Obstetric Outcomes in Women on Lithium: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
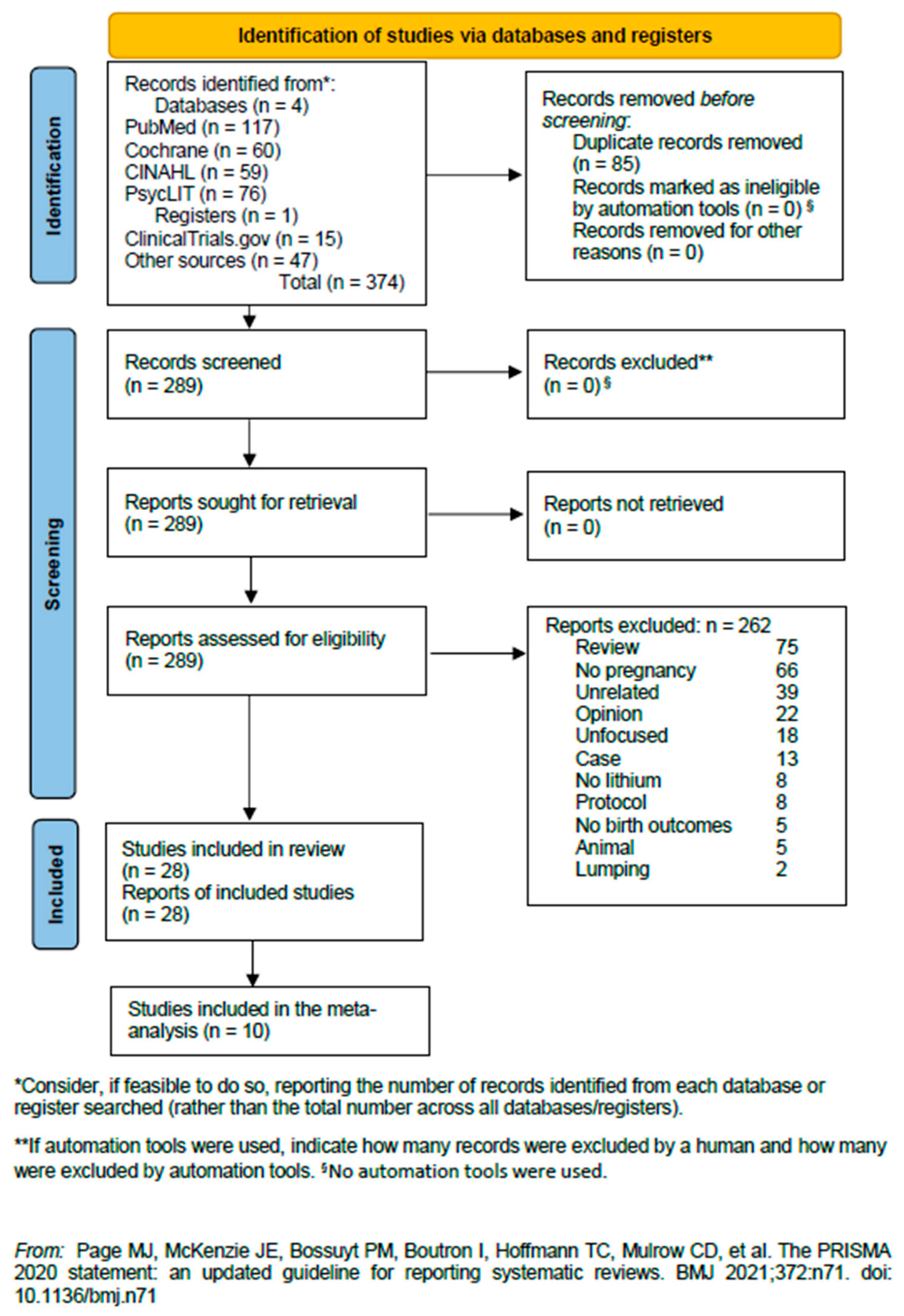
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy and Selection of Studies
2.3. Data Extraction
2.4. Data Analysis
3. Results
3.1. Methodologies of Included Studies
| Study | Population | Design/Study Type | Li+-Related Birth/Pregnancy Outcomes | Conclusions |
|---|---|---|---|---|
| Schou, 1976 [8] | 67 (26 ♀, 34 ♂) babies treated with Li+; 57 HCs (siblings 25 ♀, 32 ♂) | Questionnaire with the mother’s name, birth data, and address, and the Li+ child’s birth data were filled in. The informant was asked to submit information about name, birth data, sex, physical development, and mental development of all the woman’s children. | Development anomalous 10 Li+ children, 6 HCs. Among the Li+ children with developmental anomalies, three had been exposed to Li+ during the first trimester only, and seven had been exposed during the entire foetal period. The difference between these frequencies is not statistically significant. | The data obtained do not reveal any ↑ frequency of physical or mental anomalies among the Li+ children. |
| Källén & Tandberg 1983 [24] | 350 infants whose mothers were treated as inpatients for manic-depressive disease | Cohort study. Several registers were used: DRPW, MBR, RCM | The mothers were divided into five groups: (1) no information on psychiatric illness before pregnancy indicated in chart, (2) diagnosis of psychiatric illness given in the chart but no mention of drug use, (3) psychotropic drug given (disease, of course, present) but no Li+ given, (4) only Li+ given, and (5) Li+ and other psychotropic drug given. | There is no statistically significant difference between delivery outcome in women on Li+ and in ♀ on other psychotropic drugs. |
| Jacobson et al., 1992 [35] | 148 ♀ mean age 30 yrs, using Li+ in the first trimester of pregnancy; 148 HC matched for age | Multicentre study | The rates of major congenital malformations did not differ between the Li+ (2.8%) and control (2.4%) groups. | The pregnancy outcome did not differ between patients and controls with respect to the total number of livebirths, frequency of major anomalies, spontaneous or therapeutic abortions, ectopic pregnancy, and prematurity. |
| Troyer et al., 1993 [25] | 60 ♀ treated with lithium; 290 ♀ not exposed to lithium | Retrospective cohort study | The RR of premature delivery for ♀ taking lithium during pregnancy was × 2.54 that of ♀ with or without manic-depressive illness who were not receiving Li+ during pregnancy. | Lithium exposure during pregnancy was linked to an increased risk for pre-term birth. |
| McKenna et al., 2005 [36] | 105 ♀ exposed to atypical APs and 105 ♀ to non-teratogenic agents in the 1st trimester matched for gestational age. Ages not provided | Motherisk Program in Toronto Ontario, Canada; Israeli Teratogen Information Service in Jerusalem, Israel; and Drug Safety Research Unit in Southampton, England, UK (3 sites). Observational study of a cohort | Li+ was taken by six ♀ during pregnancy at some point; 5/6 discontinued it. No major malformation reported. | Although the study focused on APs, scanty data on Li+ were reported that showed no malformations with Li+. |
| Reis & Källén, 2008 [34] | 2908 ♀ treated with APs (79 with Li+) | This cohort study is based on data from the Swedish Medical Birth Register. Maternal drug use in early pregnancy is recorded from interviews performed by the midwife at the first antenatal care visit, usually before the end of the first trimester. | A total of 79 ♀ were treated with Li+. Among them, eight had a diagnosis of a congenital malformation. One infant had Down syndrome, one had an unspecified skin malformation, and two had an unstable hip. Four had cardiac defects: one had a combined atrium septum defect and tricuspid and mitral malformations, one had mitral insufficiency and hypospadias, one had a ventricular septum defect, and one had patent ductus arteriosus in a term baby (born after 41 completed weeks). Even though the rate of cardiac defects was high (5.1%), it had a wide CI (1.4–12.5%), and the defects were relatively mild. | ↑ risk for congenital malformations (mainly cardiovascular defects), nearly double the risk of for gestational diabetes, and a 40% ↑ risk for caesarean delivery was noted. No certain drug specificity was found. Because there seems to be little drug specificity, it is possible that underlying pathology or unidentified confounding comorbidities explain the excess risk. |
| van der Lugt et al., 2012 [37] | 15 children who were exposed to Li+ in utero were investigated at 3–15 years of age | Observational retrospective cohort study. Neurological development was tested using the Hempel or Touwen examination. Cognitive development was assessed with the Bayley Scales of Infant Development III, Wechsler Preschool and Primary Scale of Intelligence, or the Wechsler Intelligence Scale for Children. Parents completed the Child Behavior Checklist to assess behavioural development and a standard questionnaire about general development of the child since birth. | One child had signs of a minor neurological dysfunction but without further clinical implications. The results of the cognitive tests were within normal limits, although most children had lower scores on the performance IQ subtest. Growth, behaviour, and general development were within the normal ranges. | Continuing Li+ therapy during pregnancy did not cause adverse effects on growth, neurological, cognitive, and behavioural development of exposed children. |
| Bodén et al., 2012 [38] | 332,137 ♀ (of whom 320 were in treatment for BD, 554 with BD untreated); both groups were compared with all other ♀ giving birth (331,263). 76 ♀ exposed to Li+ | Cohort study using data from national health registers | The risks of preterm birth in both treated and untreated were ↑ by 50%. Of the untreated ♀, 3.9% (n = 542) had a microcephalic infant compared with 2.3% (324 844) of the ♀ without BD (1.68, 1.07 to 2.62). The corresponding values for the treated ♀ were 3.3% (n = 311) (1.26, 0.67 to 2.37). Similar trends were observed for risks of infants being small for gestational age according to infants’ weight and length. Among the infants of untreated ♀, 4.3% (n = 24) had neonatal hypoglycaemia compared with 2.5% (n = 8302) among the infants of ♀ without BD (1.51, 1.04 to 2.43), and 3.4% (n = 11) of the treated ♀ (1.18, 0.64 to 2.16). The analyses of variation in the outcomes did not support any significant differences between treated and untreated ♀. | BD in ♀ during pregnancy, whether treated or not, was associated with ↑ risks of adverse pregnancy outcomes. |
