Two Methods of Forward Head Posture Assessment: Radiography vs. Posture and Their Clinical Comparison
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Outcome Assessments
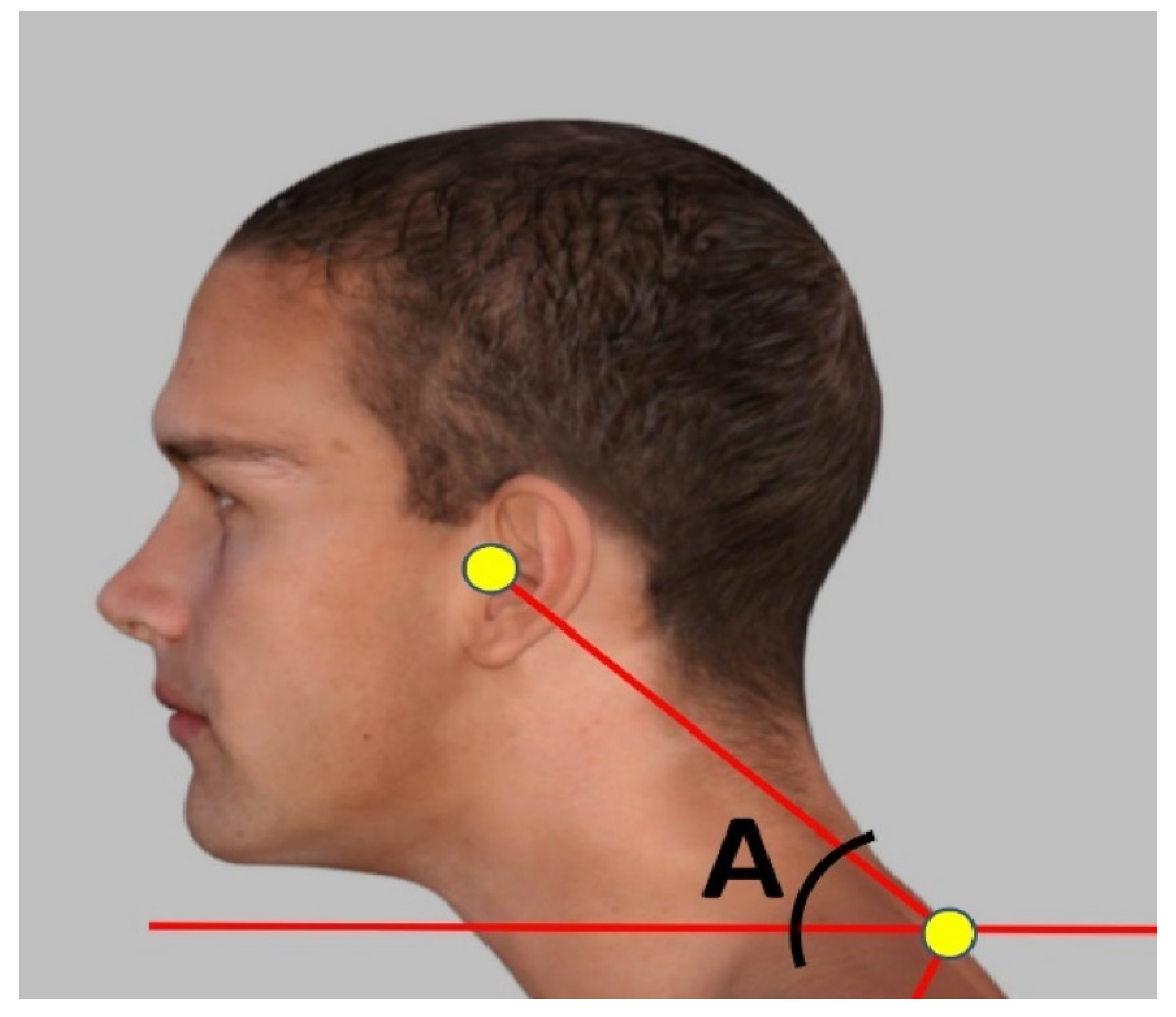
2.2.1. Forward Head Posture (FHP) Assessment with the Craniovertebral Angle (CVA)
2.2.2. Lateral Cervical Radiography: ARA C2–C7 and C2–C7 SVA
2.3. Data Analysis
3. Results
3.1. Patient Demographics
3.2. Regression Outcome
4. Discussion
4.1. Pros and Cons of the CVA
4.2. Pros and Cons of Radiographic ARA C2–C7 and C2–C7 SVA
4.3. Risk–Benefit Ratio of Exposure to Ionizing Radiation
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AHT | Anterior Head Translation |
| ARA | Absolute Rotation Angle |
| CVA | Craniovertebral Angle |
| CMP | Chronic Myofascial Pain |
| FHP | Forward Head Posture |
| ICC | Intra-examiner Correlation Coefficient |
| ROM | Range Of Motion |
| RRA | Relative Rotation Angle |
| SVA | Sagittal Vertical Axis |
References
- Harman, K.; Hubley-Kozey, C.L.; Butler, H. Effectiveness of an Exercise Program to Improve Forward Head Posture in Normal Adults: A Randomized, Controlled 10-Week Trial. J. Man. Manip. Ther. 2005, 13, 163–176. [Google Scholar] [CrossRef]
- Griegel-Morris, P.; Larson, K.; Mueller-Klaus, K.; Oatis, C.A. Incidence of Common Postural Abnormalities in the Cervical, Shoulder, and Thoracic Regions and Their Association with Pain in Two Age Groups of Healthy Subjects. Proc. Phys. Ther. 1992, 72, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, N.F.; Hassan, K.A.; Abdelmajeed, S.F.; Moustafa, I.M.; Silva, A.G. The Relationship Between Forward Head Posture and Neck Pain: A Systematic Review and Meta-Analysis. Curr. Rev. Musculoskelet. Med. 2019, 12, 562–577. [Google Scholar] [CrossRef]
