Prevention of Cardiometabolic Syndrome in Children and Adolescents Using Machine Learning and Noninvasive Factors: The CASPIAN-V Study
Abstract
:1. Introduction
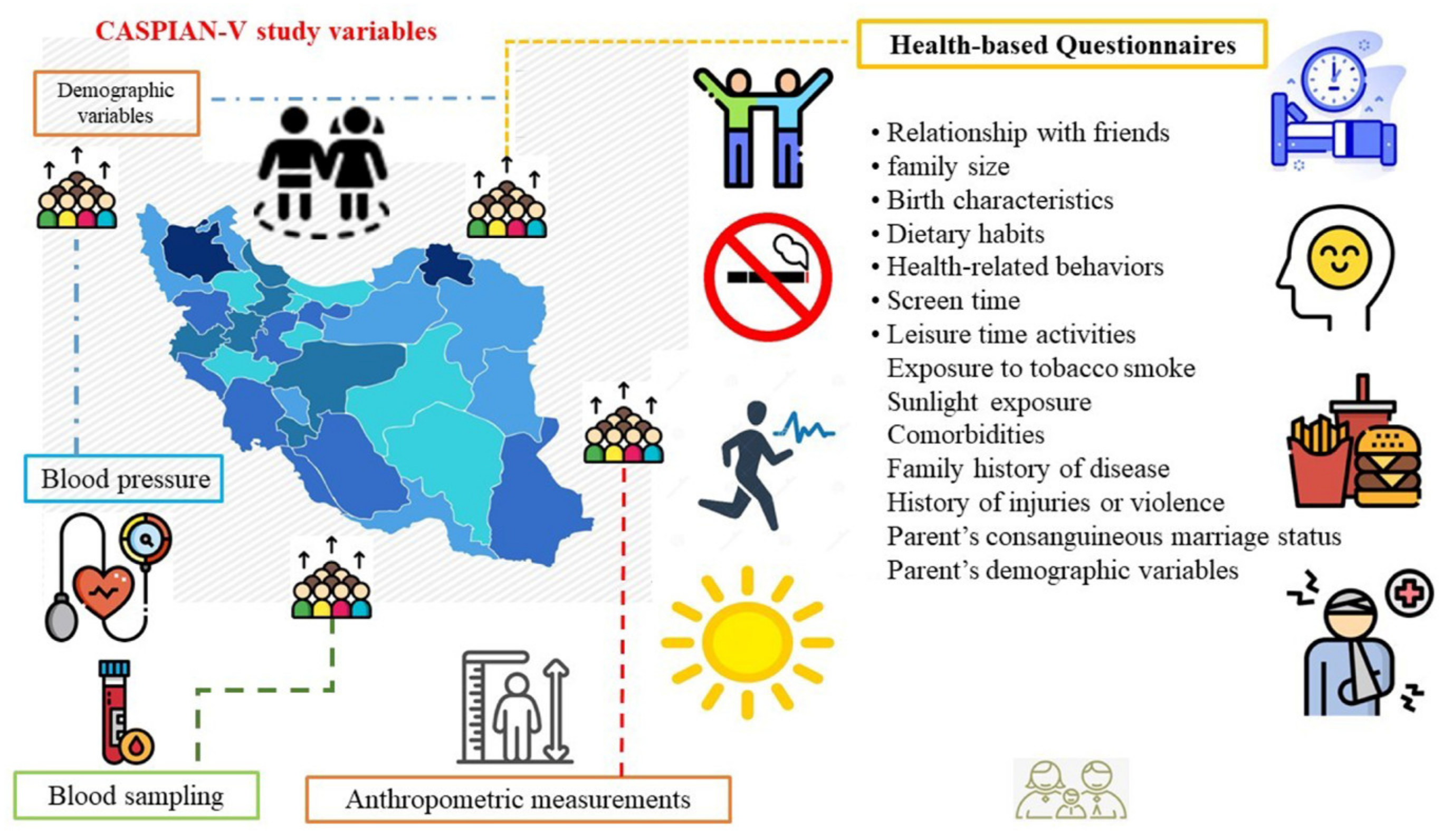
2. Materials and Methods
2.1. Materials
2.2. Procedure and Measurements
2.2.1. Questionnaires
2.2.2. Anthropometric Measurements
2.2.3. Blood Pressure Measurement
2.2.4. Blood Sampling
2.2.5. Outcome Definition
2.2.6. Ethical Statement
2.3. Predictors and Feature Extraction
2.4. Model Construction and Interpretation
2.5. Validation
2.6. Statistical Analysis
3. Results
3.1. Descriptive and Inferential Statistics
3.1.1. Demographic Characteristics
3.1.2. Social and Family Characteristics
3.1.3. Health Behaviors
3.1.4. Dietary Habits
3.1.5. Family Health History and Lifestyle Factors
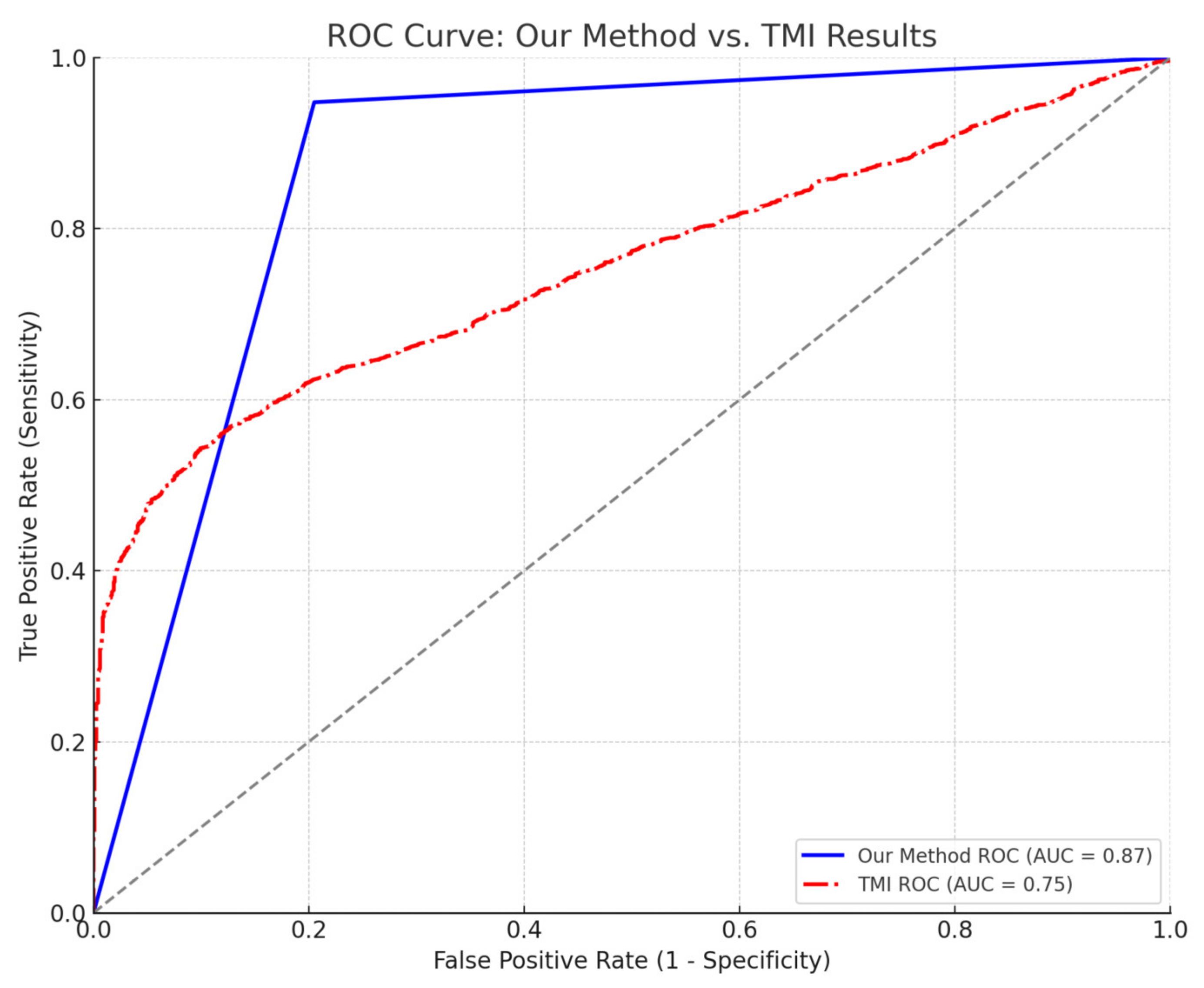
3.2. Classification Results
4. Discussion
4.1. Choice of the Classifier
4.2. Comparison with the State-of-the-Art
4.3. Selected Predictors
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, Z.; Fan, S.; Xue, Z.; Yuan, J.; Zhou, Z.; Wang, T.; Liu, J.; Bawudun, A.; Nurmamat, N.; Wang, Y.; et al. Evaluation of the appropriate predictive contributor and diagnostic threshold for the cardio-metabolic syndrome in Chinese Uyghur adults. BMC Public Health 2019, 19, 613. [Google Scholar] [CrossRef] [PubMed]
- Castro, J.P.; El-Atat, F.A.; McFarlane, S.I.; Aneja, A.; Sowers, J.R. Cardiometabolic syndrome: Pathophysiology and treatment. Curr. Hypertens. Rep. 2003, 5, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, A.K. Challenges in the treatment of cardiometabolic syndrome. Indian J. Pharmacol. 2012, 44, 155–156. [Google Scholar] [CrossRef] [PubMed]
- Dabelea, D.; Mayer-Davis, E.J.; Saydah, S.; Imperatore, G.; Linder, B.; Divers, J.; Bell, R.; Badaru, A.; Talton, J.W.; Crume, T.; et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. Jama 2014, 311, 1778–1786. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.L.; Stafford, L.K.; McLaughlin, S.A.; Boyko, E.J.; Vollset, S.E.; Smith, A.E.; Dalton, B.E.; Duprey, J.; Cruz, J.A.; Hagins, H.; et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef] [PubMed]
- Kelli, H.M.; Kassas, I.; Lattouf, O.M. Cardio metabolic syndrome: A global epidemic. J. Diabetes Metab. 2015, 6, 2. [Google Scholar] [CrossRef]
- Sarrafzadegan, N.; Mohammmadifard, N. Cardiovascular Disease in Iran in the Last 40 Years: Prevalence, Mortality, Morbidity, Challenges and Strategies for Cardiovascular Prevention. Arch. Iran. Med. 2019, 22, 204–210. [Google Scholar]
- Shams-Beyranvand, M.; Farzadfar, F.; Naderimagham, S.; Tirani, M.; Maracy, M.R. Estimation of burden of ischemic heart diseases in Isfahan, Iran, 2014: Using incompleteness and misclassification adjustment models. J. Diabetes Metab. Disord. 2017, 16, 12. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.; Fruchart, J.; Smith, S. Harmonizing the Metabolic syndrome. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef]
- Tanrikulu, M.A.; Agirbasli, M.; Berenson, G. Primordial prevention of cardiometabolic risk in childhood. In Hypertension: From Basic Research to Clinical Practice; Springer: Berlin/Heidelberg, Germany, 2016; pp. 489–496. [Google Scholar]
- Marateb, H.R.; Tasdighi, Z.; Mohebian, M.R.; Naghavi, A.; Hess, M.; Motlagh, M.E.; Heshmat, R.; Mansourian, M.; Mañanas, M.A.; Binder, H.; et al. Classification of psychiatric symptoms using deep interaction networks: The CASPIAN-IV study. Sci. Rep. 2021, 11, 15706. [Google Scholar] [CrossRef]
- Trigka, M.; Dritsas, E. Predicting the Occurrence of Metabolic Syndrome Using Machine Learning Models. Computation 2023, 11, 170. [Google Scholar] [CrossRef]
- Kim, J.; Mun, S.; Lee, S.; Jeong, K.; Baek, Y. Prediction of metabolic and pre-metabolic syndromes using machine learning models with anthropometric, lifestyle, and biochemical factors from a middle-aged population in Korea. BMC Public Health 2022, 22, 664. [Google Scholar] [CrossRef] [PubMed]
- Kupusinac, A.; Doroslovački, R.; Malbaški, D.; Srdić, B.; Stokić, E. A primary estimation of the cardiometabolic risk by using artificial neural networks. Comput. Biol. Med. 2013, 43, 751–757. [Google Scholar] [CrossRef]
