Effect of Inter-Hospital Transfer on Mortality in Patients Admitted through the Emergency Department
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
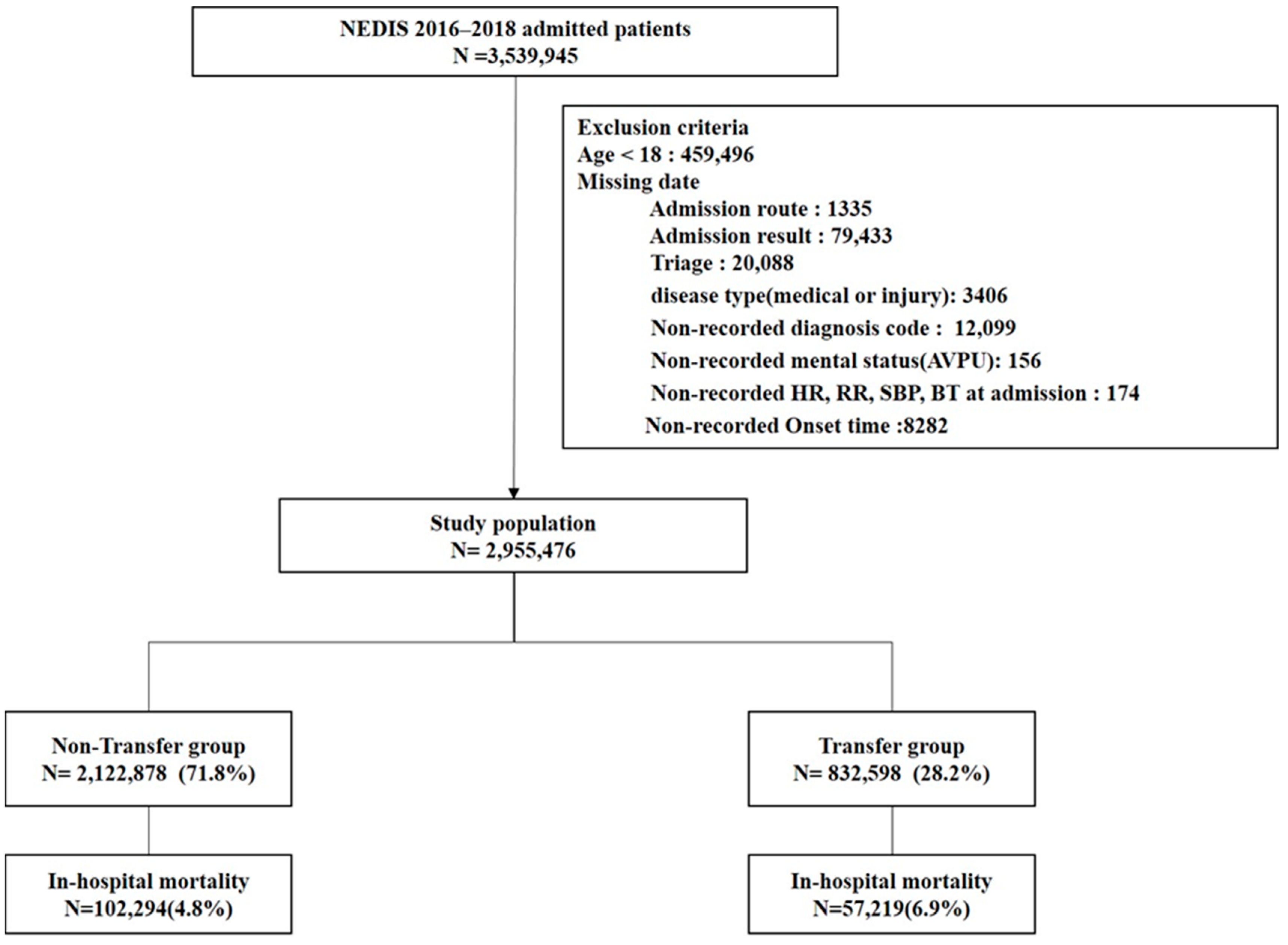
2.2. Selection of Study Patients
2.3. Data Analysis and Outcome
2.4. Statistical Analysis
3. Results
3.1. Study Population and Outcomes
3.2. Comparison of the Basic Characteristics According to Study Groups (Transfer Group vs. Non-Transfer Group) and Outcome (Survivor Group and Non-Survivor Group)
3.3. Multiple Logistic Regression Analysis for In-Hospital Mortality
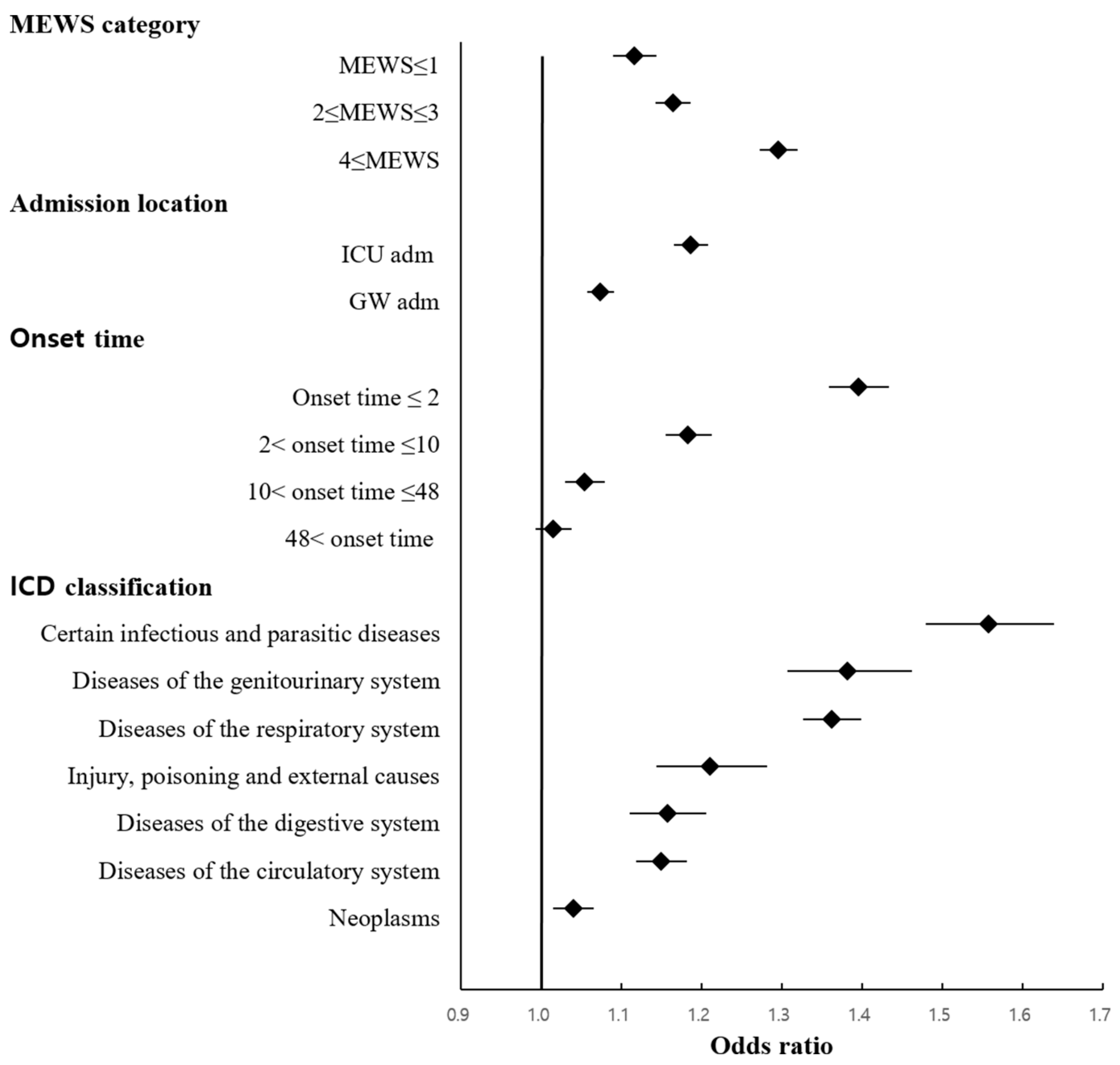
3.4. Sub-Analyses Based on MEWS, ICU Admission, Onset Time, Diagnostic Classification
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yoo, H.H.; Ro, Y.S.; Ko, E.; Lee, J.H.; Han, S.H.; Kim, T.; Shin, T.G.; Kim, S.; Chang, H. Epidemiologic trends of patients who visited nationwide emergency departments: A report from the National Emergency Department Information System (NEDIS) of Korea, 2018–2022. Clin. Exp. Emerg. Med. 2023, 10, S1–S12. [Google Scholar] [CrossRef] [PubMed]
- Westfall, J.M.; Kiefe, C.I.; Weissman, N.W.; Goudie, A.; Centor, R.M.; Williams, O.D.; Allison, J.J. Does interhospital transfer improve outcome of acute myocardial infarction? A propensity score analysis from the Cardiovascular Cooperative Project. BMC Cardiovasc. Disord. 2008, 8, 22. [Google Scholar] [CrossRef]
- Mueller, S.; Zheng, J.; Orav, E.J.; Schnipper, J.L. Inter-hospital transfer and patient outcomes: A retrospective cohort study. BMJ Qual. Saf. 2019, 28, e1. [Google Scholar] [CrossRef] [PubMed]
- Faine, B.A.; Noack, J.M.; Wong, T.; Messerly, J.T.; Ahmed, A.; Fuller, B.M.; Mohr, N.M. Interhospital Transfer Delays Appropriate Treatment for Patients with Severe Sepsis and Septic Shock: A Retrospective Cohort Study. Crit. Care Med. 2015, 43, 2589–2596. [Google Scholar] [CrossRef]
