Evaluation of the Pinhole Method Using Carbon Dioxide Laser on Facial Telangiectasia
Abstract
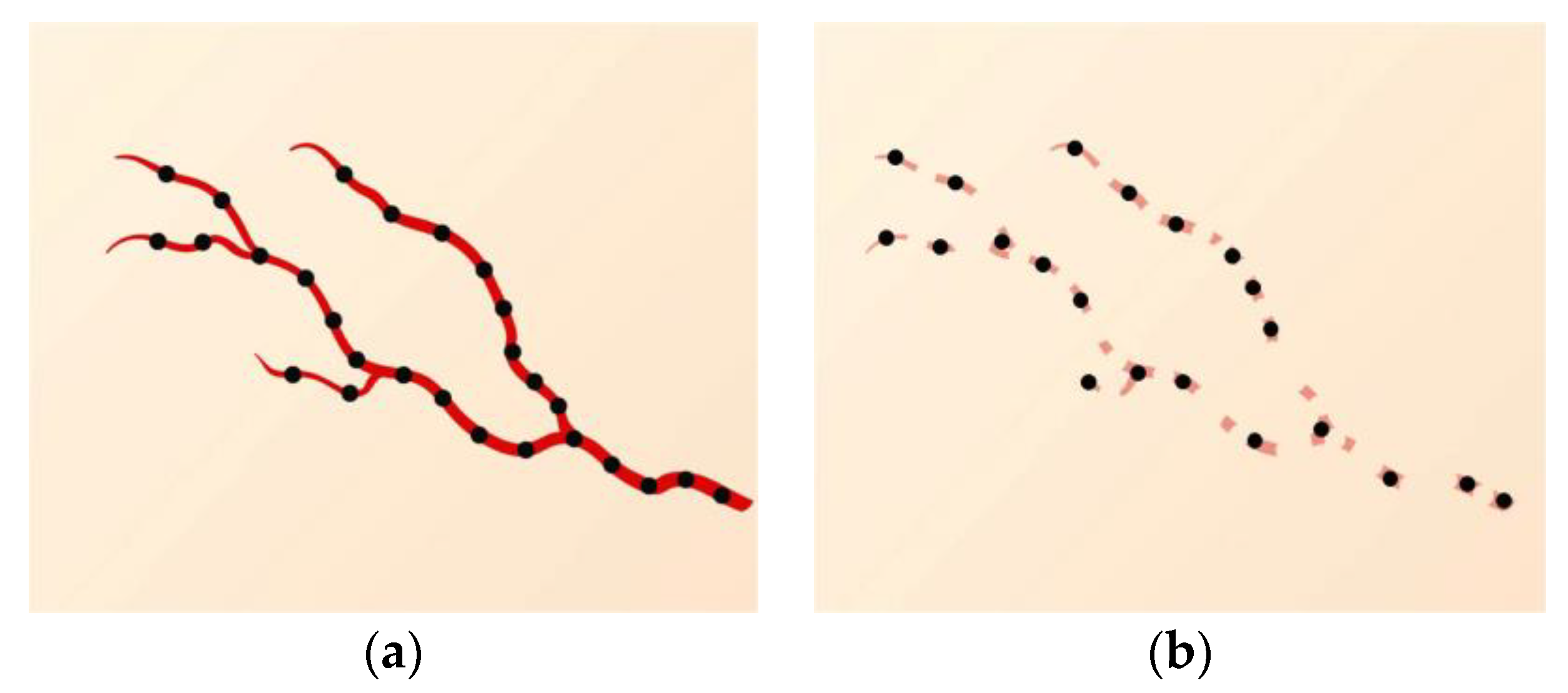
:1. Introduction
2. Materials and Methods
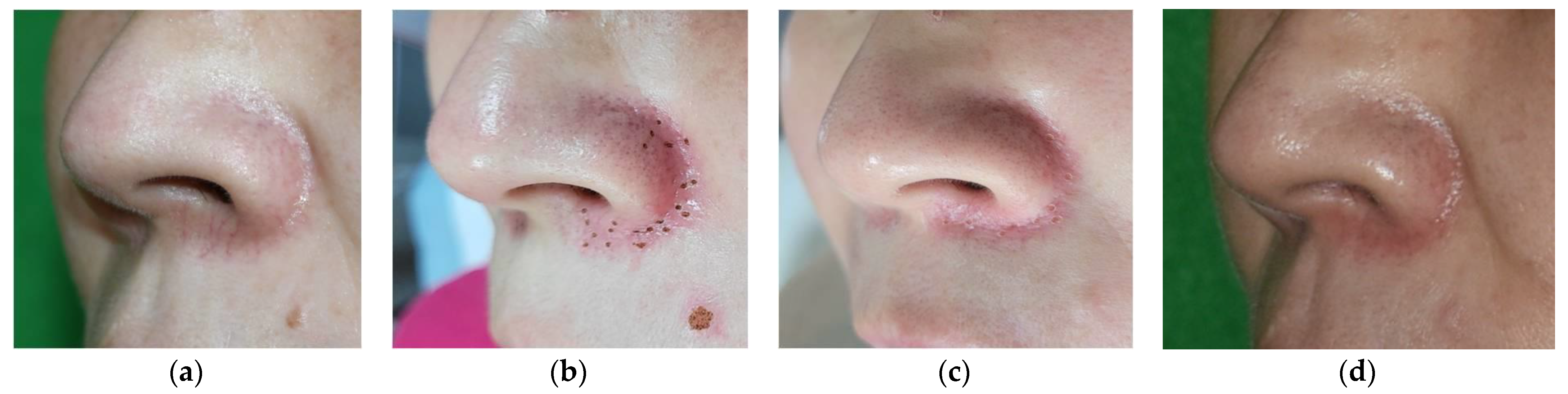
2.1. Patient Selection and Laser Methods
2.2. Outcome Assessment
2.3. Statistical Analysis
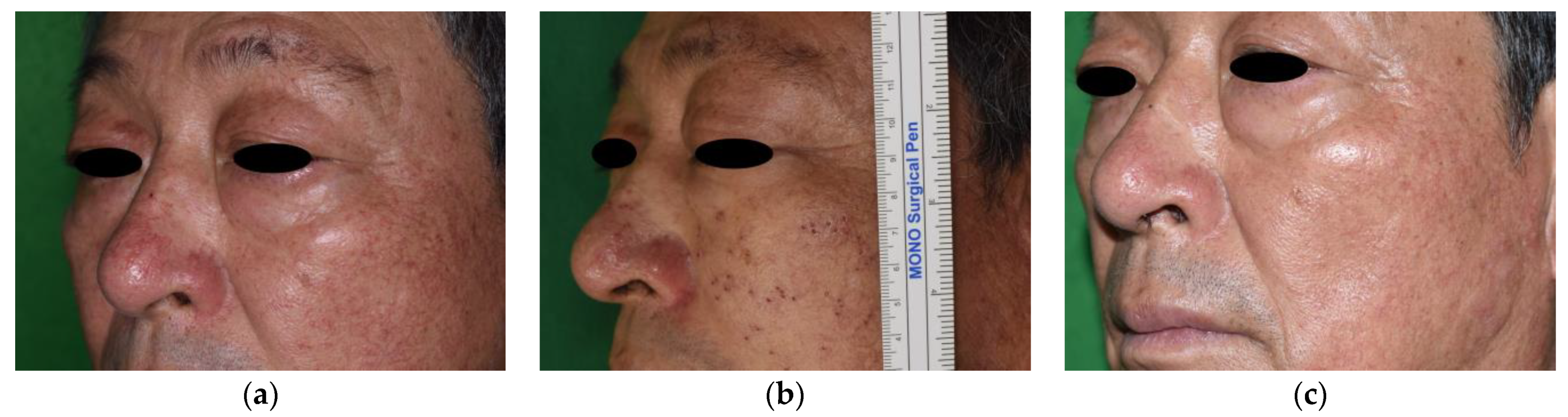
3. Results
3.1. Patients
3.2. Quantitative Evaluation (Objective)
3.3. The Patient and Observer Scar Assessment Scale (Subjective)
3.4. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gao, L.; Qu, H.; Gao, N.; Li, K.; Dang, E.; Tan, W.; Wang, G. A retrospective analysis for facial telangiectasia treatment using pulsed dye laser and intense pulsed light configured with different wavelength bands. J. Cosmet. Dermatol. 2020, 19, 88–92. [Google Scholar] [CrossRef]
- Mekic, S.; Hamer, M.A.; Wigmann, C.; Gunn, D.A.; Kayser, M.; Jacobs, L.C.; Schikowski, T.; Nijsten, T.; Pardo, L.M. Epidemiology and determinants of facial telangiectasia: A cross-sectional study. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 821–826. [Google Scholar] [CrossRef]
- Hare McCoppin, H.H.; Goldberg, D.J. Laser treatment of facial telangiectases: An update. Dermatol. Surg. 2010, 36, 1221–1230. [Google Scholar] [CrossRef]
- Lee, S.J.; No, Y.A.; Kang, J.M.; Chung, W.S.; Kim, Y.K.; Seo, S.J.; Park, K.Y. Treatment of hesitation marks on the forearm by the pinhole method. Lasers Med. Sci. 2016, 31, 1339–1342. [Google Scholar] [CrossRef] [PubMed]
- Andrews, R.H.; Dixon, R.G. Ambulatory Phlebectomy and Sclerotherapy as Tools for the Treatment of Varicose Veins and Telangiectasias. Semin. Interv. Radiol. 2021, 38, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Wittens, C.; Davies, A.H.; Bækgaard, N.; Broholm, R.; Cavezzi, A.; Chastanet, S.; de Wolf, M.; Eggen, C.; Giannoukas, A.; Gohel, M.; et al. Editor’s Choice—Management of Chronic Venous Disease: Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS). Eur. J. Vasc. Endovasc. Surg. 2015, 49, 678–737. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kauvar, A.N.; Khrom, T. Laser treatment of leg veins. Semin. Cutan. Med. Surg. 2005, 24, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Olivencia, J.A. Complications of ambulatory phlebectomy. Review of 1000 consecutive cases. Dermatol. Surg. 1997, 23, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Ramelet, A.A. Complications of ambulatory phlebectomy. Dermatol. Surg. 1997, 23, 947–954. [Google Scholar] [CrossRef] [Green Version]
- Bergan, J.J.; Weiss, R.A.; Goldman, M.P. Extensive tissue necrosis following high-concentration sclerotherapy for varicose veins. Dermatol. Surg. 2000, 26, 535–541, discussion 541–532. [Google Scholar] [CrossRef]
- Goldman, M.P.; Sadick, N.S.; Weiss, R.A. Cutaneous necrosis, telangiectatic matting, and hyperpigmentation following sclerotherapy. Etiology, prevention, and treatment. Dermatol. Surg. 1995, 21, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Davis, L.T.; Duffy, D.M. Determination of incidence and risk factors for postsclerotherapy telangiectatic matting of the lower extremity: A retrospective analysis. J. Dermatol. Surg. Oncol. 1990, 16, 327–330. [Google Scholar] [CrossRef] [PubMed]
- Guida, S.; Galimberti, M.G.; Bencini, M.; Pellacani, G.; Bencini, P.L. Telangiectasia of the face: Risk factors for reappearance in patients treated with dye laser. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 1355–1359. [Google Scholar] [CrossRef]
- Railan, D.; Parlette, E.C.; Uebelhoer, N.S.; Rohrer, T.E. Laser treatment of vascular lesions. Clin. Dermatol. 2006, 24, 8–15. [Google Scholar] [CrossRef]
- Chung, B.Y.; Han, S.S.; Moon, H.R.; Lee, M.W.; Chang, S.E. Treatment with the pinhole technique using erbium-doped yttrium aluminium garnet laser for a cafe au lait macule and carbon dioxide laser for facial telangiectasia. Ann. Dermatol. 2014, 26, 657–659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.H.; Park, H.Y.; Lee, W.S.; Kang, J.S. Sebaceous hyperplasia effectively improved by the pin-hole technique with squeezing. Ann. Dermatol. 2013, 25, 257–258. [Google Scholar] [CrossRef]
