Giant Juvenile Fibroadenoma: Case Report and Review of the Literature
Abstract
1. Introduction
2. Materials and Methods
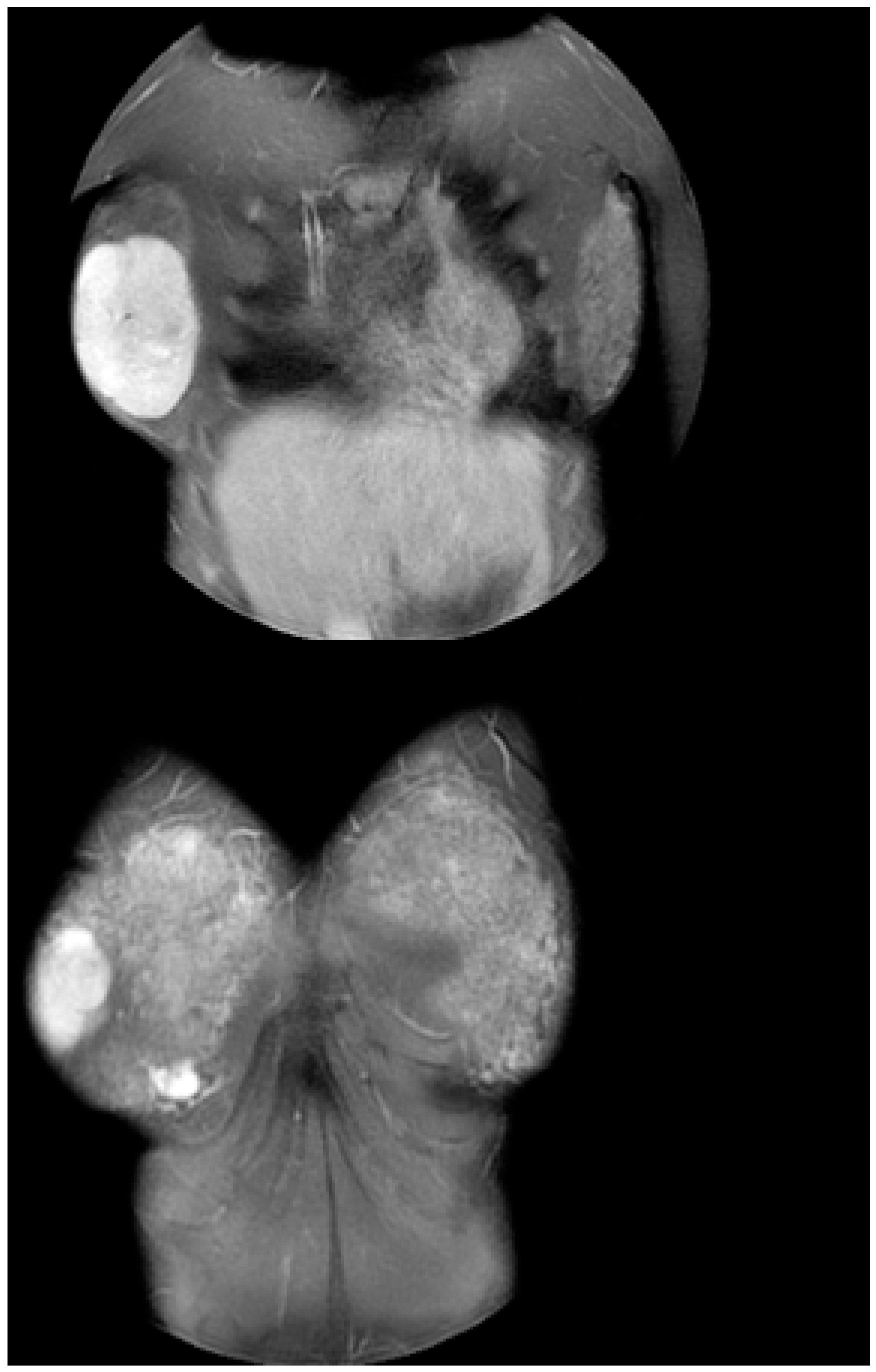
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, E.J.; Chang, Y.-W.; Oh, J.H.; Hwang, J.; Hong, S.S.; Kim, H.-J. Breast Lesions in Children and Adolescents: Diagnosis and Management. Korean J. Radiol. 2018, 19, 978–991. [Google Scholar] [CrossRef] [PubMed]
- Jayasinghe, Y.; Simmons, P.S. Fibroadenomas in adolescence. Curr. Opin. Obstet. Gynecol. 2009, 21, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Schnitt, S.J.; Collins, L.C. Pathology of benign breast disorders. In Diseases of the Breast, 4th ed.; Harris, J.R., Lippman, M.E., Morrow, M., Osborne, C.K., Eds.; Wolters Kluwer-Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2010; p. 69. [Google Scholar]
- Adolescent Health. Available online: https://www.who.int/health-topics/adolescent-health#tab=tab_1 (accessed on 26 December 2021).
