Evolution in the Management of Patella Fractures
Abstract
1. Introduction
2. Management Options
2.1. Non-Operative
2.2. Operative
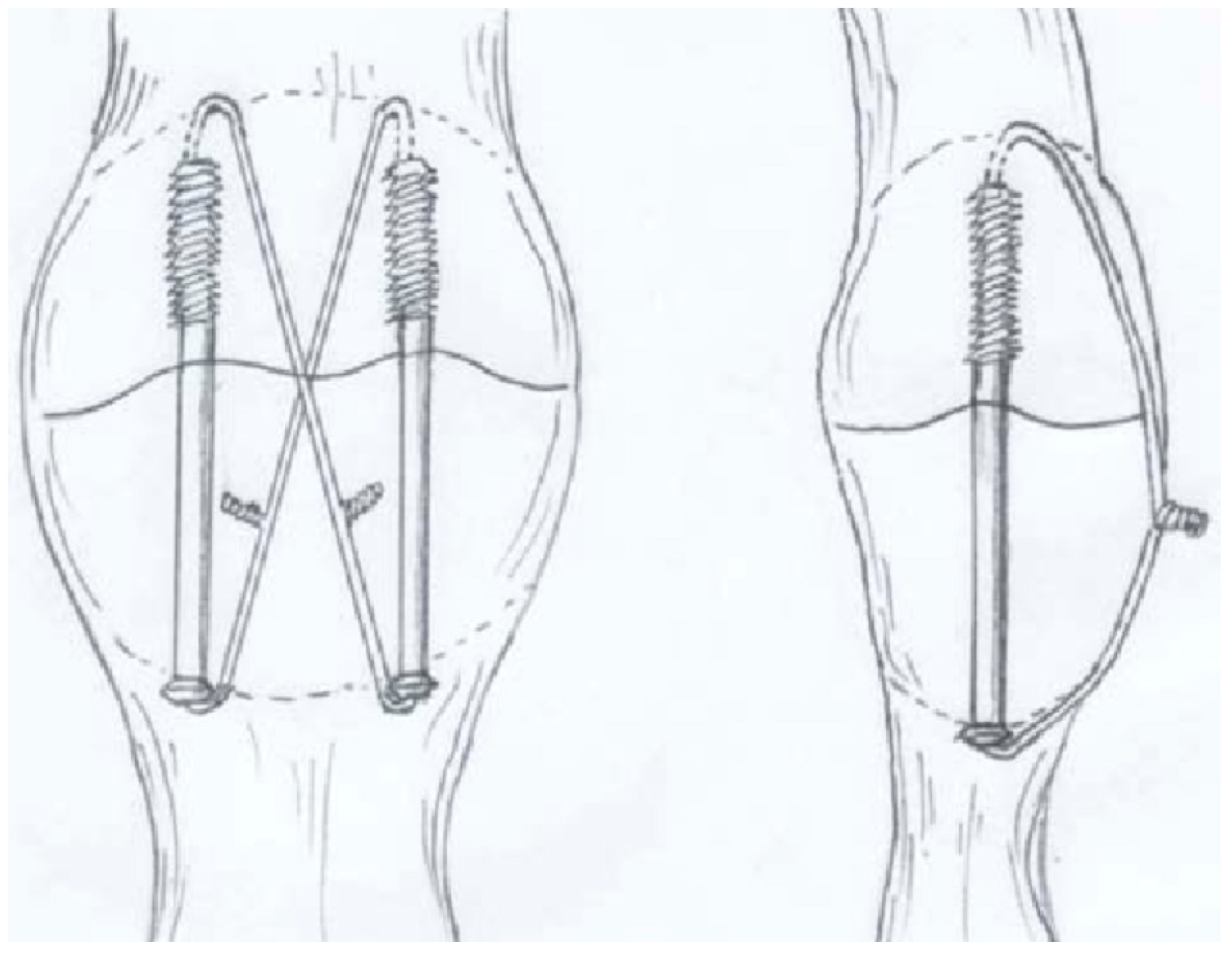
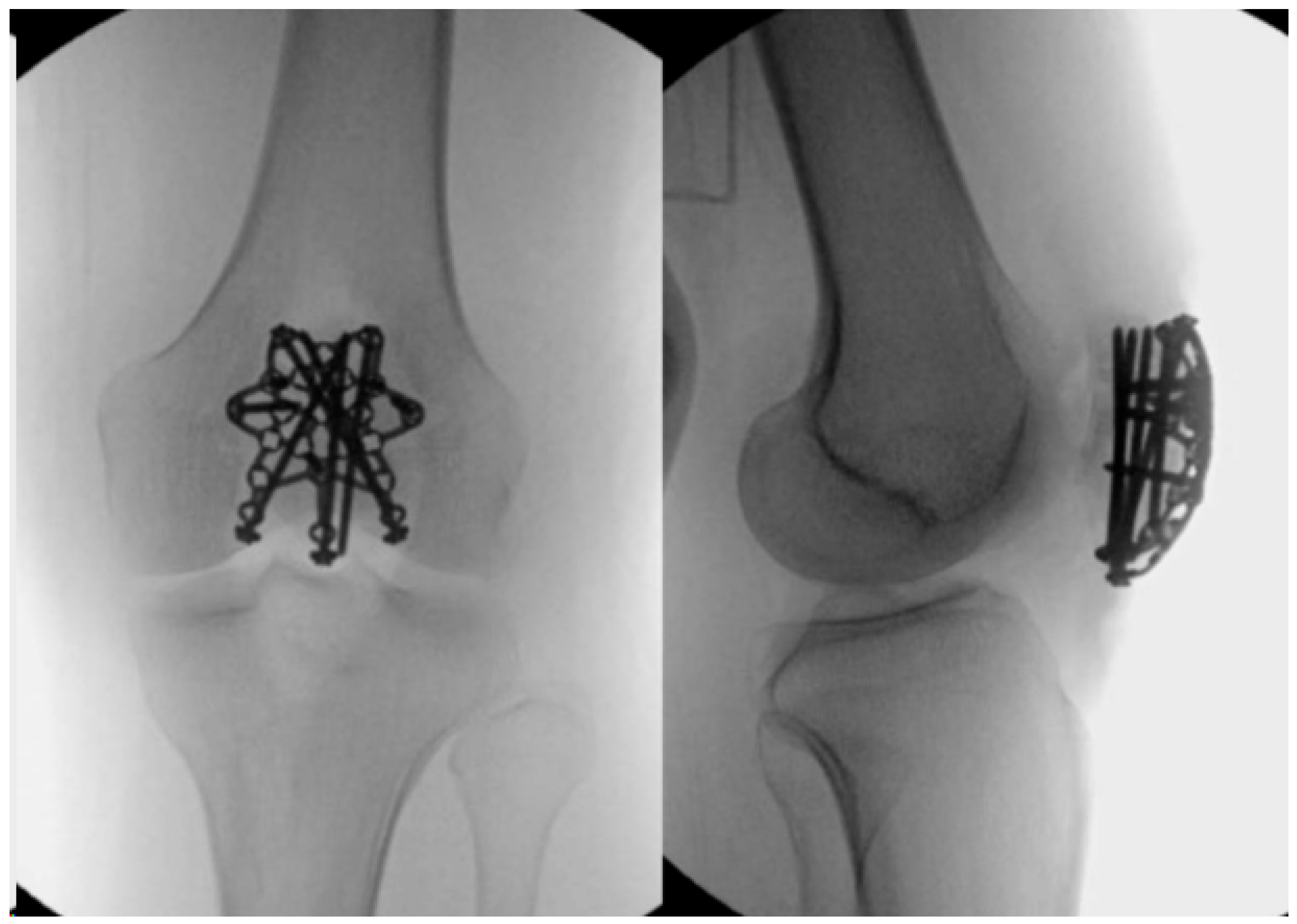
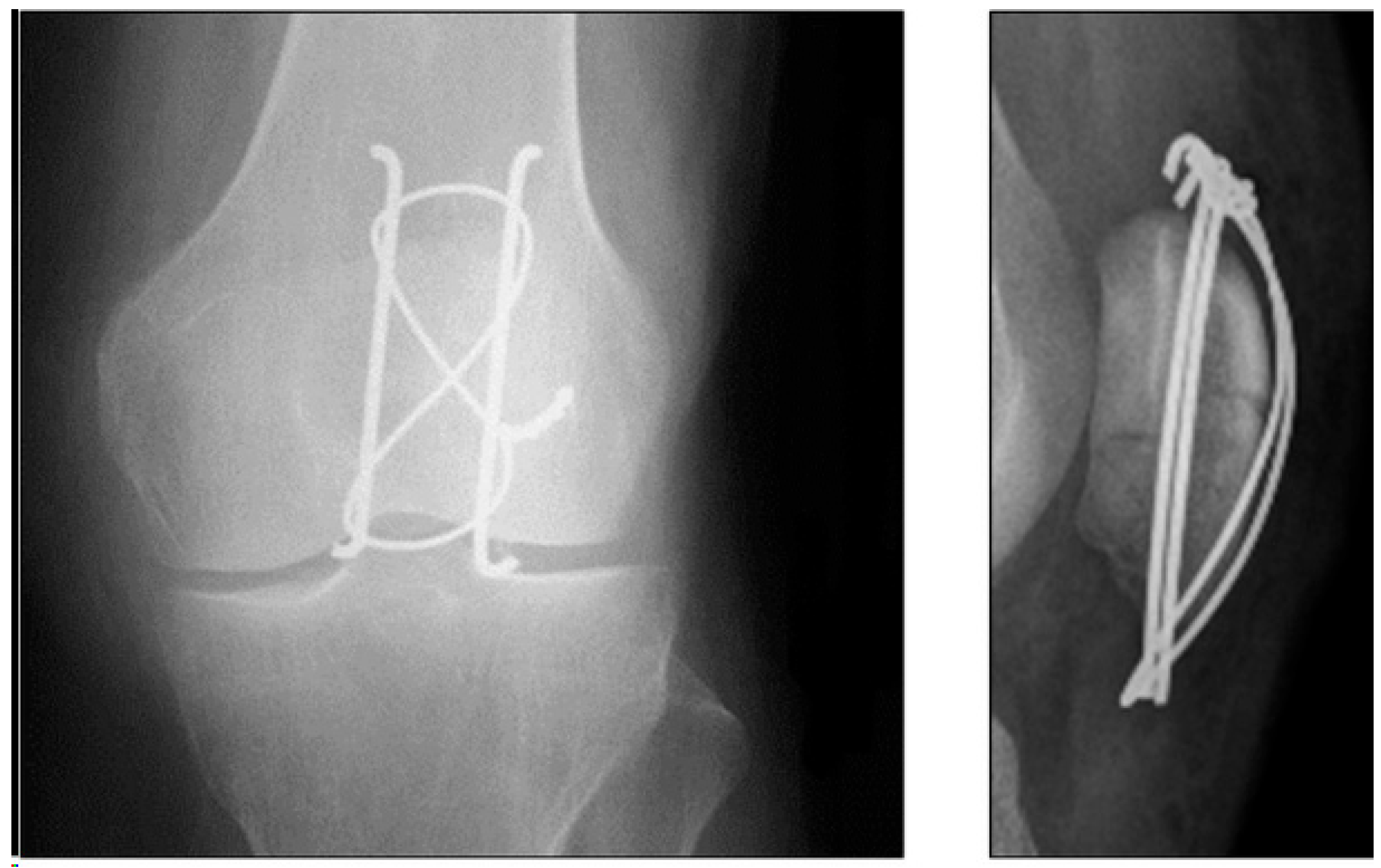
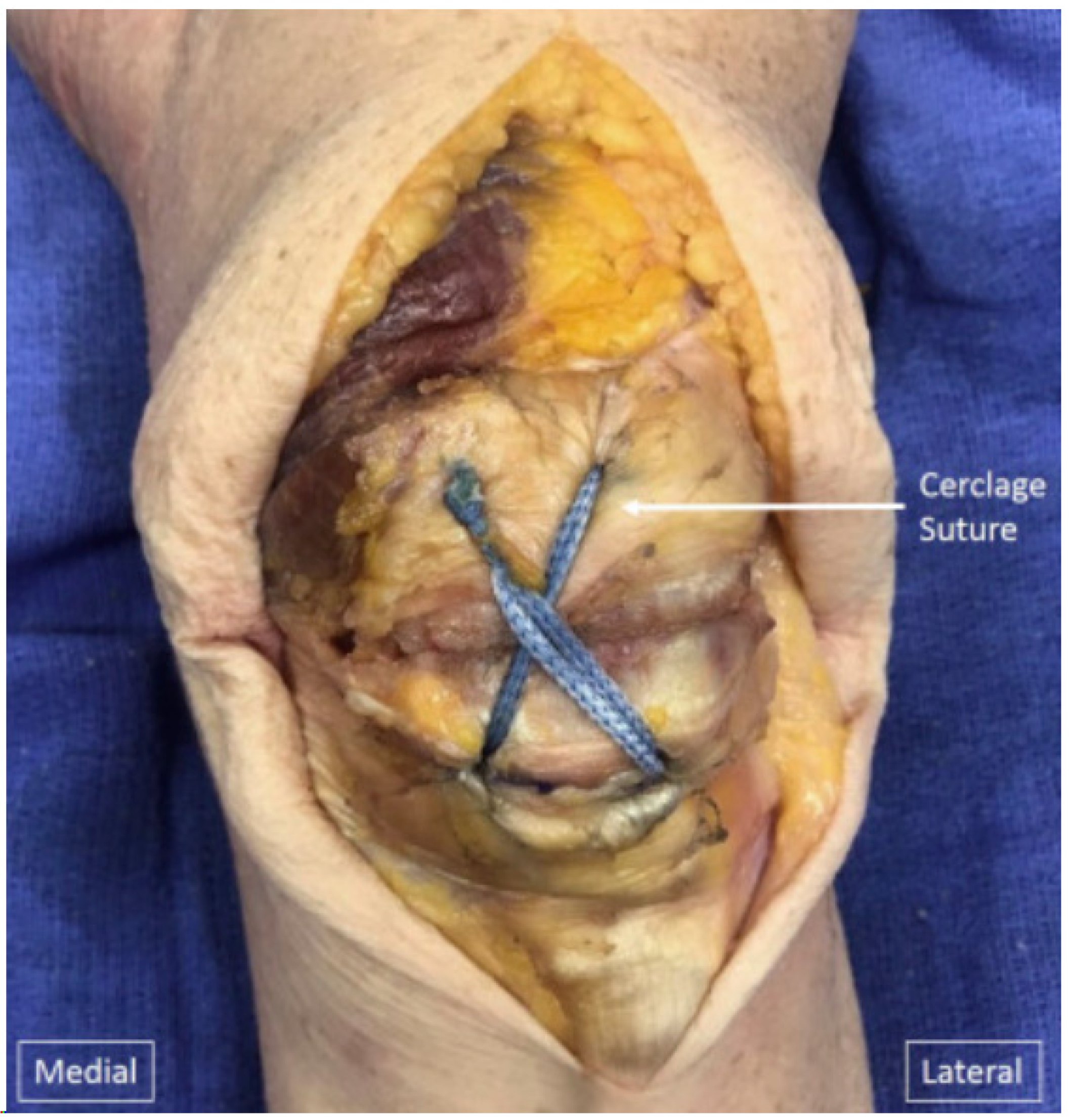
2.3. Tension Band Wire
2.4. Cannulated Screws
2.5. Locking Plates

2.6. Patellectomy
3. Comparison of Techniques
3.1. Biomechanical Studies
3.2. Clinical Studies
3.3. Sequelae of Patella Fracture
4. Conclusions
Funding
Data Availability Statement
Conflicts of Interest
References
- Neumann, M.V.; Niemeyer, P.; Südkamp, N.P.; Strohm, P.C. Patellar fractures—A review of classification, genesis, and evaluation of treatment. Acta Chir. Orthop. Traumatol. Cech. 2014, 81, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Wild, M.; Windolf, J.; Flohé, S. Patellafrakturen [Fractures of the patella]. Unfallchirurg 2010, 113, 401–411. quiz 412(In German) [Google Scholar] [CrossRef] [PubMed]
- Shirsat, N.M.; Patil, D.D. A retrospective study of patellar fractures in a tertiary care institute. MedPulse Int. J. Orthop. 2017, 3, 13–15. [Google Scholar]
- Larsen, P.; Court-Brown, C.M.; Vedel, J.O.; Vistrup, S.; Elsoe, R. Incidence and Epidemiology of Patellar Fractures. Orthopedics 2016, 39, e1154–e1158. [Google Scholar] [CrossRef]
- Larsen, P.; Rathleff, M.S.; Østgaard, S.E.; Johansen, M.B.; Elsøe, R. Patellar fractures are associated with an increased risk of total knee arthroplasty: A Matched Cohort Study of 6096 Patellar Fractures with a mean follow-up of 14.3 Years. Bone Jt. J. 2018, 100-B, 1477–1481. [Google Scholar] [CrossRef]
- Wild, M.; Khayal, T.; Miersch, D.; Windolf, J.; Hakimi, M. Die Zuggurtungsosteosynthese nach Patellafraktur. Komplikationen und mittelfristige klinische Ergebnisse [Dynamic cerclage wiring of patellar fractures. Complications and midterm functional results]. Unfallchirurg 2008, 111, 892–897. (In German) [Google Scholar] [CrossRef]
- Gray, S.D.; Kaplan, P.A.; Dussault, R.G.; Omary, R.A.; Campbell, S.E.; Chrisman, H.B.; Futterer, S.F.; McGraw, J.K.; Keats, T.E.; Hillman, B.J. Acute knee trauma: How many plain film views are necessary for the initial examination? Skelet. Radiol. 1997, 26, 298–302. [Google Scholar] [CrossRef]
- Lazaro, L.E.; Wellman, D.S.; Pardee, N.C.; Gardner, M.J.; Toro, J.B.; MacIntyre, N.R.I.I.I.; Helfet, D.L.; Lorich, D.G. Effect of Computerized Tomography on Classification and Treatment Plan for Patellar Fractures. J. Orthop. Trauma 2013, 27, 336–344. [Google Scholar] [CrossRef]
