The Influence of Increased Pedicle Screw Diameter and Thicker Rods on Surgical Results in Adolescents Undergoing Posterior Spinal Fusion for Idiopathic Scoliosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Patients
2.2. Outcome Parameters
2.3. Radiological Measures
2.4. Surgical Technique
2.5. Statistical Considerations
3. Results
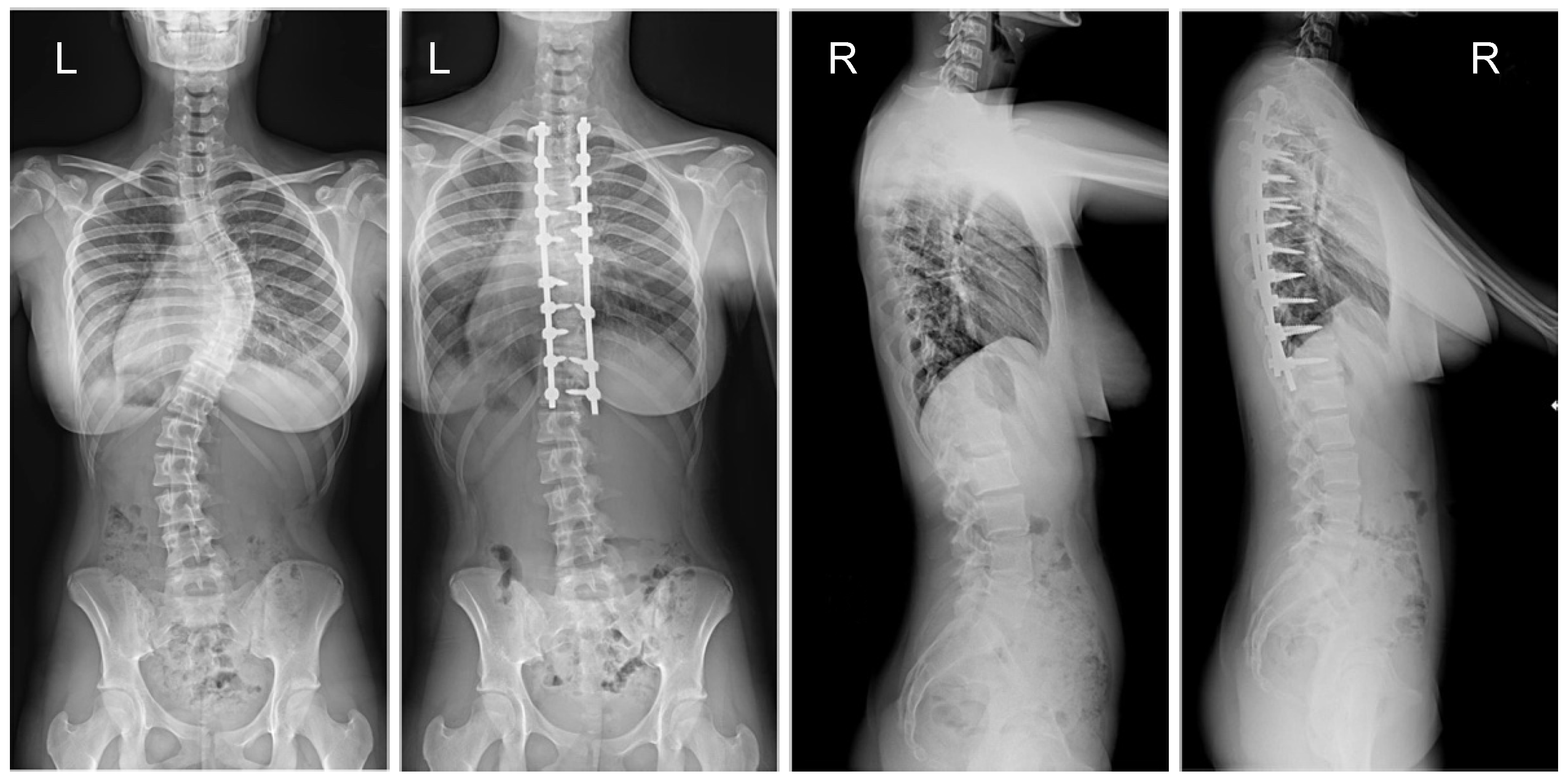
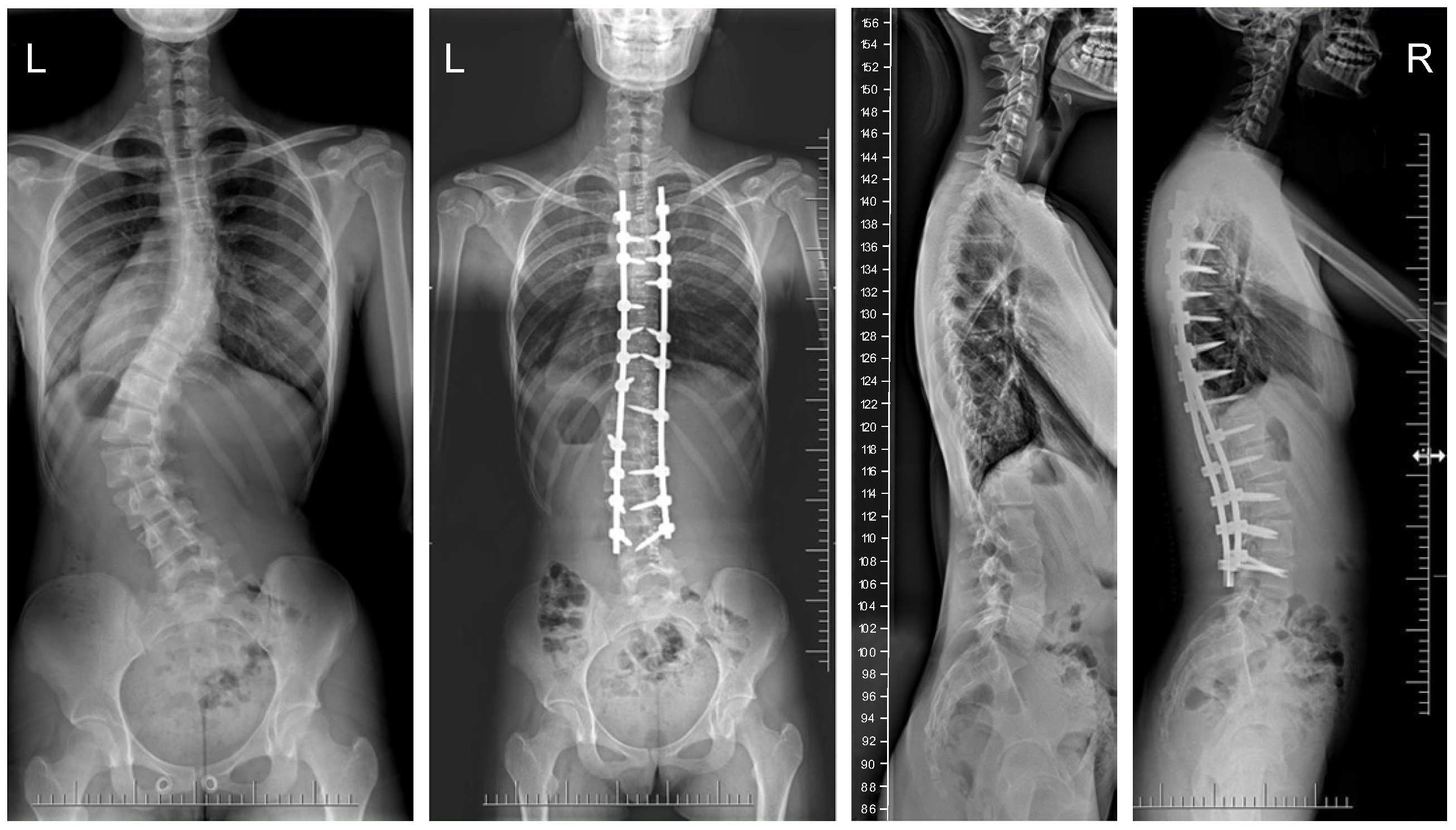
3.1. Clinical Characteristics and Radiographic Outcomes
3.2. HRQoL
3.3. Complications
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Weinstein, S.L.; Dolan, L.A.; Cheng, J.C.; Danielsson, A.; Morcuende, J.A. Adolescent idiopathic scoliosis. Lancet 2008, 371, 1527–1537. [Google Scholar] [CrossRef] [PubMed]
- Parent, S.; Newton, P.O.; Wenger, D.R. Adolescent idiopathic scoliosis: Etiology, anatomy, natural history, and bracing. Instr. Course Lect. 2005, 54, 529–536. [Google Scholar] [PubMed]
- Addai, D.; Zarkos, J.; Bowey, A.J. Current concepts in the diagnosis and management of adolescent idiopathic scoliosis. Childs Nerv. Syst. 2020, 36, 1111–1119. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.A.; Henstenburg, J.M.; Newton, P.O.; Parent, S. Updated Criteria for Fusion Level Selection in Adolescent Idiopathic Scoliosis Including Use of Three-Dimensional Analysis. J. Am. Acad. Orthop. Surg. 2023, 31, e298–e307. [Google Scholar] [CrossRef] [PubMed]
- Al-Iede, M.M.; Al-Zayadneh, E.; Bridge, C.; Alqutawneh, B.; Waters, K. Risk factors for postoperative pulmonary complications in children with severely compromised pulmonary function secondary to severe scoliosis. Pediatr. Pulmonol. 2020, 55, 2782–2790. [Google Scholar] [CrossRef] [PubMed]
- Turczynowicz, A.; Jakubów, P.; Niedźwiecka, K.; Kondracka, J.; Pużyńska, W.; Tałałaj, M.; Guszczyn, T.; Grabala, P.; Kowalczuk, O.; Kocańda, S. Mu-Opioid Receptor 1 and C-Reactive Protein Single Nucleotide Polymorphisms as Biomarkers of Pain Intensity and Opioid Consumption. Brain Sci. 2023, 13, 1629. [Google Scholar] [CrossRef] [PubMed]
- Grabala, P.; Helenius, I.J.; Buchowski, J.M.; Shah, S.A. The Efficacy of a Posterior Approach to Surgical Correction for Neglected Idiopathic Scoliosis: A Comparative Analysis According to Health-Related Quality of Life, Pulmonary Function, Back Pain and Sexual Function. Children 2023, 10, 299. [Google Scholar] [CrossRef] [PubMed]
- Tambe, A.D.; Panikkar, S.J.; Millner, P.A.; Tsirikos, A.I. Current concepts in the surgical management of adolescent idiopathic scoliosis. Bone Joint J. 2018, 100, 415–424. [Google Scholar] [CrossRef]
- Larson, A.N.; Marks, M.C.; Gonzalez Sepulveda, J.M.; Newton, P.O.; Devlin, V.J.; Peat, R.; Tarver, M.E.; Babalola, O.; Chen, A.L.; Gebben, D.; et al. Non-Fusion Versus Fusion Surgery in Pediatric Idiopathic Scoliosis: What Trade-Offs in Outcomes Are Acceptable for the Patient and Family? J. Bone Joint Surg. Am. 2024, 106, 2–9. [Google Scholar] [CrossRef]
