Omics-Based Approaches for the Characterization of Pompe Disease Metabolic Phenotypes
Abstract
:Simple Summary
Abstract
1. Introduction
2. Omics Studies Directed to the Identification of Metabolic Pompe Disease Diagnostic Biomarkers
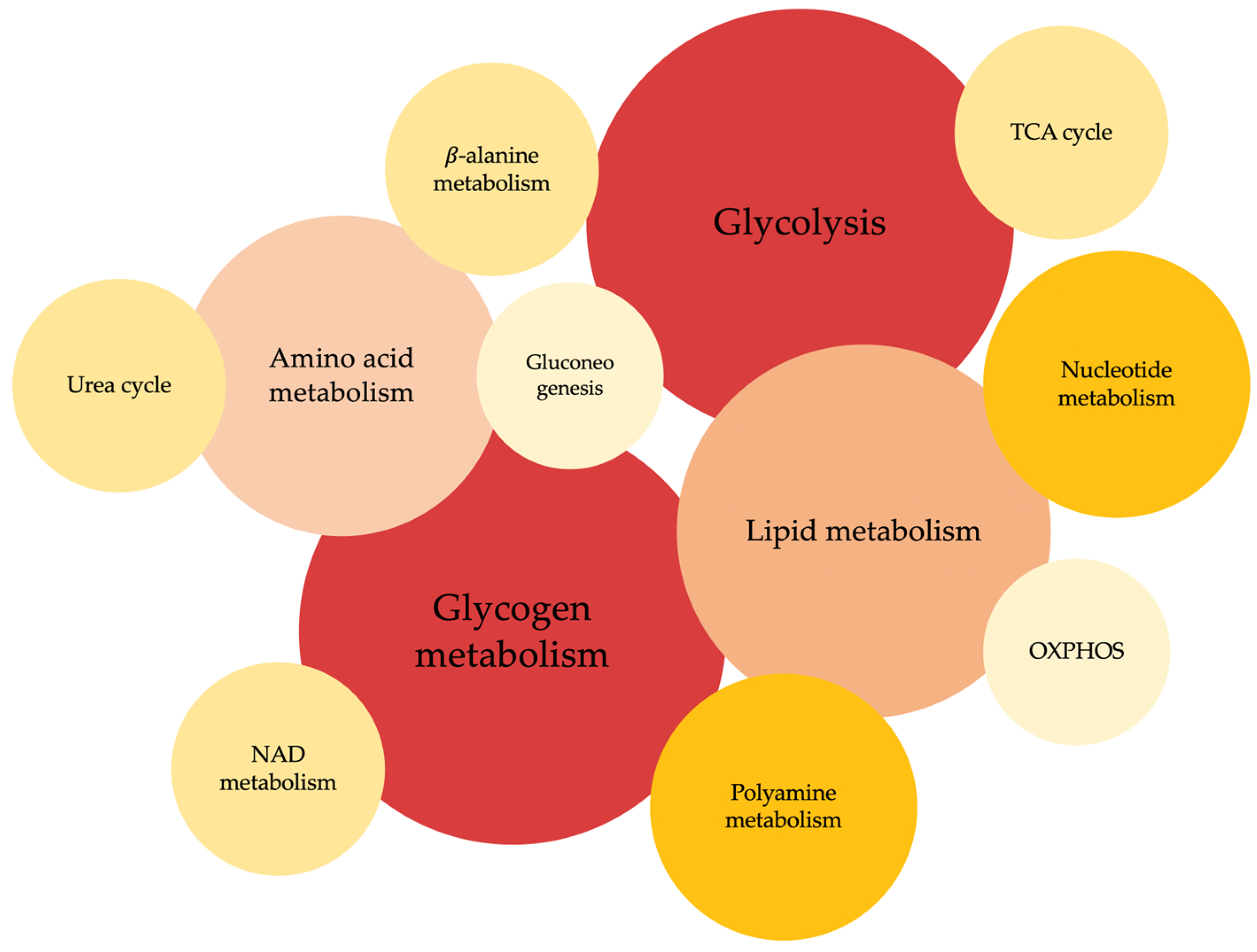
3. Omics Studies for the Characterization of Specific Pompe Disease Metabolic Phenotypes
4. Omics Studies for the Characterization of the Metabolic Response to Therapeutic Interventions in Pompe Disease
5. Conclusions
6. Future Perspectives
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kingma, S.D.K.; Bodamer, O.A.; Wijburg, F.A. Epidemiology and Diagnosis of Lysosomal Storage Disorders; Challenges of Screening. Best Pract. Res. Clin. Endocrinol. Metab. 2015, 29, 145–157. [Google Scholar] [CrossRef]
- Giugliani, R.; Federhen, A.; Michelin-Tirelli, K.; Riegel, M.; Burin, M. Relative Frequency and Estimated Minimal Frequency of Lysosomal Storage Diseases in Brazil: Report from a Reference Laboratory. Genet. Mol. Biol. 2017, 40, 31–39. [Google Scholar] [CrossRef]
- Chin, S.J.; Fuller, M. Prevalence of Lysosomal Storage Disorders in Australia from 2009 to 2020. Lancet Reg. Health West. Pac. 2022, 19, 100344. [Google Scholar] [CrossRef]
- Wang, R.Y.; Bodamer, O.A.; Watson, M.S.; Wilcox, W.R.; ACMG Work Group on Diagnostic Confirmation of Lysosomal Storage Diseases. Lysosomal Storage Diseases: Diagnostic Confirmation and Management of Presymptomatic Individuals. Genet. Med. 2011, 13, 457–484. [Google Scholar] [CrossRef]
- Zschocke, J.; Blau, N.; Duran, M.; Blaskovics, M.; Gibson, K. Physician’s Guide to the Diagnosis, Treatment, and Follow-Up of Inherited Metabolic Diseases; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- La Cognata, V.; Guarnaccia, M.; Polizzi, A.; Ruggieri, M.; Cavallaro, S. Highlights on Genomics Applications for Lysosomal Storage Diseases. Cells 2020, 9, 1902. [Google Scholar] [CrossRef]
- Hicks, J.; Wartchow, E.; Mierau, G. Glycogen Storage Diseases: A Brief Review and Update on Clinical Features, Genetic Abnormalities, Pathologic Features, and Treatment. Ultrastruct. Pathol. 2011, 35, 183–196. [Google Scholar] [CrossRef]
- Kanungo, S.; Wells, K.; Tribett, T.; El-Gharbawy, A. Glycogen Metabolism and Glycogen Storage Disorders. Ann. Transl. Med. 2018, 6, 474. [Google Scholar] [CrossRef]
- Kohler, L.; Puertollano, R.; Raben, N. Pompe Disease: From Basic Science to Therapy. Neurotherapeutics 2018, 15, 928–942. [Google Scholar] [CrossRef]
- Ausems, M.; Verbiest, J.; Hermans, M.; Kroos, M.; Beemer, F.; Wokke, J.; Sandkuijl, L.; Reuser, A.; Van Der Ploeg, A. Frequency of Glycogen Storage Disease Type II in The Netherlands: Implications for Diagnosis and Genetic Counselling. Eur. J. Hum. Genet. 1999, 7, 713–716. [Google Scholar] [CrossRef]
- Gutiérrez-Rivas, E.; Bautista, J.; Vílchez, J.J.; Muelas, N.; Díaz-Manera, J.; Illa, I.; Martínez-Arroyo, A.; Olivé, M.; Sanz, I.; Arpa, J.; et al. Dried Blood Spot for Screening for Late-Onset Pompe Disease: A Spanish Cohort. J. Neuromuscul. Dis. 2015, 2, S42. [Google Scholar] [CrossRef]
- Alonso-Pérez, J.; Segovia, S.; Domínguez-González, C.; Olivé, M.; Mendoza Grimón, M.D.; Fernández-Torrón, R.; López De Munain, A.; Muñoz-Blanco, J.L.; Ramos-Fransi, A.; Almendrote, M.; et al. Registro español de la enfermedad de Pompe: Análisis de los primeros 49 pacientes con enfermedad de Pompe del adulto. Med. Clín. 2020, 154, 80–85. [Google Scholar] [CrossRef]
- Filosto, M.; Todeschini, A.; Cotelli, M.S.; Vielmi, V.; Rinaldi, F.; Rota, S.; Scarpelli, M.; Padovani, A. Non-Muscle Involvement in Late-Onset Glycogenosis II. Acta Myol. 2013, 32, 91–94. [Google Scholar]
- Feeney, E.J.; Austin, S.; Chien, Y.-H.; Mandel, H.; Schoser, B.; Prater, S.; Hwu, W.-L.; Ralston, E.; Kishnani, P.S.; Raben, N. The Value of Muscle Biopsies in Pompe Disease: Identifying Lipofuscin Inclusions in Juvenile- and Adult-Onset Patients. Acta Neuropathol. Commun. 2014, 2, 2. [Google Scholar] [CrossRef]
- Chan, J.; Desai, A.K.; Kazi, Z.B.; Corey, K.; Austin, S.; Hobson-Webb, L.D.; Case, L.E.; Jones, H.N.; Kishnani, P.S. The Emerging Phenotype of Late-Onset Pompe Disease: A Systematic Literature Review. Mol. Genet. Metab. 2017, 120, 163–172. [Google Scholar] [CrossRef]
- Gelb, M.; Lukacs, Z.; Ranieri, E.; Schielen, P. Newborn Screening for Lysosomal Storage Disorders: Methodologies for Measurement of Enzymatic Activities in Dried Blood Spots. Int. J. Neonatal Screen. 2018, 5, 1. [Google Scholar] [CrossRef] [PubMed]
- Mokhtariye, A.; Hagh-Nazari, L.; Varasteh, A.-R.; Keyfi, F. Diagnostic Methods for Lysosomal Storage Disease. Rep. Biochem. Mol. Biol. 2019, 7, 119–128. [Google Scholar]
- Strobel, S.; Hesse, N.; Santhanakumaran, V.; Groeschel, S.; Bruchelt, G.; Krägeloh-Mann, I.; Böhringer, J. Optimization of Enzyme Essays to Enhance Reliability of Activity Measurements in Leukocyte Lysates for the Diagnosis of Metachromatic Leukodystrophy and Gangliosidoses. Cells 2020, 9, 2553. [Google Scholar] [CrossRef] [PubMed]
