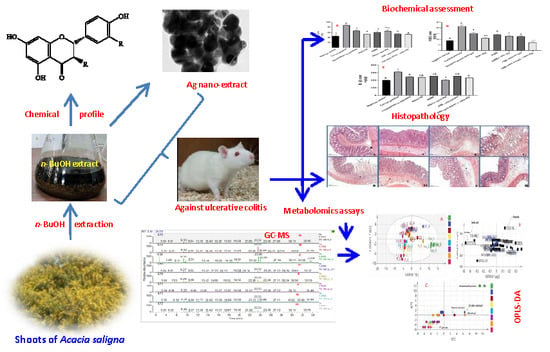
Protective Mechanism of Acacia saligna Butanol Extract and Its Nano-Formulations against Ulcerative Colitis in Rats as Revealed via Biochemical and Metabolomic Assays
Abstract
:1. Introduction
2. Materials and Methods
2.1. Plant Material, Extract Preparation and Phenolics Characterization
2.2. Drugs and Chemicals
2.3. Biosynthesis of ASBE Silver Nanoparticles (Ag-NPs)
2.4. UV–vis Spectra Measurements
2.5. Transmission Electron Microscopy (TEM)
2.6. Animals and Ethical Statements
2.7. Induction of UC in Rats
2.8. Experimental Design
2.9. Blood Collection, Colon Lesions Assessment, and Tissue Preparation
2.10. Metabolomics Samples Preparation and GC–MS Analysis
2.11. GC–MS Analysis
2.12. GC-MS Data Processing and Multivariate Chemometric Analysis
2.13. Biochemical Assessment of Colon Tissue
2.14. Histopathological Investigation
2.15. Statistical Analysis
3. Results and Discussion
3.1. Chemical Characterization of ASBE
3.2. Characterization of ASBE Silver Nanoparticles (Ag-NPs)
3.3. UV-vis Spectroscopy
3.4. Transmission Electron Microscopy (TEM)
3.5. Effect of ASBE and Its Nanoformulations against Acetic Acid induced UC in Rats Model Effect on Macroscopic Features
3.6. Effect on Colon Ulcer Indices
3.7. Effect on Inflammatory Biomarkers (COX-2, PGE2, IL-1β)
3.8. Histopathological Changes
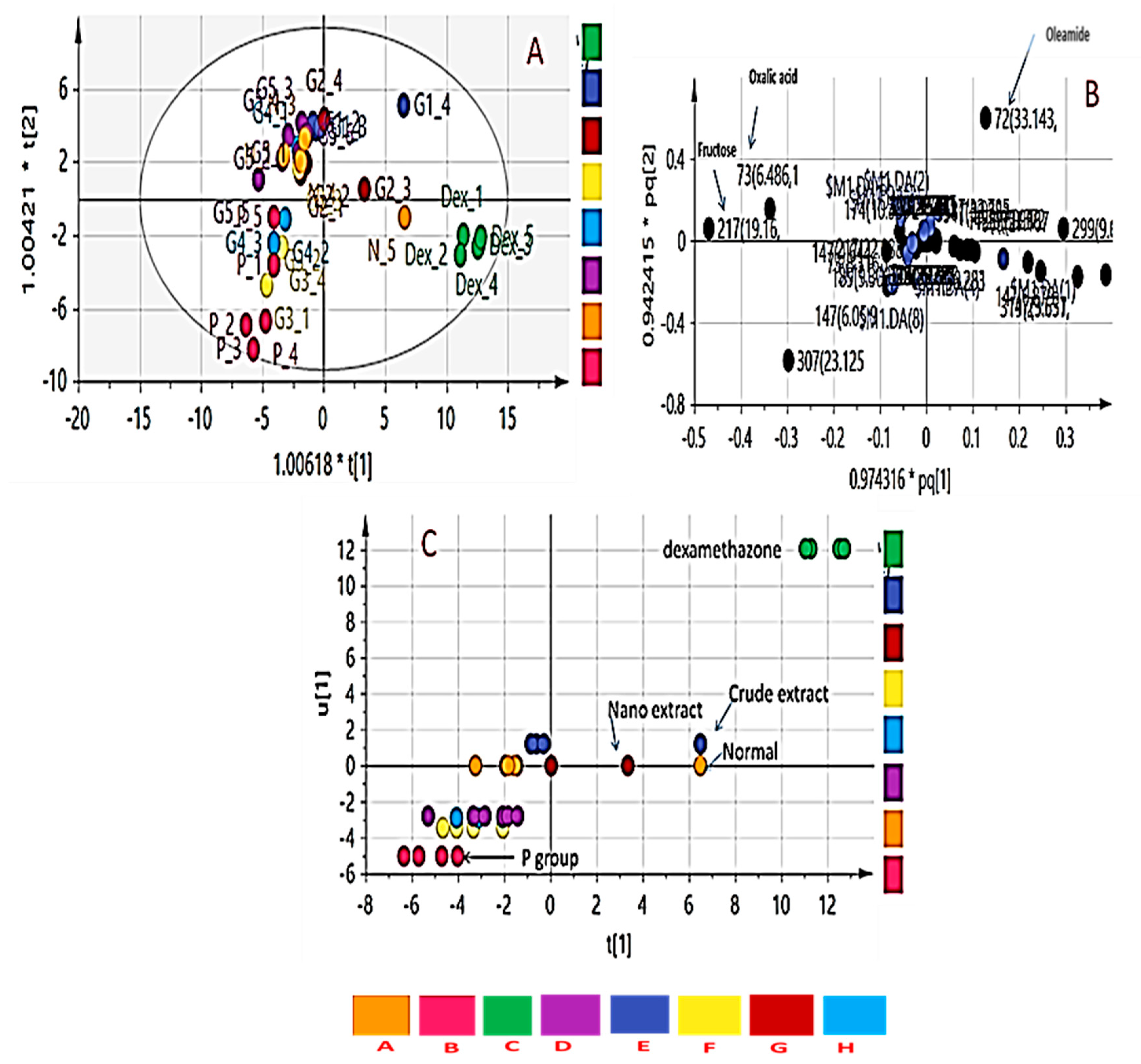
3.9. GC/MS Metabolomics Analysis of Rat Serum
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Seibel, J.; Molzberger, A.F.; Hertrampf, T.; Laudenbach-Leschowski, U.; Diel, P. Oral treatment with genistein reduces the expression of molecular and biochemical markers of inflammation in a rat model of chronic TNBS-induced colitis. Eur. J. Nutr. 2009, 48, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Hunt, R.; Quigley, E.; Abbas, Z.; Eliakim, A.; Emmanuel, A.; Goh, K.-L.; Guarner, F.; Katelaris, P.; Smout, A.; Umar, M. Coping with common gastrointestinal symptoms in the community: A global perspective on heartburn, constipation, bloating, and abdominal pain/discomfort May 2013. J. Clin. Gastroenterol. 2014, 48, 567–578. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.; Chan, F.K. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2018, 390, 2769–2778. [Google Scholar] [CrossRef]
- WHO. Diarrhoeal Disease. Fact Sheet Number 330. 2013. Available online: http://www.who.int/mediacentre/factsheets/fs330/en/ (accessed on 30 July 2015).
- Nguyen, G.T.; Phan, K.; Teng, I.; Pu, J.; Watanabe, T. A systematic review and meta-analysis of the prevalence of norovirus in cases of gastroenteritis in developing countries. Medicine 2017, 96, e8139. [Google Scholar] [CrossRef]
- Seegers, D.; Bouma, G.; Pena, A. A critical approach to new forms of treatment of Crohn’s disease and ulcerative colitis. Aliment. Pharm. Ther. 2002, 16, 53–58. [Google Scholar] [CrossRef]
- Bhol, K.; Alroy, J.; Schechter, P. Anti-inflammatory effect of topical nanocrystalline silver cream on allergic contact dermatitis in a guinea pig model. Clin. Exp. Dermatol. 2004, 29, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Bhol, K.C.; Schechter, P.J. Topical nanocrystalline silver cream suppresses inflammatory cytokines and induces apoptosis of inflammatory cells in a murine model of allergic contact dermatitis. Br. J. Dermatol. 2005, 152, 1235–1242. [Google Scholar] [CrossRef]
