The Spread of Exhaled Air and Aerosols during Physical Exercise
Abstract
:1. Introduction
2. Materials and Methods
2.1. Aerosols Measurements
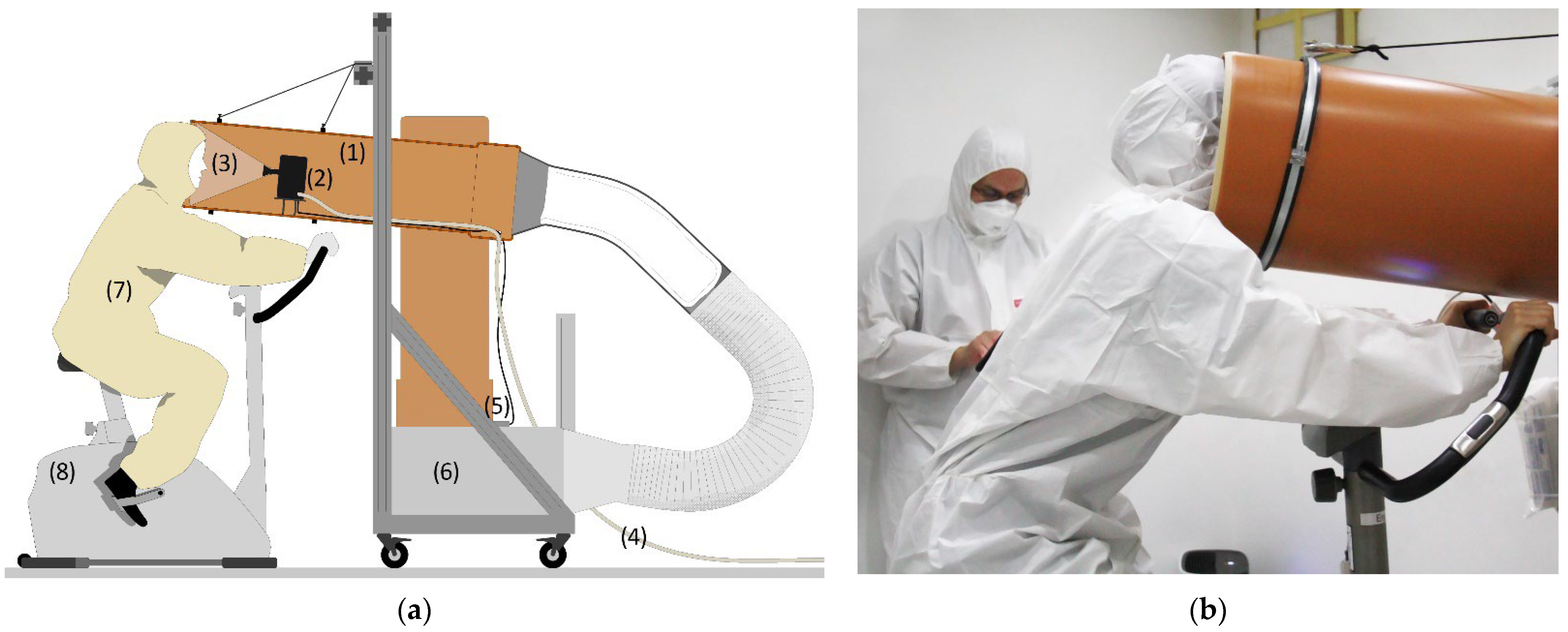
2.2. Airflow Visualization
2.3. User Satisfaction Surveys
- Demographics (gender, age, weight, height, health status, and frequency of training);
- A 32-item Face Mask Perceptions Scale (FMPS) [40] (mean 2.15 ± 0.6, median 1.9, min 1.4, max 3.1);
- The 5-item Environmental Worry Scale according to VDI 3883 Part 1, Appendix A [41] (mean 11.3 ± 2.2, median 11, min 8, max 15).
