Dental Implant Abutment Screw Loss: Presentation of 10 Cases
Abstract
:1. Introduction
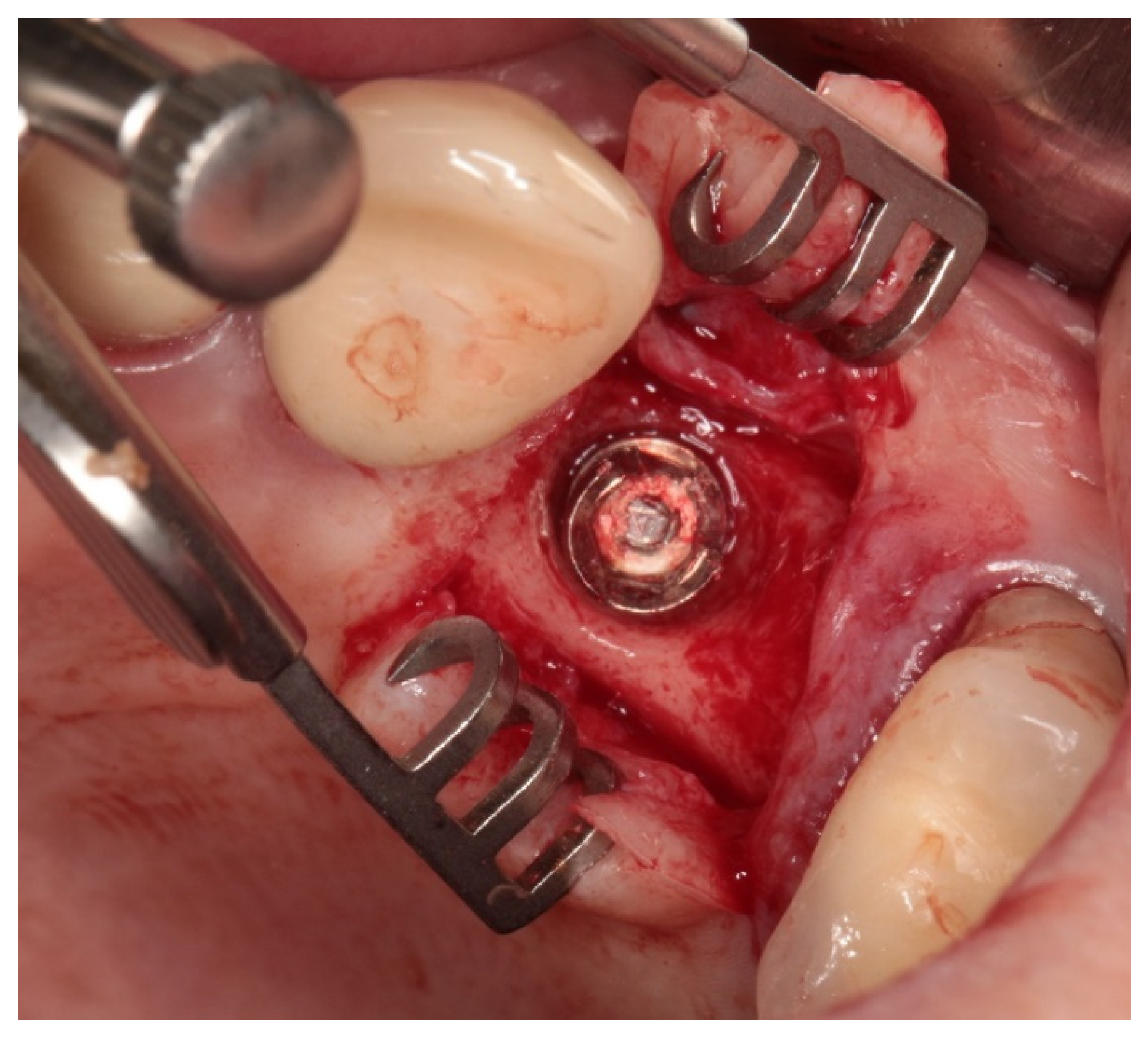
2. Materials
2.1. Clinical Study
2.2. SEM
2.3. Light Microscopy
2.4. Surface Roughness
3. Results
3.1. Clinical Observations
3.2. Material Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, K.Y.; Shin, K.S.; Jung, J.H.; Cho, H.W.; Kwon, K.H.; Kim, Y.L. Clinical Study on Screw Loosening in Dental Implant Prostheses: A 6-Year Retrospective Study. J. Korean Assoc. Oral Maxillofac. Surg. 2020, 46, 133. [Google Scholar] [CrossRef] [PubMed]
- Alsubaiy, E.F. Abutment Screw Loosening in Implants: A Literature Review. J. Fam. Med. Prim. Care 2020, 9, 5490. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; de Piva, A.M.O.D.; da Silva-Concílio, L.R.; Ausiello, P.; Kalman, L. Influence of Implant-Abutment Contact Surfaces and Prosthetic Screw Tightening on the Stress Concentration, Fatigue Life and Microgap Formation: A Finite Element Analysis. Oral 2021, 1, 88–101. [Google Scholar] [CrossRef]
- Epifania, E.; di Lauro, A.E.; Ausiello, P.; Mancone, A.; Garcia-Godoy, F.; Tribst, J.P.M. Effect of Crown Stiffness and Prosthetic Screw Absence on the Stress Distribution in Implant-Supported Restoration: A 3D Finite Element Analysis. PLoS ONE 2023, 18, e0285421. [Google Scholar] [CrossRef] [PubMed]
- Honório Tonin, B.S.; He, Y.; Ye, N.; Chew, H.P.; Fok, A. Effects of Tightening Torque on Screw Stress and Formation of Implant-Abutment Microgaps: A Finite Element Analysis. J. Prosthet. Dent. 2022, 127, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Kheder, W.; Al Kawas, S.; Khalaf, K.; Samsudin, A.R. Impact of Tribocorrosion and Titanium Particles Release on Dental Implant Complications—A Narrative Review. Jpn. Dent. Sci. Rev. 2021, 57, 182. [Google Scholar] [CrossRef] [PubMed]
- Souza, J.C.M.; Henriques, M.; Teughels, W.; Ponthiaux, P.; Celis, J.P.; Rocha, L.A. Wear and Corrosion Interactions on Titanium in Oral Environment: Literature Review. J. Bio-Tribo-Corros. 2015, 1, 13. [Google Scholar] [CrossRef]
- Corne, P.; De March, P.; Cleymand, F.; Geringer, J. Fretting-Corrosion Behavior on Dental Implant Connection in Human Saliva. J. Mech. Behav. Biomed. Mater. 2019, 94, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Tepla, T.; Pleshakov, E.; Sieniawski, J.; Bohun, L. Causes of Degradation of Titanium Dental Implants. Ukr. J. Mech. Eng. Mater. Sci. 2022, 8, 31–40. [Google Scholar] [CrossRef]
- Revathi, A.; Borrás, A.D.; Muñoz, A.I.; Richard, C.; Manivasagam, G. Degradation Mechanisms and Future Challenges of Titanium and Its Alloys for Dental Implant Applications in Oral Environment. Mater. Sci. Eng. C 2017, 76, 1354–1368. [Google Scholar] [CrossRef]
