Objective Rotational Analysis of EVO Toric ICLs Using Infrared Retinal Retroillumination Imaging
Abstract
1. Introduction
2. Materials and Methods
2.1. Preoperative and Postoperative Assessments
- Visual acuity with and without optical correction.
- Subjective refraction under physiological conditions and cycloplegia.
- Corneal topography using Scheimpflug imaging, determining the simulated keratometric power of the anterior surface (SimK) with a corneal tomographer (Pentacam Oculus, Inc., Arlington, WA, USA).
- Biometry (IOL Master 700, Carl Zeiss Meditech, Jena, Germany).
- Anterior segment optical coherence tomography (AS-OCT) (Casia 2, Tomey Corp., Nagoya, Japan).
- Follow-up Assessments
- Visual acuity with and without optical correction.
- Subjective refraction under physiological conditions.
- Anterior segment OCT during follow-up (AS-OCT).
- Infrared retroillumination iris imaging with Pentacam AXL Wave during follow-up visits at 1 and 3 months.
2.2. Lens Calculation and Implantation
2.3. Surgical Procedure
2.4. Lens Orientation Analysis
2.5. Inclusion and Exclusion Criteria
- Subjects undergoing refractive surgery with toric EVO ICL phakic lens implantation.
- Preoperative refraction up to −18.00 D of myopia.
- Preoperative corrected distance visual acuity (CDVA) of 1.0 decimal or better.
- Signed informed consent for surgery and data use for future analysis.
- Unstable refraction in the last 12 months.
- Previous corneal relaxing or perforating incisions.
- Previous ocular surgery.
- Corneal topography showing anterior or posterior curvature abnormalities.
- Ocular or systemic diseases that could affect healing (e.g., connective tissue diseases, diabetes mellitus).
2.6. Study Design and Sample Size
2.7. Variables
- Pre- and postoperative visual acuity with and without dioptric correction.
- Pre- and postoperative refraction.
- Pre- and postoperative simulated keratometry (SimK).
