Pilates Method Improves Cardiorespiratory Fitness: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Study Selection
2.2. Eligibility Criteria
Ethical Aspects
2.3. Data Extraction and Quality Assessment
2.4. Data Analysis
3. Results
3.1. Systematic Review
3.1.1. Study Selection
3.1.2. Study and Intervention Characteristics
3.1.3. Quality Assessment and Risk of Bias
3.2. Data Synthesis
3.2.1. Meta-Analysis
3.2.2. Sensitivity and Meta-Regression Analyses
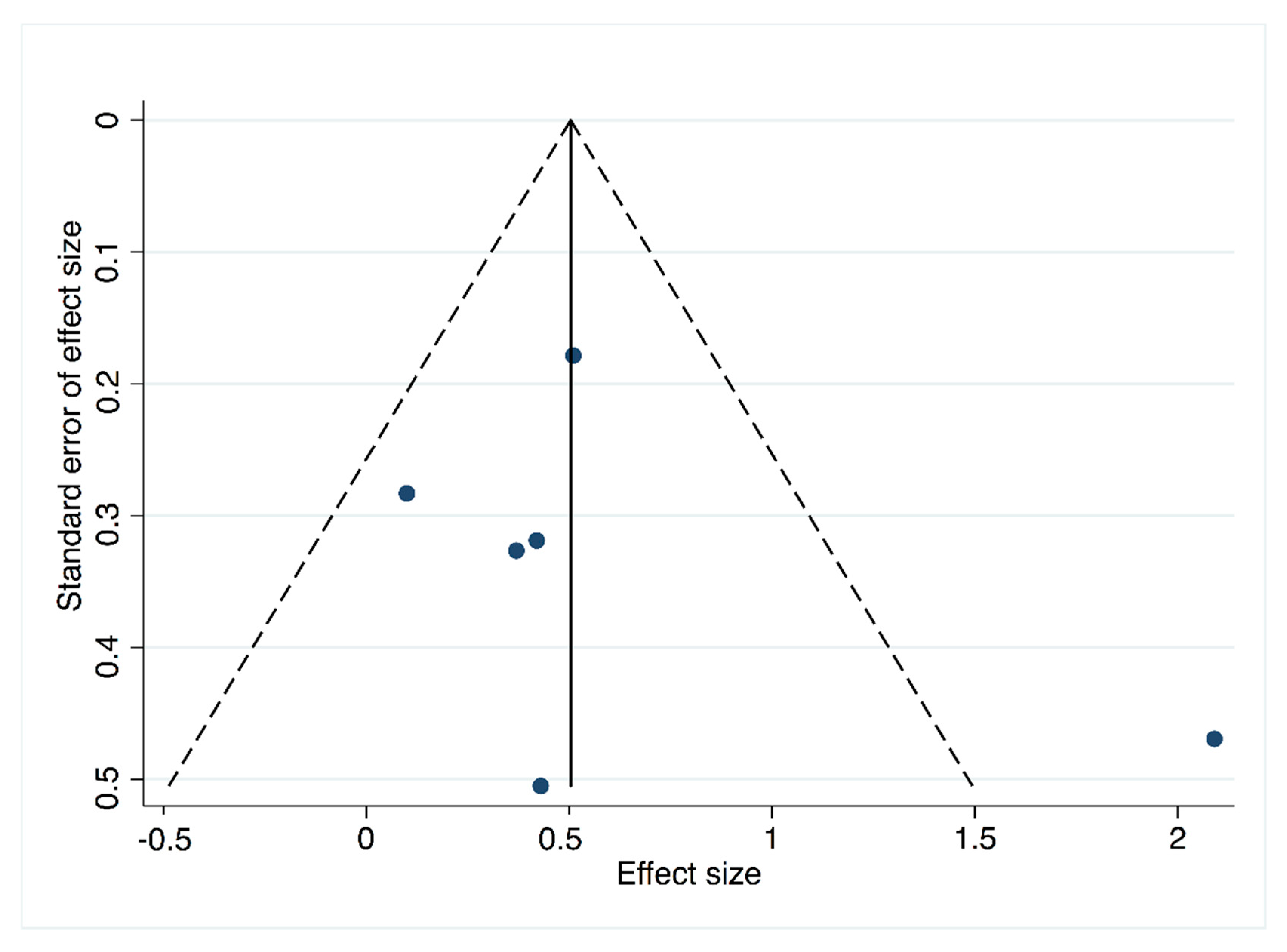
3.2.3. Publication Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A

| Pilates Method Intervention | ||||
|---|---|---|---|---|
| Author, Year | ES | LL | UL | I2 |
| Guimarães et al., 2012 [35] | 0.52 | 0.25 | 0.79 | 71.1 |
| Gildenhuys et al., 2013 [22] | 0.57 | 0.29 | 0.84 | 69.1 |
| Diamantoula et al., 2016 [46] | 0.53 | 0.25 | 0.80 | 71.1 |
| Lim HS et al., 2016 [29] | 0.53 | 0.24 | 0.83 | 71 |
| Rodrigues et al., 2016 [32] | 0.43 | 0.20 | 0.65 | 60.1 |
| Tinoco-Fernández et al., 2016 [30] | 0.56 | 0.24 | 0.89 | 71.1 |
| Mikalacki et al., 2017 [31] | 0.57 | 0.26 | 0.89 | 70.5 |
| Finatto et al., 2018 [33] | 0.39 | 0.24 | 0.54 | 19.6 |
| Rossell-Rayes et al., 2019 [45] | 0.55 | 0.27 | 0.83 | 70.6 |
| Pilates Method Intervention | ||||
|---|---|---|---|---|
| ES | LL | UL | I2 | |
| Healthy | 0.64 | 0.26 | 1.02 | 78.9 |
| Unhealthy | 0.39 | 0.14 | 0.64 | 0 |
| Coefficient | p-Value | |
|---|---|---|
| Pilates Method intervention | 0.05 | 0.05 * |
| Coefficient | p-Value | |
|---|---|---|
| Pilates Method intervention | 2.19 | 0.07 * |

Appendix B. Mean Difference Analyses for Pilates vs. CG (B1–B6: Meta-Analysis, Sensitivity Analysis, Subgroup Analysis, Meta-Regression, Publication Bias and Funnel Plot)

| Pilates vs. Control Group | |||
|---|---|---|---|
| Author, Year | MD | 95% CI | I2 |
| Guimarães et al., 2012 [35] | 2.24 | 0.89, 4.58 | 46.7 |
| Gildenhuys et al., 2013 [22] | 3.88 | 2.53, 5.24 | 0.0 |
| Lim HS et al., 2016 [29] | 2.77 | 0.85, 4.69 | 46.5 |
| Mikalacki et al., 2017 [31] | 2.59 | 0.48, 4.69 | 46.2 |
| Finatto et al., 2018 [33] | 1.71 | 0.09, 3.33 | 0.0 |
| Rossell-Rayes et al., 2019 [45] | 2.25 | 0.82, 4.67 | 46.7 |
| Pilates vs. Control Group | MD | 95% CI |
|---|---|---|
| Healthy | 2.77 | 1.12, 4.42 |
| Unhealthy | 2.67 | −0.61, 5.95 |
| Coefficient | p-Value | |
|---|---|---|
| Pilates vs. control group | 0.09 | 0.08 |
| Coefficient | p-Value | |
|---|---|---|
| Pilates vs. control group | −0.50 | 0.69 |

References
- Blair, S.N.; Kohl, H., III; Paffenbarger, R.J.; Clark, D.G.; Cooper, K.H.; Gibbons, L.W. Physical Fitness and All-Cause Mortality. Jama 1989, 262, 2395–2401. [Google Scholar] [CrossRef] [PubMed]
