Abstract
Facial hyperpigmentation is a highly prevalent dermatological condition, characterized by dark spots on the skin resulting from excess melanin production. Hyperpigmentation significantly impacts patients’ quality of life and self-esteem. Current treatments often present disadvantages linked to poor product tolerability. A topical cosmetic approach combining three lightening active ingredients (tranexamic acid, niacinamide, vitamin C) offers a new option for treating dark spots on the skin. The present in-use test under dermatological control evaluated the clinical safety and efficacy of a cream and serum containing these three ingredients, formulated with hyaluronic acid for enhanced delivery, stability, and efficacy. A total of 22 Caucasian patients with facial hyperpigmentation, both male and female, aged between 45 and 67 years, applied the cream and serum for 8 weeks. Clinical assessments, colorimetric evaluations, standardized photography, and self-assessment questionnaires were used to measure outcomes. No serious adverse effects were recorded, and the incidence of local adverse effects was low, highlighting good tolerability of the investigated test items. In most participants, significant improvements in hyperpigmented areas were recorded. Clinical scoring by the dermatologist investigator indicated a statistically significant 13% reduction in color intensity and a 6% reduction in the size of dark spots after 8 weeks of treatment. Colorimetric evaluation showed a statistically significant 1% increase in luminosity (L* parameter) and an 8% improvement in the Individual Typological Angle (ITA°) in endpoint, indicating lighter skin spots. Subjective assessments reflected high user satisfaction, with 95% of participants noting improvements in skin hydration and luminosity, and 77% reporting a reduced appearance of dark spots. Overall, the present work supports the use of tranexamic acid, niacinamide, and vitamin C as an effective and well-tolerated combined topical management option for hyperpigmentation. This combination offers a viable alternative to classical whiteners for individuals seeking to reduce facial skin coloration imbalance and improve skin tone.
1. Introduction
Hyperpigmentation is a dermatological disorder characterized by patches of skin which are darker than the surrounding areas [1]. This condition results from excess melanin production by melanocytes, which accumulates in the dermis or epidermis, forming these dark patches [1]. As an umbrella term, hyperpigmentation encompasses various cutaneous conditions with diverse etiologies that can be either congenital or acquired [2]. Common hyperpigmentation disorders include post-inflammatory hyperpigmentation (PIH), melasma, solar lentigines, ephelides, and café au lait macules [2]. These conditions can be triggered by several factors, including internal factors like genetic predisposition and hormonal changes (e.g., melasma) or external factors, such as skin inflammation leading to PIH [2]. Sun exposure is a predominant cause of hyperpigmentation, contributing to the development of lentigines, also known as “age spots” [2]. The occurrence of these dark patches increases with age due to the decrease in melanocyte counts, particularly in individuals over 40 years of age [1].
Although hyperpigmentation does not typically pose a health risk, an abnormal skin pigmentation can significantly affect an individual’s self-perception, leading to psychological distress and a diminished quality of life due to the associated stigma [3,4]. Of note, there are various approaches for the treatment of hyperpigmentation. First-line therapy typically involves topical agents, while second-line treatments encompass procedures such as chemical peels and laser therapy [5]. Hydroquinone, a hydroxyphenolic compound, is considered the gold standard for the topical treatment of hyperpigmentation [6]. Typically used in concentrations ranging from 2% to 4%, hydroquinone is often combined with retinoids and steroids in formulations like the widely prescribed Kligmans’ regimen [6]. Despite its efficacy, hydroquinone has been linked to several adverse effects, including skin irritation, facial swelling, contact dermatitis, and ochronosis [6]. Consequently, it is available only by prescription in many countries (e.g., EU members) and has been banned from over-the-counter sale by the FDA since 2020 under the CARE Act [7]. These safety concerns have driven the search for novel skin-lightening agents and new formulations which offer both equivalent efficacy and an improved safety profile. These potential agents notably include tranexamic acid (TXA), niacinamide, ascorbic acid, azelaic acid, salicylic acid, and kojic acid [8]. Additionally, the inclusion of appropriate sunscreen use in conjunction with any anti-hyperpigmentation treatment is advised to ensure effectiveness [8].
TXA, a synthetic derivative of lysine, was originally employed as a plasmin inhibitor to achieve hemostasis [9]. Recent studies have also demonstrated the potential of TXA as a local treatment for skin hyperpigmentation due to its anti-inflammatory properties. Specifically, by inhibiting the conversion of plasminogen to plasmin in keratinocytes, TXA decreases the synthesis of inflammatory mediators such as arachidonic acid and prostaglandins, whose increase induced by UV radiation stimulates melanocytes. Thus, by disrupting the keratinocyte–melanocyte interactions, TXA effectively decreases melanin production [9]. Several studies have confirmed the efficacy of topical TXA in treating hyperpigmentation, identifying optimal concentrations between 2% and 5%, with no reported serious adverse effects [8,10,11,12]. Notably, a topical formulation containing 3% TXA has demonstrated efficacy comparable to the combined effects of hydroquinone and dexamethasone in treating melasma, while exhibiting a superior safety profile [11]. Of further note, TXA is registered in the European CosIng database and is recognized by the European Chemicals Agency (ECHA) for its consumer uses in products such as cosmetics and personal care items. From a safety standpoint, topical TXA presents low overall thrombotic risks, despite its inherent procoagulant nature. Of note, higher risks are documented for the oral use of TXA in dermatology [13]. However, when used topically at a concentration of 3%, the risk of systemic side effects (i.e., including thrombosis) is significantly minimized. Studies have demonstrated that topical application of TXA at this concentration does not result in detectable systemic absorption, thereby alleviating concerns related to its procoagulant properties [13].
