Adolescents Hospitalized in an Acute Psychiatric Ward: The Difference between Males and Females in the Pre- and Pandemic/Post-Pandemic Periods
Abstract
:1. Introduction
1.1. The COVID-19 Pandemic and Adolescent Mental Health
1.2. Symptoms and Altered Behaviors in Adolescents during COVID-19
2. Materials and Methods
2.1. Study Procedure
2.2. Statistical Analysis
3. Results
- In total, 110 hospitalizations (45.6%) in the pre-pandemic period (1 July 2017–28 February 2020);
- In total, 131 hospitalizations (54.4%) in the post-pandemic period (1 March 2020–30 June 2023).
3.1. Adolescent Hospitalizations in the Pre- and Pandemic/Post-Pandemic Periods
- The mean age of adolescents was lower (15.63 ± 1.18) during the pandemic/post-pandemic period (Chi2 = 3.915, Kruskal–Wallis test, p = 0.0478);
- More adolescents treated at CANPS were hospitalized in the pandemic/post-pandemic period (SR = 4.52, p < 0.05), and more adolescents without any previous psychiatric treatment were hospitalized in the pre-pandemic (SR = 4.38, p < 0.05) (Pearson Chi2 = 21.21, p = 0.000; Fisher’s exact = 0.000);
- More adolescents used substances in the pandemic/post pandemic period in comparison with the previous period (Pearson Chi2 = 5.36, p = 0.005), especially cannabis.
- Among clinical reasons for hospitalizations, substance intoxications were more frequently recorded in the pre-pandemic period (SR = 2.67, p < 0.05);
- Among the psychiatric diagnoses at discharge, we observed the prevalence of adjustment reactions (SR = 3.57, p < 0.05) and conduct disorder (SR = 2.08, p < 0.05) in the pre-pandemic period, whereas depressive disorders (SR = 3.77, p < 0.05) and emotional disorders (SR = 4.03, p < 0.05) were prevalent in the pandemic/post-pandemic period;
- The HoNOSCA score statistically significantly differed between the two periods, with a decrease in the pandemic/post-pandemic period.
3.2. Male and Female Adolescent Hospitalizations
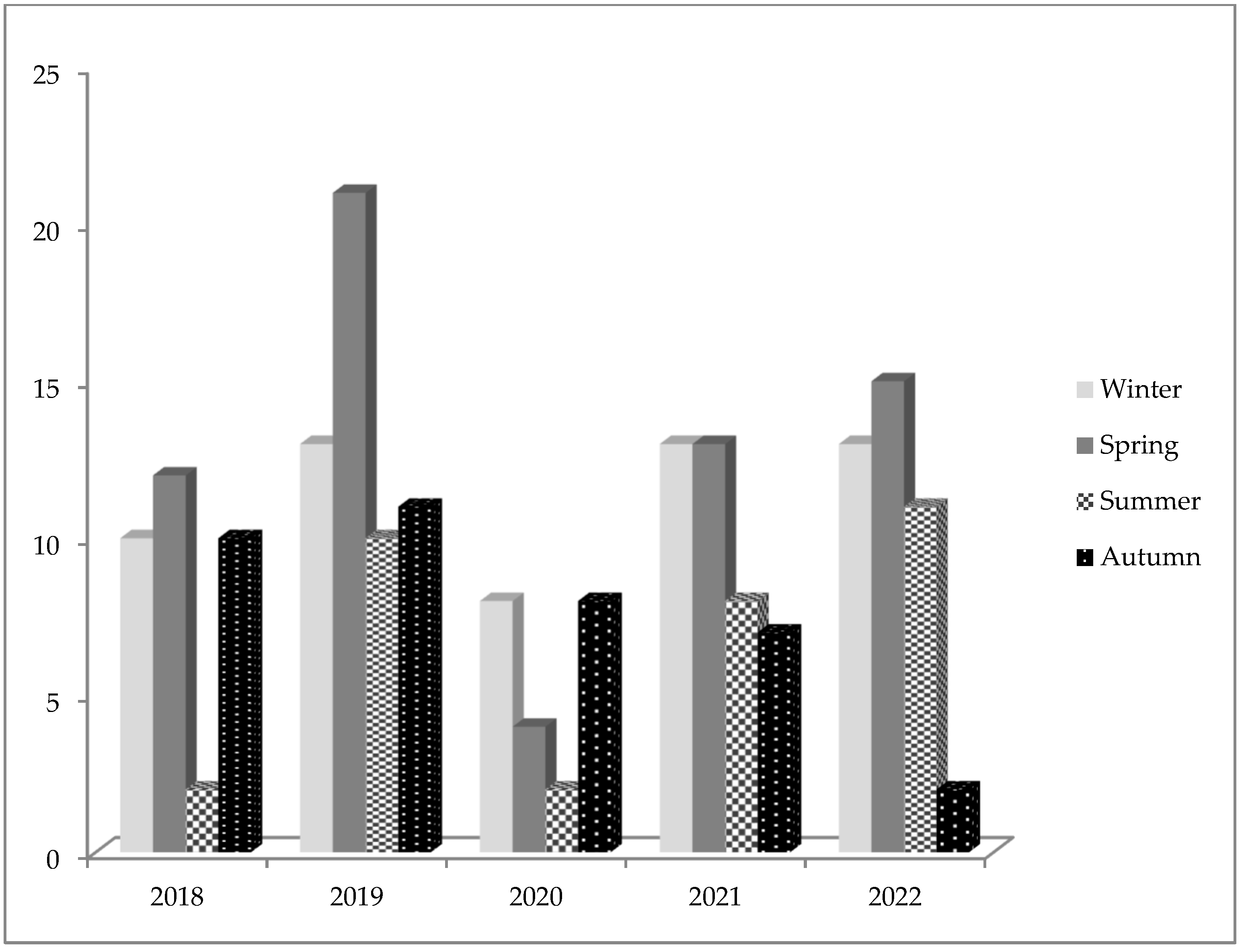
3.3. Seasonality of Hospitalizations
3.4. Multivariate Linear Regression
- The pandemic/post-pandemic period (Coeff. = −2.50, 95% Conf. Int. −4.09; −0.91; p = 0.002);