- Suk, S.I.; Kim, J.H.; Kim, S.S.; Lim, D.J. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). Eur. Spine J. 2012, 21, 13–22. [Google Scholar] [CrossRef]
- Seki, S.; Kawaguchi, Y.; Nakano, M.; Makino, H.; Mine, H.; Kimura, T. Rod rotation and differential rod contouring followed by direct vertebral rotation for treatment of adolescent idiopathic scoliosis: Effect on thoracic and thoracolumbar or lumbar curves assessed with intraoperative computed tomography. Spine J. 2016, 16, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Pankowski, R.; Roclawski, M.; Ceynowa, M.; Mikulicz, M.; Mazurek, T.; Kloc, W. Direct Vertebral Rotation Versus Single Concave Rod Rotation: Low-dose Intraoperative Computed Tomography Evaluation of Spine Derotation in Adolescent Idiopathic Scoliosis Surgery. Spine 2016, 41, 864–871. [Google Scholar] [CrossRef] [PubMed]
- Urbanski, W.; Markowski, P.; Zaluski, R.; Kokaveshi, A.; Morasiewicz, P. Direct Vertebral Rotation (DVR) Does Not. Improve Clinical and Radiological Results Compared to Differential Rod. Contouring (DRC) in Patients Treated Surgically for Idiopathic Scoliosis. J. Clin. Med. 2023, 12, 4091. [Google Scholar] [CrossRef] [PubMed]
- Lowenstein, J.; Matsumoto, H.; Vitale, M.; Weidenbaum, M.; Gomez, J.A.; Lee, F.Y.-I.; Hyman, J.E.; Roye, D.P., Jr. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: A comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine 2007, 32, 448–452. [Google Scholar] [CrossRef] [PubMed]
- Sabah, Y.; Clément, J.L.; Solla, F.; Rosello, O.; Rampal, V. Cobalt-chrome and titanium alloy rods provide similar coronal and sagittal correction in adolescent idiopathic scoliosis. Orthop. Traumatol. Surg. Res. 2018, 104, 1073–1077. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.H.; Suh, S.W.; Chang, D.G. Comparison of surgical correction rates between titanium and cobalt-chrome-alloy as rod materials in adolescent idiopathic scoliosis. Sci. Rep. 2020, 10, 10053. [Google Scholar] [CrossRef] [PubMed]
- Ruffilli, A.; Fiore, M.; Viroli, G.; Barile, F.; Manzetti, M.; Martikos, K.; Greggi, T.; Faldini, C. 5.5-mm Cobalt-Chrome vs 6-mm Titanium Alloy Rods in Surgical Treatment of Lenke 1 Adolescent Idiopathic Scoliosis with High-Density Pedicle Screws and Direct Vertebral Rotation on Differently Shaped Rods: A Retrospective Comparative Cohort Study. Int. J. Spine Surg. 2023, 17, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Ohrt-Nissen, S.; Dahl, B.; Gehrchen, M. Choice of Rods in Surgical Treatment of Adolescent Idiopathic Scoliosis: What Are the Clinical Implications of Biomechanical Properties?—A Review of the Literature. Neurospine 2018, 15, 123–130. [Google Scholar] [CrossRef]
