Exoscopic Minimally Invasive Open-Door Laminoplasty for Cervical Myelopathy: A Technical Note and Preliminary Analysis of Clinical Outcomes during the Acute Postoperative Period
Abstract
1. Introduction
2. Materials and Methods
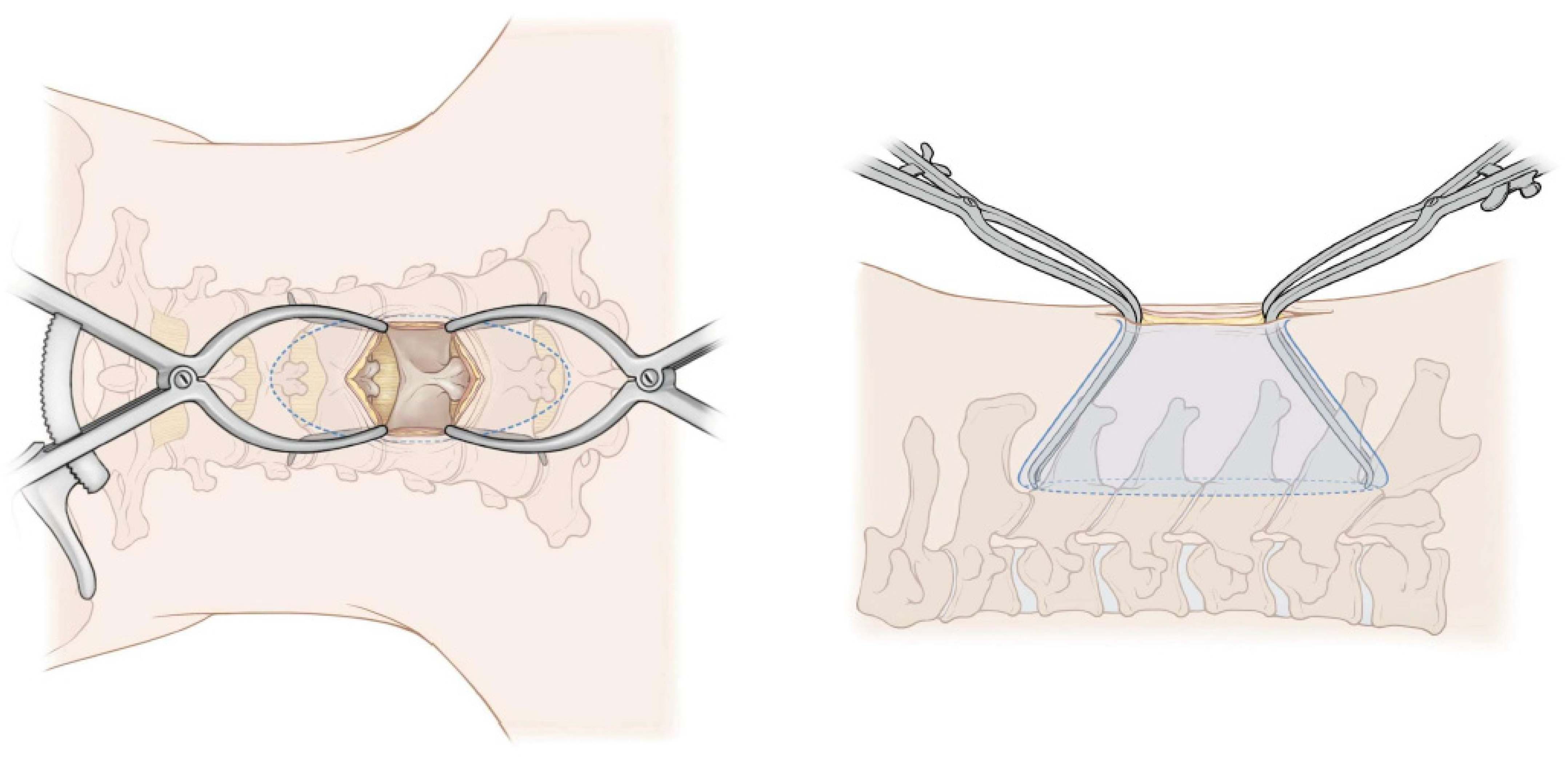
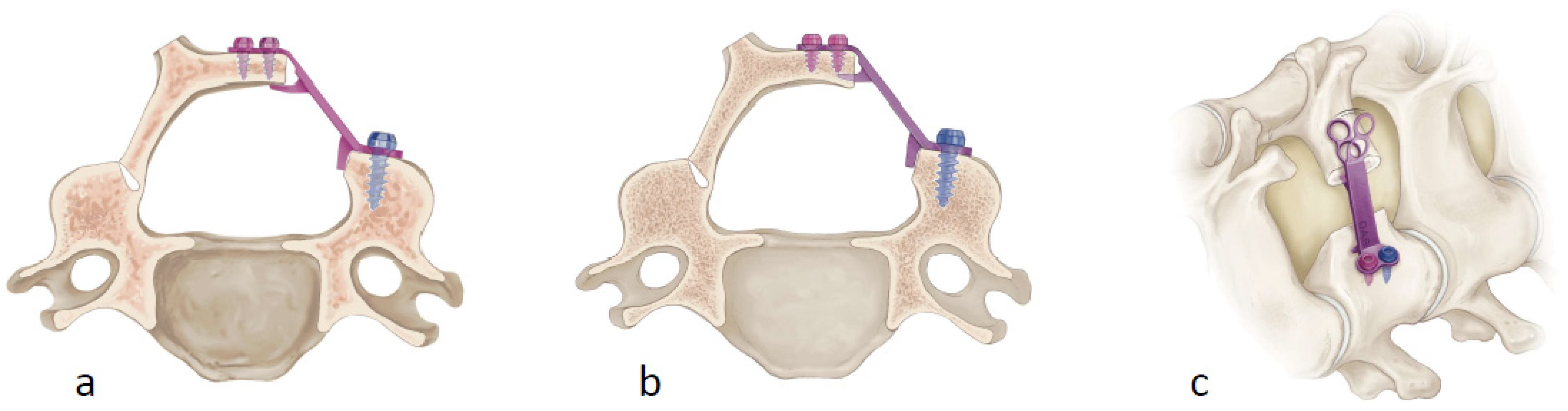
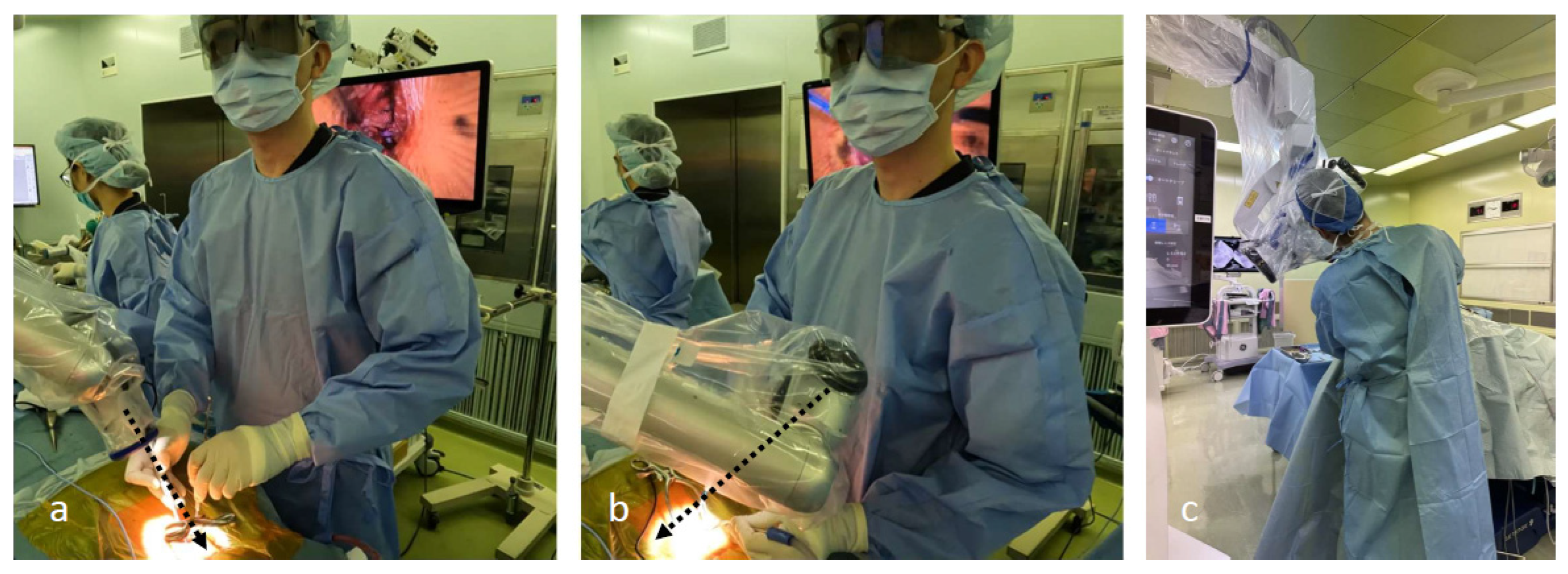
Surgical Technique for exLAP at C3–C6
3. Results
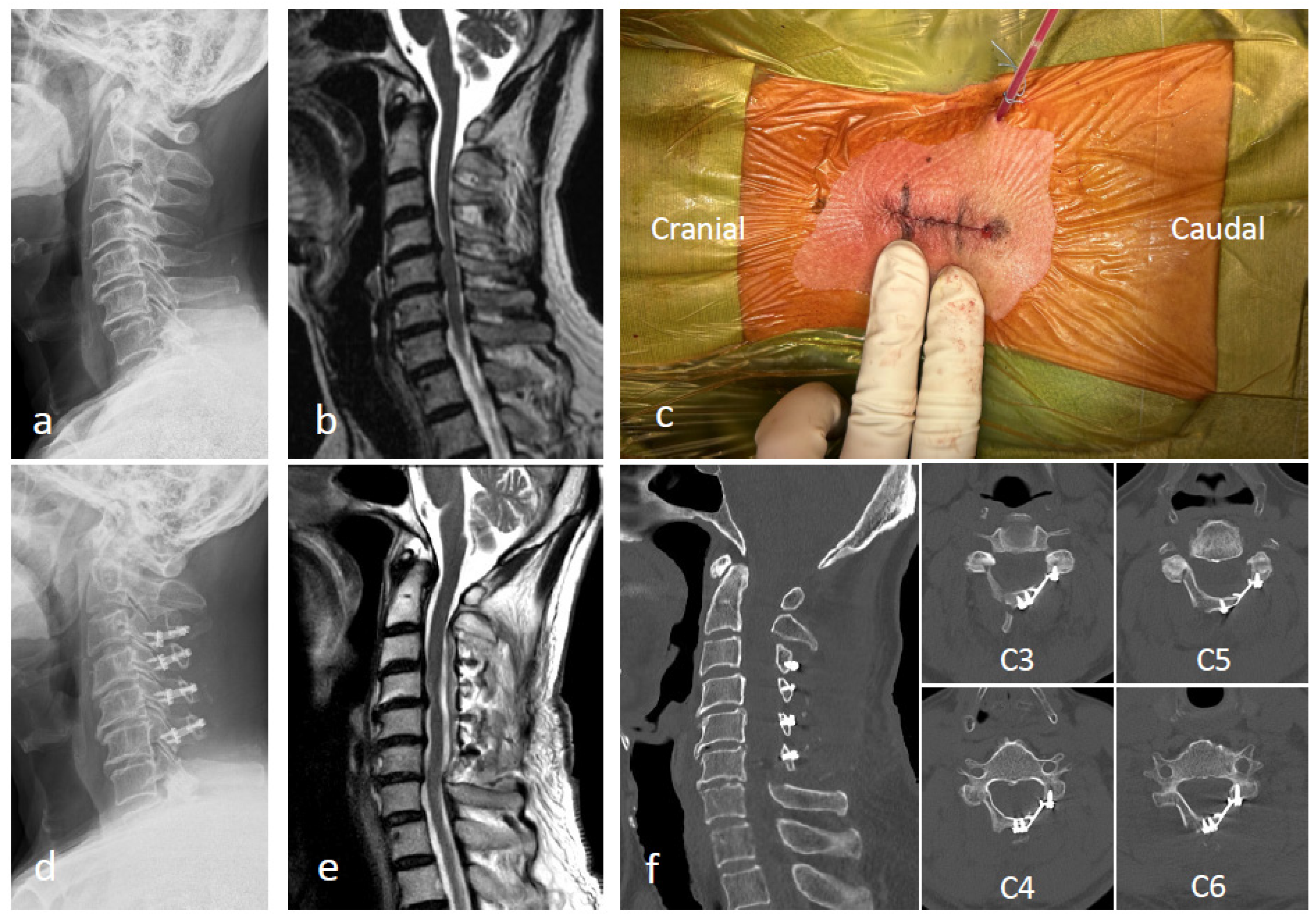
Representative Case
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chiba, K.; Ogawa, Y.; Ishii, K.; Takaishi, H.; Nakamura, M.; Maruiwa, H.; Matsumoto, M.; Toyama, Y. Long-term results of expansive open-door laminoplasty for cervical myelopathy—Average 14-year follow-up study. Spine 2006, 31, 2998–3005. [Google Scholar] [CrossRef] [PubMed]
- Hirabayashi, K.; Miyakawa, J.; Satomi, K.; Maruyama, T.; Wakano, K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine 1981, 6, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Hirabayashi, K.; Watanabe, K.; Wakano, K.; Suzuki, N.; Satomi, K.; Ishii, Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine 1983, 8, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Hirabayashi, K.; Toyama, Y.; Chiba, K. Expansive laminoplasty for myelopathy in ossification of the longitudinal ligament. Clin. Orthop. Relat. Res. 1999, 359, 35–48. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Nakamura, H.; Konishi, S.; Dohzono, S.; Toyoda, H.; Fukushima, W.; Kondo, K.; Matsuda, H. Effect of preserving paraspinal muscles on postoperative axial pain in the selective cervical laminoplasty. Spine 2008, 33, E455–E459. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Gao, Y.; Gao, K.; Yu, Z.; Lv, D.; Ma, H.; Zhai, G. Factors associated with postoperative axial symptom after expansive open-door laminoplasty: Retrospective study using multivariable analysis. Eur. Spine J. 2020, 29, 2838–2844. [Google Scholar] [CrossRef] [PubMed]
- Murai, Y.; Sato, S.; Yui, K.; Morimoto, D.; Ozeki, T.; Yamaguchi, M.; Tateyama, K.; Nozaki, T.; Tahara, S.; Yamaguchi, F.; et al. Preliminary Clinical Microneurosurgical Experience With the 4K3-Dimensional Microvideoscope (ORBEYE) System for Microneurological Surgery: Observation Study. Oper. Neurosurg. 2019, 16, 707–716. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, S.; Toda, M.; Nishimoto, M.; Ishihara, E.; Miwa, T.; Akiyama, T.; Horiguchi, T.; Sasaki, H.; Yoshida, K. Pros and cons of using ORBEYE™ for microneurosurgery. Clin. Neurol. Neurosurg. 2018, 174, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Minamide, A.; Yoshida, M.; Simpson, A.K.; Yamada, H.; Hashizume, H.; Nakagawa, Y.; Iwasaki, H.; Tsutsui, S.; Okada, M.; Takami, M.; et al. Microendoscopic laminotomy versus conventional laminoplasty for