- Quek, J.; Pua, Y.H.; Clark, R.A.; Bryant, A.L. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man. Ther. 2013, 18, 65–71. [Google Scholar] [CrossRef]
- Ahmadipoor, A.; Khademi-Kalantari, K.; Rezasoltani, A.; Naimi, S.S.; Akbarzadeh-Baghban, A. Effect of Forward Head Posture on Dynamic Balance Based on the Biodex Balance System. J. Biomed. Phys. Eng. 2022, 12, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H. Effects of Forward Head Posture on Static and Dynamic Balance Control. J. Phys. Ther. Sci. 2016, 28, 274–277. [Google Scholar] [CrossRef]
- Koseki, T.; Kakizaki, F.; Hayashi, S.; Nishida, N.; Itoh, M. Effect of Forward Head Posture on Thoracic Shape and Respiratory Function. J. Phys. Ther. Sci. 2019, 31, 63–68. [Google Scholar] [CrossRef]
- Patwardhan, A.G.; Khayatzadeh, S.; Havey, R.M.; Voronov, L.I.; Smith, Z.A.; Kalmanson, O.; Ghanayem, A.J.; Sears, W. Cervical sagittal balance: A biomechanical perspective can help clinical practice. Eur. Spine J. 2018, 27 (Suppl. S1), 25–38. [Google Scholar] [CrossRef] [PubMed]
- Ling, F.P.; Chevillotte, T.; Leglise, A.; Thompson, W.; Bouthors, C.; Le Huec, J.C. Which parameters are relevant in sagittal balance analysis of the cervical spine? A literature review. Eur. Spine J. 2018, 27 (Suppl. S1), 8–15. [Google Scholar] [CrossRef]
- Harrison, D.D. CBP Technique: The Physics of Spinal Correction. National Library of Medicine #WE 725 4318C, 1982–1997.
