Personalized Biomechanical Analysis of the Mandible Teeth Behavior in the Treatment of Masticatory Muscles Parafunction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Aspects and Study Design
2.2. Finite Element Model
2.3. Design Options and Loading Conditions
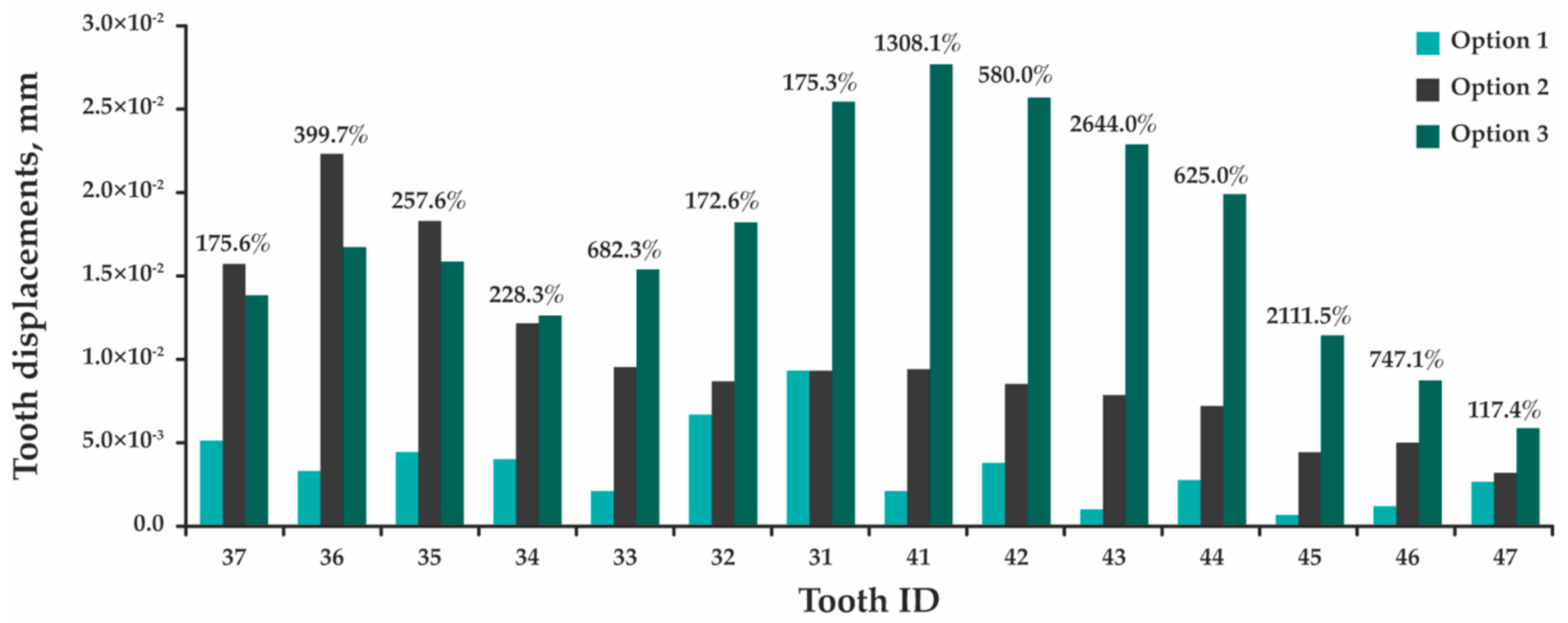
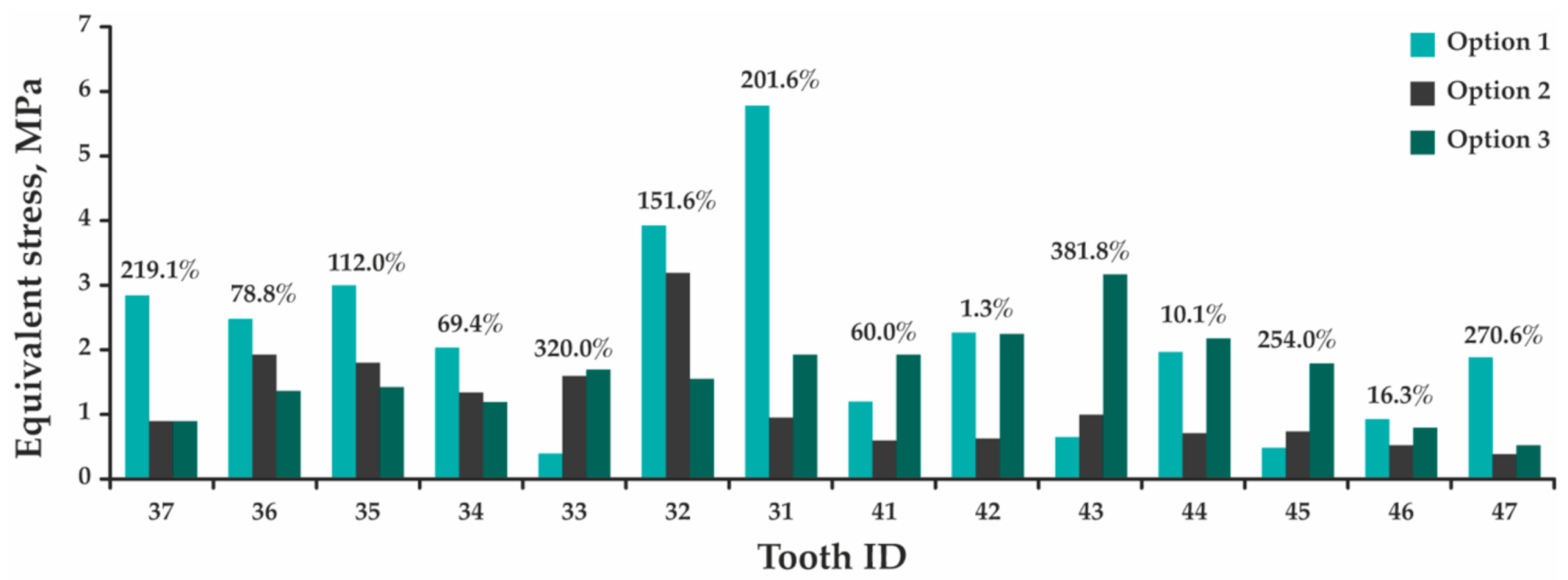
- Option 1: The model of the dentition without the installed splint;
- Option 2: The model of the dentition with a splint installed after production;
- Option 3: The model of the dentition with a splint installed after grinding.
3. Results
4. Discussion
5. Limitation of the Study
6. Conclusions
- The presented technology makes it possible to take into account the individual geometric characteristics of the jaw components (teeth, periodontium, and dentition, in general) of a particular patient when planning dental orthopedic treatment of mastication muscles parafunction.
- The results of the study proved the effectiveness of using the splint in order to change the distribution of functional load in the treatment of patients with mastication muscles parafunction.
- The potential applicability of PMMA as a splint material for the treatment of mastication muscle parafunction has been established. However, additional research is required, taking into account the various loading conditions that arise during the operation of the jaw (biting processes and unilateral chewing).
