Mid-Term Clinical and Radiographic Results of Complex Hip Revision Arthroplasty Based on 3D Life-Sized Model: A Prospective Case Series
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol
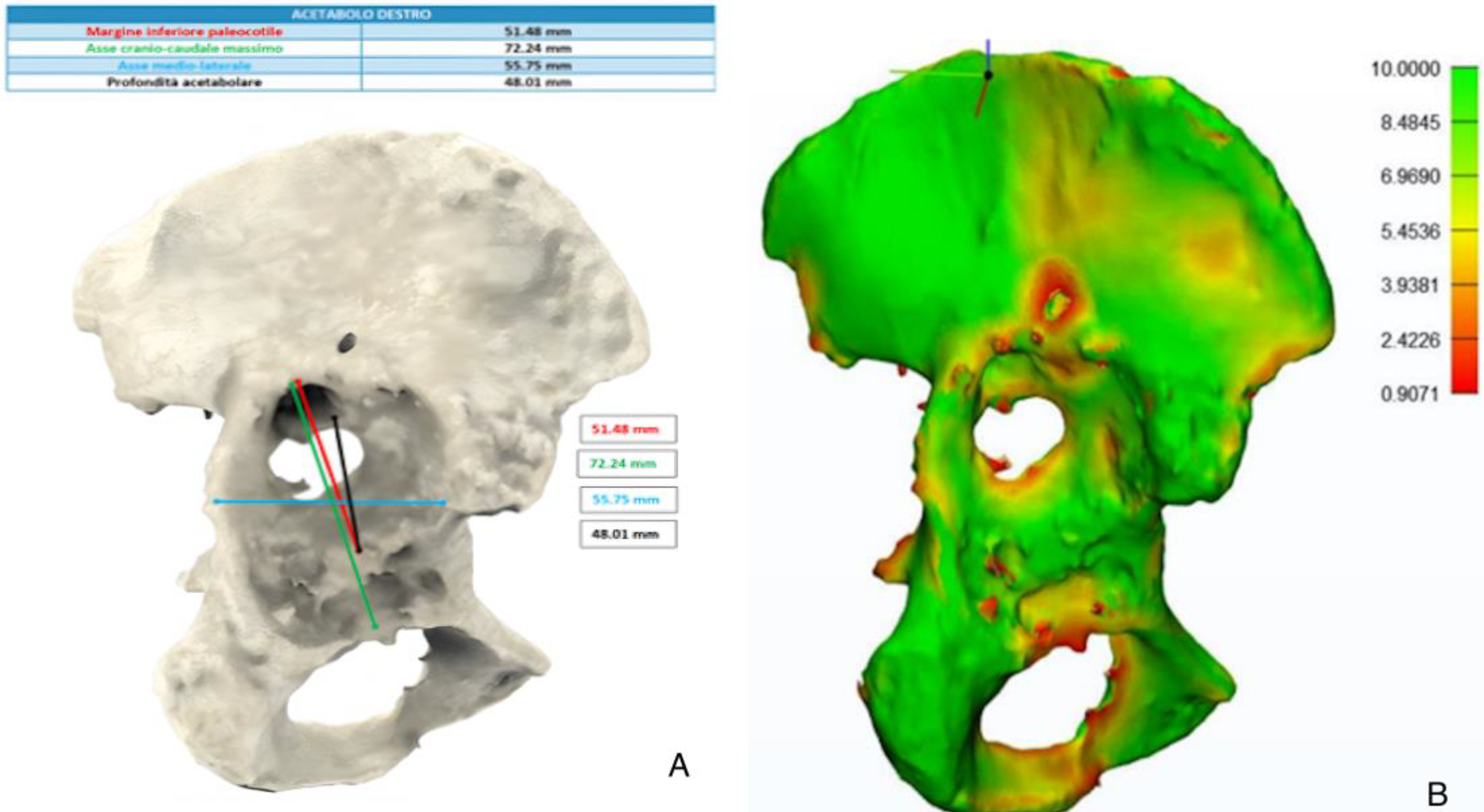
2.2. Design of 3D Models
2.3. Statistical Analysis
3. Results
3.1. Demographics
3.2. Clinical and Radiographic Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Andrzejewski, K.; Domżalski, M.; Komorowski, P.; Poszepczyński, J.; Rokita, B.; Elgalal, M. Optimization of Revision Hip Arthroplasty Workflow by Means of Detailed Pre-Surgical Planning Using Computed Tomography Data, Open-Source Software and Three-Dimensional-Printed Models. Diagnostics 2023, 13, 2516. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-W.; Won, S.-H.; Moon, S.-Y.; Lee, Y.-K.; Ha, Y.-C.; Koo, K.-H. Burden and Future Projection of Revision Total Hip Arthroplasty in South Korea. BMC Musculoskelet. Disord. 2021, 22, 375. [Google Scholar] [CrossRef]
- Karachalios, T.; Komnos, G.; Koutalos, A. Total Hip Arthroplasty: Survival and Modes of Failure. EFORT Open Rev. 2018, 3, 232–239. [Google Scholar] [CrossRef]
- Bücking, T.M.; Hill, E.R.; Robertson, J.L.; Maneas, E.; Plumb, A.A.; Nikitichev, D.I. From Medical Imaging Data to 3D Printed Anatomical Models. PLoS ONE 2017, 12, e0178540. [Google Scholar] [CrossRef]
- Goh, G.D.; Sing, S.L.; Lim, Y.F.; Thong, J.L.J.; Peh, Z.K.; Mogali, S.R.; Yeong, W.Y. Machine Learning for 3D Printed Multi-Materials Tissue-Mimicking Anatomical Models. Mater. Des. 2021, 211, 110125. [Google Scholar] [CrossRef]
- Duan, X.; Wang, B.; Yang, L.; Kadakia, A.R. Applications of 3D Printing Technology in Orthopedic Treatment. BioMed Res. Int. 2021, 2021, 9892456. [Google Scholar] [CrossRef]
- Segaran, N.; Saini, G.; Mayer, J.L.; Naidu, S.; Patel, I.; Alzubaidi, S.; Oklu, R. Application of 3D Printing in Preoperative Planning. J. Clin. Med. 2021, 10, 917. [Google Scholar] [CrossRef]
- Zhang, H.; Guan, J.; Zhang, Z.; Chen, X.; Ma, X.; Zhao, J.; Zhou, J. Restoring Rotation Center in Total Hip Arthroplasty for Developmental Dysplasia of the Hip with the Assistance of Three Dimensional Printing Technology: A Pilot Study. Orthop. Surg. 2022, 14, 119–128. [Google Scholar] [CrossRef]
- Yu, A.W.; Duncan, J.M.; Daurka, J.S.; Lewis, A.; Cobb, J. A Feasibility Study into the Use of Three-Dimensional Printer Modelling in Acetabular Fracture Surgery. Adv. Orthop. 2015, 2015, 617046. [Google Scholar] [CrossRef]
- Small, T.; Krebs, V.; Molloy, R.; Bryan, J.; Klika, A.K.; Barsoum, W.K. Comparison of Acetabular Shell Position Using Patient Specific Instruments vs. Standard Surgical Instruments: A Randomized Clinical Trial. J. Arthroplast. 2014, 29, 1030–1037. [Google Scholar] [CrossRef]