- Subbe, C.P.; Kruger, M.; Rutherford, P.; Gemmel, L. Validation of a modified Early Warning Score in medical admissions. QJM Mon. J. Assoc. Physicians 2001, 94, 521–526. [Google Scholar] [CrossRef]
- Ranasinghe, I.; Barzi, F.; Brieger, D.; Gallagher, M. Long-term mortality following interhospital transfer for acute myocardial infarction. Heart Br. Card. Soc. 2015, 101, 1032–1040. [Google Scholar] [CrossRef] [PubMed]
- Dharma, S.; Dakota, I.; Andriantoro, H.; Firdaus, I.; Anandira, C.P.; Radi, B. Interhospital Transfer versus Direct Admission in Patients with Acute ST-Segment Elevation Myocardial Infarction. Int. J. Angiol. 2023, 32, 121–127. [Google Scholar] [CrossRef]
- Sakowitz, S.; Bakhtiyar, S.S.; Gao, Z.; Mallick, S.; Vadlakonda, A.; Coaston, T.; Balian, J.; Chervu, N.; Benharash, P. Interhospital Transfer for Emergency General Surgery: A Contemporary National Analysis. Am. Surg. 2024, 31348241244642. [Google Scholar] [CrossRef]
- Emanuelson, R.D.; Brown, S.J.; Termuhlen, P.M. Interhospital transfer (IHT) in emergency general surgery patients (EGS): A scoping review. Surg. Open Sci. 2022, 9, 69–79. [Google Scholar] [CrossRef]
- Pomponio, M.K.; Khan, I.S.; Evans, L.T.; Simmons, N.E.; Ball, P.A.; Ryken, T.C.; Hong, J. Association between interhospital transfer and increased in-hospital mortality in patients with spinal epidural abscesses. Spine J. Off. J. N. Am. Spine Soc. 2022, 22, 921–926. [Google Scholar] [CrossRef]
- Hill, A.D.; Fowler, R.A.; Nathens, A.B. Impact of interhospital transfer on outcomes for trauma patients: A systematic review. J. Trauma 2011, 71, 1885–1900; discussion 1901. [Google Scholar] [CrossRef] [PubMed]
- Tseng, Y.H.; Kao, C.C.; Lin, C.C.; Chen, C.W.; Lu, M.S.; Lu, C.H.; Huang, Y.K. Does Interhospital Transfer Influence the Outcomes of Patients Receiving Surgery for Acute Type A Aortic Dissection? Type A Aortic Dissection: Is Transfer Hazardous or Beneficial? Emerg. Med. Int. 2019, 2019, 5692083. [Google Scholar] [CrossRef] [PubMed]
