The Impact of COVID-19 Pandemic First Wave on Healthcare Workers: A New Perspective from Qualifying PTSD Criterion A to Assessing Post-Traumatic Growth
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Assessments
2.3. Impact of Event Scale-Revised (IES-R)
2.4. Post-Traumatic Growth Inventory-Short Form (PTGI-SF)
2.5. Statistical Analysis
3. Results
3.1. Post-Traumatic and Post-Traumatic Growth Features
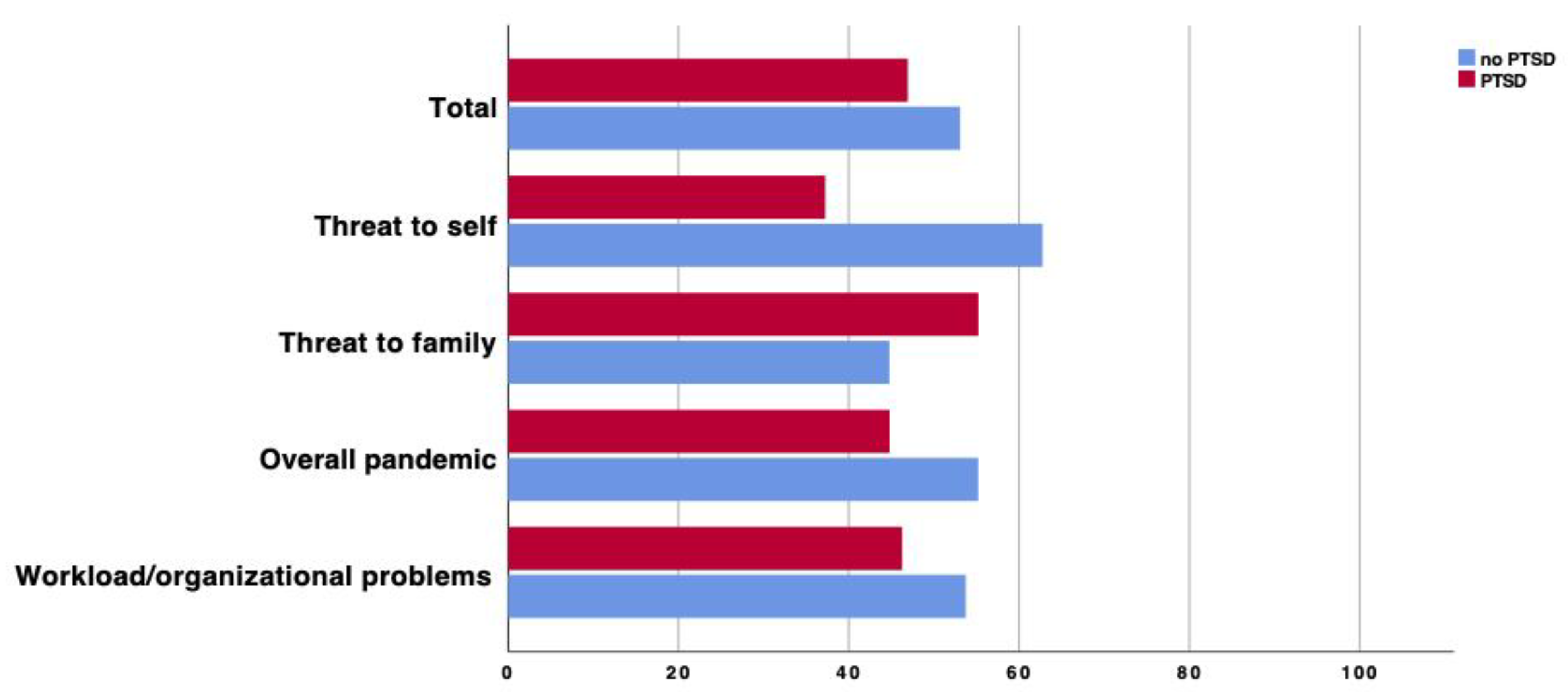
3.2. Predictors of PTSD
4. Discussion
4.1. Type of Trauma, PTSD Prevalence and Post-Traumatic Growth Features
4.2. Predictors of PTSD
4.3. Modifiable Factors in the Management of the Pandemic
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J. Trauma. Stress 1996, 9, 455–472. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. Target Article: “Posttraumatic Growth: Conceptual Foundations and Empirical Evidence”. Psychol. Inq. 2004, 15, 1–18. [Google Scholar] [CrossRef]
- Feingold, J.H.; Hurtado, A.; Feder, A.; Peccoralo, L.; Southwick, S.M.; Ripp, J.; Pietrzak, R.H. Posttraumatic growth among health care workers on the frontlines of the COVID-19 pandemic. J. Affect. Disord. 2022, 296, 35–40. [Google Scholar] [CrossRef]
- Cui, P.P.; Wang, P.P.; Wang, K.; Ping, Z.; Wang, P.; Chen, C. Post-traumatic growth and influencing factors among frontline nurses fighting against COVID-19. Occup. Environ. Med. 2021, 78, 129–135. [Google Scholar] [CrossRef]
- Peng, X.; Zhao, H.; Yang, Y.; Rao, Z.; Hu, D.; He, Q. Post-traumatic Growth Level and Its Influencing Factors Among Frontline Nurses During the COVID-19 Pandemic. Front. Psychiatry 2021, 12, 632360. [Google Scholar] [CrossRef]
- Beck, J.G.; Grant, D.M.; Read, J.P.; Clapp, J.D.; Coffey, S.F.; Miller, L.M.; Palyo, S.A. The impact of event scale-revised: Psychometric properties in a sample of motor vehicle accident survivors. J. Anxiety Disord. 2008, 22, 187–198. [Google Scholar] [CrossRef] [Green Version]
- Fattori, A.; Cantù, F.; Comotti, A.; Tombola, V.; Colombo, E.; Nava, C.; Brambilla, P. Hospital workers mental health during the COVID-19 pandemic: Methods of data collection and characteristics of study sample in a university hospital in Milan (Italy). BMC Med. Res. Methodol. 2021, 21, 163. [Google Scholar] [CrossRef]
- Craparo, G.; Faraci, P.; Rotondo, G.; Gori, A. The Impact of Event Scale-Revised: Psychometric properties of the Italian version in a sample of flood victims. Neuropsychiatr Dis. Treat 2013, 9, 1427–1432. [Google Scholar] [CrossRef] [Green Version]
- Creamer, M.; Bell, R.; Failla, S. Psychometric properties of the impact of event scale—Revised. Behav. Res. Ther. 2003, 41, 1489–1496. [Google Scholar] [CrossRef]
- Aljaberi, M.A.; Lee, K.H.; Alareqe, N.A.; Qasem, M.A.; Alsalahi, A.; Abdallah, A.M. Rasch Modeling and Multilevel Confirmatory Factor Analysis for the Usability of the Impact of Event Scale-Revised (IES-R) during the COVID-19 Pandemic. Healthcare 2022, 10, 1858. [Google Scholar] [CrossRef]