- Niño, M.Y.; Wijgerde, M.; De Faria, D.O.S.; Hoogeveen-Westerveld, M.; Bergsma, A.J.; Broeders, M.; Van Der Beek, N.A.M.E.; Van Den Hout, H.J.M.; Van Der Ploeg, A.T.; Verheijen, F.W.; et al. Enzymatic Diagnosis of Pompe Disease: Lessons from 28 Years of Experience. Eur. J. Hum. Genet. 2021, 29, 434–446. [Google Scholar] [CrossRef]
- Wasserstein, M.P.; Orsini, J.J.; Goldenberg, A.; Caggana, M.; Levy, P.A.; Breilyn, M.; Gelb, M.H. The Future of Newborn Screening for Lysosomal Disorders. Neurosci. Lett. 2021, 760, 136080. [Google Scholar] [CrossRef]
- Sun, A. Lysosomal Storage Disease Overview. Ann. Transl. Med. 2018, 6, 476. [Google Scholar] [CrossRef]
- Ames, E.G.; Fisher, R.; Kleyn, M.; Ahmad, A. Current Practices for U.S. Newborn Screening of Pompe Disease and MPSI. Int. J. Neonatal Screen. 2020, 6, 72. [Google Scholar] [CrossRef] [PubMed]
- Kronn, D.F.; Day-Salvatore, D.; Hwu, W.-L.; Jones, S.A.; Nakamura, K.; Okuyama, T.; Swoboda, K.J.; Kishnani, P.S.; on behalf of the Pompe Disease Newborn Screening Working Group. Management of Confirmed Newborn-Screened Patients With Pompe Disease Across the Disease Spectrum. Pediatrics 2017, 140, S24–S45. [Google Scholar] [CrossRef]
- Gragnaniello, V.; Pijnappel, P.W.W.M.; Burlina, A.P.; In ’T Groen, S.L.M.; Gueraldi, D.; Cazzorla, C.; Maines, E.; Polo, G.; Salviati, L.; Di Salvo, G.; et al. Newborn Screening for Pompe Disease in Italy: Long-Term Results and Future Challenges. Mol. Genet. Metab. Rep. 2022, 33, 100929. [Google Scholar] [CrossRef]
- Lee, N.-C.; Chang, K.-L.; In ’T Groen, S.L.M.; De Faria, D.O.S.; Huang, H.-J.; Pijnappel, W.W.M.P.; Hwu, W.-L.; Chien, Y.-H. Outcome of Later-Onset Pompe Disease Identified Through Newborn Screening. J. Pediatr. 2022, 244, 139–147.e2. [Google Scholar] [CrossRef]
- Faraguna, M.C.; Crescitelli, V.; Fornari, A.; Barzaghi, S.; Savasta, S.; Foiadelli, T.; Veraldi, D.; Paoletti, M.; Pichiecchio, A.; Gasperini, S. Treatment Dilemma in Children with Late-Onset Pompe Disease. Genes 2023, 14, 362. [Google Scholar] [CrossRef] [PubMed]
- Leslie, N.; Bailey, L. Pompe Disease. In GeneReviews®; Adam, M.P., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J., Gripp, K.W., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. [Google Scholar]
- van der Ploeg, A.T.; Reuser, A.J.J. Pompe’s Disease. Lancet 2008, 372, 1342–1353. [Google Scholar] [CrossRef] [PubMed]
- Isaacs, H.; Savage, N.; Badenhorst, M.; Whistler, T. Acid Maltase Deficiency: A Case Study and Review of the Pathophysiological Changes and Proposed Therapeutic Measures. J. Neurol. Neurosurg. Psychiatry 1986, 49, 1011–1018. [Google Scholar] [CrossRef]
- Kishnani, P.S.; Hwu, W.-L.; Mandel, H.; Nicolino, M.; Yong, F.; Corzo, D. A Retrospective, Multinational, Multicenter Study on the Natural History of Infantile-Onset Pompe Disease. J. Pediatr. 2006, 148, 671–676.e2. [Google Scholar] [CrossRef]
- Hamdan, M.A.; El-Zoabi, B.A.; Begam, M.A.; Mirghani, H.M.; Almalik, M.H. Antenatal Diagnosis of Pompe Disease by Fetal Echocardiography: Impact on Outcome after Early Initiation of Enzyme Replacement Therapy. J. Inherit. Metab. Dis. 2010, 33, 333–339. [Google Scholar] [CrossRef]
- Cohen, J.L.; Chakraborty, P.; Fung-Kee-Fung, K.; Schwab, M.E.; Bali, D.; Young, S.P.; Gelb, M.H.; Khaledi, H.; DiBattista, A.; Smallshaw, S.; et al. In Utero Enzyme-Replacement Therapy for Infantile-Onset Pompe’s Disease. N. Engl. J. Med. 2022, 387, 2150–2158. [Google Scholar] [CrossRef]
- Martínez, M.; Romero, M.G.; Guereta, L.G.; Cabrera, M.; Regojo, R.M.; Albajara, L.; Couce, M.L.; Pipaon, M.S.D. Infantile-Onset Pompe Disease with Neonatal Debut: A Case Report and Literature Review. Medicine 2017, 96, e9186. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Zhang, L.; Quan, S. Enzyme Replacement Therapy for Infantile-Onset Pompe Disease. Cochrane Database Syst. Rev. 2017, 2017, CD011539. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Desai, A.K.; Gupta, P.; Dempsey, K.; Bhambhani, V.; Hopkin, R.J.; Ficicioglu, C.; Tanpaiboon, P.; Craigen, W.J.; Rosenberg, A.S.; et al. Transforming the Clinical Outcome in CRIM-Negative Infantile Pompe Disease Identified via Newborn Screening: The Benefits of Early Treatment with Enzyme Replacement Therapy and Immune Tolerance Induction. Genet. Med. 2021, 23, 845–855. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, T. In Utero Enzyme Replacement Therapy (ERT) for Prenatally Diagnosed Lysosomal Storage Disorders (LSDs); NIH National Library of Medicine: Bethesda, MD, USA, 2022. [Google Scholar]
- Lim, J.-A.; Li, L.; Raben, N. Pompe Disease: From Pathophysiology to Therapy and Back Again. Front. Aging Neurosci. 2014, 6, 177. [Google Scholar] [CrossRef]
- Alandy-Dy, J.; Wencel, M.; Hall, K.; Simon, J.; Chen, Y.; Valenti, E.; Yang, J.; Bali, D.; Lakatos, A.; Goyal, N.; et al. Variable Clinical Features and Genotype-Phenotype Correlations in 18 Patients with Late-Onset Pompe Disease. Ann. Transl. Med. 2019, 7, 276. [Google Scholar] [CrossRef]
- Beck, M. Variable Clinical Presentation in Lysosomal Storage Disorders. J. Inherit. Metab. Dis. 2001, 24 (Suppl. S2), 47–51; discussion 45–46. [Google Scholar] [CrossRef]