- Nicholson, J.K.; Lindon, J.C.; Holmes, E. ‘Metabonomics’: Understanding the metabolic responses of living systems to pathophysiological stimuli via multivariate statistical analysis of biological NMR spectroscopic data. Xenobiotica 1999, 29, 1181–1189. [Google Scholar] [CrossRef]
- Chen, C.; Shah, Y.M.; Morimura, K.; Krausz, K.W.; Miyazaki, M.; Richardson, T.A.; Morgan, E.T.; Ntambi, J.M.; Idle, J.R.; Gonzalez, F.J. Metabolomics reveals that hepatic stearoyl-CoA desaturase 1 downregulation exacerbates inflammation and acute colitis. Cell Metab. 2008, 7, 135–147. [Google Scholar] [CrossRef] [Green Version]
- Moco, S.; Vervoort, J.; Bino, R.J.; De Vos, R.C.; Bino, R. Metabolomics technologies and metabolite identification. TrAC Trend. Anal. Chem. 2007, 26, 855–866. [Google Scholar] [CrossRef]
- Tsugawa, H.; Tsujimoto, Y.; Sugitate, K.; Sakui, N.; Nishiumi, S.; Bamba, T.; Fukusaki, E. Highly sensitive and selective analysis of widely targeted metabolomics using gas chromatography/triple-quadrupole mass spectrometry. J. Biosci. Bioeng. 2014, 117, 122–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mushtaq, S.; Abbasi, B.H.; Uzair, B.; Abbasi, R. Natural products as reservoirs of novel therapeutic agents. EXCLI J. 2018, 17, 420–451. [Google Scholar] [PubMed]
- Wang, T.-Y.; Li, Q.; Bi, K.-S. Bioactive flavonoids in medicinal plants: Structure, activity and biological fate. Asian J. Pharm. Sci. 2018, 13, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Farrag, A.R.H.; Abdallah, H.M.; Khattab, A.R.; Elshamy, A.I.; El Gendy, A.E.-N.G.; Mohamed, T.A.; Farag, M.A.; Efferth, T.; Hegazy, M.-E.F. Antiulcer activity of Cyperus alternifolius in relation to its UPLC-MS metabolite fingerprint: A mechanistic study. Phytomedicine 2019, 62, 152970. [Google Scholar] [CrossRef]
- Rather, L.J.; Shahid, S.; Mohammad, F. Acacia nilotica (L.): A review of its traditional uses, phytochemistry, and pharmacology. Sustain. Chem. Pharm. 2015, 2, 12–30. [Google Scholar] [CrossRef]
- Malviya, S.; Rawat, S.; Kharia, A.; Verma, M. Medicinal attributes of Acacia nilotica Linn.-A comprehensive review on ethnopharmacological claims. Int. J. Pharm. Life Sci. 2011, 2, 830–837. [Google Scholar]
- Gedara, S.R.; Galala, A.A. New cytotoxic spirostane saponin and biflavonoid glycoside from the leaves of Acacia saligna (Labill.) HL Wendl. Nat. Prod. Res. 2014, 28, 324–329. [Google Scholar] [CrossRef]
- El-Toumy, S.A.; Salib, J.; Mohamed, W.; Morsy, F. Phytochemical and antimicrobial studies on Acacia saligna leaves. Egypt. J. Chem. 2010, 53, 705–717. [Google Scholar]
- Abd El-Gawad, A.M.; El-Amier, Y.A. Allelopathy and potential impact of invasive Acacia saligna on plant diversity in deltaic mediterranean coast of Egypt. Int. J. Environ. Res. 2015, 9, 923–932. [Google Scholar]
- Geissler, P.W.; Harris, S.A.; Prince, R.J.; Olsen, A.; Achieng’Odhiambo, R.; Oketch-Rabah, H.; Madiega, P.A.; Andersen, A.; Mølgaard, P. Medicinal plants used by Luo mothers and children in Bondo district, Kenya. J. Ethnopharmacol. 2002, 83, 39–54. [Google Scholar] [CrossRef]