- Tea, M.-K.M.; Asseryanis, E.; Kroiss, R.; Kubista, E.; Wagner, T. Surgical breast lesions in adolescent females. Pediatr. Surg. Int. 2008, 25, 73–75. [Google Scholar] [CrossRef] [PubMed]
- Dupont, W.D.; Page, D.L.; Parl, F.F.; Vnencak-Jones, C.L.; Plummer, W.D.; Rados, M.S.; Schuyler, P.A. Long-Term Risk of Breast Cancer in Women with Fibroadenoma. N. Engl. J. Med. 1994, 331, 10–15. [Google Scholar] [CrossRef]
- Sosin, M.; Pulcrano, M.; Feldman, E.D.; Patel, K.M.; Nahabedian, M.Y.; Weissler, J.M.; Rodriguez, E.D. Giant juvenile fibroadenoma: A systematic review with diagnostic and treatment recommendations. Gland. Surg. 2015, 4, 312–321. [Google Scholar] [CrossRef]
- Song, B.S.; Kim, E.-K.; Seol, H.; Seo, J.-H.; Lee, J.A.; Kim, D.H.; Lim, J.S. Giant juvenile fibroadenoma of the breast: A case report and brief literature review. Ann. Pediatr. Endocrinol. Metab. 2014, 19, 45–48. [Google Scholar] [CrossRef]
- Makkar, N. Bilateral Giant Juvenile Fibroadenoma of Breast. J. Clin. Diagn. Res. 2017, 11, ED10–ED12. [Google Scholar] [CrossRef]
- Celik, S.U.; Celik, D.B.; Yetiskin, E.; Ergun, E.; Percinel, S.; Demirer, S. Giant juvenile fibroadenoma of the breast: A clinical case. Arch. Argent. de Pediatr. 2017, 115, e428–e431. [Google Scholar] [CrossRef]
- Jategaonkar, P.A. Super-giant Juvenile Breast Fibroadenoma: World’s First Case. J. Coll. Physicians Surg. Pak. 2018, 28, 257–258. [Google Scholar] [CrossRef]
- Juarez, A.M.; Juarez, C.A.S.; Martinez, I.M.A.; Mondragon, E.R. Breast-conserving surgery in giant juvenile fibroadenoma: A case report. AME Surg. J. 2021, 1, 18. [Google Scholar] [CrossRef]
- Kupsik, M.; Yep, B.; Sulo, S.; Memmel, H. Giant juvenile fibroadenoma in a 9-year-old: A case presentation and review of the current literature. Breast Dis. 2017, 37, 95–98. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Khan, M.; Rafique, S. Giant Bilateral Juvenile Fibroadenoma of the Breast in Prepubescent Girl. J. Coll. Physicians Surg. Pak. 2015, 25, S95–S96. [Google Scholar] [CrossRef]
- Gaurav, K.; Chandra, G.; Neelam, K.; Kumar, S.; Singla, H.; Yadav, S.K. A pre-pubertal girl with giant juvenile fibroadenoma: A rare case report. Int. J. Surg. Case Rep. 2015, 16, 87–89. [Google Scholar] [CrossRef] [PubMed]
- Rashid, N.F.A.; Firdaus, C.A.M.; Norjazliney, A.J. A case report of juvenile giant fibroadenoma of the breast: How common? Tzu Chi Med J. 2017, 29, 177–179. [Google Scholar] [CrossRef] [PubMed]
- Gkali, C.; Giannos, A.; Primetis, E.; Chalazonitis, A.; Anastasiadi, T.; Feida, E.; Sotiropoulou, M.; Dimitrakakis, C.; Antoniou, A. Giant Juvenile Fibroadenoma in a 12-Year-Old Girl. Ultrasound Q. 2017, 33, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Nishtha; Kaur, N.; Tanveer, N.; Naskar, S. A Diagnostic Enigma—a Rare Presentation of Juvenile Fibroadenoma in a Premenarchal Girl. J. Pediatr. Adolesc. Gynecol. 2021, 34, 558–560. [Google Scholar] [CrossRef] [PubMed]
- Giannos, A.; Stavrou, S.; Gkali, C.; Chra, E.; Marinopoulos, S.; Chalazonitis, A.; Dimitrakakis, C.; Drakakis, P. A prepubertal giant juvenile fibroadenoma in a 12-year-old girl: Case report and brief literature review. Int. J. Surg. Case Rep. 2017, 41, 427–430. [Google Scholar] [CrossRef]
- Bayramoglu, Z.; Yılmaz, R.; Caliskan, E.; Onder, S.; Akkavak, G.; Adaletli, I. Unilateral rapid enlargement of an adolescent breast: Pseudoangiomatous stromal hyperplasia in a giant juvenile fibroadenoma. Breast J. 2018, 24, 648–649. [Google Scholar] [CrossRef]