- Domínguez-González, C.; Díaz-Marín, C.; Juntas-Morales, R.; Nascimiento-Osorio, A.; Rivera-Gallego, A.; Díaz-Manera, J. Survey on the Management of Pompe Disease in Routine Clinical Practice in Spain. Orphanet. J. Rare Dis. 2022, 17, 426. [Google Scholar] [CrossRef]
- Parenti, G.; Medina, D.L.; Ballabio, A. The Rapidly Evolving View of Lysosomal Storage Diseases. EMBO Mol. Med. 2021, 13, e12836. [Google Scholar] [CrossRef]
- Davidson, B.A.; Hassan, S.; Garcia, E.J.; Tayebi, N.; Sidransky, E. Exploring Genetic Modifiers of Gaucher Disease: The next Horizon. Hum. Mutat. 2018, 39, 1739–1751. [Google Scholar] [CrossRef]
- Hassan, S.; Sidransky, E.; Tayebi, N. The Role of Epigenetics in Lysosomal Storage Disorders: Uncharted Territory. Mol. Genet. Metab. 2017, 122, 10–18. [Google Scholar] [CrossRef]
- Pavlova, E.V.; Shatunov, A.; Wartosch, L.; Moskvina, A.I.; Nikolaeva, L.E.; Bright, N.A.; Tylee, K.L.; Church, H.J.; Ballabio, A.; Luzio, J.P.; et al. The Lysosomal Disease Caused by Mutant VPS33A. Hum. Mol. Genet. 2019, 28, 2514–2530. [Google Scholar] [CrossRef] [PubMed]
- Steel, D.; Zech, M.; Zhao, C.; Barwick, K.E.S.; Burke, D.; Demailly, D.; Kumar, K.R.; Zorzi, G.; Nardocci, N.; Kaiyrzhanov, R.; et al. Loss-of-Function Variants in HOPS Complex Genes VPS16 and VPS41 Cause Early Onset Dystonia Associated with Lysosomal Abnormalities. Ann. Neurol. 2020, 88, 867–877. [Google Scholar] [CrossRef] [PubMed]
- Savarese, M.; Torella, A.; Musumeci, O.; Angelini, C.; Astrea, G.; Bello, L.; Bruno, C.; Comi, G.P.; Di Fruscio, G.; Piluso, G.; et al. Targeted Gene Panel Screening Is an Effective Tool to Identify Undiagnosed Late Onset Pompe Disease. Neuromuscul. Disord. 2018, 28, 586–591. [Google Scholar] [CrossRef] [PubMed]
- Cammarata, G.; Scalia, S.; Colomba, P.; Zizzo, C.; Pisani, A.; Riccio, E.; Montalbano, M.; Alessandro, R.; Giordano, A.; Duro, G. A Pilot Study of Circulating MicroRNAs as Potential Biomarkers of Fabry Disease. Oncotarget 2018, 9, 27333–27345. [Google Scholar] [CrossRef] [PubMed]
- Tarallo, A.; Carissimo, A.; Gatto, F.; Nusco, E.; Toscano, A.; Musumeci, O.; Coletta, M.; Karali, M.; Acampora, E.; Damiano, C.; et al. MicroRNAs as Biomarkers in Pompe Disease. Genet. Med. 2019, 21, 591–600. [Google Scholar] [CrossRef]
- Carrasco-Rozas, A.; Fernández-Simón, E.; Lleixà, M.C.; Belmonte, I.; Pedrosa-Hernandez, I.; Montiel-Morillo, E.; Nuñez-Peralta, C.; Llauger Rossello, J.; Segovia, S.; De Luna, N.; et al. Identification of Serum MicroRNAs as Potential Biomarkers in Pompe Disease. Ann. Clin. Transl. Neurol. 2019, 6, 1214–1224. [Google Scholar] [CrossRef]
- Bobillo Lobato, J.; Jiménez Hidalgo, M.; Jiménez Jiménez, L.M. Biomarkers in Lysosomal Storage Diseases. Diseases 2016, 4, 40. [Google Scholar] [CrossRef]
- Holmes, E.; Wilson, I.D.; Nicholson, J.K. Metabolic Phenotyping in Health and Disease. Cell 2008, 134, 714–717. [Google Scholar] [CrossRef]
- Babu, M.; Snyder, M. Multi-Omics Profiling for Health. Mol. Cell Proteom. 2023, 22, 100561. [Google Scholar] [CrossRef]
- Ng, Q.X.; Yau, C.E.; Yaow, C.Y.L.; Chong, R.I.H.; Chong, N.Z.-Y.; Teoh, S.E.; Lim, Y.L.; Soh, A.Y.S.; Ng, W.K.; Thumboo, J. What Has Longitudinal “Omics” Studies Taught Us about Irritable Bowel Syndrome? A Systematic Review. Metabolites 2023, 13, 484. [Google Scholar] [CrossRef]
- Jiang, P.-C.; Fan, J.; Zhang, C.-D.; Bai, M.-H.; Sun, Q.-Q.; Chen, Q.-P.; Mao, W.; Tang, B.-F.; Lan, H.-Y.; Zhou, Y.-Y.; et al. Unraveling Colorectal Cancer and Pan-Cancer Immune Heterogeneity and Synthetic Therapy Response Using Cuproptosis and Hypoxia Regulators by Multi-Omic Analysis and Experimental Validation. Int. J. Biol. Sci. 2023, 19, 3526–3543. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-F.; Yang, C.C.; Liao, H.-C.; Huang, L.-Y.; Chiang, C.-C.; Ho, H.-C.; Lai, C.-J.; Chu, T.-H.; Yang, T.-F.; Hsu, T.-R.; et al. Very Early Treatment for Infantile-Onset Pompe Disease Contributes to Better Outcomes. J. Pediatr. 2016, 169, 174–180.e1. [Google Scholar] [CrossRef] [PubMed]
- Chien, Y.-H.; Hwu, W.-L.; Lee, N.-C. Pompe Disease: Early Diagnosis and Early Treatment Make a Difference. Pediatr. Neonatol. 2013, 54, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Kishnani, P.S.; Corzo, D.; Leslie, N.D.; Gruskin, D.; Van Der Ploeg, A.; Clancy, J.P.; Parini, R.; Morin, G.; Beck, M.; Bauer, M.S.; et al. Early Treatment with Alglucosidase Alfa Prolongs Long-Term Survival of Infants with Pompe Disease. Pediatr. Res. 2009, 66, 329–335. [Google Scholar] [CrossRef]
- Fatehi, F.; Ashrafi, M.R.; Babaee, M.; Ansari, B.; Beiraghi Toosi, M.; Boostani, R.; Eshraghi, P.; Fakharian, A.; Hadipour, Z.; Haghi Ashtiani, B.; et al. Recommendations for Infantile-Onset and Late-Onset Pompe Disease: An Iranian Consensus. Front. Neurol. 2021, 12, 739931. [Google Scholar] [CrossRef] [PubMed]
- Bolano-Diaz, C.; Diaz-Manera, J. Therapeutic Options for the Management of Pompe Disease: Current Challenges and Clinical Evidence in Therapeutics and Clinical Risk Management. TCRM 2022, 18, 1099–1115. [Google Scholar] [CrossRef]
