Videocapillaroscopy of the Oral Mucosa in Patients with Diabetic Foot: Possible Diagnostic Role of Microangiopathic Damage?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
- Patients without foot ulcers with a history of diabetes of more than 10 years (WFU), coding of diagnosis type 1 or 2 was established, based on clinical/GP records (HbA1c);
- Patients with neuropathic diabetic foot (diagnosed through positive results in the Semmens-Weinstein monofilament test (10 g monofilament to determine the loss of protective sensations-Darco footfilament), absence of patellar and Achilles reflexes, presence of deformity and possible plantar ulcers) (NDF); the patients have to meet all these criteria for consider them as neuropathic;
- Patients with ischemic diabetic foot (diagnosed on the basis of clinical parameters like color and temperature and doppler examination of the vessels in the lower limbs; positive markers like Ankle-Brachial Pressure Index (ABPI) were also used) (IDF).
2.2. Exclusion Criteria
- Patients with oral pathologies (candidiasis, lichen planus, glossitis, periodontitis, etc., so patients had a healthy mucosa) and systemic pathologies (vitamin and mineral deficiencies, autoimmune disorders, etc.);
- Patients with previous vascular intervention e.g., femoral bypass graft/ treated vascular disease were excluded;
- Smokers, patients who had reported a previous appearance of mycosis, hypertensive patients (because of the collateral effects of their pharmacological therapy) and, in general, patients submitted to daily pharmacological treatments (except those for diabetic disease).
- A central body, containing the light source (halogen lamp), the video capture electronics, the main manual controls for adjusting brightness, contrast, color balance, etc.;
- An optical probe with a 200× terminal and 2 m long cord. The probe has a rotating focusing wheel;
- A PC with dedicated software (VideoCap software version 8.1) capable of capturing, storing and editing capillaroscopic images.
- The sites investigated for each patient were the following:
- Labial mucosa, at the level of the lower lip;
- The retro-commissural region of the buccal mucosa;
- Masticatory mucosa (adherent alveolar mucosa in the case of an edentulous patient).
- -
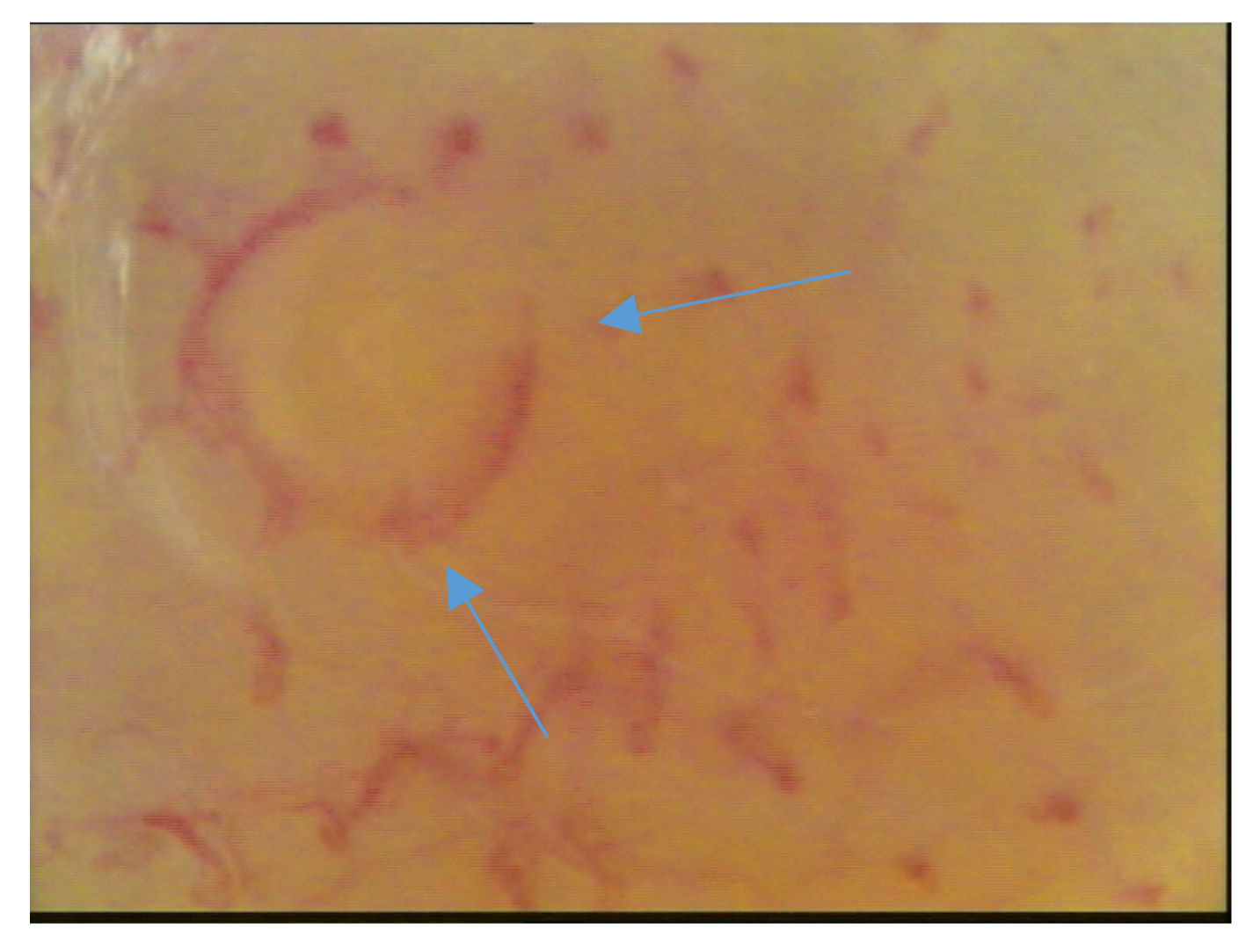
- The density of the capillary loops (the number of loops visible per square millimeter) (Figure 2);
- -
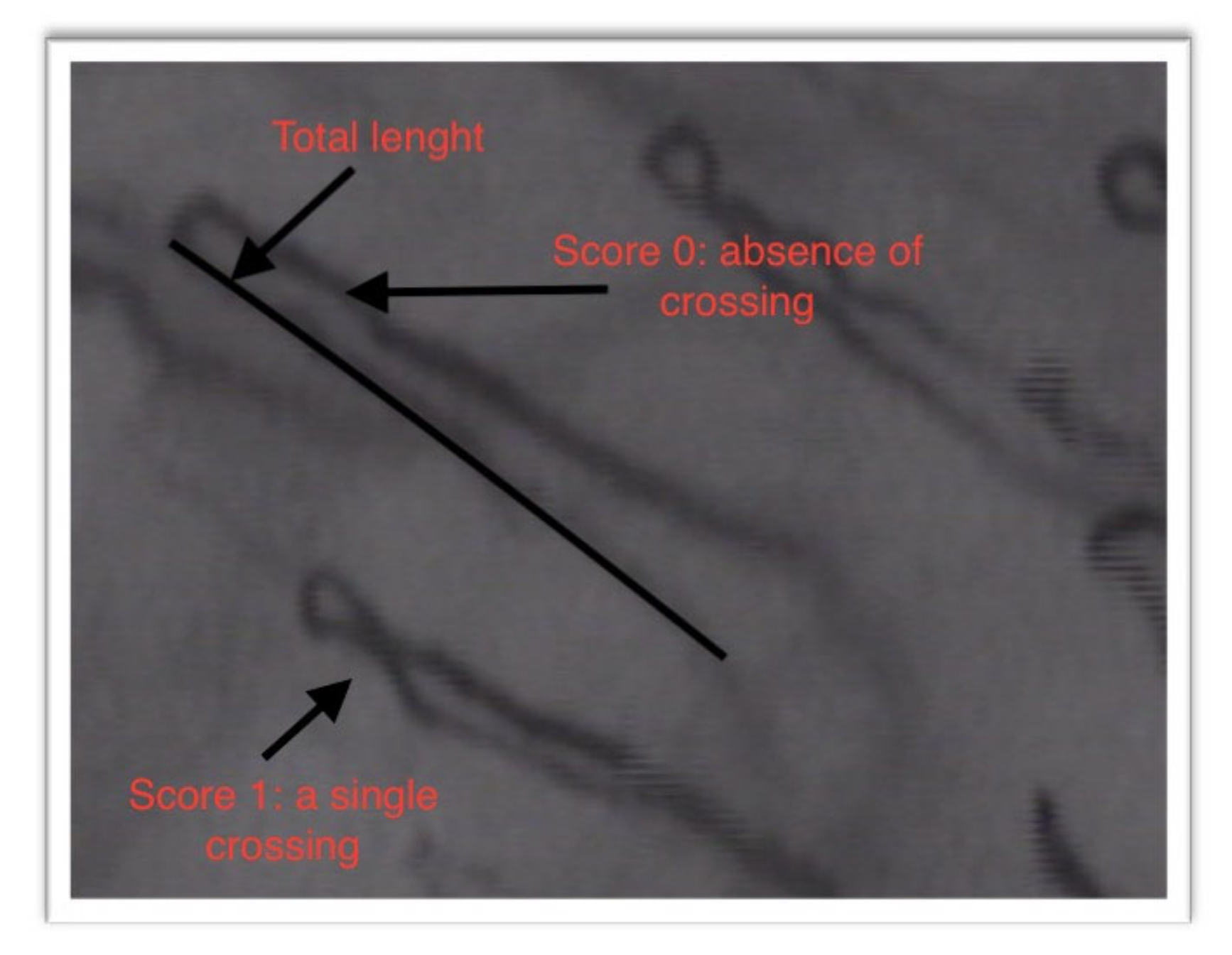
- Total length of the capillary loops and their size (Figure 3);
- -
- The degree of tortuosity of the capillary loops: the evaluation of the tortuosity of the capillary loops was carried out by attributing points from 0 to 3, according to the number of crossings that they had:
- Score 0: absence of crossing
- Score 1: a single crossing
- Score 2: more than double crossings
- Score 3: distorted loops
- -
- Presence/absence of capillary loops with atypical morphology.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Grennan, D. Diabetic Foot Ulcers. JAMA 2019, 321, 114. [Google Scholar] [CrossRef]
- Gherman, D.; Dumitrescu, C.I.; Ciocan, A.; Melincovici, C.S. Histopathological changes in major amputations due to diabetic foot—A review. Rom. J. Morphol. Embryol. 2018, 59, 699–702. [Google Scholar]
- Mishra, S.C.; Chhatbar, K.C.; Kashikar, A.; Mehndiratta, A. Diabetic foot. BMJ 2017, 359, j5064. [Google Scholar] [CrossRef] [Green Version]
- Mennes, O.A.; Van Netten, J.J.; Slart, R.H.; Steenbergen, W. Novel Optical Techniques for Imaging Microcirculation in the Diabetic Foot. Curr. Pharm. Des. 2018, 24, 1304–1316. [Google Scholar] [CrossRef] [Green Version]
- Mennes, O.A.; Van Netten, J.J.; Van Baal, J.G.; Steenbergen, W. Assessment of microcirculation in the diabetic foot with laser speckle contrast imaging. Physiol. Meas. 2019, 40, 065002. [Google Scholar] [CrossRef]
- Dinh, T. Microcirculation of the Diabetic Foot. Curr. Pharm. Des. 2005, 11, 2301–2309. [Google Scholar] [CrossRef]
- Noor, S.; Zubair, M.; Ahmad, J. Diabetic foot ulcer—A review on pathophysiology, classification and microbial etiology. Diabetes Metab. Syndr. Clin. Res. Rev. 2015, 9, 192–199. [Google Scholar] [CrossRef]
