Evaluating the Protective Role of Vitamin A Supplementation in Periodontal Health: A Comprehensive Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria and Information Sources
2.2. Search Strategy
2.3. Data Collection and Selection Process
2.4. Data Items
2.5. Risk of Bias and Quality Assessment
2.6. Synthesis Methods
3. Results
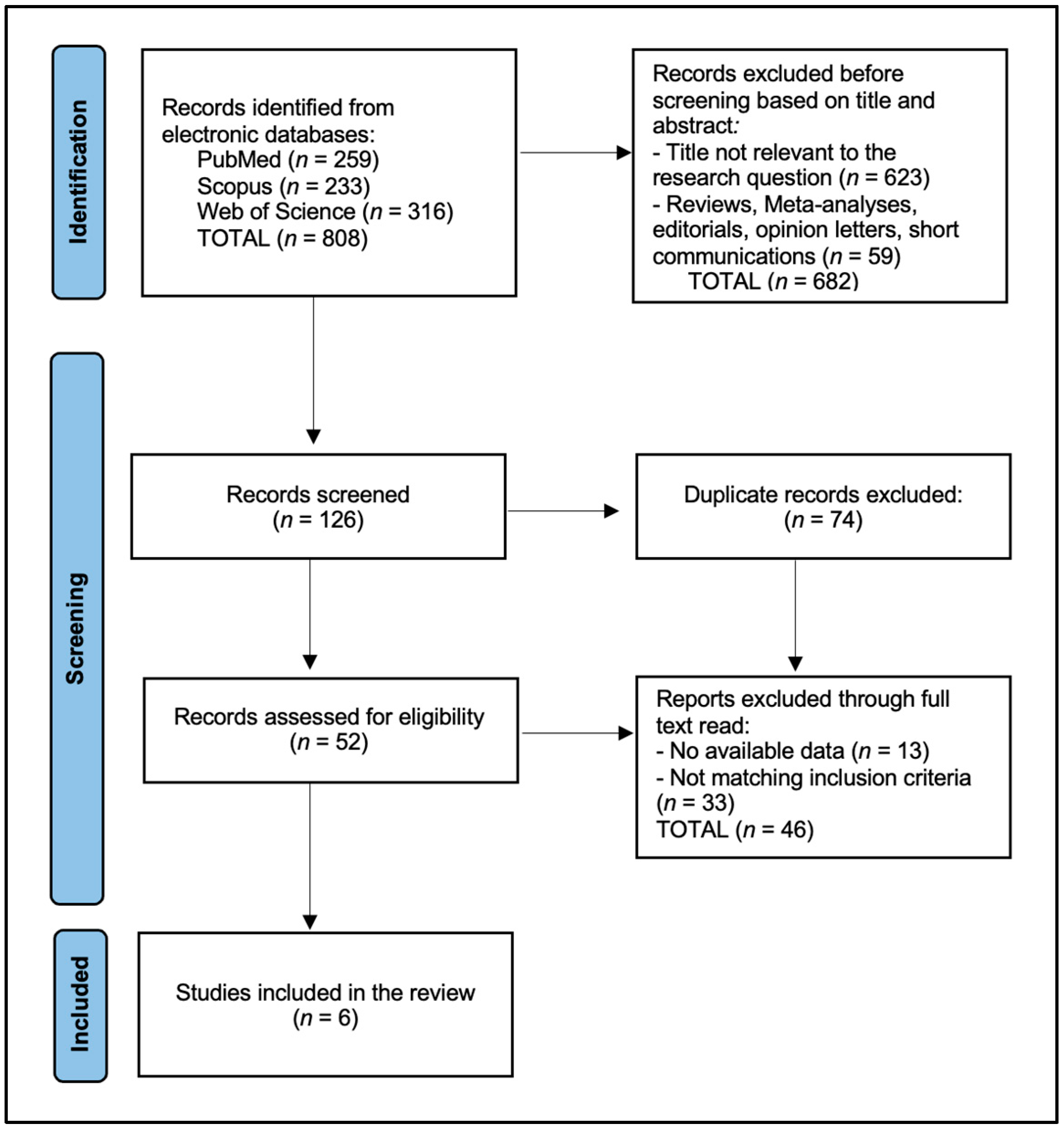
3.1. Study Selection and Study Characteristics
3.2. Results of Individual Studies
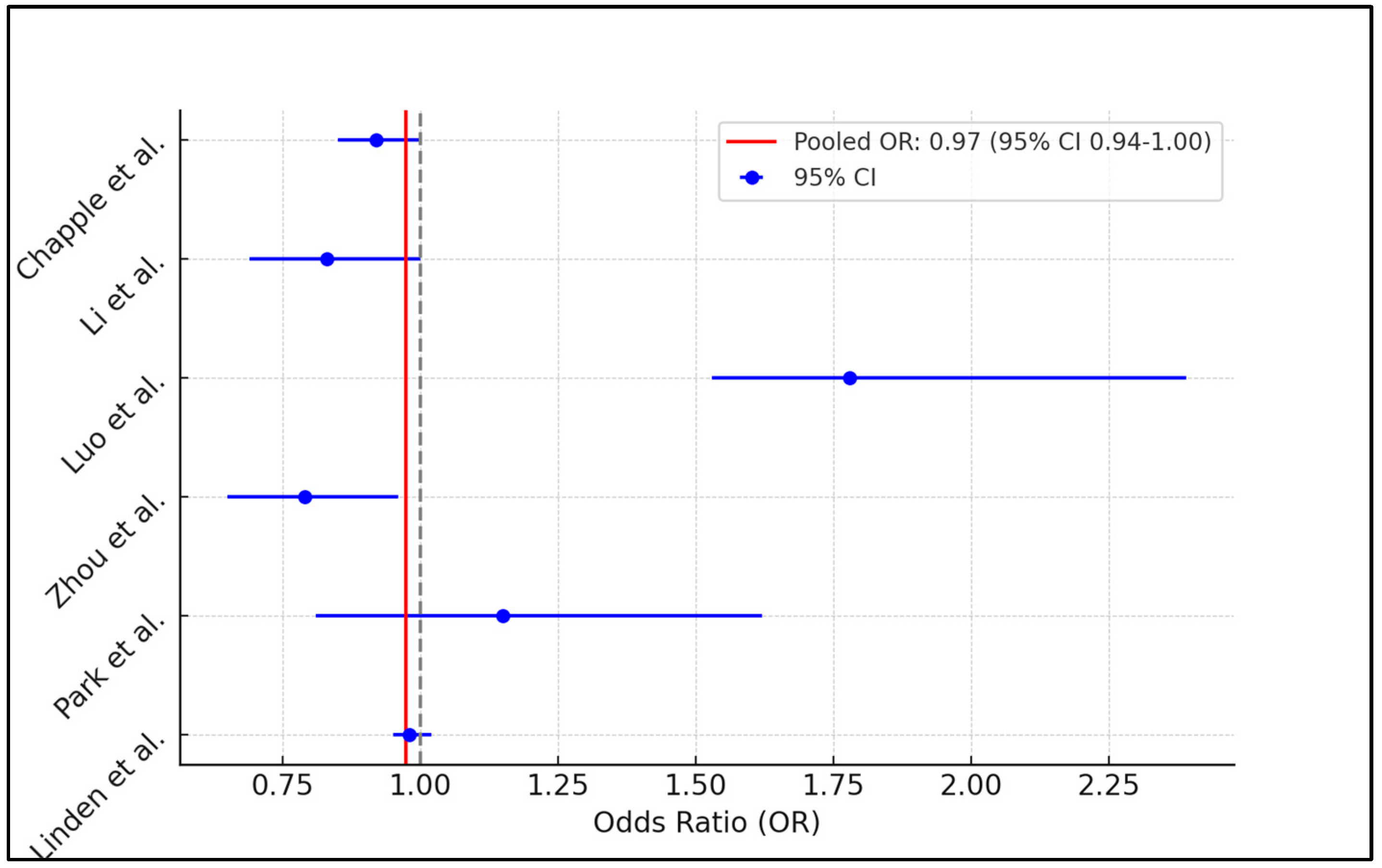
3.3. Results of Synthesis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nazir, M.A. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int. J. Health Sci. 2017, 11, 72–80. [Google Scholar] [PubMed] [PubMed Central]
- Jepsen, S.; Blanco, J.; Buchalla, W.; Carvalho, J.C.; Dietrich, T.; Dörfer, C.; Eaton, K.A.; Figuero, E.; Frencken, J.E.; Graziani, F.; et al. Prevention and control of dental caries and periodontal diseases at individual and population level: Consensus report of group 3 of joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J. Clin. Periodontol. 2017, 44 (Suppl. S18), S85–S93. [Google Scholar] [CrossRef] [PubMed]
- Mi, N.; Zhang, M.; Ying, Z.; Lin, X.; Jin, Y. Vitamin intake and periodontal disease: A meta-analysis of observational studies. BMC Oral Health 2024, 24, 117. [Google Scholar] [CrossRef] [PubMed]
- Deandra, F.A.; Ketherin, K.; Rachmasari, R.; Sulijaya, B.; Takahashi, N. Probiotics and metabolites regulate the oral and gut microbiome composition as host modulation agents in periodontitis: A narrative review. Heliyon 2023, 3, e13475. [Google Scholar] [CrossRef] [PubMed]
- Cagetti, M.G.; Wolf, T.G.; Tennert, C.; Camoni, N.; Lingström, P.; Campus, G. The Role of Vitamins in Oral Health. A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 938. [Google Scholar] [CrossRef] [PubMed]
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Zohaib, S.; Almas, K. The Role of Nutrition in Periodontal Health: An Update. Nutrients 2016, 8, 530. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Amato, M.; Di Spirito, F.; D’Ambrosio, F.; Boccia, G.; Moccia, G.; De Caro, F. Probiotics in Periodontal and Peri-Implant Health Management: Biofilm Control, Dysbiosis Reversal, and Host Modulation. Microorganisms 2022, 18, 2289. [Google Scholar] [CrossRef] [PubMed]