Niacinamide (or nicotinamide) is a component of the vitamin B3 complex, serving as a precursor to the key coenzymes nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP). These coenzymes play critical roles in cellular energy metabolism and DNA repair mechanisms, supporting fundamental processes which are vital for cellular integrity and function [14]. Thus, niacinamide exerts multiparametric beneficial effects on skin health due to its various properties, such as anti-inflammatory and antioxidant actions, partly attributable to its role as a coenzyme precursor [15,16]. It is widely used in dermatological topical formulas due to its ability to regulate sebum production, improve skin barrier functions, and ameliorate skin aging signs [15]. Furthermore, previous studies have demonstrated niacinamide’s efficacy in addressing hyperpigmentation, wherein it inhibits melanosome transfer from melanocytes to keratinocytes, decreasing the transfer of melanin to the superficial layers of the skin [15,16]. Additionally, niacinamide suppresses tyrosinase activity, consequently impeding melanin synthesis [15,16]. In cosmetic formulations, niacinamide’s water solubility and stability make it a well-tolerated agent, usually formulated at 4% to 5% concentrations [14]. Clinical trials have demonstrated its efficacy in reducing hyperpigmentation and improving overall skin tone evenness [16].
Currently, many whitening creams promise a unified and radiant complexion, but their effectiveness is often not clinically proven or tested in vitro. Moreover, they can even pose unacceptable skin risks, particularly with the rise of homemade cosmetics manufactured by unqualified or unexperienced individuals [17]. Thus, the efficacy of a cream and serum protocol was prospectively clinically assessed herein (i.e., use of a combined approach) for its ability to manage facial hyperpigmentation, after repeated applications under normal conditions of use. Formulated with 3% TXA and 5% niacinamide, the cream was designed to harness the combined functions of these compounds. The serum was developed to complement the cream’s effects, also containing 3% TXA and 5% niacinamide. The serum additionally contained 2% vitamin C, known for its antioxidant properties, complementing the skin-tone-unifying effects of TXA and niacinamide by scavenging free radicals. Both formulations were enriched with hyaluronic acid (HA) to improve skin moisture and texture. Overall, the aim of the in-use test under dermatological control was to conjointly clinically assess the safety and efficacy of both topical formulas described hereabove. The primary hypothesis was that the test items are safe for human use under normal application conditions and that the test items procure whitening effects on facial dark spots. Generally, this work reported in-use evaluations for a topical cosmetic protocol developed for the management of facial hyperpigmentation.
2. Materials and Methods
2.1. In-Use Test Design
The presented 8-week pilot in-use test under dermatological control was conducted at a contract research organization (CRO; Cosmocare) in Barcelona, Spain, from March to May 2023. Participants aged 45 to 67 years exhibiting facial spots associated with skin aging, sunspots, and melasma, were enrolled in the in-use test under dermatological control. This age bracket was retained as it is representative of individuals who currently use a combination of cream and serum in their daily lives. Specifically, the inclusion of menopausal or post-menopausal female participants was preferred, justifying the retained age bracket. In terms of inclusion criteria, both female and male participants were included, reflecting a range of Caucasian skin types. Based on dermatological assessments at the time of inclusion, the participants’ Fitzpatrick skin types ranged from II to IV. Of note, the in-use test under dermatological control restricted the portion of participants with sensitive facial skin to a maximum of 60%, and those with skin displaying atopic tendencies to a maximum of 25%. All participants provided informed consent and demonstrated comprehension of the study language. Participants were required to maintain their cosmetic routines unchanged during the study (i.e., in the studied skin area) and for the preceding 15 days. Additionally, participants were required to refrain from intense sun or UV radiation exposure for at least one month prior to and during the study period. The defined timepoints and phases of the study are presented in Table 1.

Table 1.
Overview of the clinical study design.
The exclusion criteria for the study encompassed (i) known intolerance or allergy to medications or other substances that might present unjustified risks; (ii) history of intolerance or allergy to similar cosmetic products; (iii) pregnancy or lactation; and (iv) current use of medications, such as acetylsalicylic acid or derivatives, antibiotics, anti-inflammatories, corticosteroids, antidepressants, antihistamines, or immunosuppressive treatments. Specifically, participants did not take medications and treatments that could either increase the likelihood of adverse reactions or interfere with the accurate assessment of the study’s outcomes. For example, any medication that increases skin sensitivity to sunlight (e.g., retinoids or some antibiotics and antifungals) was excluded. Another example is anti-inflammatories and corticosteroids, which can suppress inflammatory responses and might mask any irritation or adverse reactions caused by the study products. Additionally, individuals undergoing allergy desensitization treatment or presenting dermatological abnormalities in the studied skin area, such as irritation, erythema, scars, pigmentation disorders, abundant ephelides or nevi, were excluded from the study.
2.2. In-Use Test Demographics
The in-use test under dermatological control included 22 participants aged 45 to 67 years, all of whom completed the study without any deviations from the protocol (Table 2 and Table S1).

Table 2.
Participant demographics for the in-use test under dermatological control.
All the participants presented skin hyperpigmentation of the face. The participants exhibited a variety of skin types, including dry, normal, oily, and mixed oily (Table 2, Table S1). One participant reported skin sensitivity, and one participant presented skin with atopic tendency prior to the start of the in-use test under dermatological control (Table S1). One participant was excluded from the colorimetric analysis because the data obtained were outliers.