- Blair, J.B.; Kampert, H.W.; Kohl, C.E., III; Barlow, C.A.; Macera, R.S.; Paffenbarger, L.W., Jr.; Gibbons, S.N. The Influences of cardiovascular fitness and other precursers on cardiovascular disease and all-cause mortality in men and women. Aerobics center longitudinal study. J. Am. Med. Assoc. 1996, 276, 205–210. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef] [PubMed]
- Croci, I.; Coombes, J.S.; Sandbakk, S.B. Non-alcoholic fatty liver disease: Prevalence and all-cause mortality according to sedentary behaviour and cardiorespiratory fitness. The HUNT Study. Prog. Cardiovasc. Dis. 2019, 62, 127–134. [Google Scholar] [CrossRef]
- Pozuelo-Carrascosa, D.P.; Alvarez-Bueno, C.; Cavero-Redondo, I.; Morais, S.; Lee, I.M.; Martínez-Vizcaíno, V. Cardiorespiratory fitness and site-specific risk of cancer in men: A systematic review and meta-analysis. Eur. J. Cancer 2019, 113, 58–68. [Google Scholar] [CrossRef]
- Steell, L.; Ho, F.K.; Sillars, A. Dose-response associations of cardiorespiratory fitness with all-cause mortality and incidence and mortality of cancer and cardiovascular and respiratory diseases: The UK Biobank cohort study. Br. J. Sports Med. 2019, 53, 1371–1378. [Google Scholar] [CrossRef]
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, 2011–2030. [Google Scholar] [CrossRef]
- Davidson, T.; Vainshelboim, B.; Kokkinos, P.; Myers, J.; Ross, R. Cardiorespiratory fitness versus physical activity as predictors of all-cause mortality in men. Am. Heart J. 2018, 196, 156–162. [Google Scholar] [CrossRef]
- Lavie, C.J.; Wisløff, U.; Després, J.-P. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e653–e659. [Google Scholar] [CrossRef]
- Kodama, S. Cardiorespiratory Fitness as a Quantitative Predictor of All-Cause Mortality and Cardiovascular Events. J. Am. Med. Assoc. 2009, 301, 2024–2035. [Google Scholar] [CrossRef]
- Lee, C.D.; Blair, S.N.; Jackson, A.S. Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men. Am. J. Clin. Nutr. 1999, 69, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Harber, M.P.; Kaminsky, L.A.; Arena, R. Impact of Cardiorespiratory Fitness on All-Cause and Disease-Specific Mortality: Advances Since 2009. Prog. Cardiovasc. Dis. 2017, 60, 11–20. [Google Scholar] [CrossRef] [PubMed]
- American College of Sports Medicine. American College of Sports Medicine Position Stand. Med. Sci. Sport Exerc. 1998, 30, 975–991. [Google Scholar] [CrossRef]
- Pescatello, L.; Arena, R.; Riebe, D.; Thompson, P. ACSM’s Guidelines for Exercsie Testing and Prescription, 9th ed.; Wolters Kluwer Health: Philadelphia, PA, USA, 2014; pp. 269–299. [Google Scholar]