- Period of previous psychiatric treatments (Coeff. = −0.39, 95% Conf. Int. 0.18; 0.60; p = 0.000);
- Female sex (Coeff. = −2.77, 95% Conf. Int. −4.33; −1.21; p = 0.00).
4. Discussion
Limitations and Advantages of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Italian Society of Child Neuropsychiatry (Società Italiana di Neuropsichiatria dell’Infanzia e dell’Adolescenza—SINPIA). Available online: https://sinpia.eu/wp-content/uploads/2022/04/04_SINPIA_Comunicato-Vaccini-Minori-con-Fragilita%CC%80_03.02.2022.pdf (accessed on 22 June 2024).
- World Health Organization. Coping through Crisis: COVID-19 Pandemic Experiences and Adolescent Mental Health and Well-Being in the WHO European Region. 2023. Available online: https://www.who.int/europe/publications/i/item/WHO-EURO-2023-7680-47447-69735 (accessed on 22 June 2024).
- Devoe, D.J.; Han, A.; Anderson, A.; Katzman, D.K.; Patten, S.B.; Soumbasis, A.; Flanagan, J.; Paslakis, G.; Vyver, E.; Marcoux, G.; et al. The impact of the COVID-19 pandemic on eating disorders: A systematic review. Int. J. Eating Disord. 2022, 56, 5–25. [Google Scholar] [CrossRef] [PubMed]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J. Am. Acad. Child. Adolesc. Psychiatry 2020, 59, 1218–1239.e3. [Google Scholar] [CrossRef] [PubMed]
- Khamesan, B.; Khatibzade-Nasari, N.; Zare, S.; Rostami-Gooran, N.; Baghestani-Koozehgar, R. Long-term effects of the COVID-19 lockdown on weight status, eating habits, and lifestyle changes related to school-aged children in Bandar Abbas, Iran. BMC Public Health 2024, 24, 1981. [Google Scholar] [CrossRef]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020, 291, 113264. [Google Scholar] [CrossRef] [PubMed]
- Samji, H.; Wu, J.; Ladak, A.; Vossen, C.; Stewart, E.; Dove, N.; Long, D.; Snell, G. Review: Mental health impacts of the COVID-19 pandemic on children and youth—A systematic review. Child Adolesc. Ment. Health 2022, 27, 173–189. [Google Scholar] [CrossRef]
- Stanley, M. A Return to “Normal” Assessing Mental Health Concerns Among U.S. Teens. 2021. Available online: https://www.morganstanley.com/assets/pdfs/reemergence-program-teen-survey-factsheet.pdf (accessed on 22 June 2024).