- Han, S.; Hyun, S.J.; Kim, K.J.; Jahng, T.A.; Kim, H.J. Comparative Study Between Cobalt Chrome and Titanium Alloy Rods for Multilevel Spinal Fusion: Proximal Junctional Kyphosis More Frequently Occurred in Patients Having Cobalt Chrome Rods. World Neurosurg. 2017, 103, 404–409. [Google Scholar] [CrossRef]
- Huang, T.H.; Ma, H.L.; Wang, S.T.; Chou, P.H.; Ying, S.H.; Liu, C.L.; Yu, W.K.; Chang, M.C. Does the size of the rod affect the surgical results in adolescent idiopathic scoliosis? 5.5-mm versus 6.35-mm rod. Spine J. 2014, 14, 1545–1550. [Google Scholar] [CrossRef]
- Sarwahi, V.; Hasan, S.; Koutsogiannis, P.; Visahan, K.; Rao, H.; Patil, A.; Lo, Y.; Amaral, T.; DiMauro, J.P. Effect of Pedicle Screw Size on Surgical Outcomes Following Surgery for 412 Adolescent Idiopathic Scoliosis Patients. Spine 2023, 48, 1544–1551. [Google Scholar] [CrossRef] [PubMed]
- Grabala, P.; Helenius, I.J.; Grabala, M.; Shah, S.A. Influences of Increasing Pedicle Screw Diameter on Widening Vertebral Pedicle Size during Surgery in Spinal Deformities in Children and Adolescents without Higher Risk of Pedicle and Vertebral Breaches. J. Clin. Med. 2023, 12, 5368. [Google Scholar] [CrossRef] [PubMed]
- Bowden, D.; Michielli, A.; Merrill, M.; Will, S. Systematic review and meta-analysis for the impact of rod materials and sizes in the surgical treatment of adolescent idiopathic scoliosis. Spine Deform. 2022, 10, 1245–1263. [Google Scholar] [CrossRef] [PubMed]
- Tsirikos, A.I.; García-Martínez, S. Long-Term Health-Related Quality of Life (QOL) after Paediatric Spinal Deformity Surgery and Comparison with the General. Population J. Clin. Med. 2023, 12, 7142. [Google Scholar] [CrossRef] [PubMed]
- Soini, V.; Syvänen, J.; Helenius, L.; Raitio, A.; Helenius, I. Health-related quality of life after segmental pedicle screw instrumentation: A matched comparison of patients with neuromuscular and adolescent idiopathic scoliosis. Acta Orthop. 2023, 94, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Lenke, L.G. Lenke classification system of adolescent idiopathic scoliosis: Treatment recommendations. Instr. Course Lect. 2005, 54, 537–542. [Google Scholar] [PubMed]
- Charalampidis, A.; Jiang, F.; Wilson, J.R.F.; Badhiwala, J.H.; Brodke, D.S.; Fehlings, M.G. The Use of Intraoperative Neurophysiological Monitoring in Spine Surgery. Global Spine J. 2020, 10 (Suppl. 1), 104S–114S. [Google Scholar] [CrossRef] [PubMed]
- Skaggs, D.L.; Lee, C.; Myung, K.S. Neuromonitoring Changes Are Common and Reversible with Temporary Internal Distraction for Severe Scoliosis. Spine Deform. 2014, 2, 61–69. [Google Scholar] [CrossRef]
- Daubs, M.D.; Kim, Y.J.; Lenke, L.G. Pedicle screw fixation (T1, T2, and T3). Instr. Course Lect. 2007, 56, 247–255. [Google Scholar]
- Chang, S.Y.; Kim, J.H.; Mok, S.; Chang, B.S.; Lee, C.K.; Kim, H. The Use of High-Density Pedicle Screw Construct with Direct Vertebral Derotation of the Lowest Instrumented Vertebra in Selective Thoracic Fusion for Adolescent Idiopathic Scoliosis: Comparison of Two Surgical Strategies. Asian Spine J. 2023, 17, 338–346. [Google Scholar] [CrossRef]