- Huberti, H.H.; Hayes, W.C.; Stone, J.L.; Shybut, G.T. Force ratios in the quadriceps tendon and ligamentum patellae. J. Orthop. Res. 1984, 2, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Loudon, J.K. Biomechanics and pathomechanics of the patellofemoral joint. Int. J. Sports Phys. Ther. 2016, 11, 820–830. [Google Scholar]
- LeBrun, C.T.; Langford, J.R.; Sagi, H.C. Functional outcomes after operatively treated patella fractures. J. Orthop. Trauma 2012, 26, 422–426. [Google Scholar] [CrossRef]
- Reilly, D.T.; Martens, M. Experimental analysis of the quadriceps muscle force and patello-femoral joint reaction force for various activities. Acta Orthop. Scand. 1972, 43, 126–137. [Google Scholar] [CrossRef]
- Bradko, V.; Stoll, W.T.; Haruno, L.S.; Rosenfeld, S.B.; McKay, S.D. Two cases of combined patellar tendon avulsion from the tibia and patella. SICOT J. 2018, 4, 17. [Google Scholar] [CrossRef]
- Melvin, J.S.; Mehta, S. Patellar fractures in adults. J. Am. Acad. Orthop. Surg. 2011, 19, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Boström, A. Fracture of the patella. A study of 422 patellar fractures. Acta Orthop. Scand. Suppl. 1972, 143, 1–80. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Zou, C.; Kenmegne, G.R.; Yin, Y.; Lin, Y.; Fang, Y. Management of comminuted patellar fractures using suture reduction technique combined with the modified Kirschner-wirge tension band. BMC Surg. 2023, 23, 251. [Google Scholar] [CrossRef]
- Gao, G.X.; Mahadev, A.; Lee, E.H. Sleeve fracture of the patella in children. J. Orthop. Surg. 2008, 16, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Dai, L.Y.; Zhang, W.M. Fractures of the patella in children. Knee Surg. Sports Traumatol. Arthrosc. 1999, 7, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Hunt, D.M.; Somashekar, N. A review of sleeve fractures of the patella in children. Knee 2005, 12, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.Y.; Lin, W.C.; Wang, J.W. Inferior sleeve fracture of the patella. J. Chin. Med. Assoc. 2011, 74, 98–101. [Google Scholar] [CrossRef]
- Ditchfield, A.; Sampson, M.A.; Taylor, G.R. Case reports. Ultrasound diagnosis of sleeve fractures of the patella. Clin. Radiol. 2000, 55, 721–722. [Google Scholar] [CrossRef]
- Bates, D.G.; Hresko, M.T.; Jaramillo, D. Patellar sleeve fracture: Demonstration with MR imaging. Radiology 1994, 193, 825–827. [Google Scholar] [CrossRef] [PubMed]
- Yeung, E.; Ireland, J. An unusual double patella: A case report. Knee 2004, 11, 129–131. [Google Scholar] [CrossRef] [PubMed]