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moller, E. The chewing apparatus. An electromyographic study of the action of the muscles of mastication and its correlation to facial morphology. Acta Physiol. Scand. Suppl. 1966, 280, 1–229. [Google Scholar] [PubMed]
- Sessle, B.J. Identification of alfa and gamma trigeminal motoneurons and affects of stimulation of amegdala, cerebellum and cerebral cortex. Exp. Neurol. 1999, 54, 303–322. [Google Scholar] [CrossRef]
- Creugers, N.H.; Spijker, A.V. Tooth wear and occlusion: Friends or foes? Int. J. Prosthodont. 2007, 20, 348–350. [Google Scholar]
- Shahidi, S.; Salehi, P.; Abedi, P.; Dehbozorgi, M.; Hamedani, S.; Berahman, N. Comparison of the bony changes of TMJ in patients with and without TMD complaints using CBCT. J. Dent. (Shiraz, Islamic Repub. Iran) 2018, 19, 142–149. [Google Scholar]
- Ono, Y.; Suganuma, T.; Shinya, A.; Furuya, R.; Baba, K. Effects of sleep bruxism on periodontal sensation and tooth displacement in the molar region. Cranio 2008, 26, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Castroflorio, T.; Bargellini, A.; Rossini, G.; Cugliari, G.; Deregibus, A. Sleep bruxism and related risk factors in adults: A systematic literature review. Arch. Oral Biol. 2017, 83, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Silva, A.; Peña-Durán, C.; Tobar-Reyes, J.; Frugone-Zambra, R. Sleep and awake bruxism in adults and its relationship with temporomandibular disorders: A systematic review from 2003 to 2014. Acta Odontol. Scand. 2017, 75, 36–58. [Google Scholar] [CrossRef] [PubMed]
- Toyama, N.; Ekuni, D.; Taniguchi-Tabata, A.; Kataoka, K.; Yamane-Takeuchi, M.; Fujimori, K.; Kobayashi, T.; Fukuhara, D.; Irie, K.; Azuma, T.; et al. Awareness of Clenching and Underweight are Risk Factors for Onset of Crowding in Young Adults: A Prospective 3-Year Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 690. [Google Scholar] [CrossRef] [Green Version]
- De Meyer, M.D.; De Boever, J.A. The role of bruxism in the appearance of temporomandibular joint disorders. Rev. Belge Med. Dent (1984) 1997, 52, 124–138. [Google Scholar]
- Machado, E.; Dal-Fabbro, C.; Cunali, P.A.; Kaizer, O.B. Prevalence of sleep bruxism in children: A systematic review. Dental Press J. Orthod. 2014, 19, 54–61. [Google Scholar] [CrossRef] [Green Version]