- Game, F. Classification of diabetic foot ulcers. Diabetes Metab. Res. Rev. 2016, 32, 186–194. [Google Scholar] [CrossRef]
- Monteiro-Soares, M.; Martins-Mendes, D.; Vaz-Carneiro, A.; Sampaio, S.; Dinis-Ribeiro, M. Classification systems for lower extremity amputation prediction in subjects with active diabetic foot ulcer: A systematic review and meta-analysis. Diabetes Metab. Res. Rev. 2014, 30, 610–622. [Google Scholar] [CrossRef]
- Sharma, S.; Schaper, N.C.; Rayman, G. Microangiopathy: Is it relevant to wound healing in diabetic foot disease? Diabetes Metab. Res. Rev. 2020, 36 (Suppl. S1), e3244. [Google Scholar] [CrossRef] [Green Version]
- Barwell, N.D.; Devers, M.C.; Kennon, B.; Hopkinson, H.E.; McDougall, C.; Young, M.J.; Robertson, H.M.A.; Stang, D.; Dancer, S.J.; Seaton, A.; et al. Diabetic foot infection: Antibiotic therapy and good practice recommendations. Int. J. Clin. Pr. 2017, 71, e13006. [Google Scholar] [CrossRef] [Green Version]
- Migdalis, I.; Czupryniak, L.; Lalic, N.; Leslie, R.D.; Papanas, N.; Valensi, P. The Diabetic Foot. J. Diabetes Res. 2017, 2017, 3585617. [Google Scholar] [CrossRef] [Green Version]
- Scardina, G.A.; Ruggieri, A.; Messina, P. Oral microcirculation observed in vivo by videocapillaroscopy: A review. J. Oral Sci. 2009, 51, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Scardina, G.A.; Messina, P. Study of the microcirculation of oral mucosa in healthy subjects. Ital. J. Anat. Embryol. 2003, 108, 39–48. [Google Scholar]
- Scardina, G.A.; Messina, M.; Melilli, D.; Cumbo, E.; Carini, F.; Tomasello, G.; Messina, P. Permanence of Modifications in Oral Microcirculation in Ex-Smokers. Med. Sci. Monit. 2019, 25, 866–871. [Google Scholar] [CrossRef]
- Tchero, H.; Kangambega, P.; Lin, L.; Mukisi-Mukaza, M.; Brunet-Houdard, S.; Briatte, C.; Retali, G.R.; Rüsch, E. Cost of diabetic foot in France, Spain, Italy, Germany and United Kingdom: A systematic review. Ann. d’Endocrinologie 2018, 79, 67–74. [Google Scholar] [CrossRef]
- Hile, C.; Veves, A. Diabetic neuropathy and microcirculation. Curr. Diabetes Rep. 2003, 3, 446–451. [Google Scholar] [CrossRef]
