Carbapenem-Resistant Enterobacteriaceae Bacteremia in Pediatric Patients in Latin America and the Caribbean: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Results
2.1. Analysis of Epidemiological Reports
2.2. Risk of Bias Assessment
3. Discussion
3.1. Limitations
3.2. Contributions of This Study
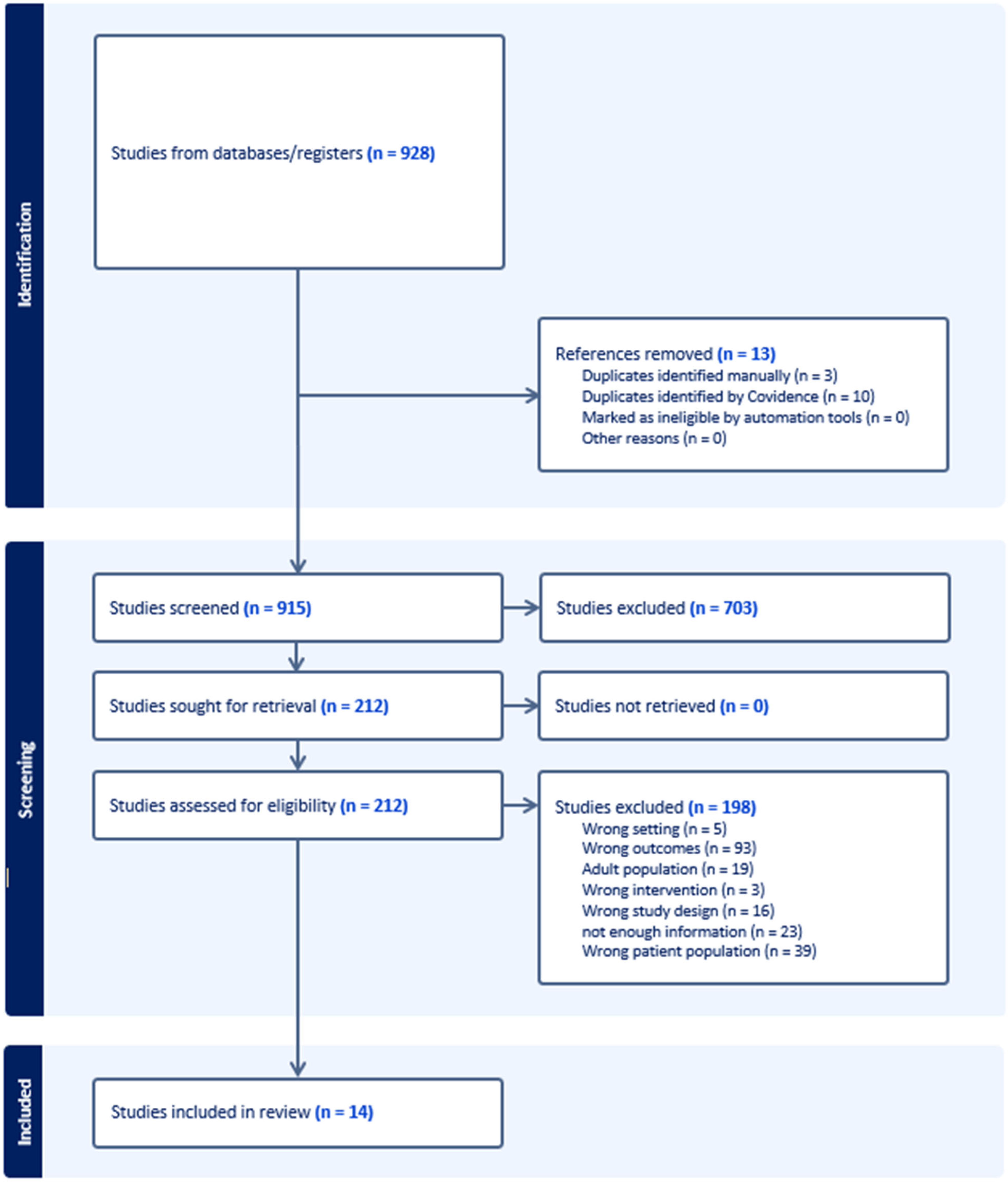
4. Material and Methods
4.1. Eligibility Criteria
4.2. Outcomes of Interest
4.3. Study Selection, Data Extraction, and Assessment of the Risk of Bias in Included Studies
4.4. Data Synthesis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global Burden of Bacterial Antimicrobial Resistance in 2019: A Systematic Analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Ciapponi, A.; Bardach, A.; Sandoval, M.M.; Palermo, M.C.; Navarro, E.; Espinal, C.; Quirós, R. Systematic Review and Meta-Analysis of Deaths Attributable to Antimicrobial Resistance, Latin America. Emerg. Infect. Dis. 2023, 29, 2335–2344. [Google Scholar] [CrossRef]
- Meng, H.; Yang, J.; Niu, M.; Zhu, H.; Zhou, Y.; Lu, J. Risk Factors and Clinical Outcomes of Carbapenem-Resistant Klebsiella Pneumoniae Bacteraemia in Children: A Retrospective Study. Int. J. Antimicrob. Agents 2023, 62, 106933. [Google Scholar] [CrossRef]
- Osei Sekyere, J.; Reta, M.A.; Bernard Fourie, P. Risk Factors For, and Molecular Epidemiology and Clinical Outcomes Of, Carbapenem- and Polymyxin-Resistant Gram-Negative Bacterial Infections in Pregnant Women, Infants, and Toddlers: A Systematic Review and Meta-Analyses. Ann. N. Y. Acad. Sci. 2021, 1502, 54–71. [Google Scholar] [CrossRef]
- Logan, L.K.; Nguyen, D.C.; Scaggs Huang, F.A.; Qureshi, N.K.; Charnot-Katsikas, A.; Bartlett, A.H.; Zheng, X.; Hujer, A.M.; Domitrovic, T.N.; Marshall, S.H.; et al. A Multi-Centered Case-Case-Control Study of Factors Associated with Klebsiella Pneumoniae Carbapenemase-Producing Enterobacteriaceae Infections in Children and Young Adults. Pediatr. Infect. Dis. J. 2019, 38, 490–495. [Google Scholar] [CrossRef]
- Pan American Health Organization. Epidemiological Alert: Emergence and Increase of New Combinations of Carbapenemases in Enterobacterales in Latin America and the Caribbean; Pan American Health Organization: Washington, DC, USA, 2021. [Google Scholar]
- Fasciana, T.; Antonelli, A.; Bianco, G.; Lombardo, D.; Codda, G.; Roscetto, E.; Perez, M.; Lipari, D.; Arrigo, I.; Galia, E.; et al. Multicenter Study on the Prevalence of Colonization due to Carbapenem-Resistant Enterobacterales Strains before and during the First Year of COVID-19, Italy 2018–2020. Front. Public Health 2023, 11, 1270924. [Google Scholar] [CrossRef]