- Preoperatively calculated and final lens orientation obtained by infrared retroillumination image, and the difference in degrees.
- Effect of lens misalignment on refractive error and uncorrected visual acuity.
- Rotational stability of the implanted lens at 3 months post-surgery.
2.8. Statistical Analysis
3. Results
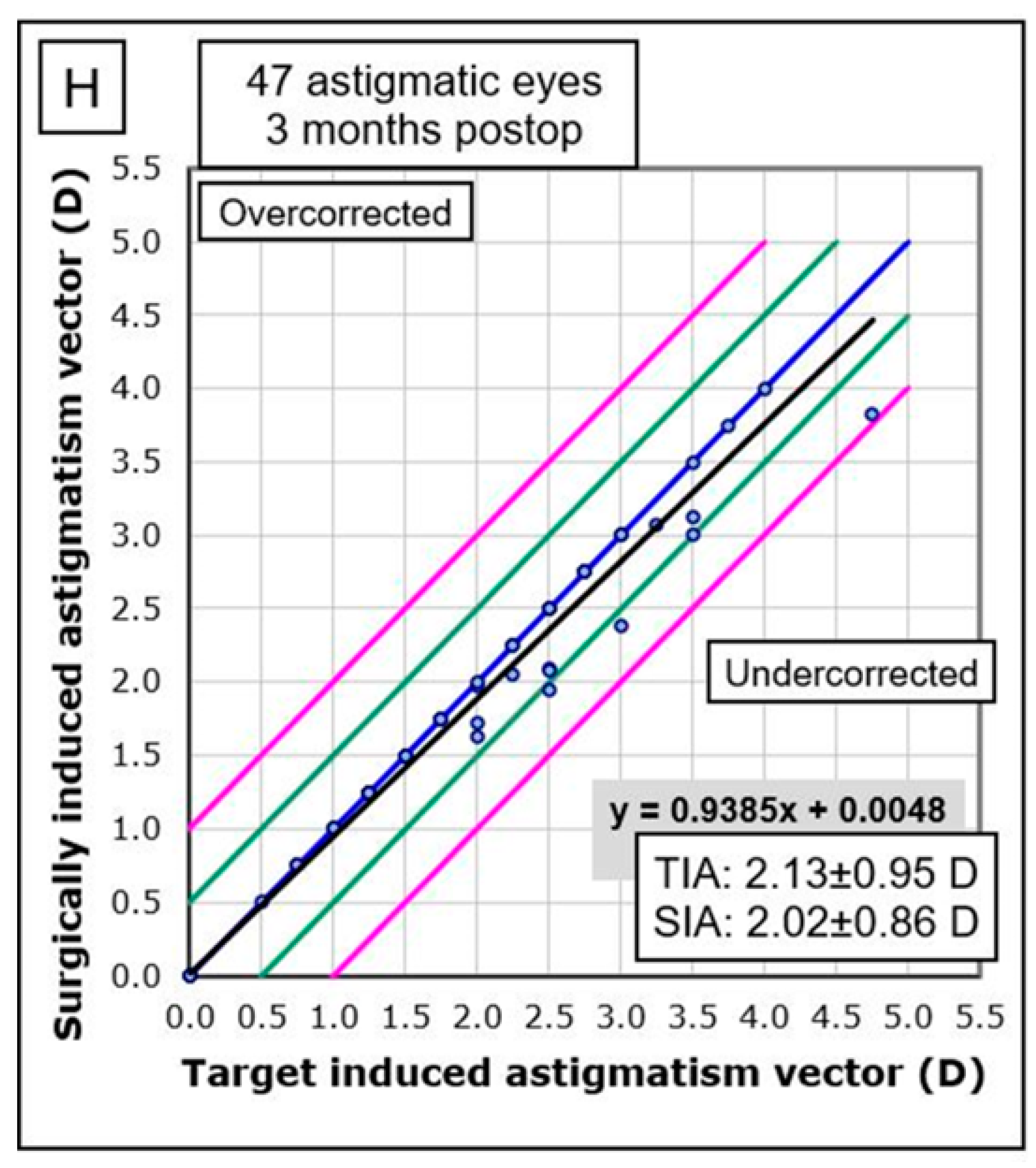
3.1. Surgically Induced Astigmatism (SIA)
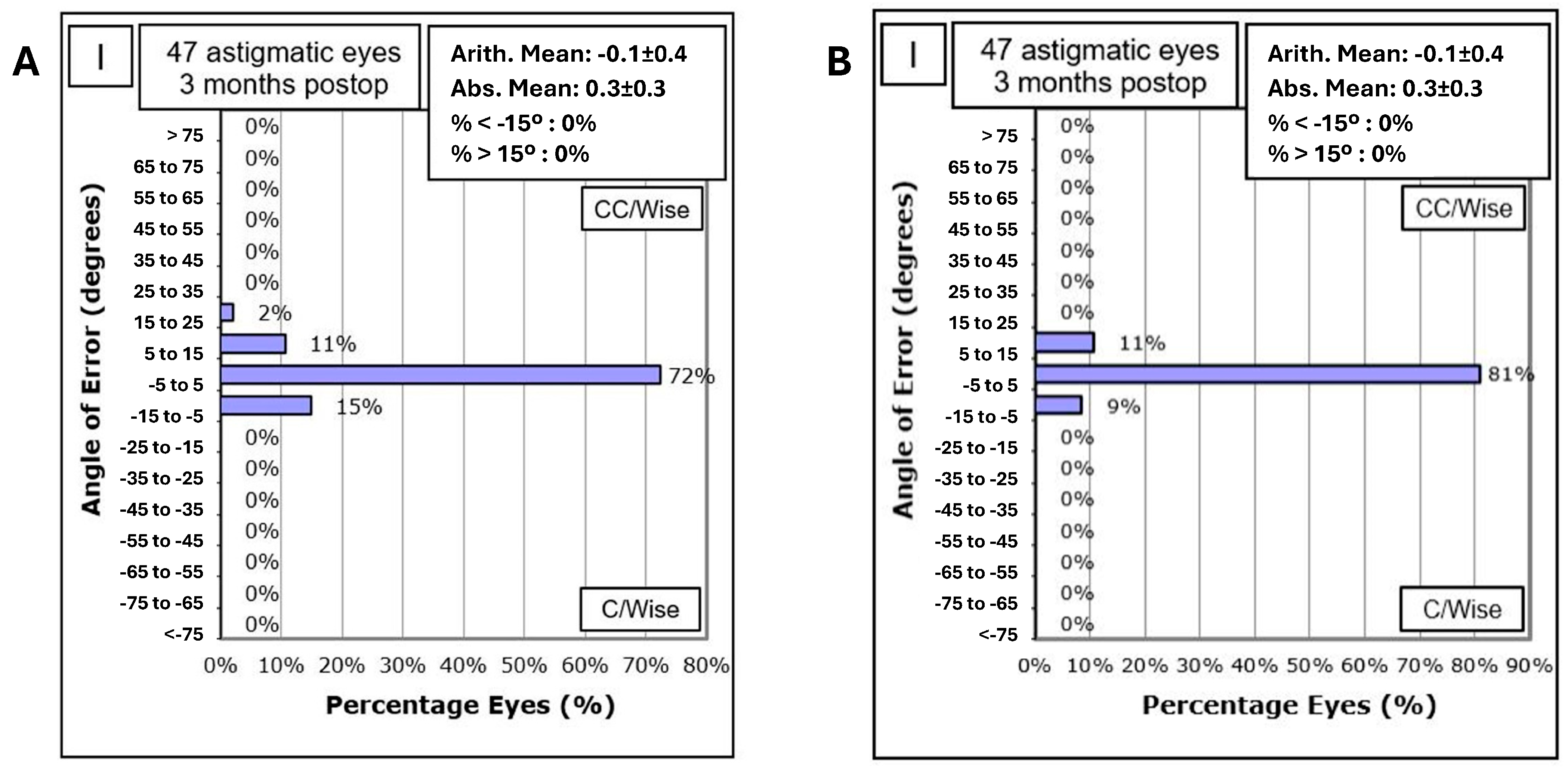
3.2. Rotational Stability
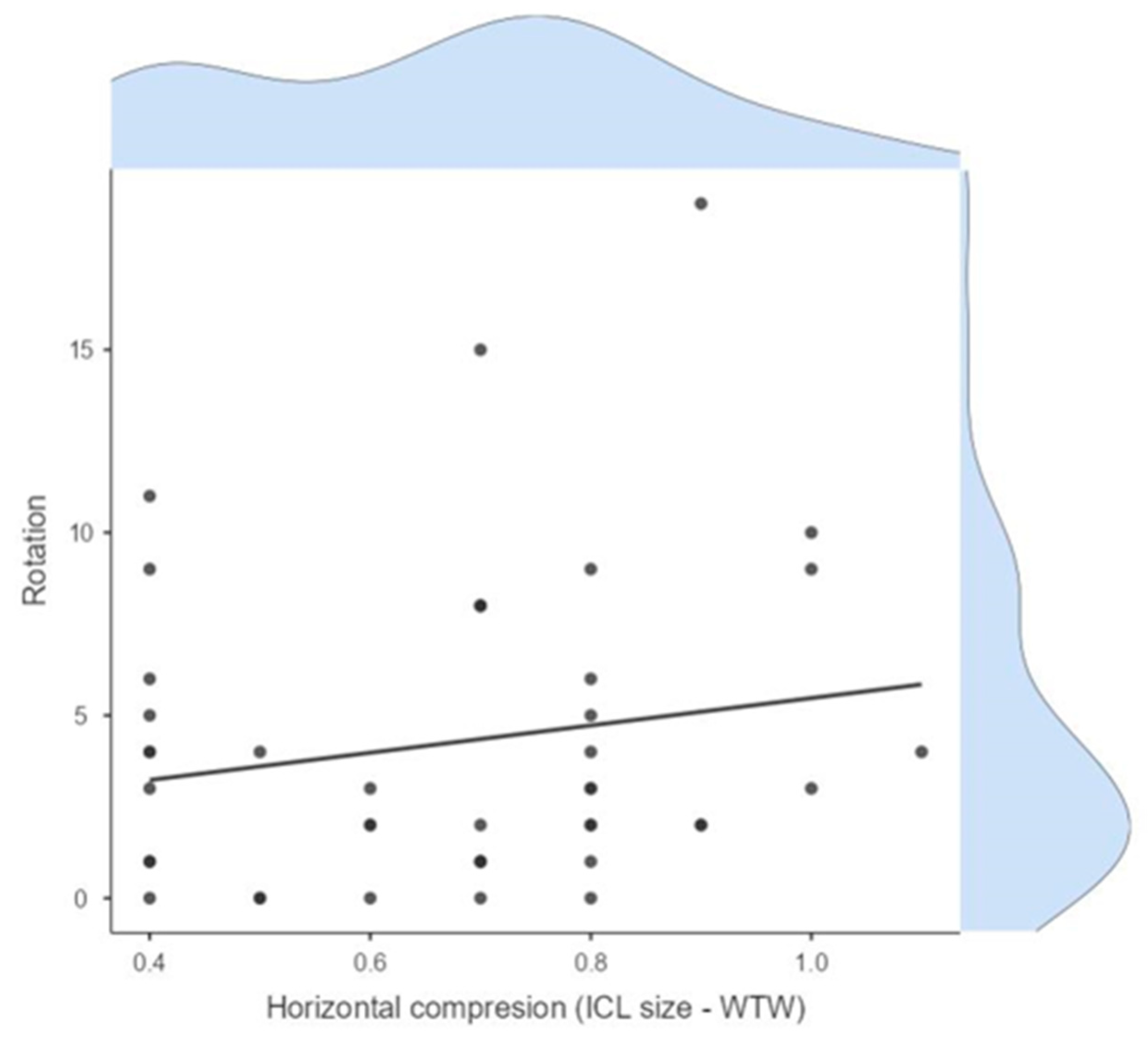
3.3. Correlation with Vault Size and Horizontal Compression
3.4. Correction Accuracy
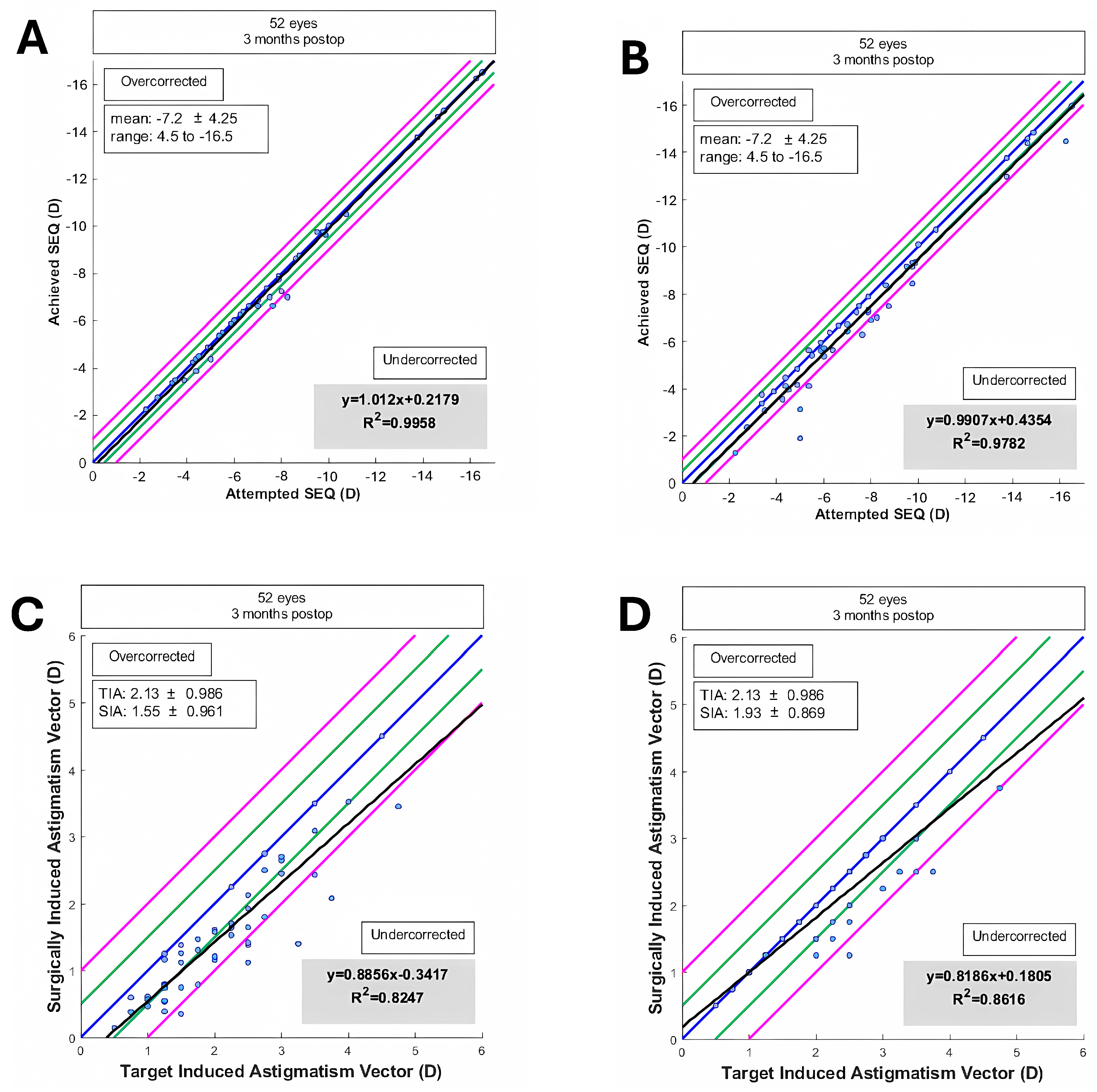
3.5. Predictability in SEQ and Cylinder
3.6. Summary of Findings
- The corneal SIA generated by the surgeon in EVO ICL toric implantation was low, with a mean of 0.32 D and a vector SIA of 0.12 D at 100°.
- The mean refractive SIA of 2.02 D was similar to the mean preoperative refractive astigmatism of 2.07 D, resulting in a correction index (CI) of 0.96.