- Hollenbeak, C.S.; Spackman, D.E.; Ben-Joseph, R.H.; Okamoto, L.J.; Luce, B.R.; Schwartz, J.S.; Sullivan, S.D. Predicting the prevalence of cardiometabolic risk factors when clinical data are limited. Value Health 2007, 10, S4–S11. [Google Scholar] [CrossRef]
- Ashley-Martin, J.; Ensenauer, R.; Maguire, B.; Kuhle, S. Predicting cardiometabolic markers in children using tri-ponderal mass index: A cross-sectional study. Arch. Dis. Child. 2019, 104, 577–582. [Google Scholar] [CrossRef]
- Ojanen, X.; Cheng, R.; Törmäkangas, T.; Rappaport, N.; Wilmanski, T.; Wu, N.; Fung, E.; Nedelec, R.; Sebert, S.; Vlachopoulos, D.; et al. Towards early risk biomarkers: Serum metabolic signature in childhood predicts cardio-metabolic risk in adulthood. eBioMedicine 2021, 72, 103611. [Google Scholar] [CrossRef]
- Kelishadi, R.; Heidari-Beni, M.; Qorbani, M.; Motamed-Gorji, N.; Motlagh, M.E.; Ziaodini, H.; Taheri, M.; Ahadi, Z.; Aminaee, T.; Heshmat, R. Association between neck and wrist circumferences and cardiometabolic risk in children and adolescents: The CASPIAN-V study. Nutrition 2017, 43–44, 32–38. [Google Scholar] [CrossRef]
- WHO. Physical status: The use and interpretation of anthropometry. In Report of a WHO Expert Committee; WHO Technical Report Series 854; World Health Organization: Geneva, Switzerland, 1995. [Google Scholar]
- Fredriks, A.M.; van Buuren, S.; Wit, J.M.; Verloove-Vanhorick, S. Body index measurements in 1996–1997 compared with 1980. Arch. Dis. Child. 2000, 82, 107–112. [Google Scholar] [CrossRef]
- Knowles, K.; Paiva, L.; Sanchez, S.; Revilla, L.; Lopez, T.; Yasuda, M.; Yanez, N.; Gelaye, B.; Williams, M. Waist circumference, body mass index, and other measures of adiposity in predicting cardiovascular disease risk factors among Peruvian adults. Int. J. Hypertens. 2011, 2011, 931402. [Google Scholar] [CrossRef]
- Rosner, B.; Cook, N.R.; Daniels, S.; Falkner, B. Childhood blood pressure trends and risk factors for high blood pressure: The NHANES experience 1988–2008. Hypertension 2013, 62, 247–254. [Google Scholar] [CrossRef]
- Zimmet, P.; Alberti, K.G.; Kaufman, F.; Tajima, N.; Silink, M.; Arslanian, S.; Wong, G.; Bennett, P.; Shaw, J.; Caprio, S. The metabolic syndrome in children and adolescents-an IDF consensus report. Pediatr. Diabetes 2007, 8, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Kavey, R.-E.W.; Daniels, S.R.; Lauer, R.M.; Atkins, D.L.; Hayman, L.L.; Taubert, K. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation 2003, 107, 1562–1566. [Google Scholar] [CrossRef] [PubMed]
- Genuth, S.; Alberti, K.; Bennett, P.; Buse, J.; DeFronzo, R.; Kahn, R.; Kitzmiller, J.; Knowler, W.C.; Lebovitz, H.; Lernmark, A. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003, 26, 3160–3168. [Google Scholar] [PubMed]
- Soofi, M.; Pasdar, Y.; Karami Matin, B.; Hamzeh, B.; Rezaei, S.; Kazemi Karyani, A.; Moradi Nazar, M.; Soltani, S.; Hajizadeh, M.; Salimi, Y.; et al. Socioeconomic-related inequalities in oral hygiene behaviors: A cross-sectional analysis of the PERSIAN cohort study. BMC Oral. Health 2020, 20, 63. [Google Scholar] [CrossRef]
- Alharbi, K.K.; Al-Sheikh, Y.A.; Alsaadi, M.M.; Mani, B.; Udayaraja, G.K.; Kohailan, M.; Ali Khan, I. Screening for obesity in the offspring of first-cousin consanguineous couples: A Phase-I study in Saudi Arabia. Saudi J. Biol. Sci. 2020, 27, 242–246. [Google Scholar] [CrossRef]
- Meller, F.O.; Loret de Mola, C.; Assunção, M.C.F.; Schäfer, A.A.; Dahly, D.L.; Barros, F.C. Birth order and number of siblings and their association with overweight and obesity: A systematic review and meta-analysis. Nutr. Rev. 2018, 76, 117–124. [Google Scholar] [CrossRef]
- Evensen, E.; Emaus, N.; Kokkvoll, A.; Wilsgaard, T.; Furberg, A.-S.; Skeie, G. The relation between birthweight, childhood body mass index, and overweight and obesity in late adolescence: A longitudinal cohort study from Norway, The Tromsø Study, Fit Futures. BMJ Open 2017, 7, e015576. [Google Scholar] [CrossRef]
- Kelishadi, R.; Farajian, S. The protective effects of breastfeeding on chronic non-communicable diseases in adulthood: A review of evidence. Adv. Biomed. Res. 2014, 3, 3. [Google Scholar] [CrossRef]
- Angoorani, P.; Mostafaei, S.; Kiani, T.; Ejtahed, H.-S.; Motlagh, M.E.; Shafiee, G.; Gorabi, A.M.; Qorbani, M.; Heshmat, R.; Kelishadi, R. Determinants of childhood blood pressure using structure equation model: The CASPIAN–V study. BMC Cardiovasc. Disord. 2020, 20, 193. [Google Scholar] [CrossRef]