- Manfredini, D.; Winocur, E.; Guarda-Nardini, L.; Paesani, D.; Lobbezoo, F. Epidemiology of bruxism in adults: A systematic review of the literature. J. Orofac. Pain 2013, 27, 99–110. [Google Scholar] [CrossRef] [Green Version]
- Gurbuz, O.; Altinbas, K.; Oflezer, C.; Kurt, E.; Arslan, M.D. Signs of bruxism and temporomandibular disorders among patients with bipolar disorder. Balk. J. Dent. Med. 2017, 21, 152–157. [Google Scholar] [CrossRef] [Green Version]
- Winocur, E.; Hermesh, H.; Littner, D.; Shiloh, R.; Peleg, L.; Eli, I. Signs of bruxism and temporomandibular disorders among psychiatric patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, 60–63. [Google Scholar] [CrossRef]
- Castroflorio, T.; Icardi, K.; Torsello, F.; Deregibus, A.; Debernardi, C.; Bracco, P. Reproducibility of surface EMG in the human masseter and anterior temporalis muscle areas. Cranio 2005, 23, 130–137. [Google Scholar] [CrossRef]
- Solberg, W.K.; Clark, G.T.; Rugh, J.D. Nocturnal electromyographic evaluation of bruxism patients undergoing short term splint therapy. J. Oral Rehabil. 1975, 2, 215–223. [Google Scholar] [CrossRef]
- Orskov, L.; Bak, J.F.; Abildgård, N.; Schmitz, O.; Andreasen, F.; Richter, E.A.; Skjaerbaek, C.; Møller, N. Inhibition of muscle glycogen synthase activity and non-oxidative glucose disposal during hypoglycaemia in normal man. Diabetologia 1996, 39, 226–234. [Google Scholar] [CrossRef] [Green Version]
- Voss, T.S.; Vendelbo, M.H.; Kampmann, U.; Pedersen, S.B.; Nielsen, T.S.; Johannsen, M.; Svart, M.V.; Jessen, N.; Møller, N. Effects of insulin-induced hypoglycaemia on lipolysis rate, lipid oxidation and adipose tissue signalling in human volunteers: A randomised clinical study. Diabetologia 2017, 60, 143–152. [Google Scholar] [CrossRef] [Green Version]
- Nukazawa, S.; Yoshimi, H.; Sato, S. Autonomic nervous activities associated with bruxism events during sleep. Cranio 2018, 36, 106–112. [Google Scholar] [CrossRef]
- Sato, S.; Slavicek, R. The masticatory organ and stress management. Stomat. Occ. Med. 2008, 1, 51–57. [Google Scholar] [CrossRef]
- Pavone, B.W. Bruxism and its effect on the natural teeth. J. Prosthet. Dent. 1985, 53, 692–696. [Google Scholar] [CrossRef]
