Abstract
The loosening or fracture of the prosthetic abutment screw is the most frequently reported complication in implant dentistry. Thin diamond-like carbon (DLC) films offer a low friction coefficient and high wear resistance, functioning as a solid lubricant to prevent the weakening of the implant–abutment system. This study evaluated the effects of DLC nanofilms on the reverse torque of prosthetic abutments after simulated chewing. Abutments with 8° and 11° taper connections, with and without DLC or silver-doped DLC coatings, were tested. The films were deposited through the plasma enhanced chemical vapor deposition process. After two million cycles of mechanical loading, reverse torque was measured. Analyses with scanning electron microscopy were conducted on three samples of each group before and after mechanical cycling to verify the adaptation of the abutments. Tribology, Raman and energy-dispersive spectroscopy analyses were performed. All groups showed a reduction in insertion torque, except the DLC-coated 8° abutments, which demonstrated increased reverse torque. The 11° taper groups experienced the most torque loss. The nanofilm had no significant effect on maintaining insertion torque, except for the DLC8 group, which showed improved performance.
1. Introduction
The internal conical connections have been developed to improve the biomechanical properties of implants [1] and to reduce the incidence of problems usually found in conventional connections. Stability may vary according to the conicity degree, geometries, and surface interface [2].
However, regardless of the connection type, screw-retained abutment systems present a gap in the abutment–implant interface. This space allows for possible micro infiltration and bacterial colonization [3] and may be responsible for abutment micromovement, leading to mechanical failures (loosening and fracture of the screw) [4] with consequent preload loss.
A screw system failure occurs in two stages. The first stage starts when external forces, such as mastication, act on the system. At this point, screw threads slide over the implant’s internal threads and/or wear out, causing thread height to diminish, consequently leading to a loss of screw preload. The second stage occurs when the decrease in preload leads to torque loss in the threads and, consequently, to loss of direct contact between the screw and the implant’s internal threads [5].
The compression and preload amounts are determined by several variables. These include the elasticity modulus of the materials used in the manufacturing of the fixing screw and the parts to be attached to it, the coefficient of friction of sliding surfaces [6], component adaptation, the lubrication system [7], applied torque and speed of application, the head and screw threads geometry, and their superficial roughness [8].
Studies have shown that most of the screwing strength, when applied to prosthetic screws, is lost due to the friction between micro-roughness and the metal surfaces, which limits screw rotation [9,10].
The preload maintenance will depend, in part, on the accommodation effect (settling effect) obtained between the surfaces [11], since they are not smooth and full contact between them does not occur. Additionally, such micro-roughness suffers wear and deformation, which leads to contact loss between the coupling threads and consequent preload loss [12].
Reverse torque, the force required to remove an implant abutment, is crucial for assessing the mechanical stability of implant–abutment connections. Studies have shown that both indexed and non-indexed abutments experience significant torque loss after insertion [13,14]. However, non-indexed abutments generally demonstrate better torque retention compared to indexed abutments [15]. The implant material also influences reverse torque values, with hydroxyapatite-coated implants exhibiting significantly higher torque removal values than titanium implants [16]. Additionally, mandibular implants tend to show greater torque resistance than maxillary implants. These findings suggest that factors such as abutment design, implant material, and placement location play important roles in maintaining implant stability. Understanding reverse torque values is essential for determining appropriate torque levels for abutment fastening and ensuring the long-term success of implant-supported restorations [13]. Hence, reducing friction between metallic surfaces could increase rotation and, consequently, the preload. The addition of a lubricant to this interface has been a proposed alternative [10]. Thin diamond-like carbon coating (DLC) offers a low friction coefficient and high resistance to wear [17], acting as a solid lubricant. The unique properties of DLC coatings depend on the ratio of sp3/sp2 phases, which can be tailored for specific applications [18]. These coatings are widely used in orthopedic, cardiovascular, and dental applications, and for various biomedical devices such as vascular stents, prosthetic heart valves, and surgical instruments [19]. Known for their hemocompatibility, they are applied to artificial heart surfaces in contact with blood and are effective in pressure sensors, chemical electrodes, and biochemical sensors. They promote rapid endothelization of implants, minimize platelet activation, and reduce thrombus formation. DLC coatings are considered highly promising for biomedical applications, with growing potential in automotive and adhesive uses as well [18,19].
In the literature, the coatings used in implant dentistry are intended for the prior preparation of the implant and consider their advantages in the osseointegration process. For example, common coating materials include carbon, bisphosphonates, bioactive glass, fluoride, hydroxyapatite (HA), and titanium nitride (TiN) [20]. HA remains the most biocompatible, while bioglass shows promise. TiN coatings may reduce bacterial colonization, enhance fibroblast proliferation, and improve mechanical properties [21].
The use of DLC film on screws offers another perspective on the use of coatings, serving as a solid lubricant in the fixation of prostheses and aiming for the perfect coupling of prosthetic components on implants.
The advantage of the use of this type of lubricant is the possibility of incorporating nanoparticles (V, Ti, F, H, Ag) into its microstructure, allowing for an improvement of this film with additional biological properties. The incorporation of silver particles may be particularly advantageous because of its known bactericidal effect [22]. To prevent supra- and sub-gingival biofilm formation and plaque accumulation, allowing antimicrobial function on implant abutments and/or prostheses would be advantageous for the prevention of peri-implantitis, which would subsequently increase the long-term success of the implant [23]. A suitable deposition method of DLC coating containing silver nanoparticles is the plasma enhanced chemical vapor deposition [24].
Implants with conical connections are generally manufactured with a difference in the angles of the conicities between the implant and the abutment. This fact directly influences the behavior of the implant system in general, the size of the microgap, the tension generated in the bone tissue, the loss of preload of the screw, and, in particular, the removal torque [25]. Tapered implants show advantages in low-density bone and immediate loading scenarios, increasing primary stability and minimizing stability loss at compression sites [26]. Research on dental implant taper angles suggests that increasing the abutment taper angle can significantly improve fracture resistance, with 8° and 10° angles showing higher fracture forces compared to 6° [27]. When comparing internal conical connections with different taper angles (5.4°, 12°, 45°, and 60°), no significant differences were found in bacterial leakage under dynamic loading conditions [28].
This study aimed to cover the prosthetic abutments of two different conical connections with DLC nanofilms to evaluate their effect on reverse torque after masticatory cycling.
The null hypotheses were:
- There is no influence of the presence of films on reverse torque after mechanical cycling. Reverse torque is a critical parameter in assessing the long-term stability of dental implants, as it reflects the ability of the abutment to resist loosening under functional loads. By testing this null hypothesis, the study aimed to determine whether the application of nanofilms introduces any beneficial or detrimental effects on reverse torque, which could influence clinical outcomes.