- Prati, G.; Pietrantoni, L. Italian Adaptation and Confirmatory Factor Analysis of the Full and the Short Form of the Posttraumatic Growth Inventory. J. Loss Trauma 2014, 19, 12–22. [Google Scholar] [CrossRef]
- Carmassi, C.; Dell’Oste, V.; Bui, E.; Foghi, C.; Bertelloni, C.A.; Atti, A.R.; Buselli, R.; Di Paolo, M.; Goracci, A.; Malacarne, P.; et al. The interplay between acute post-traumatic stress, depressive and anxiety symptoms on healthcare workers functioning during the COVID-19 emergency: A multicenter study comparing regions with increasing pandemic incidence. J. Affect. Disord. 2022, 298, 209–216. [Google Scholar] [CrossRef]
- Carmassi, C.; Cerveri, G.; Bertelloni, C.A.; Marasco, M.; Dell’Oste, V.; Massimetti, E.; Gesi, C.; Dell’Osso, L. Mental health of frontline help-seeking healthcare workers during the COVID-19 outbreak in the first affected hospital in Lombardy, Italy. Psychiatry Res. 2021, 298, 113763. [Google Scholar] [CrossRef]
- Ghio, L.; Patti, S.; Piccinini, G.; Modafferi, C.; Lusetti, E.; Mazzella, M.; Del Sette, M. Anxiety, Depression and Risk of Post-Traumatic Stress Disorder in Health Workers: The Relationship with Burnout during COVID-19 Pandemic in Italy. IJERPH 2021, 18, 9929. [Google Scholar] [CrossRef]
- Conti, C.; Fontanesi, L.; Lanzara, R.; Rosa, I.; Porcelli, P. Fragile heroes. The psychological impact of the COVID-19 pandemic on health-care workers in Italy. PLoS ONE 2020, 15, e0242538. [Google Scholar] [CrossRef]
- Collantoni, E.; Saieva, A.; Meregalli, V.; Girotto, C.; Carretta, G.; Boemo, D.; Bordignon, G.; Capizzi, A.; Contessa, C.; Nesoti, M.; et al. Psychological Distress, Fear of COVID-19, and Resilient Coping Abilities among Healthcare Workers in a Tertiary First-Line Hospital during the Coronavirus Pandemic. JCM 2021, 10, 1465. [Google Scholar] [CrossRef]
- Yunitri, N.; Chu, H.; Kang, X.L.; Jen, H.-J.; Pien, L.-C.; Tsai, H.-T.; Kamil, A.R.; Chou, K.-R. Global prevalence and associated risk factors of posttraumatic stress disorder during COVID-19 pandemic: A meta-analysis. Int. J. Nurs. Stud. 2022, 126, 104136. [Google Scholar] [CrossRef]
- Cluver, L.; Lachman, J.M.; Sherr, L.; Wessels, I.; Krug, E.; Rakotomalala, S.; Blight, S.; Hillis, S.; Bachman, G.; Green, O.; et al. Parenting in a time of COVID-19. Lancet 2020, 395, e64. [Google Scholar] [CrossRef]
- Carmassi, C.; Cerveri, G.; Bui, E.; Gesi, C.; Dell’Osso, L. Defining effective strategies to prevent post-traumatic stress in healthcare emergency workers facing the COVID-19 pandemic in Italy. CNS Spectr. 2021, 26, 553–554. [Google Scholar] [CrossRef]