- Kitchlu, A.; Shapiro, J.; Slater, J.; Brimble, K.S.; Dirk, J.S.; Jeyakumar, N.; Dixon, S.N.; Garg, A.X.; Harel, Z.; Harvey, A.; et al. Interhospital Transfer and Outcomes in Patients with AKI: A Population-Based Cohort Study. Kidney360 2020, 1, 1195–1205. [Google Scholar] [CrossRef]
- Baig, S.H.; Gorth, D.J.; Yoo, E.J. Critical Care Utilization and Outcomes of Interhospital Medical Transfers at Lower Risk of Death. J. Intensive Care Med. 2022, 37, 679–685. [Google Scholar] [CrossRef]
- Sokol-Hessner, L.; White, A.A.; Davis, K.F.; Herzig, S.J.; Hohmann, S.F. Interhospital transfer patients discharged by academic hospitalists and general internists: Characteristics and outcomes. J. Hosp. Med. 2016, 11, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Durairaj, L.; Will, J.G.; Torner, J.C.; Doebbeling, B.N. Prognostic factors for mortality following interhospital transfers to the medical intensive care unit of a tertiary referral center. Crit. Care Med. 2003, 31, 1981–1986. [Google Scholar] [CrossRef]
- Teng, C.Y.; Davis, B.S.; Rosengart, M.R.; Carley, K.M.; Kahn, J.M. Assessment of Hospital Characteristics and Interhospital Transfer Patterns of Adults with Emergency General Surgery Conditions. JAMA Netw. Open 2021, 4, e2123389. [Google Scholar] [CrossRef]
- Ofoma, U.R.; Dahdah, J.; Kethireddy, S.; Maeng, D.; Walkey, A.J. Case Volume-Outcomes Associations Among Patients with Severe Sepsis Who Underwent Interhospital Transfer. Crit. Care Med. 2017, 45, 615–622. [Google Scholar] [CrossRef]
- Mueller, S.K.; Fiskio, J.; Schnipper, J. Interhospital Transfer: Transfer Processes and Patient Outcomes. J. Hosp. Med. 2019, 14, 486–491. [Google Scholar] [CrossRef]
- Murshed, I.; Gupta, A.K.; Camilos, A.N.; Sabab, A.; Bacchi, S.; Kovoor, J.G.; Chan, J.C.Y.; Maddern, G.J. Surgical interhospital transfer mortality: National analysis. Br. J. Surg. 2023, 110, 591–598. [Google Scholar] [CrossRef]