- Liang, H.; Ji, T.; Zhang, Y.; Wang, Y.; Guo, W. Reconstruction with 3D-Printed Pelvic Endoprostheses after Resection of a Pelvic Tumour. Bone Jt. J. 2017, 99-B, 267–275. [Google Scholar] [CrossRef]
- La Camera, F.; Loppini, M.; Della Rocca, A.; de Matteo, V.; Grappiolo, G. Total Hip Arthroplasty with a Monoblock Conical Stem in Dysplastic Hips: A 20-Year Follow-Up Study. J. Arthroplast. 2020, 35, 3242–3248. [Google Scholar] [CrossRef]
- Javan, R.; Ellenbogen, A.L.; Greek, N.; Haji-Momenian, S. A Prototype Assembled 3D-Printed Phantom of the Glenohumeral Joint for Fluoroscopic-Guided Shoulder Arthrography. Skeletal Radiol. 2019, 48, 791–802. [Google Scholar] [CrossRef]
- Paprosky, W.G.; Perona, P.G.; Lawrence, J.M. Acetabular Defect Classification and Surgical Reconstruction in Revision Arthroplasty. A 6-Year Follow-up Evaluation. J. Arthroplast. 1994, 9, 33–44. [Google Scholar] [CrossRef]
- Sporer, S.M.; Paprosky, W.G. Acetabular Revision Using a Trabecular Metal Acetabular Component for Severe Acetabular Bone Loss Associated with a Pelvic Discontinuity. J. Arthroplast. 2006, 21, 87–90. [Google Scholar] [CrossRef]
- Ranawat, C.S.; Dorr, L.D.; Inglis, A.E. Total Hip Arthroplasty in Protrusio Acetabuli of Rheumatoid Arthritis. J. Bone Joint Surg. Am. 1980, 62, 1059–1065. [Google Scholar] [PubMed]
- DeLee, J.G.; Charnley, J. Radiological Demarcation of Cemented Sockets in Total Hip Replacement. Clin. Orthop. 1976, 121, 20–32. [Google Scholar]
- Weeden, S.H.; Schmidt, R.H. The Use of Tantalum Porous Metal Implants for Paprosky 3A and 3B Defects. J. Arthroplast. 2007, 22, 151–155. [Google Scholar] [CrossRef]
- Sporer, S.M.; Paprosky, W.G. The Use of a Trabecular Metal Acetabular Component and Trabecular Metal Augment for Severe Acetabular Defects. J. Arthroplast. 2006, 21, 83–86. [Google Scholar] [CrossRef]
- Brooker, A.F.; Bowerman, J.W.; Robinson, R.A.; Riley, L.H. Ectopic Ossification Following Total Hip Replacement. Incidence and a Method of Classification. J. Bone Joint Surg. Am. 1973, 55, 1629–1632. [Google Scholar]
- Fehring, K.A.; Howe, B.M.; Martin, J.R.; Taunton, M.J.; Berry, D.J. Preoperative Evaluation for Pelvic Discontinuity Using a New Reformatted Computed Tomography Scan Protocol. J. Arthroplast. 2016, 31, 2247–2251. [Google Scholar] [CrossRef]
- Berhouet, J.; Samargandi, R. Emerging Innovations in Preoperative Planning and Motion Analysis in Orthopedic Surgery. Diagnostics 2024, 14, 1321. [Google Scholar] [CrossRef] [PubMed]
- Berry, D.J.; Lewallen, D.G.; Hanssen, A.D.; Cabanela, M.E. Pelvic Discontinuity in Revision Total Hip Arthroplasty. J. Bone Joint Surg. Am. 1999, 81, 1692–1702. [Google Scholar] [CrossRef] [PubMed]