- Rafeek, N.; Rangasami, R.; Dhanraj, K.; Joseph, S. Multimodality approach in the diagnosis and management of bilateral giant juvenile breast fibroadenoma. BMJ Case Rep. 2016, 2016, bcr2016217588. [Google Scholar] [CrossRef]
- Kitazawa, M.; Futamura, M.; Tokumaru, Y.; Kohyama, K.; Nakakami, A.; Yoshida, K. Breast reconstruction using a tissue expander after enucleation of a giant fibroadenoma: A case report. Int. J. Surg. Case Rep. 2021, 90, 106723. [Google Scholar] [CrossRef]
- Wang, T.; Zhu, L. Mammotome-assisted removal with minimal incision of large juvenile fibroadenoma of breast. Medicine 2020, 99, e19442. [Google Scholar] [CrossRef] [PubMed]
- Heng, S.S.L.; Yahya, M.M.; Sulaiman, W.A.W.; Saad, A.Z.M. A harmless evil: Giant fungating benign breast mass in an adolescent mimicking malignancy - Case report. Int. J. Surg. Case Rep. 2020, 80, 105202. [Google Scholar] [CrossRef] [PubMed]
- Ezer, S.S.; Oguzkurt, P.; Ince, E.; Temiz, A.; Bolat, F.A.; Hicsonmez, A. Surgical Treatment of the Solid Breast Masses in Female Adolescents. J. Pediatr. Adolesc. Gynecol. 2013, 26, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Matz, D.; Kerivan, L.; Reintgen, M.; Akman, K.; Lozicki, A.; Causey, T.; Clynes, C.; Giuliano, R.; Acs, G.; Cox, J.; et al. Breast Preservation in Women With Giant Juvenile Fibroadenoma. Clin. Breast Cancer 2013, 13, 219–222. [Google Scholar] [CrossRef]
- Arowolo, O.; Akinkuolie, A.; Adisa, A.; Obonna, G.; Olasode, B.J. Giant fibroadenoma presenting like fungating breast cancer in a Nigerian teenager. Afr. Heal. Sci. 2013, 13, 162–165. [Google Scholar] [CrossRef]
- Biswas, S.K.; Rahman, A.T.; Paul, A.C.; Mollah, M.; Chowdhury, V. Giant Juvenile Fibroadenoma of the Breast: Report of 2 Cases. Faridpur Med. Coll. J. 2012, 7, 42–45. [Google Scholar] [CrossRef]
- Cheng, P.J.; Vu, L.T.; Cass, D.; Hicks, M.J.; Brandt, M.L.; Kim, E. Endoscopic specimen pouch technique for removal of giant fibroadenomas of the breast. J. Pediatr. Surg. 2012, 47, 803–807. [Google Scholar] [CrossRef]
- Kaur, N.; Saini, S.; Somasekhar, S.; Gupta, A. Bilateral Florid Juvenile Fibroadenomas of the Breast in an Adolescent: A Rare Indication for Subcutaneous Mastectomy. J. Pediatr. Adolesc. Gynecol. 2015, 28, e135–e137. [Google Scholar] [CrossRef]
- Heilmann, T.; Leuschner, I.; Hilpert, F.; Kümper, C.; Strauss, A.; Mundhenke, C.; Jonat, W.; Bauer, M. Diagnosis and management of an unilateral giant fibroadenoma of the breast in pregnancy. Arch. Gynecol. Obstet. 2011, 285, 235–237. [Google Scholar] [CrossRef]
- Izadpanah, A.; Karunanayake, M.; Izadpanah, A.; Sinno, H.; Gilardino, M. An Atypical Growth of a Giant Fibroadenoma after Trauma. J. Pediatr. Adolesc. Gynecol. 2012, 25, e115–e117. [Google Scholar] [CrossRef]
- Marshall, A.P.; Spottswood, S.E.; Grau, A.M.; Jackson, G.P. Juvenile fibroadenoma and granular cell tumor of the breast in an adolescent. J. Pediatr. Surg. 2012, 47, 1930–1933. [Google Scholar] [CrossRef]
- Chepla, K.; Armijo, B.; Ponsky, T.; Soltanian, H. Benefits of immediate dermoglandular preserving reconstruction following giant fibroadenoma excision in two patients. J. Plast. Reconstr. Aesthetic Surg. 2011, 64, e244–e247. [Google Scholar] [CrossRef] [PubMed]
- Ng, W.K.; Mrad, M.A.; Brown, M.H. Juvenile Fibroadenoma of the Breast: Treatment and Literature Review. Can. J. Plast. Surg. 2011, 19, 105–107. [Google Scholar] [CrossRef] [PubMed]
- Nikumbh, D.B.; Desai, S.R.; Madan, P.S.; Patil, N.J.; Wader, J.V. Bilateral Giant Juvenile Fibroadenomas of Breasts:A Case Report. Pathol. Res. Int. 2011, 2011, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Yagnik, V. Juvenile Giant Fibroadenoma. Clin. Pract. 2011, 1, e49. [Google Scholar] [CrossRef] [PubMed]