- Amimo, J.O.; Michael, H.; Chepngeno, J.; Raev, S.A.; Saif, L.J.; Vlasova, A.N. Immune Impairment Associated with Vitamin A Deficiency: Insights from Clinical Studies and Animal Model Research. Nutrients 2022, 14, 5038. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Huang, Z.; Liu, Y.; Qi, G.; Brand, D.; Zheng, S.G. Role of Vitamin A in the Immune System. J. Clin. Med. 2018, 7, 258. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ustianowski, Ł.; Ustianowska, K.; Gurazda, K.; Rusiński, M.; Ostrowski, P.; Pawlik, A. The Role of Vitamin C and Vitamin D in the Pathogenesis and Therapy of Periodontitis-Narrative Review. Int. J. Mol. Sci. 2023, 24, 6774. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Murererehe, J.; Uwitonze, A.M.; Nikuze, P.; Patel, J.; Razzaque, M.S. Beneficial Effects of Vitamin C in Maintaining Optimal Oral Health. Front. Nutr. 2022, 8, 805809. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kaur, G.; Kathariya, R.; Bansal, S.; Singh, A.; Shahakar, D. Dietary antioxidants and their indispensable role in periodontal health. J. Food Drug Anal. 2016, 24, 239–246. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Behfarnia, P.; Dadmehr, M.; Hosseini, S.N.; Mirghaderi, S.A. The effect of Vitamin E supplementation on treatment of chronic periodontitis. Dent. Res. J. 2021, 18, 62. [Google Scholar] [PubMed] [PubMed Central]
- Spahr, A.; Divnic-Resnik, T. Impact of health and lifestyle food supplements on periodontal tissues and health. Periodontol. 2000 2022, 90, 146–175. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barnawi, B.M.; Alrashidi, N.S.; Albalawi, A.M.; Alakeel, N.S.; Hamed, J.T.; Barashid, A.A.; Alduraibi, M.S.; Alhussain, G.S.; Alghadeer, J.Y.; Alarifi, N.A.; et al. Nutritional Modulation of Periodontal Diseases: A Narrative Review of Recent Evidence. Cureus 2023, 15, e50200. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shetty, A.S.; Shenoy, R.; Bajaj, P.D.; Rao, A.; Ks, A.; Pai, M.; Br, A.; Jodalli, P. Role of nutritional supplements on oral health in adults—A systematic review. F1000Research 2023, 12, 492. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Varela-López, A.; Navarro-Hortal, M.D.; Giampieri, F.; Bullón, P.; Battino, M.; Quiles, J.L. Nutraceuticals in Periodontal Health: A Systematic Review on the Role of Vitamins in Periodontal Health Maintenance. Molecules 2018, 23, 1226. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chapple, I.L.C.; Milward, M.R.; Dietrich, T. The Prevalence of Inflammatory Periodontitis Is Negatively Associated with Serum Antioxidant Concentrations. J. Nutr. 2007, 137, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Shang, Q.; Yang, D.; Peng, J.; Zhao, H.; Xu, H.; Chen, Q. Abnormal Micronutrient Intake Is Associated with the Risk of Periodontitis: A Dose-response Association Study Based on NHANES 2009–2014. Nutrients 2022, 14, 2466. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Luo, P.; Xu, H.; Chen, Y.; Wu, S. Periodontal disease severity is associated with micronutrient intake. Aust. Dent. J. 2018, 63, 193–201. [Google Scholar] [CrossRef]
- Zhou, S.; Chen, J.; Cao, R. Association between retinol intake and periodontal health in US adults. BMC Oral Health 2023, 23, 61. [Google Scholar] [CrossRef]
- Park, J.-A.; Lee, J.-H.; Lee, H.-J.; Jin, B.-H.; Bae, K.-H. Association of Some Vitamins and Minerals with Periodontitis in a Nationally Representative Sample of Korean Young Adults. Biol. Trace Element Res. 2016, 178, 171–179. [Google Scholar] [CrossRef]
- Linden, G.J.; McClean, K.M.; Woodside, J.V.; Patterson, C.C.; Evans, A.; Young, I.S.; Kee, F. Antioxidants and periodontitis in 60-70-year-old men. J. Clin. Periodontol. 2009, 36, 843–849. [Google Scholar] [CrossRef] [PubMed]
- El-Sayed, K.M.F.; Cosgarea, R.; Sculean, A.; Doerfer, C. Can vitamins improve periodontal wound healing/regeneration? Periodontol. 2000 2024, 94, 539–602. [Google Scholar] [CrossRef] [PubMed]
- Atalay, N.; Balci, N.; Toygar, H.U.; Yardimci, G.; Gürsoy, U.K. Serum, saliva, and gingival tissue human β-defensin levels in relation to retinoic acid use. J. Periodontol. 2023, 94, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Huang, D.; Liu, Y.; Qiu, Y.; Lu, S. Diet-derived circulating antioxidants, periodontitis and dental caries: A Mendelian randomization study. J. Periodontal Res. 2024; in press. [Google Scholar] [CrossRef] [PubMed]