- Bukhari, I.A.; Khan, R.A.; Gilani, A.H.; Ahmed, S.; Saeed, S.A. Analgesic, anti-inflammatory and anti-platelet activities of the methanolic extract of Acacia modesta leaves. Inflammopharmacology 2010, 18, 187–196. [Google Scholar] [CrossRef]
- Xiong, J.; Grace, M.H.; Esposito, D.; Wang, F.; Lila, M.A. Phytochemical characterization and anti-inflammatory properties of Acacia mearnsii leaves. Nat. Prod. Commun. 2016, 11, 649–653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Afsar, T.; Khan, M.R.; Razak, S.; Ullah, S.; Mirza, B. Antipyretic, anti-inflammatory and analgesic activity of Acacia hydaspica R. Parker and its phytochemical analysis. BMC Complem. Altern. Med. 2015, 15, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elshamy, A.I.; Ammar, N.M.; Hassan, H.A.; Al-Rowaily, S.L.; Raga, T.R.; El Gendy, A.; Abd-ElGawad, A.M. Essential oil and its nanoemulsion of Araucaria heterophylla resin: Chemical characterization, anti-inflammatory, and antipyretic activities. Ind. Crops Prod. 2020, 148, 112272. [Google Scholar] [CrossRef]
- Buzea, C.; Pacheco, I.I.; Robbie, K. Nanomaterials and nanoparticles: Sources and toxicity. Biointerphases 2007, 2, MR17–MR71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Irving, B. Nanoparticle drug delivery systems. Innov. Pharm. Biotechnol. 2007, 24, 58–62. [Google Scholar]
- Jiminez, J.A.; Uwiera, T.C.; Inglis, G.D.; Uwiera, R.R.E. Animal models to study acute and chronic intestinal inflammation in mammals. Gut Pathog. 2015, 7, 29. [Google Scholar] [CrossRef] [Green Version]
- Gonzalez, R.; Rodriguez, S.; Romay, C.; GONZÁLEZ, A.; ARMESTO, J.; REMIREZ, D.; MERINO, N. Anti-inflammatory activity of phycocyanin extract in acetic acid-induced colitis in rats. Pharm. Res. 1999, 39, 55–59. [Google Scholar] [CrossRef]
- Boulos, L. Flora of Egypt; Al Hadara Publishing: Cairo, Egypt, 1999. [Google Scholar]
- Tackholm, V. Students’ Flora of Egypt, 2nd ed.; Cairo University Press: Cairo, Egypt, 1974. [Google Scholar]
- Abdallah, H.M.I.; Elshamy, A.I.; El Gendy, A.E.-N.G.; Abd El-Gawad, A.M.; Omer, E.A.; De Leo, M.; Pistelli, L. Anti-inflammatory, antipyretic, and antinociceptive effects of a Cressa cretica aqueous extract. Planta Med. 2017, 83, 1313–1320. [Google Scholar] [CrossRef]
- Elshamy, A.I.; Abdallah, H.M.I.; El Gendy, A.E.-N.G.; El-Kashak, W.; Muscatello, B.; De Leo, M.; Pistelli, L. Evaluation of anti-inflammatory, antinociceptive, and antipyretic activities of Prunus persica var. nucipersica (nectarine) kernel. Planta Med. 2019, 85, 1016–1023. [Google Scholar] [CrossRef]
- Emam, M.; El Raey, M.A.; Eisa, W.H.; El-Haddad, A.E.; Osman, S.M.; El-Ansari, M.A.; Rabie, A.-G.M. Green synthesis of silver nanoparticles from Caesalpinia gilliesii (Hook) leaves: Antimicrobial activity and in vitro cytotoxic effect against BJ-1 and MCF-7 cells. J. Appl. Pharm. Sci. 2017, 7, 226–233. [Google Scholar]
- Hegazy, G.A.; Alnoury, A.M.; Gad, H.G. The role of Acacia Arabica extract as an antidiabetic, antihyperlipidemic, and antioxidant in streptozotocin-induced diabetic rats. Saudi Med. J. 2013, 34, 727–733. [Google Scholar] [PubMed]
