Circulating RKIP and pRKIP in Early-Stage Lung Cancer: Results from a Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Sample Collection and Analysis
2.3. Statistical Analysis
3. Results
3.1. Evaluation of RKIP and pRKIP Levels in Urine Samples
3.2. Evaluation of RKIP and pRKIP Levels in Serum Samples
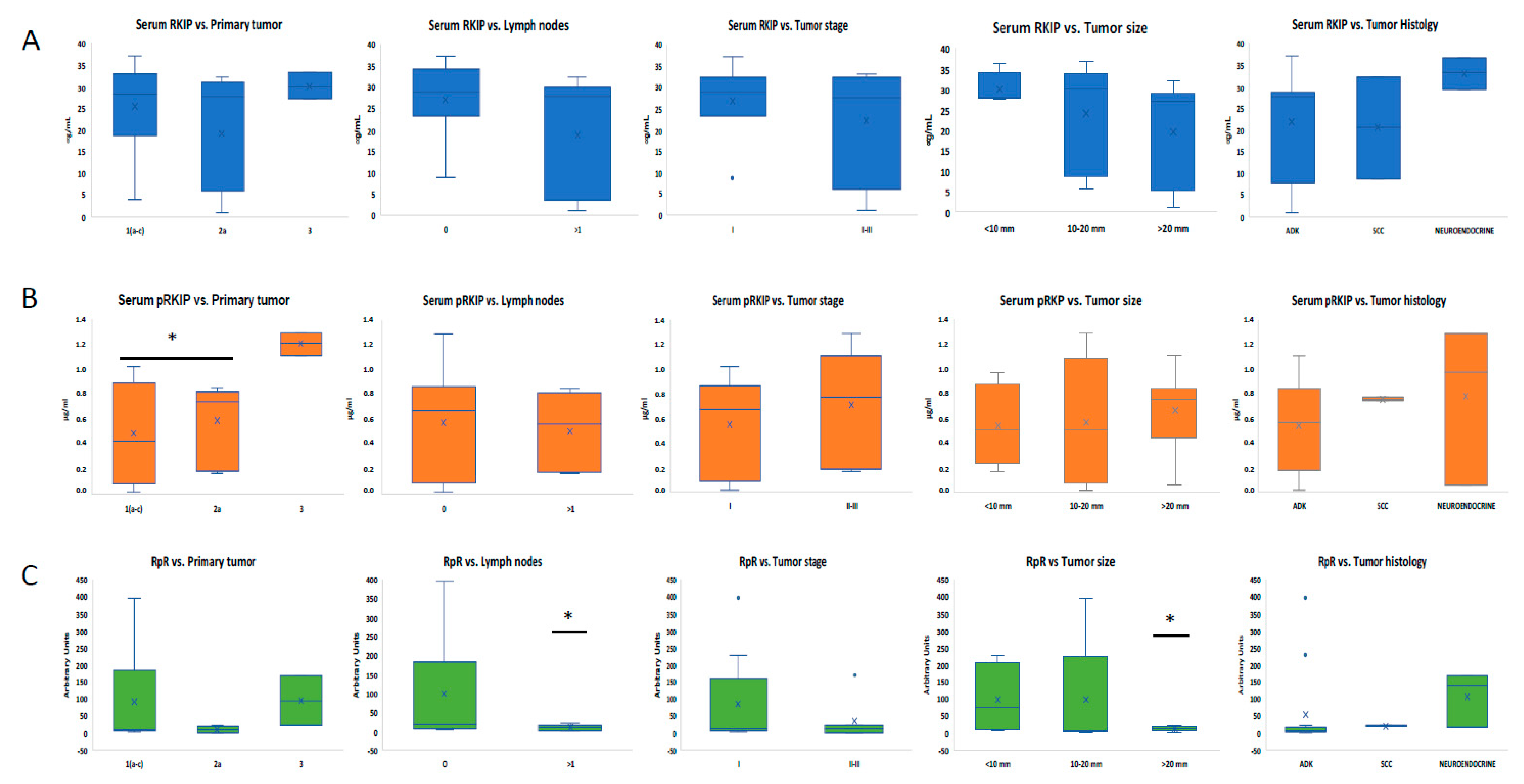
3.3. Analysis of Serum RKIP and pRKIP Levels According to Tumor Characteristics
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Alexander, M.; Kim, S.Y.; Cheng, H. Update 2020: Management of Non-Small Cell Lung Cancer. Lung 2020, 198, 897–907. [Google Scholar] [CrossRef] [PubMed]
- Chu, G.C.W.; Lazare, K.; Sullivan, F. Serum and blood based biomarkers for lung cancer screening: A systematic review. BMC Cancer 2018, 18, 181. [Google Scholar] [CrossRef]
- Van Kimmenade, R.R.; Januzzi, J.L., Jr. Emerging biomarkers in heart failure. Clin. Chem. 2012, 58, 127–138. [Google Scholar] [CrossRef]
- Conserva, F.; Barozzino, M.; Pesce, F.; Divella, C.; Oranger, A.; Papale, M.; Sallustio, F.; Simone, S.; Laviola, L.; Giorgino, F.; et al. Urinary miRNA-27b-3p and miRNA-1228-3p correlate with the progression of Kidney Fibrosis in Diabetic Nephropathy. Sci. Rep. 2019, 9, 11357. [Google Scholar] [CrossRef]
- Harris, A.C.; Ferrara, J.L.; Braun, T.M.; Holler, E.; Teshima, T.; Levine, J.E.; Choi, S.W.; Landfried, K.; Akashi, K.; Lugt, M.V.; et al. Plasma biomarkers of lower gastrointestinal and liver acute GVHD. Blood 2012, 119, 2960–2963. [Google Scholar] [CrossRef]
- Ben Ameur, R.; Molina, L.; Bolvin, C.; Kifagi, C.; Jarraya, F.; Ayadi, H.; Molina, F.; Granier, C. Proteomic approaches for discovering biomarkers of diabetic nephropathy. Nephrol. Dial. Transplant. 2010, 25, 2866–2875. [Google Scholar] [CrossRef]
- Ning, J.; Ge, T.; Jiang, M.; Jia, K.; Wang, L.; Li, W.; Chen, B.; Liu, Y.; Wang, H.; Zhao, S.; et al. Early diagnosis of lung cancer: Which is the optimal choice? Aging 2021, 13, 6214–6227. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pepe, M.S.; Etzioni, R.; Feng, Z.; Potter, J.D.; Thompson, M.L.; Thornquist, M.; Winget, M.; Yasui, Y. Phases of biomarker development for early detection of cancer. J. Natl. Cancer Inst. 2001, 93, 1054–1061. [Google Scholar] [CrossRef]