- Suk, S.I.; Lee, C.K.; Kim, W.J.; Chung, Y.J.; Park, Y.B. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine 1995, 20, 1399–1405. [Google Scholar] [CrossRef] [PubMed]
- Suk, S.I. Pedicle screw instrumentation for adolescent idiopathic scoliosis: The insertion technique, the fusion levels and direct vertebral rotation. Clin Orthop Surg. 2011, 3, 89–100. [Google Scholar] [CrossRef]
- Ponte, A.; Orlando, G.; Siccardi, G. The True Ponte Osteotomy: By the One Who Developed It. Spine Deform. 2018, 6, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Floccari, L.; Poppino, K.; Greenhill, D.; Sucato, D. Ponte osteotomies in a matched series of large, A.I.S curves increase surgical risk without improving outcomes. Spine Deform. 2021, 9, 1411–1418. [Google Scholar] [CrossRef]
- Shaheen, M.; Koltsov, J.; Cohen, S.; Langner, J.; Kaur, J.; Segovia, N.; Vorhies, J. Complication risks and costs associated with Ponte osteotomies in surgical treatment of adolescent idiopathic scoliosis: Insights from a national database. Spine Deform. 2022, 10, 1339–1348. [Google Scholar] [CrossRef]
- Faldini, C.; Viroli, G.; Traversari, M.; Manzetti, M.; Ialuna, M.; Sartini, F.; Cargeli, A.; Parisi, S.C.; Ruffilli, A. Ponte Osteotomies in the Surgical Treatment of Adolescent Idiopathic Scoliosis: A Systematic Review of the Literature and Meta-Analysis of Comparative Studies. Children 2024, 11, 92. [Google Scholar] [CrossRef]
- Dalal, A.; Upasani, V.V.; Bastrom, T.P.; Yaszay, B.; Shah, S.A.; Shufflebarger, H.L.; Newton, P.O. Apical vertebral rotation in adolescent idiopathic scoliosis: Comparison of uniplanar and polyaxial pedicle screws. J. Spinal Disord. Tech. 2011, 24, 251–257. [Google Scholar] [CrossRef]
- Crawford, C.H., 3rd; O’Shaughnessy, B.A.; Kuklo, T.R. Basic pedicle screw and construct biomechanics. In The Textbook of Spinal Surgery, 3rd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA; p. 201174–8.
- Tsagkaris, C.; Calek, A.K.; Fasser, M.R.; Spirig, J.M.; Caprara, S.; Farshad, M.; Widmer, J. Bone density optimized pedicle screw insertion. Front. Bioeng. Biotechnol. 2023, 11, 1270522. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Zhao, J.; Sun, X.J.; Zhou, X.H.; Zhang, K.; Xie, Y.Z. Optimizing Lumbar Pedicle Screw Trajectory Utilizing a 3D-Printed Drill Guide to Ensure Placement of Pedicle Screws into Higher Density Bone May Improve Pedicle Screw Pullout Resistance. World Neurosurg. 2022, 158, e459–e464. [Google Scholar] [CrossRef]
- Kim, Y.J.; Lenke, L.G.; Cho, S.K.; Bridwell, K.H.; Sides, B.; Blanke, K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine 2004, 29, 2040–2048. [Google Scholar] [CrossRef]
- Zhang, M.; Chen, W.; Wang, S.; Du, Y.; Zhang, J.; Pu, F. Correlation between supine flexibility and postoperative correction in adolescent idiopathic scoliosis. BMC Musculoskelet. Disord. 2023, 24, 126. [Google Scholar] [CrossRef] [PubMed]