- Thomas, G.R.; Corso, A.; Pasterán, F.; Shal, J.; Sosa, A.; Pillonetto, M.; de Souza Peral, R.T.; Hormazábal, J.C.; Araya, P.; Saavedra, S.Y.; et al. Increased Detection of Carbapenemase-Producing Enterobacterales Bacteria in Latin America and the Caribbean during the COVID-19 Pandemic. Emerg. Infect. Dis. 2022, 28, e220415. [Google Scholar] [CrossRef]
- Meatherall, B.L.; Gregson, D.; Ross, T.; Pitout, J.D.D.; Laupland, K.B. Incidence, Risk Factors, and Outcomes of Klebsiella Pneumoniae Bacteremia. Am. J. Med. 2009, 122, 866–873. [Google Scholar] [CrossRef]
- García-Betancur, J.C.; Appel, T.M.; Esparza, G.; Gales, A.C.; Levy-Hara, G.; Cornistein, W.; Vega, S.; Nuñez, D.; Cuellar, L.; Bavestrello, L.; et al. Update on the Epidemiology of Carbapenemases in Latin America and the Caribbean. Expert Rev. Anti-Infect. Ther. 2021, 19, 197–213. [Google Scholar] [CrossRef]
- Tumbarello, M.; Spanu, T.; Sanguinetti, M.; Citton, R.; Montuori, E.; Leone, F.; Fadda, G.; Cauda, R. Bloodstream Infections Caused by Extended-Spectrum-Beta-Lactamase-Producing Klebsiella Pneumoniae: Risk Factors, Molecular Epidemiology, and Clinical Outcome. Antimicrob. Agents Chemother. 2006, 50, 498–504. [Google Scholar] [CrossRef]
- Stewardson, A.J.; Marimuthu, K.; Sengupta, S.; Allignol, A.; El-Bouseary, M.; Carvalho, M.J.; Hassan, B.; Delgado-Ramirez, M.A.; Arora, A.; Bagga, R.; et al. Effect of Carbapenem Resistance on Outcomes of Bloodstream Infection Caused by Enterobacteriaceae in Low-Income and Middle-Income Countries (PANORAMA): A Multinational Prospective Cohort Study. Lancet Infect. Dis. 2019, 19, 601–610. [Google Scholar] [CrossRef]
- Nirmal, G.; Jithin, T.K.; Gopakumar, K.G.; Parthiban, R.; Nair, C. Prevalence and Outcomes of Carbapenem-Resistant Bloodstream Infection in Children With Cancer. J. Pediatr. Hematol. Oncol. 2023, 45, e678–e682. [Google Scholar] [CrossRef]
- Martino, F.; Tijet, N.; Melano, R.; Petroni, A.; Heinz, E.; De Belder, D.; Faccone, D.; Rapoport, M.; Biondi, E.; Rodrigo, V.; et al. Isolation of Five Enterobacteriaceae Species Harbouring blaNDM-1 and Mcr-1 Plasmids from a Single Paediatric Patient. PLoS ONE 2019, 14, e0221960. [Google Scholar]
- Ruvinsky, S.; Voto, C.; Roel, M.; Deschutter, V.; Ferraro, D.; Aquino, N.; Reijtman, V.; Galvan, M.E.; Motto, E.; García, M.; et al. Carbapenem-Resistant Enterobacteriaceae Bloodstream Infections: A Case-Control Study from a Pediatric Referral Hospital in Argentina. Front. Public Health 2022, 10, 983174. [Google Scholar] [CrossRef]
- Alvares, P.A.; Arnoni, M.V.; da Silva, C.B.; Sáfadi, M.A.P.; Mimica, M.J. Carbapenem-Resistant Gram-Negative Bloodstream Infections in Critically Ill Children: Outcome and Risk Factors in a Tertiary Teaching Hospital in South America. J. Hosp. Infect. 2019, 101, 188–189. [Google Scholar] [CrossRef]
