Determinants of Operative Time in Arthroscopic Rotator Cuff Repair
Abstract
:1. Introduction
1.1. Background
1.2. Aims
- (1)
- To determine what factors were associated with faster rotator cuff repairs in our practice.
- (2)
- To determine whether arthroscopic rotator cuff repairs can be performed in under 5 min.
2. Materials and Methods
2.1. Aim 1: Determinants of Operative Time
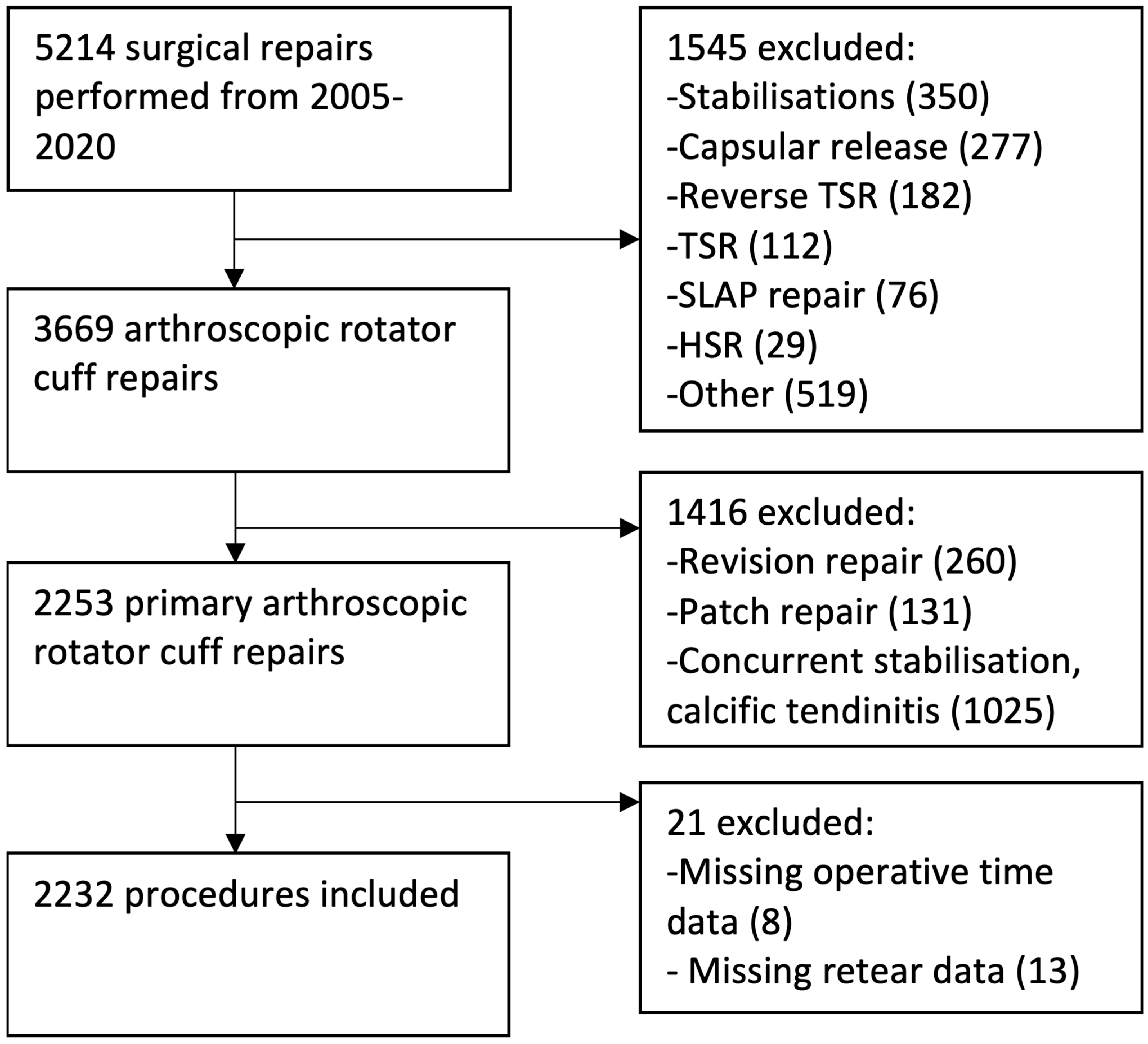
2.1.1. Inclusion and Exclusion Criteria
2.1.2. Pre-Operative Data
2.1.3. Operative Procedure
2.1.4. Operative Time
2.1.5. Intra-Operative Data
2.1.6. Repair Integrity
2.1.7. Statistical Analysis
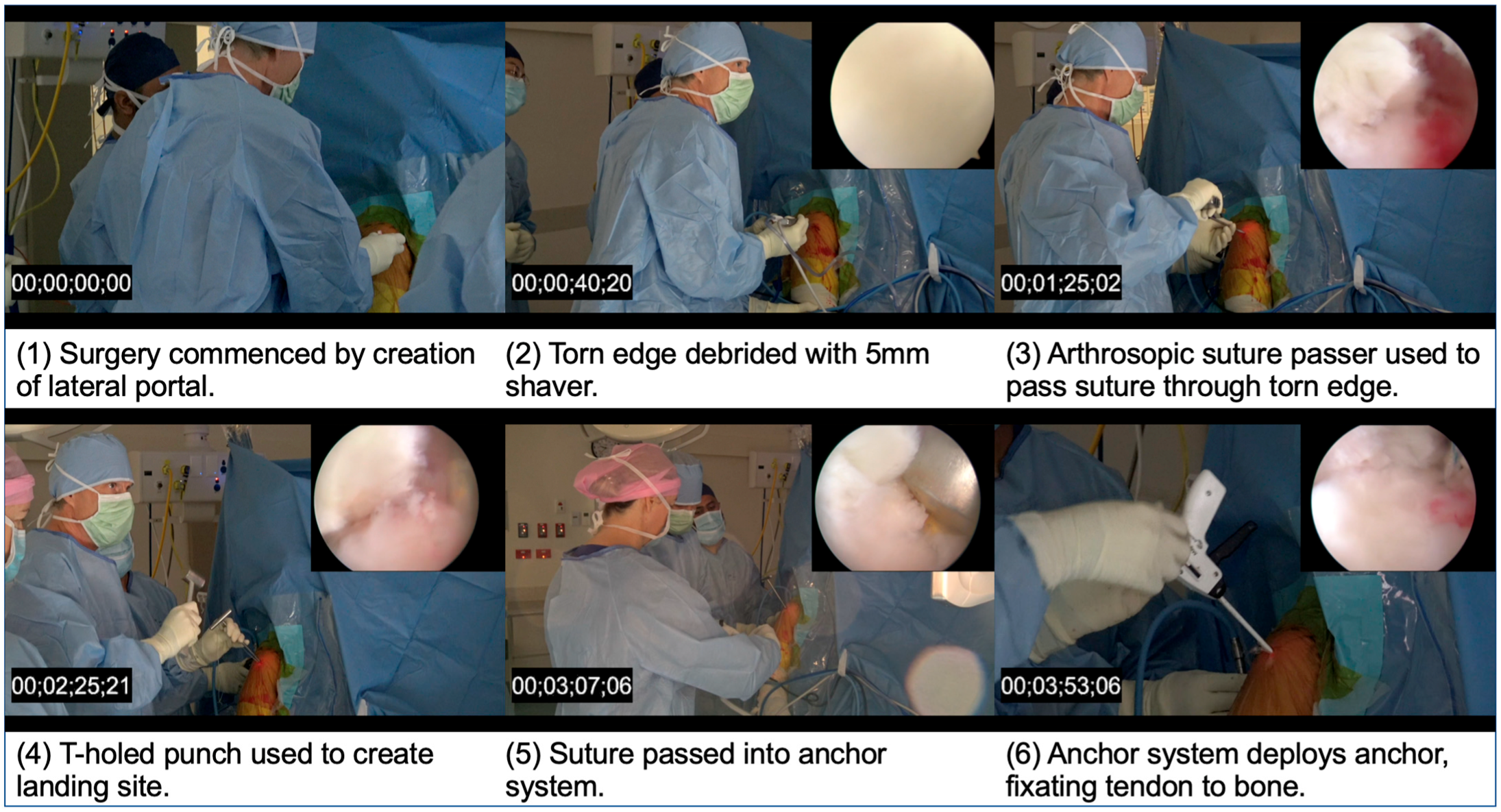
2.2. Aim 2: Capturing a Less Than 5-Min Rotator Cuff Repair
3. Results
3.1. Aim 1: Determinants of Operative Time
3.1.1. Cohort
3.1.2. Demographics
3.1.3. Multivariate Analysis
3.1.4. Effect of Surgical Technique
3.1.5. Number of Anchors
3.1.6. Effect of Surgeon Experience
3.1.7. Tear Size
3.1.8. Effect of Assistant Surgeon Experience
3.1.9. Sex
3.1.10. Repair Quality
3.1.11. Effect of Hospital Type
3.1.12. Factors That Did Not Affect Operative Time
3.2. Aim 2: Sub 5-Min Arthroscopic Rotator Cuff Repair
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jain, N.B.; Higgins, L.D.; Losina, E.; Collins, J.; Blazar, P.E.; Katz, J.N. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet. Disord. 2014, 15, 4. [Google Scholar] [CrossRef] [Green Version]
- Jain, N.B.; Pietrobon, R.; Guller, U.; Ahluwalia, A.S.; Higgins, L.D. Influence of provider volume on length of stay, operating room time, and discharge status for rotator cuff repair. J. Shoulder Elb. Surg. 2005, 14, 407–413. [Google Scholar] [CrossRef]
- Churchill, R.S.; Ghorai, J.K. Total cost and operating room time comparison of rotator cuff repair techniques at low, intermediate, and high volume centers: Mini-open versus all-arthroscopic. J. Shoulder Elbow. Surg. 2010, 19, 716–721. [Google Scholar] [CrossRef]
- Curry, E.J.; Logan, C.; Suslavich, K.; Whitlock, K.; Berkson, E.; Matzkin, E. Factors impacting arthroscopic rotator cuff repair operational throughput time at an ambulatory care center. Orthop. Rev. 2018, 10, 7577. [Google Scholar] [CrossRef] [Green Version]
- Warrender, W.J.; Brown, O.L.; Abboud, J.A. Outcomes of arthroscopic rotator cuff repairs in obese patients. J. Shoulder Elb. Surg. 2011, 20, 961–967. [Google Scholar] [CrossRef]