- Vora, V.; Crawford, A.; Babekhir, N.; Boachie-Adjei, O.; Lenke, L.; Peskin, M.; Charles, G.; Kim, Y. A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs: Myth or reality. Spine 2007, 32, 1869–1874. [Google Scholar] [CrossRef] [PubMed]
- Kwok, A.W.; Finkelstein, J.A.; Woodside, T.; Hearn, T.C.; Hu, R.W. Insertional torque and pull-out strengths of conical and cylindrical pedicle screws in cadaveric bone. Spine 1996, 21, 2429–2434. [Google Scholar] [CrossRef] [PubMed]
- Cho, W.; Cho, S.K.; Wu, C. The biomechanics of pedicle screw-based instrumentation. J. Bone Joint Surg. Br. 2010, 92, 1061–1065. [Google Scholar] [CrossRef] [PubMed]
- Lamerain, M.; Bachy, M.; Dubory, A.; Kabbaj, R.; Scemama, C.; Vialle, R. All-Pedicle Screw Fixation with 6-mm Diameter Cobalt-Chromium Rods Provides Optimized Sagittal Correction of Adolescent Idiopathic Scoliosis. Clin. Spine Surg. 2017, 30, E857–E863. [Google Scholar] [CrossRef] [PubMed]
- Clement, J.L.; Chau, E.; Kimkpe, C.; Vallade, M.J. Restoration of thoracic kyphosis by posterior instrumentation in adolescent idiopathic scoliosis: Comparative radiographic analysis of two methods of reduction. Spine 2008, 33, 1579–1587. [Google Scholar] [CrossRef] [PubMed]
- Tsirikos, A.I.; McMillan, T.E. All Pedicle Screw versus Hybrid Hook-Screw Instrumentation in the Treatment of Thoracic Adolescent Idiopathic Scoliosis (AIS): A Prospective Comparative Cohort Study. Healthcare 2022, 10, 1455. [Google Scholar] [CrossRef] [PubMed]
- Inceoglu, S.; Ferrara, L.; McLain, R. Pedicle screw fixation strength: Pullout versus insertional torque. Spine J. 2004, 4, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Matsukawa, K.; Yato, Y.; Imabayashi, H. Impact of screw diameter and length on pedicle screw fixation strength in osteoporotic vertebrae: A finite element analysis. Asian Spine J. 2021, 15, 566–574. [Google Scholar] [CrossRef]
- Gonzalvo, A.; Fitt, G.; Liew, S.; de la Harpe, D.; Vrodos, N.; McDonald, M.; Rogers, M.; Wilde, P. Correlation between pedicle size and the rate of pedicle screw misplacement in the treatment of thoracic fractures: Can we predict how difficult the task will be? Br. J. Neurosurg. 2015, 29, 508–512. [Google Scholar] [CrossRef]
- Cho, S.; Skovrlj, B.; Ly, U.; Caridi, J.; Lenke, L. The effect of increasing pedicle screw size on thoracic spinal canal dimensions: An anatomic study. Spine 2014, 39, e1195–e1200. [Google Scholar] [CrossRef]
- Ledonio, C.; Polly, D.; Vitale, M.; Wang, Q.; Richards, B.S. Pediatric pedicle screws: Comparative effectiveness and safety: A systematic literature review from the Scoliosis Research Society and the Pediatric Orthopaedic Society of North America task force. J. Bone Joint Surg. Am. 2011, 93, 1227–1234. [Google Scholar] [CrossRef]