- Yang, J.H.; Han, S.S.; Won, C.H.; Chang, S.E.; Lee, M.W.; Choi, J.H.; Moon, K.C. Treatment of elastosis perforans serpiginosa with the pinhole method using a carbon dioxide laser. Dermatol. Surg. 2011, 37, 524–526. [Google Scholar] [CrossRef]
- Lee, S.J.; Cho, S.; Kim, Y.K.; Cho, S.B. Scar revision by the pinhole method using a 10,600-nm carbon dioxide laser. J. Cosmet. Laser Ther. 2013, 15, 37–38. [Google Scholar] [CrossRef]
- Lee, S.M.; Kim, Y.J.; Chang, S.E. Pinhole carbon dioxide laser treatment of secondary anetoderma associated with juvenile xanthogranuloma. Dermatol. Surg. 2012, 38, 1741–1743. [Google Scholar] [CrossRef]
- Fearmonti, R.; Bond, J.; Erdmann, D.; Levinson, H. A review of scar scales and scar measuring devices. Eplasty 2010, 10, e43. [Google Scholar]
- Draaijers, L.J.; Tempelman, F.R.; Botman, Y.A.; Tuinebreijer, W.E.; Middelkoop, E.; Kreis, R.W.; Van Zuijlen, P.P. The patient and observer scar assessment scale: A reliable and feasible tool for scar evaluation. Plast. Reconstr. Surg. 2004, 113, 1960–1965, discussion 1966–1967. [Google Scholar] [CrossRef]
- Cassuto, D.A.; Ancona, D.M.; Emanuelli, G. Treatment of facial telangiectasias with a diode-pumped Nd:YAG laser at 532 nm. J. Cutan. Laser Ther. 2000, 2, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Garden, J.M.; Bakus, A.D. Clinical efficacy of the pulsed dye laser in the treatment of vascular lesions. J. Dermatol. Surg. Oncol. 1993, 19, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.; Dover, J.S.; Arndt, K.A. Treatment of facial telangiectasia with variable-pulse high-fluence pulsed-dye laser: Comparison of efficacy with fluences immediately above and below the purpura threshold. Dermatol. Surg. 2003, 29, 681–684, discussion 685. [Google Scholar] [CrossRef]