- Swain, D.P.; Franklin, B.A. VO(2) reserve and the minimal intensity for improving cardiorespiratory fitness. Med. Sci. Sport Exerc. 2002, 34, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Eliks, M.; Zgorzalewicz-Stachowiak, M.; Zeńczak-Praga, K. Application of Pilates-based exercises in the treatment of chronic non-specific low back pain: State of the art. Postgrad. Med. J. 2019, 95, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Lau, C.; Yu, R.; Woo, J. Effects of a 12-Week hatha yoga intervention on cardiorespiratory endurance, muscular strength and endurance, and flexibility in Hong Kong Chinese Adults: A controlled clinical trial. Evid. Based Complement. Altern Med. 2015, 2015, 958727. [Google Scholar] [CrossRef] [PubMed]
- De Souza, R.O.B.; de Faria Marcon, L.; de Arruda, A.S.F.; Pontes Junior, F.L.; de Melo, R.C. Effects of Mat Pilates on Physical Functional Performance of Older Adults. Am. J. Phys. Med. Rehabil. 2018, 97, 414–425. [Google Scholar] [CrossRef]
- De Alvarenga, G.M.; Charkovski, S.A.; Dos Santos, L.K.; da Silva, M.A.B.; Tomaz, G.O.; Gamba, H.R. The influence of inspiratory muscle training combined with the Pilates method on lung function in elderly women: A randomized controlled trial. Clinics 2018, 73, e356. [Google Scholar] [CrossRef]
- Sarmento, L.A.; Pinto, J.S.S.T.; da Silva, A.P.P.; Cabral, C.M.N.; Chiavegato, L.D. Effect of conventional physical therapy and Pilates in functionality, respiratory muscle strength and ability to exercise in hospitalized chronic renal patients: A randomized controlled trial. Clin Rehabil. 2017, 31, 508–520. [Google Scholar] [CrossRef]
- Tozim, B.M.; Navega, M.T. Effect of pilates method on inspiratory and expiratory muscle strength in the elderly. Rev. Bras. Cineantropometria Desempenho Hum. 2018, 20, 1–9. [Google Scholar] [CrossRef]
- Gildenhuys, G.; Fourie, M.; Shaw, I.; Shaw, B.; Toriola, A.; Witthuhn, J. Evaluation of Pilates training on agility, functional mobility and cardiorespiratory fitness in elderly women: Health and fitness. Afr. J. Phys. Act. Health Sci. 2013, 19, 505–512. [Google Scholar]
- Irez, G.B.; Ozdemir, R.A.; Evin, R.; Irez, S.G.; Korkusuz, F. Integrating pilates exercise into an exercise program for 65+ year-old women to reduce falls. J. Sport Sci. Med. 2011, 10, 105–111. [Google Scholar]
- De Siqueira Rodrigues, B.G.; Ali Cader, S.; Bento Torres, N.V.O.; de Oliveira, E.M.; Martin Dantas, E.H. Pilates method in personal autonomy, static balance and quality of life of elderly females. J. Bodyw. Mov. Ther. 2010, 14, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Lastra, M.A.; Martínez-Aldao, D.; Molina, A.J.; Ayán, C. Pilates for people with multiple sclerosis: A systematic review and meta-analysis. Mult. Scler. Relat. Disord. 2019, 28, 199–212. [Google Scholar] [CrossRef]