- Sun, F.; Cheng, W.; Zhao, B.H.; Song, G.Q.; Lin, Z. Evaluation the Loosening of Abutment Screws in Fluid Contamination: An in Vitro Study. Sci. Rep. 2022, 12, 10797. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Min, J.; Chen, X.; Yu, P.; Tan, X.; Zhang, Q.; Yu, H. Effects of Two Fretting Damage Modes on the Dental Implant–Abutment Interface and the Generation of Metal Wear Debris: An in Vitro Study. Fatigue Fract. Eng. Mater. Struct. 2021, 44, 847–858. [Google Scholar] [CrossRef]
- Rodrigues, D.C.; Urban, R.M.; Jacobs, J.J.; Gilbert, J.L. In Vivo Severe Corrosion and Hydrogen Embrittlement of Retrieved Modular Body Titanium Alloy Hip-Implants. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 88, 206–219. [Google Scholar] [CrossRef] [PubMed]
- Chin, M.Y.H.; Sandham, A.; de Vries, J.; van der Mei, H.C.; Busscher, H.J. Biofilm Formation on Surface Characterized Micro-Implants for Skeletal Anchorage in Orthodontics. Biomaterials 2007, 28, 2032–2040. [Google Scholar] [CrossRef] [PubMed]
- Ossowska, A.; Zieliński, A. The Mechanisms of Degradation of Titanium Dental Implants. Coatings 2020, 10, 836. [Google Scholar] [CrossRef]
- Prestat, M.; Thierry, D. Corrosion of Titanium under Simulated Inflammation Conditions: Clinical Context and in Vitro Investigations. Acta Biomater. 2021, 136, 72–87. [Google Scholar] [CrossRef] [PubMed]
- El-Sheikh, M.A.Y.; Mostafa, T.M.N.; El-Sheikh, M.M. Effect of Different Angulations and Collar Lengths of Conical Hybrid Implant Abutment on Screw Loosening after Dynamic Cyclic Loading. Int. J. Implant Dent. 2018, 4, 39. [Google Scholar] [CrossRef]
- Fokas, G.; Ma, L.; Chronopoulos, V.; Janda, M.; Mattheos, N. Differences in Micromorphology of the Implant-Abutment Junction for Original and Third-Party Abutments on a Representative Dental Implant. J. Prosthet. Dent. 2019, 121, 143–150. [Google Scholar] [CrossRef]
- Michalakis, K.X.; Lino, P.; Muftu, S.; Pissiotis, A.; Hirayama, H. The Effect of Different Implant-Abutment Connections on Screw Joint Stability. J. Oral Implantol. 2014, 40, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Cashman, P.M.; Schneider, R.L.; Schneider, G.B.; Stanford, C.M.; Clancy, J.M.; Qian, F. In Vitro Analysis of Post-Fatigue Reverse-Torque Values at the Dental Abutment/Implant Interface for a Unitarian Abutment Design. J. Prosthodont. 2011, 20, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.; Shin, S.Y. Influence of the Implant Abutment Types and the Dynamic Loading on Initial Screw Loosening. J. Adv. Prosthodont. 2013, 5, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Ghanbarzadeh, J.; Dashti, H.; Abbasi, M.; Nakhaei, M. Torque Removal Evaluation of One-Piece and Two-Piece Abutment Screws under Dry and Wet Conditions. J. Mashhad Dent. Sch. 2015, 39, 89–98. [Google Scholar] [CrossRef]