- Braun, W.; Wiedemann, M.; Rüter, A.; Kundel, K.; Kolbinger, S. Indications and results of nonoperative treatment of patellar fractures. Clin. Orthop. Relat. Res. 1993, 289, 197–201. [Google Scholar] [CrossRef]
- Pritchett, J.W. Nonoperative treatment of widely displaced patella fractures. Am. J. Knee Surg. 1997, 10, 145–147, discussion 147–148. [Google Scholar] [PubMed]
- Billings, J.S.; Oxon, D.C.L. The history literature of surgery. In System of Surgery; Dennis, F., Ed.; Lea Brothers: Philadelphia, PA, USA, 1895; Volume I, p. 136. [Google Scholar]
- Lister, J. A new operation for fracture of the patella. Br. Med. J. 1877, 2, 850. [Google Scholar]
- Dennis, F.S. The treatment of the fractured patella by the metallic suture. N. Y. Med. J. 1886, 43, 372–373. [Google Scholar]
- Hey-Groves, E.W. A note on the extension apparatus of the knee joint. Br. J. Surg. 1937, 4, 747–748. [Google Scholar]
- Horwitz, T.; Lambert, R.G. Patellectomy in the military service; a report of 19 cases. Surg. Gynecol. Obstet. 1946, 82, 423–426. [Google Scholar]
- Thiem, C. Uber die Grosse der Unfallfolgen bei der blutigen und unblutigen behandlung der einfachen (subcutanen) querbruche der kniesheibe. Verh. Dtsch. Ges. Chir. 1905, 34, 374–393. [Google Scholar]
- Byrd, W.A. On the wire ligature in the treatment of ununited fractures and in resections of bones for deformity. N. Y. Med. J. 1876, 23, 449–465. [Google Scholar]
- Wilson, J.W. Joseph Nash McDowell, M.D. Regist. Ky. Hist. Soc. 1970, 68, 341–369. [Google Scholar]
- Malgaigne, J.F. Traité des Fractures et des Luxations; Baillière: Paris, France, 1847. [Google Scholar]
- Cameron, J.C. Transverse fracture of the patella. Glasg. Med. J. 1878, 10, 289–294. [Google Scholar]
- Volkmann, R. Die Sehnennaht bei Querbrüchen der Kniescheibe. Centrallbl. Chir. 1880, 7, 385–387. [Google Scholar]
- Muller, M.E.; Allgower, M.; Schneider, R.; Willenegger, H. Manual of Internal Fixation: Techniques Recommended by the AO Group; Springer: Berlin/Heidelberg, Germany, 1979; pp. 248–253. [Google Scholar]
- Wild, M.; Fischer, K.; Hilsenbeck, F.; Hakimi, M.; Betsch, M. Treating patella fractures with a fixed-angle patella plate-A prospective observational study. Injury 2016, 47, 1737–1743. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.E.; Allgöwer, M.; Schneider, R.; Willenegger, H. Manual of Internal Fixation, 3rd ed.; Springer: Berlin/Heidelberg, Germany; New York, NY, USA, 1991. [Google Scholar]
- Rüedi, T.P.; Buckley, R.E.; Moran, C.G. AO Principles of Fracture Management, 2nd ed.; Thieme: Stuttgart, Germany; New York, NY, USA, 2007. [Google Scholar]