- El-Sayed, K.M.F.; Bittner, A.; Schlicht, K.; Mekhemar, M.; Enthammer, K.; Höppner, M.; Es-Souni, M.; Schulz, J.; Laudes, M.; Graetz, C.; et al. Ascorbic Acid/Retinol and/or Inflammatory Stimuli’s Effect on Proliferation/Differentiation Properties and Transcriptomics of Gingival Stem/Progenitor Cells. Cells 2021, 10, 3310. [Google Scholar] [CrossRef]
- Costa, P.D.; Canaan, J.C.R.; Castelo, P.M.; Fonseca, D.C.; Pereira-Dourado, S.M.; Murata, R.M.; Pardi, V.; Pereira, L.J. Influence of Micronutrient Intake, Sociodemographic, and Behavioral Factors on Periodontal Status of Adults Assisted by a Public Health Care System in Brazil: A Cross-Sectional Multivariate Analysis. Nutrients 2021, 13, 973. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- El-Sayed, K.M.F.; Hein, D.; Dörfer, C.E. Retinol/inflammation affect stemness and differentiation potential of gingival stem/progenitor cells via Wnt/β-catenin. J. Periodontal Res. 2019, 54, 413–423. [Google Scholar] [CrossRef] [PubMed]
- Hans, M.; Malik, P.K.; Hans, V.M.; Chug, A.; Kumar, M. Serum levels of various vitamins in periodontal health and disease—A cross sectional study. J. Oral Biol. Craniofac. Res. 2023, 13, 471–475, Erratum in: J. Oral Biol. Craniofac. Res. 2024, 14, 360–361. [Google Scholar] [CrossRef] [PubMed]
- Saleh, M.H.A.; Decker, A.; Tattan, M.; Tattan, O.; Decker, J.; Alrmali, A.; Wang, H.-L. Supplement Consumption and Periodontal Health: An Exploratory Survey Using the BigMouth Repository. Medicina 2023, 59, 919. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Study and Author | Country | Study Year | Study Design | Quality Assessment |
|---|---|---|---|---|
| 1 [21] Chapple et al. | USA | 2007 | Cross-sectional | Medium |
| 2 [22] Li et al. | China | 2022 | Cross-sectional | Medium |
| 3 [23] Luo et al. | China | 2018 | Cross-sectional | Medium |
| 4 [24] Zhou et al. | USA | 2023 | Cross-sectional | High |
| 5 [25] Park et al. | South Korea | 2016 | Cross-sectional | Medium |
| 6 [26] Linden et al. | UK | 2009 | Cross-sectional | High |
| Study and Author | Number of Participants (Study Groups) | Comparison Group | Age (Category/Mean/Median), Years | Gender (Male) |
|---|---|---|---|---|