- Liu, J.J.; Bao, Y.; Huang, X.; Shi, J.; Lu, L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc. Health 2020, 4, 347–349. [Google Scholar] [CrossRef] [PubMed]
- Rankin, K.; Sweeny, K.; Xu, S. Associations between subjective time perception and well-being during stressful waiting periods. Stress Health 2019, 35, 549–559. [Google Scholar] [CrossRef] [PubMed]
- Pawluk, E.J.; Koerner, N. The relationship between negative urgency and generalized anxiety disorder symptoms: The role of intolerance of negative emotions and intolerance of uncertainty. Anxiety Stress Coping 2016, 29, 606–615. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.J.; Zhang, L.G.; Wang, L.L.; Guo, Z.C.; Wang, J.Q.; Chen, J.C.; Liu, M.; Chen, X.; Chen, J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- Mensi, M.M.; Capone, L.; Rogantini, C.; Orlandi, M.; Ballante, E.; Borgatti, R. COVID-19-related psychiatric impact on Italian adolescent population: A cross-sectional cohort study. J. Community Psychol. 2021, 49, 1457–1469. [Google Scholar] [CrossRef]
- Saulle, R.; De Sario, M.; Bena, A.; Capra, P.; Culasso, M.; Davoli, M.; De Lorenzo, A.; Lattke, L.S.; Marra, M.; Mitrova, Z.; et al. School closures and mental health, wellbeing and health behaviours among children and adolescents during the second COVID-19 wave: A systematic review of the literature. Epidemiol. Prev. 2022, 46, 333–352. [Google Scholar] [CrossRef]
- Oliveira, J.M.D.; Butini, L.; Pauletto, P.; Lehmkuhl, K.M.; Stefani, C.M.; Bolan, M.; Guerra, E.; Dick, B.; De Luca Canto, G.; Massignan, C. Mental health effects prevalence in children and adolescents during the COVID-19 pandemic: A systematic review. Worldviews Evid Based Nurs. 2022, 12, 130–137. [Google Scholar] [CrossRef] [PubMed]
- De Luca, L.; Giletta, M.; Nocentini, A.; Menesini, E. Non-Suicidal Self-Injury in Adolescence: The Role of Pre-Existing Vulnerabilities and COVID-19-Related Stress. J. Youth Adolesc. 2022, 51, 2383–2395. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 2021, 5, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Bacaro, V.; Meneo, D.; Curati, S.; Buonanno, C.; De Bartolo, P.; Riemann, D.; Mancini, F.; Martoni, M.; Baglioni, C. The impact of COVID-19 on Italian adolescents’ sleep and its association with psychological factors. J. Sleep Res. 2022, 31, e13689. [Google Scholar] [CrossRef]
- Salfi, F.; Lauriola, M.; D’Atri, A.; Amicucci, G.; Viselli, L.; Tempesta, D.; Ferrara, M. Demographic, psychological, chronobiological, and work-related predictors of sleep disturbances during the COVID-19 lockdown in Italy. Sci. Rep. 2021, 11, 11416. [Google Scholar] [CrossRef] [PubMed]
- Nobari, H.; Fashi, M.; Eskandari, A.; Villafaina, S.; Murillo-Garcia, Á.; Pérez-Gómez, J. Effect of COVID-19 on Health-Related Quality of Life in Adolescents and Children: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4563. [Google Scholar] [CrossRef]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19: A Meta-analysis. JAMA Pediatr. 2021, 175, 1142–1150. [Google Scholar] [CrossRef]