- High rotational stability was observed at 1-month post-surgery, with 72% of eyes showing less than 5° rotation and 96% less than 10° rotation.
- A trend of lower UDVA was observed depending on the ICL rotation and the astigmatic power through the parallel coordinates graph.
- Rotational stability of the toric EVO ICL could not be associated with the size of the postoperative vault (Pearson correlation coefficient = 0.10, p = 0.50) nor with the horizontal compression of the lens (WTW-ICL size) (Pearson correlation coefficient = 0.17, p = 0.25) (Table 1).
- Good concordance was found between the estimated rotation of the toric EVO ICL by vector calculation and that observed by retroillumination. However, the calculated method underestimated the rotation of the pIOL, and it was dependent on cylinder power and exact postoperative refraction, while the observed method by retroillumination was independent of these variables.
- The difference between the TIA and refractive SIA vectors was practically zero, indicating good correction of refractive cylinder.
- High predictability in SEQ and cylinder was achieved, with 69% of eyes within ±0.50 D and 88% within ±1.00 D for subjective refraction, and 96% within ±0.50 D and 98% within ±1.00 D for objective aberrometry measurements.
4. Discussion
- The sample size was relatively small, particularly for eyes with ATR and oblique astigmatism. Larger sample sizes are needed to confirm the findings.
- The follow-up period was limited to three months. Longer follow-up studies are necessary to evaluate the long-term stability and safety of the procedure.
- This study was conducted at a single center, which may limit the generalizability of the results.
5. Conclusions
- High rotational stability, with 72% of lenses showing less than 5° rotation and 96% less than 10° at one month postoperatively.
- Excellent refractive predictability, with 96% of eyes within ±1.00 D and 84% within ±0.50 D of the intended correction.