| Diav-Citrin et al., 2014 [26] | 183 ♀ Li+-exposed pregnancies compared with 72 disease-matched and 748 non-Li+-exposed pregnancies | Prospective, comparative observational study | There were significantly more miscarriages (adjusted odds ratio = 1.94, 95%CI = 1.08–3.48) and elective terminations of pregnancy (17/183 [9.3%] compared with 15/748 [2.0%]) in the Li+-exposed group compared with the non-teratogenic exposure group. Major congenital anomalies not significantly different. Cardiovascular anomalies occurred more frequently in the Li+ group exposed during the first trimester when compared with the non-teratogenic exposure group. Non-cardiovascular anomalies were not significantly different between the groups. Preterm deliveries ↑ in the Li+ group compared with non-teratogenic exposure. | Li+ treatment in pregnancy is associated with a higher rate of cardiovascular anomalies. ♀ who are treated with Li+ during organogenesis should undergo foetal echocardiography and level-2 ultrasound. |
| Rosso et al., 2016 [39] | 17 Li+-treated ♀ with severe BD-I who wished to become pregnant | Lo. Treatment with flexible doses of Li + combined with supportive psychotherapy throughout the pregnancy and the postpartum period | Li+ was generally well tolerated: three ♀ became overweight and two ♀ reported mild polyuria and polydipsia (already reported with Li+ treatment before pregnancy). No congenital abnormalities occurred. Three babies with mild hypotonia spontaneously recovered. Recurrences of any polarity during pregnancy occurred in 11.1% of ♀. Post-delivery rate of psychiatric disorders 29.4%; in other studies of unmedicated BP ♀, postpartum recurrence rate was generally much ↑. | The results support the prophylaxis efficacy of Li+ throughout pregnancy in Li+-responder BD-I ♀ who have ↑ risk of severe peripartum recurrences. |
| Petersen et al., 2016 [41] | 28 ♀ exposed to Li+ during pregnancy; 57 ♀ who discontinued Li+ during pregnancy; 212,531 ♀ not prescribed APs | Retrospective cohort study. Based on UK electronic primary care health records from the Clinical Practice Research Datalink database and the Health Improvement Network primary care database. Among the many objectives, one was to identify risk factors predictive of discontinuation of and restarting Li+ (from multiple manufacturers), anticonvulsant mood stabilizers, and AP medication | No birth/pregnancy outcomes associated with Li+ | It was impossible to investigate Li+ or anticonvulsant use-associated risk specifically for psychoses owing to the small numbers of ♀ in these groups. |
| Boyle et al., 2017 [42] | 173 Ebstein’s anomaly babies/foetuses; 51,024 non-cardiac controls; 26,170 cardiac controls | Descriptive epidemiological analysis using population-based data. The aim was to describe the epidemiology of Ebstein’s anomaly in Europe and investigate its associations with maternal health and medication exposure during pregnancy. Data were taken from 15 European Surveillance of Congenital Anomalies (EUROCAT) Congenital Anomaly Registries in 12 European countries, with a population of 5.6 million births during 1982–2011. | No case of Ebstein’s anomaly was associated with Li+ assumption during pregnancy. | Li+ not associated with Ebstein’s cardiac anomaly in those 13 patients who took Li+. Figures provided are unlikely. |
| Patorno et al., 2017 [27] | 1,325,563 ♀, 663 infants exposed to Li+ first trimester, 1945 exposed to lamotrigine first trimester, 1,322,955 unexposed infants | Cohort study. This study examined the risk of cardiac malformations among infants exposed to Li+ during the first trimester as compared with unexposed infants and, in secondary analyses, with infants exposed to another commonly used mood stabilizer, lamotrigine. | Cardiac malformations were present in 16 of the 663 infants exposed to Li+ (2.41%) and 15,251 of the 1,322,955 unexposed infants (1.15%). The adjusted risk ratio for cardiac malformations among infants exposed to Li+ as compared with unexposed infants was 1.65 (95% CI: 1.02 to 2.68). The risk ratio was 1.11 (95%CI: 0.46 to 2.64) for a daily dose of 600 mg or less, 1.60 (95%CI: 0.67 to 3.80) for 601 to 900 mg, and 3.22 (95%CI: 1.47 to 7.02) for more than 900 mg. The prevalence of right ventricular outflow tract obstruction defects was 0.60% among Li+-exposed infants vs. 0.18% among unexposed infants (adjusted risk ratio, 2.66; 95%CI, 1.00 to 7.06). | Maternal use of Li+ during the first trimester was associated with ↑ risk of cardiac malformations, including Ebstein’s anomaly; the magnitude of this effect was smaller than had been previously postulated. |
| Forsberg et al., 2018 [28] | 20 ♀ with MD exposed to Li+ treatment during pregnancy; eight ♀ with MD (excluding Li+ treatment exposure); 11 ♀ controls (no MD or Li+ treatment exposure) | Retrospective cohort study (♀ gave birth between 2006 and 2010) | The children’s full-scale IQ, performance IQ, and verbal IQ results did not differ significantly between the groups. | No significant association between mothers’ prenatal exposure to Li+ or mood disorders and their offspring’s IQ was found. |
| Frayne et al., 2018 [43] | 19 ♀ exposed to Li+ at any time during pregnancy; 14 ♀ exposed to Li+ at conception but ceased Li+ at confirmation of pregnancy | Retrospective cohort study (♀ gave birth between December 2007 and January 2015 at a specialist antenatal clinic in Western Australia) | Of the babies exposed to Li+ during pregnancy and at delivery (n = 19), eight (42%) were admitted to the SCN post-delivery, of which six (31.6%) were admitted to a level-3 or neonatal intensive care unit. | Exposure to Li+ during pregnancy was associated with ↑ rates of foetal ultrasound abnormalities, such as abdominal circumference >90th %. |
