Incidence of Orbital Side Effects in Zygomaticomaxillary Complex and Isolated Orbital Walls Fractures: A Retrospective Study in South Italy and a Brief Review of the Literature
Abstract
1. Introduction
2. Materials and Methods
3. Results
- Zygomatic orbital fractures, the most frequent, in 60% (242 cases)
- Fractures of the orbital floor in 26% (104 cases)
- Fractures of the medial wall in 9% (38 cases)
- Fractures of the lateral wall in 3% (12 cases)
- Fractures of the orbital roof in 1% (6 cases)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Jho Johnson, N.R.; Singh, N.R.; Oztel, M.; Vangaveti, V.N.; Rahmel, B.B.; Ramalingam, L. Ophthalmological injuries associated with fractures of the orbitozygomaticomaxillary complex. Br. J. Oral Maxillofac. Surg. 2018, 56, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Converse, J.M.; Smith, B. Blowout fracture of the floor of the orbit. Trans. Am. Acad. Ophthalmol. Otolaryngol. 1960, 64, 676–688. [Google Scholar] [PubMed]
- Cornelius, C.P.; Mayer, P.; Ehrenfeld, M.; Metzger, M.C. The orbits—Anatomical features in view of innovative surgical methods. Facial Plast. Surg. 2014, 30, 487–508. [Google Scholar] [CrossRef] [PubMed]
- Burnstine, M.A. Clinical recommendations for repair of isolated orbital floor fractures: An evidence-based analysis. Ophthalmology 2002, 109, 1207–1210. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.W.; Lim, J.S.; Yoo, G.; Byeon, J.H. An analysis of pure blowout fractures and associated ocular symptoms. J. Craniofac. Surg. 2013, 24, 703–707. [Google Scholar] [CrossRef] [PubMed]
- Tong, L.; Bauer, R.J.; Buchman, S.R. A current 10-year retrospective survey of 199 surgically treated orbital floor fractures in a nonurban tertiary care center. Plast. Reconstr. Surg. 2001, 108, 612–621. [Google Scholar] [CrossRef]
- Turvey, T.A.; Golden, B.A. Orbital anatomy for the surgeon. Oral. Maxillofac. Surg. Clin. N. Am. 2012, 24, 525–536. [Google Scholar] [CrossRef]
- Parameswaran, A.; Marimuthu, M.; Panwar, S.; Hammer, B. Orbital Fractures. In Oral and Maxillofacial Surgery for the Clinician; Bonanthaya, K., Panneerselvam, E., Manuel, S., Kumar, V.V., Rai, A., Eds.; Springer: Singapore, 2021. [Google Scholar] [CrossRef]
- Boffano, P.; Roccia, F.; Gallesio, C.; Karagozoglu, K.H.; Forouzanfar, T. Diplopia and orbital wall fractures. J. Craniofac. Surg. 2014, 25, e183–e185. [Google Scholar] [CrossRef]