- Marateb, H.R.; Mohebian, M.R.; Javanmard, S.H.; Tavallaei, A.A.; Tajadini, M.H.; Heidari-Beni, M.; Mañanas, M.A.; Motlagh, M.E.; Heshmat, R.; Mansourian, M.; et al. Prediction of dyslipidemia using gene mutations, family history of diseases and anthropometric indicators in children and adolescents: The CASPIAN-III study. Comput. Struct. Biotechnol. J. 2018, 16, 121–130. [Google Scholar] [CrossRef]
- Heshmat, R.; Hemati, Z.; Payab, M.; Hamzeh, S.S.; Motlagh, M.E.; Shafiee, G.; Taheri, M.; Ziaodini, H.; Qorbani, M.; Kelishadi, R. Prevalence of different metabolic phenotypes of obesity in Iranian children and adolescents: The CASPIAN V study. J. Diabetes Metab. Disord. 2018, 17, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Khashayar, P.; Kasaeian, A.; Heshmat, R.; Motlagh, M.E.; Mahdavi Gorabi, A.; Noroozi, M.; Qorbani, M.; Kelishadi, R. Childhood overweight and obesity and associated factors in iranian children and adolescents: A multilevel analysis; the CASPIAN-IV study. Front. Pediatr. 2018, 6, 393. [Google Scholar] [CrossRef] [PubMed]
- Shah, B.; Cost, K.T.; Fuller, A.; Birken, C.S.; Anderson, L.N. Sex and gender differences in childhood obesity: Contributing to the research agenda. BMJ Nutr. Prev. Health 2020, 3, 387. [Google Scholar] [CrossRef] [PubMed]
- Angoorani, P.; Mahmoodi, Z.; Ejtahed, H.-S.; Heshmat, R.; Motlagh, M.E.; Qorbani, M.; Kelishadi, R. Determinants of life satisfaction and self-rated health in Iranian children and adolescents: A structure equation model. BMC Pediatr. 2022, 22, 4. [Google Scholar] [CrossRef]
- Pipoyan, D.; Stepanyan, S.; Stepanyan, S.; Beglaryan, M.; Costantini, L.; Molinari, R.; Merendino, N. The Effect of Trans Fatty Acids on Human Health: Regulation and Consumption Patterns. Foods 2021, 10, 2452. [Google Scholar] [CrossRef]
- Unal, I. Defining an Optimal Cut-Point Value in ROC Analysis: An Alternative Approach. Comput. Math. Methods Med. 2017, 2017, 3762651. [Google Scholar] [CrossRef]
- Baradaran Mahdavi, S.; Mansourian, M.; Shams, E.; Qorbani, M.; Heshmat, R.; Motlagh, M.E.; Ziaodini, H.; Dashti, R.; Taheri, M.; Kelishadi, R. Association of Sunlight Exposure with Sleep Hours in Iranian Children and Adolescents: The CASPIAN-V Study. J. Trop. Pediatr. 2020, 66, 4–14. [Google Scholar] [CrossRef]
- Bishop, C.M. Pattern Recognition and Machine Learning; Springer: New York, NY, USA, 2006; p. 738. [Google Scholar]
- Lafi, S.Q.; Kaneene, J.B. An explanation of the use of principal-components analysis to detect and correct for multicollinearity. Prev. Vet. Med. 1992, 13, 261–275. [Google Scholar] [CrossRef]
- Jakobsen, J.C.; Gluud, C.; Wetterslev, J.; Winkel, P. When and how should multiple imputation be used for handling missing data in randomised clinical trials—A practical guide with flowcharts. BMC Med. Res. Methodol. 2017, 17, 162. [Google Scholar] [CrossRef]
- van Buuren, S.; Groothuis-Oudshoorn, K. mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of the 22nd ACM Sigkdd International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Friedman, J.; Hastie, T.; Tibshirani, R. Additive logistic regression: A statistical view of boosting (With discussion and a rejoinder by the authors). Ann. Stat. 2000, 28, 337–407. [Google Scholar] [CrossRef]
- Friedman, J.H. Greedy Function Approximation: A Gradient Boosting Machine. Ann. Stat. 2001, 29, 1189–1232. [Google Scholar] [CrossRef]
- Bergstra, J.; Bardenet, R.; Bengio, Y.; Kégl, B. Algorithms for hyper-parameter optimization. Adv. Neural Inf. Process. Syst. 2011, 24, 2546–2554. [Google Scholar]
- Yu, T.; Zhu, H. Hyper-parameter optimization: A review of algorithms and applications. arXiv 2020, arXiv:2003.05689. [Google Scholar]
- Mansourian, M.; Marateb, H.R.; Mansourian, M.; Mohebbian, M.R.; Binder, H.; Mañanas, M.Á. Rigorous performance assessment of computer-aided medical diagnosis and prognosis systems: A biostatistical perspective on data mining. In Modelling and Analysis of Active Biopotential Signals in Healthcare; IOP Publishing: Bristol, UK, 2020; Volume 2. [Google Scholar] [CrossRef]
- ISO/IEC TS 4213; Information Technology—Artificial Intelligence—Assessment of Machine Learning Classification Performance. International Organization for Standardization: Geneva, Switzerland, 2022.