- Kabnick, L.S.; Ombrellino, M. Ambulatory phlebectomy. Semin. Interv. Radiol. 2005, 22, 218–224. [Google Scholar] [CrossRef] [Green Version]
- Bowes, L.E.; Goldman, M.P. Sclerotherapy of reticular and telangiectatic veins of the face, hands, and chest. Dermatol. Surg. 2002, 28, 46–51. [Google Scholar] [PubMed]
- Goldman, M.P.; Bergan, J.J. Sclerotherapy: Treatment of Varicose and Telangiectatic Leg Veins, 4th ed.; Mosby/Elsevier: Philadelphia, PA, USA, 2007. [Google Scholar]
- Goldman, P.M. Polidocanol (aethoxysklerol) for sclerotherapy of superficial venules and telangiectasias. J. Dermatol. Surg. Oncol. 1989, 15, 204–209. [Google Scholar] [CrossRef]
- Anderson, R.R.; Parrish, J.A. Selective photothermolysis: Precise microsurgery by selective absorption of pulsed radiation. Science 1983, 220, 524–527. [Google Scholar] [CrossRef] [Green Version]
- Piccolo, D.; Crisman, G.; Kostaki, D.; Cannarozzo, G.; Sannino, M.; Chimenti, S. Rhodamine intense pulsed light versus conventional intense pulsed light for facial telangiectasias. J. Cosmet. Laser Ther. 2016, 18, 80–85. [Google Scholar] [CrossRef]

| Male (n = 35) | Female (n = 37) | Total (n = 72) | |
|---|---|---|---|
| Age (years) | 58.1 (23–78) | 44.2 (24–75) | 53.5 (23–78) |
| Lesions | 104 | 51 | 155 |
| Length (mm) | 12.3 ± 3.8 | 10.8 ± 2.0 | 11.8 ± 3.4 |
| Location n (%) | |||
| Forehead | 9 (8.7) | 6 (11.8) | 15 (9.7) |
| Glabella | 0 | 1 (2.0) | 1 (0.6) |
| Eyebrow | 1 (1.0) | 0 | 1 (0.6) |
| Eyelid | 2 (1.9) | 3 (5.9) | 5 |
| Temporal area | 3 (2.9) | 0 | 3 |
| Cheek | 32 (30.8) | 11(21.6) | 43 |
| Nose | 46 (44.2) | 22 (43.1) | 68 |
| Philtrum | 7 (6.7) | 1 (2.0) | 8 |
| Chin | 2 (1.9) | 4 (7.8) | 6 |
| Submandibular area | 2 (1.9) | 3 (5.9) | 5 |
| Length of Lesion (mm) | |||||
|---|---|---|---|---|---|
| 0 Month | 1 Month | 3 Months | 6 Months | p-Value * | |
| Total (n = 155) | 11.8 ± 3.4 | 5.7 ± 1.9 | 0.9 ± 1.0 | 0.2 ± 0.7 | <0.01 |