- Buell, M.G.; Berin, M.C. Neutrophil-independence of the initiation of colonic injury. Digest. Dis. Sci. 1994, 39, 2575–2588. [Google Scholar] [CrossRef]
- Minaian, M.; Ghannadi, A.; Karimzadeh, A. Anti-ulcerogenic effect of ginger (rhizome of Zingiber officinale Roscoe) on cystemine induced duodenal ulcer in rats. DARU J. Pharm. Sci. 2006, 14, 97–101. [Google Scholar]
- Hassan, H.A.; Ammar, N.M.; Serag, A.; Shaker, O.G.; El Gendy, A.; Abdel-Hamid, A.Z. Metabolomics driven analysis of obesity-linked colorectal cancer patients via GC-MS and chemometrics: A pilot study. Microchem. J. 2020, 155, 104742. [Google Scholar] [CrossRef]
- Raish, M.; Ahmad, A.; Jan, B.L.; Alkharfy, K.M.; Mohsin, K.; Ahamad, S.R.; Ansari, M.A. GC-MS-based metabolomic profiling of thymoquinone in streptozotocin-induced diabetic nephropathy in rats. Nat. Prod. Commun. 2017, 12, 553–558. [Google Scholar] [CrossRef] [Green Version]
- Suvarana, K.; Layton, C.; Bancroft, J. Theory And Practice of Histological Techniques; Churchill Livingstone: New York, NY, USA, 2012; Volume 7. [Google Scholar]
- Rivero, P.J.; Goicoechea, J.; Urrutia, A.; Arregui, F.J. Effect of both protective and reducing agents in the synthesis of multicolor silver nanoparticles. Nanoscale Res. Lett. 2013, 8, 101. [Google Scholar] [CrossRef] [Green Version]
- Ragab, T.I.; Nada, A.A.; Ali, E.A.; Soliman, A.A.; Emam, M.; El Raey, M.A. Soft hydrogel based on modified chitosan containing P. granatum peel extract and its nano-forms: Multiparticulate study on chronic wounds treatment. Int. J. Biol. Macromol. 2019, 135, 407–421. [Google Scholar] [CrossRef]
- D’Argenio, G.; Mazzone, G.; Tuccillo, C.; Ribecco, M.T.; Graziani, G.; Gravina, A.G.; Caserta, S.; Guido, S.; Fogliano, V.; Caporaso, N. Apple polyphenols extract (APE) improves colon damage in a rat model of colitis. Diges. Liver Dis. 2012, 44, 555–562. [Google Scholar] [CrossRef]
- Hartmann, R.M.; Martins, M.I.M.; Tieppo, J.; Fillmann, H.S.; Marroni, N.P. Effect of Boswellia serrata on antioxidant status in an experimental model of colitis rats induced by acetic acid. Diges. Liver Dis. 2012, 57, 2038–2044. [Google Scholar] [CrossRef]
- Harputluoglu, M.; Demirel, U.; Yücel, N.; Karadağ, N.; Temel, I.; Firat, S.; Ara, C.; Aladağ, M.; Karincaoğlu, M.; Hilmioğlu, F. The effects of Gingko biloba extract on acetic acid-induced colitis in rats. Turk. J. Gastroenterol. 2006, 17, 177–182. [Google Scholar] [PubMed]
- El-Abhar, H.S.; Hammad, L.N.; Gawad, H.S.A. Modulating effect of ginger extract on rats with ulcerative colitis. J. Ethnopharmacol. 2008, 118, 367–372. [Google Scholar] [CrossRef]
- Popov, S.V.; Markov, P.A.; Nikitina, I.R.; Petrishev, S.; Smirnov, V.; Ovodov, Y.S. Preventive effect of a pectic polysaccharide of the common cranberry Vaccinium oxycoccos L. on acetic acid-induced colitis in mice. World J. Gastroenterol. 2006, 12, 6646–6651. [Google Scholar] [CrossRef] [PubMed]
- Al-Rejaie, S.S.; Abuohashish, H.M.; Ahmed, M.M.; Aleisa, A.M.; Alkhamees, O. Possible biochemical effects following inhibition of ethanol-induced gastric mucosa damage by Gymnema sylvestre in male Wistar albino rats. Pharm. Biol. 2012, 50, 1542–1550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sands, B.E. Therapy of inflammatory bowel disease. Gastroenterology 2000, 118, S68–S82. [Google Scholar] [CrossRef]