- Riley, P.; Glenny, A.M.; Worthington, H.V.; Jacobsen, E.; Robertson, C.; Durham, J.; Davies, S.; Petersen, H.; Boyers, D. Oral splints for patients with temporomandibular disorders or bruxism: A systematic review and economic evaluation. Health Technol. Assess. 2020, 24, 1–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Moraissi, E.A.; Farea, R.; Qasem, K.A.; Al-Wadeai, M.S.; Al-Sabahi, M.E.; Al-Iryani, G.M. Effectiveness of occlusal splint therapy in the management of temporomandibular disorders: Network meta-analysis of randomized controlled trials. Int. J. Oral Maxillofac. Surg. 2020, 49, 1042–1056. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Baek, H.S.; Song, D.S.; Kim, H.C.; Kim, H.G.; Kim, B.J.; Kim, M.S.; Shin, S.H.; Jung, S.H.; Kim, C.H. Effect of simultaneous therapy of arthrocentesis and occlusal splints on temporomandibular disorders: Anterior disc displacement without reduction. J. Korean Assoc. Oral Maxillofac. Surg. 2013, 39, 14–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nitzan, D.W. Intraarticular pressure in the functioning human temporomandibular joint and its alteration by uniform elevation of the occlusal plane. J. Oral Maxillofac. Surg. 1994, 52, 671–679. [Google Scholar] [CrossRef]
- Tatli, U.; Benlidayi, M.E.; Ekren, O.; Salimov, F. Comparison of the effectiveness of three different treatment methods for temporomandibular joint disc displacement without reduction. Int. J. Oral Maxillofac. Surg. 2017, 46, 603–609. [Google Scholar] [CrossRef]
- Gholampour, S.; Gholampour, H.; Khanmohammadi, H. Finite element analysis of occlusal splint therapy in patients with bruxism. BMC Oral Health 2019, 19, 205. [Google Scholar] [CrossRef] [Green Version]
- Molteni, R. Prospects and challenges of rendering tissue density in Hounsfield units for cone beam computed tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 105–119. [Google Scholar] [CrossRef]
- Gupta, D.K.; Tuli, A.; Jain, A. 3D printed material application in orthodontics. In Proceedings of the International Conference on Aspects of Materials Science and Engineering, Chandigarh, India, 29–30 May 2020; Volume 28, pp. 1635–1642. [Google Scholar] [CrossRef]
- Bhushan, B.; Burton, Z. Adhesion and friction properties of polymers in microfluidic devices. Nanotechnology 2005, 16, 467. [Google Scholar] [CrossRef]