- Espíndula, R.C.; Nadas, G.B.; Rosa, M.I.D.; Foster, C.; Araújo, F.C.D.; Grande, A.J. Pilates for breast cancer: A systematic review and meta-analysis. Rev Assoc Med. Bras. 2006, 63, 1006–1011. [Google Scholar] [CrossRef]
- Mollinedo-Cardalda, I.; Cancela-Carral, J.M.; Vila-Suárez, M.H. Effect of a Mat Pilates Program with TheraBand on Dynamic Balance in Patients with Parkinson’s Disease: Feasibility Study and Randomized Controlled Trial. Rejuvenation Res. 2017, 21, 423–430. [Google Scholar] [CrossRef]
- Teixeira de Carvalho, F.; de Andrade Mesquita, L.S.; Pereira, R.; Neto, O.P.; Amaro Zangaro, R. Pilates and Proprioceptive Neuromuscular Facilitation Methods Induce Similar Strength Gains but Different Neuromuscular Adaptations in Elderly Women. Exp. Aging Res. 2017, 43, 440–452. [Google Scholar] [CrossRef]
- Lim, H.S.; Kim, Y.L.; Lee, S.M. The effects of Pilates exercise training on static and dynamic balance in chronic stroke patients: A randomized controlled trial. J. Phys. Ther. Sci. 2016, 28, 1819–1824. [Google Scholar] [CrossRef]
- Tinoco-Fernández, M.; Jiménez-Martín, M.; Sánchez-Caravaca, M.A.; Fernández-Pérez, A.M.; Ramírez-Rodrigo, J.; Villaverde-Gutiérrez, C. The Pilates method and cardiorespiratory adaptation to training. Res. Sport Med. 2016, 24, 281–286. [Google Scholar] [CrossRef]
- Mikalački, M.; Čokorilo, N.; Ruiz-Montero, P.J. The effects of a pilates-aerobic program on maximum exercise capacity of adult women. Rev. Bras. Med. Esporte 2017, 23, 246–249. [Google Scholar] [CrossRef]
- Rodrigues, A.Q.; Martins, F.M.; Barbosa, A.C.; Figueiredo, P.S.; Lima, M.O.; Vieira, E.R. Effects of an eleven-week pilates exercise program on progressive-speed walking capacity in sedentary young women: A pilot study. Hum. Mov. 2016, 17, 102–106. [Google Scholar] [CrossRef]
- Finatto, P.; Da Silva, E.S.; Okamura, A.B.; Almada, B.P.; Oliveira, H.B.; Peyre-Tartaruga, L.A. Pilates training improves 5-km run performance by changing metabolic cost and muscle activity in trained runners. PLoS ONE 2018, 13, e0194057. [Google Scholar] [CrossRef]