3. Results
3.1. Aerosols Measurements
3.2. Airflow Visualization
3.3. User Satisfaction Surveys
4. Discussion and Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A


| Female Subjects | Male Subjects | All Subjects | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0.3–0.5 µm | 0.5–1.0 µm | 1.0–5.0 µm | >5.0 µm | Sum | 0.3–0.5 µm | 0.5–1.0 µm | 1.0–5.0 µm | >5.0 µm | Sum | 0.3–0.5 µm | 0.5–1.0 µm | 1.0–5.0 µm | >5.0 µm | Sum | |
| No mask: Measured values [particles/s] | |||||||||||||||
| Min | 21.79 | 0.00 | 0.00 | 0.00 | 32.92 | 67.56 | 1.44 | 1.04 | 0.00 | 141.83 | 21.79 | 0.00 | 0.00 | 0.00 | 32.92 |
| Max | 117.70 | 39.36 | 26.24 | 0.95 | 184.24 | 597.20 | 146.50 | 33.44 | 1.31 | 777.75 | 597.20 | 146.50 | 33.44 | 1.31 | 777.75 |
| Mean | 67.08 | 16.57 | 7.03 | 0.18 | 90.87 | 249.20 | 52.48 | 13.45 | 0.49 | 315.62 | 158.14 | 34.53 | 10.24 | 0.34 | 203.25 |
| Median | 65.75 | 14.31 | 4.12 | 0.00 | 83.93 | 172.72 | 45.19 | 10.14 | 0.38 | 213.87 | 99.17 | 26.09 | 4.98 | 0.06 | 160.72 |
| SD | 29.08 | 12.74 | 8.77 | 0.35 | 48.60 | 181.51 | 45.08 | 11.65 | 0.49 | 218.52 | 158.70 | 37.68 | 10.80 | 0.45 | 194.13 |
| Surgical mask: Measured values [particles/s] | |||||||||||||||
| Min | 0.00 | 0.00 | 2.05 | 0.00 | 2.14 | 0.00 | 0.00 | 0.00 | 0.01 | 0.29 | 0.00 | 0.00 | 0.00 | 0.00 | 0.29 |
| Max | 20.46 | 9.18 | 7.92 | 0.59 | 36.32 | 143.78 | 74.20 | 15.38 | 1.05 | 234.07 | 143.78 | 74.20 | 15.38 | 1.05 | 234.07 |
| Mean | 5.05 | 3.04 | 4.80 | 0.27 | 13.16 | 40.70 | 24.29 | 7.79 | 0.46 | 73.23 | 22.87 | 13.66 | 6.30 | 0.36 | 43.19 |
| Median | 0.00 | 0.89 | 4.91 | 0.27 | 6.30 | 13.16 | 14.95 | 7.21 | 0.34 | 35.65 | 0.00 | 4.48 | 6.25 | 0.34 | 13.46 |
| SD | 7.77 | 3.75 | 2.18 | 0.25 | 13.07 | 53.10 | 26.35 | 5.06 | 0.34 | 83.87 | 41.92 | 21.61 | 4.17 | 0.31 | 67.12 |
| Surgical mask: Emission reduction compared to no mask [%] | |||||||||||||||
| Min | 67.8 | 29.2 | 47.1 | 53.9 | 53.8 | 87.6 | 71.6 | 31.8 | 17.1 | 83.5 | 67.8 | 29.2 | 31.8 | 17.1 | 53.8 |
| Max | 100.0 | 99.6 | 69.8 | 53.9 | 98.0 | 100.0 | 100.0 | 100.0 | 99.2 | 99.9 | 100.0 | 100.0 | 100.0 | 99.2 | 99.9 |
| Mean | 93.2 | 71.2 | 58.4 | 53.9 | 81.7 | 96.9 | 89.5 | 62.7 | 62.0 | 92.5 | 94.7 | 81.4 | 61.5 | 60.0 | 87.1 |
| Median | 100.0 | 78.1 | 58.4 | 53.9 | 86.2 | 100.0 | 100.0 | 62.5 | 69.7 | 95.1 | 100.0 | 81.5 | 62.5 | 61.8 | 90.9 |
| SD | 11.8 | 25.9 | 11.4 | 0.0 | 16.1 | 5.4 | 12.9 | 23.2 | 33.9 | 6.3 | 9.9 | 21.8 | 20.7 | 29.6 | 13.3 |
| FFP2 mask: Measured values [particles/s] | |||||||||||||||
| Min | 0.00 | 0.00 | 1.32 | 0.00 | 1.41 | 0.00 | 0.00 | 0.41 | 0.00 | 0.92 | 0.00 | 0.00 | 0.41 | 0.00 | 0.92 |