- Poh, M.M.; Ballard, T.N.; Wendel, J.J. Beckwith-Wiedemann Syndrome and Juvenile Fibroadenoma. Ann. Plast. Surg. 2010, 64, 803–806. [Google Scholar] [CrossRef] [PubMed]
- Biggers, B.D.; Lamont, J.P.; Etufugh, C.N.; Knox, S.K. Inframammary Approach for Removal of Giant Juvenile Fibroadenomas. J. Am. Coll. Surg. 2009, 208, e1–e4. [Google Scholar] [CrossRef]
- Calcaterra, V.; Coscia, D.R.; Sgarella, A.; Burroni, B.; Podetta, M.; Andorno, A.; Ferrari, A.; Larizza, D. Recurrence of giant juvenile breast fibroadenoma in a girl with Turner’s syndrome. J. Pediatr. Endocrinol. Metab. 2009, 22, 281–284. [Google Scholar] [CrossRef]
- Kozomara, D.; Šutalo, N.; Galić, G.; Jurišić, S.; Trninć, Z. Giant unilateral breast juvenile fibroadenoma-the aesthetic outcome of surgical treatment should be considered. Med. Acad. Most. 2016, 28, 72–75. [Google Scholar]
- Gobbi, D.; Dall’Igna, P.; Alaggio, R.; Nitti, D.; Cecchetto, G. Giant fibroadenoma of the breast in adolescents: Report of 2 cases. J. Pediatr. Surg. 2009, 44, e39–e41. [Google Scholar] [CrossRef]
- Mukhopadhyay, M.; Patra, R.; Mondal, S.; Ghosh, A.; Ray, A.K. Bilateral giant juvenile fibroadenoma of breasts. J. Indian Assoc. Pediatr. Surg. 2009, 14, 68–69. [Google Scholar] [CrossRef]
- Wolfram, D.; Behensky, H.; Piza-Katzer, H. Unilateral Gigantomastia Related to Juvenile Fibroadenoma with Idiopathic Thoracic Scoliosis. J. Pediatr. Adolesc. Gynecol. 2009, 22, e25–e27. [Google Scholar] [CrossRef]
- Dolmans, G.H.; Hoogbergen, M.M.; van Rappard, J.H. Giant fibroadenoma of one breast: Immediate bilateral reconstruction. J. Plast. Reconstr. Aesthetic Surg. 2007, 60, 1156–1157. [Google Scholar] [CrossRef] [PubMed]
- Moore, R.L.; Mungara, A.; Shayan, K.; Wallace, A.M. Bilaterally symmetric juvenile fibroadenomas and tubular breast deformity in a prepubescent girl. J. Pediatr. Surg. 2007, 42, 1133–1136. [Google Scholar] [CrossRef] [PubMed]
- Ahuja, A.; Seth, A. Juvenile fibroadenoma of breast. Indian Pediatr. 2005, 42, 72. [Google Scholar] [PubMed]
- Lee, C.; Kim, Y.; Seo, Y.; Pak, S.; Lee, S. Treatment of Multiple Bilateral Juvenile Fibroadenomas in a Teenage Breast by Central Pedicle Breast Reduction, with Vertical and Short Horizontal Scar: Case Report. Aesthetic Plast. Surg. 2004, 28, 228–230. [Google Scholar] [CrossRef]
- Zacharia, T.T.; Lakhar, B.; Ittoop, A.; Menachery, J. Giant Fibroadenoma. Breast J. 2003, 9, 53. [Google Scholar] [CrossRef]
- Hanna, R.M.; Ashebu, S.D. Giant fibroadenoma of the breast in an Arab population. Australas. Radiol. 2002, 46, 252–256. [Google Scholar] [CrossRef]
- Wechselberger, G.; Schoeller, T.; Piza-Katzer, H. Juvenile fibroadenoma of the breast. Surgery 2002, 132, 106–107. [Google Scholar] [CrossRef]
- Celik, M.F.; Dural, A.C.; Unsal, M.G.; Akarsu, C.; Alim, E.R.; Kapan, S.; Kalayci, M.U.; Alis, H. Giant juvenile fibroadenoma. Turk. J. Surg. 2015, 31, 96–98. [Google Scholar] [CrossRef]
- Davis, S.E.; Wallace, A.M. A 19 Year Old with Complete Androgen Insensitivity Syndrome and Juvenile Fibroadenoma of the Breast. Breast J. 2001, 7, 430–433. [Google Scholar] [CrossRef] [PubMed]
- Tantrige, P.M.; Hassanally, D. Recurrent giant juvenile fibroadenomas with hemihypertrophy. Breast Dis. 2011, 33, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Baxi, A.A.M. Multiple Bilateral Giant Juvenile Fibroadenomas of Breast. Eur. J. Surg. 2000, 166, 828–830. [Google Scholar] [CrossRef] [PubMed]
- Kamei, S.T.Y. Natural skin reduction and breast recovery using a tissue expander after enucleation of a giant breast tumour. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2000, 34, 383–385. [Google Scholar] [CrossRef] [PubMed]