- de Oliveira, M.S.; de Assis, D.B.; Freire, M.P.; do Prado, G.V.B.; Machado, A.S.; Abdala, E.; Pierrotti, L.C.; Mangini, C.; Campos, L.; Caiaffa Filho, H.H.; et al. Treatment of KPC-Producing Enterobacteriaceae: Suboptimal Efficacy of Polymyxins. Clin. Microbiol. Infect. 2015, 21, 179.e1–179.e7. [Google Scholar] [CrossRef]
- Higashino, H.R.; Marchi, A.P.; Martins, R.C.R.; Batista, M.V.; Perdigão Neto, L.V.; Lima, V.A.C.D.C.; Rossi, F.; Guimarães, T.; Levin, A.S.; Rocha, V.; et al. Colistin-Resistant Klebsiella pneumoniae Co-Harboring KPC and MCR-1 in a Hematopoietic Stem Cell Transplantation Unit. Bone Marrow Transplant. 2018, 54, 1118–1120. [Google Scholar] [CrossRef]
- Nascimento, A.D.S.; Passaro, M.F.; Silva, P.S.D.S.; Rodriguez, S.F.; Martins, M.K.; Oliveira, S.C.P.; Moriel, P.; Visacri, M.B. Off-Label Use of Ceftazidime-Avibactam in a Premature Infant with Multidrug-Resistant Klebsiella Pneumoniae Infection: A Case Report. J. Pharm. Pract. 2023, 36, 1020–1025. [Google Scholar] [CrossRef]
- Márquez-Herrera, K.; Rojas-Vega, A.; Camacho-Moreno, G. Caracterización de Pacientes Con Aislamiento de Klebsiella Productora de Carbapenemasa En Un Hospital Pediátrico de Tercer Nivel de Bogotá, Colombia. Infectio 2016, 20, 231–237. [Google Scholar] [CrossRef]
- Perez, P.; Patiño, J.; Estacio, M.; Pino, J.; Manzi, E.; Medina, D. Bacteremia in Pediatric Patients with Hematopoietic Stem Cell Transplantation. Hematol. Transfus. Cell Ther. 2020, 42, 5. [Google Scholar] [CrossRef]
- Mera, F.S.C.; Chacón, J.A.R.; Lupercio, A.N.C.; Domínguez, D.C.L.; Martínez, A.G.C. Marcadores Hematológicos Y Bioquímicos Para El Diagnóstico Precoz de Bacteriemias Causadas Por Enterobacteriaceae Resistentes a Los Carbapenémicos. Rev. Médica-Científica CAMbios HECAM 2022, 20, 67–73. [Google Scholar]
- Aquino-Andrade, A.; Merida-Vieyra, J.; Arias de la Garza, E.; Arzate-Barbosa, P.; De Colsa Ranero, A. Carbapenemase-Producing Enterobacteriaceae in Mexico: Report of Seven Non-Clonal Cases in a Pediatric Hospital. BMC Microbiol. 2018, 18, 38. [Google Scholar] [CrossRef]
- Rodríguez-Palacios, M.M.; Servicio de Epidemiologia; Control de Infecciones Hospital Nacional; Ministerio de Salud Pública y Bienestar Social; Takahasi-Álvarez, V.; Vega-Bogado, M.E.; Servicio de Microbiología; Departamento de Laboratorio; Comité de Control de Infecciones; Hospital Nacional; et al. Ministerio de Salud Pública y Bienestar Social Caracterización Clínica Y Epidemiológica de Brote a Serratia Marcescens En Una Unidad de Cuidado Intensivo Pediátrico Hospital Nacional de Itaugua. Paraguay. Abril a Setiembre 2015. DEL NAC. 2016, 8, 19–33. [Google Scholar]