| Max | 14.10 | 2.88 | 9.59 | 1.95 | 15.59 | 18.09 | 22.55 | 10.23 | 1.69 | 51.05 | 18.09 | 22.55 | 10.23 | 1.95 | 51.05 |
| Mean | 2.96 | 0.64 | 5.23 | 0.90 | 9.73 | 3.01 | 5.43 | 3.70 | 0.52 | 12.67 | 2.99 | 3.03 | 4.46 | 0.71 | 11.20 |
| Median | 0.00 | 0.00 | 4.89 | 0.77 | 11.14 | 0.00 | 0.63 | 1.78 | 0.37 | 3.40 | 0.00 | 0.11 | 2.73 | 0.37 | 7.09 |
| SD | 5.16 | 1.06 | 3.41 | 0.83 | 5.14 | 6.74 | 8.26 | 3.64 | 0.55 | 17.90 | 6.00 | 6.36 | 3.61 | 0.73 | 13.25 |
| FFP2 mask: Emission reduction compared to no mask [%] | |||||||||||||||
| Min | 77.8 | 92.7 | 38.3 | 29.2 | 71.6 | 97.0 | 84.6 | 69.4 | 59.7 | 93.4 | 77.8 | 84.6 | 38.3 | 29.2 | 71.6 |
| Max | 100.0 | 100.0 | 63.5 | 29.2 | 98.7 | 100.0 | 100.0 | 93.5 | 100.0 | 99.6 | 100.0 | 100.0 | 93.5 | 100.0 | 99.6 |
| Mean | 95.1 | 98.5 | 50.9 | 29.2 | 85.3 | 99.5 | 96.3 | 83.3 | 76.8 | 97.3 | 97.3 | 97.4 | 68.9 | 64.9 | 91.3 |
| Median | 100.0 | 100.0 | 50.9 | 29.2 | 86.2 | 100.0 | 99.2 | 83.3 | 70.8 | 98.0 | 100.0 | 100.0 | 69.4 | 65.2 | 95.1 |
| SD | 8.2 | 2.9 | 12.6 | 0.0 | 10.4 | 1.1 | 5.9 | 8.1 | 17.0 | 2.2 | 6.2 | 4.8 | 19.1 | 25.3 | 9.6 |
References
- Thomas, R.J. Particle Size and Pathogenicity in the Respiratory Tract. Virulence 2013, 4, 847–858. [Google Scholar] [CrossRef] [PubMed]
- Gralton, J.; Tovey, E.; Mclaws, M.-L.; Rawlinson, W.D. The Role of Particle Size in Aerosolised Pathogen Transmission: A Review. J. Infect. 2011, 62, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Li, Y. Airborne Spread of Infectious Agents in the Indoor Environment. Am. J. Infect. Control 2016, 44, S102–S108. [Google Scholar] [CrossRef] [PubMed]
- Wells, W.F. On Air-Borne Infection. Am. J. Epidemiol. 1934, 20, 611–618. [Google Scholar] [CrossRef]
- Brown, J.H.; Cook, K.M.; Ney, F.G.; Hatch, T. Influence of Particle Size upon the Retention of Particulate Matter in the Human Lung. Am. J. Public Health Nations Health 1950, 40, 450–480. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, A.; Krishan, J.; Bathula, S.; Mayya, Y.S. Modeling the Viral Load Dependence of Residence Times of Virus-Laden Droplets from COVID-19-Infected Subjects in Indoor Environments. Indoor Air 2021, 31, 1786–1797. [Google Scholar] [CrossRef] [PubMed]
- Morawska, L.; Johnson, G.R.; Ristovski, Z.D.; Hargreaves, M.H.; Mengersen, K.L.; Chao, C.Y.H.; Wan, M.P.; Li, Y.; Xie, X.; Katoshevski, D. Droplets Expelled during Human Expiratory Activities and Their Origin. In Proceedings of the 11th International Conference on Indoor Air Quality and Climate, Copenhagen, Denmark, 17 August 2008. [Google Scholar]