2.3. Investigational Test Items
The evaluated cosmetic formulations consisted of a cream and a serum. Both formulations were specifically developed for the presented in-use test under dermatological control in order to evaluate the safety and efficacy of the combined use of the retained active ingredients. Both formulas were prepared by ingredient homogenization at 70 °C in a pressurized reactor (Krieger, Muttenz, Switzerland), followed by controlled cooling and active ingredient incorporation at 20 °C. The semi-solid oil-in-water cream formulation comprised 3% tranexamic acid (Ami Lifesciences, Vadodara, India), 5% niacinamide (DSM, Heerlen, The Netherlands), and 0.25% sodium hyaluronate (hyaluronic acid; Givaudan, Vernier, Switzerland). The cream was conditioned in 50 mL airless clear glass containers and was conserved at ambient temperature before use. The complete ingredients of the cream formula were as follows (INCI denomination): Aqua (water), C15–19 Alkane, Dicaprylyl Carbonate, 2,3-Butanediol, Glyceryl Polymethacrylate, Niacinamide, Lactobacillus Ferment, Tranexamic Acid, Talc, Polyglycerin-6, Polyglyceryl-6 Laurate, Sodium Hyaluronate, Tocopherol, Sodium Acrylate/Sodium Acryloyldimethyl Taurate Copolymer, Sorbitan Isostearate, Sorbitan Oleate, Parfum (Fragrance), Citric Acid. The commercial reference of the cosmetic cream formulation was “T.X.A Intense Corrector Lightening Cream”. The serum formulation contained 3% tranexamic acid (Ami Lifesciences, Vadodara, India), 5% niacinamide (DSM, Heerlen, The Netherlands), 0.25% sodium hyaluronate (hyaluronic acid; Givaudan, Vernier, Switzerland), 0.75% hydrolyzed hyaluronic acid (i.e., low and medium-molecular-weight hyaluronic acid; Givaudan, Vernier, Switzerland), and 2% ascorbyl glucoside (i.e., vitamin C; Hayashibara, Okayama, Japan). The serum was conditioned in 30 mL airless clear glass containers and was conserved at ambient temperature before use. The ingredients of the serum formula were as follows (INCI denomination): Aqua (Water), 2,3-Butanediol, Niacinamide, Lactobacillus Ferment, Dimethicone, Tranexamic Acid, Ascorbyl Glucoside, Butylene Glycol, Hydrolyzed Hyaluronic Acid, Sodium Hyaluronate, Sodium Polyglutamate, Decyl Glucoside, Potassium Hydroxide, Polysilicone-11, PPG-26-Buteth-26, Parfum (Fragrance), Caprylyl Glycol, Citric Acid, Sodium Citrate, PEG-40 Hydrogenated Castor Oil. The commercial reference of the cosmetic serum formulation was “T.X.A Intense Corrector Lightening Serum”. Finished product density was determined with a Ph. Eur. pycnometer and pH values were determined on a SevenExcellence pH meter S400 (Mettler Toledo, Greifensee, Switzerland).
2.4. Protocol for Test Item Application
For the in-use test under dermatological control, participants followed specific guidelines for applying the cream and serum to the face and neck twice per day, in the morning and evening for 8 weeks. Participants applied 2 pumps of serum (or as much as necessary based on individual needs to cover the facial skin), onto clean and dry skin, gently massaging the area in circular motions until the product was fully absorbed (Figure S1). This care was followed by the application of 2 pumps of cream, which were applied in the same manner. It is noted that product quantity standardization could be implemented (e.g., fixed number of pump strokes, dispensing a fixed volume using a glass pipette) for future studies using larger participant groups. Following application of the test items, participants applied sunscreen with an SPF 50+ to the studied skin area. Participants were instructed not to use any other cosmetic products similar to those being tested during the in-use test under dermatological control, except for their usual cosmetic routine. All applications were performed by the participants at home under normal usage conditions. On the days of clinical examination, no other cosmetic products were applied.
2.5. Endpoints and Clinical Assessments
2.5.1. Clinical Assessments
An initial assessment of each participant’s compliance with the study criteria and the general condition of their facial skin was conducted by the dermatologist investigator. This assessment was followed by a clinical evaluation to identify facial hyperpigmentation spots. A specific pigmentation spot was identified for each participant. Two evaluation criteria were chosen, namely the intensity of the color and the size of the spot in centimeters. A semi-quantitative scale from 1 to 9 was established to assess the spot color, with the value 1 being very dark and the value 9 being very light.
2.5.2. Photographic Recording
To visually assess the appearance of the dark spots before and after repeated applications of the test items, multiple facial photographs were taken using the Observ 520® instrument (Reviderm, Sauerlach, Germany). For each participant, four photographs were taken. Two baseline images were gathered before applying any product to the skin and follow-up images were gathered after 56 days of repeated applications of the test items.
2.5.3. Colorimetric Evaluation of Dark Spots
Colorimetric evaluation was performed using a Chromameter CR-400 (Konica Minolta, Tokyo, Japan) to determine the intensity of skin pigmentation by calculating the Individual Typology Angle (ITA°). The ITA° value was calculated using the following formula:
Wherein the variable L* corresponded to luminosity/clarity, the variable b* corresponded to yellow-blue chromaticity, and the ITA° value corresponded to the individual typological angle [18]. Namely, the parameter L*, measured with the Chromameter CR-400, indicated the lightness of the spot, with a maximum value of 100 representing very light spots and a minimum value of 0 representing very dark spots. Changes in the L* value over time can indicate darkening or lightening of the skin. The parameter b* represented the skin chromaticity from yellow to blue. Positive values of b* are indicative of yellowness, whereas negative values suggest bluish tones. With these parameters determined, the ITA° could be calculated, where higher ITA° values were inversely related to pigmentation intensity (i.e., high values corresponded to light skin tones) [19]. Regarding anti-spot efficacy of the investigational protocol, pre-application values were used as a control (i.e., D0) for endpoint assessments, as previously methodologically described [20,21].
2.5.4. Participant Questionnaires
Participant-reported satisfaction was measured through a standardized user satisfaction questionnaire, which included subjective evaluations of the product’s texture, user experience, product effectiveness, and tolerability. Following a predefined test item usage period, participants completed the questionnaire at home, providing their feedback on various attributes of the products. In detail, the questionnaire was designed to capture various aspects of the care experience, including general satisfaction, suitability for skin type, sensory attributes (e.g., smell, texture), application characteristics (e.g., spreadability, absorption), and overall cosmetic efficacy.