- Kuncheva, L. Fundamentals of Pattern Recognition. In Combining Pattern Classifiers; Kuncheva, L., Ed.; John Wiley & Sons: Hoboken, NJ, USA, 2004; pp. 1–43. [Google Scholar]
- Forseth, B.; Noel-MacDonnell, J.R.; Hampl, S.; Carlson, J.A.; Halpin, K.; Davis, A.; Phillips, T.; Shook, R.P. Relationship between youth cardiometabolic health and physical activity in medical records. PLoS ONE 2024, 19, e0303583. [Google Scholar] [CrossRef] [PubMed]
- Gul Siraz, U.; Hatipoglu, N.; Mazicioglu, M.M.; Ozturk, A.; Cicek, B.; Kurtoglu, S. Triponderal mass index is as strong as body mass index in the determination of obesity and adiposity. Nutrition 2023, 105, 111846. [Google Scholar] [CrossRef]
- Zhang, T.; Lu, G.; Wu, X.Y. Associations between physical activity, sedentary behaviour and self-rated health among the general population of children and adolescents: A systematic review and meta-analysis. BMC Public Health 2020, 20, 1343. [Google Scholar] [CrossRef]
- Näslindh-Ylispangar, A.; Sihvonen, M.; Vanhanen, H.; Kekki, P. Self-rated health and risk factors for metabolic syndrome among middle-aged men. Public Health Nurs. 2005, 22, 515–522. [Google Scholar] [CrossRef]
- Mota, J.; Santos, R.M.; Silva, P.; Aires, L.; Martins, C.; Vale, S. Associations between self-rated health with cardiorespiratory fitness and obesity status among adolescent girls. J. Phys. Act. Health 2012, 9, 378–381. [Google Scholar] [CrossRef]
- Qorbani, M.; Heidari-Beni, M.; Ejtahed, H.-S.; Shafiee, G.; Goodarzi, F.; Tamehri Zadeh, S.S.; Khademian, M.; Mohammadian Khonsari, N.; Motlagh, M.E.; Asayesh, H. Association of vitamin D status and cardio-metabolic risk factors in children and adolescents: The CASPIAN-V study. BMC Nutr. 2021, 7, 71. [Google Scholar] [CrossRef]
- Durá-Travé, T.; Gallinas-Victoriano, F.; Peñafiel-Freire, D.M.; Urretavizcaya-Martinez, M.; Moreno-González, P.; Chueca-Guindulain, M.J. Hypovitaminosis D and cardiometabolic risk factors in adolescents with severe obesity. Children 2020, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Fleury, N.; Geldenhuys, S.; Gorman, S. Sun exposure and its effects on human health: Mechanisms through which sun exposure could reduce the risk of developing obesity and cardiometabolic dysfunction. Int. J. Environ. Res. Public Health 2016, 13, 999. [Google Scholar] [CrossRef] [PubMed]
- Heshmat, R.; Qorbani, M.; Shahr Babaki, A.E.; Djalalinia, S.; Ataei-Jafari, A.; Motlagh, M.E.; Ardalan, G.; Arefirad, T.; Rezaei, F.; Asayesh, H. Joint association of screen time and physical activity with cardiometabolic risk factors in a national sample of Iranian adolescents: The CASPIANIII study. PLoS ONE 2016, 11, e0154502. [Google Scholar] [CrossRef]
- Cureau, F.; Ekelund, U.; Bloch, K.; Schaan, B. Does body mass index modify the association between physical activity and screen time with cardiometabolic risk factors in adolescents? Findings from a country-wide survey. Int. J. Obes. 2017, 41, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Carson, V.; Janssen, I. Volume, patterns, and types of sedentary behavior and cardio-metabolic health in children and adolescents: A cross-sectional study. BMC Public Health 2011, 11, 274. [Google Scholar] [CrossRef]
- Ceballos, F.C.; Hazelhurst, S.; Clark, D.W.; Agongo, G.; Asiki, G.; Boua, P.R.; Xavier Gómez-Olivé, F.; Mashinya, F.; Norris, S.; Wilson, J.F. Autozygosity influences cardiometabolic disease-associated traits in the AWI-Gen sub-Saharan African study. Nat. Commun. 2020, 11, 5754. [Google Scholar] [CrossRef]
- Bhasin, P.; Kapoor, S. Impact of consanguinity on cardio-metabolic health and other diseases: Findings from an Afro-Indian tribal community. J. Community Genet. 2015, 6, 129–135. [Google Scholar] [CrossRef]
- Azemati, B.; Kelishadi, R.; Ahadi, Z.; Shafiee, G.; Taheri, M.; Ziaodini, H.; Qorbani, M.; Heshmat, R. Association between junk food consumption and cardiometabolic risk factors in a national sample of Iranian children and adolescents population: The CASPIAN-V study. Eat. Weight. Disord. EWD 2020, 25, 329–335. [Google Scholar] [CrossRef]
- Rocha, N.P.; Milagres, L.C.; Longo, G.Z.; Ribeiro, A.Q.; Novaes, J.F. Association between dietary pattern and cardiometabolic risk in children and adolescents: A systematic review. J. Pediatr. 2017, 93, 214–222. [Google Scholar] [CrossRef]
- Asghari, G.; Yuzbashian, E.; Mirmiran, P.; Mahmoodi, B.; Azizi, F. Fast Food Intake Increases the Incidence of Metabolic Syndrome in Children and Adolescents: Tehran Lipid and Glucose Study. PLoS ONE 2015, 10, e0139641. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V.; Lehmkuhl, E.; Mahmoodzadeh, S. Gender Aspects of the Role of the Metabolic Syndrome as a Risk Factor for Cardiovascular Disease. Gend. Med. 2007, 4 (Suppl. B), S162–S177. [Google Scholar] [CrossRef] [PubMed]
- Barstad, L.H.; Júlíusson, P.B.; Johnson, L.K.; Hertel, J.K.; Lekhal, S.; Hjelmesæth, J. Gender-related differences in cardiometabolic risk factors and lifestyle behaviors in treatment-seeking adolescents with severe obesity. BMC Pediatr. 2018, 18, 61. [Google Scholar] [CrossRef] [PubMed]
- Pucci, G.; Alcidi, R.; Tap, L.; Battista, F.; Mattace-Raso, F.; Schillaci, G. Sex- and gender-related prevalence, cardiovascular risk and therapeutic approach in metabolic syndrome: A review of the literature. Pharmacol. Res. 2017, 120, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Aljahdali, A.A.; Peterson, K.E.; Cantoral, A.; Ruiz-Narvaez, E.; Tellez-Rojo, M.M.; Kim, H.M.; Hébert, J.R.; Wirth, M.D.; Torres-Olascoaga, L.A.; Shivappa, N.; et al. Diet Quality Scores and Cardiometabolic Risk Factors in Mexican Children and Adolescents: A Longitudinal Analysis. Nutrients 2022, 14, 896. [Google Scholar] [CrossRef]