- Gerami, A.; Dadgar, S.; Rakhshan, V.; Jannati, P.; Sobouti, F. Displacement and force distribution of splinted and tilted mandibular anterior teeth under occlusal loads: An in silico 3D finite element analysis. Prog. Orthod. 2016, 17, 16. [Google Scholar] [CrossRef] [Green Version]
- Fill, T.S.; Carey, J.P.; Toogood, R.W.; Major, P.W. Experimentally Determined Mechanical Properties of, and Models for, the Periodontal Ligament: Critical Review of Current Literature. J. Dent Biomech. 2011, 2011, 312980. [Google Scholar] [CrossRef] [Green Version]
- Throckmorton, G.S.; Rasmussen, J.; Carloss, R. Calibration of T-Scan® sensors for recording bite forces in denture patients. J. Oral Rehabil. 2009, 36, 636–643. [Google Scholar] [CrossRef]
- Petersmann, S.; Spoerk, M.; Van De Steene, W.; Üçal, M.; Wiener, J.; Pinter, G.; Arbeiter, F. Mechanical properties of polymeric implant materials produced by extrusion-based additive manufacturing. J. Mech. Behav. Biomed. Mater. 2020, 104, 103611. [Google Scholar] [CrossRef]
- Gribov, D.A.; Krupnin, A.E.; Levchenko, I.M.; Butkov, D.S.; Arutyunov, S.D. Personalized biomechanical analysis of mandible teeth loosening during periodontal treatment with non-removable polymer splints. Ser. Biomech. 2019, 33, 14–26. [Google Scholar]
- Gribov, D.A.; Krupnin, E.A.; Levchenko, I.M.; Butkov, D.S.; Arutyunov, S.D. The effect of various loading scenarios on the stress-strained state of mandible anterior teeth with periodontitis immobilized by splints; finite element analysis. Ser. Biomech. 2020, 34, 12–19. [Google Scholar]
- Natali, A.N.; Pavan, P.G.; Scarpa, C. Numerical analysis of tooth mobility: Formulation of a non-linear constitutive law for the periodontal ligament. Dent. Mater. 2004, 20, 623–629. [Google Scholar] [CrossRef]
- Staninec, M.; Marshall, G.W.; Hilton, J.F.; Pashley, D.H.; Gansky, S.A.; Marshall, S.J.; Kinney, J.H. Ultimate tensile strength of dentin: Evidence for a damage mechanics approach to dentin failure. J. Biomed. Mater. Res. 2002, 63, 342–345. [Google Scholar] [CrossRef]
- Craig, R.G.; Peyton, F.A. Elastic and mechanical properties of human dentin. J. Dent. Res. 1958, 37, 710–718. [Google Scholar] [CrossRef]