- Kishnani, P.S.; Goldenberg, P.C.; DeArmey, S.L.; Heller, J.; Benjamin, D.; Young, S.; Bali, D.; Smith, S.A.; Li, J.S.; Mandel, H.; et al. Cross-Reactive Immunologic Material Status Affects Treatment Outcomes in Pompe Disease Infants. Mol. Genet. Metab. 2010, 99, 26–33. [Google Scholar] [CrossRef]
- Meenu, M.; Verma, V.K.; Seth, A.; Sahoo, R.K.; Gupta, P.; Arya, D.S. Association of Monoamine Oxidase A with Tumor Burden and Castration Resistance in Prostate Cancer. Curr. Ther. Res. Clin. Exp. 2020, 93, 100610. [Google Scholar] [CrossRef]
- Van Der Ploeg, A.; Carlier, P.G.; Carlier, R.-Y.; Kissel, J.T.; Schoser, B.; Wenninger, S.; Pestronk, A.; Barohn, R.J.; Dimachkie, M.M.; Goker-Alpan, O.; et al. Prospective Exploratory Muscle Biopsy, Imaging, and Functional Assessment in Patients with Late-Onset Pompe Disease Treated with Alglucosidase Alfa: The EMBASSY Study. Mol. Genet. Metab. 2016, 119, 115–123. [Google Scholar] [CrossRef]
- Stevens, D.; Milani-Nejad, S.; Mozaffar, T. Pompe Disease: A Clinical, Diagnostic, and Therapeutic Overview. Curr. Treat Opt. Neurol. 2022, 24, 573–588. [Google Scholar] [CrossRef]
- Do, H.V.; Khanna, R.; Gotschall, R. Challenges in Treating Pompe Disease: An Industry Perspective. Ann. Transl. Med. 2019, 7, 291. [Google Scholar] [CrossRef] [PubMed]
- Cheon, C.K. Considerations for Evaluating the Effectiveness and Long-Term Outcome of Enzyme Replacement Therapy in Pompe Disease. Clin. Exp. Pediatr. 2020, 63, 14–15. [Google Scholar] [CrossRef]
- Claeys, K.G.; D’Hondt, A.; Fache, L.; Peers, K.; Depuydt, C.E. Six-Minute Walk Distance Is a Useful Outcome Measure to Detect Motor Decline in Treated Late-Onset Pompe Disease Patients. Cells 2022, 11, 334. [Google Scholar] [CrossRef] [PubMed]
- Starosta, R.T.; Singh, P.; Nguyen, H.T.; Leestma, K.; Manwaring, L.; Peterman, L.; Kata, K.; Colombo, J.; Hulbert, M.; Granadillo, J.L.; et al. Treatment Dilemmas in an Individual Diagnosed with Infantile-Onset Pompe Disease and Sickle-Cell Anemia. Mol. Genet. Metab. 2022, 135, S116. [Google Scholar] [CrossRef]
- Kishnani, P.S.; Steiner, R.D.; Bali, D.; Berger, K.; Byrne, B.J.; Case, L.E.; Crowley, J.F.; Downs, S.; Howell, R.R.; Kravitz, R.M.; et al. Pompe Disease Diagnosis and Management Guideline. Genet. Med. 2006, 8, 267–288. [Google Scholar] [CrossRef] [PubMed]
- Schoser, B.; Stewart, A.; Kanters, S.; Hamed, A.; Jansen, J.; Chan, K.; Karamouzian, M.; Toscano, A. Survival and Long-Term Outcomes in Late-Onset Pompe Disease Following Alglucosidase Alfa Treatment: A Systematic Review and Meta-Analysis. J. Neurol. 2017, 264, 621–630. [Google Scholar] [CrossRef]
- Raben, N.; Schreiner, C.; Baum, R.; Takikita, S.; Xu, S.; Xie, T.; Myerowitz, R.; Komatsu, M.; Van der Meulen, J.H.; Nagaraju, K.; et al. Suppression of Autophagy Permits Successful Enzyme Replacement Therapy in a Lysosomal Storage Disorder–Murine Pompe Disease. Autophagy 2010, 6, 1078–1089. [Google Scholar] [CrossRef]
- Puertollano, R.; Raben, N. New Therapies for Pompe Disease: Are We Closer to a Cure? Lancet Neurol. 2021, 20, 973–975. [Google Scholar] [CrossRef]
- Ebbink, B.J.; Poelman, E.; Aarsen, F.K.; Plug, I.; Régal, L.; Muentjes, C.; Beek, N.A.M.E.; Lequin, M.H.; Ploeg, A.T.; Hout, J.M.P. Classic Infantile Pompe Patients Approaching Adulthood: A Cohort Study on Consequences for the Brain. Dev. Med. Child Neurol. 2018, 60, 579–586. [Google Scholar] [CrossRef]
- Desai, A.K.; Li, C.; Rosenberg, A.S.; Kishnani, P.S. Immunological Challenges and Approaches to Immunomodulation in Pompe Disease: A Literature Review. Ann. Transl. Med. 2019, 7, 285. [Google Scholar] [CrossRef]
- Desai, A.K.; Baloh, C.H.; Sleasman, J.W.; Rosenberg, A.S.; Kishnani, P.S. Benefits of Prophylactic Short-Course Immune Tolerance Induction in Patients with Infantile Pompe Disease: Demonstration of Long-Term Safety and Efficacy in an Expanded Cohort. Front. Immunol. 2020, 11, 1727. [Google Scholar] [CrossRef] [PubMed]
- Baik, A.D.; Calafati, P.T.; Aaron, N.A.; Mehra, A.; Moller-Tank, S.; Miloscio, L.; Wang, L.; Praggastis, M.; Birnbaum, M.S.; Pan, C.; et al. Targeted Delivery of Acid Alpha-Glucosidase Corrects Skeletal Muscle Phenotypes in Pompe Disease Mice. bioRxiv 2020. [Google Scholar] [CrossRef]
- Baik, A.D.; Calafati, P.; Zhang, X.; Aaron, N.A.; Mehra, A.; Moller-Tank, S.; Miloscio, L.; Praggastis, M.; Giovannone, N.; Pan, C.; et al. Cell Type-Selective Targeted Delivery of a Recombinant Lysosomal Enzyme for Enzyme Therapies. Mol. Ther. 2021, 29, 3512–3524. [Google Scholar] [CrossRef]
- Dhillon, S. Avalglucosidase Alfa: First Approval. Drugs 2021, 81, 1803–1809. [Google Scholar] [CrossRef] [PubMed]
- Unnisa, Z.; Yoon, J.K.; Schindler, J.W.; Mason, C.; van Til, N.P. Gene Therapy Developments for Pompe Disease. Biomedicines 2022, 10, 302. [Google Scholar] [CrossRef] [PubMed]
- Blair, H.A. Cipaglucosidase Alfa: First Approval. Drugs 2023, 83, 739–745. [Google Scholar] [CrossRef]
- Noonberg, S. A Phase 1, Randomized, Double-Blind, Placebo-Controlled, Single and Multiple Ascending Dose Study of MZE001 to Evaluate the Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics in Healthy Subject; ClinicalTrials.gov Identifier: NCT05249621; National Library of Medicine: Bethesda, MD, USA, 2022.