- Hartmann, A.; Lange, J.; Rotheudt, H.; Kriegel, M. Emissionsrate und Partikelgröße von Bioaerosolen Beim Atmen, Sprechen und Husten; Technische Universität Berlin: Berlin, Germany, 2020. [Google Scholar]
- Milton, D.K.; Fabian, M.P.; Cowling, B.J.; Grantham, M.L.; Mcdevitt, J.J. Influenza Virus Aerosols in Human Exhaled Breath: Particle Size, Culturability, and Effect of Surgical Masks. PLoS Pathog. 2013, 9, E1003205. [Google Scholar] [CrossRef] [PubMed]
- Lindsley, W.; Blachere, F.; Thewlis, R.; Vishnu, A.; Davis, K.; Cao, G.; Palmer, J.; Clark, K.; Fisher, M.; Khakoo, R.; et al. Measurements of Airborne Influenza Virus in Aerosol Particles from Human Coughs. PLoS ONE 2010, 5, E15100. [Google Scholar] [CrossRef]
- Tang, J.W. The Effect of Environmental Parameters on the Survival of Airborne Infectious Agents. J. R. Soc. Interface 2009, 6 (Suppl. S6), S737–S746. [Google Scholar] [CrossRef]
- Scharfman, B.E.; Techet, A.H.; Bush, J.W.M.; Bourouiba, L. Visualization of Sneeze Ejecta: Steps of Fluid Fragmentation Leading to Respiratory Droplets. Exp. Fluids 2016, 57, 24. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.W.; Liebner, T.J.; Craven, B.A.; Settles, G.S. A Schlieren Optical Study of the Human Cough with and without Wearing Masks for Aerosol Infection Control. J. R. Soc. Interface 2009, 6 (Suppl. S6), S727–S736. [Google Scholar] [CrossRef] [PubMed]
- Darby, S.; Chulliyallipalil, K.; Przyjalgowski, M.; Mcgowan, P.; Jeffers, S.; Giltinan, A.; Lewis, L.; Smith, N.; Sleator, R.D. COVID-19: Mask Efficacy Is Dependent on Both Fabric and Fit. Future Microbiol. 2021, 16, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Alhazzani, W.; Møller, M.H.; Arabi, Y.M.; Loeb, M.; Gong, M.N.; Fan, E.; Oczkowski, S.; Levy, M.M.; Derde, L.; Dzierba, A.; et al. Surviving Sepsis Campaign: Guidelines on the Management of Critically ill Adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020, 46, 854–887. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions. Available online: Https://Www.Who.Int/News-Room/Commentaries/Detail/Transmission-Of-Sars-CoV-2-Implications-For-Infection-Prevention-Precautions (accessed on 6 June 2022).
- Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Healthcare Personnel during the Coronavirus Disease 2019 (COVID-19) Pandemic. Available online: Https://Www.Cdc.Gov/Coronavirus/2019-Ncov/Hcp/Infection-Control-Recommendations.Html (accessed on 6 June 2022).
- Marshall, H.D.; Iacoviello, V. How SARS-CoV-2 Evolution Shapes Public Health: Five Key Turning Points in Mask Recommendations during the COVID-19 Pandemic. Available online: Https://Www.Ebsco.Com/Blogs/Health-Notes/How-Sars-CoV-2-Evolution-Shapes-Public-Health-Five-Key-Turning-Points-Mask (accessed on 6 June 2022).