- Boyette, J.R.; Pemberton, J.D.; Bonilla-Velez, J. Management of orbital fractures: Challenges and solutions. Clin. Ophthalmol. 2015, 9, 2127–2137. [Google Scholar] [CrossRef]
- Ellis, E., 3rd; el-Attar, A.; Moos, K.F. An analysis of 2067 cases of zygomatic-orbital fracture. J. Oral Maxillofac. Surg. 1985, 43, 417–428. [Google Scholar] [CrossRef]
- Nakamura, T.; Gross, C. Facial fractures: Analysis of five years of experience. Arch. Otolaryngol. 1973, 97, 288–290. [Google Scholar] [CrossRef] [PubMed]
- Gwyn, P.P.; Carraway, J.H.; Horton, C.E. Facial fractures-injuries and associated complications. Plast. Reconstr. Surg. 1971, 47, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Miloro, M. Peterson’s Principles of Oral and Maxillofacial Surgery; People’s Medical Publishing House: Shelton, CT, USA, 2004. [Google Scholar]
- Hauck, M.J.; Tao, J.P.; Burgett, R.A. Computed Tomography Exophthalmometry. Ophthalmic Surg. Lasers Imaging Retina 2010, 22, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Folkestad, L.; Lindgren, G.; Moller, C.; Granström, G. Diplopia in orbital fractures: A simple method to assess ocular motility. Acta Otolaryngol. 2007, 127, 156Y166. [Google Scholar] [CrossRef] [PubMed]
- Timmis, P. Exophthalmos. J. Laryngol. Otol. 1957, 71, 744–753. [Google Scholar] [CrossRef] [PubMed]
- Bartoli, D.; Fadda, M.T.; Battisti, A.; Cassoni, A.; Pagnoni, M.; Riccardi, E.; Sanzi, M.; Valentini, V. Retrospective analysis of 301 patients with orbital floor fracture. J. Craniomaxillofac. Surg. 2015, 43, 244–247. [Google Scholar] [CrossRef] [PubMed]
- Hitchin, A.D.; Shuker, S.T. Some observations on zygomatic fractures in the Eastern Region of Scotland. Br. J. Oral Surg. 1973, 11, 114–117. [Google Scholar] [CrossRef]
- Ramphul, A.; Hoffman, G. Does Preoperative Diplopia Determine the Incidence of Postoperative Diplopia After Repair of Orbital Floor Fracture? An Institutional Review. J. Oral. Maxillofac. Surg. 2017, 75, 565–575. [Google Scholar] [CrossRef]
- Burm, J.S.; Chung, C.H.; Oh, S.J. Pure orbital blowout fracture: New concepts and importance of medial orbital blowout fracture. Plast. Reconstr. Surg. 1999, 103, 1839–1849. [Google Scholar] [CrossRef]