- Simmons, R.M.; Cance, W.G.; Iacicca, M.V. A Giant Juvenile Fibroadenoma in a 12-Year-Old Girl: A Case for Breast Conservation. Breast J. 2000, 6, 418–420. [Google Scholar] [CrossRef] [PubMed]
- Silfen, R.; Skoll, P.J.; Hudson, D.A. Florid Juvenile (Cellular) Fibroadenomatosis in the Adolescent: A Case for Subcutaneous Mastectomy? Aesthetic Plast. Surg. 1999, 23, 413–415. [Google Scholar] [CrossRef]
- Tian, J.; Liu, X.; Chen, Q. Giant fibroma of breast in an adolescent female by inverted “T” incision: A case report and literature review. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2020, 45, 204–207. [Google Scholar] [CrossRef]
- Hoffman, S. Giant fibroadenoma of the breast: Immediate reconstruction following excision. Br. J. Plast. Surg. 1978, 31, 170–172. [Google Scholar] [CrossRef]
- Yu, J. Treatment of Giant Juvenile Breast Fibroadenoma by Single Hole Breast Endoscopy: A Case Report. Acta Endocrinol. (Bucharest) 2021, 17, 552–553. [Google Scholar] [CrossRef]
- Zeeshan, S.; Shaikh, K.; Tariq, M.U.; Vohra, L.M. Giant Juvenile Fibroadenoma of the breast in a 13-year-old Pakistani girl with excellent cosmetic outcome after subareolar enucleation–A case report. Int. J. Surg. Case Rep. 2021, 79, 450–454. [Google Scholar] [CrossRef]
- Baral, S.; Gyawali, M.; Thapa, N.; Chhetri, R.K.; Dahal, P. Giant juvenile fibroadenoma in an adolescent female: A case report. Clin. Case Rep. 2020, 8, 3488–3492. [Google Scholar] [CrossRef]
- Islam, S.; Saroop, S.; Bheem, V.; Naraynsingh, V. Largest giant juvenile fibroadenoma of the breast. BMJ Case Rep. 2019, 12, e227277. [Google Scholar] [CrossRef] [PubMed]
- Mashiloane, J.M.C.D. Juvenile fibroadenoma during pregnancy. J. Obstet. Gynaecol. 2000, 20, 86. [Google Scholar] [CrossRef] [PubMed]
- Ugburo, A.O.; Olajide, T.O.; Fadeyibi, I.O.; Mofikoya, B.O.; Lawal, A.O.; Osinowo, A.O. Differential diagnosis and management of giant fibroadenoma: Comparing excision with reduction mammoplasty incision and excision with inframammary incision. J. Plast. Surg. Hand Surg. 2012, 46, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Greydanus, D.E.; Parks, D.S.; Farrell, E.G. Breast Disorders in Children and Adolescents. Pediatr. Clin. N. Am. 1989, 36, 601–638. [Google Scholar] [CrossRef]
- Smith, G.; Burrows, P. Ultrasound diagnosis of fibroadenoma—Is biopsy always necessary? Clin. Radiol. 2008, 63, 511–515. [Google Scholar] [CrossRef]
- Templeman, C.; Hertweck, S.P. Breast disorders in the pediatric and adolescent patient. Obstet. Gynecol. Clin. N. Am. 2000, 27, 19–34. [Google Scholar] [CrossRef]
- Sklair-Levy, M.; Sella, T.; Alweiss, T.; Craciun, I.; Libson, E.; Mally, B. Incidence and Management of Complex Fibroadenomas. Am. J. Roentgenol. 2008, 190, 214–218. [Google Scholar] [CrossRef]
- Emans, S.J.; Laufer, M.R.; DiVasta, A. The breast: Examination and lesions. In Pediatric & Adolescent Gynecology, 7th ed.; Lippincott Williams & Wilkins (LWW): Philadelphia, PA, USA, 2019; p. 781. [Google Scholar]
- Golatta, M.; Harcos, A.; Pavlista, D.; Danes, J.; Klein, R.; Simovich, P.; Gruber, I.; Hahn, M. Ultrasound-guided cryoablation of breast fibroadenoma: A pilot trial. Arch. Gynecol. Obstet. 2014, 291, 1355–1360. [Google Scholar] [CrossRef]
- Kaufman, C.S.; Littrup, P.J.; A Freman-Gibb, L.; Francescatti, D.; Stocks, L.H.; Smith, S.J.; Henry, A.C.; Bailey, L.; Harness, J.K.; Simmons, R. Office-Based cryoablation of breast fibroadenomas: 12-month followup. J. Am. Coll. Surg. 2004, 198, 914–923. [Google Scholar] [CrossRef]