- Barbieri, V.; Wiedermann, C.J.; Kaman, A.; Erhart, M.; Piccoliori, G.; Plagg, B.; Mahlknecht, A.; Ausserhofer, D.; Engl, A.; Ravens-Sieberer, U. Quality of Life and Mental Health in Children and Adolescents after the First Year of the COVID-19 Pandemic: A Large Population-Based Survey in South Tyrol, Italy. Int. J. Environ. Res. Public Health 2022, 19, 5220. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Erhart, M.; Devine, J.; Gilbert, M.; Reiss, F.; Barkmann, C.; Siegel, N.A.; Simon, A.M.; Hurrelmann, K.; Schlack, R.; et al. Child and Adolescent Mental Health During the COVID-19 Pandemic: Results of the Three-Wave Longitudinal COPSY Study. J. Adolesc. Health 2022, 71, 570–578. [Google Scholar] [CrossRef]
- Nikolaidis, A.; DeRosa, J.; Kass, M.; Droney, I.; Alexander, L.; Di Martino, A.; Bromet, E.; Merikangas, K.; Milham, M.P.; Paksarian, D. Heterogeneity in COVID-19 pandemic-induced lifestyle stressors predicts future mental health in adults and children in the US and UK. J. Psychiatr. Res. 2022, 147, 291–300. [Google Scholar] [CrossRef]
- Di Lorenzo, R.; Cimino, N.; Di Pietro, E.; Pollutri, G.; Neviani, V.; Ferri, P. A 5-year retrospective study of demographic, anamnestic, and clinical factors related to psychiatric hospitalizations of adolescent patients. Neuropsychiatr. Dis. Treat. 2016, 12, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Davico, C.; Marcotulli, D. Impact of the COVID-19 Pandemic on Child and Adolescent Psychiatric Emergencies. J. Clin. Psychiatry 2021, 82, 20m13467. [Google Scholar] [CrossRef]
- Mercader Rubio, I.; Sánchez-López, P. Psychological Consequences of Fear of COVID-19: Symptom Analysis of Triggered Anxiety and Depression Disorders in Adolescents and Young Adults. Int. J. Environ. Res. Public Health 2022, 19, 14171. [Google Scholar] [CrossRef] [PubMed]
- Di Lorenzo, R.; Pinelli, M.; Bertani, D.; Cutino, A.; Dragone, D.; Elia, C.; Farina, R.; Fiore, G.; Luisi, F.; Panico, S.; et al. The Impact of COVID-19 Pandemic on Psychiatric Emergencies in Two Different Settings: Emergency Room and Community Mental Health Service. Front. Psychiatry 2022, 13, 894939. [Google Scholar] [CrossRef] [PubMed]
- Richard, V.; Dumont, R.; Lorthe, E.; Loizeau, A.; Baysson, H.; Zaballa, M.E.; Pennacchio, F.; Barbe, R.P.; Posfay-Barbe, K.M.; Guessous, I.; et al. Impact of the COVID-19 pandemic on children and adolescents: Determinants and association with quality of life and mental health-a cross-sectional study. Child Adolesc. Psychiatry Ment. Health 2023, 17, 17. [Google Scholar] [CrossRef] [PubMed]
- Di Lorenzo, R.; Frattini, N.; Dragone, D.; Farina, R.; Luisi, F.; Ferrari, S.; Bandiera, G.; Rovesti, S.; Ferri, P. Psychiatric Emergencies During the COVID-19 Pandemic: A 6-Month Observational Study. Neuropsychiatr. Dis. Treat. 2021, 17, 1763–1778. [Google Scholar] [CrossRef]
- Youngminds. Coronavirus: Impact on Young People with Mental Health Needs. 2020. Available online: https://www.youngminds.org.uk/media/xq2dnc0d/youngminds-coronavirus-report-march2020.pdf (accessed on 23 June 2024).