- Nacht, J.; Macht, M.; Ginde, A.A. Interhospital transfers from U.S. emergency departments: Implications for resource utilization, patient safety, and regionalization. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2013, 20, 888–893. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total N = 2,955,476 | Transfer Group N = 832,598 (28.2%) | Non-Transfer Group N = 2,122,878 (71.8%) | p-Value |
|---|---|---|---|---|
| Age (year ± SD) | 60.92 ± 18.5 | 62.84 ± 18.5 | 60.16 ± 18.4 | <0.001 |
| Age (year), median (IQR) | 63 (48–76) | 66 (51–78) | 62 (48–75) | <0.001 |
| Sex, male, n (%) | 1,574,549 (53.3) | 444,651 (53.4) | 1,129,898 (53.2) | 0.005 |
| Insurance type—medical aid, n (%) | 257,892 (8.7) | 75,769 (9.1) | 182,123 (8.6) | <0.001 |
| Disease type, injury (%) | 539,576 (18.3) | 131,775 (15.8) | 407,801 (19.2) | <0.001 |
| KTAS, n (%) | <0.001 | |||
| 1 | 74,307 (2.5) | 25,984 (3.1) | 48,323 (2.3) | |
| 2 | 454,484 (15.4) | 155,089 (18.6) | 299,395 (14.1) | |
| 3 | 1,571,340 (53.2) | 477,616 (57.4) | 1,093,724 (51.5) | |
| 4 | 758,818 (25.7) | 152,424 (18.3) | 606,394 (28.6) | |
| 5 | 96,527 (3.3) | 21,485 (2.6) | 75,042 (3.5) | |
| Classification of emergency medical center, n (%) | <0.001 | |||
| Regional emergency medical center | 1,069,842 (36.2) | 378,002 (45.4) | 691,840 (32.6) | |
| Local emergency medical center | 1,885,634 (63.8) | 454,596 (54.6) | 1,431,038 (67.4) | |
| Modified Early Warning Score—SBP (mmHg), n (%) | <0.001 | |||
| 0 (101 ≤ SBP ≤ 199) | 2,504,048 (84.7) | 695,080 (83.5) | 1,808,968 (85.2) | |
| 1 (81 ≤ SBP ≤ 100) | 292,546 (9.9) | 92,783 (11.1) | 199,763 (9.4) | |
| 2 (71 ≤ SBP ≤ 80 or ≥200) | 118,115 (4.0) | 33,278 (4.0) | 84,837 (4.0) | |
| 3 (SBP < 70) | 40,767 (1.4) | 11,457 (1.4) | 29,310 (1.4) | |
| Modified Early Warning Score—HR (rate/min), n (%) | <0.001 | |||
| 0 (51 ≤ HR ≤ 100) | 2,223,667 (75.2) | 629,128 (75.6) | 1,594,539 (75.1) | |
| 1 (41 ≤ HR ≤ 50 or 101 ≤ HR ≤ 110) | 324,285 (11.0) | 96,084 (11.5) | 228,201 (10.7) | |