- Berberi, A.; Maroun, D.; Kanj, W.; Amine, E.Z.; Philippe, A. Micromovement Evaluation of Original and Compatible Abutments at the Implant-Abutment Interface. J. Contemp. Dent. Pract. 2016, 17, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Pournasiri, I.; Farid, F.; Zaker Jafari, H.; Simdar, N.; Maleki, D. Screw Loosening of Original and Non-Original Abutments in Implant Dentistry: An in Vitro Study. J. Osseointegration 2022, 14, 155–158. [Google Scholar] [CrossRef]
- Alonso-Pérez, R.; Bartolomé, J.; Ferreiroa, A.; Salido, M.; Pradíes, G. Evaluation of the Mechanical Behavior and Marginal Accuracy of Stock and Laser-Sintered Implant Abutments. Int. J. Prosthodont. 2017, 30, 136–138. [Google Scholar] [CrossRef] [PubMed]
- Solá-Ruíz, M.F.; Selva-Otaolaurruchi, E.; Senent-Vicente, G.; González-de-Cossio, I.; Amigó-Borrás, V. Accuracy Combining Different Brands of Implants and Abutments. Med. Oral Patol. Oral Cir. Buccal 2013, 18, e332. [Google Scholar] [CrossRef] [PubMed]
- Cameron, S.M.; Joyce, A.; Brousseau, J.S.; Parker, M.H. Radiographic Verification of Implant Abutment Seating. J. Prosthet. Dent. 1998, 79, 298–303. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira Mota, V.P.; Braga, M.S.; Loss, A.A.; Mello, H.N.; Rosetti, E.P.; de-Azevedo-Vaz, S.L. Detection of Misfits at the Abutment-Prosthesis Interface in the Esthetic Zone: Implications of the Radiographic Technique and the Magnitude of the Misfit. J. Prosthet. Dent. 2023, 130, 239.e1–239.e9. [Google Scholar] [CrossRef] [PubMed]









| Case No. | Implant Side Anterior/Lateral | Denture Type | Implant Type/Abutment Dimensions and Manufacturer | Case Description |
|---|---|---|---|---|
| 1 | lateral | single crown 46 | IRES 4.1 mm × 8 mm | The tested screw was used to attach a single crown in the lateral section 46 (mandibular first molar, right side) to an implant with a diameter of 4.1 × length of 8 mm. The implant was implanted in 2018, the crown was made in 2019, and the screw worked for four years. The patient did not come for regular check-ups and only came to the emergency room due to loosening of the crown. |
| 2 | anterior + lateral | bridge 6 pts. 21–26 | ZIMMER 3.7 mm × 13 mm ZIMMER 4.1 mm × 11.5 mm ZIMMER 4.1 mm × 10 mm ZIMMER 4.1 mm × 10 mm | The four screws tested attached a six-point bridge to implants in sections 21–26 (front and lateral sections of the maxilla, left side). Implant in the incisor area with a diameter of 3.7 mm and a length of 13 mm, implant in the canine area with a diameter of 4.1 mm and a length of 11.5 mm, in the area of the first premolar with a diameter of 4.1 mm and a length of 10 mm, and last implant in the area of the molar tooth with a diameter 4 and 10 mm long. Implant placement in 2016. The prosthetic work was installed in 2020, the screws lasted for three years. The patient did not come for regular check-ups and started treatment in another office, which resulted in overloading the bridge on implants 21–26 and breaking two of the four implant-fixing screws in the premolar and molar area. |