- Komatsu, K. Mechanical strength and viscoelastic response of the periodontal ligament in relation to structure. J. Dent. Biomech. 2010, 2010, 502318. [Google Scholar] [CrossRef]
- Huang, A.; Yao, W.; Chen, F. Analysis of fatigue life of PMMA at Different frequencies based on a new damage mechanics model. Math. Probl. Eng. 2014, 2014, 352676. [Google Scholar] [CrossRef]







| Material Name | Young’s Modulus (MPa) | Poisson’s Ratio |
|---|---|---|
| Tooth [30] | 20,300.00 | 0.26 |
| PDL [31] | 68.90 | 0.45 |
| PMMA [28,29] | 2200.00 | 0.35 |
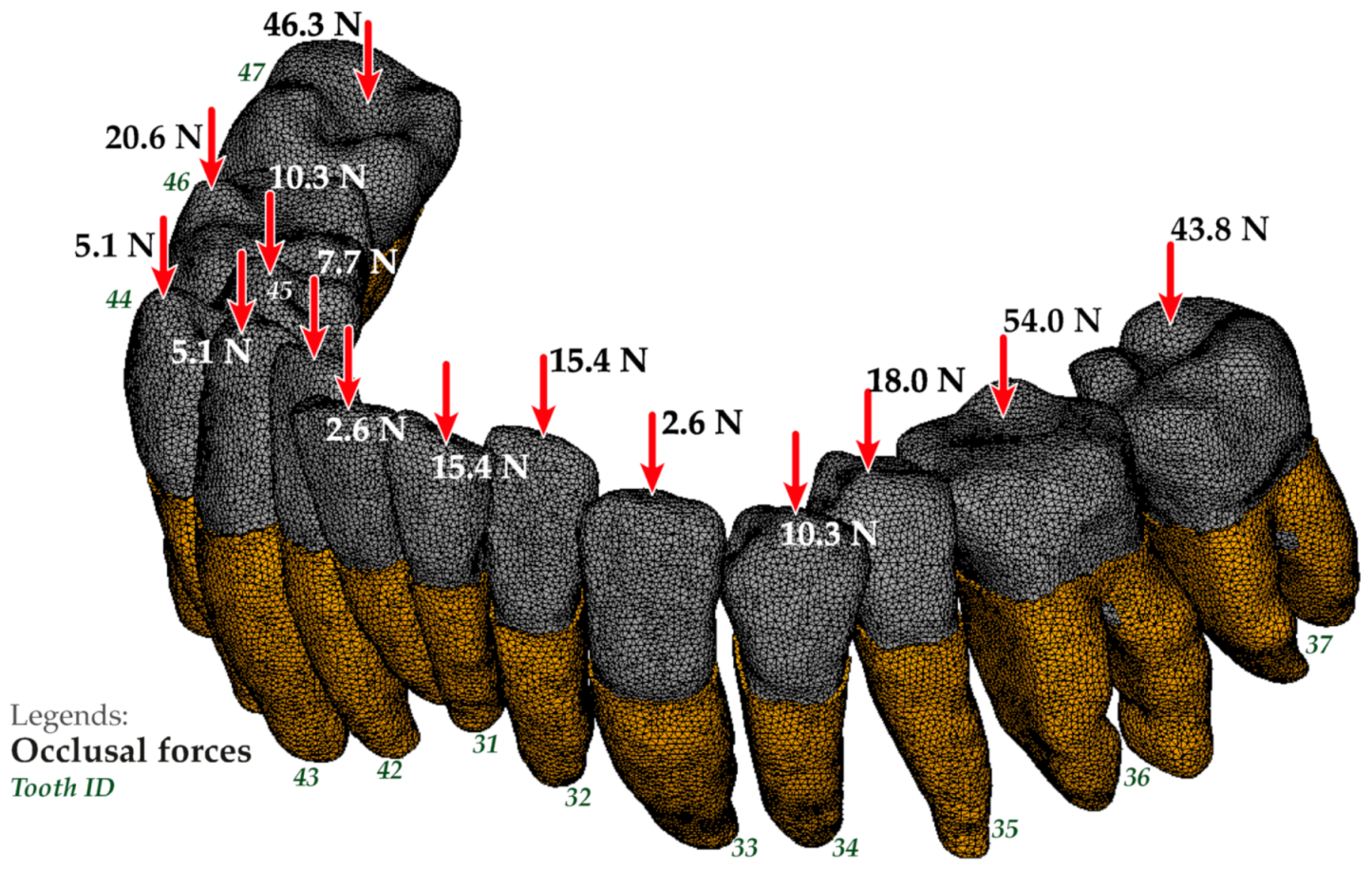
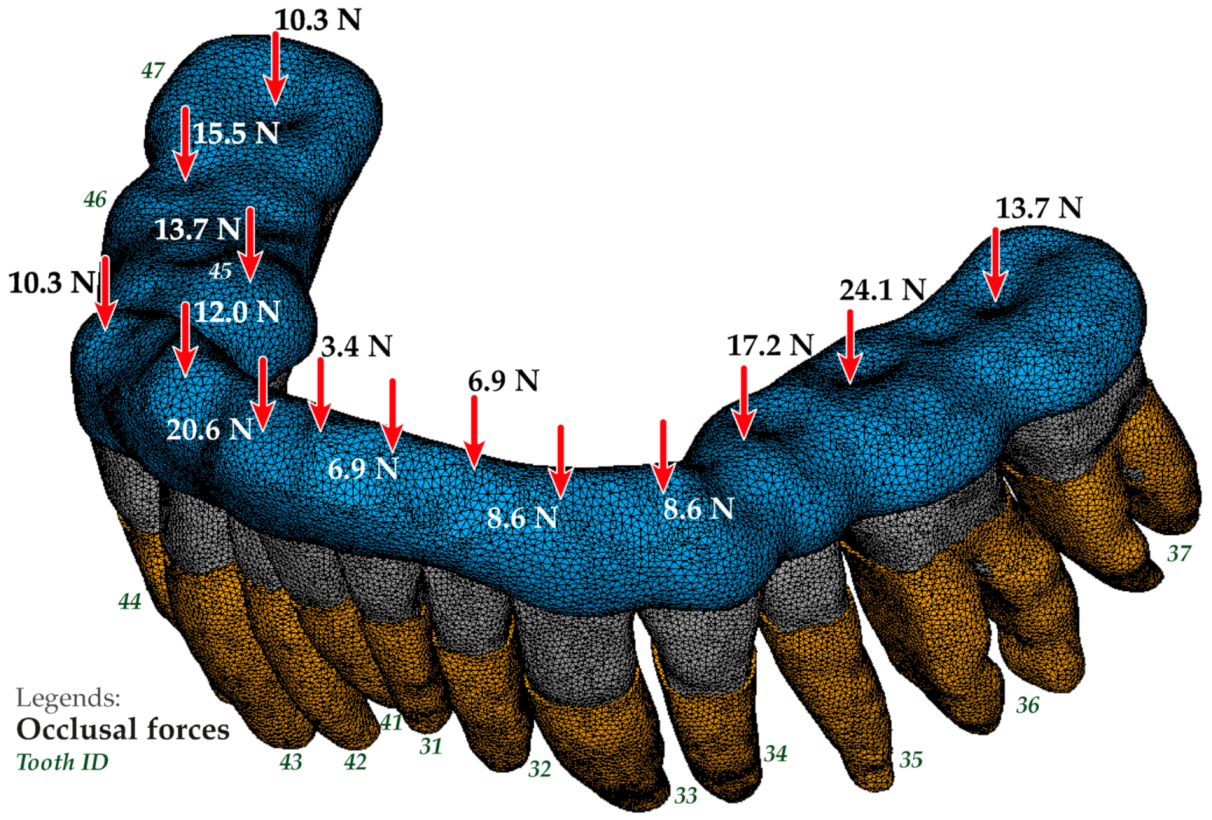
| Tooth ID | Measurement 1 [N (%)] | Measurement 2 [N (%)] | Measurement 3 [N (%)] |
|---|---|---|---|
| 37 | 43.8 (17) | 6.3 (5) | 13.7 (8) |
| 36 | 54.0 (21) | 44.3 (35) | 24.1 (14) |
| 35 | 18.0 (7) | 16.4 (13) | 17.2 (10) |
| 34 | 10.3 (4) | 11.4 (9) | 8.6 (5) |
| 33 | 2.6 (1) | 6.3 (5) | 8.6 (5) |
| 32 | 15.4 (6) | 1.3 (1) | 6.9 (4) |
| 31 | 15.4 (6) | 1.3 (1) | 6.9 (4) |
| 41 | 2.6 (1) | 1.3 (1) | 3.4 (2) |
| 42 | 7.7 (3) | 5.1 (4) | 20.6 (12) |
| 43 | 5.1 (2) | 5.1 (4) | 12.0 (7) |
| 44 | 10.3 (4) | 3.8 (3) | 10.3 (6) |
| 45 | 5.1 (2) | 2.5 (2) | 13.7 (8) |
| 46 | 20.6 (8) | 15.2 (12) | 15.5 (9) |
| 47 | 46.3 (18) | 6.3 (5) | 10.3 (6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gribov, D.; Antonik, M.; Butkov, D.; Stepanov, A.; Antonik, P.; Kharakh, Y.; Pivovarov, A.; Arutyunov, S. Personalized Biomechanical Analysis of the Mandible Teeth Behavior in the Treatment of Masticatory Muscles Parafunction. J. Funct. Biomater. 2021, 12, 23. https://doi.org/10.3390/jfb12020023
Gribov D, Antonik M, Butkov D, Stepanov A, Antonik P, Kharakh Y, Pivovarov A, Arutyunov S. Personalized Biomechanical Analysis of the Mandible Teeth Behavior in the Treatment of Masticatory Muscles Parafunction. Journal of Functional Biomaterials. 2021; 12(2):23. https://doi.org/10.3390/jfb12020023
Chicago/Turabian StyleGribov, Denis, Mikhail Antonik, Denis Butkov, Alexandr Stepanov, Pavel Antonik, Yaser Kharakh, Anton Pivovarov, and Sergey Arutyunov. 2021. "Personalized Biomechanical Analysis of the Mandible Teeth Behavior in the Treatment of Masticatory Muscles Parafunction" Journal of Functional Biomaterials 12, no. 2: 23. https://doi.org/10.3390/jfb12020023