- Brantley, A.G.; Mayfield, J.K.; Koeneman, J.B.; Clark, K.R. The effects of pedicle screw fit: An in vitro study. Spine 1994, 19, 1752–1758. [Google Scholar] [CrossRef] [PubMed]
- Holewijn, R.; Schlosser, T.; Bisschop, A.; Van der Veen, A.; Stadhouder, A.; Van Royen, B.; Castelein, R.; Kleuver, M. How Does Spinal Release and Ponte Osteotomy Improve Spinal Flexibility? The Law of Diminishing Returns. Spine Deform. 2015, 2, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Kothe, R.; O’Holleran, J.; Liu, W.; Panjabi, M. Internal architecture of the thoracic pedicle: An Ananatomic study. Spine 1996, 21, 264–270. [Google Scholar] [CrossRef]
- Sudo, H.; Abe, Y.; Kokabu, T.; Ito, M.; Abumi, K.; Ito, Y.M.; Iwasaki, N. Correlation analysis between change in thoracic kyphosis and multilevel facetectomy and screw density in main thoracic adolescent idiopathic scoliosis surgery. Spine J. 2016, 16, 1049–1054. [Google Scholar] [CrossRef]
- Ashman, R.B.; Birch, J.G.; Bone, L.B.; Corin, J.D.M.; Herring, J.A.; Johnston, C.E.I.; Ritterbush, J.F.; Roach, J.W. Mechanical testing of spinal instrumentation. Clin. Orthop. Relat. Res. 1988, 227, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Wang, Y.; Zhao, Z.; Zhang, Y. The safe placement of upper and middle thoracic pedicle screws in pediatric deformity. J. Spinal Disord. Tech. 2011, 24, 55–59. [Google Scholar] [CrossRef]
- Grabala, P.; Helenius, I.J.; Kowalski, P.; Grabala, M.; Zacha, S.; Deszczynski, J.M.; Albrewczynski, T.; Galgano, M.A.; Buchowski, J.M.; Chamberlin, K.; et al. The Child’s Age and the Size of the Curvature Do Not Affect the Accuracy of Screw Placement with the Free-Hand Technique in Spinal Deformities in Children and Adolescents. J. Clin. Med. 2023, 12, 3954. [Google Scholar] [CrossRef]
- Samdani, A.; Ranade, A.; Sciubba, D.; Cahill, P.J.; Antonacci, M.D.; Clements, D.H.; Betz, R.R. Accuracy of free-hand placement of thoracic pedicle screws in adolescent idiopathic scoliosis: How much of a difference does surgeon experience make? Eur. Spine J. 2010, 19, 91–95. [Google Scholar] [CrossRef]
- Sarwahi, V.; Wendolowski, S.; Gecelter, R.; Amaral, T.; Lo, Y.; Wollowick, A.; Thornhill, B. Are we underestimating the significance of pedicle screw misplacement? Spine 2016, 41, e548–e555. [Google Scholar] [CrossRef] [PubMed]
- Sarwahi, V.; Ayan, S.; Amaral, T.; Wendolowski, S.; Gecelter, R.; Lo, Y.; Thornhill, B. Can postoperative radiographs accurately identify screw misplacements? Spine Deform. 2017, 5, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Hicks, J.; Singla, A.; Arlet, V. Complications of pedicle screw fixation in scoliosis surgery: A systematic review. Spine 2010, 35, e465–e470. [Google Scholar] [CrossRef] [PubMed]
- Belmont, P.; Klemme, W.; Robinson, M.; Polly, D. Accuracy of thoracic pedicle screws in patients with and without coronal plane spinal deformities. Spine 2002, 27, 1558–1566. [Google Scholar] [CrossRef]