The questionnaire consisted of 34 questions, divided into three main sections (i.e., Serum Evaluation [Questions 1–7], Cream Evaluation [Questions 8–14], and Combined Serum and Cream Evaluation [Questions 15–34]). Each question allowed for responses on a 4-point Likert scale, with (i) “Strongly agree”, (ii) “Somewhat agree”, (iii) “Somewhat disagree”, and (iv) “Strongly disagree”. Additionally, specific questions assessed the overall product evaluation and product preference by the participants. The responses were collected and analyzed to determine the levels of satisfaction and perceived efficacy of the test items. The frequency and percentage of all response options were reported for each question.
On a methodological note, the terms “strongly agree” and “rather agree” are commonly used in Likert scale questionnaires to capture varying degrees of agreement from participants. While these responses are subjective, they specifically serve to quantify subjective opinions in a standardized manner. The tool was standardized using a consistent 4-point Likert scale, which is a widely accepted method to quantify subjective opinions. The questionnaire was validated through pilot testing to ensure that participants understood the questions and that the scale accurately captured their level of agreement. Clear instructions were provided to participants, further reducing variability in responses.
2.5.5. Cutaneous Acceptability of Test Items
To evaluate the cutaneous acceptability of the test items, endpoint clinical examinations were conducted by the dermatologist investigator. The evaluations focused on identifying any cutaneous reactions potentially associated with test item use. The dermatologist investigator assessed the reactions based on the cause–effect relationship using the following criteria: (i) “No relation”, (ii) “Doubtful relation”, (iii) “Probable relation”, and (iv) “Very probable relation”. The interpretation of the results was based on the characteristics of the reactions, including intensity, location, duration, and frequency.
2.6. Statistical Analyses
A quantitative analysis of the clinical evaluation data was performed. Values obtained at the end of the study (i.e., D56) were compared to initial values (i.e., D0) using the non-parametric Wilcoxon test (i.e., two-tailed, significance cutoff of p-value < 0.05). Data were presented as means ± standard deviations. The quantitative analysis was performed for the instrumental colorimetric measurements using a paired t-test to compare the values obtained at the end of the study with the initial values. Data were expressed as means ± standard deviations and the significance cutoff for the paired t-test was of p-value < 0.05. Detailed statistical results may be found in the Results section. The statistical calculations and/or data presentation were performed using Microsoft Excel 365 v.2405 (Microsoft Corporation, Redmond, WA, USA), Microsoft PowerPoint 365 v.2405, and GraphPad Prism v.8.0.2 (GraphPad Software, San Diego, CA, USA).
3. Results
3.1. Test Item Formulation Analysis
Prior to the in-use test under dermatological control, the two test items were firstly technically benchmarked and analyzed from a product formulation perspective. Within a cream, key ingredients such as TXA and niacinamide provide specific functional benefits like skin-lightening effects [9,10,22]. Excipients support the function and delivery of key ingredients by improving the texture, preservation, and overall user experience [23,24]. For an emulsion, the temperature of incorporation is crucial for maintaining the integrity of key ingredients, as it affects their stability, efficacy, and the overall consistency of the final product [25,26]. The following tables outline the key ingredients of the two investigated cosmetic formulations, their respective roles, percentages, and temperatures of incorporation (Table 3 and Table 4).

Table 3.
Key active ingredients of the investigated cream formulation, their roles, percentages, and temperatures of incorporation. The cream formulation in finished form consisted of a white O/W emulsion with a density of 0.98 and a pH value of 5.25.

Table 4.
Key active ingredients of the investigated serum formulation, their roles, percentages, and temperatures of incorporation. The serum formulation in finished form consisted of a colorless fluid serum with a density of 1.04 and a pH value of 6.65.
Overall, the investigated test items were confirmed to present appropriate galenic forms, primary packaging, and physical characteristics for the considered clinical applications (Table 3 and Table 4). The listed indications for use of both products comprised post-care treatment for skin lightening, skin brightening, skin pigmentation, skin tone enhancement, and dark spot management.
3.2. Cutaneous Acceptability
The dermatologist investigator’s clinical evaluation of the tolerance parameters (i.e., erythema, dryness, burning, stinging, itching, and scaling) showed that the test items were very well tolerated over the 8-week study period. No cutaneous manifestation was imputed to the test items after 8 weeks of facial application under normal conditions of use (Figure S1). Specifically, no serious adverse effects or signs of intolerance were reported during the study or associated with the investigated test items. Adverse effects were seldom reported and were not associated with the investigated test items. Overall, the test items were assessed as being very well tolerated in the study conditions.
3.3. Standardized Photography Results
Standardized digital images capturing the facial skin of three selected study participants were acquired at the pre-treatment baseline (i.e., left column) and at week 8 (i.e., right column; Figure 1).
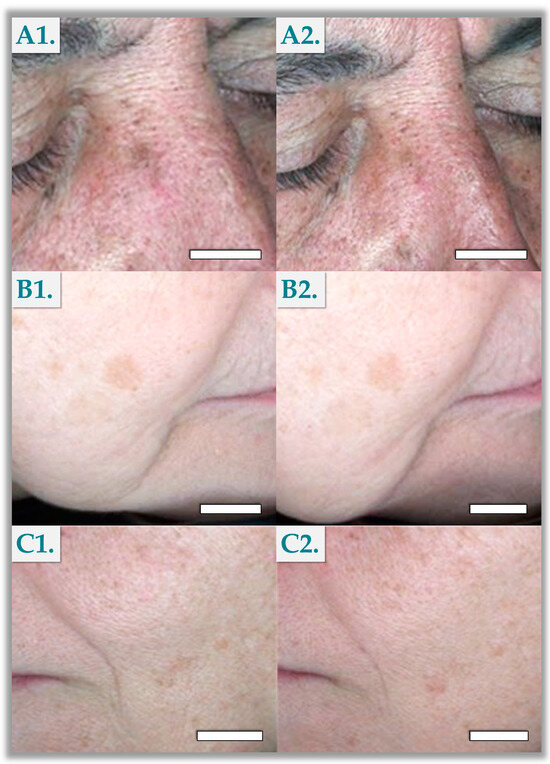
Figure 1.