- Blocken, B.; Van Druenen, T.; Ricci, A.; Kang, L.; Van Hooff, T.; Qin, P.; Xia, L.; Ruiz, C.A.; Arts, J.H.; Diepens, J.F.L.; et al. Ventilation and Air Cleaning to Limit Aerosol Particle Concentrations in a Gym during the COVID-19 Pandemic. Build. Environ. 2021, 193, 107659. [Google Scholar] [CrossRef]
- Klompas, M.; Rhee, C. Aerosol Generation during Exercise: Implications for Preventing Viral Transmission in and out of the Exercise Laboratory. Chest 2021, 160, 1174–1176. [Google Scholar] [CrossRef]
- Mutsch, B.; Heiber, M.; Grätz, F.; Hain, R.; Schönfelder, M.; Kaps, S.; Schranner, D.; Kähler, C.J.; Wackerhage, H. Aerosol Particle Emission Increases Exponentially above Moderate Exercise Intensity Resulting in Superemission during Maximal Exercise. Proc. Natl. Acad. Sci. USA 2022, 119, E2202521119. [Google Scholar] [CrossRef]
- Sajgalik, P.; Garzona-Navas, A.; Csécs, I.; Askew, J.W.; Lopez-Jimenez, F.; Niven, A.S.; Johnson, B.D.; Allison, T.G. Characterization of Aerosol Generation during Various Intensities of Exercise. Chest 2021, 160, 1377–1387. [Google Scholar] [CrossRef]
- Zheng, C.; Poon, E.T.-C.; Wan, K.; Dai, Z.; Wong, S.H.-S. Effects of Wearing A Mask during Exercise on Physiological and Psychological Outcomes in Healthy Individuals: A Systematic Review and Meta-Analysis. Sports Med. 2022, 53, 125–150. [Google Scholar] [CrossRef]
- Ipek, S.; Yurttutan, S.; Güllü, U.U.; Dalkıran, T.; Acıpayam, C.; Doğaner, A. Is N95 Face Mask Linked to Dizziness and Headache? Int. Arch. Occup. Environ. Health 2021, 94, 1627–1636. [Google Scholar] [CrossRef]
- Yoshihara, A.; Dierickx, E.E.; Brewer, G.J.; Sekiguchi, Y.; Stearns, R.L.; Casa, D.J. Effects of Face Mask Use on Objective and Subjective Measures of Thermoregulation during Exercise in the Heat. Sports Health 2021, 13, 463–470. [Google Scholar] [CrossRef]
- Mahjoub Mohammed Merghani, K.; Sagot, B.; Gehin, E.; Da, G.; Motzkus, C. A Review on the Applied Techniques of Exhaled Airflow and Droplets Characterization. Indoor Air 2021, 31, 7–25. [Google Scholar] [CrossRef]
- Melling, A. Tracer Particles and Seeding for Particle Image Velocimetry. Meas. Sci. Technol. 1997, 8, 1406–1416. [Google Scholar] [CrossRef]
- Mueller, D.; Renz, U. Particle Streak Tracking System (Pst) to Measure Flow Fields in Ventilated Rooms. In Proceedings of the Roomvent 2000, the 7th International Conference on Air Distribution in Rooms, Reading, UK, 9–12 July 2000; Volume 1, pp. 325–331. [Google Scholar]
- Tao, Y.; Inthavong, K.; Petersen, P.; Mohanarangam, K.; Yang, W.; Tu, J. Experimental Visualisation of Wake Flows Induced by Different Shaped Moving Manikins. Build. Environ. 2018, 142, 361–370. [Google Scholar] [CrossRef]
- Settles, G.S. Schlieren and Shadowgraph Techniques; Springer: Berlin/Heidelberg, Germany, 2001; ISBN 978-3-642-63034-7. [Google Scholar]
- Kerl, J.; Gena, A.W.; Alsaad, H.; Voelker, C.; Dellweg, D. Influence of Wearing Masks on Exhaled Air Aerodynamics. J. Med. Eng. Technol. 2022, 46, 231–242. [Google Scholar] [CrossRef] [PubMed]
- Dellweg, D.; Kerl, J.; Gena, A.W.; Alsaad, H.; Voelker, C. Exhalation Spreading during Nasal High-Flow Therapy at Different Flow Rates. Crit. Care Med. 2021, 49, E693–E700. [Google Scholar] [CrossRef]
- Becher, L.; Gena, A.W.; Alsaad, H.; Richter, B.; Spahn, C.; Voelker, C. The Spread of Breathing Air From Wind Instruments and Singers Using Schlieren Techniques. Indoor Air 2021, 31, 1798–1814. [Google Scholar] [CrossRef]
- Alsaad, H.; Voelker, C. Qualitative Evaluation of the Flow Supplied by Personalized Ventilation Using Schlieren Imaging and Thermography. Build. Environ. 2020, 167, 106450. [Google Scholar] [CrossRef]
- ISO 21501-4; Determination of Particle Size Distribution—Single Particle Light Interaction Methods—Part 4: Light Scattering Airborne Particle Counter For Clean Spaces. International Organization For Standardization: Geneva, Switzerland, 2018.