- Ham, M.; Moss, A.C. Mesalamine in the treatment and maintenance of remission of ulcerative colitis. Expert Rev. Clin. Pharmacol. 2012, 5, 113–123. [Google Scholar] [CrossRef]
- Su, C.; Salzberg, B.A.; Lewis, J.D.; Deren, J.J.; Kornbluth, A.; Katzka, D.A.; Stein, R.B.; Adler, D.R.; Lichtenstein, G.R. Efficacy of anti-tumor necrosis factor therapy in patients with ulcerative colitis. Am. J. Gastroenterol. 2002, 97, 2577–2584. [Google Scholar] [CrossRef]
- Lichtenstein, G.R.; Abreu, M.T.; Cohen, R.; Tremaine, W. American gastroenterological Association Institute medical position statement on corticosteroids, immunomodulators, and infliximab in inflammatory bowel disease. Gastroenterology 2006, 130, 935–939. [Google Scholar] [CrossRef]
- Timmer, A.; Patton, P.H.; Chande, N.; McDonald, J.W.; MacDonald, J.K. Azathioprine and 6-mercaptopurine for maintenance of remission in ulcerative colitis. Cochrane Database Syst. Rev. 2016, 2016, CD000478. [Google Scholar] [CrossRef]
- Griaham, M. Oxidants and free radicals in inflammatory bowel disease. Lancet 1994, 344, 859–861. [Google Scholar] [CrossRef]
- Pavlick, K.P.; Laroux, F.S.; Fuseler, J.; Wolf, R.E.; Gray, L.; Hoffman, J.; Grisham, M.B. Role of reactive metabolites of oxygen and nitrogen in inflammatory bowel disease. Free Radic. Biol. Med. 2002, 33, 311–322. [Google Scholar] [CrossRef]
- Tahan, G.; Aytac, E.; Aytekin, H.; Gunduz, F.; Dogusoy, G.; Aydin, S.; Tahan, V.; Uzun, H. Vitamin E has a dual effect of anti-inflammatory and antioxidant activities in acetic acid–induced ulcerative colitis in rats. Can. J. Surg. 2011, 54, 333–338. [Google Scholar] [CrossRef] [Green Version]
- Stucchi, A.; Reed, K.; O’Brien, M.; Cerda, S.; Andrews, C.; Gower, A.; Bushell, K.; Amar, S.; Leeman, S.; Becker, J. A new transcription factor that regulates TNF-α gene expression, LITAF, is increased in intestinal tissues from patients with CD and UC. Inflamm. Bowel Dis. 2006, 12, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Bessler, H.; Djaldetti, R.; Salman, H.; Bergman, M.; Djaldetti, M. IL-1β, IL-2, IL-6 and TNF-α production by peripheral blood mononuclear cells from patients with Parkinson’s disease. Biomed. Pharmacother. 1999, 53, 141–145. [Google Scholar] [CrossRef]
- Nehmé, A.; Edelman, J. Dexamethasone inhibits high glucose–, TNF-α–, and IL-1β–induced secretion of inflammatory and angiogenic mediators from retinal microvascular pericytes. Investig. Ophthalmol. Vis. Sci. 2008, 49, 2030–2038. [Google Scholar] [CrossRef] [PubMed]
- Sheikpranbabu, S.; Kalishwaralal, K.; Venkataraman, D.; Eom, S.H.; Park, J.; Gurunathan, S. Silver nanoparticles inhibit VEGF-and IL-1β-induced vascular permeability via Src dependent pathway in porcine retinal endothelial cells. J. Nanobiotechnol. 2009, 7, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Otani, T.; Yamaguchi, K.; Scherl, E.; Du, B.; Tai, H.-H.; Greifer, M.; Petrovic, L.; Daikoku, T.; Dey, S.K.; Subbaramaiah, K. Levels of NAD+-dependent 15-hydroxyprostaglandin dehydrogenase are reduced in inflammatory bowel disease: Evidence for involvement of TNF-α. Am. J. Physiol. Gastrointest. Liver Physiol. 2006, 290, G361–G368. [Google Scholar] [CrossRef]