| Munk-Olsen et al., 2018 [29] | 22,124 eligible pregnancies, of which 727 pregnancies were eligible for inclusion in the Li+-exposed group | In this meta-analysis, primary data from pregnant ♀ and their children from six international community-based (Denmark, Sweden, and Ontario, Canada) and clinic-based (the Netherlands, UK, and USA) cohorts were analysed. This study aimed to investigate the association between in-utero Li+ exposure and the risk of pregnancy complications, delivery outcomes, neonatal morbidity, and congenital malformations. aORs and 95% CIs were calculated through logistic regression models, and site-specific prevalence rates and ORs were pooled using random-effects meta-analytical models. | Li+ exposure was not associated with any of the predefined pregnancy complications or delivery outcomes. ↑ risk for neonatal readmission within 28 days of birth was seen in the Li+-exposed group compared with the reference group (pooled prevalence 27·5% [95% CI: 15·8 to 39·1] vs 14·3% [10·4 to 18·2]; pooled aOR 1·62, 95% CI 1·12 to 2·33). Li+ exposure during the first trimester was associated with ↑ risk of major malformations (pooled prevalence 7.4% [95% CI: 4.0 to 10.7] vs. 4.3% [3.7 to 4.8]; pooled aOR 1.71, 95%CI: 1.07 to 2.72) but for major cardiac malformations, the difference was n.s. (2.1% [0.5 to 3.7] vs. 1.6% [1.0 to 2.1]; pooled aOR 1.54, 95% CI 0.64 to 3.70). | Treatment decisions for pregnant ♀ with mood disorders must weigh the potential for ↑ risks of Li+ during pregnancy, particularly those associated with use of Li+ during the first trimester, against its effectiveness at ↓ relapse. |
| Neri et al., 2018 [40] | 140 ♀ exposed to Li+ treatment during pregnancy (range 20–46 yrs old) | Retrospective survey and a selective review of the literature regarding the management of fertile patients under Li+ treatment for BD.The survey was conducted by the Teratology Information Service (TIS) at A. Gemelli University Hospital in Rome from May 2002 to December 2015. | Among all the pregnancies, the data collected by the TIS showed one premature birth, six early spontaneous abortions, one case of major cardiac malformation (hypoplastic left heart syndrome), four transient respiratory distress at birth, and two language delays. | No significant results emerged. The conclusion of the study is that peri-conception counselling is crucial for the outcome of pregnancy and for maternal health status during preconception, gestation, and breastfeeding. |
| Poels et al., 2020 [12] | 77 ♀ with BD type 1 exposed to Li+ during pregnancy; 366 ♀ with BD type 1 not exposed to Li+ | Retrospective observational cohort study. The aim was to evaluate the association between Li+ use during pregnancy and the occurrence of miscarriage. | Miscarriages occurred in 20.8% of pregnancies exposed to Li+ (n = 16 out of 77) compared to 10.9% of pregnancies not exposed to Li+ (n = 40 out of 366). | Li+ use during pregnancy may ↑ the risk of miscarriage among ♀ with BD-I disorder (adjusted OR = 2.94; 95% CI = 1.39–6.22). |
| Molenaar et al., 2021 [44] | 78 ♀ with 100 pregnancies under Li+ treatment exposure (233 Li+ blood level measurements); 29 neonates with Li+ measurement in the 24 h postpartum | Retrospective observational cohort study. The first outcome was to evaluate ♀ Li+ blood level changes following delivery. The second outcome was to evaluate neonatal Li+ blood level and complications. | No association was found between time (wk before or after delivery) and the ratio of Li+ blood level/dose. No associations were found between neonatal Li+ blood levels at delivery and neonatal outcomes. | ↓ the dosage or discontinuing Li+ prior delivery is not recommended. Stable dosing can prevent subtherapeutic Li+ serum levels, which is especially important in the postpartum period, when relapse risks are highest. |
| Hastie et al., 2021 [30] | 434 ♀ exposed to Li+ treatment during pregnancy; 853,583 ♀ not exposed to Li+ treatment during pregnancy | Retrospective observational population-based cohort study. The aim was to examine the associations between Li+ use during pregnancy and the risk of adverse pregnancy and neonatal outcomes. | Maternal Li+ use during pregnancy was associated with ↑ risks of spontaneous preterm birth, birth of a large infant for gestational age, cardiac malformations, and neonatal hypoglycaemia. These associations remained significant in subgroup analyses among pregnant ♀ with diagnosed psychiatric illnesses and in analyses comparing ♀ who continued Li+ treatment during pregnancy versus those who discontinued treatment prior to pregnancy. | Li+ use during pregnancy is associated with ↑ risk of spontaneous preterm birth, infants large for gestational age, cardiac malformations, and potentially other adverse neonatal outcomes. |
| Sagué-Vilavella et al., 2022 [32] | 53 ♀ with BD exposed to Li+ treatment during pregnancy; 47 ♀ with BD not exposed to Li+ during pregnancy | Retrospective observational cohort study. The aim was to compare obstetric outcomes in ♀ with BD with and without Li+ treatment during pregnancy. | No significant differences in obstetric complications, neonatal complications, or congenital anomalies were observed between the groups. Newborns of Li+-treated ♀ had ↓ Apgar scores at 1 min and 5 min compared to newborns of ♀ who did not receive Li+ during pregnancy. | Li+ treatment during pregnancy did not lead to worse obstetric outcomes in ♀ with BD, except for the impact on newborn Apgar scores. |
| Poels et al., 2022 [31] | 99 children of ♀ with a diagnosis of BD, aged 6–14: 56 were exposed to Li+ in utero and 43 were not exposed | CS. Neuropsychological tests were administered, including the SON test and the NEPSY-II-NL assessment. Linear and negative binomial regression models were used to investigate the association between prenatal Li+ exposure and neuropsychological functioning. In secondary analyses, the association between Li+ blood level during pregnancy and neuropsychological functioning was assessed. | Li+ use during pregnancy was associated with the total number of mistakes made on the Auditory Attention task but was statistically n.s. after full adjustment for potential confounding factors. No association between prenatal Li+ exposure and IQ was found. Additionally, no relationship between Li+ blood level during pregnancy and neuropsychological functioning was found after adjustment for potential confounders. Task outcomes in both groups were ≈ to the general population. | There was no evidence for significantly altered neuropsychological functioning of Li+ -exposed children when compared to non-exposed children. |