- Gwinner, C.; Märdian, S.; Schwabe, P.; Schaser, K.D.; Krapohl, B.D.; Jung, T.M. Current concepts review: Fractures of the patella. GMS Interdiscip. Plast. Reconstr. Surg. DGPW 2016, 5, Doc01. [Google Scholar] [CrossRef] [PubMed]
- Bostrom, M.P.; Asnis, S.E.; Ernberg, J.J.; Wright, T.M.; Giddings, V.L.; Berberian, W.S.; Missri, A.A. Fatigue testing of cerclage stainless steel wire fixation. J. Orthop. Trauma 1994, 8, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, J.; Bried, J.; Dohm, M.; McMurtry, M. Biomechanical evaluation of various forms of fixation of transverse patellar fractures. J. Orthop. Trauma 1987, 1, 219–222. [Google Scholar] [CrossRef] [PubMed]
- Berg, E.E. Open reduction internal fixation of displaced transverse patella fractures with figure-eight wiring through parallel cannulated compression screws. J. Orthop. Trauma 1997, 11, 573–576. [Google Scholar] [CrossRef] [PubMed]
- Burvant, J.G.; Thomas, K.A.; Alexander, R.; Harris, M.B. Evaluation of methods of internal fixation of transverse patella fractures: A biomechanical study. J. Orthop. Trauma 1994, 8, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Lotke, P.A.; Ecker, M.L. Transverse fractures of the patella. Clin. Orthop. Relat. Res. 1981, 158, 180–184. [Google Scholar] [CrossRef]
- Weber, M.J.; Janecki, C.J.; McLeod, P.; Nelson, C.L.; Thompson, J.A. Efficacy of various forms of fixation of transverse fractures of the patella. J. Bone Jt. Surg. Am. 1980, 62, 215–220. [Google Scholar] [CrossRef]
- Steinmetz, S.; Brügger, A.; Chauveau, J.; Chevalley, F.; Borens, O.; Thein, E. Practical guidelines for the treatment of patellar fractures in adults. Swiss Med. Wkly. 2020, 150, w20165. [Google Scholar] [CrossRef]
- Wendl, K.; Zinser, R.; Hochstein, P.; Grützner, P.A. Frakturen der Kniescheibe. Trauma Berufskrankh. 2002, 4, 30–37. [Google Scholar] [CrossRef]
- Eggink, K.M.; Jaarsma, R.L. Mid-term (2–8 years) follow-up of open reduction and internal fixation of patella fractures: Does the surgical technique influence the outcome? Arch. Orthop. Trauma Surg. 2011, 131, 399–404. [Google Scholar] [CrossRef]
- Smith, S.T.; Cramer, K.E.; Karges, D.E.; Watson, J.T.; Moed, B.R. Early complications in the operative treatment of patella fractures. J. Orthop. Trauma 1997, 11, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.A.; Liu, W.; Zurakowski, D.; Smith, R.M.; Harris, M.B.; Vrahas, M.S. Factors predicting failure of patella fixation. J. Trauma Acute Care Surg. 2012, 72, 1051–1055. [Google Scholar] [CrossRef] [PubMed]