- Sporer, S.M.; O’Rourke, M.; Paprosky, W.G. The Treatment of Pelvic Discontinuity during Acetabular Revision. J. Arthroplast. 2005, 20, 79–84. [Google Scholar] [CrossRef]
- Abdelnasser, M.K.; Klenke, F.M.; Whitlock, P.; Khalil, A.M.; Khalifa, Y.E.; Ali, H.M.; Siebenrock, K.A. Management of Pelvic Discontinuity in Revision Total Hip Arthroplasty: A Review of the Literature. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2015, 25, 120–126. [Google Scholar] [CrossRef]
- Aprato, A.; Olivero, M.; Iannizzi, G.; Bistolfi, A.; Sabatini, L.; Masse, A. Pelvic Discontinuity in Acetabular Revisions: Does CT Scan Overestimate It? A Comparative Study of Diagnostic Accuracy of 3D-Modeling and Traditional 3D CT Scan. Musculoskelet. Surg. 2020, 104, 171–177. [Google Scholar] [CrossRef]
- Tu, Q.; Ding, H.-W.; Chen, H.; Shen, J.-J.; Miao, Q.-J.; Liu, B.; Yu, G.-W.; Huang, X.-H.; Zhu, C.-R.; Tang, Y.; et al. Preliminary Application of 3D-Printed Individualised Guiding Templates for Total Hip Arthroplasty in Crowe Type IV Developmental Dysplasia of the Hip. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2022, 32, 334–344. [Google Scholar] [CrossRef]
- Li, Q.; Chen, X.; Lin, B.; Ma, Y.; Liao, J.X.; Zheng, Q. Three-Dimensional Technology Assisted Trabecular Metal Cup and Augments Positioning in Revision Total Hip Arthroplasty with Complex Acetabular Defects. J. Orthop. Surg. 2019, 14, 431. [Google Scholar] [CrossRef]
- Ballard, D.H.; Mills, P.; Duszak, R.; Weisman, J.A.; Rybicki, F.J.; Woodard, P.K. Medical 3D Printing Cost-Savings in Orthopedic and Maxillofacial Surgery: Cost Analysis of Operating Room Time Saved with 3D Printed Anatomic Models and Surgical Guides. Acad. Radiol. 2020, 27, 1103–1113. [Google Scholar] [CrossRef]
- Smith, C.F.; Tollemache, N.; Covill, D.; Johnston, M. Take Away Body Parts! An Investigation into the Use of 3D-Printed Anatomical Models in Undergraduate Anatomy Education. Anat. Sci. Educ. 2018, 11, 44–53. [Google Scholar] [CrossRef]



| Case Number | Shell Diameter (mm) | Augment | Insert | Stem Revision | Bone Graft | Cage | Bioball | Previous Surgeries (n°) |
|---|---|---|---|---|---|---|---|---|
| 1 | 60 | No | Avantage | No | No | No | No | 3 |
| 2 | 52 | No | E-Poly | Yes | No | No | No | 2 |
| 3 | 56 | No | Avantage | Yes | No | No | No | 3 |
| 4 | 58 | Yes | E-Poly | Yes | No | No | No | 4 |
| 5 | 66 | Yes | E-Poly | No | Yes | No | No | 4 |
| 6 | 56 | No | Avantage | Yes | No | No | No | 2 |
| 7 | 66 | No | Avantage | No | Yes | No | No | 2 |
| 8 | 56 | Yes | E-Poly | No | Yes | No | Yes | 1 |
| 9 | 60 | Yes | E-Poly | No | No | No | No | 2 |
| 10 | 50 | Yes | E-Poly | No | No | No | Yes | 2 |
| 11 | 70 | No | Avantage | No | No | Yes | Yes | 3 |
| 12 | 60 | No | E-Poly | Yes | No | Yes | No | 1 |