- Jackson, B.L.; Harrison, D.D.; Robertson, G.A.; Barker, W.F. Chiropractic biophysics lateral cervical film analysis reliability. J. Manip. Physiol. Ther. 1993, 16, 384–391. [Google Scholar]
- Harrison, D.D.; Janik, T.J.; Troyanovich, S.J.; Holland, B. Comparisons of lordotic cervical spine curvatures to a theoretical ideal model of the static sagittal cervical spine. Spine 1996, 21, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.A.; Scheer, J.K.; Smith, J.S.; Deviren, V.; Bess, S.; Hart, R.A.; Lafage, V.; Shaffrey, C.I.; Schwab, F.; Ames, C.P.; et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2012, 71, 662–669. [Google Scholar] [CrossRef]
- Norton, T.C.; Oakley, P.A.; Haas, J.W.; Harrison, D.E. Positive Outcomes Following Cervical Acceleration-Deceleration (CAD) Injury Using Chiropractic BioPhysics® Methods: A Pre-Auto Injury and Post-Auto Injury Case Series. J. Clin. Med. 2023, 12, 6414. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Tian, S.; Zhang, J.; He, M.; Deng, L.; Ding, W.; Wang, Z.; Yang, D. Comparison of Cervical Sagittal Parameters among Patients with Neck Pain and Patients with Cervical Spondylotic Radiculopathy and Cervical Spondylotic Myelopathy. Orthop. Surg. 2024, 16, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Pivotto, L.R.; Navarro, I.J.R.L.; Candotti, C.T. Radiography and photogrammetry-based methods of assessing cervical spine posture in the sagittal plane: A systematic review with meta-analysis. Gait Posture 2021, 84, 357–367. [Google Scholar] [CrossRef]
- Mylonas, K.; Tsekoura, M.; Billis, E.; Aggelopoulos, P.; Tsepis, E.; Fousekis, K. Reliability and Validity of Non-radiographic Methods of Forward Head Posture Measurement: A Systematic Review. Cureus 2022, 14, e27696. [Google Scholar] [CrossRef]
- Moustafa, I.M.; Diab, A.A.; Hegazy, F.; Harrison, D.E. Demonstration of Central Conduction Time and Neuroplastic Changes after Cervical Lordosis Rehabilitation in Asymptomatic Subjects: A Randomized, Placebo-Controlled Trial. Sci. Rep. 2021, 11, 15379. [Google Scholar] [CrossRef]
- Moustafa, I.; Youssef, A.S.; Ahbouch, A.; Harrison, D.E. Demonstration of Autonomic Nervous Function and Cervical Sensorimotor Control After Cervical Lordosis Rehabilitation: A Randomized Controlled Trial. J. Athl. Train. 2021, 56, 427–436. [Google Scholar] [CrossRef] [PubMed]
- van Niekerk, S.M.; Louw, Q.; Vaughan, C.; Grimmer-Somers, K.; Schreve, K. Photographic measurement of upper-body sitting posture of high school students: A reliability and validity study. BMC Musculoskelet. Disord. 2008, 9, 113. [Google Scholar] [CrossRef]
- Moustafa, I.M.; Diab, A.A.; Hegazy, F.; Harrison, D.E. Does Improvement towards a Normal Cervical Sagittal Configuration Aid in the Management of Cervical Myofascial Pain Syndrome: A 1- Year Randomized Controlled Trial. BMC Musculoskelet. Disord. 2018, 19, 396. [Google Scholar] [CrossRef]
- Yip, C.H.; Chiu, T.T.; Poon, A.T. The relationship between head posture and severity and disability of patients with neck pain. Man. Ther. 2008, 13, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Singla, D.; Veqar, Z.; Hussain, M.E. Photogrammetric Assessment of Upper Body Posture Using Postural Angles: A Literature Review. J. Chiropr. Med. 2017, 16, 131–138. [Google Scholar] [CrossRef]