- Marmor, H.N.; Zorn, J.T.; Deppen, S.A.; Massion, P.P.; Grogan, E.L. Biomarkers in Lung Cancer Screening: A Narrative Review. Curr. Chall. Thorac. Surg. 2023, 5, 5. [Google Scholar] [CrossRef] [PubMed]
- Ke, M.; Shen, H.; Wang, L.; Luo, S.; Lin, L.; Yang, J.; Tian, R. Identification, Quantification, and Site Localization of Protein Posttranslational Modifications via Mass Spectrometry-Based Proteomics. Adv. Exp. Med. Biol. 2016, 919, 345–382. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.E.; Kim, N.I.; Lee, J.S.; Park, M.H.; Yoon, J.H. Reduced RKIP Expression is Associated With Breast Neoplastic Progression and is Correlated With Poor Outcomes and Aberrant Methylation in Breast Carcinoma. Appl. Immunohistochem. Mol. Morphol. AIMM 2017, 25, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Zhang, Z.; Zhang, Z.; Li, J.Y.; Cui, J.; Shi, W.P.; Dong, X.W.; Yuan, L.; Lin, P.; Chen, Z.N.; et al. Aberrant expression of miR-362 promotes lung cancer metastasis through downregulation of sema3A. J. Immunol. Res. 2018, 2018, 1687097. [Google Scholar] [CrossRef]
- Gong, Z.; Chen, X.; Zhang, Y.C.; Liu, C.; Wang, Z.; Xu, X.; Zhu, J.; Xue, T. LncRNA GATA6-AS1 Inhibits the Progression of Non-Small Cell Lung Cancer via Repressing microRNA-543 to Up-Regulating RKIP. Cancer Manag. Res. 2020, 12, 9327–9338. [Google Scholar] [CrossRef]
- Huerta-Yepez, S.; Yoon, N.K.; Hernandez-Cueto, A.; Mah, V.; Rivera-Pazos, C.M.; Chatterjee, D.; Vega, M.I.; Maresh, E.L.; Horvath, S.; Chia, D.; et al. Expression of phosphorylated raf kinase inhibitor protein (pRKIP) is a predictor of lung cancer survival. BMC Cancer. 2011, 11, 259. [Google Scholar] [CrossRef]
- Al-Mulla, F.; Bitar, M.S.; Thiery, J.P.; Zea, T.T.; Chatterjee, D.; Bennett, L.; Park, S.; Edwards, J.; Yeung, K.C. Clinical implications for loss or diminution of expression of Raf-1 kinase inhibitory protein and its phosphorylated form in ductal breast cancer. Am. J. Cancer Res. 2013, 3, 446–464. [Google Scholar]
- Papale, M.; Netti, G.S.; Stallone, G.; Ranieri, E. Understanding Mechanisms of RKIP Regulation to Improve the Development of New Diagnostic Tools. Cancers 2022, 14, 5070. [Google Scholar] [CrossRef]
- Klysik, J.; Theroux, S.J.; Sedivy, J.M.; Moffit, J.S.; Boekelheide, K. Signaling crossroads: The function of Raf kinase inhibitory protein in cancer, the central nervous system and reproduction. Cell. Signal. 2008, 20, 1–9. [Google Scholar] [CrossRef]