- Behroozian, A.; Beckman, J.A. Microvascular Disease Increases Amputation in Patients with Peripheral Artery Disease. Arter. Thromb. Vasc. Biol. 2020, 40, 534–540. [Google Scholar] [CrossRef]
- Ogawa, K.; Sasaki, H.; Yamasaki, H.; Okamoto, K.; Matsuno, S.; Shono, T.; Doi, T.; Arimoto, K.; Furuta, H.; Nishi, M.; et al. Peripheral nerve functions may deteriorate parallel to the progression of microangiopathy in diabetic patients. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 313–321. [Google Scholar] [CrossRef]
- Pérez-Panero, A.J.; Ruiz-Muñoz, M.; Cuesta-Vargas, A.I.; Gónzalez-Sánchez, M. Prevention, assessment, diagnosis and management of diabetic footbased on clinical practice guidelines: A systematic review. Medicine 2019, 98, e16877. [Google Scholar] [CrossRef]
- Fang, F.; Wang, J.; Wang, Y.-F.; Peng, Y.-D. Microangiopathy in diabetic polyneuropathy revisited. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 6456–6462. [Google Scholar]
- Scardina, G.A.; Citarrella, R.; Messina, P. Diabetic Microagiopathy of Oral Mucosa Depends on Disease Duration and Therapy. Med. Sci. Monit. 2017, 23, 5613–5619. [Google Scholar] [CrossRef] [Green Version]
- Wadowski, P.P.; Kautzky-Willer, A.; Gremmel, T.; Koppensteiner, R.; Wolf, P.; Ertl, S.; Weikert, C.; Schörgenhofer, C.; Jilma, B. Sublingual microvasculature in diabetic patients. Microvasc. Res. 2020, 129, 103971. [Google Scholar] [CrossRef]
- Scardina, G.A.; Cacioppo, A.; Pisano, T.; Messina, P. In vivo evaluation of labial microcirculation in diabetics: A comparison with healthy subjects. Panminerva Med. 2011, 53, 81–85. [Google Scholar]
- Scardina, G.A.; Cacioppo, A.; Messina, P. Periodontal microcirculation in diabetics: An in vivo non-invasive analysis by means of videocapillaroscopy. Med. Sci. Monit. 2012, 18, CR58–CR64. [Google Scholar] [CrossRef]



| Characteristics of the Subjects | HS | WFU | NDF | IDF |
|---|---|---|---|---|
| Mean age | 66.43 ± 10.64 | 63.31 ± 12.01 | 63 ± 9.3 | 75 ± 11.6 |
| Age range | 44–78 | 28–72 | 43–79 | 52–97 |