- Littrup, P.J.; Freeman-Gibb, L.; Andea, A.; White, M.; Amerikia, K.C.; Bouwman, D.; Harb, T.; Sakr, W. Cryotherapy for Breast Fibroadenomas. Radiology 2005, 234, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, R.; Skornick, Y.; Kaplan, O. Management of breast fibroadenomas. J. Gen. Intern. Med. 1998, 13, 640–645. [Google Scholar] [CrossRef] [PubMed]
- West, K.W.; Rescorla, F.J.; Scherer, L.; Grosfeld, J.L. Diagnosis and treatment of symptomatic breast masses in the pediatric population. J. Pediatr. Surg. 1995, 30, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Chao, T.-C.; Lo, Y.-F.; Chen, S.-C.; Chen, M.-F. Sonographic features of phyllodes tumors of the breast. Ultrasound Obstet. Gynecol. 2002, 20, 64–71. [Google Scholar] [CrossRef] [PubMed]
- ACOG Committee on Adolescent Health Care ACOG Committee Opinion No. 350: Breast Concerns in the Adolescent. Obstet. Gynecol. 2006, 108, 1329–1336. [CrossRef] [PubMed]



| Authors | Country | Size (cm) | Unilateral–Bilateral | Location (Right/Left) | Age (Years) | Menarcheal Status (pre/post) | Treatment | No. of Patients |
|---|---|---|---|---|---|---|---|---|
| Celik et al. 2015 [52] | Turkey | 9.5 × 8 × 6 | unilateral | right | 10 | N/A | total lump excision | 1 |
| Yu et al. 2021 [61] | China | 9.65 × 5.80 × 5.5 | unilateral | left | 11 | N/A | single-hole breast endoscopic resection | 1 |
| Zeeshan et al. 2021 [62] | Pakistan | 13.5 × 11.5 × 6 | unilateral | left | 13 | post | total lump excision | 1 |
| Baral et al. 2020 [63] | Nepal | 9 × 7 | unilateral | right | 18 | post | total lump excision | 1 |
| Islam et al. 2019 [64] | Trinidad and Tobago | 28 × 25 | unilateral | left | 16 | post | total lump excision | 1 |
| Makkar et al. 2017 [9] | India | right lump: 6 × 5/ left lumps: 10 × 6 and 2 × 3 | bilateral | N/A | 14 | pre | bilateral total lump excisions | 1 |
| Celik S. et al. 2017 [10] | India | 17 × 13 × 5.5 | unilateral | left | 14 | post | total lump excision | 1 |
| Jategaonkar et al. 2018 [11] | India | right lump: 63 × 47/ left lump: 51 × 39 | bilateral | N/A | 17 | N/A | bilateral simple mastectomy with synchronous breast reconstructions | 1 |
| Juarez et al. 2021 [12] | Mexico | 16 × 13 | unilateral | left | 14 | N/A | total lump excision | 1 |
| Kupsik et al. 2017 [13] | USA | 11.2 × 8.5 × 6.7 | unilateral | right | 9 | pre | total lump excision | 1 |
| Khan et al. 2015 [14] | Pakistan | right lump: 6 × 5/ left lump: 10 × 15 | bilateral | N/A | 10 | pre | bilateral total lump excisions | 1 |
| Giannos et al. 2017 [19] | Greece | 14 × 12 | unilateral | right | 12 | pre | total lump excision | 1 |
| Gaurav et al. 2015 [15] | India | 20 × 20 | unilateral | left | 10 | pre | total lump excision | 1 |
| Mohd Firdaus et al. 2017 [16] | Malaysia | 12 × 9 × 5 | unilateral | right | 12 | N/A | total lump excision | 1 |
| Gkali et al. 2017 [17] | Greece | 15 × 13 | unilateral | right | 12 | pre | total lump excision | 1 |
| Nishtha et al. 2021 [18] | India | 15.5 × 9 × 10.5 | unilateral | right | 14 | pre | total lump excision | 1 |
| Bayramoglu et al. 2018 [20] | Turkey | 8.3 × 9.9 × 5.5 | unilateral | left | 14 | N/A | partial mastectomy with synchronous breast reconstruction with an implant | 1 |
| Rafeek et al. 2016 [21] | India | right lump: 39 × 22 × 17/ left lump: 40 × 24 × 18 | bilateral | N/A | 13 | post | bilateral total lump excisions with synchronous reduction mammoplasty | 1 |
| Kitazawa et al. 2022 [22] | Japan | 13 × 9 × 4.5 | unilateral | left | 14 | N/A | total lump excision | 1 |
| Wang et al. 2020 [23] | China | 6 × 6 | unilateral | left | 19 | N/A | total lump excision | 1 |