- Umweltbundesamt. Gesundheitliche Bewertung von Kohlendioxid in der Innenraumluft. Mitteilungen der Ad-Hoc-Arbeitsgruppe Innenraumrichtwerte der Innenraumlufthygiene-Kommission des Umweltbundesamtes und der Obersten Landesgesundheitsbehörden. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 2008, 51, 1358–1369. [Google Scholar] [CrossRef]
- Gena, A.W.; Voelker, C.; Settles, G.S. Qualitative and Quantitative Schlieren Optical Measurement of the Human Thermal Plume. Indoor Air 2020, 30, 757–766. [Google Scholar] [CrossRef]
- Borg, G. Borg’s Perceived Exertion and Pain Scales; Human Kinetics: Champaign, IL, USA, 1998; ISBN 0-88011-623-4. [Google Scholar]
- Löllgen, H. Borg-Skala Standards der Sportmedizin. Dtsch. Z. Sportmed. 2004, 55, 299–300. [Google Scholar]
- Howard, M.C. Understanding Face Mask Use to Prevent Coronavirus and Other Illnesses: Development of a Multidimensional Face Mask Perceptions Scale. Br. J. Health Psychol. 2020, 25, 912–924. [Google Scholar] [CrossRef] [PubMed]
- VDI. Effects and Assessment Of Odours: Assessment Of Odour Annoyance-Questionnaires; Verein Deutscher Ingenieure: Düsseldorf, Germany, 2015; VDI 3883; Pt 1. [Google Scholar]
- Jones, R.M.; Brosseau, L.M. Aerosol Transmission of Infectious Disease. J. Occup. Environ. Med. 2015, 57, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Wilson, N.M.; Marks, G.B.; Eckhardt, A.; Clarke, A.; Young, F.; Garden, F.L.; Stewart, W.; Cook, T.M.; Tovey, E.R. The Effect of Respiratory Activity, Non-Invasive Respiratory Support and Facemasks on Aerosol Generation and Its Relevance to COVID-19. Anaesthesia 2021, 76, 1465–1474. [Google Scholar] [CrossRef]
- Farghadan, A.; Poorbahrami, K.; Jalal, S.; Oakes, J.M.; Coletti, F.; Arzani, A. Particle Transport and Deposition Correlation with Near-Wall Flow Characteristic under Inspiratory Airflow in Lung Airways. Comput. Biol. Med. 2020, 120, 103703. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.-K.; Solano, T.; Shoele, K. Bridge The Gap: Correlate Face Mask Leakage and Facial Features with 3d Morphable Face Models. J. Expo. Sci. Environ. Epidemiol. 2022, 32, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Oestenstad, R.K.; Bartolucci, A.A. Factors Affecting the Location and Shape of Face Seal Leak Sites on Half-Mask Respirators. J. Occup. Environ. Hyg. 2010, 7, 332–341. [Google Scholar] [CrossRef] [PubMed]
- Oestenstad, R.K.; Perkins, L.L. An Assessment of Critical Anthropometric Dimensions for Predicting the Fit of A Half-Mask Respirator. Am. Ind. Hyg. Assoc. J. 1992, 53, 639–644. [Google Scholar] [CrossRef]
- Oestenstad, R.K.; Dillion, H.K.; Perkins, L.L. Distribution of Faceseal Leak Sites on A Half-Mask Respirator and Their Association with Facial Dimensions. Am. Ind. Hyg. Assoc. J. 1990, 51, 285–290. [Google Scholar] [CrossRef]