- Falla, D.; Jull, G.; Russell, T.; Vicenzino, B.; Hodges, P. Effect of Neck Exercise on Sitting Posture in Patients with Chronic Neck Pain. Phys. Ther. 2007, 87, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Diab, A.A.; Moustafa, I.M. The efficacy of forward head correction on nerve root function and pain in cervical spondylotic radiculopathy: A randomized trial. Clin. Rehabil. 2012, 26, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Holland, B.; Harrison, D.D.; Janik, T.J. Further reliability analysis of the Harrison radiographic line-drawing methods: Crossed ICCs for lateral posterior tangents and modified Risser-Ferguson method on AP views. J. Manip. Physiol. Ther. 2002, 25, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Song, K.S.; Park, S.H.; Kang, H.; Daniel Riew, K. Does whole-spine lateral radiograph with clavicle positioning reflect the correct cervical sagittal alignment? Eur. Spine J. 2015, 24, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Gore, D.R.; Sepic, S.B.; Gardner, G.M. Roentgenographic findings of the cervical spine in asymptomatic people. Spine 1986, 11, 521–524. [Google Scholar] [CrossRef]
- Roguski, M.; Benzel, E.C.; Curran, J.N.; Magge, S.N.; Bisson, E.F.; Krishnaney, A.A.; Steinmetz, M.P.; Butler, W.E.; Heary, R.F.; Ghogawala, Z. Postoperative cervical sagittal imbalance negatively affects outcomes after surgery for cervical spondylotic myelopathy. Spine 2014, 39, 2070–2077. [Google Scholar] [CrossRef]
- Moore, D.S.; Notz, W.I.; Flinger, M.A. The Basic Practice of Statistics, 6th ed.; W. H. Freeman and Company: New York, NY, USA, 2013; p. 138. [Google Scholar]
- Tafti, A.; Byerly, D.W. X-Ray Image Acquisition. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK563236/ (accessed on 19 February 2024).
- Stincel, O.R.; Oravitan, M.; Pantea, C.; Almajan-Guta, B.; Mirica, N.; Boncu, A.; Avram, C. Assessment of Forward Head. Posture and Ergonomics in Young IT Professionals—Reasons to Worry? Med. Lav. 2023, 114, e2023006. [Google Scholar] [CrossRef]
- Szczygieł, E.; Fudacz, N.; Golec, J.; Golec, E. The impact of the position of the head on the functioning of the human body: A systematic review. Int. J. Occup. Med. Environ. Health 2020, 33, 559–568. [Google Scholar] [CrossRef]
- Boland, D.M.; Neufeld, E.V.; Ruddell, J.; Dolezal, B.A.; Cooper, C.B. Inter- and intra-rater agreement of static posture analysis using a mobile application. J. Phys. Ther. Sci. 2016, 28, 3398–3402. [Google Scholar] [CrossRef] [PubMed]
- Kan, S.; Fortuna, J.; Nur, S. Can a Mobile Application Be Used to Assess Postural Alignment in Clinic? Canadian Society for Biomechanics: Hamilton, ON, USA, 2016. [Google Scholar]
- Hopkins, B.B.; Vehrs, P.R.; Fellingham, G.W.; George, J.D.; Hager, R.; Ridge, S.T. Validity and Reliability of Standing Posture Measurements Using a Mobile Application. J. Manip. Physiol. Ther. 2019, 42, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Molaeifar, S.; Yazdani, F.; Yoosefinejad, A.K.; Karimi, M.T. Correlation between craniovertebral angle in the sagittal plane and angles and indices measured in the frontal plane at the moment of inducing forward head posture. Work 2021, 68, 1221–1227. [Google Scholar] [CrossRef]
- Cote, R.; Vietas, C.; Kolakowski, M.; Lombardo, K.; Prete, J.; Dashottar, A. Inter and intra-rater reliability of measuring photometric craniovertebral angle using a cloud-based video communication platform. Int. J. Telerehabil. 2021, 13. [Google Scholar] [CrossRef]