- Dy, C.J.; Little, M.T.; Berkes, M.B.; Ma, Y.; Roberts, T.R.; Helfet, D.L.; Lorich, D.G. Meta-analysis of re-operation, non-union, and infection after open reduction and internal fixation of patella fractures. J. Trauma Acute Care Surg. 2012, 73, 928–932. [Google Scholar] [CrossRef] [PubMed]
- Kocadal, O.; Pepe, M.; Gunes, Z.; Aksahin, E.; Duran, S.; Aktekin, C.N. Is There Any Difference between the Biomechanical Strengths of the Current Fixation Techniques for Comminuted Distal Patellar Fractures? (Comparison of Distal Patella Fracture Fixation Techniques). Acta Orthop. Belg. 2017, 83, 550–557. [Google Scholar] [PubMed]
- Thelen, S.; Schneppendahl, J.; Baumgärtner, R.; Eichler, C.; Koebke, J.; Betsch, M.; Hakimi, M.; Windolf, J.; Wild, M. Cyclic long-term loading of a bilateral fixed-angle plate in comparison with tension band wiring with K-wires or cannulated screws in transverse patella fractures. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 311–317. [Google Scholar] [CrossRef]
- Tian, Y.; Zhou, F.; Ji, H.; Zhang, Z.; Guo, Y. Cannulated screw and cable are superior to modified tension band in the treatment of transverse patella fractures. Clin. Orthop. Relat. Res. 2011, 469, 3429–3435. [Google Scholar] [CrossRef]
- Schnabel, B.; Scharf, M.; Schwieger, K.; Windolf, M.; van der Pol, B.; Braunstein, V.; Appelt, A. Biomechanical comparison of a new staple technique with tension band wiring for transverse patella fractures. Clin. Biomech. 2009, 24, 855–859. [Google Scholar] [CrossRef] [PubMed]
- Ha, C.; Sun, J.I. The treatment of patellar fracture with modified tension band wiring, using cannulated screws. J. Korean Fract. Soc. 2004, 17, 117. [Google Scholar] [CrossRef]
- Avery, M.C.; Jo, S.; Chang, A.; Ricci, W.M.; McAndrew, C.; Miller, A.N.; Tang, S. Cannulated Screw Prominence in Tension Band Wiring of Patella Fractures Increases Fracture Gapping: A Cadaver Study. Clin. Orthop. Relat. Res. 2019, 477, 1249–1255. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.M.; Applin, D.T.; McGrady, L.M.; Wang, M.; Schmeling, G.J. Biomechanical Comparison of Tension Band Fixation of Patella Transverse Fracture: Headless Screws versus Headed Screws. J. Orthop. Trauma 2019, 33, e240–e245. [Google Scholar] [CrossRef] [PubMed]
- Monaco, E.; Bruni, G.; Daggett, M.; Saithna, A.; Cardarelli, S.; Proietti, L.; Ferretti, A. Patellar Fracture Fixation Using Suture Tape Cerclage. Arthrosc. Tech. 2020, 9, e783–e789. [Google Scholar] [CrossRef] [PubMed]