- Asadi, S.; Cappa, C.D.; Barreda, S.; Wexler, A.S.; Bouvier, N.M.; Ristenpart, W.D. Efficacy of Masks and Face Coverings in Controlling outward Aerosol Particle Emission from Expiratory Activities. Sci. Rep. 2020, 10, 15665. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Omidvarborna, H.; Kumar, P. Efficacy of Facemasks in Mitigating Respiratory Exposure to Submicron Aerosols. J. Hazard. Mater. 2022, 422, 126783. [Google Scholar] [CrossRef] [PubMed]
- Dbouk, T.; Drikakis, D. On Respiratory Droplets and Face Masks. Phys. Fluids 2020, 32, 63303. [Google Scholar] [CrossRef] [PubMed]
- Macintyre, C.R.; Cauchemez, S.; Dwyer, D.E.; Seale, H.; Cheung, P.; Browne, G.; Fasher, M.; Wood, J.; Gao, Z.; Booy, R.; et al. Face Mask Use and Control of Respiratory Virus Transmission in Households. Emerg. Infect. Dis. 2009, 15, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Diaz, K.T.; Smaldone, G.C. Quantifying Exposure Risk: Surgical Masks and Respirators. Am. J. Infect. Control 2010, 38, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Dhanak, M.; Frankenfield, J. Visualizing The Effectiveness of Face Masks in Obstructing Respiratory Jets. Phys. Fluids 2020, 32, 61708. [Google Scholar] [CrossRef]
- Khosronejad, A.; Kang, S.; Wermelinger, F.; Koumoutsakos, P.; Sotiropoulos, F. A Computational Study of Expiratory Particle Transport and Vortex Dynamics During Breathing with and Without Face Masks. Phys. Fluids 2021, 33, 66605. [Google Scholar] [CrossRef]
- Jang, S.; Han, S.H.; Rhee, J.-Y. Cluster of Coronavirus Disease Associated with Fitness Dance Classes, South Korea. Emerg. Infect. Dis. 2020, 26, 1917–1920. [Google Scholar] [CrossRef] [PubMed]
- Haller, S.; Güsewell, S.; Egger, T.; Scanferla, G.; Thoma, R.; Leal-Neto, O.B.; Flury, D.; Brucher, A.; Lemmenmeier, E.; Möller, J.C.; et al. Impact of Respirator Versus Surgical Masks on SARS-CoV-2 Acquisition in Healthcare Workers: A Prospective Multicentre Cohort. Antimicrob. Resist. Infect. Control 2022, 11, 27. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, G.; Thiede, B.; Hejazi, B.; Schlenczek, O.; Bodenschatz, E. An Upper Bound on One-to-One Exposure to Infectious Human Respiratory Particles. Proc. Natl. Acad. Sci. USA 2021, 118, e2110117118. [Google Scholar] [CrossRef]
- Cabanillas-Barea, S.; Rodríguez-Sanz, J.; Carrasco-Uribarren, A.; López-De-Celis, C.; González-Rueda, V.; Zegarra-Chávez, D.; Cedeño-Bermúdez, S.; Pérez-Bellmunt, A. Effects of Using the Surgical Mask and FFP2 during the 6-min Walking Test. A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 12420. [Google Scholar] [CrossRef]
- Fikenzer, S.; Uhe, T.; Lavall, D.; Rudolph, U.; Falz, R.; Busse, M.; Hepp, P.; Laufs, U. Effects of Surgical and FFP2/N95 Face Masks on Cardiopulmonary Exercise Capacity. Clin. Res. Cardiol. 2020, 109, 1522–1530. [Google Scholar] [CrossRef]