- Hill, J.; Inder, T.; Neil, J.; Dierker, D.; Harwell, J.; Van Essen, D. Similar patterns of cortical expansion during human development and evolution. Proc. Natl. Acad. Sci. USA 2010, 107, 13135–13140. [Google Scholar] [CrossRef]
- Tang, Y.; Kirk, B. Cannabis use among adolescents and young adults during the COVID-19 pandemic: A systematic review. Drug Alcohol Depend. Rep. 2024, 11, 100232. [Google Scholar] [CrossRef]
- Dumas, T.M.; Ellis, W. What Does Adolescent Substance Use Look Like During the COVID-19 Pandemic? Examining Changes in Frequency, Social Contexts, and Pandemic-Related Predictors. J. Adolesc. Health 2020, 67, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Nadeem, E.; Van Meter, A.R. The Impact of the COVID-19 Pandemic on Adolescents: An Opportunity to Build Resilient Systems. Am. J. Health Promot. 2023, 37, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Evensen, M.; Hart, R.K.; Godøy, A.A.; Hauge, L.J.; Lund, I.O.; Knudsen, A.K.S.; Grøtting, M.W.; Surén, P.; Reneflot, A. Impact of the COVID-19 pandemic on mental healthcare consultations among children and adolescents in Norway: A nationwide registry study. Eur. Child. Adolesc. Psychiatry 2023, 32, 1025–1035. [Google Scholar] [CrossRef] [PubMed]
- Rocchi, M.B.; Sisti, D.; Cascio, M.T.; Preti, A. Seasonality and suicide in Italy: Amplitude is positively related to suicide rates. J. Affect. Disord. 2007, 100, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Krause, T.M.; Lane, S.D. Trends and Seasonality of Emergency Department Visits and Hospitalizations for Suicidality Among Children and Adolescents in the US from 2016 to 2021. JAMA Netw Open 2023, 6, e2324183. [Google Scholar] [CrossRef] [PubMed]
- Gracia, R.; Pamias, M.; Mortier, P.; Alonso, J.; Pérez, V.; Palao, D. Is the COVID-19 pandemic a risk factor for suicide attempts in adolescent girls? J. Affect. Disord. 2021, 292, 139–141. [Google Scholar] [CrossRef] [PubMed]
- Thorvaldsen, S.; Hansen, K.T.; Forsbergm, J.T. Children and adolescents weathering the storm: Resilience in the presence of bullying victimization, harassment, and pandemic lockdown in northern Norway. Scand. J. Psychol. 2024, 65, 735–746. [Google Scholar] [CrossRef] [PubMed]
- Akın, A.; Sarrar, L. Understanding Adolescent Mental Health in the COVID-19 Era: A Psychodynamic Approach. Children 2024, 11, 772. [Google Scholar] [CrossRef]
- Sprang, G.; Silman, M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013, 7, 105–110. [Google Scholar] [CrossRef]
- Cama, S.F.; Miyamoto, B.E.; DeJong, S.M. Impact on Child Psychiatry. Psychiatr. Clin. N. Am. 2022, 45, 133–146. [Google Scholar] [CrossRef]
- Carosella, K.A.; Wiglesworth, A.; Silamongkol, T.; Tavares, N.; Falke, C.A.; Fiecas, M.B.; Klimes-Dougan, B. Non-suicidal Self-Injury in the Context of COVID-19: The Importance of Psychosocial Factors for Female Adolescents. J. Affect. Disord. Rep. 2021, 4, 100137. [Google Scholar] [CrossRef]
- Mental Health of Adolescents in Italy, Child Neuropsychiatrists (SINPIA): “Acts of Self-Harm on the Rise”. Available online: https://sinpia.eu/wp-content/uploads/2023/09/CS_SINPIA_Giornata-Mondiale-Prevenzione-Suicidio-DEF1.pdf (accessed on 23 June 2024).
- Pompili, M.; Vichi, M.; Innamorati, M.; Lester, D.; Yang, B.; De Leo, D.; Girardi, P. Suicide in Italy during a time of economic recession: Some recent data related to age and gender based on a nationwide register study. Health Soc. Care Community 2014, 22, 361–367. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Suicide Prevention. Available online: https://www.who.int/health-topics/suicide#tab=tab_1 (accessed on 23 June 2024).