- Wells, C.; Kolt, G.S.; Bialocerkowski, A. Defining Pilates exercise: A systematic review. Complement. Ther. Med. 2012, 20, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Guimarães, G.V.; Carvalho, V.O.; Bocchi, E.A.; d’Avila, V.M. Pilates in Heart Failure Patients: A Randomized Controlled Pilot Trial. Cardiovasc. Ther. 2012, 30, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement (Chinese edition). J. Chinese Integr. Med. 2009, 7, 889–896. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available online: http://crtha.iums.ac.ir/files/crtha/files/cochrane.pdf (accessed on 22 October 2019).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ Effect. Public Health Pract. Proj. 1998, 2–5, in press. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Stiles, C.R.; Hagen, N.A.; Biondo, P.D.; Cummings, G.G. Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological research. J. Eval. Clin. Pract. 2012, 18, 12–18. [Google Scholar] [CrossRef]
- Thalheimer, W.; Cook, S. How to calculate effect sizes from published research articles: A simplified methodology. Work Res. 2002, 1, 1–9. [Google Scholar] [CrossRef]
- Schwarzer, G. Methods for Meta-analysis in Medical Research; Sutton, A.J., Abrams, K.R., Jones, D.R., Sheldon, T.A., Song, F., Eds.; Wiley: Chichester, UK, 2000; No. of pages: Xvii+317. Statist. Med. 2003, 22, 3112–3114; ISBN 0-471-49066-0. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Egger, M.; Smith, G.D. Investigating and dealing with publication and other biases in meta-analysis. Br. Med. J. 2001, 323, 101–105. [Google Scholar] [CrossRef]
- Wolkodoff, N.; Peterson, S.; Miller, J. The Fitness Effects of A Combined Aerobic and Pilates Program An Eight-Week Study Using The Stamina AeroPilates Pro XP555. AeroPilates Pro XP 555 Study 2008. [Google Scholar] [CrossRef]
- Rayes, A.B.R.; de Lira, C.A.B.; Viana, R.B. The effects of Pilates vs. aerobic training on cardiorespiratory fitness, isokinetic muscular strength, body composition, and functional tasks outcomes for individuals who are overweight/obese: A clinical trial. PeerJ 2019, 7, e6022. [Google Scholar] [CrossRef] [PubMed]
- Diamantoula, P.; Nikolaos, A.; Helen, S. Aqua pilates versus land pilates: Physical fitness outcomes. J. Phys. Educ. Sport 2016, 16, 573–578. [Google Scholar] [CrossRef]
- Daussin, F.N.; Ponsot, E.; Dufour, S.P. Improvement of VO2max by cardiac output and oxygen extraction adaptation during intermittent versus continuous endurance training. Eur. J. Appl. Physiol. 2007, 101, 377–383. [Google Scholar] [CrossRef] [PubMed]




| Population | Intervention | Outcome |
|---|---|---|
| Adults | Pilates | “Cardiorespiratory fitness” |
| OR | OR | OR |
| Middle aged | Mind-body | “Aerobic fitness” |
| OR | OR | OR |
| Young adult | Exercise Movement Techniques (Mesh) | “Aerobic capacity” |
| OR | ||
| “Heart rate” | ||
| OR | ||
| Cardiorespiratory fitness (Mesh) |