- Lorenz, K.; Lohse, M.J.; Quitterer, U. Protein kinase C switches the Raf kinase inhibitor from Raf-1 to GRK-2. Nature 2003, 426, 574–579. [Google Scholar] [CrossRef]
- Yeung, K.C.; Rose, D.W.; Dhillon, A.S.; Yaros, D.; Gustafsson, M.; Chatterjee, D.; McFerran, B.; Wyche, J.; Kolch, W.; Sedivy, J.M. Raf kinase inhibitor protein interacts with NF-kappaB-inducing kinase and TAK1 and inhibits NF-kappaB activation. Mol. Cell. Biol. 2001, 21, 7207–7217. [Google Scholar] [CrossRef] [PubMed]
- Cross-Knorr, S.; Lu, S.; Perez, K.; Guevara, S.; Brilliant, K.; Pisano, C.; Quesenberry, P.J.; Resnick, M.B.; Chatterjee, D. RKIP phosphorylation and STAT3 activation is inhibited by oxaliplatin and camptothecin and are associated with poor prognosis in stage II colon cancer patients. BMC cancer 2013, 13, 463. [Google Scholar] [CrossRef] [PubMed]
- Frankenberger, C.; Rabe, D.; Bainer, R.; Sankarasharma, D.; Chada, K.; Krausz, T.; Gilad, Y.; Becker, L.; Rosner, M.R. Metastasis Suppressors Regulate the Tumor Microenvironment by Blocking Recruitment of Prometastatic Tumor-Associated Macrophages. Cancer Res. 2015, 75, 4063–4073. [Google Scholar] [CrossRef]
- Yang, S.F.; Ma, R.; Pan, L.L.; Cao, J.; Sheng, N. RKIP and peroxiredoxin 2 expression predicts the proliferative potential of gastric cancer stem cells. Oncol. Lett. 2018, 15, 3173–3177. [Google Scholar] [CrossRef] [PubMed]
- Datar, I.; Qiu, X.; Ma, H.Z.; Yeung, M.; Aras, S.; de la Serna, I.; Al-Mulla, F.; Thiery, J.P.; Trumbly, R.; Fan, X.; et al. RKIP regulates CCL5 expression to inhibit breast cancer invasion and metastasis by controlling macrophage infiltration. Oncotarget 2015, 6, 39050–39061, Erratum in Oncotarget 2016, 7, 26925. [Google Scholar] [CrossRef]
- Bedri, S.K.; Nilsson, O.B.; Fink, K.; Månberg, A.; Hamsten, C.; Ayoglu, B.; Manouchehrinia, A.; Nilsson, P.; Olsson, T.; Hillert, J.; et al. Plasma protein profiling reveals candidate biomarkers for multiple sclerosis treatment. PLoS ONE 2019, 14, e0217208. [Google Scholar] [CrossRef]
- Zhong, W.; Edfors, F.; Gummesson, A.; Bergström, G.; Fagerberg, L.; Uhlén, M. Next generation plasma proteome profiling to monitor health and disease. Nat. Commun. 2021, 12, 2493. [Google Scholar] [CrossRef] [PubMed]