| Variables, n (%) | Pre-Pandemic Period n = 110 (45.6) | Pandemic/Post-Pandemic Period n = 131 (54.4) | Total n = 241 | Statistical Test Probability |
|---|---|---|---|---|
| Sex, n (%) | ||||
| male | 61 (56.0) * | 49 (37.1) | 110 | Pearson Chi2 = 8.54 p = 0.003 * SR > 2, p < 0.05 |
| female | 48 (44.0) | 83 (62.9) * | 131 | |
| Age (years), m ± DS | 15.94 ± 1.01 | 15.63 ± 1.18 | 15.77 ± 1.14 | Chi2 = 3.915 Kruskal–Wallis test, p = 0.0478 |
| Previous Psychiatric Treatments, n (%) | ||||
| CANPS | 67 (60.9) | 114 (87.0) * | 181 (75.1) | Pearson Chi2 = 21.21 p = 0.000 * SR > 2, p < 0.05 Fisher’s exact = 0.000 |
| Private psychiatrist | 2 (1.8) | 2 (1.5) | 4 (1.7) | |
| Other or more services | 5 (4.5) | 3 (2.3) | 8 (3.3) | |
| No previous psychiatric treatment | 34 (30.9) * | 12 (9.2) | 46 (19.1) | |
| PREVIOUS HOSPITALIZATIONS IN SPDC, n (%) | ||||
| Present | 60 (55.0) | 60 (45.5) | 120 (49.8) | Pearson Chi2 = 1.83 p = 0.176 |
| Absent | 49 (45.0) | 72 (54.5) | 121 (50.2) | |
| Previous Psychiatric Treatment Period (year), m ± DS | 2.95 ± 3.70 | 3.46 ± 4.40 | 3.18 ± 4.03 | Chi2 = 0.113 Kruskal–Wallis test, p = 0.7365 |
| Hospitalization Regime, n (%) | ||||
| Voluntary | 107 (98.2) | 129 (97.7) | 236 (97.9) | Pearson Chi2 = 0.4242 p = 0.515 |
| Involuntary | 3 (1.8) | 3 (2.7) | 5 (2.1) | |
| Substance Use, n (%) | ||||
| Present | 83 (76.1) | 115 (87.1) * | 197 (81.7) | Pearson Chi2 = 5.36 p = 0.005 * SR > 2, p < 0.05 |
| Absent | 26 (23.9) * | 17 (12.9) | 44 (18.3) | |
| Treatment Adherence, n (%) | ||||
| Sufficient | 56 (51.4) | 84 (63.6) | 140 (58.1) | Pearson Chi2 = 0.21 p = 0.900 |
| Insufficient | 53 (48.6) | 48 (36.4) | 101 (41.9) | |
| Variables, n (%) | Pre-Pandemic Period n = 110 (45.6) | Pandemic/Post-Pandemic Period n = 131 (54.4) | Total n = 241 | Statistical Test Probability |
|---|---|---|---|---|
| Clinical Reason for Hospitalization, n (%) | ||||
| Suicidal risk/suicidal behavior | 53 (48.2) | 71 (54.2) | 124 (51.5) | Pearson Chi2 = 25.78 p = 0.007 Fisher’s exact = 0.002 * SR > 2, p < 0.05 |
| Acute psychosis symptoms | 11 (10.0) | 17 (13.0) | 28 (11.6) | |
| Depressive symptoms | 1 (0.9) | 5 (3.8) | 6 (2.5) | |
| Acute anxiety symptoms | 7 (6.4) | 2 (1.5) | 9 (3.7) | |
| Aggressive behavior | 20 (18.2) | 34 (25.0) | 54 (22.4) | |
| Environmental maladjustment conditions | 1 (0.9) | 0 | 1 (0.4) | |
| Substance intoxication | 8 (7.3) * | 1 (0.8) | 9 (3.7) | |
| Runaway from home or community | 3 (2.7) | 0 | 3 (1.2) | |
| Other symptoms or psychiatric illness conditions | 6 (5.5) | 1 (0.8) | 7 (2.9) | |
| Psychiatric Diagnosis at Discharge, n (%) | ||||
| Schizophrenia spectrum disorders | 12 (10.9) | 25 (19.1) | 37 (15.4) | Pearson Chi2 = 50.88 p = 0.000 * SR > 2, p < 0.05 |
| Depressive disorders | 4 (3.6) | 25 (19.1) * | 29 (12) | |
| Anxiety disorders | 5 (4.5) | 4 (3.1) | 9 (3.7) | |
| Personality disorders | 11 (10.0) | 13 (9.9) | 24 (10.0) | |
| Eating disorders | 1 (0.9) | 0 | 1 (04) | |