- DLC coating does not present different mechanical behavior compared to silver nanoparticle-doped DLC coating. This hypothesis was formulated to compare the mechanical performance of two different types of coatings: pure DLC and silver-doped DLC. Silver doping is known for its antimicrobial properties, but it is important to evaluate whether adding silver nanoparticles affects the mechanical integrity of the coating, particularly in terms of reverse torque after mechanical cycling. By examining this hypothesis, this study sought to clarify whether silver doping compromises the mechanical benefits of DLC or enhances them without negatively impacting reverse torque stability.
- The DLC films do not interfere with reverse torque regardless of abutment wall angulations (8° and 11°). The angulation of the abutment walls can influence the mechanical interaction between the abutment and the implant, potentially affecting the distribution of stresses and the overall stability of the connection. This hypothesis was crucial to determine whether the mechanical benefits or potential drawbacks of DLC films are consistent across different abutment designs, or if they are dependent on specific geometric factors.
2. Materials and Methods
2.1. Samples
Seventy-eight internal conical-type abutments were randomly distributed into six groups (n = 13) according to two variables: wall angulations (8° and 11°) and surface treatment (C, control group without coating; DLC, coated with DLC film; DLC-Ag, coated with silver nanoparticles doped DLC).
Thirty-nine solid abutments (internal conical 8°, Ø4.0 × 7.0 − thread M2.0) CMAC 7.0 − batch: 153012 (Titaniumfix—São José dos Campos, SP, Brazil) and thirty-nine direct abutments (11° internal conical, Ø4.0 × 5.5 − thread M1.6) 406.015 − batch: 098510 (Titaniumfix) were used.
Thirty-nine internal octagon implants (Ø4.0 × 13.0) with internal conical 8° abutments and thirty-nine double hexagon implants (Ø4.0 × 13.0) with internal conical 11° abuments, both manufactured by Titaniumfix, were used.
The implants were inserted in a polyurethane (elasticity modulus of 3.6 GPa—F16, AXSON, São Paulo, Brazil) cylindrical sample, positioned through a clamp and a metallic matrix to perform perforation and avoid movement. The samples were fixed at an inclination of 30°. A digital caliper (Digimess, São Paulo, Brazil) was used to ensure the height of the installation. All these steps were performed as recommended in the ISO 14801:2007 standard. Briefly, the implants were positioned such that the platform was precisely located at a height of 3.0 ± 0.5 mm above the surface of the fixation block. The installation process used specialized wrenches tailored for the specific implants (codes CMSWA and 612.305, Titaniumfix, São José dos Campos, Brazil), in conjunction with a calibrated torque wrench. A digital caliper (Digimess, Nikeypar, São Paulo, Brazil) was utilized to accurately verify the installation height. Subsequently, the abutments were affixed using a torque wrench explicitly designed for the installation and removal of the prosthetic abutments in use (code CMDTAC, Titaniumfix, São José dos Campos, Brazil), with the tightening torque applied via a digital torque wrench (TQ-680, Instrutherm, São Paulo, Brazil) featuring a precision of 0.01 Ncm. The tightening torque was administered following the manufacturer’s specifications, applying 32 Ncm for the solid abutment and 20 Ncm for the direct abutment. Ten minutes after the initial tightening, the same torque values were reapplied. Upon achieving the desired tightening torque, the hemispherical loading devices were meticulously positioned on the abutments.
2.2. Film Deposition and Abutments Installation
The films were deposited over the abutments (threads and base) via pulsed DC-discharged plasma-enhanced vapor deposition (PECVD) at 20 kHz.
After the substrate cleansing process (argonium plasma, flow 20 sccm) for 40 min at 7.5 × 10−5 Torr), a silicon carbon-rich thin film was deposited over the samples as an interlayer [29], using hexamethyldisiloxane (HMDSO, C6H18OSi2) as the precursor gas at 1.0 × 10−2 Torr for 30 min. After this period, a transition layer was deposited using a mixture of HMDSO and methane at a pressure of 1.6 × 10−1 Torr for 10 min.
For the deposition of the DLC nanofilm itself, the HMDSO flow was closed, and the methane flow was maintained at 13 sccm and the argon flow at 5 sccm for 1 h and 30 min, at a pressure of 1.1 × 10−1 Torr (groups DLC8 and DLC11).
Before the deposition of silver-doped DLC film, the silver–hexane solution (30–50 nm) was stirred in ultrasound for 15 min to disperse particles homogeneously in the solution. The same cleaning and transition layer deposition steps were performed. The silver-doped DLC film deposition started; the hexane with silver nanoparticles flow was maintained at 12 sccm and the argon flow at 5 sccm for 1 h and 30 min, at a pressure of 8 × 10−2 Torr (DLC-Ag8 and DLC-Ag11). The deposition power was maintained at around 200 w. The cathodic tension and the electric current were kept constant during the entire deposition process.
After all the previous steps, each abutment (C8, C11, DLC8, DLC11, DLC-Ag8, DLC-Ag11) was fixed over proper implants. The abutments were installed using a digital torque meter (TQ-680, Instrutherm, São Paulo, Brazil) according to the manufacturer’s instructions (32 Ncm for 8° solid abutment and 20 Ncm for 11° direct abutment). Ten minutes later, additional screwing was performed with the same torque value.
Hemispheric loading devices were machined from stainless steel at A.S. Technology Comp. Esp. Ltda. (São José dos Campos, Brazil), according to the parameters described in ISO 14801:2007. The devices were custom-designed and machined for each abutment model to ensure a perfect fit and to avoid movement.
2.3. Mechanical Cycling and Reverse Torque Analysis
These hemispherical loading devices were positioned over the abutments, and the set was subjected to mechanical cycling (ER-11000 Plus, Erios, São Paulo, Brazil) at 2 Hz for 2 × 106 cycles, with samples immersed in distilled water (n = 13). The sample size was based on a previous study by Figueiredo et al. [30], which adopted a significance level of 5% and a beta power of 80% using the Bonding test data, and determined that a total of at least 8 samples were needed. The frequency and number of adopted cycles were followed according to the parameters described in the ISO 14801:2007 norm. The applied load was 120 Ncm, which is equivalent to the average physiological masticatory load. The tip used for load application had a flat end, which provided a stable contact point on the hemispherical loading device, as also specified by the ISO 14801:2007 norm. At the end of the cycling, the samples were removed from the cycler, and reverse torque values were registered using the same digital torque meter (TQ-680).