- Green, L.B.; Pietrobon, R.; Paxton, E.; Higgins, L.D.; Fithian, D. Sources of variation in readmission rates, length of stay, and operative time associated with rotator cuff surgery. J. Bone Jt. Surg. 2003, 85, 1784–1789. [Google Scholar] [CrossRef]
- Morris, J.H.; Malik, A.T.; Hatef, S.; Neviaser, A.S.; Bishop, J.Y.; Cvetanovich, G.L. Cost of Arthroscopic Rotator Cuff Repairs Is Primarily Driven by Procedure-Level Factors: A Single-Institution Analysis of an Ambulatory Surgery Center. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 85, 1784–1789. [Google Scholar] [CrossRef]
- Le, B.T.N.; Wu, X.L.; Lam, P.H.; Murrell, G.A.C. Factors Predicting Rotator Cuff Retears: An Analysis of 1000 Consecutive Rotator Cuff Repairs. Am. J. Sports Med. 2014, 42, 1134–1142. [Google Scholar] [CrossRef]
- Hill, J.R.; McKnight, B.; Pannell, W.C.; Heckmann, N.; Sivasundaram, L.; Mostofi, A.; Omid, R.; Hatch, G.F. Risk Factors for 30-Day Readmission Following Shoulder Arthroscopy. Arthrosc. J. Arthrosc. Relat. Surg. 2017, 33, 55–61. [Google Scholar] [CrossRef]
- Agarwalla, A.; Gowd, A.K.; Yao, K.; Bohl, D.D.; Amin, N.H.; Verma, N.N.; Forsythe, B.; Liu, J.N. A 15-Minute Incremental Increase in Operative Duration Is Associated with an Additional Risk of Complications Within 30 Days After Arthroscopic Rotator Cuff Repair. Orthop. J. Sports Med. 2019, 7, 2325967119860752. [Google Scholar] [CrossRef] [Green Version]
- Pauzenberger, L.; Grieb, A.; Hexel, M.; Laky, B.; Anderl, W.; Heuberer, P. Infections following arthroscopic rotator cuff repair: Incidence, risk factors, and prophylaxis. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 595–601. [Google Scholar] [CrossRef]
- Day, M.; Westermann, R.; Duchman, K.; Gao, Y.; Pugely, A.; Bollier, M.; Wolf, B. Comparison of Short-term Complications After Rotator Cuff Repair: Open Versus Arthroscopic. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 1130–1136. [Google Scholar] [CrossRef]
- Adla, D.N.; Rowsell, M.; Pandey, R. Cost-effectiveness of open versus arthroscopic rotator cuff repair. J. Shoulder Elb. Surg. 2010, 19, 258–261. [Google Scholar] [CrossRef]
- Hui, Y.J.; Teo, A.Q.A.; Sharma, S.; Tan, B.H.M.; Kumar, V.P. Immediate costs of mini-open versus arthroscopic rotator cuff repair in an Asian population. J. Orthop. Surg. 2017, 25, 2309499016684496. [Google Scholar] [CrossRef]