| Heng et al. 2020 [24] | Malaysia | 10.6 × 14.5 × 15.1 | unilateral | right | 19 | post | mastectomy with synchronous breast reconstruction | 1 |
| Tian et al. 2020 [59] | China | 22 × 16 × 11 | unilateral | right | 18 | N/A | total lump excision | 1 |
| Kaur et al. 2015 [30] | India | numerous tumors on both breasts, number not specified, size 1.5–2.5 | bilateral | N/A | 15 | post | bilateral subcutaneous mastectomy | 1 |
| Kozomara et al. 2016 [41] | Boznia Herzegovina | 20 × 20 × 15 | unilateral | left | 16 | N/A | reduction mammoplasty technique of the left breast | 1 |
| Ezer et al. 2013 [25] | Turkey | P1: 25 × 12/ P2: 30 × 16/ P3: 45 × 20/ P4: 60 × 35 | unilateral | not specified | P1: 14, P2: 17, P3: 10, P4: 14 | N/A | total lump excision | 4 |
| Matz et al. 2013 [26] | USA | 8.9 × 9.8 × 8.8 | unilateral | left | 13 | N/A | total lump excision | 1 |
| Arowolo et al. 2013 [27] | Nigeria | 20 × 30 | unilateral | left | 14 | pre | total lump excision with synchronous breast reconstruction | 1 |
| Biswas et al. 2012 [28] | Bangladesh | P1: 15 × 13/ P2: 11 × 11 | unilateral | P1: right, P2: left | P1: 14, P2: 16 | N/A | total lump excision | 2 |
| Sosin et al. 2012 [7] | USA | 12.1 | unilateral | right | 13 | N/A | total lump excision | 1 |
| Cheng et al. 2012 [29] | USA | P1: 5/ P2: 8/ P3: 10.5 | unilateral | P1: left, P2: left, P3: left | P1: 17, P2: 13, P3: 15 | N/A | endoscopic specimen pouch technique | 3 |
| Heilmann et al. 2012 [31] | Germany | 13 × 12.5 × 4.5 | unilateral | right | 17 | post | total lump excision | 1 |
| Izadpanah et al. 2012 [32] | Canada | 7.3 × 9.3 × 8.9 | unilateral | left | 12 | post | total lump excision | 1 |
| Chepla et al. 2011 [34] | USA | P1: 11.6 × 9.8 × 11.3/ P2: 15 × 4 × 4 | unilateral | P1: left/P2: right | P1: 10, P2: 16 | N/A | total lump excision | 2 |
| Ng et al. 2011 [35] | Canada | 19 | unilateral | right | 17 | N/A | total lump excision | 1 |
| Nikumbh et al. 2011 [36] | India | right lump: 15 × 12/ left lump: 17 × 15 | bilateral | N/A | 12 | pre | total excision of bilateral breast lumps conserving the normal breast tissue, nipple, and areola by the plastic surgeon | 1 |
| Tantrige et al. 2011 [54] | UK | 12 | unilateral | left | 13 | N/A | total lump excision | 1 |
| Yagnik et al. 2011 [37] | India | 13 × 11 × 12 | unilateral | right | 15 | N/A | total lump excision | 1 |
| Poh et al. 2010 [38] | USA | not described | bilateral | N/A | 12 | post | Right breast: excision of 6 discreet masses through vertical incision, laterally based pedicle used for nipple–areola complex/Left breast: subcutaneous mastectomy through “inverted T” incision, nipple–areola complex was salvaged as a free nipple graft. | 1 |
| Biggers et al. 2009 [39] | USA | P1: 5.9/ P2: 10.5/ P3: 12/ P4: 17 | unilateral | not specified | P1: 11/ P2: 12/ P3: 14/ P4: 15 | N/A | total lump excision (inframammary approach) | 4 |
| Calcaterra et al. 2009 [40] | Italy | 14 × 16 × 17 | unilateral | right | 12 | N/A | total lump excision (inframammary approach) | 1 |
| Gobbi et al. 2009 [42] | Italy | P1: 8/ P2: 10 | unilateral | P1: left/ P2: left | P1: 12/ P2: 15 | P1: N/A/ P2: post | total lump excision | 2 |
| Mukhopadhyay et al. 2009 [43] | India | right lump: 22 × 20/ left lump: 18 × 16 | bilateral | N/A | 11 | pre | bilateral lump excision conserving normal breast tissue, nipple, and areola | 1 |
| Wolfram et al. 2009 [44] | Austria | 5 | unilateral | right | 15 | N/A | total lump excision | 1 |
| Dolmans et al. 2007 [45] | Netherlands | 9 × 9 | unilateral | left | 18 | N/A | nipple-sparing subcutaneous mastectomy of the left breast | 1 |