Two methods were adopted for data analysis. The first method considered the absolute difference (Ncm) by subtracting the reverse torque (Tr) from the insertion torque (Ti). The second method calculated the relative difference (%) by dividing the absolute difference by the Ti.
2.4. Morphological Analysis of Abutments Adaptation
The samples (C, DLC, and DLC-Ag non-cycled and C cycled, DLC cycled and DLC-Ag cycled) (n = 3) were analyzed via scanning electron microscopy (SEM Inspect S50, FEI Company, Orlando, FL, USA) in BSE mode with 1000× magnification. For this analysis, the implants with their respective fixed abutments were cut along their axis until the fixing screw was exposed. Then, they were sanded with an automatic sanding machine polisher using 400- and 1200-grit wet sandpaper and cleansed with alcohol in an ultrasound bath (5 min).
2.5. Characterization of Films
The film thicknesses were obtained by measuring the steps formed between the covered and uncovered surface of additional silicon samples positioned in the plasma deposition chamber, using an Alpha-Step 500 profilometer (Tencor, San Diego, CA, USA).
During the process of film deposition over the abutments, additional titanium plate samples (14 × 14 mm) were prepared and coated with the different nanofilms for analysis and characterization. The scratch test was performed using a tribometer (CETR Biomedical Tribometer, CETR-Bruker, Campbell, CA, USA). The adherence of the film to the substrate and the coefficient of friction were analyzed on two coated plates (n = 2) at 24.8 °C and 46% relative humidity. The test was carried out at the speed of 0.1 mm/s with a progressive load from 0.2 Ncm to 20 Ncm over a 100 mm area using a Rockwell-type diamond tip (Rockwell C, CETR-Bruker, Campbell, CA, USA). The initial failure point was determined as the point at which a crack occurred, or film delamination was observed. Three tests were carried out per sample, aiming to determine the critical load.
The coefficient of friction analysis was performed using a spherical steel tip (4 mmᴓ) with a progressive load of 2 Ncm (5 mm/s, 5 mm during 1000 s).
Roughness analysis (Ra) was carried out using a digital optical profilometer (WYKI NT 1100, Vecco, New York, NY, USA) in VSI mode at 20× magnification. Five Ra measurements were made in each sample (n = 2) for each surface treatment (C, DLC, and DLC-Ag).
The chemical composition and structure of the films were analyzed via energy-dispersive spectroscopy (EDS) and Raman scattering spectroscopy (Renishaw 2000, Renishaw, New Mills, UK), which operates with a scattered argonium laser at 514 nm.
2.6. Statistical Analysis
A significance level of 5% was adopted. The GraphPad Prism 6 software program (GraphPad Software, San Diego, CA, USA) was used to perform statistical analysis. The data were tested for normality using the the D’Agostino–Pearson normality test. Reverse torque tests were analyzed using the Kruskal–Wallis test and Dunn’s multiple comparison test to evaluate the effects of the nanofilms. The Mann–Whitney test was used to determine differences in the mechanical behavior of each wall angulation. The methodology was reviewed by an independent statistician.
3. Results
Some groups of data did not present a normal distribution according to the D’Agostino–Pearson normality test.
The results for absolute difference (Ncm) and relative difference (%) are presented in Table 1 and Figure 1. Positive values indicate torque loss and negative values indicate torque gain. The Kruskal–Wallis test (for groups 8° and 11°, respectively) demonstrated significant differences for both groups in terms of absolute difference (p = 0.0396; p = 0.0017) and relative difference (p = 0.0355; p = 0.0014).

Table 1.
Medians from the statistical analysis of the absolute difference values (Ncm) and the relative values (%). p-values, obtained by searching for the effect of conicity values using the Mann–Whitney test are presented.
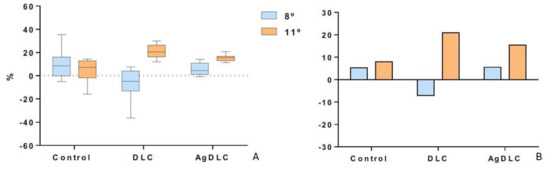
Figure 1.
Boxplot of the relative difference (%) of the torque values (A). Column graph of the average relative difference (%) of the torque values (B).
Considering the coatings, according to Dunn’s multiple comparisons test, differences occurred between C and DLC groups for both 8° and 11°. In the internal conical connection with an angle of 8°, the DLC group exhibited the lowest torque loss. In the internal conical connection with an angle of 11°, the DLC group exhibited the highest torque loss.
According to the Mann–Whitney test, torque loss values did not present differences between the control groups with 8° and 11° wall angulations. In the coated groups, the internal conical connection with an angle of 11°, coated with both nanofilms, demonstrated the highest torque loss values.
Morphological Analysis of Abutment Adaptation
Deformations observed on the threads of abutment screws and internal threads of implants, apart from the internal connections of implants, were verified. The samples presented a perfect adaptation of the pillar–implant interface for both cycled and non-cycled groups, and there were no qualitative differences in the thread images (Figure 2).
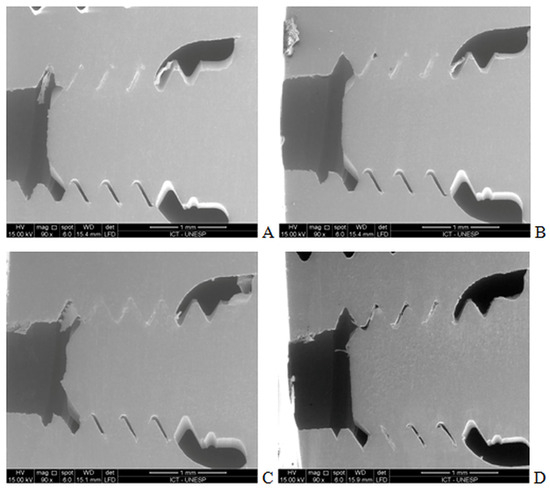
Figure 2.
Thread images of C8 pre-cycling (A), post-cycling (B), DLC8 pre-cycling (C), and post-cycling (D) at 90× magnification in SE mode.
The thickness of the DLC nanofilm was 1.58 μm and the thickness of the DLC-Ag nanofilm was 2.91 μm. Since the deposition time was the same for both films, this difference in thickness is probably due to the fact that each molecule of methane, the precursor gas for the DLC film, has only one carbon atom, while hexane, the precursor gas for the AgDLC film, has six carbon atoms.