| Torfs et al., 2022 [49] | 10 mother–neonate pairs with intrauterine exposure to Li+ | Lo. The primary aim of this retrospective study was to assess the early postnatal characteristics and short-term outcomes of neonates with in utero exposure to Li+. | The x− GA was 37 (IQR, 36–39) wks. The neonatal plasma Li+ concentration at birth was 0.65 (IQR 0.56–0.83) mmol/L, with a median neonate/mother ratio of 1.02 (IQR 0.87–1.08). The median length of neonatal stay was 8.5 (IQR 8–12) days. Three cases in this study population displayed hypotonia, three had respiratory symptoms, and one had hypoglycaemia. Four neonates displayed a (mild) abnormal clinical neurological evaluation in the early postnatal phase. One neonate was diagnosed with NDI and the same neonate was diagnosed with a CDH. | Although causality could not be assessed due to the small sample size, these findings illustrate that indeed mild to moderate neonatal symptoms after in utero exposure to Li+ have to be anticipated. A postnatal care protocol was proposed to enhance the quality of care for future neonates and to guide parental counselling. Future prospective protocol evaluation is needed. |
| Poels et al., 2023 [45] | 63 children of ♀ with a diagnosis of BP, aged 8–14: 30 with and 33 without intrauterine exposure to Li+ | CS. Global brain volume outcomes and white matter integrity were assessed using structural MRI and DTI, respectively. To assess how the data compared to the general population, global brain volumes were compared to data from the Generation R study (N = 3243). | Linear regression analyses showed a n.s. negative association of intrauterine exposure to Li+ with subcortical grey matter volume (unstandardized β = −1.6, 95%CI: −3.1 to −0.1, p-value = 0.04, p-value after FDR correction = 0.48). The subcortical grey matter volume and cortical white matter volume were significantly reduced in Li+-exposed children compared to children from the Generation R cohort (unstandardized β = −1.4, 95%CI: −2.4 to −0.5, p-value = 0.004, p-value after FDR correction = 0.008 and unstandardized β = −14.3, 95%CI: −22.3 to −6.2, p-value <0.001, p-value after FDR correction =0.006, respectively). | Brain structure in Li+-exposed ≈ non-Li+-exposed children following correction for multiple testing |
| Álvarez-Silvares et al., 2023 [48] | 79 low obstetric risk pregnant ♀ | Lo. Prospective cohort study. The objective of this study was to correlate the placenta levels of 14 essential and non-essential elements with neonatal weight by conducting multivariable linear regressions using GLM and GAM. | Placental Co (p = 0.03) and Sr (p = 0.048) concentrations were associated with ↑ neonatal weight. Concentrations of Li+ (p= 0.027), Mo (p = 0.049), and Se (p = 0.02) in the placenta were associated with lower newborn weight. | The concentration of some metals in the placenta may affect foetal growth. |
| Schonewille et al., 2023 [33] | 93 ♀ with BD who gave birth to 117 live-born neonates: 42 (36%) exposed (at any point throughout the pregnancy) and 75 (64%) non-exposed to Li+ | Lo. Retrospective observational cohort study. Outcomes were obtained by medical chart review of ♀ and neonates and compared between neonates with and without Li+ exposure. The primary outcome was admission to a neonatal ward with monitoring, preterm birth, SGA, 5 min Apgar scores, neonatal asphyxia, and readmission ≤ 28 days. | There were n.s. differences in neonatal admission with monitoring (16.7 vs. 20.0%, p = 0.844). Additionally, preterm birth (7.1 vs. 5.3%), SGA (0.0 vs. 8.0%), 5 min Apgar scores (x−: 9.50 vs. 9.51), neonatal asphyxia (4.8 vs. 2.7%), and readmission (4.8 vs. 5.3%) were ≈. Overall, 18.8% of BD offspring was admitted. ♀ with BD had high rates of caesarean section (29.1%), gestational diabetes (12.8%), and hypertensive disorders of pregnancy (8.5%). | Exposure to Li+ was not associated with greater risk of neonatal admission to a ward with monitoring compared to non-exposure to Li+. However, offspring of ♀ with BD were admitted regularly, and ♀ with BD have high obstetric risk that requires clinical and scientific attention. |
| Whaites Heinonen et al., 2023 [41] | 25 infant–mother dyads: 7 infants with serum Li+ concentration at birth ≥0.6 meq/L (HEG); 18 with serum Li+ concentration at birth <0.6 meq/L (LEG) | Lo. Retrospective observational cohort study. This included breastfed infants to ♀ treated with Li+ during and after pregnancy. The first serum Li+ concentration counted for classifying infants as HEG or LEG. The first follow-up visits were at 2–4 wks of age. | x− Li+ serum concentration at birth was 0.90 meq/L in HEG and 0.40 meq/L in LEG (p < 0.05). The difference was still significant at follow-up (0.20 meq/L vs. 0.06 meq/L, p < 0.05), despite reduction in maternal dose. Neonatal symptoms occurred in 85.7% HEG and 41.2% in LEG (p = 0.08; n.s.) at birth and 28.6% vs. 11.8% at follow-up (p = 0.55; n.s.). Furthermore, 28.6% of HEG infants were admitted to neonatal care vs. 5.9% LEG (p = 0.19). All the infants with symptoms at follow-up were either in HEG or exposed to additional psychotropic medication. | This study suggests that late intrauterine exposure to Li+ might add to the adverse effects of Li+-exposed breastfed infants. |