- Gosal, H.S.; Singh, P.; Field, R.E. Clinical experience of patellar fracture fixation using metal wire or non-absorbable polyester—A study of 37 cases. Injury 2001, 32, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Bryant, T.L.; Anderson, C.L.; Stevens, C.G.; Conrad, B.P.; Vincent, H.K.; Sadasivan, K.K. Comparison of cannulated screws with FiberWire or stainless steel wire for patella fracture fixation: A pilot study. J. Orthop. 2014, 12, 92–96. [Google Scholar] [CrossRef]
- Taha, M.E.; Schneider, K.; Clarke, E.C.; O’Briain, D.E.; Smith, M.M.; Cunningham, G.; Cass, B.; Young, A.A. A Biomechanical Comparison of Different Suture Materials Used for Arthroscopic Shoulder Procedures. Arthroscopy 2020, 36, 708–713. [Google Scholar] [CrossRef]
- Patel, V.R.; Parks, B.G.; Wang, Y.; Ebert, F.R.; Jinnah, R.H. Fixation of patella fractures with braided polyester suture: A biomechanical study. Injury 2000, 31, 1–6. [Google Scholar] [CrossRef]
- Posner, A.D.; Hutchinson, I.; Zimmerman, J. Patellar Fracture Fixation with Cannulated Compression Screws and FiberTape Cerclage. Arthrosc. Tech. 2021, 10, e1447–e1453, ISSN 2212-6287. [Google Scholar] [CrossRef]
- Carpenter, J.E.; Kasman, R.; Matthews, L.S. Fractures of the patella. Instr. Course Lect. 1994, 43, 97–108. [Google Scholar] [CrossRef]
- DePuy Synthes. Validation Lab Report. October 2020 Windchill # 0000307351. Available online: https://www.jnjmedtech.com/en-US/product/variable-angle-locking-patella-plating-system (accessed on 24 February 2024).
- DePuy Synthes Validation Lab Report. Lateral Patella Plates. May 2021. Windchill #0000308557. Available online: https://www.jnjmedtech.com/en-US/product/variable-angle-locking-patella-plating-system (accessed on 24 February 2024).
- DePuy Synthes. Drawing. August 2020. Windchill # 02_137_000. Available online: https://www.jnjmedtech.com/en-US/product/variable-angle-locking-patella-plating-system (accessed on 24 February 2024).
- Arthrex, Inc. Data on File (APT-03733); Arthrex, Inc.: Naples, FL, USA, 2018. [Google Scholar]
- Buschbeck, S.; Götz, K.; Klug, A.; Barzen, S.; Gramlich, Y.; Hoffmann, R. Comminuted AO-C3 fractures of the patella: Good outcome using anatomically contoured locking plate fixation. Int. Orthop. 2022, 46, 1395–1403. [Google Scholar] [CrossRef]
- Kumar, S.; Mittal, S.; Manhas, V.; Sharma, V. Functional and radiological outcomes following plating for displaced fractures of the patella: A pilot study. Injury 2022, 53, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.J.; Ok, S.; Lee, J.; Choi, S. Can multiple miniplates improve the treatment of comminuted patellar fracture? BMC Musculoskelet. Disord. 2023, 24, 936. [Google Scholar] [CrossRef] [PubMed]