- A low prevalence of secondary surgical interventions, with only 0.21% of eyes requiring repositioning and 0.09% requiring lens exchange due to sizing errors.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Packer, M. The implantable collamer lens with a central port: Review of the literature. Clin. Ophthalmol. 2018, 12, 2427–2438. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Vega-Cueto, L.; Alfonso-Bartolozzi, B.; Lisa, C.; Madrid-Costa, D.; Alfonso, J.F. Seven-year follow-up of posterior chamber phakic intraocular lens with central port design. Eye Vis. 2021, 8, 23. [Google Scholar] [CrossRef] [PubMed]
- Alfonso-Bartolozzi, B.; Fernández-Vega-Cueto, L.; Lisa, C.; Palacios, A.; Madrid-Costa, D.; Alfonso, J.F. Ten-year follow-up of posterior chamber phakic intraocular lens with central port design in patients with low and normal vault. J. Cataract Refract. Surg. 2024, 50, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Plaza, E.; López-de la Rosa, A.; López-Miguel, A.; Holgueras, A.; Maldonado, M.J. EVO/EVO+ Visian Implantable Collamer Lenses for the correction of myopia and myopia with astigmatism. Expert Rev. Med. Devices 2023, 20, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Cano-Ortiz, A.; Sánchez-Ventosa, Á.; Membrillo, A.; Castillo, R.; Gomera, A.; López-Pérez, M.D.; Villarrubia, A. Astigmatism correction with toric implantable collamer lens in low and high astigmatism groups. Eur. J. Ophthalmol. 2022, 32, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Wei, P.; Li, J.; Jiao, X.; Yu, Z.; Song, H. Short-term clinic observation of misalignment and rotational stability after implantable collamer lens implantation. Graefes Arch. Clin. Exp. Ophthalmol. 2022, 261, 1473–1481. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Zhao, J.; Yang, W.; Sun, L.; Qian, Y.; Wang, X.; Zhou, X. Influence of Ocular Residual Astigmatism and Target-Induced Astigmatism on the Efficacy of the Implantation of a Toric Implantable Collamer Lens With Central Hole for Myopic Astigmatism Correction. Front. Med. 2022, 8, 737358. [Google Scholar] [CrossRef] [PubMed]
- Savini, G.; Alessio, G.; Perone, G.; Rossi, S.; Schiano-Lomoriello, D. Rotational stability and refractive outcomes of a single-piece aspheric toric intraocular lens with 4 fenestrated haptics. J. Cataract Refract. Surg. 2019, 45, 1275–1279. [Google Scholar] [CrossRef] [PubMed]
- Balparda, K.; Silva-Quintero, L.A.; Herrera-Chalarca, T. Unilateral toxic anterior segment syndrome after immediate sequential bilateral phakic intraocular lens implantation. J. Cataract Refract. Surg. Online Case Rep. 2022, 10, e00072. [Google Scholar] [CrossRef]
- Carreras-Díaz, H.; Carreras-Díaz, M.D.R.; University Hospital of Girona Doctor Josep Trueta, Gerona 17007, Spain; Lorente-Velázquez, A.; Departament of Optometry and Vision, Faculty of Optics and Optometry, Complutense University of Madrid, Madrid 28040, Spain. Refractive outcomes after V4c Toric collamer lens implantation over 1y of follow-up. Int. J. Ophthalmol. 2024, 17, 1322–1330. [Google Scholar] [CrossRef] [PubMed]