| 2 (111 ≤ HR ≤ 129 or HR < 40) | 307,617 (10.4) | 81,172 (9.7) | 226,445 (10.7) | |
| 3 (HR ≥ 130) | 99,907 (3.4) | 26,214 (3.1) | 73,693 (3.5) | |
| Modified Early Warning Score—RR (rate/min), n (%) | <0.001 | |||
| 0 (9 ≤ RR ≤ 14) | 47,861 (1.6) | 16,489 (2.0) | 31,372 (1.5) | |
| 1 (15 ≤ RR ≤ 20) | 2,417,676 (81.8) | 666,434 (80.0) | 1,751,242 (82.5) | |
| 2 (21 ≤ RR ≤ 29 or RR < 9) | 429,021 (14.5) | 133,162 (16.0) | 295,859 (13.9) | |
| 3 (RR ≥ 30) | 60,918 (2.1) | 16,513 (2.0) | 44,405 (2.1) | |
| Modified Early Warning Score—Temperature, T (°C), n (%) | ||||
| 0 (35 ≤ T ≤ 38.4) | 2,753,402 (93.2) | 796,036 (95.6) | 1,957,366 (92.2) | |
| 2 (T ≥ 38.5 or T < 35) | 202,074 (6.8) | 36,562 (4.4) | 165,512 (7.8) | |
| Modified Early Warning Score—AVPU score, n (%) | <0.001 | |||
| Alert (A) | 2,696,346 (91.2) | 736,775 (88.5) | 1,959,571 (92.3) | |
| Reacting to voice (V) | 131,688 (4.5) | 47,981 (5.8) | 83,707 (3.9) | |
| Reacting to Pain (P) | 99,390 (3.4) | 38,293 (4.6) | 61,097 (2.9) | |
| Unresponsive (U) | 28,052 (0.9) | 9549 (1.1) | 18,503 (0.9) | |
| Onset time (Interval from onset of symptom to admission at ED) (hour), median (IQR), n (%) | 10 (2–48) | 22 (5–72) | 7 (2–38) | <0.001 |
| Onset time (Interval from onset of symptom to admission at ED) (hour, IQR) | <0.001 | |||
| Onset time ≤ 2 | 814,951 (27.6) | 96,015 (11.5) | 718,936 (33.9) | |
| 2 < onset time ≤ 10 | 693,418 (23.5) | 232,577 (27.9) | 460,841 (21.7) | |
| 10 < onset time ≤ 48 | 753,402 (25.5) | 243,565 (29.3) | 509,837 (24.0) | |
| 48 < onset time | 693,705 (23.5) | 260,441 (31.3) | 433,264 (20.4) | |
| ED LOS (hour), median (IQR), n (%) | 4.17 (2.40–7.73) | 4.5 (2.6–8.4) | 4.0 (2.4–7.5) | <0.001 |
| Hospital day (day), median (IQR), n (%) | 6 (3–13) | 7 (3–15) | 5 (2–12) | <0.001 |
| ICU admission N, (%) | 512,723 (17.3) | 191,768 (23.0) | 320,955 (15.1) | <0.001 |
| In-hospital mortality N, (%) | 159,513 (5.4) | 57,219 (6.9) | 102,294 (4.8) | <0.001 |