- Hämäläinen, M.; Nieminen, R.; Vuorela, P.; Heinonen, M.; Moilanen, E. Anti-inflammatory effects of flavonoids: Genistein, kaempferol, quercetin, and daidzein inhibit STAT-1 and NF-κB activations, whereas flavone, isorhamnetin, naringenin, and pelargonidin inhibit only NF-κB activation along with their inhibitory effect on iNOS expression and NO production in activated macrophages. Mediat. Inflamm. 2007, 2007, 45673. [Google Scholar]
- Al-Rejaie, S.S.; Abuohashish, H.M.; Al-Enazi, M.M.; Al-Assaf, A.H.; Parmar, M.Y.; Ahmed, M.M. Protective effect of naringenin on acetic acid-induced ulcerative colitis in rats. World J. Gastroenterol. 2013, 19, 5633–5644. [Google Scholar] [CrossRef]
- Bilia, A.R.; Guccione, C.; Isacchi, B.; Righeschi, C.; Firenzuoli, F.; Bergonzi, M.C. Essential oils loaded in nanosystems: A developing strategy for a successful therapeutic approach. Evid. Based Complementary Altern. Med. 2014, 2014, 651593. [Google Scholar] [CrossRef] [Green Version]
- Bhol, K.C.; Schechter, P.J. Effects of nanocrystalline silver (NPI 32101) in a rat model of ulcerative colitis. Digest. Dis. Sci. 2007, 52, 2732–2742. [Google Scholar] [CrossRef] [PubMed]
- Siczek, K.; Zatorski, H.; Chmielowiec-Korzeniowska, A.; Pulit-Prociak, J.; Śmiech, M.; Kordek, R.; Tymczyna, L.; Banach, M.; Fichna, J. Synthesis and evaluation of anti-inflammatory properties of silver nanoparticle suspensions in experimental colitis in mice. Chem. Biol. Drug Des. 2017, 89, 538–547. [Google Scholar] [CrossRef] [PubMed]
- Song, W.-B.; Lv, Y.-H.; Zhang, Z.-S.; Li, Y.-N.; Xiao, L.-P.; Yu, X.-P.; Wang, Y.-Y.; Ji, H.-L.; Ma, L. Soluble intercellular adhesion molecule-1, D-lactate and diamine oxidase in patients with inflammatory bowel disease. World J. Gastroenterol. 2009, 15, 3916–3919. [Google Scholar] [CrossRef] [PubMed]
- Vernia, P.; Caprilli, R.; Latella, G.; Barbetti, F.; Magliocca, F.M.; Cittadini, M. Fecal lactate and ulcerative colitis. Gastroenterology 1988, 95, 1564–1568. [Google Scholar] [CrossRef]
- Schicho, R.; Nazyrova, A.; Shaykhutdinov, R.; Duggan, G.; Vogel, H.J.; Storr, M. Quantitative metabolomic profiling of serum and urine in DSS-induced ulcerative colitis of mice by 1H NMR spectroscopy. J. Proteome Res. 2010, 9, 6265–6273. [Google Scholar] [CrossRef]
- Martin, F.-P.J.; Rezzi, S.; Philippe, D.; Tornier, L.; Messlik, A.; Hölzlwimmer, G.; Baur, P.; Quintanilla-Fend, L.; Loh, G.; Blaut, M. Metabolic assessment of gradual development of moderate experimental colitis in IL-10 deficient mice. J. Proteome Res. 2009, 8, 2376–2387. [Google Scholar] [CrossRef]
- Schicho, R.; Shaykhutdinov, R.; Ngo, J.; Nazyrova, A.; Schneider, C.; Panaccione, R.; Kaplan, G.G.; Vogel, H.J.; Storr, M. Quantitative metabolomic profiling of serum, plasma, and urine by 1H NMR spectroscopy discriminates between patients with inflammatory bowel disease and healthy individuals. J. Proteome Res. 2012, 11, 3344–3357. [Google Scholar] [CrossRef]