| 3 | lateral | bridge 3 pts. 15–17 | ZIMMER 3.7 mm × 11.5 mm ZIMMER 4.7 mm × 8 mm | The loosened screw came from a 3-point bridge based on two implants in the lateral part of the maxilla, right side 15–17. Implants in the area of the first premolar (14) with a diameter of 3.7 mm and a length of 11.5 mm (implanted in 2017) and the second one in the area of the first molar of the maxilla, right side (16) with a diameter of 4.7 mm and a length of 8 mm (implanted in 2018). The bridge was constructed in 2021, the screw operated for two years. The patient came for follow-up visits and the screw was tightened once. |
| 4 | lateral | single crown 14 | ZIMMER 4.1 mm × 10 mm | The tested screw attached a single crown placed on the right side of the maxillary first premolar (14), lateral section. Implant with a diameter of 4.1 mm and a length of 10 mm. It was implanted in 2014. The prosthetic work was installed in 2015. The screw functioned for eight years. The patient did not attend regular follow-up visits. The screw did not come loose before. |
| 5 | lateral | single crown 37 | ZIMMER 3.7 mm × 8 mm | The screw comes from a single crown on an implant placed near the second molar of the mandible on the left side (37), lateral section. The 3.7 mm diameter and 8 mm long implant was placed in 2015, and the single crown was placed in 2016. The screw lasted for six years. The patient came for follow-up visits sporadically and irregularly, and the screw was tightened twice. |
| 6 | lateral | single crown 36 | ZIMMER 3.7 mm × 10 mm | The screw comes from a single crown on an implant placed near the first molar of the mandible, left side (36), lateral section. An implant with a diameter of 3.7 mm and a length of 10 mm was implanted in 2015. A single crown on the implant was placed in 2016. The screw functioned for six years. The patient came for follow-up visits sporadically, irregularly. The screw was tightened once. |
| 7 | lateral | bridge 3 pts. 44–46 | IRES 3.75 mm × 11.5 mm IRES 3.75 mm × 10 mm | The screw tested comes from a 3-point bridge in the lateral section 44–46 mounted on two implants. Implants in the area of the mandibular first premolar (44) with a diameter of 3.75 mm and a length of 11.5 mm. And the second one in the area of the first molar of the mandible, right side (46), with a diameter of 3.75 and a length of 10 mm were implanted in 2018. The prosthetic work was installed in 2019. The tested screw functioned for four years. The patient did not come for regular check-ups, and the screws did not loosen earlier. The examination revealed, in addition to the loose screw, a fracture of the implant 46. |