| 1 [21] Chapple et al. | Mild disease: 1567 patients Severe disease: 609 patients | No periodontal disease: 20,784 | Mild disease: 52.2 Severe disease: 56.4 | Mild disease: 61.1% Severe disease: 68.1% |
| 2 [22] Li et al. | Moderate/severe periodontitis: 3994 patients | No periodontal disease: 4965 | 56.7 | 57.9% |
| 3 [23] Luo et al. | Moderate disease: 2274 patients Severe disease: 676 patients | No periodontal disease: 3465 | Moderate disease: 55.3 Severe disease: 54.5 | Moderate disease: 54.1% Severe disease: 70.4% |
| 4 [24] Zhou et al. | Moderate/severe periodontitis: 3380 | No periodontal disease: 5701 | 50.8 | 48.3% |
| 5 [25] Park et al. | Periodontitis: 279 patients | No periodontal disease: 1770 | 33.1 | 52.3% |
| 6 [26] Linden et al. | Periodontitis: 96 patients | Mild/no periodontal disease: 1162 | 64.2 | 100% |
| Study and Author | Periodontal Disease Assessment | Smoking Status and Diabetes Status | Vitamin A Assessment | Risk Assessment (OR/HR/RR—95% CI) |
|---|---|---|---|---|
| 1 [21] Chapple et al. | At least one site with both clinical attachment loss ≥4 mm and probing pocket depth of ≥4 mm | Mild disease (smoking): 25.8% Severe disease (smoking): 21.4% Mild disease (diabetes): 12.2% Severe disease (diabetes): 15.3% | 1st quintile: 1.33 umol/L 2nd quintile: 1.68 umol/L 3rd quintile: 1.92 umol/L 4th quintile: 2.20 umol/L 5th quintile: 2.69 umol/L | Sufficient vitamin A OR: 0.92 (95% CI: 0.85–1.00) |
| 2 [22] Li et al. | ≥2 Interproximal sites with a clinical attachment loss (CAL) of ≥4 mm; ≥2 Interproximal sites with a periodontal probing depth of ≥5 mm | Smoking: 17.8% Diabetes: 21.2% | Protective daily vitamin A cutoff: 526.7 retinol activity equivalents | Sufficient vitamin A OR: 0.83 (95% CI: 0.69–1.00) |
| 3 [23] Luo et al. | At least two interproximal sites with PD of at least 5 mm not occurring on the same tooth, or at least two interproximal sites that are not on the same tooth and that have an AL of at least 4 mm | Moderate disease (smoking): 29.8% Severe disease (smoking): 27.4% Moderate disease (diabetes): 15.4% Severe disease (diabetes): 13.6% | Moderate disease ≤261 ug: 26.5% Severe disease ≤261 ug: 31.0% | ≤61 ug (insufficient) vs. ≥786 ug (sufficient) OR: 1.78 (95% CI: 1.53–2.39) |