- Yazici, M.; Pekmezci, M.; Cil, A.; Alanay, A.; Acaroglu, E.; Oner, F.C. The effect of pedicle expansion on pedicle morphology and biomechanical stability in the immature porcine spine. Spine 2006, 31, E826–E829. [Google Scholar] [CrossRef]
- Rinella, A.S.; Cahill, P.; Ghanayem, A. Thoracic pedicle expansion after pedicle screw placement in a pediatric cadaveric spine. In Proceedings of the Podium Presentation: Scoliosis Research Society (SRS) 2004 Annual Meeting, Buenos Aires, Argentina, 6 September 2004. [Google Scholar]



| G1 (n = 132) | G2 (n = 128) | p | |
|---|---|---|---|
| Age | 14.8 (6.1) | 14.8 (5.2) | 0.856 |
| Height | 161 (8) | 162 (9) | 0.921 |
| Mean follow-up | 44 (8) | 42 (9) | 0.032 |
| Weight | 57 (14) | 59 (13) | 0.918 |
| Sex (n) | |||
| M | 13 | 15 | |
| F | 119 | 113 | |
| BMI | 21 (5) | 21 (4) | 0.992 |
| Risser grade | 3.6 (1.8) | 3.2 (1.2) | 0.979 |
| Time of surgery | 252 (62.4) | 344 (82.8) | 0.443 |
| Blood loss | 480 (288) | 632 (278) | 0.295 |
| Lenke type * | |||
| I | 67 | 68 | N.S. |
| II | 27 | 25 | N.S. |
| III | 5 | 4 | N.S. |
| IV | 6 | 5 | N.S. |
| V | 16 | 14 | N.S. |
| VI | 11 | 12 | N.S. |
| Fusion levels | 10.2 (2.8) | 9.8 (3.2) | 0.781 |
| Screw density% | 75 (12) | 75 (10) | 0.482 |
| Implant complications | 3 | 4 | 0.783 |
| Variable | G1 (n = 132) | G2 (n = 128) | p |
|---|---|---|---|
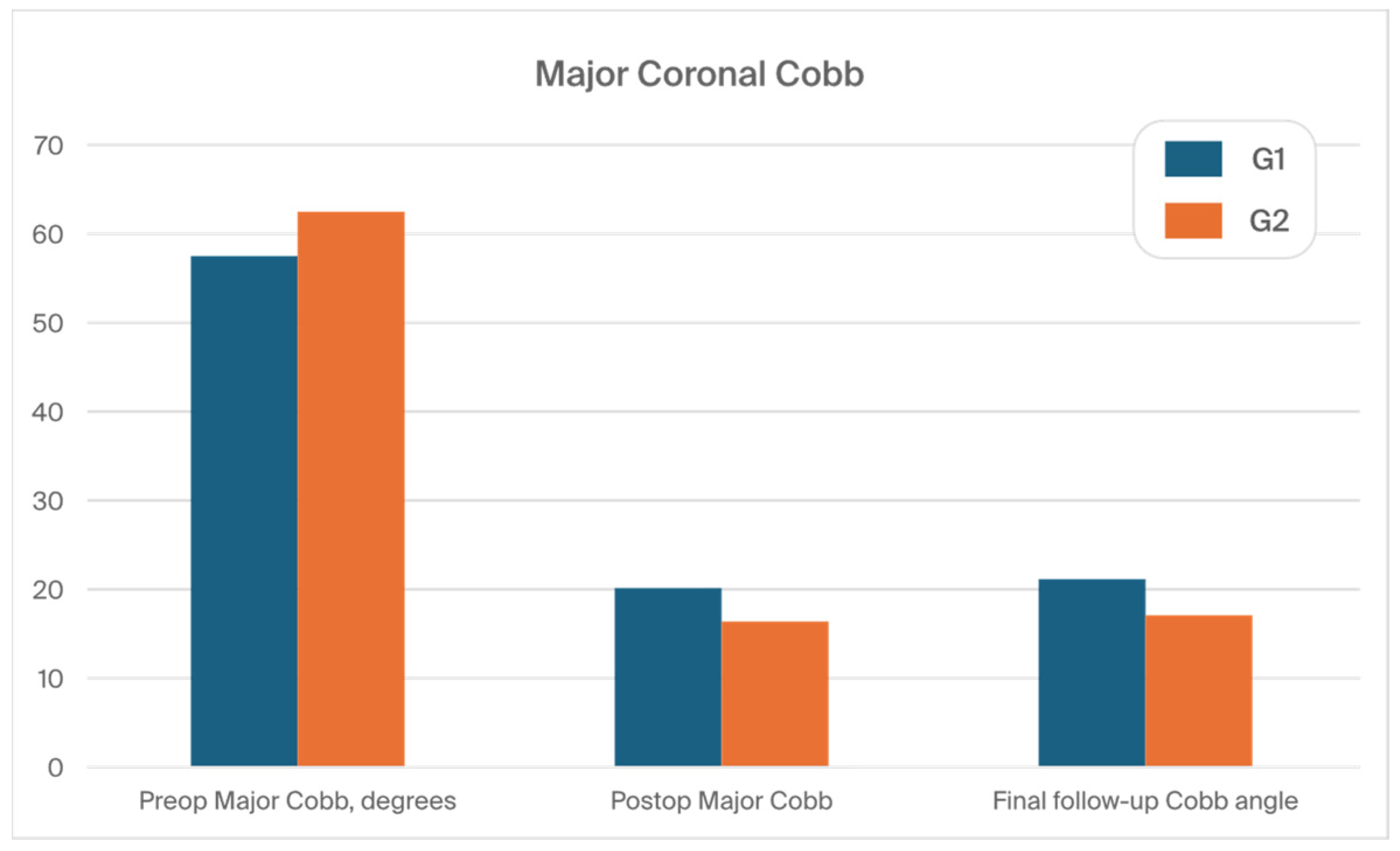
| Preop major Cobb, degrees | 57.6 (11.9) | 62.5 (12.1) | 0.949 |
| Postop major Cobb | 19.8 (10.2) | 16.6 (8.2) | 0.001 |
| Final follow-up Cobb angle | 21.3 (9.2) | 17.1 (7.2) | 0.001 |
| % Cobb correction, postoperative | 69.8 (12.8) | 74.5 (11.2) | 0.001 |
| % Correction (FFU) | 61% (15) | 68% (14) | 0.001 |
| Flexibility rate | 35% (11) | 33% (8) | 0.382 |
| Ponte osteotomy levels (n) | 5.8 (2.2) | 5.6 (2.5) | 0.978 |
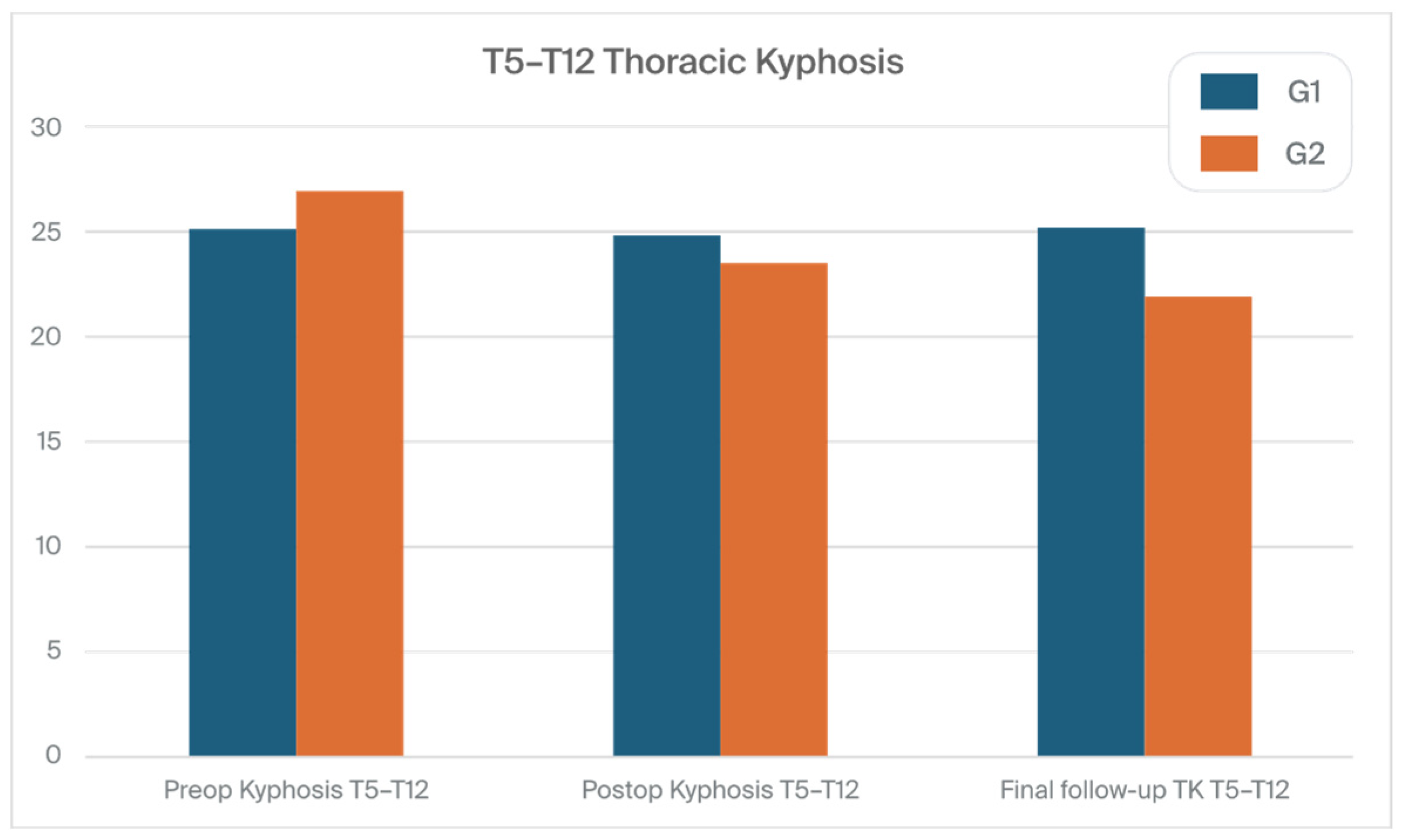
| Preop kyphosis T5–T12 | 25.1 (15.5) | 26.9 (15.8) | 0.779 |
| Postop kyphosis T5–T12 | 24.8 (8.8) | 23.5 (10.8) | 0.012 |
| Final follow-up TK T5–T12 | 25.2 (9.8) | 21.9 (10.2) | 0.001 |
| Preop kyphosis T2–T5 | 12.2 (8.8) | 10 (8.9) | 0.289 |
| Postop kyphosis T2–T5 | 15.2 (9.8) | 13 (5.9) | 0.028 |
| Postop kyphosis T2-T5 (FFU) | 16.7 (9.2) | 9.6 (6.8) | 0.001 |
| Preop kyphosis T2–T12 | 31.2 (14.8) | 33.5 (13.6) | 0.676 |
| Postop kyphosis T2–T12 | 33.1 (11.8) | 31.4 (12.6) | 0.539 |
| Postop kyphosis T2–T12 (FFU) | 34.3 (10.7) | 35 (9.8) | 0.195 |
| Preop lumbar lordosis | 50.8 (10.2) | 50.2 (9.6) | 0.487 |
| Postop lumbar lordosis | 44.2 (12.4) | 46.4 (11.8) | 0.946 |
| Final follow-up lumbar lordosis | 50.2 (11.8) | 49.5 (12.3) | 0.126 |
| Preoperative apical vertebral translation, mm | 67 (15.5) | 69 (13.8) | 0.282 |
| Postoperative apical vertebral translation, mm | 21 (6.2) | 20.8 (5.2) | 0.081 |
| Apical vertebral translation at final follow-up, mm | 24 (5.8) | 22 (4.8) | 0.001 |