- Funtikova, A.N.; Navarro, E.; Bawaked, R.A.; Fíto, M.; Schröder, H. Impact of diet on cardiometabolic health in children and adolescents. Nutr. J. 2015, 14, 118. [Google Scholar] [CrossRef]
- Aekplakorn, W.; Kessomboon, P.; Sangthong, R.; Chariyalertsak, S.; Putwatana, P.; Inthawong, R.; Nitiyanant, W.; Taneepanichskul, S.; The NHES IV Study Group. Urban and rural variation in clustering of metabolic syndrome components in the Thai population: Results from the fourth National Health Examination Survey 2009. BMC Public Health 2011, 11, 854. [Google Scholar] [CrossRef]
- Johnson III, J.A.; Johnson, A.M. Urban-rural differences in childhood and adolescent obesity in the United States: A systematic review and meta-analysis. Child. Obes. 2015, 11, 233–241. [Google Scholar] [CrossRef]
- Nowicki, G.J.; Ślusarska, B.; Naylor, K.; Prystupa, A.; Rudnicka-Drożak, E.; Halyuk, U.; Pokotylo, P. The relationship between the metabolic syndrome and the place of residence in the local community on the example of the janów lubelski district in eastern Poland: A population-based study. Diabetes Metab. Syndr. Obes. 2021, 14, 2041–2056. [Google Scholar] [CrossRef]
- Schwab, U.; Lauritzen, L.; Tholstrup, T.; Haldorsson, T.I.; Riserus, U.; Uusitupa, M.; Becker, W. Effect of the amount and type of dietary fat on cardiometabolic risk factors and risk of developing type 2 diabetes, cardiovascular diseases, and cancer: A systematic review. Food Nutr. Res. 2014, 58, 25145. [Google Scholar] [CrossRef]
- Morenga, L.T.; Montez, J.M. Health effects of saturated and trans-fatty acid intake in children and adolescents: Systematic review and meta-analysis. PLoS ONE 2017, 12, e0186672. [Google Scholar] [CrossRef]
- Micha, R.; Mozaffarian, D. Saturated fat and cardiometabolic risk factors, coronary heart disease, stroke, and diabetes: A fresh look at the evidence. Lipids 2010, 45, 893–905. [Google Scholar] [CrossRef] [PubMed]
- Jelenkovic, A.; Silventoinen, K.; Tynelius, P.; Myrskylä, M.; Rasmussen, F. Association of birth order with cardiovascular disease risk factors in young adulthood: A study of one million Swedish men. PLoS ONE 2013, 8, e63361. [Google Scholar] [CrossRef] [PubMed]
- Aurpibul, L.; Butler, É.M.; Wongthanee, A.; Rerkasem, A.; Pruenglampoo, S.; Mangklabruks, A.; Rerkasem, K.; Derraik, J.G. Birth order is associated with an increased risk of obesity in young adults in Thailand. J. Epidemiol. Community Health 2021, 75, 305–308. [Google Scholar] [CrossRef] [PubMed]
- Ponzo, V.; Pellegrini, M.; Costelli, P.; Vázquez-Araújo, L.; Gayoso, L.; D’Eusebio, C.; Ghigo, E.; Bo, S. Strategies for reducing salt and sugar intakes in individuals at increased cardiometabolic risk. Nutrients 2021, 13, 279. [Google Scholar] [CrossRef] [PubMed]
- Tragomalou, A.; Moschonis, G.; Manios, Y.; Kassari, P.; Ioakimidis, I.; Diou, C.; Stefanopoulos, L.; Lekka, E.; Maglaveras, N.; Delopoulos, A. Novel e-health applications for the management of cardiometabolic risk factors in children and adolescents in Greece. Nutrients 2020, 12, 1380. [Google Scholar] [CrossRef]
- Anjana, R.M.; Lakshminarayanan, S.; Deepa, M.; Farooq, S.; Pradeepa, R.; Mohan, V. Parental history of type 2 diabetes mellitus, metabolic syndrome, and cardiometabolic risk factors in Asian Indian adolescents. Metabolism 2009, 58, 344–350. [Google Scholar] [CrossRef]
- Li, C.; Ford, E.S.; Zhao, G.; Mokdad, A.H. Prevalence of pre-diabetes and its association with clustering of cardiometabolic risk factors and hyperinsulinemia among U.S. adolescents: National Health and Nutrition Examination Survey 2005–2006. Diabetes Care 2009, 32, 342–347. [Google Scholar] [CrossRef]
- Ejtahed, H.-S.; Heshmat, R.; Motlagh, M.E.; Hasani-Ranjbar, S.; Ziaodini, H.; Taheri, M.; Ahadi, Z.; Aminaee, T.; Shafiee, G.; Goodarzi, A. Association of parental obesity with cardiometabolic risk factors in their children: The CASPIAN-V study. PLoS ONE 2018, 13, e0193978. [Google Scholar] [CrossRef]
- Kelishadi, R.; Mirmoghtadaee, P.; Qorbani, M.; Motlagh, M.E.; Heshmat, R.; Taslimi, M.; Mahmoudarabi, M.; Ardalan, G.; Larijani, B. Tooth brushing and cardiometabolic risk factors in adolescents: Is there an association? The CASPIAN-III study. Int. J. Prev. Med. 2013, 4, 271. [Google Scholar]
- Tanaka, A.; Takeuchi, K.; Furuta, M.; Takeshita, T.; Suma, S.; Shinagawa, T.; Shimazaki, Y.; Yamashita, Y. Relationship of toothbrushing to metabolic syndrome in middle-aged adults. J. Clin. Periodontol. 2018, 45, 538–547. [Google Scholar] [CrossRef]
- Baskaradoss, J.K.; Tavares, M.; Al-Mulla, F.; Al-Ozairi, E.; Abu-Farha, M.; Bin-Hasan, S.; Alsumait, A.; Devarajan, S.; Alqaderi, H. Association between Frequency of Toothbrushing and Metabolic Syndrome among Adolescents: A 5-Year Follow-Up Study. Int. J. Environ. Res. Public Health 2022, 19, 508. [Google Scholar] [CrossRef]
- Ellis, P.D. The Essential Guide to Effect Sizes: Statistical Power, Meta-Analysis, and the Interpretation of Research Results; Cambridge University Press: Cambridge, UK, 2010. [Google Scholar]
- Colquhoun, D. An investigation of the false discovery rate and the misinterpretation of p-values. R. Soc. Open Sci. 2014, 1, 140216. [Google Scholar] [CrossRef]
- Guilherme, H.O.; Nesbitt, G.C.; Murphy, J.G.; Habermann, T.M. Mayo Clinic Medical Manual and Mayo Clinic Internal Medicine Review; CRC Press: Boca Raton, FL, USA, 2007. [Google Scholar]
- Ghosh, A.K. Mayo Clinic Internal Medicine Review, 8th ed.; mcGraw-Hill: New York, NY, USA, 2008; 1101p, ISBN 978-1420084788. [Google Scholar]
| Item | Type | Description |
|---|---|---|
| 1 | Q | Oral hygiene behavior [26]: How many times per day do you brush your teeth? |
| A | (1) once daily, (2) twice daily, (3) three times a day, (4) four times and more a day, and (5) never | |