| 8 | lateral | single crown 24 | IRES 4.1 mm × 11.5 mm | The tested screw was used to attach a single crown to the implant in the area of the maxillary first premolar, left side (24), lateral section. Implant with a diameter of 4.1 mm and a length of 11.5 mm was implanted in 2019. The crown was installed in 2021. The screw worked for two years. The patient came for follow-up visits and the screw was tightened once. |
| 9 | lateral | single crown 46 | IDI 3.7 mm × 12 mm | The broken screw attached a single crown to the implant in the area of the first mandibular premolar, right side (46) in the lateral section. Implant with a diameter of 3.7 mm and a length of 12 mm was implanted in 2009. The screw worked for one year. The patient did not come for follow-up visits. |
| 10 | lateral | single crown 36 | ZIMMER 4.1 mm × 10 mm | Patient 10. The broken screw attached a single crown to the implant in the area of the first molar of the mandible, left side (36), lateral section. Implant with a diameter of 4.1 mm and a length of 10 mm was implanted in 2020. The crown was attached in 2020. The screw lasted three years and was tightened twice. The patient did not attend regular follow-up visits. |
| Case No. | Clinical Inspection | Optical/SEM Inspection | Lifetime Years |
|---|---|---|---|
| 1 | 1 screws loosening | extremely numerous deep pits | 4 |
| 2 | 2 fractured screws 2 screws loosening | extremely numerous deep pits | 3 |
| 3 | 1 screws loosening | less numerous deep pits | 2 |
| 4 | 1 screws loosening | numerous deep pits brownish sediment | 8 |
| 5 | 1 screws loosening | numerous deep pits | 7 |
| 6 | 1 screws loosening | moderately numerous deep pits | 7 |
| 7 | 1 screws loosening | numerous deep pits white sediment | 4 |
| 8 | 1 screws loosening | crack on the shank below head extremely numerous deep pits | 2 |
| 9 | 1 fractured screw | few initial shallow pits difficult to see | 1 |
| 10 | 1 fractured screw | numerous deep pits | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soleimani, M.; Żmudzki, J.; Pakieła, W.; Jaśkowska, A.; Krasny, K. Dental Implant Abutment Screw Loss: Presentation of 10 Cases. J. Funct. Biomater. 2024, 15, 96. https://doi.org/10.3390/jfb15040096
Soleimani M, Żmudzki J, Pakieła W, Jaśkowska A, Krasny K. Dental Implant Abutment Screw Loss: Presentation of 10 Cases. Journal of Functional Biomaterials. 2024; 15(4):96. https://doi.org/10.3390/jfb15040096
Chicago/Turabian StyleSoleimani, Maryam, Jarosław Żmudzki, Wojciech Pakieła, Anna Jaśkowska, and Kornel Krasny. 2024. "Dental Implant Abutment Screw Loss: Presentation of 10 Cases" Journal of Functional Biomaterials 15, no. 4: 96. https://doi.org/10.3390/jfb15040096
APA StyleSoleimani, M., Żmudzki, J., Pakieła, W., Jaśkowska, A., & Krasny, K. (2024). Dental Implant Abutment Screw Loss: Presentation of 10 Cases. Journal of Functional Biomaterials, 15(4), 96. https://doi.org/10.3390/jfb15040096