- Norrholm, S.D.; Zalta, A.; Zoellner, L.; Powers, A.; Tull, M.T.; Reist, C.; Schnurr, P.P.; Weathers, F.; Friedman, M.J. Does COVID-19 count?: Defining Criterion A trauma for diagnosing PTSD during a global crisis. Depress. Anxiety 2021, 38, 882–885. [Google Scholar] [CrossRef]
- Maia, Â.; Sousa, B.; Correia-Santos, P.; Morgado, D. Posttraumatic stress symptoms and posttraumatic growth in a community sample exposed to stressful events: A (not so) curvilinear relationship. Traumatology 2022, 28, 98–108. [Google Scholar] [CrossRef]
- Shalev, A.; Liberzon, I.; Marmar, C. Post-Traumatic Stress Disorder. N. Engl. J. Med. 2017, 376, 2459–2469. [Google Scholar] [CrossRef]
- Brewin, C.R.; Andrews, B.; Valentine, J.D. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J. Consult. Clin. Psychol. 2000, 68, 748–766. [Google Scholar] [CrossRef]
- Fauerbach, J.A.; Lawrence, J.; Haythornthwaite, J.; McGuire, M.; Munster, A. Preinjury psychiatric illness and postinjury adjustment in adult burn survivors. Psychosomatics 1996, 37, 547–555. [Google Scholar] [CrossRef]
- Bedaso, A.; Kediro, G.; Ebrahim, J.; Tadesse, F.; Mekonnen, S.; Gobena, N.; Gebrehana, E. Prevalence and determinants of post-traumatic stress disorder among road traffic accident survivors: A prospective survey at selected hospitals in southern Ethiopia. BMC Emerg. Med. 2020, 20, 52. [Google Scholar] [CrossRef]
- Bassi, M.; Negri, L.; Delle Fave, A.; Accardi, R. The relationship between post-traumatic stress and positive mental health symptoms among health workers during COVID-19 pandemic in Lombardy, Italy. J. Affect. Disord. 2021, 280, 1–6. [Google Scholar] [CrossRef]
- Di Mattei, V.; Perego, G.; Milano, F.; Mazzetti, M.; Taranto, P.; Di Pierro, R.; De Panfilis, C.; Madeddu, F.; Preti, E. The “Healthcare Workers’ Wellbeing (Benessere Operatori)” Project: A Picture of the Mental Health Conditions of Italian Healthcare Workers during the First Wave of the COVID-19 Pandemic. IJERPH 2021, 18, 5267. [Google Scholar] [CrossRef]
- Bongelli, R.; Canestrari, C.; Fermani, A.; Muzi, M.; Riccioni, I.; Bertolazzi, A.; Burro, R. Associations between Personality Traits, Intolerance of Uncertainty, Coping Strategies, and Stress in Italian Frontline and Non-Frontline HCWs during the COVID-19 Pandemic—A Multi-Group Path-Analysis. Healthcare 2021, 9, 1086. [Google Scholar] [CrossRef]
- Trumello, C.; Bramanti, S.M.; Ballarotto, G.; Candelori, C.; Cerniglia, L.; Cimino, S.; Crudele, M.; Lombardi, L.; Pignataro, S.; Viceconti, M.L.; et al. Psychological Adjustment of Healthcare Workers in Italy during the COVID-19 Pandemic: Differences in Stress, Anxiety, Depression, Burnout, Secondary Trauma, and Compassion Satisfaction between Frontline and Non-Frontline Professionals. IJERPH 2020, 17, 8358. [Google Scholar] [CrossRef]
- Orrù, G.; Marzetti, F.; Conversano, C.; Vagheggini, G.; Miccoli, M.; Ciacchini, R.; Panait, E.; Gemignani, A. Secondary Traumatic Stress and Burnout in Healthcare Workers during COVID-19 Outbreak. IJERPH 2021, 18, 337. [Google Scholar] [CrossRef]