Clinical imaging results for participants N°8 (A1,A2), N°12 (B1,B2), and N°18 (C1,C2). Scale bars = 5 mm.
The presented images illustrated the improvement in hyperpigmentation signs, reflecting typical improvements observed across the study population (Figure 1). Specifically, the monitored facial dark spots were observed to be dampened or less pronounced upon endpoint clinical examination of a majority of the participants. At that time, the monitored dark spots generally appeared less pronounced (i.e., less dark sharp edges) and appeared to blend better with the surrounding skin (Figure 1).
3.4. Colorimetric Evaluations
The values obtained at the end of the study, after repeated applications of the tested products, were compared with the initial values, using the paired t-test (i.e., two-tail, significance at p-value < 0.05). At week 8, the degree of skin pigmentation in the monitored dark spots, as measured by the ITA° parameter, showed a significant increase of 8% (p-value = 0.0162), indicating a notable lightening result (Table 5).

Table 5.
Results of the colorimetric evaluation (i.e., Chromameter CR-400) of facial dark spots. One participant was excluded from the analysis because the data obtained were outliers. Raw data may be found in Table S2.
This result was corroborated by a corresponding 1% increase in the L* parameter (p-value = 0.0326), reflecting an improvement in the luminosity of the skin on the corresponding dark spots (Table 5). Additionally, there was no significant change in the b* parameter, which remained stable (p-value = 0.9359), indicating consistent yellow–blue chromaticity of the skin throughout the treatment period (Table 5).
3.5. Self-Assessment Questionnaires
Participant self-assessment questionnaires revealed high levels of user satisfaction and perceived effectiveness of the investigated test items (Table S3). Over the 8-week study, 95% of the participants reported that the products left their skin hydrated, and 86% noted improvements in skin comfort, softness, and even tone. Additionally, 77% of participants observed a reduction in the size and intensity of dark spots, and 82% indicated they would purchase the products, underscoring their overall satisfaction and positive user experience.
3.6. Clinical Scoring Results
The values obtained at the end of the study, after repeated applications of the tested products, were compared with the initial values, using the non-parametric Wilcoxon test (i.e., two-tail, significance at p-value < 0.05). As measured by the dermatologist investigator’s subjective scale, the test items significantly decreased the color intensity of the dark spots by week 8 (p < 0.0001; Table 6).

Table 6.
Results of the clinical scoring of facial dark spots by the dermatologist investigator. Raw data may be found in Tables S4 and S5.
Mean intensity scores indicated a 13% lightening of the monitored dark spots (Table 6). Additionally, the test items were found to significantly reduce the spot size by week 8 compared to baseline (p-value = 0.0020). Indeed, the initial mean spot size was 1.02 ± 0.14 cm at baseline and 0.95 ± 0.13 at week 8, reflecting a mean decrease of 6% (Table 6).
4. Discussion
4.1. Combining Functional Ingredients for Topical Management of Hyperpigmentation
TXA has emerged as a prominent topical agent in the realm of cosmeceuticals, particularly for addressing skin hyperpigmentation. TXA primarily functions by inhibiting plasmin production. Originally, this mechanism was therapeutically used to reduce bleeding, as plasmin activates fibrinolysis [8]. In vitro studies have shown that this inhibition reduces keratinocytes’ production of arachidonic acid and prostaglandins, which are mediators that stimulate melanocytes and activate tyrosinases, key enzymes for melanin synthesis [27]. Therefore, by reducing plasmin activity, TXA decreases melanin production. Additionally, in vitro studies have also shown that TXA inhibits vascular endothelial growth factor receptors (VEGFR) on melanocytes, which further decreases tyrosinase activity and melanin synthesis, making it a potent anti-pigmentation ingredient (Figures S2 and S3) [28,29,30,31,32,33]. Beyond its anti-pigmentation properties, TXA accelerates skin barrier recovery, enhancing overall skin appearance and health [9,10,11]. TXA’s stability and efficacy in topical formulations contribute to its widespread use and acceptance in cosmetic skincare regimens aimed at locally managing hyperpigmentation [10].
While TXA directly intervenes in the pigmentation pathway in melanocytes, niacinamide focuses on preventing melanosome transfer and enhancing barrier functions. Thus, niacinamide’s skin-lightening effect is primarily attributed to its ability to inhibit melanosome transfer [16,22,34,35]. Niacinamide reduces the production of pro-inflammatory cytokines and prostaglandins generated by keratinocytes. These inflammatory molecules normally signal melanocytes to increase melanin synthesis and promote the transfer of melanosomes to keratinocytes. By disrupting these signals, niacinamide decreases the transfer of melanin to keratinocytes, thereby reducing the development of pigmentation on the skin’s surface and promoting an even skin tone (Figure S4) [36,37]. Beyond its role in addressing hyperpigmentation, niacinamide addresses several key issues associated with skin aging [22,35,38,39,40]. Niacinamide notably exhibits ROS inhibition properties, protecting skin cells from oxidative stress induced by environmental factors such as UV radiation [22,41]. Its ability to effectively modulate pro-inflammatory cytokines influences the synthesis of metallopeptidases (MMPs), which are stimulated by ROS and inflammatory cytokines and contribute to skin degradation [42,43]. These properties consolidate niacinamide as a multifaceted ingredient, not only addressing hyperpigmentation but also improving overall skin health and mitigating signs of aging [22,44,45,46,47,48,49,50]. Thus, the combined use of niacinamide and TXA introduces complementary mechanisms of action for treating hyperpigmentation, while also enhancing skin barrier functions [32,33,38,51].