- Melgarejo Touchet, N.; Busignani, S.; Dunjo, P.; Brítez, M.; Kawabata, A.; Silvagni, M.; Rojas, C.; Mereles, E.; López, E.; Salinas, J.; et al. Primer Reporte de Enterobacterales Dobles Productores de Carbapenemasas En Hospitales de Paraguay. Mem. Inst. Investig. Cienc. Salud 2021, 19, 35–43. [Google Scholar] [CrossRef]
- Mayta-Barrios, M.M.; Ramirez-Illescas, J.J.; Pampa-Espinoza, L.; Yagui-Moscoso, M.J.A. Molecular characterization of carbapenemases in Peru during 2019. Rev. Peru. Med. Exp. Salud Publica 2021, 38, 113–118. [Google Scholar] [CrossRef]
- López-Cubillos, J.F.; Díaz, A.; Cárdenas, V.C.; Camacho-Moreno, G.; Cantor, E.; Arcila, E.M.; Hurtado, I.C.; Correa, A.M.; Tierradentro, T.M.; Ramirez, O.; et al. Carbapenem Resistance in Enterobacterales Bloodstream Infections among Children with Cancer or Post-Haematopoietic Stem Cell Transplant: A Retrospective Cohort Study. J. Antimicrob. Chemother. 2023, 78, 2462–2470. [Google Scholar] [CrossRef]
- Zhang, Y.; Guo, L.-Y.; Song, W.-Q.; Wang, Y.; Dong, F.; Liu, G. Risk Factors for Carbapenem-Resistant K. Pneumoniae Bloodstream Infection and Predictors of Mortality in Chinese Paediatric Patients. BMC Infect. Dis. 2018, 18, 248. [Google Scholar] [CrossRef]
- Ara-Montojo, M.F.; Escosa-García, L.; Alguacil-Guillén, M.; Seara, N.; Zozaya, C.; Plaza, D.; Schuffelmann-Gutiérrez, C.; de la Vega, Á.; Fernández-Camblor, C.; Ramos-Boluda, E.; et al. Predictors of Mortality and Clinical Characteristics among Carbapenem-Resistant or Carbapenemase-Producing Enterobacteriaceae Bloodstream Infections in Spanish Children. J. Antimicrob. Chemother. 2021, 76, 220–225. [Google Scholar] [CrossRef]
- Liu, Y.-C.; Lu, C.-Y.; Yen, T.-Y.; Chang, L.-Y.; Chen, J.-M.; Lee, P.-I.; Huang, L.-M. Clinical Characteristics and Outcomes of Carbapenem-Resistant Enterobacterales Bacteremia in Pediatric Patients. J. Microbiol. Immunol. Infect. 2023, 56, 84–92. [Google Scholar] [CrossRef]
- van Loon, K.; Voor In ’t Holt, A.F.; Vos, M.C. A Systematic Review and Meta-Analyses of the Clinical Epidemiology of Carbapenem-Resistant Enterobacteriaceae. Antimicrob. Agents Chemother. 2018, 62, e01730-17. [Google Scholar] [CrossRef]
- Pannaraj, P.S.; Bard, J.D.; Cerini, C.; Weissman, S.J. Pediatric Carbapenem-Resistant Enterobacteriaceae in Los Angeles, California, a High-Prevalence Region in the United States. Pediatr. Infect. Dis. J. 2015, 34, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Ruvinsky, S.; Monaco, A.; Perez, G.; Taicz, M.; Inda, L.; Epelbaum, C.; Kijko, I.; Constanzo, P.; Bologna, R. Effectiveness of a program to improve antibiotic use in children hospitalized in a children’s tertiary care facility in Argentina. Arch. Argent Pediatr. 2014, 2, 124–131. [Google Scholar]