| Variable | Total N = 2,955,476 | Survivor Group N = 2,795,963 (94.6) | Non-Survivor Group N = 159,513 (5.4) | p-Value |
|---|---|---|---|---|
| Age (year ± SD) | 62.98 ± 17.8 | 60.34 ± 18.5 | 71.09 ± 14.1 | <0.001 |
| Age (year), median (IQR) | 63 (48–76) | 62 (48–76) | 74 (62–81) | |
| Sex, male, n (%) | 1,574,549 (53.3) | 1,478,706 (52.9) | 95,843 (60.1) | <0.001 |
| Insurance type—medical aid, n (%) | 257,892 (8.7) | 239,608 (8.6) | 18,284 (11.5) | <0.001 |
| Disease type, injury, n (%) | 539,576 (18.3) | 527,411 (18.9) | 12,165 (7.6) | <0.001 |
| KTAS, n (%) | <0.001 | |||
| 1 | 74,307 (2.5) | 51,078 (1.8) | 23,229 (14.6) | |
| 2 | 454,484 (15.4) | 409,693 (14.7) | 44,791 (28.1) | |
| 3 | 1,571,340 (53.2) | 1,500,353 (53.7) | 70,987 (44.5) | |
| 4 | 758,818 (25.7) | 741,630 (26.5) | 17,188 (10.8) | |
| 5 | 96,527 (3.3) | 93,209 (3.3) | 3318 (2.1) | |
| Classification of emergency medical center, n (%) | <0.001 | |||
| Regional emergency medical center | 1,069,842 (36.2) | 1,009,838 (36.1) | 60,004 (37.6) | |
| Local emergency medical center | 1,885,634 (63.8) | 1,786,125 (63.9) | 99,509 (62.4) | |
| Onset time (Interval from onset of symptom to admission at ED) (hour), median (IQR) | 10 (2–48) | 10 (2–48) | 9 (2–48) | |
| Onset time (Interval from onset of symptom to admission at ED) (hour, IQR) | <0.001 | |||
| Onset time ≤ 2 | 814,951 (27.6) | 768,352 (27.5) | 46,599 (29.2) | |
| 2 < onset time ≤ 10 | 693,418 (23.5) | 656,960 (23.5) | 36,458 (22.9) | |
| 10 < onset time ≤ 48 | 753,402 (25.5) | 716,178 (25.6) | 37,224 (23.3) | |
| 48 < onset time | 693,705 (23.5) | 654,473 (23.4) | 39,232 (24.6) | |
| ED LOS (hour), median (IQR) | 4.17 (2.40–7.73) | 4.13 (2.40–7.65) | 4.75 (2.66–9.27) | <0.001 |
| Hospital day (day), median (IQR) | 6 (3–13) | 6 (3–12) | 8 (2–20) | <0.001 |
| ICU admission, n (%) | 512,723 (17.3) | 439,224 (15.7) | 73,499 (46.1) | <0.001 |
| Inter-hospital transfer, n (%) | <0.001 | |||
| Yes | 832,598 (28.2) | 775,379 (27.7) | 57,219 (35.9) | |