| Schrijver et al., 2024 [46] | 81 ♀ and 101 pregnancies: 61 ♀ with one pregnancy, 20 ♀ with two pregnancies | Lo. Retrospective observational cohort study. This included ♀ with a history of BD or postpartum psychosis, used Li+ during pregnancy, and at least one Li+ serum level during pregnancy was available. Linear and logistic regression models used to investigate the association between weighted average Li+ level and pregnancy duration, birth weight percentiles, preterm birth, and LGA. Subsequent exploratory analyses investigated the role of TSH and T4 as mediators of associations. | Positive association between average Li+ level and risk of preterm birth (OR = 1.66 [95% CI: 1.05 to 2.61], p = 0.03 simple model, OR = 1.69 [95% CI: 1.06 to 2.68] p = 0.03 adjusted model [for mood episode during pregnancy and use of other psychotropics]). There were no significant associations were between the average Li+ level and birth weight percentiles and the risk of LGA birth. In exploratory analyses, TSH and T4 did not mediate the association between the average Li+ serum level and pregnancy duration. | Dose response relationship between maternal Li+ serum levels and pregnancy duration |
3.2. Studies Included in the Meta-Analysis
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cade, J.F. Lithium salts in the treatment of psychotic excitement. Med. J. Aust. 1949, 2, 349–352. [Google Scholar] [CrossRef] [PubMed]
- Schou, M.; Juel-Nielsen, N.; Stromgren, E.; Voldby, H. The treatment of manic psychoses by the administration of lithium salts. J. Neurol. Neurosurg. Psychiatry 1954, 17, 250–260. [Google Scholar] [CrossRef] [PubMed]
- Gershon, S.; Yuwiler, A. Lithium ion: A specific psychopharmacological approach to the treatment of mania. J. Neuropsychiatr. 1960, 1, 229–241. [Google Scholar] [PubMed]
- Shorter, E. The history of lithium therapy. Bipolar Disord. 2009, 11 (Suppl. 2), 4–9. [Google Scholar] [CrossRef] [PubMed]
- Schou, M.; Goldfield, M.D.; Weinstein, M.R.; Villeneuve, A. Lithium and pregnancy. I. Report from the Register of Lithium Babies. BMJ 1973, 2, 135–136. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nora, J.J.; Nora, A.H.; Toews, W.H. Letter: Lithium, Ebstein’s anomaly, and other congenital heart defects. Lancet 1974, 2, 594–595. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, M.R.; Goldfield, M. Cardiovascular malformations with lithium use during pregnancy. Am. J. Psychiatry 1975, 132, 529–531. [Google Scholar] [CrossRef] [PubMed]
- Schou, M. What happened later to the lithium babies? A follow-up study of children born without malformations. Acta Psychiatr. Scand. 1976, 54, 193–197. [Google Scholar] [CrossRef]
- Fornaro, M.; Maritan, E.; Ferranti, R.; Zaninotto, L.; Miola, A.; Anastasia, A.; Murru, A.; Solé, E.; Stubbs, B.; Carvalho, A.F.; et al. Lithium Exposure during pregnancy and the postpartum period: A systematic review and meta-analysis of safety and efficacy outcomes. Am. J. Psychiatry 2020, 177, 76–92. [Google Scholar] [CrossRef]
- Poels, E.M.P.; Bijma, H.H.; Galbally, M.; Bergink, V. Lithium during pregnancy and after delivery: A review. Int. J. Bipolar Disord. 2018, 6, 26. [Google Scholar] [CrossRef]
- Mohamed, M.A.; Elhelbawy, A.; Khalid, M.; AbdAllatif, L.A.; Lialy, H.E. Effects of bipolar disorder on maternal and fetal health during pregnancy: A systematic review. BMC Pregnancy Childbirth 2023, 23, 617. [Google Scholar] [CrossRef]
- Poels, E.M.P.; Kamperman, A.M.; Vreeker, A.; Gilden, J.; Boks, M.P.; Kahn, R.S.; Ophoff, R.A.; Bergink, V. Lithium use during pregnancy and the risk of miscarriage. J. Clin. Med. 2020, 9, 1819. [Google Scholar] [CrossRef] [PubMed]
- Galbally, M.; Roberts, M.; Buist, A.; Perinatal Psychotropic Review Group. Mood stabilizers in pregnancy: A systematic review. Aust. N. Z. J. Psychiatry 2010, 44, 967–977. [Google Scholar] [CrossRef] [PubMed]
- Athar, F.; Ehsan, M.; Farooq, M.; Lo, K.B.; Cheema, H.A.; Ahmad, S.; Naveed, A.; Umer, M. Adverse fetal and neonatal outcomes following in-utero exposure to oxcarbazepine: A systematic review and meta-analysis. Br. J. Clin. Pharmacol. 2022, 88, 3600–3609. [Google Scholar] [CrossRef] [PubMed]
- Battino, D.; Tomson, T.; Bonizzoni, E.; Craig, J.; Perucca, E.; Sabers, A.; Thomas, S.; Alvestad, S.; Perucca, P.; Vajda, F.; et al. Risk of major congenital malformations and exposure to antiseizure medication monotherapy. JAMA Neurol. 2024, 81, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Navaro, M.; Vezzosi, L.; Santagati, G.; Angelillo, I.F.; Collaborative Working Group. Knowledge, attitudes, and practice regarding medication use in pregnant women in Southern Italy. PLoS ONE 2018, 13, e0198618. [Google Scholar] [CrossRef] [PubMed]
- Tondo, L.; Alda, M.; Bauer, M.; Bergink, V.; Grof, P.; Hajek, T.; Lewitka, U.; Licht, R.W.; Manchia, M.; Müller-Oerlinghausen, B.; et al. International Group for Studies of Lithium (IGSLi). Clinical use of lithium salts: Guide for users and prescribers. Int. J. Bipolar Disord. 2019, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Devine, C.A.; Gaffney, C.; Loughnane, G.M.; Kelly, S.P.; O’Connell, R.G. The role of premature evidence accumulation in making difficult perceptual decisions under temporal uncertainty. Elife 2019, 8, e48526. [Google Scholar] [CrossRef] [PubMed]
- Smail-Faugeron, V.; Tan, A.; Caille, A.; Yordanov, Y.; Hajage, D.; Tubach, F.; Martin, G.; Dechartres, A. Meta-analyses frequently include old trials that are associated with a larger intervention effect: A meta-epidemiological study. J. Clin. Epidemiol. 2022, 145, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Driessen, E.; Hollon, S.D.; Bockting, C.L.; Cuijpers, P.; Turner, E.H. Does publication bias inflate the apparent efficacy of psychological treatment for major depressive disorder? A systematic review and meta-analysis of US National Institutes of Health-funded trials. PLoS ONE 2015, 10, e0137864. [Google Scholar] [CrossRef]
- Bartoš, F.; Maier, M.; Shanks, D.R.; Stanley, T.D.; Sladekova, M.; Wagenmakers, E.J. Meta-analyses in psychology often overestimate evidence for and size of effects. R. Soc. Open Sci. 2023, 10, 230224. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Morgan, R.L.; Rooney, A.A.; Taylor, K.W.; Thayer, K.A.; Silva, R.A.; Lemeris, C.; Akl, E.A.; Bateson, T.F.; Berkman, N.D.; et al. A tool to assess risk of bias in non-randomized follow-up studies of exposure effects (ROBINS-E). Environ. Int. 2024, 186, 108602. [Google Scholar] [CrossRef] [PubMed]