- Stok, M.; De Boer, H.; Huston, M.W.; Jacobs, E.H.; Roovers, O.; Visser, T.P.; Jahr, H.; Duncker, D.J.; Van Deel, E.D.; Reuser, A.J.J.; et al. Lentiviral Hematopoietic Stem Cell Gene Therapy Corrects Murine Pompe Disease. Mol. Ther. Methods Clin. Dev. 2020, 17, 1014–1025. [Google Scholar] [CrossRef]
- Ghosh, A.; Liao, A.; O’Leary, C.; Mercer, J.; Tylee, K.; Goenka, A.; Holley, R.; Jones, S.A.; Bigger, B.W. Strategies for the Induction of Immune Tolerance to Enzyme Replacement Therapy in Mucopolysaccharidosis Type I. Mol. Ther. Methods Clin. Dev. 2019, 13, 321–333. [Google Scholar] [CrossRef]
- Lim, J.; Li, L.; Shirihai, O.S.; Trudeau, K.M.; Puertollano, R.; Raben, N. Modulation of MTOR Signaling as a Strategy for the Treatment of Pompe Disease. EMBO Mol. Med. 2017, 9, 353–370. [Google Scholar] [CrossRef]
- Lim, J.-A.; Sun, B.; Puertollano, R.; Raben, N. Therapeutic Benefit of Autophagy Modulation in Pompe Disease. Mol. Ther. 2018, 26, 1783–1796. [Google Scholar] [CrossRef]
- Molares-Vila, A.; Corbalán-Rivas, A.; Carnero-Gregorio, M.; González-Cespón, J.L.; Rodríguez-Cerdeira, C. Biomarkers in Glycogen Storage Diseases: An Update. IJMS 2021, 22, 4381. [Google Scholar] [CrossRef] [PubMed]
- Young, S.P.; Piraud, M.; Goldstein, J.L.; Zhang, H.; Rehder, C.; Laforet, P.; Kishnani, P.S.; Millington, D.S.; Bashir, M.R.; Bali, D.S. Assessing Disease Severity in Pompe Disease: The Roles of a Urinary Glucose Tetrasaccharide Biomarker and Imaging Techniques. Am. J. Med. Genet. C Semin. Med. Genet. 2012, 160C, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Chien, Y.-H.; Goldstein, J.L.; Hwu, W.-L.; Smith, P.B.; Lee, N.-C.; Chiang, S.-C.; Tolun, A.A.; Zhang, H.; Vaisnins, A.E.; Millington, D.S.; et al. Baseline Urinary Glucose Tetrasaccharide Concentrations in Patients with Infantile- and Late-Onset Pompe Disease Identified by Newborn Screening. In JIMD Reports; Zschocke, J., Baumgartner, M., Morava, E., Patterson, M., Rahman, S., Peters, V., Eds.; Springer: Berlin/Heidelberg, Germany, 2014; Volume 19, pp. 67–73. ISBN 978-3-662-46189-1. [Google Scholar]
- Saville, J.T.; Fuller, M. Experience with the Urinary Tetrasaccharide Metabolite for Pompe Disease in the Diagnostic Laboratory. Metabolites 2021, 11, 446. [Google Scholar] [CrossRef]
- An, Y.; Young, S.P.; Kishnani, P.S.; Millington, D.S.; Amalfitano, A.; Corzo, D.; Chen, Y.-T. Glucose Tetrasaccharide as a Biomarker for Monitoring the Therapeutic Response to Enzyme Replacement Therapy for Pompe Disease. Mol. Genet. Metab. 2005, 85, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Young, S.P.; Zhang, H.; Corzo, D.; Thurberg, B.L.; Bali, D.; Kishnani, P.S.; Millington, D.S. Long-Term Monitoring of Patients with Infantile-Onset Pompe Disease on Enzyme Replacement Therapy Using a Urinary Glucose Tetrasaccharide Biomarker. Genet. Med. 2009, 11, 536–541. [Google Scholar] [CrossRef]
- Sluiter, W.; Van Den Bosch, J.C.; Goudriaan, D.A.; Van Gelder, C.M.; De Vries, J.M.; Huijmans, J.G.M.; Reuser, A.J.J.; Van Der Ploeg, A.T.; Ruijter, G.J.G. Rapid Ultraperformance Liquid Chromatography–Tandem Mass Spectrometry Assay for a Characteristic Glycogen-Derived Tetrasaccharide in Pompe Disease and Other Glycogen Storage Diseases. Clin. Chem. 2012, 58, 1139–1147. [Google Scholar] [CrossRef]
- Manwaring, V.; Prunty, H.; Bainbridge, K.; Burke, D.; Finnegan, N.; Franses, R.; Lam, A.; Vellodi, A.; Heales, S. Urine Analysis of Glucose Tetrasaccharide by HPLC; a Useful Marker for the Investigation of Patients with Pompe and Other Glycogen Storage Diseases. J. Inherit. Metab. Dis. 2012, 35, 311–316. [Google Scholar] [CrossRef]
- De Souza, H.M.R.; Scalco, F.B.; Garrett, R.; De C Marques, F.F. Development of a Kit for Urine Collection on Filter Paper as an Alternative for Pompe Disease Screening and Monitoring by LC-HRMS. Anal. Methods 2023, 15, 3932–3939. [Google Scholar] [CrossRef]
- Semeraro, M.; Sacchetti, E.; Deodato, F.; Coşkun, T.; Lay, I.; Catesini, G.; Olivieri, G.; Rizzo, C.; Boenzi, S.; Dionisi-Vici, C. A New UHPLC-MS/MS Method for the Screening of Urinary Oligosaccharides Expands the Detection of Storage Disorders. Orphanet. J. Rare Dis. 2021, 16, 24. [Google Scholar] [CrossRef]
- ICIEM 2013 12th International Congress of Inborn Errors of Metabolism. J. Inherit. Metab. Dis. 2013, 36, 55–90. [CrossRef]
- Bobillo Lobato, J.; Durán Parejo, P.; Tejero Díez, P.; Jiménez Jiménez, L.M. Glucosa tetrasacárido como biomarcador diagnóstico de la enfermedad de Pompe: Estudio en 35 pacientes. Med. Clín. 2013, 141, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.K.; Liao, H.C.; Hsieh, Y.P.; Chen, Y.C.; Yang, C.F.; Niu, D.M. Glucose Tetrasaccharide (Glc4) Level in Urine Sample as a Biomarker for Pompe Patients. Ann. Transl. Med. 2015, 3 (Suppl. S2), AB067. [Google Scholar]
- Mashima, R.; Okuyama, T.; Ohira, M. Biomarkers for Lysosomal Storage Disorders with an Emphasis on Mass Spectrometry. Int. J. Mol. Sci. 2020, 21, 2704. [Google Scholar] [CrossRef]
- Sidorina, A.; Catesini, G.; Levi Mortera, S.; Marzano, V.; Putignani, L.; Boenzi, S.; Taurisano, R.; Garibaldi, M.; Deodato, F.; Dionisi-Vici, C. Combined Proteomic and Lipidomic Studies in Pompe Disease Allow a Better Disease Mechanism Understanding. J. Inherit. Metab. Dis. 2021, 44, 705–717. [Google Scholar] [CrossRef] [PubMed]
- De Moraes, M.B.M.; de Souza, H.M.R.; de Oliveira, M.L.C.; Peake, R.W.A.; Scalco, F.B.; Garrett, R. Combined Targeted and Untargeted High-Resolution Mass Spectrometry Analyses to Investigate Metabolic Alterations in Pompe Disease. Metabolomics 2023, 19, 29. [Google Scholar] [CrossRef]
- Hagemeijer, M.C.; van den Bosch, J.C.; Bongaerts, M.; Jacobs, E.H.; van den Hout, J.M.P.; Oussoren, E.; Ruijter, G.J.G. Analysis of Urinary Oligosaccharide Excretion Patterns by UHPLC/HRAM Mass Spectrometry for Screening of Lysosomal Storage Disorders. J. Inherit. Metab. Dis. 2023, 46, 206–219. [Google Scholar] [CrossRef]
- Schoser, B. Pompe Disease: What Are We Missing? Ann. Transl. Med. 2019, 7, 292. [Google Scholar] [CrossRef]