- Mostafaee, N.; Pirayeh, N.; HasanNia, F.; Negahban, H.; Kasnavi, M. Examining accuracy of and determining the best cutoff point for photographic-based postural angles to discriminate between slight and moderate-to-severe forward head posture. Physiother. Theory Pract. 2024, 40, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Nouh, M.R. Imaging of the spine: Where do we stand? World J. Radiol. 2019, 11, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Doody, M.M.; Lonstein, J.E.; Stovall, M.; Hacker, D.G.; Luckyanov, N.; Land, C.E. Breast cancer mortality after diagnostic radiography: Findings from the U.S. Scoliosis Cohort Study. Spine 2000, 25, 2052–2063. [Google Scholar] [CrossRef] [PubMed]
- Fullenlove, T.M.; Williams, A.J. Comparative roentgen findings in symptomatic and asymptomatic backs. Radiology 1957, 68, 572–574. [Google Scholar] [CrossRef] [PubMed]
- Schwanke, N.L.; Pohl, H.H.; Reuter, C.P.; Borges, T.S.; de Souza, S.; Burgos, M.S. Differences in body posture, strength and flexibility in schoolchildren with overweight and obesity: A quasi-experimental study. Man. Ther. 2016, 22, 138–144. [Google Scholar] [CrossRef]
- Goo, B.W.; Oh, J.H.; Kim, J.S.; Lee, M.Y. Effects of cervical stabilization with visual feedback on craniovertebral angle and proprioception for the subjects with forward head posture. Medicine 2024, 103, e36845. [Google Scholar] [CrossRef]
- Nightingale, R.W.; Camacho, D.L.; Armstrong, A.J.; Robinette, J.J.; Myers, B.S. Inertial properties and loading rates affect buckling modes and injury mechanisms in the cervical spine. J. Biomech. 2000, 33, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.F.; Lui, E.M. Structural Instability: Theory and Implementation; Elsevier: New York, NY, USA, 1987; pp. 4–10. [Google Scholar]
- Oakley, P.O.A.; Moustafa, I.M.; Harrison, D.E. Restoration of Cervical and Lumbar Lordosis: CBP® Methods Overview. In Spinal Deformities in Adolescents, Adults and Older Adults; IntechOpen: London, UK, 2021. [Google Scholar] [CrossRef]
- Frane, N.; Bitterman, A. Radiation Safety and Protection. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK557499/ (accessed on 19 February 2024).
- Tafti, D.; Maani, C.V. X-ray Production. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK537046/ (accessed on 19 February 2024).
- Katzman, W.B.; Parimi, N.; Gladin, A.; Fan, B.; Wong, S.S.; Mergenthaler, J.; Lane, N.E. Reliability of sagittal vertical axis measurement and association with measures of age-related hyperkyphosis. J. Phys. Ther. Sci. 2018, 30, 1417–1423. [Google Scholar] [CrossRef] [PubMed]
- Hammerberg, E.M.; Wood, K.B. Sagittal profile of the elderly. J. Spinal Disord. Tech. 2003, 16, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Asai, Y.; Tsutsui, S.; Oka, H.; Yoshimura, N.; Hashizume, H.; Yamada, H.; Akune, T.; Muraki, S.; Matsudaira, K.; Kawaguchi, H.; et al. Sagittal spino-pelvic alignment in adults: The Wakayama Spine Study. PLoS ONE 2017, 12, e0178697. [Google Scholar] [CrossRef] [PubMed]
- Ames, C.P.; Smith, J.S.; Eastlack, R.; Blaskiewicz, D.J.; Shaffrey, C.I.; Schwab, F.; Bess, S.; Kim, H.J.; Mundis, G.M., Jr.; Klineberg, E.; et al. Reliability assessment of a novel cervical spine deformity classification system. J. Neurosurg. Spine 2015, 23, 673–683. [Google Scholar] [CrossRef] [PubMed]
- Marques, C.; Granström, E.; MacDowall, A.; Moreira, N.C.; Skeppholm, M.; Olerud, C. Accuracy and Reliability of X-ray Measurements in the Cervical Spine. Asian Spine J. 2020, 14, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Troyanovich, S.J.; Harrison, D.E.; Harrison, D.D.; Holland, B.; Janik, T.J. Further analysis of the reliability of the posterior tangent lateral lumbar radiographic mensuration procedure: Concurrent validity of computer-aided X-ray digitization. J. Manip. Physiol. Ther. 1998, 21, 460–467. [Google Scholar]