- Akturk, H.; Sutcu, M.; Somer, A.; Aydın, D.; Cihan, R.; Ozdemir, A.; Coban, A.; Ince, Z.; Citak, A.; Salman, N. Carbapenem Resistant Klebsiella Pneumoniae Colonization in Pediatric and Neonatal Intensive Care Units: Risk Factors for Progression to Infection. Braz. J. Infect. Dis. 2016, 20, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.-W.; Park, S.; Kim, A.R.; Han, J.; Lee, J.; Seo, H.; Sung, H.; Kim, M.-N.; Chang, E.; Bae, S.; et al. Clinical Characteristics of and Risk Factors for Subsequent Carbapenemase-Producing Enterobacterales (CPE) Bacteraemia in Rectal CPE Carriers. Int. J. Antimicrob. Agents 2023, 62, 106959. [Google Scholar] [CrossRef]
- Almasian Tehrani, N.; Azimi, L.; Armin, S.; Soleimani, N.; Fallah, F.; Karimi, A.; Shamsian, B.S.; Nazari, S.; Alebouyeh, M. Endogenous Bacteremia Caused by Intestinal Colonization of Carbapenem-Resistant Enterobacteriaceae (CRE) in Immunocompromised Children. Trop. Med. Infect. Dis. 2023, 8, 402. [Google Scholar] [CrossRef]
- Nabarro, L.E.B.; Shankar, C.; Pragasam, A.K.; Mathew, G.; Jeyaseelan, V.; Veeraraghavan, B.; Verghese, V.P. Clinical and Bacterial Risk Factors for Mortality in Children with Carbapenem-Resistant Enterobacteriaceae Bloodstream Infections in India. Pediatr. Infect. Dis. J. 2017, 36, e161–e166. [Google Scholar] [CrossRef]
- Pérez-Galera, S.; Bravo-Ferrer, J.M.; Paniagua, M.; Kostyanev, T.; de Kraker, M.E.A.; Feifel, J.; Sojo-Dorado, J.; Schotsman, J.; Cantón, R.; Daikos, G.L.; et al. Risk Factors for Infections Caused by Carbapenem-Resistant Enterobacterales: An International Matched Case-Control-Control Study (EURECA). EClinicalMedicine 2023, 57, 101871. [Google Scholar] [CrossRef]
- Bonomo, R.A.; Burd, E.M.; Conly, J.; Limbago, B.M.; Poirel, L.; Segre, J.A.; Westblade, L.F. Carbapenemase-Producing Organisms: A Global Scourge. Clin. Infect. Dis. 2018, 66, 1290–1297. [Google Scholar] [CrossRef]
- Lalaoui, R.; Djukovic, A.; Bakour, S.; Hadjadj, L.; Sanz, J.; Salavert, M.; López-Hontangas, J.L.; Sanz, M.A.; Ubeda, C.; Rolain, J.-M. Genomic Characterization of Citrobacter Freundii Strains Coproducing OXA-48 and VIM-1 Carbapenemase Enzymes Isolated in Leukemic Patient in Spain. Antimicrob. Resist. Infect. Control 2019, 8, 167. [Google Scholar] [CrossRef]
- Tang, Y.; Zhou, Y.; Meng, C.; Huang, Y.; Jiang, X. Co-Occurrence of a Novel VIM-1 and FosA3-Encoding Multidrug-Resistant Plasmid and a KPC-2-Encoding pKP048-like Plasmid in a Clinical Isolate of Klebsiella Pneumoniae Sequence Type 11. Infect. Genet. Evol. 2020, 85, 104479. [Google Scholar] [CrossRef]
- Sellera, F.P.; Da Silva, L.C.B.A.; Lincopan, N. Rapid Spread of Critical Priority Carbapenemase-Producing Pathogens in Companion Animals: A One Health Challenge for a Post-Pandemic World. J. Antimicrob. Chemother. 2021, 76, 2225–2229. [Google Scholar] [CrossRef] [PubMed]