Table 2 presents data from the scratch test. The results demonstrated that, during the test, the film kept its adherence to the entire interior thread and was removed only in one sample of the DLC-Ag at an applied force of 9.7 N. Thread analysis revealed a shell-format film saturation, suggesting good adherence to the substrate. The mean values of the scratch test were lower for the DLC-Ag nanofilm compared to the DLC nanofilm.

Table 2.
Scratch test values for DLC and DLC-Ag. The moment of the first crack was LC1 and the first delamination was LC2.
Regarding the coefficient of friction (COF), performed using a spherical steel tip (4 mmᴓ) with a progressive load of 2 Ncm, the control group presented the highest COF (0.46 ± 0.14), followed by DLC (0.15 ± 0.2) and DLC-Ag (0.12 ± 0.2). The low coefficient of friction and high hardness of the DLC layer offered some benefits in preventing the deformation of the implant top.
The average surface roughness measurements (Ra—mm), carried out using a digital optical profilometer, were 0.4 ± 0.02 (C), 0.4 ± 0.07 (DLC), and 0.3 ± 0.01 (DLC-Ag). Ra represents the average between the values of the peaks and valleys present in the tested area.
Figure 3 shows the Raman spectra of DLC and DLC-Ag. The Raman spectra revealed that the G band was larger in the DLC nanofilm, indicating a higher concentration of sp2 hybridization in the silver-doped film. The D bands did not present significant changes.
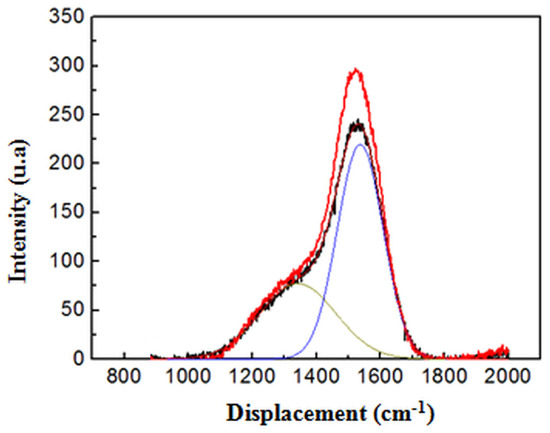
Figure 3.
Raman spectra of silver doped Ag-DLC (in black) and undoped DLC (in red). The presence of silver on the film changes the position and the intensities of the bands G that compose each spectrum. Raman spectra revealed that the G band is larger in the DLC film. The spectra include the fitting curves. Blue curve indicates the Lorentzian curves for the G-band without Gaussian convolution. Yellow curve indicates the Lorentzian curves for the D-band without the same Gaussian convolution.
EDS quantitative analysis demonstrated an atomic percentage of 90.5% C, 2.4% Si, 7.1% Ti, and 0.5% Ag in the DLC-Ag group, and 89.0% C, 2.1% Si, and 8.5% Ti in the DLC group.
4. Discussion
This in vitro assessment evaluated the effect of taper angles on the internal conical connections of implant systems and two different DLC nanofilms on the reverse torque of abutment screws after load cycling. We obtained great results with both DLC and DLC-Ag nanofilms in the internal conical connection with an angle of 8°. Torque loss values were lower than the values of the control group. We only accepted the second null hypothesis, which stated that DLC coating does not present a different mechanical behavior compared to silver nanoparticle-doped DLC coating.
The results of the present study, particularly the differences in coating types (DLC vs. silver-doped DLC) and abutment angulations (8° vs. 11°), can have several potential impacts on clinical outcomes. The DLC8 group showed superior reverse torque compared to other groups, including those with silver-doped DLC. This suggests that the DLC coating might provide better mechanical stability, reducing the risk of abutment loosening. In clinical practice, this could translate to longer-lasting implant stability, less frequent need for adjustments or retightening, and a lower risk of complications related to screw loosening, ultimately reducing overall healthcare costs and improving patient satisfaction.
DLC coatings are known for their hardness and wear resistance [17], which can reduce material wear over time. In contrast, the addition of silver nanoparticles, which could offer antimicrobial properties [22] and reduce the risk of peri-implantitis, altered the mechanical properties of the coating. The silver-doped DLC demonstrates lower mechanical stability, which accelerates the wear and potentially shortens the lifespan of the abutment, increasing the need for earlier intervention or replacement. This study showed that 11° abutments experienced higher torque loss than 8° abutments. Clinically, this could mean that implants with a steeper taper (11°) might be more prone to loosening over time, especially if not coupled with an optimal coating. This could lead to a higher likelihood of abutment failure, necessitating more frequent follow-ups, retightening, or even implant replacement.
Bone density is a critical factor in the success of dental implants and the planning of treatment. Various preoperative methods exist for assessing jawbone density, many of which show strong correlations with clinical outcomes [31]. Computed tomography provides valuable insights into bone quality before implant placement, highlighting significant variations in density across different oral regions [32]. The anterior mandible typically exhibits the highest bone density, followed by the anterior maxilla, posterior mandible, and posterior maxilla [32]. Additionally, bone density varies significantly between individuals and even within different areas of the same jaw [33]. Factors such as bone quality, bone quantity, and overall patient health are critical to implant success [34]. While it is generally observed that women have a lower bone density than men, no significant correlation has been established between bone density and patient age [33]. These findings underscore the importance of carefully selecting the abutment angulation and conducting a patient-specific assessment to customize implant treatment according to each patient’s unique anatomical and functional needs. For example, a patient with higher occlusal forces might benefit more from an 8° abutment with a diamond-like carbon (DLC) coating, which can minimize the risk of abutment loosening and enhance long-term stability.
We proved that the internal conical angle of 11° resulted in higher torque loss values, consequently enhancing the chance of implant failure. Although clinical studies have verified that a low torque (less than 30 Ncm) is sufficient to ensure dental implant osseointegration [35], and all studies reviewed by Lemos et al. [36] reported high survival rates irrespective of the insertion torque, we suspect that the torque loss in the 11° internal cone was related to the insertion torque of 20 Ncm used in our study, which is considered a low torque.
The thickness of DLC coatings plays a significant role in their performance, with thicker coatings providing better friction reduction under elastohydrodynamic lubrication conditions [37]. Additionally, DLC coatings can serve as an effective galvanic corrosion barrier between titanium abutments and nickel–chromium superstructures without compromising the fit and integrity of prosthetic assemblies [38]. While DLC coatings have shown potential to enhance the reliability of dental implant-supported restorations, their effectiveness may vary depending on the coating method and thickness [37,39].