- Martini, M.L.; Neifert, S.N.; Chapman, E.K.; Mroz, T.E.; Rasouli, J.J. Cervical Spine Alignment in the Sagittal Axis: A Review of the Best Validated Measures in Clinical Practice. Global Spine J. 2021, 11, 1307–1312. [Google Scholar] [CrossRef]
- Kato, M.; Namikawa, T.; Matsumura, A.; Konishi, S.; Nakamura, H. Effect of Cervical Sagittal Balance on Laminoplasty in Patients with Cervical Myelopathy. Global Spine J. 2017, 7, 154–161. [Google Scholar] [CrossRef]
- Xu, Z.; Rao, H.; Zhang, L.; Li, G.; Xu, Z.; Xu, W. Anterior cervical discectomy and fusion versus hybrid decompression and fusion for the treatment of 3-level cervical spondylotic myelopathy: A comparative analysis of cervical sagittal balance and outcomes. World Neurosurg. 2019, 132, e752–e758. [Google Scholar] [CrossRef]
- Fan, X.-W.; Wang, Z.-W.; Gao, X.-D.; Ding, W.-Y.; Yang, D.-L. The change of cervical sagittal parameters plays an important role in clinical outcomes of cervical spondylotic myelopathy after multi-level anterior cervical discectomy and fusion. J. Orthop. Surg. Res. 2019, 14, 429. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.D.; Harrison, D.E.; Janik, T.J.; Cailliet, R.; Ferrantelli, J.R.; Haas, J.W.; Holland, B. Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: Results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine 2004, 29, 2485–2492. [Google Scholar] [CrossRef] [PubMed]
- McAviney, J.; Schulz, D.; Bock, R.; Harrison, D.E.; Holland, B. Determining the relationship between cervical lordosis and neck complaints. J. Manip. Physiol. Ther. 2005, 28, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Schultz, C.H.; Fairley, R.; Murphy, L.S.; Doss, M. The Risk of Cancer from CT Scans and Other Sources of Low-Dose Radiation: A Critical Appraisal of Methodologic Quality. Prehosp. Disaster Med. 2020, 35, 3–16. [Google Scholar] [CrossRef]








| Variable | Mean ± SD | ||
|---|---|---|---|
| Age (years) | 32.5 ± 7.5 | ||
| Weight (kg) | 77 ± 10.5 | ||
| Neck pain intensity (NRS) | 5.2 ± 0.8 | ||
| Gender (%) | |||
| Male | 63.3 | ||
| Female | 36.7 | ||
| FHP Variables | Mean ± SD | Maximum | Minimum |
| AHT Tz C2–C7 (cm) | 2.46 ± 0.62 | 3.7 | 1.5 |
| ARA C2–C7 (°) | −6.80 ± 5.98 | −17 | 0 |
| CVA (°) | 44.9 ± 3.33 | 51 | 40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oakley, P.A.; Moustafa, I.M.; Haas, J.W.; Betz, J.W.; Harrison, D.E. Two Methods of Forward Head Posture Assessment: Radiography vs. Posture and Their Clinical Comparison. J. Clin. Med. 2024, 13, 2149. https://doi.org/10.3390/jcm13072149
Oakley PA, Moustafa IM, Haas JW, Betz JW, Harrison DE. Two Methods of Forward Head Posture Assessment: Radiography vs. Posture and Their Clinical Comparison. Journal of Clinical Medicine. 2024; 13(7):2149. https://doi.org/10.3390/jcm13072149
Chicago/Turabian StyleOakley, Paul A., Ibrahim M. Moustafa, Jason W. Haas, Joseph W. Betz, and Deed E. Harrison. 2024. "Two Methods of Forward Head Posture Assessment: Radiography vs. Posture and Their Clinical Comparison" Journal of Clinical Medicine 13, no. 7: 2149. https://doi.org/10.3390/jcm13072149
APA StyleOakley, P. A., Moustafa, I. M., Haas, J. W., Betz, J. W., & Harrison, D. E. (2024). Two Methods of Forward Head Posture Assessment: Radiography vs. Posture and Their Clinical Comparison. Journal of Clinical Medicine, 13(7), 2149. https://doi.org/10.3390/jcm13072149