cervical spondylotic myelopathy: 5-year follow-up study. J. Neurosurg. Spine 2017, 27, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.B.; Ma, Y.J.; Ma, H.J.; Zhang, X.Y.; Zhou, H.G. Clinical efficacy of posterior percutaneous endoscopic unilateral laminotomy with bilateral decompression for symptomatic cervical spondylotic myelopathy. Orthop. Surg. 2022, 14, 876–884. [Google Scholar] [CrossRef] [PubMed]
- Santiago, P.; Fessler, R.G. Minimally invasive surgery for the management of cervical spondylosis. Neurosurgery 2007, 60, S160–S165. [Google Scholar] [CrossRef] [PubMed]
- Benglis, D.M.; Guest, J.D.; Wang, M.Y. Clinical feasibility of minimally invasive cervical laminoplasty. Neurosurg. Focus 2008, 25, E3. [Google Scholar] [CrossRef] [PubMed]
- Yamane, K.; Sugimoto, Y.; Tanaka, M.; Arataki, S.; Takigawa, T.; Ozaki, T. Laminar closure rates in patients with cervical myelopathies treated with either open-door laminoplasty with reattachment of spinous processes and extensor musculature or Hirabayashi open-door laminoplasty: A case-control study. Eur. Spine J. 2016, 25, 1869–1874. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, T. Skip laminectomy—A new treatment for cervical spondylotic myelopathy, preserving bilateral muscular attachments to the spinous processes: A preliminary report. Spine J. 2002, 2, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Yuan, W.; Zhu, Y.; Liu, X.; Zhou, X.; Cui, C. Laminoplasty versus skip laminectomy for the treatment of multilevel cervical spondylotic myelopathy: A systematic review. Arch. Orthop. Trauma Surg. 2014, 134, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Li, Y.; Zhao, J.; Zou, Y.; Gu, R.; Li, H. Skip Laminectomy Compared with Laminoplasty for Cervical Compressive Myelopathy: A Systematic Review and Meta-Analysis. World Neurosurg. 2018, 120, 296–301. [Google Scholar] [CrossRef]




| Characteristics | Group M (exLAP) | Group H (Conventional) | p-Value |
|---|---|---|---|
| Patients (no.) | 17 | 11 | |
| Age (years) | 70 ± 11 | 71 ± 10 | 0.932 |
| Sex | |||
| Male | 13 | 9 | |
| Female | 4 | 2 | |
| Diagnosis | |||
| CSM | 15 | 7 | |
| OPLL | 2 | 4 | |
| Preoperative lordosis angle (°) | 12 ± 10 | 4 ± 13 | 0.116 |
| Skin incision length (mm) | 34 ± 2 | 84 ± 14 | <0.001 |
| Operative time (min) | 89 ± 17 | 81 ± 31 | 0.360 |
| Intraoperative blood loss (mL) | 37 ± 54 | 62 ± 54 | 0.246 |
| NRS Scores for Neck Pain | Group M (exLAP) | Group H (Conventional) | p-Value |
|---|---|---|---|
| Day 3 | 4.0 ± 2.1 | 6.6 ± 2.3 | 0.004 |
| Day 5 | 3.5 ± 1.2 | 5.1 ± 2.3 | 0.025 |
| Day 7 | 2.4 ± 1.1 | 4.9 ± 2.0 | <0.001 |
| Day 14 | 1.0 ± 1.1 | 3.1 ± 1.2 | <0.001 |
| Group M (exLAP) | Group H (Conventional) | p-Value | |
|---|---|---|---|