| 2 | Q | The number of close friends [26] |
| A | (1) none, (2) one friend, (3) two friends, and (4) three or more friends | |
| 3, 4 | Q | Father’s education; Mother’s education |
| A | (1) illiterate, (2) Quranic Literacy, (3) primary, (4) intermediate, (5) diploma, (6) Bachelor, (7) upper than bachelor, (8) died | |
| 5 | Q | Number of family members |
| A | Count variable | |
| 6 | Q | Consanguineous marriage [27] |
| A | (1) no, (2) yes | |
| 7 | Q | Birth order [28] |
| A | Count variable | |
| 8 | Q | Birthweight category [29] |
| A | (1) <2500 g, (2) 2500–400 g, (3) >4000 g | |
| 9 | Q | Breastfeeding [30]: How many months did breastfeeding occur in the first two years after birth? |
| A | Count variable | |
| 10–14 | Q | Family history of hypertension [31]; Family history of dyslipidemia [32]; Family history of diabetes [33]; Family history of obesity [34]; Family history of cancer |
| A | (1) no, (2) yes | |
| 15 | Q | Residence [34] |
| A | (1) urban, (2) rural | |
| 16 | Q | Age group |
| A | 7–10, B. 11–14- and C. 15–18-year-old | |
| 17 | Q | Gender [35] |
| A | (1) male, (2) female | |
| 18 | Q | Self-rated health [36]: How would you describe your general state of health? |
| A | (1) perfect, (2) good, (3) bad, and (4) very bad | |
| 19 | Q | Discretionary salt |
| A | (1) always, (2) sometimes, (3) rarely, and (4) no | |
| 20 | Q | Dietary fat type [37] |
| A | Saturated fats, (2) trans fats, (3) monounsaturated fats, and (4) polyunsaturated fats. |
| Item | Type | Description |
|---|---|---|
| 21 | V | Healthy diet |
| Q | Five questions: Diet beverage, fresh fruit, dried fruit, fresh fruit juice, and fresh/boiled vegetable consumption | |
| A | “Daily”, “weekly”, “rarely”, and “never” | |
| C | The answers were summed up, and the tertiles were calculated, resulting in a three-category ordinal variable (“low”, “moderate”, and “high”). | |
| 22 | V | Unhealthy diet |
| Q | Six questions: Sweets, fast food, soda, junk food, sugar-sweetened fruit juice, and discretionary sugar consumption | |
| A | “Daily,” “weekly”, “rarely”, and “never” | |
| C | The answers were summed up, and the tertiles were calculated, resulting in a three-category ordinal variable (“low”, “moderate”, and “high”). | |
| 23 | V | Screen time |
| Q | Six questions: Q1, Q2: How many hours a day do you watch TV (on weekdays/weekends)? Q3, Q4: How many hours a day do you do your class exercises (on weekdays/weekends)? Q5, Q6: How many hours a day do you use a computer (on weekdays/weekends)? | |
| A | (1) never, (2) 1 h, (3) 2 h, (4) 3 h, and (5) four or more hours. | |
| C | The answers to the questions were summed up, and the cut-off of 10 was used to create a dichotomous variable (<10: No, ≥10: Yes). The optimal” cut-point was calculated to minimize the error rate (ER) criteria [38] in CMR ROC Analysis. | |
| 24 | V | Sunlight exposure [39] |
| Q | Four questions: Q1, Q2: How much exposure to outdoor sunlight (on weekdays/weekends)? Q3: What parts of the body are exposed to sunlight during sunlight exposure? Q4: Do you use sunscreen creams? | |
| A | Q1, Q2: (1) less than 5 min, (2) between 5 and 30 min, and (3) more than 30 min Q3: (1) hands, face, legs, (2) hands, face, arms, and (3) hands, face Q4: (1) never, (2) sometimes, and (3) always | |
| C | Using Principal Component Analysis (PCA) [11], the primary principal component was extracted from the responses to the questions. Subjects were subsequently classified into “low”, “medium”, and “high” sunlight exposure groups according to the tertiles of the principal component. |
| Characteristics | Non-CMS (N = 1169) | CMS (N = 5663) | Overall (N = 6832) | p-Value |
|---|---|---|---|---|
| Number of close friends | ||||
| None | 54 (4.6%) | 240 (4.2%) | 294 (4.3%) | 0.3932 |
| One friend | 212 (18.1%) | 934 (16.5%) | 1146 (16.8%) | |
| Two friends | 333 (28.5%) | 1594 (28.1%) | 1927 (28.2%) | |
| Three or more friends | 570 (48.8%) | 2895 (51.1%) | 3465 (50.7%) | |
| Oral hygiene behavior | ||||
| Never | 47 (4.0%) | 225 (4.0%) | 272 (4.0%) | 0.6016 |
| Less than once a week | 52 (4.4%) | 204 (3.6%) | 256 (3.7%) | |
| At least once a week | 124 (10.6%) | 666 (11.8%) | 790 (11.6%) | |
| Only once a week | 62 (5.3%) | 289 (5.1%) | 351 (5.1%) | |
| Once a day | 626 (53.6%) | 2974 (52.5%) | 3600 (52.7%) | |
| More than once a day | 258 (22.1%) | 1305 (23.0%) | 1563 (22.9%) | |
| Self-rated health | ||||
| Average | 241 (20.6%) | 1023 (18.1%) | 1264 (18.5%) | 0.0640 |
| Bad | 4 (0.3%) | 46 (0.8%) | 50 (0.7%) | |
| Good | 428 (36.6%) | 2075 (36.6%) | 2503 (36.6%) | |
| Perfect | 496 (42.4%) | 2519 (44.5%) | 3015 (44.2%) | |
| Age group | ||||
| 7–10 y | 396 (33.9%) | 1737 (30.7%) | 2133 (31.2%) | 0.0107 |
| 11–14 y | 505 (43.2%) | 2404 (42.5%) | 2909 (42.6%) | |
| 15–18 y | 268 (22.9%) | 1522 (26.9%) | 1790 (26.2%) | |
| Residence | ||||
| Rural | 360 (30.8%) | 1366 (24.1%) | 1726 (25.3%) | <0.001 |
| Urban | 809 (69.2%) | 4297 (75.9%) | 5106 (74.7%) | |
| Number of family members | ||||
| Mean (SD) | 4.91 (1.54) | 4.81 (1.47) | 4.83 (1.48) | 0.0631 |
| Median [Min, Max] | 5.00 [1.00, 17.0] | 5.00 [0, 15.0] | 5.00 [0, 17.0] | |
| Father education | ||||
| Upper than bachelor | 53 (4.6%) | 280 (5.0%) | 333 (4.9%) | 0.0413 |
| Bachelor | 104 (8.9%) | 586 (10.3%) | 690 (10.1%) | |
| Diploma | 264 (22.6%) | 1398 (24.7%) | 1662 (24.3%) | |
| Intermediate | 290 (24.8%) | 1366 (24.1%) | 1656 (24.2%) | |
| Primary | 264 (22.6%) | 1240 (21.9%) | 1504 (22.0%) | |
| Quranic Literacy | 17 (1.5%) | 55 (1.0%) | 72 (1.1%) | |
| Illiterate | 158 (13.5%) | 612 (10.8%) | 770 (11.3%) | |
| Father died | 19 (1.6%) | 126 (2.2%) | 145 (2.1%) | |
| Mother education | ||||