| 13 | 60 | Yes | Avantage | No | Yes | No | No | 1 |
| 14 | 52 | No | Constrained liner | No | No | No | No | 1 |
| 15 | 68 | No | Avantage | No | Yes | Yes | No | 1 |
| 16 | No | No | E-poly | No | No | Yes | No | 1 |
| 17 | 70 | Yes | Avantage | Yes | Yes | Yes | No | 1 |
| 18 | 58 | No | E-Poly | No | No | No | No | 1 |
| 19 | 52 | Yes | E-Poly | No | No | No | No | 1 |
| 20 | 42 | No | E-poly | Yes | Yes | No | No | 1 |
| 21 | 70 | No | Avantage | No | No | Yes | No | 1 |
| 22 | 60 | No | Avantage | Yes | No | No | No | 3 |
| 23 | 56 | No | E-poly | No | No | No | No | 1 |
| 24 | 52 | No | E-poly | Yes | No | No | No | 4 |
| 25 | 58 | No | E-poly | No | No | No | Yes | 2 |
| Pre-Operative (N° = 25) | Post-Operative (N° = 25) | p Value | |
|---|---|---|---|
| HHS | 34.8 ± 8.1 | 81.6 ± 10.4 | p < 0.001 |
| VAS | 6.7 ± 1.4 | 2.4 ± 1.0 | p < 0.001 |
| Severe Limping | 14 | 0 | |
| Moderate Limping | 7 | 0 | |
| Low Limping | 4 | 4 | |
| None Limping | 0 | 21 | |
| LLD (cm) | 2.0 ± 1.2 | 0.6 ± 0.6 | p < 0.001 |
| Average COR vertical position (cm) | 3.5 ± 1.7 | 2.0 ± 0.7 | p < 0.05 |
| Average COR horizontal position (cm) | 3.9 ± 1.5 | 3.2 ± 0.5 | p < 0.05 |
| Acetabular component abduction angle | 59.7 ± 29.6 | 46.0 ± 3.9 | p < 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
La Camera, F.; Di Matteo, V.; Pisano, A.; Guazzoni, E.; Favazzi, C.M.; Chiappetta, K.; Morenghi, E.; Grappiolo, G.; Loppini, M. Mid-Term Clinical and Radiographic Results of Complex Hip Revision Arthroplasty Based on 3D Life-Sized Model: A Prospective Case Series. J. Clin. Med. 2024, 13, 5496. https://doi.org/10.3390/jcm13185496
La Camera F, Di Matteo V, Pisano A, Guazzoni E, Favazzi CM, Chiappetta K, Morenghi E, Grappiolo G, Loppini M. Mid-Term Clinical and Radiographic Results of Complex Hip Revision Arthroplasty Based on 3D Life-Sized Model: A Prospective Case Series. Journal of Clinical Medicine. 2024; 13(18):5496. https://doi.org/10.3390/jcm13185496
Chicago/Turabian StyleLa Camera, Francesco, Vincenzo Di Matteo, Alessandro Pisano, Edoardo Guazzoni, Carlo Maria Favazzi, Katia Chiappetta, Emanuela Morenghi, Guido Grappiolo, and Mattia Loppini. 2024. "Mid-Term Clinical and Radiographic Results of Complex Hip Revision Arthroplasty Based on 3D Life-Sized Model: A Prospective Case Series" Journal of Clinical Medicine 13, no. 18: 5496. https://doi.org/10.3390/jcm13185496
APA StyleLa Camera, F., Di Matteo, V., Pisano, A., Guazzoni, E., Favazzi, C. M., Chiappetta, K., Morenghi, E., Grappiolo, G., & Loppini, M. (2024). Mid-Term Clinical and Radiographic Results of Complex Hip Revision Arthroplasty Based on 3D Life-Sized Model: A Prospective Case Series. Journal of Clinical Medicine, 13(18), 5496. https://doi.org/10.3390/jcm13185496






