |||||
| QoLI | 16.6 ± 0.5 | 14.2 | −15 | 14.2 | 0 |
| MRMI | 38 ± 0.0 | 40 | 5 | 40.0 | 0 |
| SRD | 1.3 ± 0.2 | 1.4 | 11 | 1.4 | 0 |
| SCIM | 71.0 | 73.0 | 3 | 79.0 | 8 |
| CIQ | 11.3 | 15.0 | 33 | 16.0 | 7 |
| SWLS | 17.0 | 12.0 | −29 | 13.0 | 8 |
| Participant 7 | |||||
| QoLI | 21.7 ± 1.4 | 23.3 | 8 | 24.7 | 6 |
| MRMI | 39.0 ± 0.0 | 40.0 | 3 | 40.0 | 0 |
| SRD | 1.7 ± 0.1 | 1.8 | 2 | 1.7 | −5 |
| SCIM | 81.0 | 92.0 | 14 | 94.0 | 2 |
| CIQ | 16.4 | 22.0 | 34 | 16.5 | −25 |
| SWLS | 26.0 | 28.0 | 8 | 29.0 | 4 |
References
- Sadowsky, C.L.; McDonald, J.W. Activity-based restorative therapies: Concepts and applications in spinal cord injury-related neurorehabilitation. Dev. Disabil. Res. Rev. 2009, 15, 112–116. [Google Scholar] [CrossRef]
- Behrman, A.L.; Bowden, M.G.; Nair, P.M. Neuroplasticity after spinal cord injury and training: An emerging paradigm shift in rehabilitation and walking recovery. Phys. Ther. 2006, 86, 1406–1425. [Google Scholar] [CrossRef]
- Field-Fote, E.C.; Lindley, S.D.; Sherman, A.L. Locomotor training approaches for individuals with spinal cord injury: A preliminary report of walking-related outcomes. J. Neurol. Phys. Ther. 2005, 29, 127–137. [Google Scholar] [CrossRef]
- Hutchinson, K.J.; Gomez-Pinilla, F.; Crowe, M.J.; Ying, Z.; Basso, D.M. Three exercise paradigms differentially improve sensory recovery after spinal cord contusion in rats. Brain 2004, 127 Pt 6, 1403–1414. [Google Scholar] [CrossRef]
- Zholudeva, L.V.; Qiang, L.; Marchenko, V.; Dougherty, K.J.; Sakiyama-Elbert, S.E.; Lane, M.A. The Neuroplastic and Therapeutic Potential of Spinal Interneurons in the Injured Spinal Cord. Trends Neurosci. 2018, 41, 625–639. [Google Scholar] [CrossRef] [PubMed]
- Gazula, V.R.; Roberts, M.; Luzzio, C.; Jawad, A.F.; Kalb, R.G. Effects of limb exercise after spinal cord injury on motor neuron dendrite stucture. J. Comp. Neurol. 2004, 476, 130–145. [Google Scholar] [CrossRef] [PubMed]
- Goldshmit, Y.; Lythgo, N.; Galea, M.P.; Turnley, A.M. Treadmill training after spinal cord hemisection in mice promotes axonal sprouting and synapse formation and improves motor recovery. J. Neurotrauma. 2008, 25, 449–465. [Google Scholar] [CrossRef]
- Walker, J.R.; Detloff, M.R. Plasticity in Cervical Motor Circuits following Spinal Cord Injury and Rehabilitation. Biology 2021, 10, 976. [Google Scholar] [CrossRef] [PubMed]
- Backus, D.; Apple, D.L.H. Systematic Review of Activity-Based Interventions to Improve Neurological Outcomes after SCI January 1998–March 2009. In Disability Research Right to Know. (n.d.). Available online: http://www.bu.edu/drrk/research-syntheses/spinal-cord-injuries/activity-based-interventions (accessed on 29 August 2023).