- Wojdała, A.L.; Chiasserini, D.; Bellomo, G.; Paciotti, S.; Gaetani, L.; Paoletti, F.P.; Parnetti, L. Phosphatidylethanolamine Binding Protein 1 (PEBP1) in Alzheimer’s Disease: ELISA Development and Clinical Validation. J. Alzheimers Dis. 2022, 88, 1459–1468. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nilsson, J.; Gobom, J.; Sjödin, S.; Brinkmalm, G.; Ashton, N.J.; Svensson, J.; Johansson, P.; Portelius, E.; Zetterberg, H.; Blennow, K.; et al. Cerebrospinal fluid biomarker panel for synaptic dysfunction in Alzheimer’s disease. Alzheimers Dement. 2021, 13, e12179. [Google Scholar] [CrossRef]
- Papale, M.; Vocino, G.; Lucarelli, G.; Rutigliano, M.; Gigante, M.; Rocchetti, M.T.; Pesce, F.; Sanguedolce, F.; Bufo, P.; Battaglia, M.; et al. Urinary RKIP/p-RKIP is a potential diagnostic and prognostic marker of clear cell renal cell carcinoma. Oncotarget 2017, 8, 40412–40424. [Google Scholar] [CrossRef]
- Gasparri, R.; Capuano, R.; Guaglio, A.; Caminiti, V.; Canini, F.; Catini, A.; Sedda, G.; Paolesse, R.; Di Natale, C.; Spaggiari, L. Volatolomic urinary profile analysis for diagnosis of the early stage of lung cancer. J. Breath. Res. 2022, 16, 046008. [Google Scholar] [CrossRef] [PubMed]
- Balkwill, F.; Charles, K.A.; Mantovani, A. Smoldering and polarized inflammation in the initiation and promotion of malignant disease. Cancer Cell. 2005, 7, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Gabriela-Freitas, M.; Pinheiro, J.; Raquel-Cunha, A.; Cardoso-Carneiro, D.; Martinho, O. RKIP as an Inflammatory and Immune System Modulator: Implications in Cancer. Biomolecules. 2019, 9, 769. [Google Scholar] [CrossRef] [PubMed]
- Elinav, E.; Nowarski, R.; Thaiss, C.A.; Hu, B.; Jin, C.; Flavell, R.A. Inflammation-induced cancer: Crosstalk between tumours, immune cells and microorganisms. Nat. Rev. Cancer 2013, 13, 759–771. [Google Scholar] [CrossRef] [PubMed]
- Zebisch, A.; Caraffini, V.; Sill, H. RAF Kinase Inhibitor Protein in Myeloid Leukemogenesis. Int. J. Mol. Sci. 2019, 20, 5756. [Google Scholar] [CrossRef] [PubMed]


| COHORT 1 | COHORT 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| All | Lung Cancer | Healthy Controls | p-Value | All | Lung Cancer | Healthy Controls | p-Value | |
| Subjects (n) | 42 (100) | 21 (100) | 21 (100) | 41 (100) | 18 (100) | 21 (100) | ||