- Li, H.; Li, J.; Wang, Y.; Yang, T. Proteomic Analysis of Effluents from Perfused Human Heart for Transplantation: Identification of Potential Biomarkers for Ischemic Heart Damage. Proteome Sci. 2012, 10, 21. [Google Scholar] [CrossRef]
- Ahmed, Z.; Ravandi, A.; Maguire, G.F.; Emili, A.; Draganov, D.; La Du, B.N.; Kuksis, A.; Connelly, P.W. Multiple Substrates for Paraoxonase-1 during Oxidation of Phosphatidylcholine by Peroxynitrite. Biochem. Biophys. Res. Commun. 2002, 290, 391–396. [Google Scholar] [CrossRef]
- Ramsay, S.L.; Maire, I.; Bindloss, C.; Fuller, M.; Whitfield, P.D.; Piraud, M.; Hopwood, J.J.; Meikle, P.J. Determination of Oligosaccharides and Glycolipids in Amniotic Fluid by Electrospray Ionisation Tandem Mass Spectrometry: In Utero Indicators of Lysosomal Storage Diseases. Mol. Genet. Metab. 2004, 83, 231–238. [Google Scholar] [CrossRef]
- Mak, J.; Cowan, T.M. Detecting Lysosomal Storage Disorders by Glycomic Profiling Using Liquid Chromatography Mass Spectrometry. Mol. Genet. Metab. 2021, 134, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Pančík, F.; Pakanová, Z.; Nemčovič, M.; Květoň, F.; Šalingová, A.; Hlavatá, A.; Kozmon, S.; Baráth, P. Application of MALDI-TOF Mass Spectrometry for Non-Invasive Diagnostics of Mucopolysaccharidosis IIIA. J. Inborn Errors Metab. Screen. 2023, 11, e2022022. [Google Scholar] [CrossRef]
- Young, S.P.; Stevens, R.D.; An, Y.; Chen, Y.-T.; Millington, D.S. Analysis of a Glucose Tetrasaccharide Elevated in Pompe Disease by Stable Isotope Dilution–Electrospray Ionization Tandem Mass Spectrometry. Anal. Biochem. 2003, 316, 175–180. [Google Scholar] [CrossRef]
- Piraud, M.; Pettazzoni, M.; de Antonio, M.; Vianey-Saban, C.; Froissart, R.; Chabrol, B.; Young, S.; Laforêt, P.; French Pompe study group. Urine Glucose Tetrasaccharide: A Good Biomarker for Glycogenoses Type II and III? A Study of the French Cohort. Mol. Genet. Metab. Rep. 2020, 23, 100583. [Google Scholar] [CrossRef]
- Kinton, S.; Dufault, M.R.; Zhang, M.; George, K. Transcriptomic Characterization of Clinical Skeletal Muscle Biopsy from Late-Onset Pompe Patients. Mol. Genet. Metab. 2023, 138, 107526. [Google Scholar] [CrossRef]
- Moriggi, M.; Capitanio, D.; Torretta, E.; Barbacini, P.; Bragato, C.; Sartori, P.; Moggio, M.; Maggi, L.; Mora, M.; Gelfi, C. Muscle Proteomic Profile before and after Enzyme Replacement Therapy in Late-Onset Pompe Disease. Int. J. Mol. Sci. 2021, 22, 2850. [Google Scholar] [CrossRef]
- Meena, N.K.; Ralston, E.; Raben, N.; Puertollano, R. Enzyme Replacement Therapy Can Reverse Pathogenic Cascade in Pompe Disease. Mol. Ther. Methods Clin. Dev. 2020, 18, 199–214. [Google Scholar] [CrossRef] [PubMed]
- Nascimbeni, A.C.; Fanin, M.; Masiero, E.; Angelini, C.; Sandri, M. The Role of Autophagy in the Pathogenesis of Glycogen Storage Disease Type II (GSDII). Cell Death Differ. 2012, 19, 1698–1708. [Google Scholar] [CrossRef]
- Nascimbeni, A.C.; Fanin, M.; Masiero, E.; Angelini, C.; Sandri, M. Impaired Autophagy Contributes to Muscle Atrophy in Glycogen Storage Disease Type II Patients. Autophagy 2012, 8, 1697–1700. [Google Scholar] [CrossRef]
- Sandri, M. Autophagy in Health and Disease. 3. Involvement of Autophagy in Muscle Atrophy. Am. J. Physiol. Cell Physiol. 2010, 298, C1291–C1297. [Google Scholar] [CrossRef]
- Sandri, M. Protein Breakdown in Muscle Wasting: Role of Autophagy-Lysosome and Ubiquitin-Proteasome. Int. J. Biochem. Cell Biol. 2013, 45, 2121–2129. [Google Scholar] [CrossRef]
- Slonim, A.E.; Coleman, R.A.; McElligot, M.A.; Najjar, J.; Hirschhorn, K.; Labadie, G.U.; Mrak, R.; Evans, O.B.; Shipp, E.; Presson, R. Improvement of Muscle Function in Acid Maltase Deficiency by High-Protein Therapy. Neurology 1983, 33, 34–38. [Google Scholar] [CrossRef]
- Umpleby, A.M.; Wiles, C.M.; Trend, P.S.; Scobie, I.N.; Macleod, A.F.; Spencer, G.T.; Sonksen, P.H. Protein Turnover in Acid Maltase Deficiency before and after Treatment with a High Protein Diet. J. Neurol. Neurosurg. Psychiatry 1987, 50, 587–592. [Google Scholar] [CrossRef]
- Slonim, A.E.; Bulone, L.; Goldberg, T.; Minikes, J.; Slonim, E.; Galanko, J.; Martiniuk, F. Modification of the Natural History of Adult-Onset Acid Maltase Deficiency by Nutrition and Exercise Therapy. Muscle Nerve 2007, 35, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Tarnopolsky, M.A.; Nilsson, M.I. Nutrition and Exercise in Pompe Disease. Ann. Transl. Med. 2019, 7, 282. [Google Scholar] [CrossRef] [PubMed]
- Sechi, A.; Zuccarelli, L.; Grassi, B.; Frangiamore, R.; De Amicis, R.; Marzorati, M.; Porcelli, S.; Tullio, A.; Bacco, A.; Bertoli, S.; et al. Exercise Training Alone or in Combination with High-Protein Diet in Patients with Late Onset Pompe Disease: Results of a Cross over Study. Orphanet. J. Rare Dis. 2020, 15, 143. [Google Scholar] [CrossRef]
- Schoser, B.G.H.; Müller-Höcker, J.; Horvath, R.; Gempel, K.; Pongratz, D.; Lochmüller, H.; Müller-Felber, W. Adult-Onset Glycogen Storage Disease Type 2: Clinico-Pathological Phenotype Revisited. Neuropathol. Appl. Neurobiol. 2007, 33, 544–559. [Google Scholar] [CrossRef]
- Lewandowska, E.; Wierzba-Bobrowicz, T.; Rola, R.; Modzelewska, J.; Stepień, T.; Lugowska, A.; Pasennik, E.; Ryglewicz, D. Pathology of Skeletal Muscle Cells in Adult-Onset Glycogenosis Type II (Pompe Disease): Ultrastructural Study. Folia Neuropathol. 2008, 46, 123–133. [Google Scholar]
- Raben, N.; Wong, A.; Ralston, E.; Myerowitz, R. Autophagy and Mitochondria in Pompe Disease: Nothing Is so New as What Has Long Been Forgotten. Am. J. Med. Genet. C Semin. Med. Genet. 2012, 160C, 13–21. [Google Scholar] [CrossRef]
- Lim, J.-A.; Li, L.; Kakhlon, O.; Myerowitz, R.; Raben, N. Defects in Calcium Homeostasis and Mitochondria Can Be Reversed in Pompe Disease. Autophagy 2015, 11, 385–402. [Google Scholar] [CrossRef]
- Plotegher, N.; Duchen, M.R. Mitochondrial Dysfunction and Neurodegeneration in Lysosomal Storage Disorders. Trends Mol. Med. 2017, 23, 116–134. [Google Scholar] [CrossRef] [PubMed]