| Moore et al. 2007 [46] | USA | right breast fibrofatty mass (1040 g): 17.0 × 15.0 × 7.0/ left breast fibrofatty mass (1111 g): 18.5 × 16 × 7.5 | bilateral | N/A | 9 | pre | bilateral subtotal mastectomies | 1 |
| Ahuja et al. 2005 [47] | India | not described | unilateral | right | 12 | N/A | total lump excision | 1 |
| Lee et al. 2004 [48] | South Korea | multiple nodules, the largest: 17 × 3 × 3, others not described | bilateral | N/A | 11 | post | central pedicle reduction mammoplasty | 1 |
| Zacharia et al. 2003 [49] | India | 8 × 5 | unilateral | right | 13 | N/A | total lump excision | 1 |
| Hanna et al. 2002 [50] | Kuwait | right lump: 6 × 6 × 5/ left lump: 5.5 × 5 × 6 | bilateral | N/A | 15 | N/A | not specified | 1 |
| Wechselberger et al. 2002 [51] | Austria | not described | unilateral | right | 15 | N/A | total lump excision | 1 |
| Davis et al. 2001 [53] | USA | 5 × 3.5 × 2.5 | unilateral | right | 19 | N/A (CAIS) | total lump excision | 1 |
| Baxi et al. 2000 [55] | India | right breast: 17 firm nodules (mean diameter 4, range 1–8)/ left breast: 9 (mean diameter 8, range 1–11) | bilateral | N/A | 16 | post | total lump excision | 1 |
| Kamei et al. 2000 [56] | Japan | P1: 11 × 10 × 5/ P2: 10 × 9 × 8 | unilateral | left | P1: 19/ P2: 17 | N/A | total lump excision | 2 |
| Simmons et al. 2000 [57] | USA | 16 | unilateral | right | 12 | N/A | total lump excision | 1 |
| Silfen et al. 1999 [58] | South Africa | not described | bilateral | N/A | 13 | N/A | bilateral reduction mammoplasty | 1 |
| Hoffman et al. 1978 [60] | US | not described | unilateral | right | 13 | N/A | total lump excision with synchronous reduction mammoplasty | 1 |
| Song et al. 2014 [8] | South Korea | 13 × 8 | unilateral | right | 12 | post | total lump excision | 1 |
| Mashiloane 2000 [65] | South Africa | not described | unilateral | right | 16 | post (during pregnancy) | mastectomy | 1 |
| Ugburo et al. 2012 [66] | Nigeria | not described | 14 patients unilateral, 2 patients bilateral | not specified | mean 14.06 ± 0.42 (range 12–18) | post | total lump excision | 16 |
| Eleftheriades et al. 2022 (our case) | Greece | 10 × 8 × 2.5 | unilateral | right | 11 | pre | total lump excision | 1 |
| Total Number of Cases: | 87 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eleftheriades, A.; Tsarna, E.; Toutoudaki, K.; Paschalidou, E.; Christopoulos, N.; Georgopoulos, I.; Mitropoulou, G.; Christopoulos, P. Giant Juvenile Fibroadenoma: Case Report and Review of the Literature. J. Clin. Med. 2023, 12, 1855. https://doi.org/10.3390/jcm12051855
Eleftheriades A, Tsarna E, Toutoudaki K, Paschalidou E, Christopoulos N, Georgopoulos I, Mitropoulou G, Christopoulos P. Giant Juvenile Fibroadenoma: Case Report and Review of the Literature. Journal of Clinical Medicine. 2023; 12(5):1855. https://doi.org/10.3390/jcm12051855
Chicago/Turabian StyleEleftheriades, Anna, Ermioni Tsarna, Konstantina Toutoudaki, Eleni Paschalidou, Nikolaos Christopoulos, Ioannis Georgopoulos, Georgia Mitropoulou, and Panagiotis Christopoulos. 2023. "Giant Juvenile Fibroadenoma: Case Report and Review of the Literature" Journal of Clinical Medicine 12, no. 5: 1855. https://doi.org/10.3390/jcm12051855
APA StyleEleftheriades, A., Tsarna, E., Toutoudaki, K., Paschalidou, E., Christopoulos, N., Georgopoulos, I., Mitropoulou, G., & Christopoulos, P. (2023). Giant Juvenile Fibroadenoma: Case Report and Review of the Literature. Journal of Clinical Medicine, 12(5), 1855. https://doi.org/10.3390/jcm12051855