- Baker, D.K.; Perez, J.L.; Watson, S.L.; McGwin, G.; Ponce, B.A. Arthroscopic vs. open rotator cuff repair: Which has a better impact profile? J. Shoulder Elb. Surg. 2017, 26, e155. [Google Scholar] [CrossRef]
- Williams, G.; Kraeutler, M.J.; Zmistowski, B.; Fenlin, J.M. No Difference in Postoperative Pain After Arthroscopic versus Open Rotator Cuff Repair. Clin. Orthop. Relat. Res. 2014, 472, 2759–2765. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Fan, L.; Zhu, Y.; Yu, H.; Xu, T.; Li, G. Comparison of clinical outcomes in all-arthroscopic versus mini-open repair of rotator cuff tears: A randomized clinical trial. Medicine 2017, 96, e6322. [Google Scholar] [CrossRef]
- Van der Zwaal, P.; Thomassen, B.J.W.; Nieuwenhuijse, M.J.; Lindenburg, R.; Swen, J.-W.A.; Van Arkel, E.R.A. Clinical Outcome in All-Arthroscopic Versus Mini-Open Rotator Cuff Repair in Small to Medium-Sized Tears: A Randomized Controlled Trial in 100 Patients With 1-Year Follow-up. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 266–273. [Google Scholar] [CrossRef]
- Ji, X.; Bi, C.; Wang, F.; Wang, Q. Arthroscopic Versus Mini-Open Rotator Cuff Repair: An Up-to-Date Meta-analysis of Randomized Controlled Trials. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 118–124. [Google Scholar] [CrossRef]
- Wu, X.L.; Baldwick, C.; Briggs, L.; Murrell, G.A.C. Arthroscopic Undersurface Rotator Cuff Repair. Tech. Shoulder Elb. Surg. 2009, 10, 112–118. [Google Scholar] [CrossRef]
- Duong, J.K.H.; Lam, P.H.; Murrell, G.A.C. Anteroposterior tear size, age, hospital, and case number are important predictors of repair integrity: An analysis of 1962 consecutive arthroscopic single-row rotator cuff repairs. J. Shoulder Elb. Surg. 2021, 30, 1907–1914. [Google Scholar] [CrossRef] [PubMed]
- Briggs, L.; Murrell, G.A.C. Diagnostic Ultrasound: Examination of the Shoulder. Tech. Shoulder Elb. Surg. 2011, 12, 101–107. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: Abingdon, UK, 1988. [Google Scholar]
- Lachenbruch, P.A. Statistical Power Analysis for the Behavioral Sciences (2nd ed.). J. Am. Stat. Assoc. 1989, 84, 1096. [Google Scholar] [CrossRef]
- Burns, K.A.; Robbins, L.; LeMarr, A.R.; Childress, A.L.; Morton, D.J.; Wilson, M.L. Rotator Cuff Repair with Knotless Technique Is Quicker and More Cost-Effective Than Knotted Technique. Arthrosc. Sports Med. Rehabil. 2019, 1, e123–e130. [Google Scholar] [CrossRef] [Green Version]