- Amin, A.; Kellam, P.J.; Warner, S.J. Treatment of a Multifragmentary Patella Fracture Using a Novel Anatomic Locking Plate. J. Orthop. Trauma 2022. [Google Scholar]
- Levack, B.; Flannagan, J.P.; Hobbs, S. Results of surgical treatment of patellar fractures. J. Bone Jt. Surg. Br. 1985, 67, 416–419. [Google Scholar] [CrossRef]
- Zderic, I.; Stoffel, K.; Sommer, C.; Höntzsch, D.; Gueorguiev, B. Biomechanical evaluation of the tension band wiring principle. A comparison between two different techniques for transverse patella fracture fixation. Injury 2017, 48, 1749–1757. [Google Scholar] [CrossRef]
- Carpenter, J.E.; Kasman, R.A.; Patel, N.; Lee, M.L.; Goldstein, S.A. Biomechanical evaluation of current patella fracture fixation techniques. J. Orthop. Trauma 1997, 11, 351–356. [Google Scholar] [CrossRef]
- Banks, K.E.; Ambrose, C.G.; Wheeless, J.S.; Tissue, C.M.; Sen, M. An alternative patellar fracture fixation: A biomechanical study. J. Orthop. Trauma 2013, 27, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Galla, M.; Lobenhoffer, P. Frakturen der Patella. Chirurg 2005, 76, 987–999. [Google Scholar] [CrossRef] [PubMed]
- Ellwein, A.; Lill, H.; DeyHazra, R.O.; Smith, T.; Katthagen, J.C. Outcomes after locked plating of displaced patella fractures: A prospective case series. Int. Orthop. 2019, 43, 2807–2815. [Google Scholar] [CrossRef] [PubMed]
- Wagner, F.C.; Neumann, M.V.; Wolf, S.; Jonaszik, A.; Izadpanah, K.; Piatek, S.; Südkamp, N.P. Biomechanical comparison of a 3.5 mm anterior locking plate to cannulated screws with anterior tension band wiring in comminuted patellar fractures. Injury 2020, 51, 1281–1287. [Google Scholar] [CrossRef] [PubMed]
- Meng, D.; Meng, Y.; Li, B.; Zeng, G.; Zhang, B.; Hou, C.; Lin, H.; Ouyang, Y. Comparison between tension band and cerclage with X-Plate and lag screws in treatment of comminuted patellar fractures. J. Orthop. Sci. 2020, 26, 409–414. [Google Scholar] [CrossRef]
- Meng, D.; Xu, P.; Shen, D.; Chen, Y.; Zhu, C.; Hou, C.; Lin, H.; Ouyang, Y. A clinical comparison study of three different methods for treatment of transverse patellar fractures. J. Orthop. Sci. 2019, 24, 142–146. [Google Scholar] [CrossRef]
- Lorich, D.G.; Fabricant, P.D.; Sauro, G.; Lazaro, L.E.; Thacher, R.R.; Garner, M.R.; Warner, S.J. Superior outcomes after operative fixation of patella fractures using a novel plating technique: A prospective cohort study. J. Orthop. Trauma 2017, 31, 241–247. [Google Scholar] [CrossRef]