- Galea, M.P. Spinal cord injury and physical activity: Preservation of the body. Spinal Cord 2012, 50, 344–351. [Google Scholar] [CrossRef]
- Atkins, K.D.; Bickel, C.S. Effects of functional electrical stimulation on muscle health after spinal cord injury. Curr. Opin. Pharmacol. 2021, 60, 226–231. [Google Scholar] [CrossRef]
- Martin, R.; Sadowsky, C.; Obst, K.; Meyer, B.; McDonald, J. Functional electrical stimulation in spinal cord injury: From theory to practice. Top. Spinal Cord Inj. Rehabil. 2012, 18, 28–33. [Google Scholar] [CrossRef]
- Dromerick, A.W.; Lum, P.S.; Hidler, J. Activity-based therapies. NeuroRx 2006, 3, 428–438. [Google Scholar] [CrossRef] [PubMed]
- Harkema, S.; Behrman, A.; Barbeau, H. Evidence-based therapy for recovery of function after spinal cord injury. Handb. Clin. Neurol. 2012, 109, 259–274. [Google Scholar] [PubMed]
- de Oliveira, C.Q.; Refshauge, K.; Middleton, J.; de Jong, L.; Davis, G.M. Effects of Activity-Based Therapy Interventions on Mobility, Independence, and Quality of Life for People with Spinal Cord Injuries: A Systematic Review and Meta-Analysis. J. Neurotrauma 2017, 34, 1726–1743. [Google Scholar] [CrossRef] [PubMed]
- Harness, E.T.; Yozbatiran, N.; Cramer, S.C. Effects of intense exercise in chronic spinal cord injury. Spinal Cord 2008, 46, 733–737. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.L. Activity-based therapy for recovery of walking in individuals with chronic spinal cord injury: Results from a randomized clinical trial. Arch. Phys. Med. Rehabil. 2014, 95, 2239–2246.e2. [Google Scholar] [CrossRef]
- Galea, M.P.; Dunlop, S.A.; Geraghty, T.; Davis, G.M.; Nunn, A.; Olenko, L. SCIPA Full-On: A Randomized Controlled Trial Comparing Intensive Whole-Body Exercise and Upper Body Exercise After Spinal Cord Injury. Neurorehabil. Neural. Repair. 2018, 32, 557–567. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Green, L.W.; Klesges, L.M.; Abrams, D.B.; Fisher, E.B.; Goldstein, M.G.; Hayman, L.L.; Ockene, J.K.; Orleans, C.T. External validity: We need to do more. Ann. Behav. Med. 2006, 31, 105–108. [Google Scholar] [CrossRef]
- Green, L.W.; Glasgow, R.E. Evaluating the Relevance, Generalization, and Applicability of Research: Issues in External Validation and Translation Methodology. Eval. Health Prof. 2006, 29, 126–153. [Google Scholar] [CrossRef]
- Boswell-Ruys, C.L.; Sturnieks, D.L.; Harvey, L.A.; Sherrington, C.; Middleton, J.W.; Lord, S.R. Validity and reliability of assessment tools for measuring unsupported sitting in people with a spinal cord injury. Arch. Phys. Med. Rehabil. 2009, 90, 1571–1577. [Google Scholar] [CrossRef]
- Walsh, J.M.; Barrett, A.; Murray, D.; Ryan, J.; Moroney, J.; Shannon, M. The Modified Rivermead Mobility Index: Reliability and convergent validity in a mixed neurological population. Disabil. Rehabil. 2010, 32, 1133–1139. [Google Scholar] [CrossRef] [PubMed]
- May, L.A.; Warren, S. Measuring quality of life of persons with spinal cord injury: External and structural validity. Spinal Cord 2002, 40, 341–350. [Google Scholar] [CrossRef]
- May, L.A.; Warren, S. Measuring quality of life of persons with spinal cord injury: Substantive and structural validation. Qual. Life Res. 2001, 10, 503–515. [Google Scholar] [CrossRef] [PubMed]
- Catz, A.; Itzkovich, M.; Tesio, L.; Biering-Sorensen, F.; Weeks, C.; Laramee, M.T.; Craven, B.C.; Tonack, M.; Hitzig, S.L.; Glaser, E.; et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord 2007, 45, 275–291. [Google Scholar] [CrossRef] [PubMed]
- Kratz, A.L.; Chadd, E.; Jensen, M.P.; Kehn, M.; Kroll, T. An examination of the psychometric properties of the community integration questionnaire (CIQ) in spinal cord injury. J. Spinal Cord Med. 2015, 38, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Post, M.W.; van Leeuwen, C.M.; van Koppenhagen, C.F.; De Groot, S. Validity of the Life Satisfaction questions, the Life Satisfaction Questionnaire, and the Satisfaction With Life Scale in persons with spinal cord injury. Arch. Phys. Med. Rehabil. 2012, 93, 1832–1837. [Google Scholar] [CrossRef]
- Health NSWG. Safety Monitoring and Reporting for Clinical Trials Conducted in NSW Public Health Organisations; Health NSWG: Sydney, NSW, Australia, 2017.