| Author | Design | Participants’ Characteristics | Mean Age | Sample Size (% Female) | Frequency | Period | Type of Pilates | Certified Instructor | Detailed Protocol | Outcome Measure | Outcome Results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wolkodoff 2008 [44] | CT | Sedentary (healthy) | PG = 23–64 | n = 20 PG = 14 (85.7%) CG = 6 (83.3%) | 40′/3.2xwk | 8wks | Both | NA | Yes | -Peak VO2 mL/kg/min (Oxycon Mobile) | CG change = 0.38 PG change = 6.06 17% of change in PG |
| Guimarães et al., 2012 [35] | RCPT | Heart failure | PG = 46 ± 12 CRG = 44 ± 11 | n = 16 PG = 8 (38%) CRG = 8 (19%) | 60′/2xwk | 16wks | Mat | Yes | Yes | -Peak VO2 mLO2/kg/min (Vmax 229 model, SensorMedics, Yorba Linda, CA, USA) | PG: improvements in peak VO2 (p = 0.01) Comparing both groups, PG showed greater improvement on peak VO2 (p = 0.02) |
| Gildenhuys et al., 2013 [22] | RCT | Elderly women (healthy) | PG = 66 ± 5 CG = 65 ± 5 | n = 50 PG = 25 (100%) CG = 25 (100%) | 60′/3xwk | 8wks | Mat | Yes | NA | -VO2 max mL.kg−1 min−1 (6minWalk; indirect equation) | PG did not significantly improve VO2 max (p = 0.247) |
| Lim HS et al., 2016 [29] | RCT | Chronic stroke | PG = 63 ± 8 CG = 62 ± 7 | n = 20 PG = 10 (40%) CG = 10 (50%) | 3xwk | 8wks | Mat | Yes | Yes | -VO2 max mL/min -VO2 max per kg (metabolic analyzer: Quark b2, COSMED, Italy 2011) | PG: VO2 max and VO2 max per kg increased significantly CG: VO2 max per kg diminished significantly |
| Diamantoula et al., 2016 [46] | Q-E | Sedentary women (healthy) | PG = 26 ± 5 AP = 21.3 ± 2 | PG land = 20 (100%) AP = 20 (100%) | 2xwk | 2years | Mat/aqua | NA | NA | -VO2 max mL/min (Ergometer cycle (Amila kh803), following the Astrand-Ryhming test, based on heart rate in submaximal effort) | No differences between groups, better VO2 max in total for both groups |
| Tinoco- Fernández et al., 2016 [30] | Q-E | Sedentary students (healthy) | PG = 18–35 | n = 45 PG = 45 (78%) | 60′/3xwk | 10wks | Mat | Yes | Yes | -VO2 max L/kg/min -VO2 max L/min (MasterScreen CPX apparatus) | Increment in peak VO2 and VO2 max |
| Rodrigues et al., 2016 [32] | Q-E | Sedentary women (healthy) | PG = 23 ± 2 | PG = 10 (100%) | 45′/2xwk | 11wks | Both | NA | Yes | -VO2 max mL.kg−1 min−1 portable metabolic system (VO2000®, MedGraphics®, St. Paul, MN, USA) | Peak VO2 tended to increase, but the differences were not statistically significant |
| Mikalacki et al., 2017 [31] | CT | Adult women (healthy) | PG = 48 ± 7 CG = 47 ± 7 | n = 64 PG = 36 (100%) CG = 28 (100%) | 55–60′/2xwk | NA | NA | NA | NA | -Relative VO2 max -Absolute VO2 max (Medisoft, model 870c) | PG: significant increase on relative VO2max, absolute VO2 max -CG: not significant changes |