- Raja, B.S.; Jain, A.; Paul, S.; Choudhury, A.K.; Kalia, R.B. Plate osteosynthesis in patellar fractures: A systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2022, 32, 1627–1640. [Google Scholar] [CrossRef]
- Tsotsolis, S.; Ha, J.; Fernandes, A.R.C.; Park, J.Y.; Dewhurst, M.; Walker, T.; Ilo, K.; Park, S.R.; Patel, A.; Hester, T.; et al. To plate, or not to plate? A systematic review of functional outcomes and complications of plate fixation in patellar fractures. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 3287–3297. [Google Scholar] [CrossRef]
- Lazaro, L.E.; Cross, M.B.; Lorich, D.G. Vascular anatomy of the patella: Implications for total knee arthroplasty surgical approaches. Knee 2014, 21, 655–660. [Google Scholar] [CrossRef]
- Torchia, M.E.; Lewallen, D.G. Open fractures of the patella. J. Orthop. Trauma 1996, 10, 403–409. [Google Scholar] [CrossRef]
- Klassen, J.F.; Trousdale, R.T. Treatment of delayed and non-union of the patella. J. Orthop. Trauma 1997, 11, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Hoshino, C.M.; Tran, W.; Tiberi, J.V.; Black, M.H.; Li, B.H.; Gold, S.M.; Navarro, R.A. Complications following tension-band fixation of patellar fractures with cannulated screws compared with Kirschner wires. J. Bone Jt. Surg. Am. 2013, 95, 653–659. [Google Scholar] [CrossRef] [PubMed]
- Scapinelli, R. Blood supply of the human patella. Its relation to ischemic necrosis after fracture. J. Bone Jt. Surg. 1967, 49, 563–570. [Google Scholar] [CrossRef]
- Cameron, H.U.; Huffer, B. Avascular necrosis of the patella following total knee replacement. Acta Orthop. Belg. 1985, 51, 805–810. [Google Scholar]
- Mont, M.A.; Tomek, I.M.; Hungerford, D.S. Core decompression for steroid associated avascular necrosis of the distal femur. Clin. Orthop. 1997, 334, 124–130. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baid, M.; Narula, S.; Manara, J.R.; Blakeney, W. Evolution in the Management of Patella Fractures. J. Clin. Med. 2024, 13, 1426. https://doi.org/10.3390/jcm13051426
Baid M, Narula S, Manara JR, Blakeney W. Evolution in the Management of Patella Fractures. Journal of Clinical Medicine. 2024; 13(5):1426. https://doi.org/10.3390/jcm13051426
Chicago/Turabian StyleBaid, Mahak, Sid Narula, Jonathan R. Manara, and William Blakeney. 2024. "Evolution in the Management of Patella Fractures" Journal of Clinical Medicine 13, no. 5: 1426. https://doi.org/10.3390/jcm13051426
APA StyleBaid, M., Narula, S., Manara, J. R., & Blakeney, W. (2024). Evolution in the Management of Patella Fractures. Journal of Clinical Medicine, 13(5), 1426. https://doi.org/10.3390/jcm13051426