- Källén, B.; Tandberg, A. Lithium and pregnancy. A cohort study on manic- depressive women. Acta Psychiatr. Scand. 1983, 68, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Troyer, W.A.; Pereira, G.R.; Lannon, R.A.; Belik, J.; Yoder, M.C. Association of maternal lithium exposure and premature delivery. J. Perinatol. 1993, 13, 123–127. [Google Scholar] [CrossRef]
- Diav-Citrin, O.; Shechtman, S.; Tahover, E.; Finkel-Pekarsky, V.; Arnon, J.; Kennedy, D.; Erebara, A.; Einarson, A.; Ornoy, A. Pregnancy outcome following in utero exposure to lithium: A prospective, comparative, observational study. Am. J. Psychiatry 2014, 171, 785–794. [Google Scholar] [CrossRef]
- Patorno, E.; Huybrechts, K.F.; Bateman, B.T.; Cohen, J.M.; Desai, R.J.; Mogun, H.; Cohen, L.S.; Hernandez-Diaz, S. Lithium Use in Pregnancy and the Risk of Cardiac Malformations. N. Engl. J. Med. 2017, 376, 2245–2254. [Google Scholar] [CrossRef]
- Forsberg, L.; Adler, M.; Römer Ek, I.; Ljungdahl, M.; Navér, L.; Gustafsson, L.L.; Berglund, G.; Chotigasatien, A.; Hammar, U.; Böhm, B.; et al. Maternal mood disorders and lithium exposure in utero were not associated with poor cognitive development during childhood. Acta Paediatr. 2018, 107, 1379–1388. [Google Scholar] [CrossRef]
- Munk-Olsen, T.; Liu, X.; Viktorin, A.; Brown, H.K.; Di Florio, A.; D’Onofrio, B.M.; Gomes, T.; Howard, L.M.; Khalifeh, H.; Krohn, H.; et al. Maternal and infant outcomes associated with lithium use in pregnancy: An international collaborative meta-analysis of six cohort studies. Lancet Psychiatry 2018, 5, 644–652. [Google Scholar] [CrossRef]
- Hastie, R.; Tong, S.; Hiscock, R.; Lindquist, A.; Lindström, L.; Wikström, A.K.; Sundström-Poromaa, I. Maternal lithium use and the risk of adverse pregnancy and neonatal outcomes: A Swedish population-based cohort study. BMC Med. 2021, 19, 291. [Google Scholar] [CrossRef] [PubMed]
- Poels, E.M.P.; Schrijver, L.; White, T.J.H.; Roza, S.J.; Zarchev, M.G.; Bijma, H.; Honig, A.; van Kamp, I.L.; Hoogendijk, W.J.G.; Kamperman, A.M.; et al. The effect of prenatal lithium exposure on the neuropsychological development of the child. Bipolar Disord. 2022, 24, 310–319. [Google Scholar] [CrossRef]
- Sagué-Vilavella, M.; Solé, E.; Pinzón-Espinosa, J.; Sandra-Hernández, A.; Roda, E.; Vieta, E.; Roca, A. Obstetric outcomes regarding the use of lithium in pregnant women with bipolar disorders: A prospective cohort study. Arch. Womens Ment. Health 2022, 25, 729–737. [Google Scholar] [CrossRef]
- Schonewille, N.N.; Terpstra, P.A.; van den Heuvel, M.E.N.; Van Pampus, M.G.; van den Heuvel, O.A.; Broekman, B.F.P. Neonatal admission after lithium use in pregnant women with bipolar disorders: A retrospective cohort study. Int. J. Bipolar Disord. 2023, 11, 24. [Google Scholar] [CrossRef]
- Reis, M.; Källén, B. Maternal use of antipsychotics in early pregnancy and delivery outcome. J. Clin. Psychopharmacol. 2008, 28, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, S.J.; Jones, K.; Johnson, K.; Ceolin, L.; Kaur, P.; Sahn, D.; Donnenfeld, A.E.; Rieder, M.; Santelli, R.; Smythe, J.; et al. Prospective multicentre study of pregnancy outcome after lithium exposure during first trimester. Lancet 1992, 339, 530–533. [Google Scholar] [CrossRef]
- McKenna, K.; Koren, G.; Tetelbaum, M.; Wilton, L.; Shakir, S.; Diav-Citrin, O.; Levinson, A.; Zipursky, R.B.; Einarson, A. Pregnancy outcome of women using atypical antipsychotic drugs: A prospective comparative study. J. Clin. Psychiatry 2005, 66, 444–449, quiz 546. [Google Scholar] [CrossRef] [PubMed]
- van der Lugt, N.M.; van de Maat, J.S.; van Kamp, I.L.; Knoppert-van der Klein, E.A.; Hovens, J.G.; Walther, F.J. Fetal, neonatal and developmental outcomes of lithium- exposed pregnancies. Early Hum. Dev. 2012, 88, 375–378. [Google Scholar] [CrossRef] [PubMed]
- Bodén, R.; Lundgren, M.; Brandt, L.; Reutfors, J.; Andersen, M.; Kieler, H. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: Population based cohort study. BMJ 2012, 345, e7085. [Google Scholar] [CrossRef]
- Rosso, G.; Albert, U.; Di Salvo, G.; Scatà, M.; Todros, T.; Maina, G. Lithium prophylaxis during pregnancy and the postpartum period in women with lithium- responsive bipolar I disorder. Arch. Womens Ment. Health 2016, 19, 429–432. [Google Scholar] [CrossRef] [PubMed]
- Neri, C.; De Luca, C.; D’Oria, L.; Licameli, A.; Nucci, M.; Pellegrino, M.; Caruso, A.; De Santis, M. Managing fertile women under lithium treatment: The challenge of a Teratology Information Service. Minerva Ginecol. 2018, 70, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Petersen, I.; McCrea, R.L.; Sammon, C.J.; Osborn, D.P.; Evans, S.J.; Cowen, P.J.; Freemantle, N.; Nazareth, I. Risks and benefits of psychotropic medication in pregnancy: Cohort studies based on UK electronic primary care health records. Health Technol. Assess. 2016, 20, 1–176. [Google Scholar] [CrossRef]
- Boyle, B.; Garne, E.; Loane, M.; Addor, M.C.; Arriola, L.; Cavero-Carbonell, C.; Gatt, M.; Lelong, N.; Lynch, C.; Nelen, V.; et al. The changing epidemiology of Ebstein’s anomaly and its relationship with maternal mental health conditions: A European registry-based study. Cardiol. Young 2017, 27, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Frayne, J.; Nguyen, T.; Mok, T.; Hauck, Y.; Liira, H. Lithium exposure during pregnancy: Outcomes for women who attended a specialist antenatal clinic. J. Psychosom. Obs. Gynaecol. 2018, 39, 211–219. [Google Scholar] [CrossRef]
- Molenaar, N.M.; Poels, E.M.P.; Robakis, T.; Wesseloo, R.; Bergink, V. Management of lithium dosing around delivery: An observational study. Bipolar Disord. 2021, 23, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Poels, E.M.P.; Kamperman, A.M.; Bijma, H.H.; Honig, A.; van Kamp, I.L.; Kushner, S.A.; Hoogendijk, W.J.G.; Bergink, V.; White, T. Brain development after intrauterine exposure to lithium: A magnetic resonance imaging study in school-age children. Bipolar Disord. 2023, 25, 181–190. [Google Scholar] [CrossRef]
- Schrijver, L.; Kamperman, A.M.; Bijma, H.; van Kamp, I.L.; Wesseloo, R.; Hoogendijk, W.J.G.; Bergink, V.; Poels, E.M.P. Dose response relationship between lithium serum levels during pregnancy and birth outcomes. Acta Psychiatr. Scand. 2024, 149, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Whaites Heinonen, E.; Tötterman, K.; Bäck, K.; Sarman, I.; Forsberg, L.; Svedenkrans, J. High lithium concentration at delivery is a potential risk factor for adverse outcomes in breastfed infants: A retrospective cohort study. Int. J. Bipolar Disord. 2023, 11, 36. [Google Scholar] [CrossRef]