- Merrick, B.; Tan, M.K.I.; Bisnauthsing, K.; Goldenberg, S.D. Healthcare Resource Use in Hospitalized Patients with Carbapenem-Resistant Gram-Negative Infections. J. Hosp. Infect. 2021, 110, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Fang, X.; Zhang, J.; Zheng, X.; Shangguan, S.; Chen, S.; Shen, Y.; Liu, Z.; Li, J.; Zhang, R.; et al. Impact of Carbapenem Resistance on Mortality in Patients Infected with Enterobacteriaceae: A Systematic Review and Meta-Analysis. BMJ Open 2021, 11, e054971. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Rev. Esp. Cardiol. 2021, 74, 790–799. [Google Scholar] [CrossRef]
- Freeman, M.F.; Tukey, J.W. Transformations Related to the Angular and the Square Root. Ann. Math. Stat. 1950, 21, 607–611. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-Analysis in Clinical Trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to Perform a Meta-Analysis with R: A Practical Tutorial. Evid. Based. Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef]
- Study Quality Assessment Tools. Available online: http://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 18 November 2023).
| Author and Year of Publication | Country | Study Design | Number of Patients | Male n | Age in Months Median (IQR) | Underlying Condition n (%) | Colonization n | Mortality n | Period |
|---|---|---|---|---|---|---|---|---|---|
| Martino, 2019 [14] | Argentina | Case report | 1 | 1 | 48 | Erythodermic psoriasis | Yes (during episode) | 1 | February 2014 |
| Ruvinsky, 2022 [15] | Argentina | Case–control | 46 | 23 | 36 (11.2–117) | 45: hematological diseases (23), liver transplantation (12) | 35 | 6 | January 2014–December 2019 |
| Alvares, 2019 [16] | Brazil | Case series | 6 | 5 | 19.2 (12–70) | Non-specified (5) | 2 | 4 | January 2012–December 2016 |
| de Oliveira, 2015 [17] | Brazil | Case series | 4 | 3 | 17 (5–28) | 4: cancer (2) | NR | 1 | October 2009–June 2013 |
| Higashino, 2018 [18] | Brazil | Case series | 2 | 2 | 180 | HSCT | NR | 2 | 2008–2015 |
| Nascimento, 2022 [19] | Brazil | Case report | 1 | 1 | 1 | Prematurity | NR | 0 | NR |
| Marquez Herrera, 2016 [20] | Colombia | Case series | 10 | NR | 48 | Hematological diseases (5) | No | 4 | 2012–2015 |
| Perez, 2020 [21] | Colombia | Case series | 14 | 7 | 117 (32–177) | HSCT | 5 | 4 | January 2012–January 2017 |
| Reyes Chacón, 2021 [22] | Ecuador | Case series | 41 | 23 | 12 (11–24) | Congenital heart disease (18), prematurity (15), cancer (4) | NR | 24 | May 2016-July 2018 |
| Aquino Andrade, 2018 [23] | Mexico | Case series | 3 | NR | 72 | Leukemia | NR | 3 | April 2016–July 2016 |