- Sharma, U.; Singh, R.R.; Ahuja, V.; Makharia, G.K.; Jagannathan, N.R. Similarity in the metabolic profile in macroscopically involved and un-involved colonic mucosa in patients with inflammatory bowel disease: An in vitro proton (1H) MR spectroscopy study. Magn. Reson. Imaging 2010, 28, 1022–1029. [Google Scholar] [CrossRef]
- Le Gall, G.; Noor, S.O.; Ridgway, K.; Scovell, L.; Jamieson, C.; Johnson, I.T.; Colquhoun, I.J.; Kemsley, E.K.; Narbad, A. Metabolomics of fecal extracts detects altered metabolic activity of gut microbiota in ulcerative colitis and irritable bowel syndrome. J. Proteome Res. 2011, 10, 4208–4218. [Google Scholar] [CrossRef]
- Lin, X.; Liu, X.; Xu, J.; Cheng, K.-K.; Cao, J.; Liu, T.; Liu, Q.; Zhong, H.; Shen, G.; Dong, J. Metabolomics analysis of herb-partitioned moxibustion treatment on rats with diarrhea-predominant irritable bowel syndrome. Chin. Med. 2019, 14, 18. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, S.R.; Herman, C.E.; MacIver, N.J.; Wofford, J.A.; Wieman, H.L.; Hammen, J.J.; Rathmell, J.C. Glucose uptake is limiting in T cell activation and requires CD28-mediated Akt-dependent and independent pathways. J. Immunol. 2008, 180, 4476–4486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farag, M.A.; Abdelwareth, A.; Sallam, I.E.; El Shorbagi, M.; Jehmlich, N.; Fritz, K.; Rolle-Kampczyk, U.; Ehrlich, A.; Wessjohann, L.A.; von Bergen, M. Metabolomics reveals impact of seven functional foods on metabolic pathways in a gut microbiota model. J. Advan. Res. 2020, 23, 47–59. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Liu, Y.; Li, H.; Wang, L.; Xue, L.; Yin, G.; Wu, X. Identification of psoriasis vulgaris biomarkers in human plasma by non-targeted metabolomics based on UPLC-Q-TOF/MS. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 3940–3950. [Google Scholar] [PubMed]
- Ano, Y.; Ozawa, M.; Kutsukake, T.; Sugiyama, S.; Uchida, K.; Yoshida, A.; Nakayama, H. Preventive effects of a fermented dairy product against Alzheimer’s disease and identification of a novel oleamide with enhanced microglial phagocytosis and anti-inflammatory activity. PLoS ONE 2015, 10, e0118512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dionisi, M.; Alexander, S.P.; Bennett, A.J. Oleamide activates peroxisome proliferator-activated receptor gamma (PPARγ) in vitro. Lipids Health Dis. 2012, 11, 51. [Google Scholar] [CrossRef] [Green Version]
- Oh, Y.T.; Lee, J.Y.; Lee, J.; Lee, J.H.; Kim, J.-E.; Ha, J.; Kang, I. Oleamide suppresses lipopolysaccharide-induced expression of iNOS and COX-2 through inhibition of NF-κB activation in BV2 murine microglial cells. Neurosci. Lett. 2010, 474, 148–153. [Google Scholar] [CrossRef]
- Yamanaka, M.; Ishikawa, T.; Griep, A.; Axt, D.; Kummer, M.P.; Heneka, M.T. PPARγ/RXRα-induced and CD36-mediated microglial amyloid-β phagocytosis results in cognitive improvement in amyloid precursor protein/presenilin 1 mice. J. Neurosci. 2012, 32, 17321–17331. [Google Scholar] [CrossRef] [Green Version]
- Sun, Y.; Chen, S.; Wei, R.; Xie, X.; Wang, C.; Fan, S.; Zhang, X.; Su, J.; Liu, J.; Jia, W. Metabolome and gut microbiota variation with long-term intake of Panax ginseng extracts on rats. Food Funct. 2018, 9, 3547–3556. [Google Scholar] [CrossRef]