A significant difference in the implant survival rates (14% failure rates for regular or low insertion torque as compared with 0% for high insertion torque) has been reported in implants with immediate loading [40]. Additionally, the torque loss observed in the 11° group here agrees with Ottoni et al. [41], who reported that low insertion torque (20 Ncm) is associated with a high risk of failure (9 of 10 implants failed) in implant-supported single crowns.
Based on previous studies [42,43], which showed that low-frequency cycling is more effective than continuous frequency increase cycling, a change in the ISO 14801 norm was adopted in the methods of the present study. As expected, the results demonstrated a decrease in the reverse torque values of all groups after mechanical cycling, which indicates a decrease in the torque of the screws. The DLC8 group had the lowest reverse torque loss.
The promising mechanical behavior of the DLC8 group in the present study is in accordance with previous studies [44]. Higher reverse torque values for abutment screws with DLC coating have been reported [43]. The main difference from the present study was the cycle type used. The authors performed cyclic loading using a thermomechanical testing device to represent approximately one year of clinical usage [44]. In contrast, this study used 2 × 106 cycles at 2 Hz and 120 N and water immersion, to simulate two and a half years of masticatory function [45]. In external-hex implants, the DLC coating did not influence torque loss when compared to the control group [46].
Research on the mechanical cycling of implant–abutment connections reveal significant effects on their stability and performance. Short-term cycling (36 × 104 cycles) leads to improved adaptation and sealing ability, with decreased microgap size in Morse taper connections [47]. Some studies employed long-term cyclic loading using five million cycles as the upper limit [47,48,49]. Fatigue limits varied across designs, ranging from 210–240 N for different connections to 300–800 N in another study [48]. Internal connections generally showed higher fatigue strength than external ones, while external hex designs exhibited higher static strength [49]. Zirconia abutments demonstrated higher fatigue strength than titanium in external hex configurations [49].
Some studies have evaluated the performance of coated dental prosthetic abutments under simulated masticatory loads and torque tests. DLC coatings on abutments have shown mixed results. One study found that DLC coating reduced screw loosening after mechanical cycling [46]. However, another study reported no improvement in torque maintenance for DLC-coated screws with or without diamond nanoparticles [50]. Bacchi et al. (2015) [51] observed that conventional titanium screws maintained higher loosening torque values than DLC-coated screws after cyclic loading. For zirconia abutments, a study found that ceramic coating did not significantly affect their mechanical behavior under static and dynamic loading conditions [52]. These studies demonstrate that while various coatings have been investigated for dental prosthetic abutments, their effectiveness in maintaining torque and mechanical stability varies, highlighting the need for further research in this area.
As a result of the abutment threads analysis, none of the groups presented changes in the adaptation, wear, or deformation after mechanical cycling, confirming results from previous literature [53]. Screw joint failure begins with external functional loading, which gradually reduces the preload in the joint. The DLC layer’s lower friction coefficient and greater hardness compared to pure titanium may help prevent implant abrasion, erosion, and deformation [54]. The superior torque results in the DLC8-coated groups can also be explained by this. Dziedzic et al. [55] reported that the carbon coating on screw threads reduced interface friction and enhanced preload values, thereby increasing the clamping force between the abutment and the implant platform. The DLC’s low friction coefficient enables greater preload with the same torque, thereby improving joint stability.
The factors that influence the settling effect and, consequently, screw loosening include preload, the coefficient of friction, and retightening [56]. The coefficient of friction in the DLC and DLC-Ag groups was lower than that obtained in the control group. In agreement, Raman spectra in the present study demonstrated higher sp2 hybridization concentrations in the DLC-Ag nanofilm. Tribological tests have proven that coatings with high sp2 content tend to have lower friction coefficients in dry conditions [57]. Despite differences in the coefficient of friction, our roughness measurements, expressed as Ra values, were similar in all groups. This coefficient depends not only on the roughness of the contacting surfaces, but also on loading, the hardness of the threads, and the presence, quantity, and quality of the lubricant on the surfaces. When decreased to appropriate values, the friction coefficient increases the preload and decreases the chance of screw loosening [56]. The DLC coating is an alternative method to prevent screw loosening [44].
Peri-implant diseases present a prevalence rate of 43% across Europe and 22% across South and North America [58]. Both peri-implant mucositis and peri-implantitis have an infectious etiology based on the accumulation of a biofilm composed of periodontal pathogens on the implant surface [59]. EDS analysis confirmed the successful deposition of a silver-doped film over our samples, thus our antibacterial coating on abutments could be advantageous in preventing peri-implantitis and implant failures.
This study presents certain methodological limitations that could be addressed in future research. Regarding the selection of implants, to standardize the clinical scenario, implants with the same external diameter (4.0 mm) were chosen. However, these implant models exhibit specific design characteristics that influence this standardization. The implant with an 8° taper (c-fix; Titaniumfix, Brazil) features an M2.0 internal thread (2 mm diameter) and an octagonal indexing system. In contrast, the implant with an 11° taper (b-fix; Titaniumfix, Brazil) has an M1.6 internal thread (1.6 mm diameter) and a dual hexagonal indexing system. The indexing systems impact the area occupied by the taper, which may affect the active area of each implant model. Consequently, the load distribution across each thread differs, given the variation in the threaded area and active taper area in each model. Future studies should consider standardizing the internal thread diameter and selecting implants with different diameters to determine if the active taper area associated with thread diameter influences reverse torque values after mechanical cycling. The tribological analyses conducted were qualitative only. The results for the coefficient of friction, average roughness, and scratch hardness were not subjected to statistical analysis. More detailed studies are necessary to investigate whether there is a correlation between tribological results and reverse torque values. Another analysis that was not statistically tested involved scanning electron microscopy images. The assessment of taper adaptation and thread wear was purely visual, and quantitative evaluations are required for more significant and conclusive results. Additionally, regarding the adaptation of the abutments, the application of DLC and AgDLC films was carried out across the entire active area of the abutments (taper and threads), but the effect of the films on abutment adaptation was only evaluated after fatigue testing. The differences in reverse torque values between coated and uncoated abutments may not have been as apparent due to potential misadaptation in the taper area of the abutments with DLC and AgDLC films, which could have influenced the reverse torque values. Future studies should examine the thickness of the films and their influence on taper adaptation before fatigue testing to achieve film thicknesses that do not affect adaptation.