| Frequency of analgesic use | 5 ± 3 | 8 ± 6 | 0.062 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamane, K.; Narita, W.; Takao, S.; Takeuchi, K. Exoscopic Minimally Invasive Open-Door Laminoplasty for Cervical Myelopathy: A Technical Note and Preliminary Analysis of Clinical Outcomes during the Acute Postoperative Period. J. Clin. Med. 2024, 13, 2173. https://doi.org/10.3390/jcm13082173
Yamane K, Narita W, Takao S, Takeuchi K. Exoscopic Minimally Invasive Open-Door Laminoplasty for Cervical Myelopathy: A Technical Note and Preliminary Analysis of Clinical Outcomes during the Acute Postoperative Period. Journal of Clinical Medicine. 2024; 13(8):2173. https://doi.org/10.3390/jcm13082173
Chicago/Turabian StyleYamane, Kentaro, Wataru Narita, Shinichiro Takao, and Kazuhiro Takeuchi. 2024. "Exoscopic Minimally Invasive Open-Door Laminoplasty for Cervical Myelopathy: A Technical Note and Preliminary Analysis of Clinical Outcomes during the Acute Postoperative Period" Journal of Clinical Medicine 13, no. 8: 2173. https://doi.org/10.3390/jcm13082173
APA StyleYamane, K., Narita, W., Takao, S., & Takeuchi, K. (2024). Exoscopic Minimally Invasive Open-Door Laminoplasty for Cervical Myelopathy: A Technical Note and Preliminary Analysis of Clinical Outcomes during the Acute Postoperative Period. Journal of Clinical Medicine, 13(8), 2173. https://doi.org/10.3390/jcm13082173