- Miles, E.A.; Calder, P.C. Influence of marine n-3 polyunsaturated fatty acids on immune function and a systematic review of their effects on clinical outcomes in rheumatoid arthritis. Br. J. Nutr. 2012, 107, S171–S184. [Google Scholar] [CrossRef] [Green Version]







| Group | Weight/Length Ratio (g/cm) | Lesion Score (0–5) | Ulcer Area (mm2) | Ulcer Index (UI) | Mortality (Dead/Total%) |
|---|---|---|---|---|---|
| Control Negative | 0.127 ± 0.007 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0/6 (0.0%) |
| Control Positive | 0.251 ± 0.028 a | 5.50 ± 0.879 a | 18.75 ± 0.994 a | 24.25 ± 1.546 a | 1/6 (16.66%) |
| Dexamethasone | 0.155 ± 0.016 * | 3.97 ± 0.590 *a | 11.75 ± 1.258 *a | 15.72 ± 1.118 *a | 1/6 (16.66%) |
| Nano Ag | 0.151 ± 0.004 * | 4.00 ± 0.182 *a | 8.87 ± 1.250 *a | 12.87 ± 1.109 *a | 0/6 (0.0%) |
| ASBE | 0.202 ± 0.013 *a | 4.20 ± 0.258 *a | 13.50 ± 0.577 *a | 17.70 ± 0.365 *a | 1/6 (16.66%) |
| ASBE + Nano Ag | 0.174 ± 0.011 *a | 4.02 ± 0.427 *a | 8.62 ± 1.109 *a | 12.65 ± 1.318 *a | 0/6 (0.0%) |
| ASB Nano ext. | 0.193 ± 0.015 *a | 4.17 ± 0.550 *a | 9.95 ± 0.823 *a | 14.14 ± 0.842 *a | 1/6 (16.66%) |
| ASB Nano ext. + Nano Ag | 0.146 ± 0.010 * | 3.50 ± 0.294 *a | 8.50 ± 1.291 *a | 12.00 ± 1.010 *a | 0/6 (0.0%) |
| Metabolites | Fold Change * | ||||||
|---|---|---|---|---|---|---|---|
| B/A | C/B | D/B | E/B | F/B | G/B | H/B | |
| Lactic Acid | 2.30 * | 0.095 * | 0.29 * | 0.63 | 0.79 | 0.46 * | 0.80 |
| Oxalic Acid | 1.026 | 0.15 * | 1.93 | 0.42 | 0.93 | 0.52 | 1.15 |
| Pyroglutamic Acid | 3.06 * | 16.36 * | 0.33 * | 0.117 * | 0.38 * | 0.45 * | 0.33 * |
| D-Fructose | 2.52* | 0.19 * | 0.94 | 0.84 | 0.98 | 0.85 | 1.01 |
| D- Sorbitol | 5.77 * | 1.027 | 0.89 | 0.64 | 2.46 * | 1.47 | 3.42 * |
| D-Fructose | 21.32 * | 0.018 * | 0.11 * | 0.17 * | 0.76 | 0.31 * | 0.48 |
| Arachidonic Acid | 0.25 * | 7.51 * | 3.91 * | 2.38 | 1.44 | 1.40 | 1.70 |
| Oleamide | 0.051 * | 16.84 * | 17.53 | 31.53 * | 12.66 * | 31.47 * | 14.31 |
| Erucylamide | 0.23 * | 15.90 * | 1.99 * | 0.92 | 0.73 | 0.77 | 1.49 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdallah, H.M.I.; Ammar, N.M.; Abdelhameed, M.F.; Gendy, A.E.-N.G.E.; Ragab, T.I.M.; Abd-ElGawad, A.M.; Farag, M.A.; Alwahibi, M.S.; Elshamy, A.I. Protective Mechanism of Acacia saligna Butanol Extract and Its Nano-Formulations against Ulcerative Colitis in Rats as Revealed via Biochemical and Metabolomic Assays. Biology 2020, 9, 195. https://doi.org/10.3390/biology9080195
Abdallah HMI, Ammar NM, Abdelhameed MF, Gendy AE-NGE, Ragab TIM, Abd-ElGawad AM, Farag MA, Alwahibi MS, Elshamy AI. Protective Mechanism of Acacia saligna Butanol Extract and Its Nano-Formulations against Ulcerative Colitis in Rats as Revealed via Biochemical and Metabolomic Assays. Biology. 2020; 9(8):195. https://doi.org/10.3390/biology9080195
Chicago/Turabian StyleAbdallah, Heba M.I., Naglaa M. Ammar, Mohamed F. Abdelhameed, Abd El-Nasser G. El Gendy, Tamer I. M. Ragab, Ahmed M. Abd-ElGawad, Mohamed A. Farag, Mona S. Alwahibi, and Abdelsamed I. Elshamy. 2020. "Protective Mechanism of Acacia saligna Butanol Extract and Its Nano-Formulations against Ulcerative Colitis in Rats as Revealed via Biochemical and Metabolomic Assays" Biology 9, no. 8: 195. https://doi.org/10.3390/biology9080195