| No | 2,122,878 (71.8) | 2,020,584 (72.3) | 102,294 (64.1) |
| Variable | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | p-Value | OR | 95%CI | p-Value | |
| Age(year) | 1.039 | 1.038–1.039 | <0.001 | 1.034 | 1.033–1.034 | <0.001 |
| Sex, male | 1.341 | 1.327–1.355 | <0.001 | 1.442 | 1.426–1.458 | <0.001 |
| Insurance type-medical aid | 1.381 | 1.359–1.403 | <0.001 | 1.074 | 1.055–1.092 | <0.001 |
| Disease type, n (%) | ||||||
| Medical | 2.816 | 2.764–2.869 | <0.001 | 1.912 | 1.874–1.952 | <0.001 |
| injury | 1.00 | - | - | |||
| ICU admission | 4.585 | 4.538–4.633 | <0.001 | 2.154 | 2.128–2.181 | <0.001 |
| Onset time (Interval from onset of symptom to admission at ED) (hour, IQR) | ||||||
| Onset time ≤ 2 | 1.012 | 0.998–1.026 | 0.098 | 0.684 | 0.673–0.696 | <0.001 |
| 2 < onset time ≤ 10 | 0.926 | 0.912–0.939 | <0.001 | 0.753 | 0.723–0.747 | <0.001 |
| 10 < onset time ≤ 48 | 0.867 | 0.855–0.880 | <0.001 | 0.816 | 0.803–0.828 | <0.001 |
| 48 < onset time | 1.00 | - | - | |||
| Inter-hospital transfer | ||||||
| Yes | 1.458 | 1.442–1.473 | <0.001 | 1.114 | 1.101–1.128 | <0.001 |
| No | 1.00 | - | - | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, J.-J.; Lee, S.-J.; Song, J.-H.; Lee, S.-W.; Kim, S.-J.; Han, K.-S. Effect of Inter-Hospital Transfer on Mortality in Patients Admitted through the Emergency Department. J. Clin. Med. 2024, 13, 4944. https://doi.org/10.3390/jcm13164944
Song J-J, Lee S-J, Song J-H, Lee S-W, Kim S-J, Han K-S. Effect of Inter-Hospital Transfer on Mortality in Patients Admitted through the Emergency Department. Journal of Clinical Medicine. 2024; 13(16):4944. https://doi.org/10.3390/jcm13164944
Chicago/Turabian StyleSong, Jei-Joon, Si-Jin Lee, Ju-Hyun Song, Sung-Woo Lee, Su-Jin Kim, and Kap-Su Han. 2024. "Effect of Inter-Hospital Transfer on Mortality in Patients Admitted through the Emergency Department" Journal of Clinical Medicine 13, no. 16: 4944. https://doi.org/10.3390/jcm13164944