| Preop sagittal balance, mm | 37.4 (27.8) | 39.9 (28.9) | 0.215 |
| Postop sagittal balance, mm | 39.8 (28.9) | 26.8 (23.1) | 0.112 |
| Final follow-up sagittal balance, mm | 36.6 (22.6) | 27.6 (21.4) | 0.001 |
| Preoperative coronal balance, mm | 18.5 (11.4) | 19.2 (11.8) | 0.212 |
| Postoperative coronal balance, mm | 8.8 (5.6) | 8.1 (6.9) | 0.731 |
| FFU coronal balance, mm | 9.8 (6.2) | 10.6 (7.4) | 0.493 |
| Loss of correction, degree | 5.9 (3.6) | 3.2 (3.2) | 0.001 |
| SRS-22R | G1 (n = 132) | G2 (n = 128) | |||||
|---|---|---|---|---|---|---|---|
| Parameter | Preoperative | Final Follow-Up | p-Values * | Preoperative | Final Follow-Up | p-Values | p-Values SG vs. LG at FFU |
| Function | 4.32 (0.62) | 4.62 (0.40) | 0.203 | 4.12 (0.68) | 4.52 (0.52) | 0.309 | 0.632 |
| Pain | 4.02 (0.65) | 4.28 (0.62) | 0.178 | 3.98 (0.62) | 4.38 (0.68) | 0.058 | 0.872 |
| Self-image | 3.76 (0.62) | 4.46 (0.42) | <0.001 | 3.88 (0.58) | 4.62 (0.38) | <0.001 | 0.061 |
| Mental health | 4.12 (0.62) | 4.32 (0.60) | 0.125 | 4.02 (0.82) | 4.22 (0.76) | 0.171 | 0.591 |
| Satisfaction | 3.80 (0.76) | 4.22 (0.70) | <0.001 | 3.80 (0.66) | 4.26 (0.74) | <0.001 | 0.942 |
| Total score | 3.86 (0.92) | 4.36 (0.62) | <0.001 | 3.82 (0.82) | 4.26 (0.78) | <0.001 | 0.839 |
| Complication Rates Following Posterior Final Fusion | G1 (n = 132) | G2 (n = 128) | p |
|---|---|---|---|
| Intraoperative neuromonitoring changes | 5 (3.8%) | 7 (5.5%) | <0.001 |
| Superficial wound infection | 2 (1.5%) | 2 (1.5%) | NS |
| Pneumonia | 2 (1.5%) | 2 (1.5%) | NS |
| Paresthesia from the lateral cutaneous nerve of the lower limb | 5 (3.8%) | 6 (4.7%) | NS |
| Radiculopathy | 2 (1.5%) | 3 (1.5%) | NS |
| Deep infection | 2 (1.5%) | 2 (1.5%) | NS |
| Screw misplacement (replacement) | 3 (2.3%) | 4 (2.3%) | NS |
| Pneumothorax | 2 (1.5%) | 2 (1.5%) | NS |
| Cerebrospinal fluid leakage | 3 (2.3%) | 2 (1.5%) | NS |
| Total | 26 (19.7%) | 30 (23.5%) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grabala, P.; Kowalski, P.; Grabala, M. The Influence of Increased Pedicle Screw Diameter and Thicker Rods on Surgical Results in Adolescents Undergoing Posterior Spinal Fusion for Idiopathic Scoliosis. J. Clin. Med. 2024, 13, 2174. https://doi.org/10.3390/jcm13082174
Grabala P, Kowalski P, Grabala M. The Influence of Increased Pedicle Screw Diameter and Thicker Rods on Surgical Results in Adolescents Undergoing Posterior Spinal Fusion for Idiopathic Scoliosis. Journal of Clinical Medicine. 2024; 13(8):2174. https://doi.org/10.3390/jcm13082174
Chicago/Turabian StyleGrabala, Pawel, Piotr Kowalski, and Michal Grabala. 2024. "The Influence of Increased Pedicle Screw Diameter and Thicker Rods on Surgical Results in Adolescents Undergoing Posterior Spinal Fusion for Idiopathic Scoliosis" Journal of Clinical Medicine 13, no. 8: 2174. https://doi.org/10.3390/jcm13082174