- Boyd, J.A.; Karas, S.G.; Urchek, R.J.; Farley, K.X.; Anastasio, A.T.; Gottschalk, M.B. Factors influencing operative time in arthroscopic rotator cuff repair: A comparison of knotless single-row vs. transosseous equivalent dual-row techniques. J. Shoulder Elb. Surg. 2020, 29, S48–S52. [Google Scholar] [CrossRef]
- Elkins, A.; Lam, P.H.; Murrell, G.A.C. A Novel, Fast, Safe, and Effective All-Inside Arthroscopic Rotator Cuff Repair Technique: Results of 1000 Consecutive Cases. Orthop. J. Sports Med. 2019, 7, 2325967119864088. [Google Scholar] [CrossRef]
- Chahal, J.; Mall, N.; MacDonald, P.B.; Van Thiel, G.; Cole, B.J.; Romeo, A.A.; Verma, N.N. The Role of Subacromial Decompression in Patients Undergoing Arthroscopic Repair of Full-Thickness Tears of the Rotator Cuff: A Systematic Review and Meta-analysis. Arthrosc. J. Arthrosc. Relat. Surg. 2012, 28, 720–727. [Google Scholar] [CrossRef]
- Singh, C.; Lam, P.H.; Murrell, G.A.C. Effect of Acromioplasty on Postoperative Pain Following Rotator Cuff Repair. HSS J. 2021, 17, 150–157. [Google Scholar] [CrossRef]
- Nam, J.-H.; Park, S.; Lee, H.-R.; Kim, S.H. Outcomes After Limited or Extensive Bursectomy During Rotator Cuff Repair: Randomized Controlled Trial. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 3167–3174. [Google Scholar] [CrossRef]
- Morikawa, D.; Johnson, J.D.; Kia, C.; McCarthy, M.B.R.; Macken, C.; Bellas, N.; Baldino, J.B.; Cote, M.P.; Mazzocca, A.D. Examining the Potency of Subacromial Bursal Cells as a Potential Augmentation for Rotator Cuff Healing: An In Vitro Study. Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 2978–2988. [Google Scholar] [CrossRef]
- Maruthappu, M.; Duclos, A.; Zhou, C.D.; Lipsitz, S.R.; Wright, J.; Orgill, D.; Carty, M.J. The impact of team familiarity and surgical experience on operative efficiency: A retrospective analysis. J. R. Soc. Med. 2016, 109, 147–153. [Google Scholar] [CrossRef] [Green Version]
- Rubenis, I.; Lam, P.H.; Murrell, G.A. Arthroscopic Rotator Cuff Repair Using the Undersurface Technique: A 2-Year Comparative Study in 257 Patients. Orthop. J. Sports Med. 2015, 3, 2325967115605801. [Google Scholar] [CrossRef]






| Variable | Data |
|---|---|
| Sex, n (%) | |
| Male | 1259 (56%) |