| Male (n = 104) | 12.3 ± 3.8 | 6.1 ± 0.9 | 0.6 ± 0.9 | 0.2 ± 0.5 | <0.01 |
| Female (n = 51) | 10.8 ± 2.0 | 5.0 ± 0.2 | 0.3 ± 0.7 | 0.1 ± 0.2 | <0.01 |
| FU patient (lesions) | 72 (155) | 72 (155) | 70 (152) | 65 (140) | |
| Scale Score | |||||
|---|---|---|---|---|---|
| 0 Month | 3 Months | 6 Months | p-Value * | ||
| OSAS | Vascularity | 6.6 ± 1.7 | 1.9 ± 0.8 | 1.3 ± 0.5 | <0.01 |
| Pigmentation | 6.6 ± 1.1 | 2.0 ± 0.9 | 1.4 ± 0.5 | <0.01 | |
| Thickness | 1.5 ± 0.5 | 1.0 ± 0 | 1.0 ± 0 | <0.01 | |
| Relief (irregularity) | 6.5 ± 1.2 | 1.5 ± 0.5 | 1.0 ± 0 | <0.01 | |
| Pliability | 2.1 ± 0.8 | 2.0 ± 0.8 | 2.0 ± 0.8 | 0.381 | |
| Surface area | 1.0 ± 0 | 1.0 ± 0 | 1.0 ± 0 | - | |
| Total score | 24.3 ± 2.5 | 9.4 ± 1.5 | 7.6 ± 0.9 | <0.01 | |
| PSAS | Pain | 1.5 ± 0.5 | 1.0 ± 0 | 1.0 ± 0 | <0.01 |
| Itchiness | 2.0 ± 0.9 | 1.0 ± 0 | 1.0 ± 0 | <0.01 | |
| Color difference | 8.4 ± 1.2 | 5.0 ± 0.8 | 1.5 ± 0.5 | <0.01 | |
| Stiffness | 1.4 ± 0.5 | 1.5 ± 0.5 | 1.4 ± 0.5 | - | |
| Thickness | 1.5 ± 0.5 | 1.5 ± 0.5 | 1.2 ± 0.4 | <0.01 | |
| Irregularity | 7.1 ± 0.8 | 4.0 ± 0.9 | 1.5 ± 0.5 | <0.01 | |
| Total score | 21.8 ± 1.9 | 14.0 ± 1.4 | 7.6 ± 0.9 | <0.01 | |
| POSAS | Total score | 46.1 ± 3.3 | 23.4 ± 2.8 | 15.2 ± 1.8 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Woo, S.S.; Gwak, H.; Han, S.S.; Suh, I.S.; Kim, S.H. Evaluation of the Pinhole Method Using Carbon Dioxide Laser on Facial Telangiectasia. J. Clin. Med. 2023, 12, 2849. https://doi.org/10.3390/jcm12082849
Woo SS, Gwak H, Han SS, Suh IS, Kim SH. Evaluation of the Pinhole Method Using Carbon Dioxide Laser on Facial Telangiectasia. Journal of Clinical Medicine. 2023; 12(8):2849. https://doi.org/10.3390/jcm12082849
Chicago/Turabian StyleWoo, Sang Seok, Hongki Gwak, Seung Seog Han, In Suck Suh, and Seong Hwan Kim. 2023. "Evaluation of the Pinhole Method Using Carbon Dioxide Laser on Facial Telangiectasia" Journal of Clinical Medicine 12, no. 8: 2849. https://doi.org/10.3390/jcm12082849