5. Conclusions
Based on the findings of this in vitro study, it can be concluded that the use of diamond-like carbon (DLC) coatings, particularly with an 8° abutment angulation, significantly enhances the mechanical stability of abutment screws by minimizing torque loss after load cycling. The DLC coating proved more effective than silver-doped DLC, which exhibited reduced mechanical stability. These results suggest that DLC-coated abutments may offer greater implant longevity and fewer complications related to screw loosening in clinical settings. However, the study’s limitations include the specific conditions under which the tests were conducted, which may not fully replicate the complexities of the oral environment. Further in vivo research is necessary to validate these findings and assess the long-term clinical performance of DLC coatings in various implant scenarios.
Author Contributions
A.V.P.C.: Methodology, Investigation, Formal analysis, Data curation, Writing—original draft, Visualization, Project administration; V.M.G.d.F.: Methodology, Data curation; Writing—original draft; L.L.F.: Methodology, Software, Investigation, Formal analysis, Data curation, Writing—original draft, Visualization, Project administration; A.d.M.S.: Conceptualization, Validation, Writing—review and editing, Project administration; M.G.O.: Conceptualization, Resources, Supervision; J.R.C.d.Q.: Investigation, Formal analysis, Writing—review and editing; A.S.d.S.S.: Conceptualization, Validation, Resources, Writing—review and editing, Supervision, Project administration, Funding acquisition; R.F.d.P.: Software, Investigation, Formal analysis, Writing—review and editing; L.N.J.: Conceptualization, Validation, Resources, Writing—review and editing, Supervision, Project administration, Funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
Titaniumfix (São José dos Campos, Brazil) provided the implants of this study.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data will be made available upon request.
Conflicts of Interest
There are no conflicts of interest with this research.
References
- Ceruso, F.M.; Barnaba, P.; Mazzoleni, S.; Ottria, L.; Gargari, M.; Zuccon, A.; Bruno, G.; Di Fiore, A. Implant-Abutment Connections on Single Crowns: A Systematic Review. Oral. Implantol. 2017, 10, 349–353. [Google Scholar] [CrossRef]
- Bagegni, A.; Spies, B.C.; Kern, M.; Hazard, D.; Kohal, R. The Influence of Prosthetic Crown Height and Implant-Abutment Connection Design Selection on the Long-Term Implant-Abutment Stability: A Laboratory Study. J. Mech. Behav. Biomed. Mater. 2021, 113, 104095. [Google Scholar] [CrossRef]
- Passos, S.P.; Gressler May, L.; Faria, R.; Özcan, M.; Bottino, M.A. Implant-Abutment Gap versus Microbial Colonization: Clinical Significance Based on a Literature Review. J. Biomed. Mater. Res. Part B Appl. Biomater. 2013, 101, 1321–1328. [Google Scholar] [CrossRef]
- Gois Filho, D.M.; de Gois-Santos, V.T.; Silva, R.S.; Marqueti, A.C.; Cortes, A.R.G.; Trento, C.L. Evaluation of Sealing between Abutment and Inner Connection of Cone Morse Dental Implant. Clin. Lab. Res. Dent. 2018, 2018, 1–6. [Google Scholar] [CrossRef]
- Kim, B.J.; Yeo, I.S.; Lee, J.H.; Kim, S.K.; Heo, S.J.; Koak, J.Y. The effect of screw length on fracture load and abutment strain in dental implants with external abutment connections. Int. J. Oral Maxillofac. Implant. 2012, 27, 820–823. [Google Scholar]
- Jo, J.Y.; Yang, D.S.; Huh, J.B.; Heo, J.C.; Yun, M.J.; Jeong, C.M. Influence of Abutment Materials on the Implant-Abutment Joint Stability in Internal Conical Connection Type Implant Systems. J. Adv. Prosthodont. 2014, 6, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Jörn, D.; Kohorst, P.; Besdo, S.; Rücker, M.; Stiesch, M.; Borchers, L. Influence of Lubricant on Screw Preload and Stresses in a Finite Element Model for a Dental Implant. J. Prosthet. Dent. 2014, 112, 340–348. [Google Scholar] [CrossRef]
- dos Santos, M.V.; Elias, C.N.; Cavalcanti Lima, J.H. The Effects of Superficial Roughness and Design on the Primary Stability of Dental Implants. Clin. Implant. Dent. Relat. Res. 2011, 13, 215–223. [Google Scholar] [CrossRef]
- Mangano, C.; Mangano, F.; Piattelli, A.; Iezzi, G.; Mangano, A.; La Colla, L. Prospective Clinical Evaluation of 1920 Morse Taper Connection Implants: Results after 4 Years of Functional Loading. Clin. Oral Implant. Res. 2009, 20, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Stüker, R.A.; Teixeira, E.R.; Beck, J.C.P.; Da Costa, N.P. Preload and Torque Removal Evaluation of Three Different Abutment Screws for Single Standing Implant Restorations. J. Appl. Oral Sci. 2008, 16, 55–58. [Google Scholar] [CrossRef]
- Winkler, S.; Ring, K.; Ring, J.D.; Boberick, K.G. Implant Screw Mechanics and the Settling Effect: An Overview. J. Oral Implant. 2003, 29, 242–245. [Google Scholar] [CrossRef]
- Al Jabbari, Y.S.; Fournelle, R.; Ziebert, G.; Toth, J.; Iacopino, A.M. Mechanical Behavior and Failure Analysis of Prosthetic Retaining Screws after Long-Term Use In Vivo. Part 1: Characterization of Adhesive Wear and Structure of Retaining Screws. J. Prosthodont. 2008, 17, 168–180. [Google Scholar] [CrossRef] [PubMed]
- Cerutti-Kopplin, D.; Rodrigues Neto, D.J.; Lins Do Valle, A.; Pereira, J.R. Influence of Reverse Torque Values in Abutments with or without Internal Hexagon Indexes. J. Prosthet. Dent. 2014, 112, 824–827. [Google Scholar] [CrossRef] [PubMed]