- Dyregrov, A.; Kristoffersen, J.I.; Gjestad, R. Voluntary and professional disaster-workers: Similarities and differences in reactions. J. Traum Stress 1996, 9, 541–555. [Google Scholar] [CrossRef]
- Honarmand, K.; Yarnell, C.J.; Young-Ritchie, C.; Maunder, R.; Priestap, F.; Abdalla, M.; Ball, I.M.; Basmaji, J.; Bell, C.M.; Jeffs, L.; et al. Personal, professional, and psychological impact of the COVID-19 pandemic on hospital workers: A cross-sectional survey. PLoS ONE 2022, 17, e0263438. [Google Scholar] [CrossRef]
- Asnakew, S.; Legas, G.; Liyeh, T.M.; Belete, A.; Haile, K.; Yitbarek, G.Y.; Bayih, W.A.; Feleke, D.G.; Birhane, B.M.; Amha, H.; et al. Prevalence of post-traumatic stress disorder on health professionals in the era of COVID-19 pandemic, Northwest Ethiopia, 2020: A multi-centered cross-sectional study. PLoS ONE 2021, 16, e0255340. [Google Scholar] [CrossRef]
- Wanigasooriya, K.; Palimar, P.; Naumann, D.N.; Ismail, K.; Fellows, J.L.; Logan, P.; Thompson, C.V.; Bermingham, H.; Beggs, A.D.; Ismail, T. Mental health symptoms in a cohort of hospital healthcare workers following the first peak of the COVID-19 pandemic in the UK. BJPsych Open 2021, 7, e24. [Google Scholar] [CrossRef]
- Pietrzak, R.H.; Tsai, J.; Southwick, S.M. Association of Symptoms of Posttraumatic Stress Disorder With Posttraumatic Psychological Growth Among US Veterans During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e214972. [Google Scholar] [CrossRef]
- Tsai, J.; El-Gabalawy, R.; Sledge, W.H.; Southwick, S.M.; Pietrzak, R.H. Post-traumatic growth among veterans in the USA: Results from the National Health and Resilience in Veterans Study. Psychol. Med. 2015, 45, 165–179. [Google Scholar] [CrossRef]
| B (SE) | Wald | df | p | OR | OR 95% CI | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Sex [Male] | 0.48 (0.23) | 4.59 | 1 | 0.03 | 1.62 | 1.04 | 2.52 |
| Age [Older than 40] | −0.46 (0.32) | 2.09 | 1 | 0.15 | 0.63 | 0.34 | 1.18 |
| Region [Lombardy] | 0.21 (0.25) | 0.68 | 1 | 0.41 | 0.801 | 0.75 | 2.01 |
| Date of completion [Before May 4th] | −0.24 (0.28) | 0.76 | 1 | 0.38 | 0.79 | 0.46 | 1.35 |
| Professional Role [Other] | 6.27 | 2 | 0.04 | ||||
| Nurse | −0.538 (0.36) | 1.11 | 1 | 0.29 | 0.69 | 0.34 | 1.39 |
| Physician | −1.05 (0.45) | 5.57 | 1 | 0.02 | 0.35 | 0.715 | 0.84 |
| Job seniority [more than 15 years] | 0.63 (0.32) | 3.77 | 1 | 0.05 | 1.87 | 0.99 | 3.52 |
| Previous mental disorders | 0.47 (0.22) | 4.40 | 1 | 0.04 | 1.60 | 1.03 | 2.47 |
| Workplace [Frontline] | 3.25 | 4 | 0.52 | ||||
| Medicine | 0.65 (0.56) | 1.32 | 1 | 0.25 | 1.91 | 0.63 | 5.78 |
| Surgery | −0.01 (0.49) | 0.01 | 1 | 0.99 | 1.00 | 0.37 | 2.67 |
| Territorial medicine | 0.01 (0.50) | 0.01 | 1 | 0.98 | 1.01 | 0.39 | 2.63 |