- Hyun, J.; Lim, D.H.; Eo, D.R.; Hwang, S.; Chung, E.S.; Chung, T.Y. A comparison of visual outcome and rotational stability of two types of toric implantable collamer lenses (TICL): V4 versus V4c. PLoS ONE 2017, 12, e0183335. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kang, D.S.Y.; Choi, J.Y.; Ha, B.J.; Kim, E.K.; Seo, K.Y.; Kim, T.I. Rotational stability and visual outcomes of V4c toric phakic intraocular lenses. J. Refract. Surg. 2018, 34, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, K.; Shimizu, K.; Igarashi, A.; Komatsu, M. Comparison of Collamer toric contact lens implantation and wavefront-guided laser in situ keratomileusis for high myopic astigmatism. J. Cataract Refract. Surg. 2008, 34, 1687–1693. [Google Scholar] [CrossRef] [PubMed]
- Shiga, S.; Kojima, T.; Horai, R.; Nakamura, T. Evaluation of long-term clinical outcomes after toric implantable collamer lens implantation. J. Cataract Refract. Surg. 2023, 49, 964–969. [Google Scholar] [CrossRef] [PubMed]
- Wei, R.; Li, M.; Aruma, A.; Knorz, M.C.; Yang, D.; Yu, Y.; Wang, X.; Choi, J.; Yao, P.; Zhou, X. Factors leading to realignment or exchange after implantable collamer lens implantation in 10 258 eyes. J. Cataract Refract. Surg. 2022, 48, 1190–1196. [Google Scholar] [CrossRef] [PubMed]

| Variable | Value/Statistics |
|---|---|
| Mean Corneal SIA | 0.32 D |
| Refractive SIA | 2.02 D |
| Preoperative Refractive Astigmatism | 2.07 D |
| Correction Index (CI) | 0.96 |
| Rotational Stability (<5°) | 72% |
| Rotational Stability (<10°) | 96% |
| Correlation with Vault Size | Pearson r = 0.10, p = 0.50 |
| Correlation with Horizontal Compression | Pearson r = 0.17, p = 0.25 |
| Predictability in SEQ (Subjective) | R2 = 0.9782 |
| Predictability in SEQ (Objective) | R2 = 0.9958 |
| SEQ Distribution within ±0.50 D (Subjective) | 69% |
| SEQ Distribution within ±1.00 D (Subjective) | 88% |
| SEQ Distribution within ±0.50 D (Objective) | 96% |
| SEQ Distribution within ±1.00 D (Objective) | 98% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cano-Ortiz, A.; Sánchez-Ventosa, Á.; González-Cruces, T.; Villalva-González, M.; Prados-Carmona, J.J.; Castillo-Eslava, R.; Sánchez-Tena, M.Á.; Alvarez-Peregrina, C.; Villarrubia-Cuadrado, A. Objective Rotational Analysis of EVO Toric ICLs Using Infrared Retinal Retroillumination Imaging. J. Clin. Med. 2025, 14, 2895. https://doi.org/10.3390/jcm14092895
Cano-Ortiz A, Sánchez-Ventosa Á, González-Cruces T, Villalva-González M, Prados-Carmona JJ, Castillo-Eslava R, Sánchez-Tena MÁ, Alvarez-Peregrina C, Villarrubia-Cuadrado A. Objective Rotational Analysis of EVO Toric ICLs Using Infrared Retinal Retroillumination Imaging. Journal of Clinical Medicine. 2025; 14(9):2895. https://doi.org/10.3390/jcm14092895
Chicago/Turabian StyleCano-Ortiz, Antonio, Álvaro Sánchez-Ventosa, Timoteo González-Cruces, Marta Villalva-González, Juan José Prados-Carmona, Rosa Castillo-Eslava, Miguel Ángel Sánchez-Tena, Cristina Alvarez-Peregrina, and Alberto Villarrubia-Cuadrado. 2025. "Objective Rotational Analysis of EVO Toric ICLs Using Infrared Retinal Retroillumination Imaging" Journal of Clinical Medicine 14, no. 9: 2895. https://doi.org/10.3390/jcm14092895
APA StyleCano-Ortiz, A., Sánchez-Ventosa, Á., González-Cruces, T., Villalva-González, M., Prados-Carmona, J. J., Castillo-Eslava, R., Sánchez-Tena, M. Á., Alvarez-Peregrina, C., & Villarrubia-Cuadrado, A. (2025). Objective Rotational Analysis of EVO Toric ICLs Using Infrared Retinal Retroillumination Imaging. Journal of Clinical Medicine, 14(9), 2895. https://doi.org/10.3390/jcm14092895