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2016. [Google Scholar]
- Clarke, V.; Braun, V.; Hayfield, N. Thematic analysis. Qualitative psychology: A practical guide to research methods. In Qualitative Psychology: A Practical Guide to Research Methods; Smith, J.A., Ed.; SAGE Publications: London, UK, 2015; pp. 222–248. [Google Scholar]
- Wirth, B.; van Hedel, H.J.; Kometer, B.; Dietz, V.; Curt, A. Changes in activity after a complete spinal cord injury as measured by the Spinal Cord Independence Measure II (SCIM II). Neurorehabil. Neural. Repair 2008, 22, 279–287. [Google Scholar] [CrossRef]
- Scivoletto, G.; Tamburella, F.; Laurenza, L.; Molinari, M. The spinal cord independence measure: How much change is clinically significant for spinal cord injury subjects. Disabil. Rehabil. 2013, 35, 1808–1813. [Google Scholar] [CrossRef]
- Fawcett, J.; Curt, A.; Steeves, J.; Coleman, W.; Tuszynski, M.; Lammertse, D.; Bartlett, P.F.; Blight, A.R.; Dietz, V.; Ditunno, J.; et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the iccp panel: Spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 2006, 45, 190–205. [Google Scholar] [CrossRef]
- de Oliveira, C.Q.; Middleton, J.W.; Refhaugue, K.; Davis, G.M. Activity-Based Therapy in a community Setting for independence, mobility, and sitting balance for people with spinal cord injuries. J. Cent. Nerv. Syst. Dis. 2019, 11, 1179573519841623. [Google Scholar] [CrossRef]
- Jones, M.L.; Evans, N.; Tefertiller, C.; Backus, D.; Sweatman, M.; Tansey, K.; Morrison, S. Activity-based therapy for recovery of walking in chronic spinal cord injury: Results from a secondary analysis to determine responsiveness to therapy. Arch. Phys. Med. Rehabil. 2014, 95, 2247–2252. [Google Scholar] [CrossRef]
- Dobkin, B.; Barbeau, H.; Deforge, D.; Ditunno, J.; Elashoff, R.; Apple, D.; Basso, M.; Behrman, A.; Fugate, L.; Harkema, S.; et al. The evolution of walking-related outcomes over the first 12 weeks of rehabilitation for incomplete traumatic spinal cord injury: The multicenter randomized Spinal Cord Injury Locomotor Trial. Neurorehabilit. Neural Repair 2007, 21, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Swaffield, E.; Cheung, L.; Khalili, A.; Lund, E.; Boileau, M.; Chechlacz, D.; Musselman, K.E.; Gauthier, C. Perspectives of people living with a spinal cord injury on activity-based therapy. Disabil. Rehabil. 2022, 44, 3632–3640. [Google Scholar] [CrossRef] [PubMed]
- Rutten, I.; Van den Bogaert, L.; Geerts, D. From initial encounter with mid-air haptic feedback to repeated use: The role of the novelty effect in user experience. IEEE Trans. Haptics 2020, 14, 591–602. [Google Scholar] [CrossRef] [PubMed]
- Groeneveld, I.F.; Goossens, P.H.; van Braak, I.; van der Pas, S.; Meesters, J.J.; Mishre, R.D.R.; Arwert, H.J.; Vlieland, T.P.V.; SCORE-Study Group. Patients’ outcome expectations and their fulfilment in multidisciplinary stroke rehabilitation. Ann. Phys. Rehabil. Med. 2019, 62, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, D.N.; Mahmood, B.; Ketonis, C.; Hammert, W.C. A comparison of PROMIS physical function and pain interference scores in patients with carpal tunnel syndrome: Research collection versus routine clinical collection. HAND 2020, 15, 771–775. [Google Scholar] [CrossRef]