| Services/not specified | 0.16 (0.50) | 0.10 | 1 | 0.75 | 1.17 | 0.44 | 3.10 |
| Availability of PPE 1 | −0.63 (0.22) | 8.44 | 1 | 0.01 | 0.53 | 0.35 | 0.81 |
| Type of trauma [Threat to self] | 6.69 | 3 | 0.08 | ||||
| Work-related issues | 0.566 (0.38) | 2.17 | 1 | 0.14 | 1.76 | 0.83 | 3.74 |
| Overall pandemic | 0.26 (0.30) | 0.77 | 1 | 0.38 | 1.30 | 0.72 | 2.35 |
| Threat to family | 0.73 (0.32) | 5.29 | 1 | 0.02 | 2.07 | 1.11 | 3.83 |
| Infected (self) | 0.38 (0.34) | 1.28 | 1 | 0.26 | 1.46 | 0.76 | 2.83 |
| Infected family members | 0.139 (0.23) | 0.37 | 1 | 0.55 | 1.15 | 0.73 | 1.80 |
| Deceased family members | 0.124 (0.23) | 0.29 | 1 | 0.59 | 1.13 | 0.72 | 1.79 |
| Separation from cohabiting family | −46 (0.28) | 2.78 | 1 | 0.10 | 0.63 | 0.37 | 1.09 |
| Separation from non-cohabiting family | −0.20 (0.41) | 0.23 | 1 | 0.63 | 0.82 | 0.37 | 1.84 |
| Minor children | −0.15 (0.210) | 0.49 | 1 | 0.48 | 0.86 | 0.57 | 1.30 |
| Living parents | 0.04 (0.27) | 0.03 | 1 | 0.88 | 1.04 | 0.61 | 1.78 |
| Change in usual tasks | 0.09 (0.26) | 0.12 | 1 | 0.73 | 0.91 | 0.54 | 1.84 |
| Relocation to other units | 0.01 (0.31) | 0.01 | 1 | 0.99 | 0.99 | 0.54 | 1.82 |
| Relocation to COVID-19 units | 0.41 (0.27) | 2.37 | 1 | 0.123 | 1.50 | 0.90 | 2.53 |
| Unusual exposure to suffering | 1.149 (0.23) | 25.54 | 1 | <0.01 | 3.16 | 2.02 | 4.92 |
| PTG-SF 2 relating to others | −0.14 (0.25) | 0.031 | 1 | 0.58 | 0.87 | 0.53 | 1.42 |
| PTG-SF 2 spiritual change | −0.62 (0.23) | 7.75 | 1 | <0.01 | 0.544 | 0.346 | 0.832 |
| PTG-SF 2 appreciation of life | −0.33 (0.30) | 1.23 | 1 | 0.27 | 0.72 | 0.40 | 1.29 |
| PTG-SF 2 new possibilities | 0.34 (0.27) | 1.64 | 1 | 0.20 | 1.41 | 0.83 | 2.39 |
| PTG-SF 2 personal strength | 0.48 (0.28) | 2.94 | 1 | 0.09 | 1.63 | 0.93 | 2.83 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gesi, C.; Cirnigliaro, G.; Achilli, F.; Cerioli, M.; Cafaro, R.; Boscacci, M.; Dell’Osso, B. The Impact of COVID-19 Pandemic First Wave on Healthcare Workers: A New Perspective from Qualifying PTSD Criterion A to Assessing Post-Traumatic Growth. J. Clin. Med. 2023, 12, 1862. https://doi.org/10.3390/jcm12051862
Gesi C, Cirnigliaro G, Achilli F, Cerioli M, Cafaro R, Boscacci M, Dell’Osso B. The Impact of COVID-19 Pandemic First Wave on Healthcare Workers: A New Perspective from Qualifying PTSD Criterion A to Assessing Post-Traumatic Growth. Journal of Clinical Medicine. 2023; 12(5):1862. https://doi.org/10.3390/jcm12051862
Chicago/Turabian StyleGesi, Camilla, Giovanna Cirnigliaro, Francesco Achilli, Matteo Cerioli, Rita Cafaro, Maria Boscacci, and Bernardo Dell’Osso. 2023. "The Impact of COVID-19 Pandemic First Wave on Healthcare Workers: A New Perspective from Qualifying PTSD Criterion A to Assessing Post-Traumatic Growth" Journal of Clinical Medicine 12, no. 5: 1862. https://doi.org/10.3390/jcm12051862