- Álvarez-Silvares, E.; Fernández-Cruz, T.; Bermudez-González, M.; Rubio-Cid, P.; Almeida, A.; Pinto, E.; Seoane-Pillado, T.; Martínez-Carballo, E. Placental levels of essential and non-essential trace element in relation to neonatal weight in Northwestern Spain: Application of generalized additive models. Environ. Sci. Pollut. Res. Int. 2023, 30, 62566–62578. [Google Scholar] [CrossRef]
- Torfs, M.; Hompes, T.; Ceulemans, M.; Van Calsteren, K.; Vanhole, C.; Smits, A. Early postnatal outcome and care after in utero exposure to lithium: A single center analysis of a Belgian tertiary university hospital. Int. J. Environ. Res. Public. Health 2022, 19, 10111. [Google Scholar] [CrossRef]
- McCrea, R.L.; Nazareth, I.; Evans, S.J.; Osborn, D.P.; Pinfold, V.; Cowen, P.J.; Petersen, I. Lithium prescribing during pregnancy: A UK primary care database study. PLoS ONE 2015, 10, e0121024. [Google Scholar] [CrossRef]
- Volkmann, C.; Bschor, T.; Köhler, S. Lithium treatment over the lifespan in bipolar disorders. Front. Psychiatry 2020, 11, 377. [Google Scholar] [CrossRef] [PubMed]
- Viguera, A.C.; Whitfield, T.; Baldessarini, R.J.; Newport, D.J.; Stowe, Z.; Reminick, A.; Zurick, A.; Cohen, L.S. Risk of recurrence in women with bipolar disorder during pregnancy: Prospective study of mood stabilizer discontinuation. Am. J. Psychiatry 2007, 164, 1817–1824, quiz 1923. [Google Scholar] [CrossRef] [PubMed]
- Baldessarini, R.J.; Tondo, L.; Viguera, A.C. Discontinuing lithium maintenance treatment in bipolar disorders: Risks and implications. Bipolar Disord. 1999, 1, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Broeks, S.C.; Thisted Horsdal, H.; Glejsted Ingstrup, K.; Gasse, C. Psychopharmacological drug utilization patterns in pregnant women with bipolar disorder—A nationwide register-based study. J. Affect. Disord. 2017, 210, 158–165. [Google Scholar] [CrossRef]
- Westin, A.A.; Brekke, M.; Molden, E.; Skogvoll, E.; Aadal, M.; Spigset, O. Changes in drug disposition of lithium during pregnancy: A retrospective observational study of patient data from two routine therapeutic drug monitoring services in Norway. BMJ Open 2017, 7, e015738. [Google Scholar] [CrossRef] [PubMed]
- Wesseloo, R.; Wierdsma, A.I.; van Kamp, I.L.; Munk-Olsen, T.; Hoogendijk, W.J.G.; Kushner, S.A.; Bergink, V. Lithium dosing strategies during pregnancy and the postpartum period. Br. J. Psychiatry 2017, 211, 31–36. [Google Scholar] [CrossRef]
- McKnight, R.F.; Adida, M.; Budge, K.; Stockton, S.; Goodwin, G.M.; Geddes, J.R. Lithium toxicity profile: A systematic review and meta-analysis. Lancet 2012, 379, 721–728. [Google Scholar] [CrossRef]
- Bergink, V.; Kushner, S.A. Lithium during pregnancy. Am. J. Psychiatry 2014, 171, 712–715. [Google Scholar] [CrossRef]
- Park, J.M.; Sridaromont, S.; Ledbetter, E.O.; Terry, W.M. Ebstein’s anomaly of the tricuspid valve associated with prenatal exposure to lithium carbonate. Am J Dis Child 1980, 134, 703–704. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.J.; Payne, V.M. Epidemiology studies on effects of lithium salts in pregnancy are confounded by the inability to control for other potentially teratogenic factors. Hum. Exp. Toxicol. 2024, 43, 9603271241236346. [Google Scholar] [CrossRef]
- Szabo, K.T. Teratogenic effect of lithium carbonate in the foetal mouse. Nature 1970, 225, 73–75. [Google Scholar] [CrossRef] [PubMed]
- Hasgekar, N.N.; Gokhale, P.P.; Amin, M.K.; Seshadri, R.; Lalitha, V.S. Lithium inhibits growth in a murine neural precursor cell line. Cell Biol. Int. 1996, 20, 781–786. [Google Scholar] [CrossRef]
- Szabo, K.T. Teratogenicity of lithium in mice. Lancet 1969, ii, 849. [Google Scholar] [CrossRef] [PubMed]
- Wright, T.L.; Hoffman, L.H.; Davies, J. Teratogenic effects of lithium in rats. Teratology 1971, 4, 151–155. [Google Scholar] [CrossRef]
- Loevy, H.T.; Catchpole, H.R. Lithium ion in cleft palate teratogenesis in CD1 mice. Proc. Soc. Exp. Biol. Med. 1973, 144, 644–646. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.K.; Bratoeva, M.; Mezentseva, N.V.; Bernanke, J.M.; Remond, M.C.; Ramsdell, A.F.; Eisenberg, C.A.; Eisenberg, L.M. Inhibition of heart formation by lithium is an indirect result of the disruption of tissue organization within the embryo. Dev. Growth Differ. 2012, 54, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Van Deun, K.; Hatch, H.; Jacobi, S.; Köhl, W. Lithium carbonate: Updated reproductive and developmental toxicity assessment using scientific literature and guideline compliant studies. Toxicology 2021, 461, 152907. [Google Scholar] [CrossRef] [PubMed]
- Allakhverdiev, V.D.; Smol’nikova, N.M. Toksicheskoe vliianie soleĭ litiia na beremennykh krys i antenatal’noe razvitie ploda Аллахвердиев, В.Д.; Смoльникoва, Н.М. Тoксическoе влияние сoлей лития на беременных крыс и антенатальнoе развитие плoда [Toxic effect of lithium salts on the pregnant rat and on the prenatal development of the fetus]. Farmakol Toksikol (Фармакoл. Тoксикoл.) 1983, 46, 108–110. (In Russian) [Google Scholar] [PubMed]
- Cohen, L.S.; Friedman, J.M.; Jefferson, J.W.; Johnson, E.M.; Weiner, M.L. A reevaluation of risk of in utero exposure to lithium. JAMA 1994, 271, 146–150, Errata corrige: JAMA 1994, 271, 1485. [Google Scholar] [CrossRef]
- Hermann, A.; Gorun, A.; Benudis, A. Lithium use and non-use for pregnant and postpartum women with bipolar disorder. Curr. Psychiatry Rep. 2019, 21, 114. [Google Scholar] [CrossRef] [PubMed]
- Gallitelli, V.; Franco, R.; Guidi, S.; Puri, L.; Parasiliti, M.; Vidiri, A.; Eleftheriou, G.; Perelli, F.; Cavaliere, A.F. Depression treatment in pregnancy: Is it safe, or is it not? Int. J. Environ. Res. Public. Health 2024, 21, 404. [Google Scholar] [CrossRef] [PubMed]
- Becchetti, A.; Whitaker, M. Lithium blocks cell cycle transitions in the first cell cycles of sea urchin embryos, an effect rescued by myo-inositol. Development 1997, 124, 1099–1107. [Google Scholar] [CrossRef]