- Fritz, S.; Merlo-Rains, A.; Rivers, E.; Peters, D.M.; Goodman, A.; Watson, E.T.; Carmichael, B.M.; McClenaghan, B.A. An intensive intervention for improving gait, balance, and mobility in individuals with chronic incomplete spinal cord injury: A pilot study of activity tolerance and benefits. Arch. Phys. Med. Rehabil. 2011, 92, 1776–1784. [Google Scholar] [CrossRef]
- Behrman, A.L.; Harkema, S.J. Physical rehabilitation as an agent for recovery after spinal cord injury. Phys. Med. Rehabil. Clin. N. Am. 2007, 18, 183–202. [Google Scholar] [CrossRef]
- Padula, N.; Costa, M.; Batista, A.; Gaspar, R.; Motta, C.; Palma, G.; Torriani-Pasin, C. Long-term effects of an intensive interventional training program based on activities for individuals with spinal cord injury: A pilot study. Physiother. Theory Pract. 2015, 31, 568–574. [Google Scholar] [CrossRef]
- Dobkin, B.; Apple, D.; Barbeau, H.; Basso, M.; Behrman, A.; Deforge, D.; Ditunno, J.; Dudley, G.; Elashoff, R.; Fugate, L.; et al. Weight-supported treadmill vs over-ground training for walking after acute incomplete SCI. Neurology 2006, 66, 484–493. [Google Scholar] [CrossRef]
- Harkema, S.J.; Schmidt-Read, M.; Lorenz, D.J.; Edgerton, V.R.; Behrman, A.L. Balance and ambulation improvements in individuals with chronic incomplete spinal cord injury using locomotor training-based rehabilitation. Arch. Phys. Med. Rehabil. 2012, 93, 1508–1517. [Google Scholar] [CrossRef] [PubMed]
- Backus, D.; Apple, D.; Hudson, L. Neural and functional outcomes after lower extremity and walking activity-based interventions for persons with spinal cord injury: A research synthesis. Top. Spinal Cord Inj. Rehabil. 2011, 16, 72. [Google Scholar]
- Adams, M.M.; Hicks, A.L. Comparison of the effects of body-weight-supported treadmill training and tilt-table standing on spasticity in individuals with chronic spinal cord injury. J. Spinal Cord Med. 2011, 34, 488–494. [Google Scholar] [CrossRef]
- Semerjian, T.; Montague, S.; Dominguez, J.; Davidian, A.; de Leon, R. Enhancement of quality of life and body satisfaction through the use of adapted exercise devices for individuals with spinal cord injuries. Top. Spinal Cord Inj. Rehabil. 2005, 11, 95–108. [Google Scholar] [CrossRef]
- Sharif, H.; Gammage, K.; Chun, S.; Ditor, D. Effects of FES-Ambulation Training on Locomotor Function and Health-Related Quality of Life in Individuals With Spinal Cord Injury. Top. Spinal Cord Inj. Rehabil. 2014, 20, 58–69. [Google Scholar] [CrossRef] [PubMed]
- Hitzig, S.; Craven, B.; Panjwani, A.; Kapadia, N.; Giangregorio, L.; Richards, K.; Masani, K.; Popovic, M. Randomized trial of functional electrical stimulation therapy for walking in incomplete spinal cord injury: Effects on quality of life and community participation. Top. Spinal Cord Inj. Rehabil. 2013, 19, 245–258. [Google Scholar] [CrossRef]
- Harkema, S.J.; Schmidt-Read, M.; Behrman, A.L.; Bratta, A.; Sisto, S.A.; Edgerton, V.R. Establishing the NeuroRecovery Network: Multisite rehabilitation centers that provide activity-based therapies and assessments for neurologic disorders. Arch. Phys. Med. Rehabil. 2012, 93, 1498–1507. [Google Scholar] [CrossRef]