- Fernández, R.; Fernández, J.M.; Cervera, C.; Teijeira, S.; Teijeiro, A.; Domínguez, C.; Navarro, C. Adult Glycogenosis II with Paracrystalline Mitochondrial Inclusions and Hirano Bodies in Skeletal Muscle. Neuromuscul. Disord. 1999, 9, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Colella, P.; Sellier, P.; Gomez, M.J.; Biferi, M.G.; Tanniou, G.; Guerchet, N.; Cohen-Tannoudji, M.; Moya-Nilges, M.; van Wittenberghe, L.; Daniele, N.; et al. Gene Therapy with Secreted Acid Alpha-Glucosidase Rescues Pompe Disease in a Novel Mouse Model with Early-Onset Spinal Cord and Respiratory Defects. EBioMedicine 2020, 61, 103052. [Google Scholar] [CrossRef] [PubMed]
- American Association of Neurological Surgeons (AANS); American Society of Neuroradiology (ASNR); Cardiovascular and Interventional Radiology Society of Europe (CIRSE); Canadian Interventional Radiology Association (CIRA); Congress of Neurological Surgeons (CNS); European Society of Minimally Invasive Neurological Therapy (ESMINT); European Society of Neuroradiology (ESNR); European Stroke Organization (ESO); Society for Cardiovascular Angiography and Interventions (SCAI); Society of Interventional Radiology (SIR); et al. Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke. Int. J. Stroke 2018, 13, 612–632. [Google Scholar]
- Toscano, A.; Rodolico, C.; Musumeci, O. Multisystem Late Onset Pompe Disease (LOPD): An Update on Clinical Aspects. Ann. Transl. Med. 2019, 7, 284. [Google Scholar] [CrossRef]
- van Kooten, H.A.; Harlaar, L.; van der Beek, N.a.M.E.; van Doorn, P.A.; van der Ploeg, A.T.; Brusse, E.; Erasmus MC Pompe expert committee. Discontinuation of Enzyme Replacement Therapy in Adults with Pompe Disease: Evaluating the European POmpe Consortium Stop Criteria. Neuromuscul. Disord. 2020, 30, 59–66. [Google Scholar] [CrossRef]
- Sarah, B.; Giovanna, B.; Emanuela, K.; Nadi, N.; Josè, V.; Alberto, P. Clinical Efficacy of the Enzyme Replacement Therapy in Patients with Late-Onset Pompe Disease: A Systematic Review and a Meta-Analysis. J. Neurol. 2022, 269, 733–741. [Google Scholar] [CrossRef]
- Fernando, R.; Drescher, C.; Nowotny, K.; Grune, T.; Castro, J.P. Impaired Proteostasis during Skeletal Muscle Aging. Free Radic. Biol. Med. 2019, 132, 58–66. [Google Scholar] [CrossRef]
- Xu, S.; Lun, Y.; Frascella, M.; Garcia, A.; Soska, R.; Nair, A.; Ponery, A.S.; Schilling, A.; Feng, J.; Tuske, S.; et al. Improved Efficacy of a Next-Generation ERT in Murine Pompe Disease. JCI Insight 2019, 4, e125358. [Google Scholar] [CrossRef]
- Fukuda, T.; Ahearn, M.; Roberts, A.; Mattaliano, R.J.; Zaal, K.; Ralston, E.; Plotz, P.H.; Raben, N. Autophagy and Mistargeting of Therapeutic Enzyme in Skeletal Muscle in Pompe Disease. Mol. Ther. 2006, 14, 831–839. [Google Scholar] [CrossRef]
- Raben, N.; Roberts, A.; Plotz, P.H. Role of Autophagy in the Pathogenesis of Pompe Disease. Acta Myol. 2007, 26, 45–48. [Google Scholar]
- Liu, Y.; Yi, F.; Kumar, A.B.; Kumar Chennamaneni, N.; Hong, X.; Scott, C.R.; Gelb, M.H.; Turecek, F. Multiplex Tandem Mass Spectrometry Enzymatic Activity Assay for Newborn Screening of the Mucopolysaccharidoses and Type 2 Neuronal Ceroid Lipofuscinosis. Clin. Chem. 2017, 63, 1118–1126. [Google Scholar] [CrossRef]
- Arunkumar, N.; Vu, D.C.; Khan, S.; Kobayashi, H.; Ngoc Can, T.B.; Oguni, T.; Watanabe, J.; Tanaka, M.; Yamaguchi, S.; Taketani, T.; et al. Diagnosis of Mucopolysaccharidoses and Mucolipidosis by Assaying Multiplex Enzymes and Glycosaminoglycans. Diagnostics 2021, 11, 1347. [Google Scholar] [CrossRef]
- Sista, R.S.; Eckhardt, A.E.; Wang, T.; Graham, C.; Rouse, J.L.; Norton, S.M.; Srinivasan, V.; Pollack, M.G.; Tolun, A.A.; Bali, D.; et al. Digital Microfluidic Platform for Multiplexing Enzyme Assays: Implications for Lysosomal Storage Disease Screening in Newborns. Clin. Chem. 2011, 57, 1444–1451. [Google Scholar] [CrossRef] [PubMed]
- Chien, Y.-H.; Lee, N.-C.; Chen, P.-W.; Yeh, H.-Y.; Gelb, M.H.; Chiu, P.-C.; Chu, S.-Y.; Lee, C.-H.; Lee, A.-R.; Hwu, W.-L. Newborn Screening for Morquio Disease and Other Lysosomal Storage Diseases: Results from the 8-Plex Assay for 70,000 Newborns. Orphanet. J. Rare Dis. 2020, 15, 38. [Google Scholar] [CrossRef] [PubMed]
- Sista, R.S.; Wang, T.; Wu, N.; Graham, C.; Eckhardt, A.; Winger, T.; Srinivasan, V.; Bali, D.; Millington, D.S.; Pamula, V.K. Multiplex Newborn Screening for Pompe, Fabry, Hunter, Gaucher, and Hurler Diseases Using a Digital Microfluidic Platform. Clin. Chim. Acta 2013, 424, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Loeber, J.G.; Platis, D.; Zetterström, R.H.; Almashanu, S.; Boemer, F.; Bonham, J.R.; Borde, P.; Brincat, I.; Cheillan, D.; Dekkers, E.; et al. Neonatal Screening in Europe Revisited: An ISNS Perspective on the Current State and Developments Since 2010. Int. J. Neonatal. Screen 2021, 7, 15. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.E.; Sullivan-Saarela, J.A.; Li, J.S.; Cox, G.F.; Corzo, D.; Chen, Y.-T.; Kishnani, P.S. Sibling Phenotype Concordance in Classical Infantile Pompe Disease. Am. J. Med. Genet. 2007, 143A, 2493–2501. [Google Scholar] [CrossRef]
- Fernandes, M.; Husi, H. Integrative Systems Biology Investigation of Fabry Disease. Diseases 2016, 4, 35. [Google Scholar] [CrossRef]
- Oliveira, J.P.; Ferreira, S. Multiple Phenotypic Domains of Fabry Disease and Their Relevance for Establishing Genotype-Phenotype Correlations. Appl. Clin. Genet. 2019, 12, 35–50. [Google Scholar] [CrossRef]
- Korlimarla, A.; Lim, J.-A.; Kishnani, P.S.; Sun, B. An Emerging Phenotype of Central Nervous System Involvement in Pompe Disease: From Bench to Bedside and Beyond. Ann. Transl. Med. 2019, 7, 289. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Barea, F.J.; Franco, L.; Elizondo, D.; Grootveld, M. Application of Data Augmentation Techniques towards Metabolomics. Comput. Biol. Med. 2022, 148, 105916. [Google Scholar] [CrossRef] [PubMed]
- Favret, J.M.; Weinstock, N.I.; Feltri, M.L.; Shin, D. Pre-Clinical Mouse Models of Neurodegenerative Lysosomal Storage Diseases. Front. Mol. Biosci. 2020, 7, 57. [Google Scholar] [CrossRef] [PubMed]