| Mean and Standard Deviation | ANOVA Test Statistics | |||||
|---|---|---|---|---|---|---|
| No Mask | Surgical Mask | FFP2 Mask | F(dfn/dfd) | p | Eta2tot | |
| Perceived exertion (RPE) | 12.2 ± 1.96 | 12.9 ± 2.11 | 13.2 ± 2.22 | 2.8(2/22) | 0.08 | 0.041 |
| Perceived dyspnea (RPD) | 10.8 ± 1.27 | 11.6 ± 1.9 | 13.1 ± 2.8 | 6.1(2/22) | 0.008 | 0.18 |
| Thirst sensation | 1.42 ± 0.5 | 1.67 ± 0.9 | 1.33 ± 0.9 | 1.3(2/22) | 0.28 | 0.03 |
| Thermal sensation | 6 ± 1 | 6.3 ± 1.3 | 6.4 ± 1.1 | 1.4(2/22) | 0.27 | 0.02 |
| Fatigue level | 3.4 ± 1.3 | 3.8 ± 1.2 | 3.8 ± 1.8 | 0.6(1.2/13.2) | 0.49 | 0.02 |
| Physical and Psychological Symptoms | No | 1 min | 2 min | 5 min | >5 min | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | |
| Headache | |||||||||
| No mask | 12 | 100 | - | - | - | - | |||
| Surgical mask | 12 | 100 | - | - | - | - | |||
| FFP2 mask | 12 | 100 | - | - | - | - | |||
| Dizziness | |||||||||
| No mask | 12 | 100 | - | - | - | - | |||
| Surgical mask | 11 | 91.7 | 1 | 8.3 | - | - | - | ||
| FFP2 mask | 11 | 91.7 | 1 | 8.3 | - | - | - | ||
| Facial sweating | |||||||||
| No mask | 9 | 75 | 3 | 25 | - | - | - | ||
| Surgical mask | 8 | 66.7 | 2 | 16.7 | 2 | 16.7 | - | - | |
| FFP2 mask | 10 | 83.3 | 2 | 16.7 | - | - | - | ||
| Coughing | |||||||||
| No mask | 12 | 100 | - | - | - | - | |||
| Surgical mask | 12 | 100 | - | - | - | - | |||
| FFP2 mask | 12 | 100 | - | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsaad, H.; Schälte, G.; Schneeweiß, M.; Becher, L.; Pollack, M.; Gena, A.W.; Schweiker, M.; Hartmann, M.; Voelker, C.; Rossaint, R.; et al. The Spread of Exhaled Air and Aerosols during Physical Exercise. J. Clin. Med. 2023, 12, 1300. https://doi.org/10.3390/jcm12041300
Alsaad H, Schälte G, Schneeweiß M, Becher L, Pollack M, Gena AW, Schweiker M, Hartmann M, Voelker C, Rossaint R, et al. The Spread of Exhaled Air and Aerosols during Physical Exercise. Journal of Clinical Medicine. 2023; 12(4):1300. https://doi.org/10.3390/jcm12041300
Chicago/Turabian StyleAlsaad, Hayder, Gereon Schälte, Mario Schneeweiß, Lia Becher, Moritz Pollack, Amayu Wakoya Gena, Marcel Schweiker, Maria Hartmann, Conrad Voelker, Rolf Rossaint, and et al. 2023. "The Spread of Exhaled Air and Aerosols during Physical Exercise" Journal of Clinical Medicine 12, no. 4: 1300. https://doi.org/10.3390/jcm12041300
APA StyleAlsaad, H., Schälte, G., Schneeweiß, M., Becher, L., Pollack, M., Gena, A. W., Schweiker, M., Hartmann, M., Voelker, C., Rossaint, R., & Irrgang, M. (2023). The Spread of Exhaled Air and Aerosols during Physical Exercise. Journal of Clinical Medicine, 12(4), 1300. https://doi.org/10.3390/jcm12041300