| Substance use disorders | 5 (4.5) | 6 (4.6) | 11 (4.6) | |
| Acute reaction to stress | 5 (4.5) | 6 (4.6) | 11 (4.6) | |
| Adaptation reaction | 30 (27.3) * | 11 (8.4) | 41 (17.0) | |
| Conduct disorder | 20 (18.2) * | 12 (9.2) | 32 (13.3) | |
| Emotional disorders | 0 | 18 (13.7) * | 18 (7.5) | |
| Autism | 8 (7.3) | 6 (4.6) | 14 (5.8) | |
| Intellectual dysfunction | 3 (2.7) | 3 (2.3) | 6 (2.5) | |
| Substance-induced Psychosis | 6 (5.5) | 2 (1.5) | 8 (3.3) | |
| Hospitalizations’ Duration (days), m ± DS | 10.86 ± 17.04 | 7.92 ± 7.90 | 9.26 ± 12.95 | Chi2 = 0.436 Kruskal–Wallis test, p = 0.5092 |
| HoNOSCA score, m ± DS | 25.27 ± 5.10 | 21.84 ± 6.81 | 23.49 ± 6.28 | Chi2 = 17.482 Kruskal–Wallis test, p = 0.0001 |
| Variables, n (%) | Male n = 109 (45.2) | Female n = 132 (54.8) | Total n = 241 | Statistical Test Probability |
|---|---|---|---|---|
| Age (years), m ± DS | 15.81 ± 1.21 | 15.75 ± 1.08 | 15.77 ± 1.14 | Chi2 = 0.426 Kruskal–Wallis test, p = 0.5138 |
| Hospitalization Regime, n (%) | ||||
| Voluntary | 106 (44.9) | 130 (55.1) | 236 | Pearson Chi2 = 0.45 p = 0.502 |
| Involuntary | 3 (60.0) | 2 (40.0) | 5 | |
| Substance Use, n (%) | ||||
| Present | 30 (68.2) | 14 (31.8) | 44 | Pearson Chi2 = 11.45 p = 0.001 |
| Absent | 79 (40.1) | 118 (59.9) | 197 | |
| Treatment Adherence, n (%) | ||||
| Sufficient | 57 (40.7) | 83 (59.3) | 140 | Pearson Chi2 = 2.77 p = 0.250 |
| Insufficient | 52 (51.5) | 49 (48.5) | 101 | |
| Hospitalizations’ Duration (days), m ± DS | 9.31 ± 12.22 | 9.22 ± 13.58 | 9.26 ± 12.95 | Chi2 = 0.534 Kruskal–Wallis test, p = 0.4651 |
| HoNOSCA score, m ± DS | 25.55 ± 5.77 | 21.39 ± 6.23 | 23.27 ± 6.36 | t = 5.34, t-test p = 0.0000 |
| Variables, n (%) | Pre-Pandemic Period n = 61 (56) | Pandemic/Post-Pandemic Period n = 48 (44) | Total n = 109 | Statistical Test Probability |
|---|---|---|---|---|
| Clinical Reason for Hospitalization, n (%) | ||||
| Suicidal risk/suicidal behavior | 22 (36.1) | 10 (20.8) | 32 (29.4) | Pearson Chi2 = 19.76 p = 0.011 * SR > 2, p < 0.05 Fisher’s exact = 0.002 |
| Acute psychosis symptoms | 8 (13.1) | 7 (14.6) | 15 (13.8) | |
| Depressive symptoms | 1 (1.6) | 2 (4.2) | 3 (2.8) | |
| Aggressive behavior | 17 (27.9) | 29 (60.4) * | 46 (42.2) | |
| Environmental maladjustment conditions | 1 (1.6) | 0 | 1 (0.9) | |
| Substance intoxication | 7 (11.5) * | 0 | 7 (6.4) | |
| Run away from home or community | 2 (3.3) | 0 | 2 (1.8) | |
| Other symptoms or psychiatric illness conditions | 3 (4.9) | 0 | 3 (2.8) | |
| Psychiatric Diagnosis at Discharge, n (%) | ||||
| Schizophrenia spectrum disorders | 7 (11.5) | 22 (45.8) * | 29 (26.6) | Pearson Chi2 = 39.26 p = 0.000 * SR > 2, p < 0.05 Fisher’s exact = 0.000 |
| Depressive disorders | 2 (3.3) | 5 (10.4) | 7 (6.4) | |
| Anxiety disorders | 2 (3.2) | 2 (4.2) | 4 (3.7) | |
| Personality disorders | 5 (8.2) | 4 (8.3) | 9 (8.3) | |
| Eating disorders | 1 (1.6) | 0 | 1 (0.9) | |
| Substance use disorders | 3 (4.9) | 0 (10.9) | 3 (2.8) | |