| Mean Age | 65.5 ± 6.3 | 67.1 ± 6.6 | 63.9 ± 5.5 | 0.089 | 68.0 ± 6.8 | 69.8 ± 6.7 | 66.1 ± 6.4 | 0.083 |
| Sex | ||||||||
| Female | 18 (42.9) | 10 (47.6) | 8 (38.1) | 16 (39.0) | 11 (61.1) | 5 (23.8) | ||
| Male | 24 (57.1) | 11 (52.4) | 13 (61.9) | 0.76 | 24 (58.5) | 9 (50.0) | 15 (71.4) | 0.11 |
| Smoking status | ||||||||
| Current smokers | 15 (35.7) | 7 (33.3) | 8 (38.1) | 8 (19.5) | 2 (11.1) | 6 (28.6) | ||
| Ex-smokers | 20 (47.6) | 9 (42.9) | 11 (52.4) | 25 (61.0) | 12 (66.7) | 13 (61.9) | ||
| Never-smokers | 7 (16.7) | 5 (23.8) | 2 (9.5) | 0.60 | 7 (17.1) | 6 (33.3) | 1 (4.8) | 0.081 |
| Mean Pack-years | 51.1 ± 35.3 | 58.9 ± 35.0 | 44.6 ± 35.1 | 0.24 | 30.5 ± 29.5 | 30.0 ± 29.1 | 30.9 ± 30.6 | 0.93 |
| Commorbidities | ||||||||
| AH 1 | 17 (40.5) | 11 (52.4) | 6 (28.6) | 0.21 | 19 (46.3) | 12 (66.7) | 7 (33.3) | 0.20 |
| Cardiac disease | 4 (9.5) | 4 (19.0) | 0 (0.0) | 0.11 | 3 (7.3) | 0 (0.0) | 3 (14.3) | 0.23 |
| Metabolic disease 2 | 17 (40.5) | 8 (38.1) | 9 (42.9) | 1.00 | 12 (29.3) | 5 (27.8) | 7 (33.3) | 0.73 |
| COPD 3 | 4 (9.5) | 0 (0.0) | 4 (19.0) | 0.11 | 3 (7.3) | 0 (0.0) | 3 (14.3) | 0.23 |
| COHORT 1 | COHORT 2 | ||
|---|---|---|---|
| Histology | Adenocarcinoma | 17 | 13 |
| Squamous-cell carcinoma | 1 | 2 | |
| Neuroendocrine | 3 | 3 | |
| Stage | IA | 5 | 3 |
| IA2 | 6 | 2 | |
| IA3 | 4 | 4 | |
| IB | 6 | 2 | |
| IIB | - | 3 | |
| IIIA | - | 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gasparri, R.; Papale, M.; Sabalic, A.; Catalano, V.; Deleonardis, A.; De Luca, F.; Ranieri, E.; Spaggiari, L. Circulating RKIP and pRKIP in Early-Stage Lung Cancer: Results from a Pilot Study. J. Clin. Med. 2024, 13, 5830. https://doi.org/10.3390/jcm13195830
Gasparri R, Papale M, Sabalic A, Catalano V, Deleonardis A, De Luca F, Ranieri E, Spaggiari L. Circulating RKIP and pRKIP in Early-Stage Lung Cancer: Results from a Pilot Study. Journal of Clinical Medicine. 2024; 13(19):5830. https://doi.org/10.3390/jcm13195830
Chicago/Turabian StyleGasparri, Roberto, Massimo Papale, Angela Sabalic, Valeria Catalano, Annamaria Deleonardis, Federica De Luca, Elena Ranieri, and Lorenzo Spaggiari. 2024. "Circulating RKIP and pRKIP in Early-Stage Lung Cancer: Results from a Pilot Study" Journal of Clinical Medicine 13, no. 19: 5830. https://doi.org/10.3390/jcm13195830