- Cerutti-Kopplin, D.; Rodrigues Neto, D.J.; Do Valle, A.L.; Pereira, J.R.; Pinho, L.G.N.D. Reverse Torque Values in Indexed Abutments. J. Res. Dent. 2013, 1, 192. [Google Scholar] [CrossRef][Green Version]
- Martins, C.M.; Ramos, E.V.; Kreve, S.; de Carvalho, G.A.P.; Franco, A.B.G.; de Macedo, L.G.S.; Silva, A.D.M.; Dias, S.C. Reverse Torque Evaluation in Indexed and Nonindexed Abutments of Morse Taper Implants in a Mechanical Fatigue Test. Dent. Res. J. 2019, 16, 110–116. [Google Scholar] [CrossRef]
- Carr, A.B.; Larsen, P.E.; Papazoglou, E.; McGlumphy, E. Reverse torque failure of screw-shaped implants in baboons: Baseline data for abutment torque application. Int. J. Oral Maxillofac. Implant. 1995, 10, 167–174. [Google Scholar]
- Watabe, T.; Amanov, A.; Tsuboi, R.; Sasaki, S. Friction and Fretting Wear Characteristics of Different Diamond-like Carbon Coatings against Alumina in Water-Lubricated Fretting Conditions. J. Nanosci. Nanotechnol. 2013, 13, 8167–8175. [Google Scholar] [CrossRef]
- Malisz, K.; Świeczko-Żurek, B.; Sionkowska, A. Preparation and Characterization of Diamond-like Carbon Coatings for Biomedical Applications—A Review. Materials 2023, 16, 3420. [Google Scholar] [CrossRef]
- Peng, Y.; Peng, J.; Wang, Z.; Xiao, Y.; Qiu, X. Diamond-like Carbon Coatings in the Biomedical Field: Properties, Applications and Future Development. Coatings 2022, 12, 1088. [Google Scholar] [CrossRef]
- Xuereb, M.; Camilleri, J.; Attard, N. Systematic Review of Current Dental Implant Coating Materials and Novel Coating Techniques. Int. J. Prosthodont. 2015, 28, 51–59. [Google Scholar] [CrossRef]
- del Castillo, R.; Chochlidakis, K.; Galindo-Moreno, P.; Ercoli, C. Titanium Nitride Coated Implant Abutments: From Technical Aspects And Soft Tissue Biocompatibility to Clinical Applications. A Literature Review. J. Prosthodont. 2022, 31, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.P.; Hauser-Gerspach, I.; Waltimo, T.; Stritzker, B. Antibacterial Properties of Silver Containing Diamond like Carbon Coatings Produced by Ion Induced Polymer Densification. Surf. Coat. Technol. 2011, 205, 4850–4854. [Google Scholar] [CrossRef]
- Odatsu, T.; Kuroshima, S.; Sato, M.; Takase, K.; Valanezhad, A.; Naito, M.; Sawase, T. Antibacterial Properties of Nano-Ag Coating on Healing Abutment: An in Vitro and Clinical Study. Antibiotics 2020, 9, 347. [Google Scholar] [CrossRef]
- Marciano, F.R.; Bonetti, L.F.; Santos, L.V.; Da-Silva, N.S.; Corat, E.J.; Trava-Airoldi, V.J. Antibacterial Activity of DLC and Ag–DLC Films Produced by PECVD Technique. Diam. Relat. Mater. 2009, 18, 1010–1014. [Google Scholar] [CrossRef]
- Aguirrebeitia, J.; Abasolo, M.; Vallejo, J.; Ansola, R. Dental Implants with Conical Implant-Abutment Interface: Influence of the Conical Angle Difference on the Mechanical Behavior of the Implant. Int. J. Oral Maxillofac. Implant. 2013, 28, e72–e82. [Google Scholar] [CrossRef]
- Tang, C.L.; Zhao, S.K.; Huang, C. Features and Advances of Morse Taper Connection in Oral Implant. Chin. J. Stomatol. 2017, 52, 59–62. [Google Scholar] [CrossRef]
- Wang, K.; Geng, J.; Jones, D.; Xu, W. Comparison of the Fracture Resistance of Dental Implants with Different Abutment Taper Angles. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 63, 164–171. [Google Scholar] [CrossRef]
- Ozdiler, A.; Bakir-Topcuoglu, N.; Kulekci, G.; Isik-Ozkol, G. Effects of Taper Angle and Sealant Agents on Bacterial Leakage Along the Implant-Abutment Interface: An In Vitro Study Under Loaded Conditions. Int. J. Oral Maxillofac. Implant. 2018, 33, 1071–1077. [Google Scholar] [CrossRef]
- Schauer, J.C.; Winter, J. Plasma Deposition of Elastic Wear Resistant Si-C Coatings on Nickel-Titanium for Biomedical Applications. J. Appl. Phys. 2008, 103, 113302. [Google Scholar] [CrossRef]
- de Figueiredo, V.M.G.; de Silva, A.D.M.; Massi, M.; Sobrinho, A.S.D.S.; de Queiroz, J.R.C.; Machado, J.P.B.; Do Prado, R.F.; Junior, L.N. Effect of the Nanofilm-Coated Zirconia Ceramic on Resin Cement Bond Strength. J. Dent. Res. Dent. Clin. Dent. Prospect. 2022, 16, 170–178. [Google Scholar] [CrossRef]
- Molly, L.; Molly, L. Bone Density and Primary Stability in Implant Therapy. Clin. Oral Implant. Res. 2006, 17, 124–135. [Google Scholar] [CrossRef]
- Turkyilmaz, I.; Tözüm, T.F.; Tumer, C. Bone Density Assessments of Oral Implant Sites Using Computerized Tomography. J. Oral Rehabil. 2007, 34, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Di Stefano, D.A.; Arosio, P.; Pagnutti, S.; Vinci, R.; Gherlone, E.F. Distribution of Trabecular Bone Density in the Maxilla and Mandible. Implant. Dent. 2019, 28, 340–348. [Google Scholar] [CrossRef]
- Venkatakrishnan, C.J.; Bhuminathan, S.; Chandran, C.A.R. Dental Implant Insertion Torque and Bone Density—Short Review. Biomed. Pharmacol. J. 2017, 10, 1305–1309. [Google Scholar] [CrossRef]
- Maló, P.; Lopes, A.; de Araújo Nobre, M.; Ferro, A. Immediate Function Dental Implants Inserted with Less than 30 N·cm of Torque in Full-Arch Maxillary Rehabilitations Using the All-on-4 Concept: Retrospective Study. Int. J. Oral Maxillofac. Surg. 2018, 47, 1079–1085. [Google Scholar] [CrossRef]
- Lemos, C.A.A.; Verri, F.R.; de Oliveira Neto, O.B.; Cruz, R.S.; Luna Gomes, J.M.; da Silva Casado, B.G.; Pellizzer, E.P. Clinical Effect of the High Insertion Torque on Dental Implants: A Systematic Review and Meta-Analysis. J. Prosthet. Dent. 2021, 126, 490–496. [Google Scholar] [CrossRef]