| Adjustment reaction | 14 (23) * | 1 (2.1) | 15 (13.8) | |
| Conduct disorders | 13 (21.3) | 4 (8.3) | 17 (16.6) | |
| Emotional disorders | 0 | 5 (10.4) * | 5 (4.6) | |
| Autism | 6 (9.8) | 4 (8.3) | 10 (9.2) | |
| Intellective dysfunction | 3 (4.9) | 0 | 3 (2.8) | |
| Substance-induced psychosis | 5 (8.2) | 1 (2.1) | 6 (5.5) | |
| Variables, n (%) | Pre-Pandemic Period n = 49 (36.8) | Pandemic/Post-Pandemic Period n = 84 (63.2) | Total n = 133 | Statistical Test Probability |
|---|---|---|---|---|
| Clinical Reason for Hospitalization, n (%) | ||||
| Suicidal risk/suicidal behavior | 31 (63.3) | 62 (73.8) | 92 (69.9) | Pearson Chi2 = 15.22 p = 0.055 * SR > 2, p < 0.05 Fisher’s exact = 0.028 |
| Acute psychosis symptoms | 3 (6.1) | 10 (11.9) | 13 (9.8) | |
| Depressive symptoms | 0 | 3 (3.6) | 3 (2.3) | |
| Acute anxiety symptoms | 7 (14.3) * | 2 (2.4) | 9 (6.8) | |
| Aggressive behavior | 3 (6.1) | 5 (6.0) | 8 (6.0) | |
| Environmental maladjustment conditions | 1 (2.0) | 1 (1.2) | 2 (1.5) | |
| Substance intoxication | 1 (2.0) | 0 | 1 (0.8) | |
| Runaway from home or community | 2 (4.1) | 0 | 2 (1.5) | |
| Other symptoms or psychiatric illness conditions | 1 (2.0) | 1 (1.2) | 2 (1.5) | |
| Psychiatric diagnosis At discharge, n (%) | ||||
| Schizophrenia spectrum disorders | 5 (10.2) | 3 (3.6) | 8 (6.0) | Pearson Chi2 = 28.50 p = 0.001 * SR > 2, p < 0.05 Fisher’s exact = 0.000 |
| Depressive disorders | 2 (4.1) | 21 (25.0) * | 23 (17.3) | |
| Anxiety disorders | 3 (6.1) | 2 (2.4) | 5 (3.8) | |
| Personality disorders | 6 (12.2) | 9 (10.7) | 15 (11.3) | |
| Eating disorders | 2 (4.1) | 6 (7.1) | 8 (6.0) | |
| Adjustment reaction | 21 (42.9) * | 16 (19.0) | 37 (27.8) | |
| Conduct disorders | 7 (14.3) | 8 (9.5) | 15 (11.3) | |
| Emotional disorders | 0 | 13 (15.5) * | 13 (9.8) | |
| Autism | 2 (4.1) | 2 (2.4) | 4 (3.0) | |
| Intellective dysfunction | 0 | 3 (3.6) | 3 (2.3) | |
| Substance-induced psychosis | 1 (2.0) | 1 (1.2) | 2 (1.5) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Lorenzo, R.; Bonasegla, P.; Bardelli Canzio, A.; Morgante, M.; Rovesti, S.; Ferri, P. Adolescents Hospitalized in an Acute Psychiatric Ward: The Difference between Males and Females in the Pre- and Pandemic/Post-Pandemic Periods. J. Clin. Med. 2024, 13, 4658. https://doi.org/10.3390/jcm13164658
Di Lorenzo R, Bonasegla P, Bardelli Canzio A, Morgante M, Rovesti S, Ferri P. Adolescents Hospitalized in an Acute Psychiatric Ward: The Difference between Males and Females in the Pre- and Pandemic/Post-Pandemic Periods. Journal of Clinical Medicine. 2024; 13(16):4658. https://doi.org/10.3390/jcm13164658
Chicago/Turabian StyleDi Lorenzo, Rosaria, Pietro Bonasegla, Alice Bardelli Canzio, Martina Morgante, Sergio Rovesti, and Paola Ferri. 2024. "Adolescents Hospitalized in an Acute Psychiatric Ward: The Difference between Males and Females in the Pre- and Pandemic/Post-Pandemic Periods" Journal of Clinical Medicine 13, no. 16: 4658. https://doi.org/10.3390/jcm13164658