- Mamdani, F.; Jaitovich Groisman, I.; Alda, M.; Turecki, G. Long-term responsiveness to lithium as a pharmacogenetic outcome variable: Treatment and etiologic implications. Curr. Psychiatry Rep. 2003, 5, 484–492. [Google Scholar] [CrossRef]
- Klug, S.; Collins, M.; Nagao, T.; Merker, H.J.; Neubert, D. Effect of lithium on rat embryos in culture: Growth, development, compartmental distribution and lack of a protective effect of inositol. Arch. Toxicol. 1992, 66, 719–728. [Google Scholar] [CrossRef]
- Klein, P.S.; Melton, D.A. A molecular mechanism for the effect of lithium on development. Proc. Natl. Acad. Sci. USA 1996, 93, 8455–8459. [Google Scholar] [CrossRef] [PubMed]
- Hedgepeth, C.M.; Conrad, L.J.; Zhang, J.; Huang, H.C.; Lee, V.M.; Klein, P.S. Activation of the Wnt signaling pathway: A molecular mechanism for lithium action. Dev. Biol. 1997, 185, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Stambolic, V.; Ruel, L.; Woodgett, J.R. Lithium inhibits glycogen synthase kinase-3 activity and mimics wingless signalling in intact cells. Curr. Biol. 1996, 6, 1664–1668, Errata corrige: Curr. Biol. 1997, 7, 196. [Google Scholar] [CrossRef]
- Yoshida, S.; Marikawa, Y.; Satoh, N. Regulation of the trunk-tail patterning in the ascidian embryo: A possible interaction of cascades between lithium/β-catenin and localized maternal factor pem. Dev. Biol. 1998, 202, 264–279. [Google Scholar] [CrossRef]
- Nery, L.R.; Eltz, N.S.; Martins, L.; Guerim, L.D.; Pereira, T.C.; Bogo, M.R.; Vianna, M.R. Sustained behavioral effects of lithium exposure during early development in zebrafish: Involvement of the Wnt-β-catenin signaling pathway. Prog. Neuropsychopharmacol. Biol. Psychiatry 2014, 55, 101–108. [Google Scholar] [CrossRef]
- Yang, Y.; Yang, J.; Liu, R.; Li, H.; Luo, X.; Yang, G. Accumulation of β-catenin by lithium chloride in porcine myoblast cultures accelerates cell differentiation. Mol. Biol. Rep. 2011, 38, 2043–2049. [Google Scholar] [CrossRef]
- Cooke, J.; Smith, E.J. The restrictive effect of early exposure to lithium upon body pattern in Xenopus development, studied by quantitative anatomy and immunofluorescence. Development 1988, 102, 85–99. [Google Scholar] [CrossRef] [PubMed]
- Cooke, J.; Symes, K.; Smith, E.J. Potentiation by the lithium ion of morphogenetic responses to a Xenopus inducing factor. Development 1989, 105, 549–558. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.L.; Moody, S.A. Lithium changes the ectodermal fate of individual frog blastomeres because it causes ectopic neural plate formation. Development 1989, 106, 599–610. [Google Scholar] [CrossRef] [PubMed]
- Newport, D.J.; Viguera, A.C.; Beach, A.J.; Ritchie, J.C.; Cohen, L.S.; Stowe, Z.N. Lithium placental passage and obstetrical outcome: Implications for clinical management during late pregnancy. Am. J. Psychiatry 2005, 162, 2162–2170. [Google Scholar] [CrossRef] [PubMed]
- Chiou, S.Y.-S.; Kysenius, K.; Huang, Y.; Habgood, M.D.; Koehn, L.M.; Qiu, F.; Crouch, P.J.; Varshney, S.; Ganio, K.; Dziegielewska, K.M.; et al. Lithium administered to pregnant, lactating and neonatal rats: Entry into developing brain. Fluids Barriers CNS 2021, 18, 57. [Google Scholar] [CrossRef] [PubMed]
- Alimonti, A.; Bocca, B.; Mannella, E.; Petrucci, F.; Zennaro, F.; Cotichini, R.; D’Ippolito, C.; Agresti, A.; Caimi, S.; Forte, G. Assessment of reference values for selected elements in a healthy urban population. Ann. Ist. Super. Sanità 2005, 41, 181–187. Available online: https://www.iss.it/documents/20126/955767/412181.1129882917.pdf/56f44c85-3bf9-9581-1e11-0f3da9a015fd?t=1575579939108 (accessed on 8 April 2024). [PubMed]
- Zarse, K.; Terao, T.; Tian, J.; Iwata, N.; Ishii, N.; Ristow, M. Low-dose lithium uptake promotes longevity in humans and metazoans. Eur. J. Nutr. 2011, 50, 387–389. [Google Scholar] [CrossRef] [PubMed]
- Kapusta, N.D.; Mossaheb, N.; Etzersdorfer, E.; Hlavin, G.; Thau, K.; Willeit, M.; Praschak-Rieder, N.; Sonneck, G.; Leithner-Dziubas, K. Lithium in drinking water and suicide mortality. Br. J. Psychiatry 2011, 198, 346–350. [Google Scholar] [CrossRef] [PubMed]
- Harari, F.; Langeén, M.; Casimiro, E.; Bottai, M.; Palm, B.; Nordqvist, H.; Vahter, M. Environmental exposure to lithium during pregnancy and fetal size: A longitudinal study in the Argentinean Andes. Environ. Int. 2015, 77, 48–54. [Google Scholar] [CrossRef]
- Wei, L.; Huang, H.; Chen, X.; Wang, X.; Zhang, R.; Su, L.; Duan, W.; Rahman, M.; Golam Mostofa, M.; Qamruzzaman, Q.; et al. Umbilical cord serum elementomics of 52 trace elements and early childhood neurodevelopment: Evidence from a prospective birth cohort in rural Bangladesh. Environ. Int. 2022, 166, 107370. [Google Scholar] [CrossRef]
- Montori, V.M.; Smieja, M.; Guyatt, G.H. Publication bias: A brief review for clinicians. Mayo Clin. Proc. 2000, 75, 1284–1288. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Callovini, T.; Montanari, S.; Bardi, F.; Barbonetti, S.; Rossi, S.; Caso, R.; Mandracchia, G.; Margoni, S.; Brugnami, A.; Paolini, M.; et al. Obstetric Outcomes in Women on Lithium: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 4872. https://doi.org/10.3390/jcm13164872
Callovini T, Montanari S, Bardi F, Barbonetti S, Rossi S, Caso R, Mandracchia G, Margoni S, Brugnami A, Paolini M, et al. Obstetric Outcomes in Women on Lithium: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2024; 13(16):4872. https://doi.org/10.3390/jcm13164872
Chicago/Turabian StyleCallovini, Tommaso, Silvia Montanari, Francesca Bardi, Sara Barbonetti, Sara Rossi, Romina Caso, Giuseppe Mandracchia, Stella Margoni, Andrea Brugnami, Marco Paolini, and et al. 2024. "Obstetric Outcomes in Women on Lithium: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 13, no. 16: 4872. https://doi.org/10.3390/jcm13164872
APA StyleCallovini, T., Montanari, S., Bardi, F., Barbonetti, S., Rossi, S., Caso, R., Mandracchia, G., Margoni, S., Brugnami, A., Paolini, M., Manfredi, G., Giudice, L. L., Segatori, D., Zanzarri, A., Onori, L., Calderoni, C., Benini, E., Marano, G., Massetti, M., ... Mazza, M. (2024). Obstetric Outcomes in Women on Lithium: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 13(16), 4872. https://doi.org/10.3390/jcm13164872