- Higashino, T.; Hirabayashi, S.; Eguchi, T.; Kato, Y. Straightforward factors for predicting the prognosis of blow-out fractures. J. Craniofac. Surg. 2011, 22, 1210–1214. [Google Scholar] [CrossRef]
- Eun, S.C.; Heo, C.Y.; Baek, R.M.; Minn, K.W.; Chung, C.H.; Oh, S.J. Survey and review of blowout fractures. J. Korean Soc. Plast. Reconstr. Surg. 2007, 34, 599–604. [Google Scholar]
- Tahiri, Y.; Lee, J.; Tahiri, M.; Sinno, H.; Williams, B.H.; Lessard, L.; Gilardino, M.S. Preoperative diplopia: The most important prognostic factor for diplopia after surgical repair of pure orbital blowout fracture. J. Craniofac. Surg. 2010, 21, 1038–1041. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.M.; Park, J.U.; Kwon, S.T.; Kim, S.W.; Jeong, E.C. Three-dimensional pre-bent titanium implant for concomitant orbital floor and medial wall fractures in an East asian population. Arch. Plast. Surg. 2014, 41, 480–485. [Google Scholar] [CrossRef] [PubMed]
- Thiagarajah, C.; Kersten, R.C. Medial wall fracture: An update. Craniomaxillofac. Trauma Reconstr. 2009, 2, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Park, Y.; Chung, K.J. Considerations for the management of medial orbital wall blowout fracture. Arch. Plast. Surg. 2016, 43, 229–236. [Google Scholar] [CrossRef]
- Choi, S.H.; Kang, D.H.; Gu, J.H. The Correlation between the Orbital Volume Ratio and Enophthalmos in Unoperated Blowout Fractures. Arch. Plast. Surg. 2016, 43, 518–522. [Google Scholar] [CrossRef]
- Bonavolontà, P.; Dell’aversana Orabona, G.; Abbate, V.; Vaira, L.A.; Lo Faro, C.; Petrocelli, M.; Attanasi, F.; De Riu, G.; Iaconetta, G.; Califano, L. The epidemiological analysis of maxillofacial fractures in Italy: The experience of a single tertiary center with 1720 patients. J. Craniomaxillofac. Surg. 2017, 45, 1319–1326. [Google Scholar] [CrossRef]
- Orabona, G.D.; Abbate, V.; Maglitto, F.; Committeri, U.; Improta, G.; Bonavolontà, P.; Reccia, A.; Somma, T.; Iaconetta, G.; Califano, L. Postoperative Management of Zygomatic Arch Fractures: In-House Rapid Prototyping System for the Manufacture of Protective Facial Shields. J. Craniofac. Surg. 2019, 30, 2057–2060. [Google Scholar] [CrossRef]


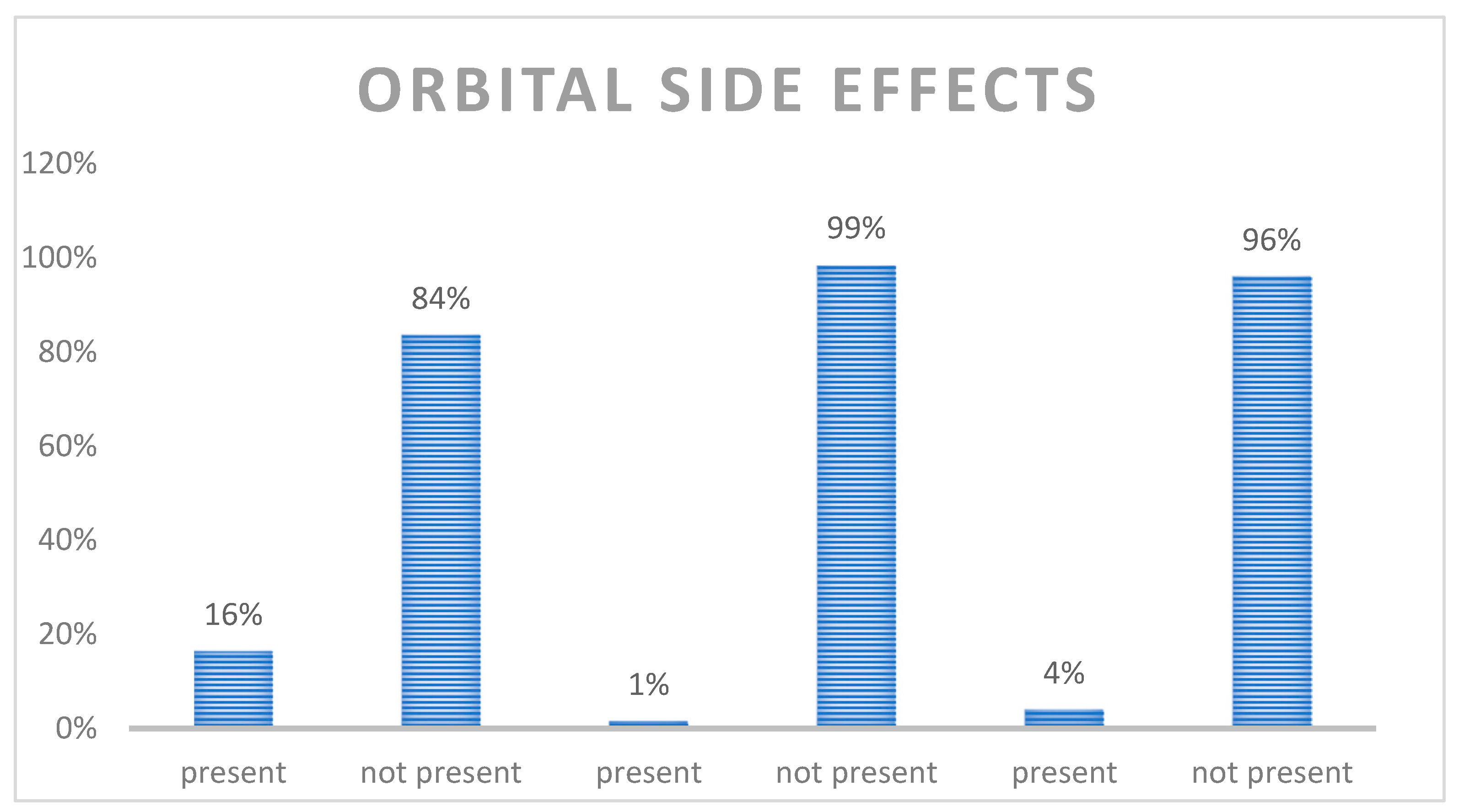


| Type of Fracture | Number of Fractures | Diplopia% |
|---|---|---|
| Orbital floor | 104 | 42% |
| Zygomaticomaxillary complex | 242 | 6% |