| Upper than bachelor | 15 (1.3%) | 91 (1.6%) | 106 (1.6%) | 0.3919 |
| Bachelor | 106 (9.1%) | 577 (10.2%) | 683 (10.0%) | |
| Diploma | 291 (24.9%) | 1504 (26.6%) | 1795 (26.3%) | |
| Intermediate | 254 (21.7%) | 1135 (20.0%) | 1389 (20.3%) | |
| Primary | 281 (24.0%) | 1398 (24.7%) | 1679 (24.6%) | |
| Quranic Literacy | 13 (1.1%) | 57 (1.0%) | 70 (1.0%) | |
| Illiterate | 205 (17.5%) | 876 (15.5%) | 1081 (15.8%) | |
| Mother died | 4 (0.3%) | 25 (0.4%) | 29 (0.4%) | |
| Consanguinity | ||||
| No | 651 (55.7%) | 3068 (54.2%) | 3719 (54.4%) | 0.3612 |
| Yes | 518 (44.3%) | 2595 (45.8%) | 3113 (45.6%) | |
| Birth order | ||||
| Mean (SD) | 2.27 (1.59) | 2.17 (1.49) | 2.19 (1.51) | 0.0485 |
| Median [Min, Max] | 2.00 [0, 11.0] | 2.00 [0, 11.0] | 2.00 [0, 11.0] | |
| Birthweight category | ||||
| 2500–4000 g | 859 (73.5%) | 4233 (74.7%) | 5092 (74.5%) | 0.2791 |
| Less than 2500 g | 122 (10.4%) | 507 (9.0%) | 629 (9.2%) | |
| More than 4000 g | 188(16.1%) | 923 (16.3%) | 1111 (16.3%) | |
| Breastfeeding | ||||
| Mean (SD) | 15.0 (8.52) | 15.1 (8.52) | 15.1 (8.52) | 0.735 |
| Median [Min, Max] | 18.0 [0, 24.0] | 18.0 [0, 24.0] | 18.0 [0, 24.0] | |
| Discretionary salt | ||||
| Always | 237 (20.3%) | 1268 (22.4%) | 1505 (22.0%) | 0.0154 |
| Sometimes | 255 (21.8%) | 1131 (20.0%) | 1386 (20.3%) | |
| Rarely | 116 (9.9%) | 705 (12.4%) | 821 (12.0%) | |
| No | 561 (48.0%) | 2559 (45.2%) | 3120 (45.7%) | |
| Family history of hypertension | ||||
| No | 452 (38.7%) | 2178 (38.5%) | 2630 (38.5%) | 0.9216 |
| Yes | 717 (61.3%) | 3485 (61.5%) | 4202 (61.5%) | |
| Family history of dyslipidemia | ||||
| No | 587 (50.2%) | 2846 (50.3%) | 3433 (50.2%) | 1.0000 |
| Yes | 582 (49.8%) | 2817 (49.7%) | 3399 (49.8%) | |
| Family history of diabetes | ||||
| No | 552 (47.2%) | 2752 (48.6%) | 3304 (48.4%) | 0.4093 |
| Yes | 617 (52.8%) | 2911 (51.4%) | 3528 (51.6%) | |
| Family history of obesity | ||||
| No | 635 (54.3%) | 2879 (50.8%) | 3514 (51.4%) | 0.0327 |
| Yes | 534 (45.7%) | 2784 (49.2%) | 3318 (48.6%) | |
| Family history of cancer | ||||
| No | 944 (80.8%) | 4552 (80.4%) | 5496 (80.4%) | 0.8018 |
| Yes | 225 (19.2%) | 1111 (19.6%) | 1336 (19.6%) | |
| Dietary fat type | ||||
| Monounsaturated fats | 478 (40.9%) | 2109 (37.2%) | 2587 (37.8%) | 0.0362 |
| Polyunsaturated fats | 181 (15.5%) | 1041 (18.4%) | 1222 (17.9%) | |
| Saturated fats | 429 (36.7%) | 2083 (36.8%) | 2512 (36.8%) | |
| Trans fats | 81 (6.9%) | 430 (7.6%) | 511 (7.5%) | |
| Gender | ||||
| Female | 602 (51.5%) | 2719 (48.0%) | 3321 (48.6%) | 0.0326 |
| Male | 567 (48.5%) | 2944 (52.0%) | 3511 (51.4%) | |
| Diet beverage consumption | ||||
| Daily | 7 (0.6%) | 46 (0.8%) | 53 (0.8%) | 0.2754 |
| Weekly | 49 (4.2%) | 275 (4.9%) | 324 (4.7%) | |
| Rarely | 210 (18.0%) | 1116 (19.7%) | 1326 (19.4%) | |
| Never | 903 (77.2%) | 4226 (74.6%) | 5129 (75.1%) | |
| Fresh fruit consumption | ||||
| Daily | 666 (57.0%) | 2928 (51.7%) | 3594 (52.6%) | 0.0101 |
| Weekly | 386 (33.0%) | 2118 (37.4%) | 2504 (37.6%) | |
| Rarely | 80 (6.8%) | 441 (7.8%) | 521 (7.6%) | |
| Never | 37 (3.2%) | 176 (3.1%) | 213 (3.1%) | |
| Dried fruit consumption | ||||
| Daily | 400 (34.2%) | 1804 (31.9%) | 2204 (32.3%) | 0.0354 |
| Weekly | 477 (40.8%) | 2410 (42.6%) | 2887 (42.3%) | |
| Rarely | 209 (17.9%) | 1134 (20.0%) | 1343 (19.7%) | |
| Never | 83 (7.1%) | 315 (5.6%) | 398 (5.8%) | |
| Fresh fruit juice consumption | ||||
| Daily | 196 (16.8%) | 971 (17.1%) | 1167 (17.1%) | 0.1903 |
| Weekly | 390 (33.3%) | 2001 (35.3%) | 2391 (35.0%) | |
| Rarely | 478 (40.9%) | 2276 (40.2%) | 2754 (40.3%) | |
| Never | 105 (9.0%) | 415 (7.3%) | 520 (7.6%) | |
| Fresh or boiled vegetable consumption | ||||
| Daily | 347 (29.7%) | 1899 (33.5%) | 2246 (32.9%) | 0.0511 |
| Weekly | 595 (50.9%) | 2652 (46.8%) | 3247 (47.5%) | |
| Rarely | 158 (13.5%) | 774 (13.7%) | 932 (13.6%) | |
| Never | 69 (5.9%) | 338 (6.0%) | 407 (6.0%) | |
| Sweets consumption | ||||
| Daily | 286 (24.5%) | 1409 (24.9%) | 1695 (24.8%) | 0.0143 |
| Weekly | 520 (44.5%) | 2597 (45.8%) | 3117 (45.6%) | |
| Rarely | 352 (30.1%) | 1537 (27.1%) | 1889 (27.6%) | |
| Never | 11 (0.9%) | 120 (2.1%) | 131 (1.9%) | |
| Fast food consumption | ||||
| Daily | 61 (5.2%) | 439 (7.8%) | 500 (7.3%) | 0.0014 |
| Weekly | 355 (30.4%) | 1510 (26.7%) | 1865 (27.3%) | |
| Rarely | 600 (51.3%) | 3042 (53.7%) | 3642 (53.3%) | |
| Never | 153 (13.1%) | 672 (11.9%) | 825 (12.1%) | |
| Soda consumption | ||||
| Daily | 23 (2.0%) | 212 (3.7%) | 235 (3.4%) | 0.0105 |
| Weekly | 276 (23.6%) | 1237 (21.8%) | 1513 (22.1%) | |
| Rarely | 627 (53.6%) | 3106 (54.8%) | 3733 (54.6%) | |
| Never | 243 (20.8%) | 1108 (19.6%) | 1351 (19.8%) | |
| Junk food consumption | ||||
| Daily | 16 (1.4%) | 126 (2.2%) | 142 (2.1%) | 0.0273 |
| Weekly | 179 (15.3%) | 908 (16.0%) | 1087 (15.9%) | |
| Rarely | 718 (61.4%) | 3568 (63.0%) | 4286 (62.7%) | |
| Never | 256 (21.9%) | 1061 (18.7%) | 1317 (19.3%) | |
| Sugar sweetened fruit juice consumption | ||||
| Daily | 72 (6.2%) | 373 (6.6%) | 445 (6.5%) | 0.2753 |
| Weekly | 246 (21.0%) | 1306 (23.1%) | 1552 (22.7%) | |
| Rarely | 665 (56.9%) | 3049 (53.8%) | 3714 (54.4%) | |
| Never | 186 (15.9%) | 935 (16.5%) | 1121 (16.4%) | |
| Discretionary sugar consumption | ||||
| Daily | 566 (48.4%) | 2766 (48.8%) | 3332 (48.8%) | 0.1030 |
| Weekly | 240 (20.5%) | 1195 (21.1%) | 1435 (21.0%) | |
| Rarely | 254 (21.7%) | 1080 (19.1%) | 1334 (19.5%) | |
| Never | 109 (9.3%) | 622 (11.0%) | 731 (10.7%) | |
| Screen time Q1 | ||||
| Never | 46 (3.9%) | 242 (4.3%) | 288 (4.2%) | 0.7006 |
| 1 h | 467 (39.9%) | 2278 (40.2%) | 2745 (40.2%) | |
| 2 h | 355 (30.4%) | 1626 (28.7%) | 1981 (29.0%) | |
| 3 h | 200 (17.1%) | 972 (17.2%) | 1172 (17.2%) | |