Vitamin C, specifically in its L-ascorbic acid form, is a potent antioxidant known for its ability to mitigate oxidative stress and inhibit melanin production by blocking the tyrosinase enzyme [52,53]. However, the poor stability of L-ascorbic acid compromises its penetration into the skin and diminishes its efficacy. In the cosmetic industry, a prevalent trend has been to replace ascorbic acid with more stable derivatives. The serum investigated in this study utilized the precursor ascorbyl glucoside, which is hydrolyzed in situ by the enzyme α-glucosidase present on skin cell membranes (Table 4) [54,55]. This approach not only enhances the stability of the formulation, but also ensures stable delivery of vitamin C’s benefits, maintaining its targeted properties [54,55,56,57]. Moreover, unlike ascorbic acid, which typically requires formulation at a low pH value of around 3.5, ascorbyl glucoside remains stable at a wider range of pH levels [46,55,57]. This characteristic allows the serum used in this study to be formulated at pH 6.65, closer to the physiological pH of the skin, thereby reducing the risk of application-related irritation [58].
Overall, the addition of vitamin C to the treatment protocol via the serum introduced an additional mechanism to combat hyperpigmentation, complementing the effects of TXA and niacinamide. Vitamin C also inhibits the enzyme tyrosinase, which plays a key role in the conversion of tyrosine to melanin [46]. This enzymatic inhibition further reduces melanin production and supports the action of TXA within melanocytes. As a potent antioxidant, vitamin C complements niacinamide’s antioxidant action through its ability to neutralize free radicals and activate intracellular antioxidant systems [59]. Vitamin C also supports niacinamide’s anti-aging effects through collagen synthesis stimulation (i.e., essential for maintaining skin firmness and elasticity), making it a valuable component in cosmeceuticals (Figure S5) [44,45,46,47,48,49]. Globally, utilizing TXA, niacinamide, and vitamin C within the same treatment regimen offers a multilevel approach to skin hyperpigmentation. Together, these mechanisms target different hyperpigmentation pathways, enhancing the likelihood of successful outcomes.
Hyaluronic acid (HA) was added to the investigated cream and serum formulations to provide complementary benefits alongside the three active ingredients. HA not only offers hydrating benefits but also enhances the penetration and stability of the active depigmenting agents, potentially increasing their efficacy [44,60,61]. By attracting and retaining moisture within the skin, HA creates a conducive environment for active ingredients to permeate [62]. Specifically, a combination of three different molecular weight HAs was utilized herein to maximize these benefits (Table 4). High-molecular-weight HA was incorporated into the investigated cream to provide hydration by forming a non-occlusive film on the surface of the epidermis, which reduces transepidermal water loss (Table 3) [60]. The serum was formulated with a blend of high, medium, and low-molecular-weight HAs (Table 4). The incorporation of medium and low-molecular-weight HA facilitates penetration into deeper dermal layers, enhancing skin protection against bacteria, and improves anti-aging properties by promoting skin firmness, as shown in Figure S6 [63]. This multi-layered approach ensures comprehensive skin hydration, protection, and rejuvenation [60]. Additionally, the hydration provided by HA helps to mitigate the risk of irritation and dryness that may result from applying the active ingredients, thereby enhancing skin comfort and patient adherence to the regimen.
Generally, the association of the various active ingredients in the investigated protocols aimed to procure effects similar to or better than those of strong tyrosinase inhibitors. Notwithstanding, it is essential to recognize that hydroquinone is currently regarded as the gold standard for treating hyperpigmentation. However, alternatives, particularly those that function as tyrosinase inhibitors (e.g., kojic acid, arbutin, and others) exist and offer potential benefits, especially in terms of safety and side effect profiles. Future studies should consider these alternatives as comparators in clinical trials. By doing so, researchers can establish a broader range of effective treatments, offering options that cater to different patient needs and preferences [64,65]. To address current limitations comprehensively, future research should prioritize large patient sample sizes, extended study durations, diverse participant demographics, and frequent assessment intervals. These steps would not only validate the current findings but also deepen the understanding of the treatment’s efficacy and safety profiles, potentially positioning alternative tyrosinase inhibitors alongside or even ahead of hydroquinone in clinical practice.
From a formulation viewpoint, the dual product approach comprising a cream and a serum was strategically employed to optimize the treatment of hyperpigmentation through layered efficacy. Namely, both formulations contained TXA and niacinamide, which enhances the effectiveness of these active agents by delivering them across different skin layers. The cream formulation not only contained the active ingredients, but also served as a protective barrier, reinforcing the skin’s surface integrity. On the other hand, serum formulations are designed to deliver active ingredients deeper into the skin, facilitating penetration and localized bioavailability of the active compounds. The serum also allowed for the incorporation of vitamin C into the regimen, adding another potent active ingredient to the treatment protocol. By combining these two formulations, the treatment regimen maximized therapeutic outcomes, addressing hyperpigmentation through both deep and superficial mechanisms. It is highlighted that the novelty of the study consisted in the first reporting of a protocol that combines a serum and a cream to achieve short-term effects on hyperpigmentation (i.e., 8 weeks of care). Thus, the goal and novelty of our study was not to assess the serum or the cream individually, but to demonstrate that the original results can be positioned and compared with those of previously published clinical studies, while achieving results within a study period of only 8 weeks.