| Medial wall | 38 | 16% |
| Lateral walls | 12 | 17% |
| Orbital roof | 6 | 0% |
| Type of Fracture | Number of Fractures | Exhophtalmos% |
| Orbital floor | 104 | 2% |
| Zygomaticomaxillary complex | 242 | 2% |
| Medial wall | 38 | 0% |
| Lateral walls | 12 | 0% |
| Orbital roof | 6 | 0% |
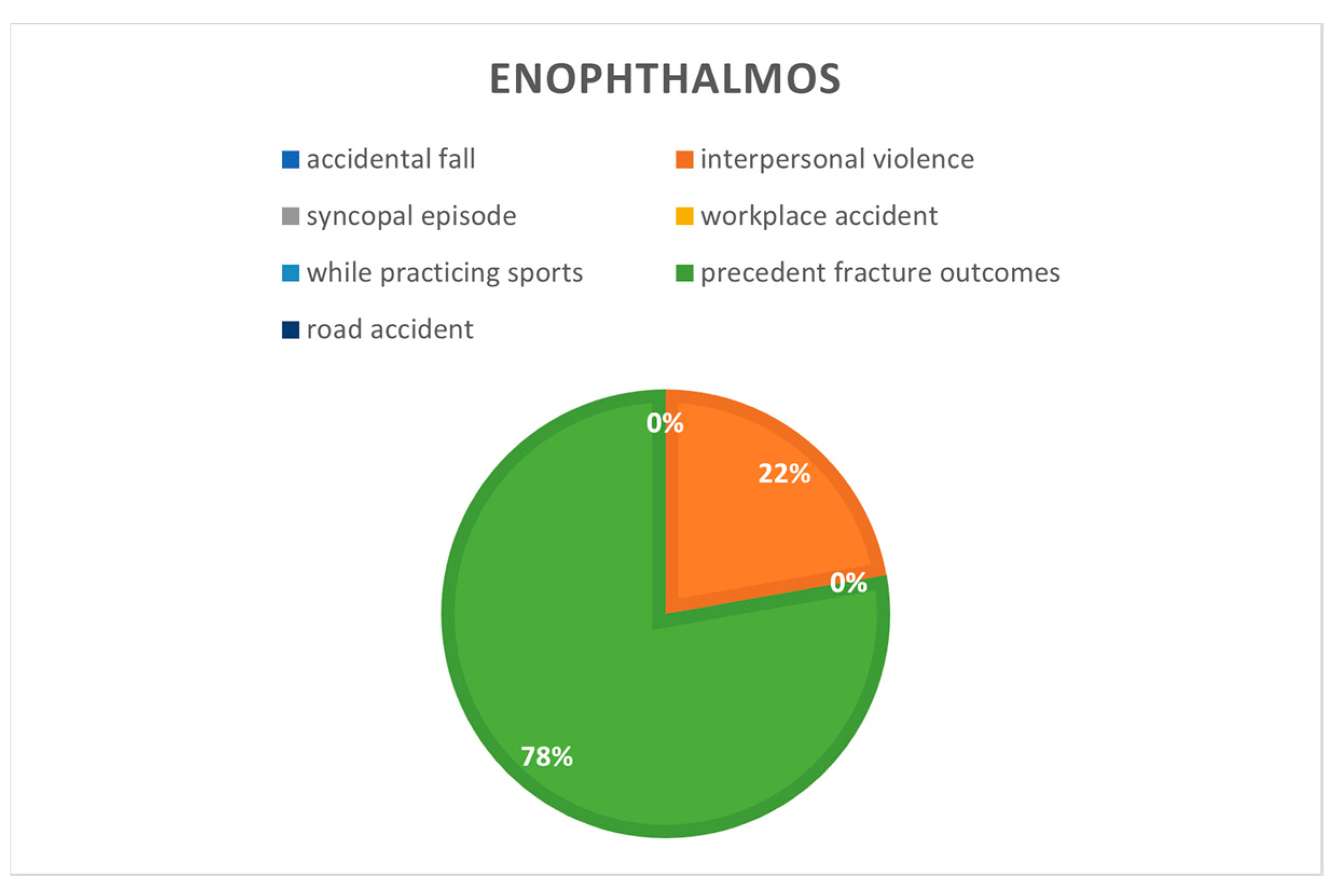
| Type of Fracture | Number of Fractures | Enophtalmos% |
| Orbital floor | 104 | 10% |
| Zygomaticomaxillary complex | 242 | 1% |
| Medial wall | 38 | 11% |
| Lateral walls | 12 | 0% |
| Orbital roof | 6 | 0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Committeri, U.; Arena, A.; Carraturo, E.; Austoni, M.; Germano, C.; Salzano, G.; De Riu, G.; Giovacchini, F.; Maglitto, F.; Abbate, V.; et al. Incidence of Orbital Side Effects in Zygomaticomaxillary Complex and Isolated Orbital Walls Fractures: A Retrospective Study in South Italy and a Brief Review of the Literature. J. Clin. Med. 2023, 12, 845. https://doi.org/10.3390/jcm12030845
Committeri U, Arena A, Carraturo E, Austoni M, Germano C, Salzano G, De Riu G, Giovacchini F, Maglitto F, Abbate V, et al. Incidence of Orbital Side Effects in Zygomaticomaxillary Complex and Isolated Orbital Walls Fractures: A Retrospective Study in South Italy and a Brief Review of the Literature. Journal of Clinical Medicine. 2023; 12(3):845. https://doi.org/10.3390/jcm12030845
Chicago/Turabian StyleCommitteri, Umberto, Antonio Arena, Emanuele Carraturo, Martina Austoni, Cristiana Germano, Giovanni Salzano, Giacomo De Riu, Francesco Giovacchini, Fabio Maglitto, Vincenzo Abbate, and et al. 2023. "Incidence of Orbital Side Effects in Zygomaticomaxillary Complex and Isolated Orbital Walls Fractures: A Retrospective Study in South Italy and a Brief Review of the Literature" Journal of Clinical Medicine 12, no. 3: 845. https://doi.org/10.3390/jcm12030845
APA StyleCommitteri, U., Arena, A., Carraturo, E., Austoni, M., Germano, C., Salzano, G., De Riu, G., Giovacchini, F., Maglitto, F., Abbate, V., Bonavolontà, P., Califano, L., & Piombino, P. (2023). Incidence of Orbital Side Effects in Zygomaticomaxillary Complex and Isolated Orbital Walls Fractures: A Retrospective Study in South Italy and a Brief Review of the Literature. Journal of Clinical Medicine, 12(3), 845. https://doi.org/10.3390/jcm12030845