| Finatto et al., 2018 [33] | RCT | Trained runners (healthy) | PG = 18 ± 1 CG = 18 ± 1 | n = 32 PG = 15–13 NA % CG = 16–15 | 60′/1xwk | 12wks | Mat | Yes | NA | -VO2 max mL.kg−1.min−1 (VO2000 (Medgraphics, Ann Arbor, USA) | PG: significantly higher values on VO2 max (p < 0.001) |
| Rayes et al., 2019 [45] | RCT | Overweight/obese | PG = 55.9 ± 6.6 CG = 45.5 ± 9.3 | n = 60 NA% PG = 22 CG = 25/17 | 60′/3xwk | 8wks | Both | Yes | Yes | -VO2 max (mL/kg/min) (motorized treadmill; Inbrasport, ATL, Porto Alegre, Brazil) | PG: Significant improvement on VO2 max CG: not significant changes |
| Pilates Method vs. Control Author, Year | ES | LL | UL | I2 |
|---|---|---|---|---|
| Guimarães et al., 2012 [35] | 0.6 | 0.12 | 1.08 | 70.8 |
| Gildenhuys et al., 2013 [22] | 0.69 | 0.20 | 1.18 | 64.4 |
| Lim HS et al., 2016 [29] | 0.62 | 0.10 | 1.14 | 70.7 |
| Mikalacki et al., 2017 [31] | 0.62 | 0.03 | 1.22 | 70.8 |
| Finatto et al., 2018 [33] | 0.4 | 0.16 | 0.64 | 0 |
| Rossell-Rayes et al., 2019 [45] | 0.63 | 0.12 | 1.15 | 70.4 |
| Pilates Method vs. Control | ||||
|---|---|---|---|---|
| ES | LL | UL | I2 | |
| Healthy | 0.80 | −0.05 | 1.65 | 85 |
| Unhealthy | 0.40 | −0.01 | 0.81 | 0 |
| Coefficient | p | |
|---|---|---|
| Pilates Method vs. control | 0.04 | 0.03 * |
| Coefficient | p-Value | |
|---|---|---|
| Pilates method vs. control group | 1.64 | 0.47 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Rodríguez, R.; Álvarez-Bueno, C.; Ferri-Morales, A.; Torres-Costoso, A.I.; Cavero-Redondo, I.; Martínez-Vizcaíno, V. Pilates Method Improves Cardiorespiratory Fitness: A Systematic Review and Meta-Analysis. J. Clin. Med. 2019, 8, 1761. https://doi.org/10.3390/jcm8111761
Fernández-Rodríguez R, Álvarez-Bueno C, Ferri-Morales A, Torres-Costoso AI, Cavero-Redondo I, Martínez-Vizcaíno V. Pilates Method Improves Cardiorespiratory Fitness: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2019; 8(11):1761. https://doi.org/10.3390/jcm8111761
Chicago/Turabian StyleFernández-Rodríguez, Rubén, Celia Álvarez-Bueno, Asunción Ferri-Morales, Ana I. Torres-Costoso, Iván Cavero-Redondo, and Vicente Martínez-Vizcaíno. 2019. "Pilates Method Improves Cardiorespiratory Fitness: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 8, no. 11: 1761. https://doi.org/10.3390/jcm8111761
APA StyleFernández-Rodríguez, R., Álvarez-Bueno, C., Ferri-Morales, A., Torres-Costoso, A. I., Cavero-Redondo, I., & Martínez-Vizcaíno, V. (2019). Pilates Method Improves Cardiorespiratory Fitness: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 8(11), 1761. https://doi.org/10.3390/jcm8111761