Overall, the combination approach with various active ingredients in the investigated cosmetic formulas was mainly based on balancing tolerability and efficacy attributes. Importantly, the integration of these ingredients into cosmetic formulations offers a potential alternative to conventional treatments, decreasing the risk of serious adverse effects. Notably, in the contemporary field of dermatology, the use of cosmeceuticals has become a pivotal strategy in managing hyperpigmentation. Cosmeceuticals draw inspiration from pharmaceutical formulations with scientifically backed active ingredients, while avoiding the potential side effects of traditional prescription ingredients such as hydroquinone [66,67]. These formulations often include ingredients that provide multiple benefits beyond simply fading dark spots, such as improving overall skin texture and delivering antioxidant protection. Unlike prescription-based therapies, dermocosmetics provide accessible and often less irritating solutions, characterized by formulations optimized for patient comfort. Moreover, these formulations can complement prescribed therapies (e.g., for melasma) or act preventively against recurrences when used as a maintenance therapy between treatments. Specifically, long-term patient adherence to treatment regimens is critical for managing conditions like skin hyperpigmentation, which require consistent and prolonged interventions [67]. Of note, studies have shown the efficiency of synergistic applications of cosmetics alongside standard therapeutic regimens to increase treatment efficacy and foster patient adherence, while maintaining high safety profiles [68,69]. By combining pharmaceutical principles with consumer preferences, cosmeceuticals meet rigorous efficacy standards in dermatology while providing accessible and user-friendly solutions. This approach has represented a significant advancement in skincare, offering patients scientifically validated options to achieve and maintain healthy skin.
4.2. Assessing Tolerability and Efficacy of TXA-Based Facial Cream and Serum
The presented in-use test under dermatological control results confirmed the significant benefits of combining TXA, niacinamide, vitamin C, and HA (Figure 1). The clinical scoring of the color intensity of the facial dark spots showed a statistically significant improvement after 8 weeks of using the test items (Table 6). This indicated that the combined use of the cream and serum effectively lightened the pigmentation of the monitored spots. The clinical data revealed that 19 out of 22 participants exhibited a positive variation in the color intensity of their spots, with most participants experiencing a 1-point improvement on the scoring scale. Percentage variations ranged from 0% to 25%, corroborating the efficacy of the test items in a real-world setting. Subjects who did not show any improvement (i.e., n = 3) had an initial high score of 7, suggesting a potential ceiling effect where the maximum improvement potential was already achieved. Conversely, subjects with lower initial scores (i.e., 4 or 5) demonstrated higher percentage improvements, indicating that the considered formulations might be more effective in the earlier stages of hyperpigmentation. These results may be attributed to the reduced amount of melanin accumulated in skin cells in the earlier stages of hyperpigmentation. Therein, the actions of the active ingredients are most important on melanin production and deposition, allowing the effects to manifest more rapidly and visibly. This element aligns with the notion that early intervention is key to prevent the progression of hyperpigmentation more efficiently, leading to more noticeable improvements. Therefore, new prospective studies aimed at understanding the physiological differences across various stages of skin hyperpigmentation would be valuable for developing more effective treatment strategies.
In addition to the clinical evaluations, the study employed colorimetric assessments as an objective measurement to assess test item efficacy. Colorimetric assessments not only validated the available subjective observations but also contributed to a deeper understanding of how the products influenced melanin levels by providing quantitative data. As mentioned in Section 3.4, the decrease in skin pigmentation was primarily observed through an 8% increase in the ITA° parameter. Alaluf et al. (2002) established that the L* parameter correlates with the melanin content in the epidermis in an exponential manner [19]. Applying this correlation to the L* values determined in this study, a 1% increase in L* corresponds to a 3% decrease in melanin in the epidermis (i.e., D0 = 17.36 µg/mg epidermis; D56 = 16.88 µg/mg epidermis). These results support the conclusion that the investigated active ingredients effectively downregulated melanin synthesis and distribution. As melanin production diminishes, the intensity of dark spots has correspondingly lightened, as evidenced by the changes observed in the ITA° parameter (Table 5). Furthermore, for lightly pigmented skin types (e.g., European, Chinese, Mexican), there is a positive linear correlation between b* and the melanin content in the skin, meaning that an increase in b* correlates with increased melanin amounts (i.e., higher yellow light component) [19]. Since L* indicates a decrease in melanin, it was expected that b* would decrease. However, the results did not show a significant change in the b* value (Table 5). This observation could indicate a saturation point for yellow pigmentation in the studied population. The minimal change in the b* value may also suggest that the formulations specifically targeted the pathways leading to darker pigmentation, rather than affecting the overall skin tone. In fact, it has been demonstrated that for L* values between 45 and 60, the corresponding b* value reaches a stationary phase, where b* changes very little as L* continues to decrease [19]. Thus, the results obtained herein aligned with the literature and supported the lightening action of the investigated cream and serum combination.
Further analysis of the clinical data revealed that the mean reduction in the size of the monitored dark spots was 6%, with the mean initial size being 1.02 cm and reducing to 0.95 cm by the end of the study (Table 6). Although the reduction in size was relatively modest, it was consistent across participants, suggesting a gradual improvement in the overall appearance of the monitored hyperpigmented spots. The observed decrease in the intensity of the hyperpigmented spots, as opposed to a more significant reduction in size, could be attributed to several factors relative to the mechanisms of melanin production and distribution within the skin. Specifically, TXA, niacinamide, and vitamin C primarily inhibit the enzymatic activity involved in melanin synthesis, specifically targeting tyrosinases and other key regulators of melanogenesis. This results in a reduction in melanin production in melanocytes, which directly contributed to a lighter appearance of existing pigmentation. The efficacy of this inhibition can manifest quickly in terms of color change, making the decrease in intensity more pronounced. On the other hand, the size of hyperpigmented spots is also influenced by the spatial distribution of melanin within the epidermis. The reduction in spot size may require processes such as keratinocyte migration and skin turnover, resulting in slower manifestation of visible improvements [70,71]. These results corroborated findings reported in the literature, such as the study conducted by Makino et al. (2023), which demonstrated that after 12 weeks of treatment in patients with PIH and solar lentigines, the reduction in dark spot size was less pronounced compared to improvements in dark spot intensity and contrast in all subgroups [21]. To further understand the relationship between spot size and intensity, future studies could analyze these parameters together to determine if there is a correlation between the decrease in spot size and the lightening of pigmentation. This could potentially provide deeper insights into the mechanisms of action of the active ingredients and help optimize formulations for better clinical outcomes.