- Edgerton, V.R.; Roy, R.R. Activity-Dependent Plasticity of Spinal Locomotion: Implications for Sensory Processing. Exerc. Sport Sci. Rev. 2009, 37, 171–178. [Google Scholar] [CrossRef]
- Edgerton, V.R.; Tillakaratne, N.J.; Bigbee, A.J.; de Leon, R.D.; Roy, R.R. Plasticity of the spinal neural circuitry after injury. Annu. Rev. Neurosci. 2004, 27, 145–167. [Google Scholar] [CrossRef]
- Roy, R.R.; Harkema, S.J.; Edgerton, V.R. Basic concepts of activity-based interventions for improved recovery of motor function after spinal cord injury. Arch. Phys. Med. Rehabil. 2012, 93, 1487–1497. [Google Scholar] [CrossRef]
- Biglan, A.; Ary, D.; Wagenaar, A.C. The value of interrupted time-series experiments for community intervention research. Prev. Sci. 2000, 1, 31–49. [Google Scholar] [CrossRef] [PubMed]
- Tate, R.L.; Perdices, M.; Rosenkoetter, U.; Shadish, W.; Vohra, S.; Barlow, D.H.; Horner, R.; Kazdin, A.; Kratochwill, T.; McDonald, S.; et al. The Single-Case Reporting Guideline In BEhavioural Interventions (SCRIBE) 2016 Statement. Phys. Ther. 2016, 96, e1–e10. [Google Scholar] [CrossRef] [PubMed]



| Participant | Age (Years) | Gender | Duration Post-Injury (mo) | Level of Injury | AIS Classification | Number of Sessions Attended | Number of Sessions per Week |
|---|---|---|---|---|---|---|---|
| 1 | 22 | M | 26 | C5 | A | 43 | 4 |
| 2 | 23 | F | 10 | C5 | A | 45 | 2 |
| 3 | 37 | F | 6 | T11 | C | 46 | 2 |
| 4 | 20 | M | 11 | C4 | B | 42 | 2 |
| 5 | 54 | M | 15 | C3 | D | 16 | 2 |
| 6 | 31 | M | 12 | C4 | B | 70 | 3 |
| 7 | 20 | F | 6 | L1 | A | 52 | 2 |
| 8 | 43 | M | 30 | T4 | B | 45 | 2 |
| 9 | 23 | F | 212 | T2 | A | 15 | 2 |
| 10 | 33 | M | 121 | T12 | B | 14 | 2 |
| 11 | 56 | M | 135 | T6 | A | 11 | 2 |
| 12 | 32 | M | 9 | C5 | B | 19 | 2 |
| 13 | 23 | M | 12 | T11 | A | 15 | 2 |
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quel de Oliveira, C.; Bundy, A.; Middleton, J.W.; Refshauge, K.; Rogers, K.; Davis, G.M. Activity-Based Therapy for Mobility, Function and Quality of Life after Spinal Cord Injuries—A Mixed-Methods Case Series. J. Clin. Med. 2023, 12, 7588. https://doi.org/10.3390/jcm12247588
Quel de Oliveira C, Bundy A, Middleton JW, Refshauge K, Rogers K, Davis GM. Activity-Based Therapy for Mobility, Function and Quality of Life after Spinal Cord Injuries—A Mixed-Methods Case Series. Journal of Clinical Medicine. 2023; 12(24):7588. https://doi.org/10.3390/jcm12247588
Chicago/Turabian StyleQuel de Oliveira, Camila, Anita Bundy, James W. Middleton, Kathryn Refshauge, Kris Rogers, and Glen M. Davis. 2023. "Activity-Based Therapy for Mobility, Function and Quality of Life after Spinal Cord Injuries—A Mixed-Methods Case Series" Journal of Clinical Medicine 12, no. 24: 7588. https://doi.org/10.3390/jcm12247588
APA StyleQuel de Oliveira, C., Bundy, A., Middleton, J. W., Refshauge, K., Rogers, K., & Davis, G. M. (2023). Activity-Based Therapy for Mobility, Function and Quality of Life after Spinal Cord Injuries—A Mixed-Methods Case Series. Journal of Clinical Medicine, 12(24), 7588. https://doi.org/10.3390/jcm12247588