| 4 [24] Zhou et al. | Moderate periodontitis: ≥2 interproximal sites with PD ≥5 mm not on the same tooth, or ≥2 interproximal sites with CAL ≥4 mm not on the same tooth; Severe periodontitis: ≥2 interproximal sites with CAL ≥6 mm not on the same tooth and ≥1 interproximal site with PD ≥5 mm | Smoking: 16.7% Diabetes: 9.5% | NR | (ORtertile3vs1 = 0.79, 95% CI: 0.65–0.96). The association was still significant in populations who were less than 60 years old (ORtertile3vs1 = 0.80, 95% CI: 0.65–0.97), non-Hispanic black (ORtertile3vs1 = 0.62, 95% CI: 0.42–0.94), PI ≤ 1.3 (ORtertile3vs1 = 0.72, 95% CI: 0.55–0.93), 1.3 < PI ≤ 3.5 (ORtertile3vs1 = 0.70, 95% CI: 0.55–0.89), non-smokers (ORtertile3vs1 = 0.63, 95% CI: 0.48–0.81), obesity (ORtertile3vs1 = 0.68, 95% CI: 0.49–0.94), and not exhibiting diabetes mellitus (ORtertile3vs1 = 0.79, 95% CI: 0.65–0.95) or hypertension (ORtertile3vs1 = 0.63, 95% CI: 0.47–0.84). |
| 5 [25] Park et al. | Periodontitis was defined as a CPI greater than or equal to 3, which indicates that at least one site had a probing pocket depth of >3.5 mm (code 4 > 5.5 mm) | Smoking: 18.7% Diabetes: 17.1% | Periodontitis <602 ug: 50% | Insufficient vitamin A OR: 1.15 (95% CI: 0.81–1.62) |
| 6 [26] Linden et al. | Severe periodontitis >15% of all sites measured had a loss of attachment (6 mm), and there was at least one site with deep pocketing (6 mm) | Smoking: 36.4% Diabetes: 11.5% | NR | OR: 0.98 (95% CI: 0.95–1.02) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luca, M.M.; Buzatu, R.; Bumbu, B.A. Evaluating the Protective Role of Vitamin A Supplementation in Periodontal Health: A Comprehensive Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 4775. https://doi.org/10.3390/jcm13164775
Luca MM, Buzatu R, Bumbu BA. Evaluating the Protective Role of Vitamin A Supplementation in Periodontal Health: A Comprehensive Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2024; 13(16):4775. https://doi.org/10.3390/jcm13164775
Chicago/Turabian StyleLuca, Magda Mihaela, Roxana Buzatu, and Bogdan Andrei Bumbu. 2024. "Evaluating the Protective Role of Vitamin A Supplementation in Periodontal Health: A Comprehensive Systematic Review and Meta-Analysis" Journal of Clinical Medicine 13, no. 16: 4775. https://doi.org/10.3390/jcm13164775