- Björling, M.; Larsson, R.; Marklund, P. The Effect of DLC Coating Thickness on Elstohydrodynamic Friction. Tribol. Lett. 2014, 55, 353–362. [Google Scholar] [CrossRef]
- Ozkomur, A.; Erbil, M.; Akova, T. Diamondlike Carbon Coating as a Galvanic Corrosion Barrier between Dental Implant Abutments and Nickel-Chromium Superstructures. Int. J. Oral Maxillofac. Implant. 2013, 28, 1037–1047. [Google Scholar] [CrossRef][Green Version]
- Bordin, D.; Coelho, P.G.; Bergamo, E.T.P.; Bonfante, E.A.; Witek, L.; Del Bel Cury, A.A. The Effect of DLC-Coating Deposition Method on the Reliability and Mechanical Properties of Abutment’s Screws. Dent. Mater. 2018, 34, e128–e137. [Google Scholar] [CrossRef]
- Cannizzaro, G.; Leone, M.; Torchio, C.; Viola, P.; Esposito, M. Immediate versus Early Loading of 7-Mm-Long Flapless-Placed Single Implants: A Split-Mouth Randomised Controlled Clinical Trial. Eur. J. Oral Implant. 2008, 1, 277–292. [Google Scholar]
- Ottoni, J.M.P.; Oliveira, Z.F.L.; Mansini, R.; Cabral, A.M. Correlation between Placement Torque and Survival of Single-Tooth Implants. Int. J. Oral Maxillofac. Implant. 2005, 20, 769–776. [Google Scholar]
- Karl, M.; Kelly, J.R. Influence of Loading Frequency on Implant Failure under Cyclic Fatigue Conditions. Dent. Mater. 2009, 25, 1426–1432. [Google Scholar] [CrossRef]
- Lee, C.K.; Karl, M.; Kelly, J.R. Evaluation of Test Protocol Variables for Dental Implant Fatigue Research. Dent. Mater. 2009, 25, 1419–1425. [Google Scholar] [CrossRef]
- Colpak, E.D.; Gumus, H.O. Effect of Surface Modifications of Abutment Screws on Reverse Torque Values: An In Vitro Study. Int. J. Prosthodont. 2020, 33, 401–409. [Google Scholar] [CrossRef]
- Rosentritt, M.; Behr, M.; Gebhard, R.; Handel, G. Influence of Stress Simulation Parameters on the Fracture Strength of All-Ceramic Fixed-Partial Dentures. Dent. Mater. 2006, 22, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Corazza, P.H.; De Moura Silva, A.; Cavalcanti Queiroz, J.R.; Salazar Marocho, S.M.; Bottino, M.A.; Massi, M.; Rodrigo, R.O. Carbon Film Coating of Abutment Surfaces: Effect on the Abutment Screw Removal Torque. Implant. Dent. 2014, 23, 434–438. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Carvalho Serra, R.D. Load Fatigue Performance of Conical Implant-Abutment Connection: Effect of Torque Level and Interface Junction. Minerva Stomatol. 2015, 64, 1–7. [Google Scholar]
- Thomé, G.; Gomes, A.; de Moura, M.; Beng, C.; Trojan, L. Evaluation of the Mechanical Reliability of Different Implant-Abutment Connections for Single Crowns According to the ISO 14801 Fatigue Test Protocol. Int. J. Oral Maxillofac. Implant. 2021, 36, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Park, I.S.; Won, S.Y.; Bae, T.S.; Song, K.Y.; Park, C.W.; Eom, T.G.; Jeong, C.M. Fatigue Characteristics of Five Types of Implant-Abutment Joint Designs. Met. Mater. Int. 2008, 14, 133–138. [Google Scholar] [CrossRef]
- Lepesqueur, L.; Figueiredo, V.; Ferreira, L.; Sobrinho, A.; Massi, M.; Bottino, M.; Nogueira Junior, L. Coating Dental Implant Abutment Screws with Diamondlike Carbon Doped with Diamond Nanoparticles: The Effect on Maintaining Torque After Mechanical Cycling. Int. J. Oral. Maxillofac. Implant. 2015, 30, 1310–1316. [Google Scholar] [CrossRef][Green Version]
- Bacchi, A.; Regalin, A.; Brilhante Bhering, C.L.; Alessandretti, R.; Spazzin, A.O. Loosening Torque of Universal Abutment Screws after Cyclic Loading: Influence of Tightening Technique and Screw Coating. J. Adv. Prosthodont. 2015, 7, 375–379. [Google Scholar] [CrossRef]
- Jiménez-Melendo, M.; Llena-Blasco, O.; Bruguera, A.; Llena-Blasco, J.; Yáñez-Vico, R.M.; García-Calderón, M.; Vaquero-Aguilar, C.; Velázquez-Cayón, R.; Gutiérrez-Pérez, J.L.; Torres-Lagares, D. Mechanical Behavior of Single-Layer Ceramized Zirconia Abutments for Dental Implant Prosthetic Rehabilitation. J. Clin. Exp. Dent. 2014, 6, e485–e490. [Google Scholar] [CrossRef] [PubMed]
- Basílio, M.d.A.; Butignon, L.E.; Arioli Filho, J.N. Effectiveness of Screw Surface Coating on the Stability of Zirconia Abutments after Cyclic Loading. Int. J. Oral Maxillofac. Implant. 2012, 27, 1061–1067. [Google Scholar]
- Kim, S.K.; Lee, J.B.; Koak, J.Y.; Heo, S.J.; Lee, K.R.; Cho, L.R.; Lee, S.S. An Abutment Screw Loosening Study of a Diamond Like Carbon-Coated CP Titanium Implant. J. Oral Rehabil. 2005, 32, 346–350. [Google Scholar] [CrossRef] [PubMed]
- Silva, D.; Dziedzic, M.; Nhata, J.; Jamcoski, V.H.; Dziedzic, M. Assessment of Preload in Carbon Coated Prosthetic Screws. RSBO 2012, 9, 137–142. [Google Scholar]
- Bulaqi, H.A.; Mousavi Mashhadi, M.; Safari, H.; Samandari, M.M.; Geramipanah, F. Dynamic nature of abutment screw retightening: Finite element study of the effect of retightening on the settling effect. J. Prosthet. Dent. 2015, 113, 412–419. [Google Scholar] [CrossRef]
- Love, C.A.; Cook, R.B.; Harvey, T.J.; Dearnley, P.A.; Wood, R.J.K. Diamond like Carbon Coatings for Potential Application in Biological Implants—A Review. Tribol. Int. 2013, 63, 141–150. [Google Scholar] [CrossRef]
- Fu, J.H.; Wang, H.L. Breaking the Wave of Peri-Implantitis. Periodontology 2000 2020, 84, 145–160. [Google Scholar] [CrossRef]
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-Implant Diseases and Conditions: Consensus Report of Workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S313–S318. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).