| 4 h or more | 101 (8.6%) | 545 (9.6%) | 646 (9.5%) | |
| Screen time Q2 | ||||
| Never | 32 (2.8%) | 190 (3.4%) | 222 (3.3%) | 0.4569 |
| 1 h | 239 (20.4%) | 1190 (21.0%) | 1429 (20.9%) | |
| 2 h | 382 (32.7%) | 1709 (30.2%) | 2091 (30.6%) | |
| 3 h | 313 (26.8%) | 1566 (27.7%) | 1879 (27.5%) | |
| 4 h or more | 203 (17.4%) | 1008 (17.8%) | 1211 (17.7%) | |
| Screen time Q3 | ||||
| Never | 4 (0.4%) | 22 (0.4%) | 26 (0.4%) | 0.8998 |
| 1 h | 395 (33.8%) | 1933 (34.1%) | 2328 (34.1%) | |
| 2 h | 289 (24.7%) | 1434 (25.3%) | 1723 (25.2%) | |
| 3 h | 216 (18.5%) | 1065 (18.8%) | 1281 (18.8%) | |
| 4 h or more | 265 (22.7%) | 1209 (21.3%) | 1474 (21.6%) | |
| Screen time Q4 | ||||
| Never | 37 (3.2%) | 221 (3.9%) | 258 (3.8%) | 0.2376 |
| 1 h | 218 (18.6%) | 1046 (18.5%) | 1264 (18.5%) | |
| 2 h | 322 (27.5%) | 1681 (29.7%) | 2003 (29.3%) | |
| 3 h | 335 (28.7%) | 1472 (26.0%) | 1807 (26.4%) | |
| 4 h or more | 257 (22.0%) | 1243 (21.9%) | 1500 (22.0%) | |
| Screen time Q5 | ||||
| Never | 765 (65.4%) | 3513 (62.0%) | 4278 (62.6%) | 0.1565 |
| 1 h | 307 (26.3%) | 1571 (27.7%) | 1878 (27.5%) | |
| 2 h | 70 (6.0%) | 407 (7.2%) | 477 (7.0%) | |
| 3 h | 14 (1.2%) | 100 (1.8%) | 114 (1.7%) | |
| 4 h or more | 13 (1.1%) | 72 (1.3%) | 85 (1.2%) | |
| Screen time Q6 | ||||
| Never | 604 (51.6%) | 2728 (48.2%) | 3332 (48.7%) | 0.0789 |
| 1 h | 314 (26.9%) | 1685 (29.8%) | 1999 (29.3%) | |
| 2 h | 149 (12.7%) | 690 (12.2%) | 839 (12.3%) | |
| 3 h | 71 (6.1%) | 352 (6.2%) | 423 (6.2%) | |
| 4 h or more | 31 (2.7%) | 208 (3.7%) | 239 (3.5%) | |
| Sunlight exposure Q1 | ||||
| Less than 5 min | 167 (14.3%) | 898 (15.9%) | 1065 (15.6%) | 0.0959 |
| 5–30 min | 534 (45.7%) | 2400 (42.4%) | 2934 (42.9%) | |
| More than 30 min | 468 (40.0%) | 2365 (41.8%) | 2833 (41.4%) | |
| Sunlight exposure Q2 | ||||
| Less than 5 min | 214 (18.3%) | 1039 (18.3%) | 1253 (18.3%) | 0.4220 |
| 5–30 min | 315 (26.9%) | 1628 (28.7%) | 1943 (28.4%) | |
| More than 30 min | 640 (54.7%) | 2996 (52.9%) | 3636 (53.2%) | |
| Sunlight exposure Q3 | ||||
| Hands, face, legs | 231 (19.8%) | 1034 (18.3%) | 1265 (18.5%) | 0.3374 |
| Hands, face | 864 (73.9%) | 4224 (74.6%) | 5088 (74.5%) | |
| Hands, face, arms | 74 (6.3%) | 405 (7.1%) | 479 (7.0%) | |
| Sunlight exposure Q4 | ||||
| Never | 486 (41.6%) | 2225 (39.3%) | 2711 (39.7%) | 0.1542 |
| Sometimes | 530 (45.4%) | 2588 (45.7%) | 3130 (45.7%) | |
| Always | 153 (13.1%) | 850 (15.0%) | 1003 (14.7%) |
| Test Folds | Cross-Validated Results | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Metric | Fold 1 | Fold 2 | Fold 3 | Fold 4 | Fold 5 | Mean | SD | Value | 95% CI Lower | 95% CI Upper |
| Sensitivity | 0.867 0.554 | 0.967 0.541 | 0.972 0.549 | 0.976 0.552 | 0.958 0.537 | 0.947 0.547 | 0.048 0.007 | 0.947 0.547 | 0.941 0.535 | 0.953 0.558 |
| Specificity | 0.600 0.897 | 0.700 0.915 | 0.845 0.872 | 0.854 0.910 | 0.940 0.876 | 0.788 0.894 | 0.137 0.017 | 0.787 0.894 | 0.764 0.887 | 0.811 0.901 |
| PPV | 0.910 0.963 | 0.939 0.968 | 0.968 0.954 | 0.970 0.967 | 0.987 0.954 | 0.955 0.961 | 0.030 0.006 | 0.955 0.961 | 0.950 0.957 | 0.961 0.966 |
| NPV | 0.480 0.294 | 0.815 0.292 | 0.864 0.286 | 0.881 0.296 | 0.823 0.282 | 0.772 0.290 | 0.167 0.005 | 0.757 0.290 | 0.733 0.279 | 0.781 0.301 |
| LR+ | 2.150 5.400 | 3.218 6.330 | 6.292 4.280 | 6.687 6.130 | 15.939 4.330 | 6.857 5.290 | 5.437 0.864 | 4.452 5.150 | 3.986 4.530 | 4.973 6.060 |
| LR- | 0.230 0.497 | 0.048 0.502 | 0.033 0.518 | 0.028 0.492 | 0.045 0.529 | 0.077 0.507 | 0.086 0.014 | 0.067 0.507 | 0.060 0.496 | 0.076 0.520 |
| Kappa | 0.420 0.249 | 0.706 0.247 | 0.825 0.232 | 0.840 0.253 | 0.850 0.225 | 0.728 0.241 | 0.182 0.011 | 0.723 0.241 | 0.700 0.231 | 0.745 0.250 |
| DOR | 9.350 10.87 | 67.717 12.600 | 191.000 8.270 | 235.202 12.450 | 354.461 8.190 | 171.545 10.480 | 136.910 1.930 | 66.102 10.16 | 55.057 8.760 | 79.362 12.200 |
| DP | 0.950 1.013 | 1.789 1.075 | 2.229 0.897 | 2.317 1.070 | 2.491 0.893 | 1.955 0.990 | 0.619 0.081 | 1.779 0.984 | 1.701 0.918 | 1.856 1.061 |
| AUC | 0.730 0.774 | 0.833 0.748 | 0.909 0.730 | 0.915 0.782 | 0.949 0.733 | 0.867 0.753 | 0.087 0.021 | 0.867 0.754 | 0.858 0.743 | 0.876 0.764 |
| MCC | 0.420 0.341 | 0.709 0.344 | 0.825 0.318 | 0.840 0.349 | 0.853 0.312 | 0.730 0.333 | 0.181 0.015 | 0.723 0.333 | 0.711 0.320 | 0.734 0.345 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marateb, H.R.; Mansourian, M.; Koochekian, A.; Shirzadi, M.; Zamani, S.; Mansourian, M.; Mañanas, M.A.; Kelishadi, R. Prevention of Cardiometabolic Syndrome in Children and Adolescents Using Machine Learning and Noninvasive Factors: The CASPIAN-V Study. Information 2024, 15, 564. https://doi.org/10.3390/info15090564
Marateb HR, Mansourian M, Koochekian A, Shirzadi M, Zamani S, Mansourian M, Mañanas MA, Kelishadi R. Prevention of Cardiometabolic Syndrome in Children and Adolescents Using Machine Learning and Noninvasive Factors: The CASPIAN-V Study. Information. 2024; 15(9):564. https://doi.org/10.3390/info15090564
Chicago/Turabian StyleMarateb, Hamid Reza, Mahsa Mansourian, Amirhossein Koochekian, Mehdi Shirzadi, Shadi Zamani, Marjan Mansourian, Miquel Angel Mañanas, and Roya Kelishadi. 2024. "Prevention of Cardiometabolic Syndrome in Children and Adolescents Using Machine Learning and Noninvasive Factors: The CASPIAN-V Study" Information 15, no. 9: 564. https://doi.org/10.3390/info15090564
APA StyleMarateb, H. R., Mansourian, M., Koochekian, A., Shirzadi, M., Zamani, S., Mansourian, M., Mañanas, M. A., & Kelishadi, R. (2024). Prevention of Cardiometabolic Syndrome in Children and Adolescents Using Machine Learning and Noninvasive Factors: The CASPIAN-V Study. Information, 15(9), 564. https://doi.org/10.3390/info15090564