| Rodriguez Palacios, 2016 [24] | Paraguay | Case report | 1 | 1 | NR | NR | NR | NR | April 2015–September 2015 |
| Touchet, 2021 [25] | Paraguay | Case series | 3 | 3 | 4.4 | NR | NR | NR | February 2021–September 2021 |
| Barrios, 2021 [26] | Perú | Case report | 1 | 0 | NR | No | NR | NR | January 2019–December 2019 |
| López Cubillos, 2023 [27] | Colombia | Case series | 56 | 36 | 126 (60–176) | HSCT | 50 | 20 | 2012–2021 |
| Variables | Pooled Estimates from Meta-Analysis % (95% CI) | I2 (%) |
|---|---|---|
| Risk factors associated with CRE-BSI | ||
| 100 (92–100) | 65 |
| 41 (2–87) | 92 |
| 91 (76–100) | 63 |
| 84 (74–93) | 0 |
| 59 (35–80) | 71 |
| 100 (92–100) | 3 |
| 51 (31–70) | 0 |
| 66 (46–84) | 0 |
| Characteristics of infection and resource use | ||
| 75 (27–100) | 64 |
| 86 (44–100) | 86 |
| 30 (13–66) | 99 |
| 34 (19–49) | 14 |
| Microbiological Isolates | n (%) |
|---|---|
| Klebsiella pneumoniae | 460 (91) |
| Escherichia coli | 23 (4.5) |
| Serratia marcescens | 8 (1.6) |
| Enterobacter cloacae | 5 (1) |
| Enterobacter spp. | 4 (0.8) |
| Klebsiella oxytoca | 2 (0.4) |
| Citrobacter spp. | 2 (0.4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruvinsky, S.; Voto, C.; Roel, M.; Portillo, V.; Naranjo Zuñiga, G.; Ulloa-Gutierrez, R.; Comandé, D.; Ciapponi, A.; Aboud, G.; Brizuela, M.; et al. Carbapenem-Resistant Enterobacteriaceae Bacteremia in Pediatric Patients in Latin America and the Caribbean: A Systematic Review and Meta-Analysis. Antibiotics 2024, 13, 1117. https://doi.org/10.3390/antibiotics13121117
Ruvinsky S, Voto C, Roel M, Portillo V, Naranjo Zuñiga G, Ulloa-Gutierrez R, Comandé D, Ciapponi A, Aboud G, Brizuela M, et al. Carbapenem-Resistant Enterobacteriaceae Bacteremia in Pediatric Patients in Latin America and the Caribbean: A Systematic Review and Meta-Analysis. Antibiotics. 2024; 13(12):1117. https://doi.org/10.3390/antibiotics13121117
Chicago/Turabian StyleRuvinsky, Silvina, Carla Voto, Macarena Roel, Victoria Portillo, Gabriela Naranjo Zuñiga, Rolando Ulloa-Gutierrez, Daniel Comandé, Agustín Ciapponi, Gabriela Aboud, Martín Brizuela, and et al. 2024. "Carbapenem-Resistant Enterobacteriaceae Bacteremia in Pediatric Patients in Latin America and the Caribbean: A Systematic Review and Meta-Analysis" Antibiotics 13, no. 12: 1117. https://doi.org/10.3390/antibiotics13121117
APA StyleRuvinsky, S., Voto, C., Roel, M., Portillo, V., Naranjo Zuñiga, G., Ulloa-Gutierrez, R., Comandé, D., Ciapponi, A., Aboud, G., Brizuela, M., & Bardach, A. (2024). Carbapenem-Resistant Enterobacteriaceae Bacteremia in Pediatric Patients in Latin America and the Caribbean: A Systematic Review and Meta-Analysis. Antibiotics, 13(12), 1117. https://doi.org/10.3390/antibiotics13121117