| Male/Female ratio | 8–7 | 8–7 | 8–7 | 8–7 |
| Mean diabetes duration | 0 | 21 ± 6.9 years | 22.6 ± 12.0 years | 23.7 ± 11.6 years |
| Variables (Mean ± SD) | Lower Lip | Retro-Commissural Buccal Mucosa | Masticatory Mucosa |
|---|---|---|---|
| HS n/mm3 | 19.04 ± 3.16 | 17.43 ± 2.34 | 26.74 ± 3.45 |
| WFU n/mm3 | 12.98 ± 3.1 (−31.83%) (S) | 11.63 ± 3.7 (−33.3%) (S) | 19.74 ± 2.4 (−26.2%) (S) |
| NDF n/mm3 | 7.32 ± 2.1 (−61.6%) (S) | 6.21 ± 3.4 (−64.4%) (S) | 13.56 ± 2.6 (−49.3%) (S) |
| IDF n/mm3 | 4.32 ± 3.2 (−77.3%) (S) | 3.2 ± 1.7 (−81.6%) (S) | 6.5 ± 2.1 (−75.7%) (S) |
| Variables (Mean ± SD) | Lower Lip | Retro-Commissural Buccal Mucosa |
|---|---|---|
| HS μm | 0.203 ± 0.023 | 0.245 ± 0.05 |
| WFU μm | 0.383 ± 0.013 (+88.7%) (S) | 0.366 ± 0.04 (+49.4%) (S) |
| NDF μm | 0.190 ± 0.04 (−6.4%) (S) | 0.205 ± 0.02 (−16.3%) (S) |
| IDF μm | 0.178 ± 0.02 (−12.3%) (S) | 0.232 ± 0.05 (−5.3%) (NS) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scardina, G.A.; Guercio, G.; Valenti, C.F.; Tegolo, D.; Messina, P. Videocapillaroscopy of the Oral Mucosa in Patients with Diabetic Foot: Possible Diagnostic Role of Microangiopathic Damage? J. Clin. Med. 2020, 9, 3641. https://doi.org/10.3390/jcm9113641
Scardina GA, Guercio G, Valenti CF, Tegolo D, Messina P. Videocapillaroscopy of the Oral Mucosa in Patients with Diabetic Foot: Possible Diagnostic Role of Microangiopathic Damage? Journal of Clinical Medicine. 2020; 9(11):3641. https://doi.org/10.3390/jcm9113641
Chicago/Turabian StyleScardina, Giuseppe A., Giovanni Guercio, Cesare F. Valenti, Domenico Tegolo, and Pietro Messina. 2020. "Videocapillaroscopy of the Oral Mucosa in Patients with Diabetic Foot: Possible Diagnostic Role of Microangiopathic Damage?" Journal of Clinical Medicine 9, no. 11: 3641. https://doi.org/10.3390/jcm9113641
APA StyleScardina, G. A., Guercio, G., Valenti, C. F., Tegolo, D., & Messina, P. (2020). Videocapillaroscopy of the Oral Mucosa in Patients with Diabetic Foot: Possible Diagnostic Role of Microangiopathic Damage? Journal of Clinical Medicine, 9(11), 3641. https://doi.org/10.3390/jcm9113641