| Female | 973 (44%) |
| Shoulder side, n (%) | |
| Right | 1338 (60%) |
| Left | 894 (40%) |
| Anteroposterior tear size, mm2 | |
| 2–24 | 1778 (77%) |
| 25–49 | 407 (18%) |
| 50–74 | 40 (2%) |
| 75–100 | 6 (0.003%) |
| Age, year | |
| Average (SD) | 59 (11) |
| Range | 15–91 |
| Hospital type, n (%) | |
| Private | 1711 (77%) |
| Public | 242 (11%) |
| Missing data | 279 (12%) |
| Repair technique, n (%) | |
| Undersurface | 1260 (56%) |
| Bursal-side | 247 (11%) |
| Undersurface and bursal-side | 483 (22%) |
| Missing data | 242 (11%) |
| Operative time, min | |
| Average (SD) | 21 (12) |
| Range | 3–97 |
| Repair integrity at 6 months, n (%) | |
| Intact | 1960 (88%) |
| Torn | 272 (12%) |
| Model | Unstandardised Coefficient | Standardised Coefficient Beta | t | Significance | f2 | Effect Direction—Faster Procedures Associated with: | |
|---|---|---|---|---|---|---|---|
| B | Standard Error | ||||||
| 18 (Constant) | 1.8 | 10 | <0.001 | ||||
| Repair technique | 8.3 | 0.7 | 0.3 | 11 | <0.001 | 0.08 | Undersurface technique |
| Number of anchors | 2.9 | 0.3 | 0.3 | 10 | <0.001 | 0.06 | Fewer anchors |
| Surgeon case number | −0.002 | <0.001 | −0.1 | −4.9 | <0.001 | 0.01 | Increased surgeon case number |
| Tear area | 0.002 | 0.001 | 0.1 | 4.3 | <0.001 | 0.01 | Smaller tears |
| Assistant case number | −0.011 | 0.003 | −0.1 | −3.9 | <0.001 | 0.008 | Increased assistant surgeon case number |
| Sex | 1.7 | 0.5 | 0.1 | 3.6 | <0.001 | 0.007 | Females |
| Repair quality | −1.1 | 0.4 | −0.1 | −3.2 | 0.001 | 0.006 | Higher ranked repair quality |
| Hospital type | −2.2 | 0.8 | −0.1 | −2.9 | 0.004 | 0.005 | Private hospital over public hospital |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stitz, D.J.; Guo, A.A.; Lam, P.H.; Murrell, G.A.C. Determinants of Operative Time in Arthroscopic Rotator Cuff Repair. J. Clin. Med. 2023, 12, 1886. https://doi.org/10.3390/jcm12051886
Stitz DJ, Guo AA, Lam PH, Murrell GAC. Determinants of Operative Time in Arthroscopic Rotator Cuff Repair. Journal of Clinical Medicine. 2023; 12(5):1886. https://doi.org/10.3390/jcm12051886
Chicago/Turabian StyleStitz, Daniel J., Allen A. Guo, Patrick H. Lam, and George A. C. Murrell. 2023. "Determinants of Operative Time in Arthroscopic Rotator Cuff Repair" Journal of Clinical Medicine 12, no. 5: 1886. https://doi.org/10.3390/jcm12051886