- Breuer, M.; Patten, S.A. A Great Catch for Investigating Inborn Errors of Metabolism-Insights Obtained from Zebrafish. Biomolecules 2020, 10, 1352. [Google Scholar] [CrossRef] [PubMed]
- Gaudioso, Á.; Silva, T.P.; Ledesma, M.D. Models to Study Basic and Applied Aspects of Lysosomal Storage Disorders. Adv. Drug Deliv. Rev. 2022, 190, 114532. [Google Scholar] [CrossRef]
- Schuchman, E.H.; Ledesma, M.D.; Simonaro, C.M. New Paradigms for the Treatment of Lysosomal Storage Diseases: Targeting the Endocannabinoid System as a Therapeutic Strategy. Orphanet. J. Rare Dis. 2021, 16, 151. [Google Scholar] [CrossRef]
- Parker, H.; Bigger, B.W. The Role of Innate Immunity in Mucopolysaccharide Diseases. J. Neurochem. 2019, 148, 639–651. [Google Scholar] [CrossRef]
- Ren, H.; Wang, G. Autophagy and Lysosome Storage Disorders. Adv. Exp. Med. Biol. 2020, 1207, 87–102. [Google Scholar] [CrossRef]
- Stepien, K.M.; Roncaroli, F.; Turton, N.; Hendriksz, C.J.; Roberts, M.; Heaton, R.A.; Hargreaves, I. Mechanisms of Mitochondrial Dysfunction in Lysosomal Storage Disorders: A Review. J. Clin. Med. 2020, 9, 2596. [Google Scholar] [CrossRef]
- Hsu, Y.-K.; Chien, Y.-H.; Shinn-Forng Peng, S.; Hwu, W.-L.; Lee, W.-T.; Lee, N.-C.; Po-Yu Huang, E.; Weng, W.-C. Evaluating Brain White Matter Hyperintensity, IQ Scores, and Plasma Neurofilament Light Chain Concentration in Early-Treated Patients with Infantile-Onset Pompe Disease. Genet. Med. 2023, 25, 27–36. [Google Scholar] [CrossRef]
- Pichiecchio, A.; Rossi, M.; Cinnante, C.; Colafati, G.S.; Icco, R.; Parini, R.; Menni, F.; Furlan, F.; Burlina, A.; Sacchini, M.; et al. Muscle MRI of Classic Infantile Pompe Patients: Fatty Substitution and Edema-Like Changes. Muscle Nerve 2017, 55, 841–848. [Google Scholar] [CrossRef] [PubMed]
- Paoletti, M.; Pichiecchio, A.; Colafati, G.S.; Conte, G.; Deodato, F.; Gasperini, S.; Menni, F.; Furlan, F.; Rubert, L.; Triulzi, F.M.; et al. Multicentric Retrospective Evaluation of Five Classic Infantile Pompe Disease Subjects Under Enzyme Replacement Therapy with Early Infratentorial Involvement. Front. Neurol. 2020, 11, 569153. [Google Scholar] [CrossRef] [PubMed]
- Biswas, N.; Chakrabarti, S. Artificial Intelligence (AI)-Based Systems Biology Approaches in Multi-Omics Data Analysis of Cancer. Front. Oncol. 2020, 10, 588221. [Google Scholar] [CrossRef] [PubMed]

| Study | Study Design | Sample | Omics-Based Approach | Major Findings † |
|---|---|---|---|---|
| Sidorina et al. [99] | 13 HC 12 PD | Plasma | nLC-MS/MS SWATH and LC-IMS/MS | nLC-MS/MS SWATH: ↑ LDHB, PKM and ↓ GPLD1 and PON1 LC-IMS/MS: ↑ phosphatidylcholines and ↓ lysophosphatidylcholines |
| Semeraro et al. [94] | Urine: 75 HC 4 PD | Urine and DUS | UHPLC-MS/MS with MRM | ↑ Glc4 and M4 |
| DUS: 12 HC 2 PD | ||||
| de Moraes et al. [100] | 21 HC 13 PD | Urine | LC-HRMAS | ↑ Glc4, creatine, sorbitol/mannitol, L-phenylalanine, N-acetyl-L-aspartic acid and ↓ N-acetyl-4-aminobutanal and 2-aminobenzoic acid |
| Hagemeijer et al. [101] | 121 HC 18 PD | Urine | UHPLC/HRAM MS | ↑ Glc4, Hex7 and Hex6 |
| Study | Study Design | Sample | Omics-Based Approach | Major Findings † |
|---|---|---|---|---|
| Lim et al. [84] | 10 WT 14 GAA-KO | Muscle tissue | CE-MS | ↑ histidine, lysine, threonine, alanine, aspartate, glutamine and serine |
| Meena et al. [112] | 6 WT 6 GAA-KO | Muscle tissue | CE-TOF/MS and CE-QqQMS | ↑ Gal1P, UDP-glucose, acetyl-CoA, citrate, succinate, fumarate, malate, carnitine, and ↓ G1P, G6P, F6P, F1,6B, pyruvate and lactate |
| Kinton et al. [110] | 10 HC 8 LOPD | Muscle tissue | Transcriptome profiling | ↑ lysosomal function, glycolysis, lipid metabolism and calcium homeostasis, and ↓ mitophagy pathway |
| Moriggi et al. [111] | 15 HC 10 LOPD | Muscle tissue | 2D-DIGE and LC-MS/MS | ↑ glycolysis and ↓ OXPHOS |
| de Moraes et al. [100] | 8 IOPD 14 LOPD | Urine | LC-HRMAS | ↓ Glc4, Hex5, Hex6, and Hex7 |
| Study | Study Design | Treatment | Sample | Omics-Based Approach | Major Findings † |
|---|---|---|---|---|---|
| Moriggi et al. [111] | 10 LOPD untreated 10 LOPD treated | ERT | Muscle tissue | LC-MS/MS | ↓ glycolysis and gluconeogenesis |
| Kinton et al. [110] | 8 LOPD untreated 8 LOPD treated | ERT | Muscle tissue | Transcriptome profiling | ↑ mitophagy and ↓ sphingolipid and phospholipid metabolism, cytosolic calcium |
| Meena et al. [121] | 6 untreated GAA-KO 6 treated GAA-KO | ERT | Muscle tissue | CE-TOF/MS and CE-QqQMS | ↓ Gal1P, UDP-glucose, acetyl-CoA, citrate, succinate, fumarate, malate, and ↑ G1P, G6P, F6P, pyruvate and lactate |
| Colella et al. [128] | 3 untreated GAA-KO 3 treated GAA-KO | AAV | Muscle tissue and spinal cord | Transcriptome profiling | In skeletal muscle: ↑ glycogen degradation, glucose and glucose-1-phosphate degradation, and serine and glycine biosynthesis In spinal cord: ↑ nervous system disease, neuroinflammation, immunity and energy sensing |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Cebrián, N.; Gras-Colomer, E.; Poveda Andrés, J.L.; Pineda-Lucena, A.; Puchades-Carrasco, L. Omics-Based Approaches for the Characterization of Pompe Disease Metabolic Phenotypes. Biology 2023, 12, 1159. https://doi.org/10.3390/biology12091159
Gómez-Cebrián N, Gras-Colomer E, Poveda Andrés JL, Pineda-Lucena A, Puchades-Carrasco L. Omics-Based Approaches for the Characterization of Pompe Disease Metabolic Phenotypes. Biology. 2023; 12(9):1159. https://doi.org/10.3390/biology12091159
Chicago/Turabian StyleGómez-Cebrián, Nuria, Elena Gras-Colomer, José Luis Poveda Andrés, Antonio Pineda-Lucena, and Leonor Puchades-Carrasco. 2023. "Omics-Based Approaches for the Characterization of Pompe Disease Metabolic Phenotypes" Biology 12, no. 9: 1159. https://doi.org/10.3390/biology12091159
APA StyleGómez-Cebrián, N., Gras-Colomer, E., Poveda Andrés, J. L., Pineda-Lucena, A., & Puchades-Carrasco, L. (2023). Omics-Based Approaches for the Characterization of Pompe Disease Metabolic Phenotypes. Biology, 12(9), 1159. https://doi.org/10.3390/biology12091159