As previously synthesized, TXA, niacinamide, and vitamin C work additively or synergistically to decrease melanin synthesis by melanocytes and melanin transfer to keratinocytes. Of note, the observed outcomes may potentially be attributed to niacinamide or TXA alone, or to a combination of these ingredients, which have been reported for TXA and niacinamide [51]. It is important to note that melanocytes are primarily located in the basal cell layer of the epidermis, the deepest layer (Figure S2) [72]. Melanin is then transferred to keratinocytes, which ascend through the epidermis to the cornified layer, a process that takes about 30 to 56 days [73]. This suggests that 8 weeks may not be sufficient to observe the full potential of the serum and cream’s action. Specifically, Feng et al. (2021) reviewed clinical studies on TXA applied for hyperpigmentation, concluding that topical formulation studies typically span 12 weeks to maximize results [72]. Notwithstanding, the effectiveness of the cream and serum combination determined herein over 8 weeks underscored the protocol’s efficacy and highlighted the significant benefits of combining active ingredients with complementary actions against hyperpigmentation.
Importantly, the efficacy results observed in this study aligned with previous findings from other clinical trials evaluating the impacts of cosmetic formulations containing similar active ingredients on skin pigmentation. For instance, Kim et al. (2017) reviewed available reports and highlighted that topical applications of TXA significantly reduced the melanin index in subjects with hyperpigmentation [31]. The Journal of Drugs in Dermatology has reported in a systematic review of randomized clinical trials that TXA demonstrates similar efficacy to hydroquinone in the treatment of melasma, but with fewer side effects [74]. For instance, a clinical trial comparing the topical application of 3% TXA with a combined treatment of 3% hydroquinone and 0.01% dexamethasone for melasma demonstrated that there was no significant difference in outcomes between the two interventions [11]. These previous findings support the use of topical TXA as an effective option for treating hyperpigmentation with fewer side effects compared to prescription medications.
Of note, the cream and serum investigated in this study are classified as cosmetics. They comply with European cosmetic ingredient regulations, therefore representing safe and efficient alternatives to prescription products in clinical applications [11,74]. Furthermore, a topical facial serum containing 3% TXA, 1% kojic acid, and 5% niacinamide was reported to be effective and well-tolerated for addressing hyperpigmentary skin conditions, including melasma [75]. Additional in vitro data suggested that TXA may act by mediating the inhibition of PGE2-stimulated human epidermal melanocytes. Importantly, the absence of serious side effects (e.g., irritations) indicated that the concentrations of active ingredients used in the investigated formulations were effective yet gentle. This balance allows for visible results without compromising safety or comfort. The incorporation of three distinct active ingredients enabled the formulations to achieve significant outcomes without the need for high concentrations of each individual component (Table 3 and Table 4). This is particularly beneficial compared to traditional treatments, which often carry a higher risk of irritation. This ultimately enhances patient adherence and overall satisfaction with the treatment regimen.
Finally, as concerns the standardized subjective feedback from the study participants, the gathered data also supported the objective clinical findings. Most participants reported improvements in the tone and appearance of their dark spots, as well as overall skin luminosity and radiance (Table S3). This subjective assessment was found to align with the objective measurements of the study and underscored the products’ acceptability and perceived efficacy. Positive feedback regarding skin tone but also aspects such as luminosity, texture, and elasticity indicated that participants experienced enhanced overall skin quality. These observations confirmed that the benefits of TXA, niacinamide, and vitamin C extend beyond reducing hyperpigmentation. As discussed in Section 4.1, these active ingredients are known to enhance skin health by supporting barrier functions, providing antioxidant-based protection, and promoting collagen synthesis. Additionally, the incorporation of HA contributed to improve hydration and skin elasticity, further improving overall skin appearance. The subjective assessments not only corroborated the clinical efficacy demonstrated through objective measurements but also highlighted the formulation’s comprehensive approach to addressing facial hyperpigmentation while improving overall skin health.
4.3. Study Limitations and Perspectives
Despite the promising safety and efficacy results set forth herein, several limitations were identified for the presented study. Namely, the sample size was relatively small, which may affect the generalizability of the findings. Consequently, future studies should include larger, more diverse populations or alternative skin types (e.g., Asian skin) to provide a more comprehensive assessment of the treatment’s effectiveness across varied demographics. Furthermore, the study duration was limited to 8 weeks. While this timeframe was appropriate to clinically observe initial improvements in facial hyperpigmentation, longer-term benefits or potential side effects of the test items require further clinical investigation.
Additionally, this study employed only baseline and endpoint measurements to evaluate intervention efficacy. While significant depigmentation was observed, incorporating intermediate assessments throughout the study period would provide additional insights into the gradual effects of the products on hyperpigmented spots, enhancing the understanding of its mechanisms and function over time. To further refine these assessments, the use of objective tools such as a Mexameter could be integrated into future studies to quantitatively measure changes in skin pigmentation with greater precision. Moreover, conducting a controlled double-blind trial would eliminate potential biases, thereby increasing the reliability of the results. Furthermore, future studies should prioritize larger sample sizes, longer study durations, diverse participant demographics, investigation of ingredient functional synergies, and more frequent assessment intervals. Such proceedings would not only validate the current findings but also enhance the deep understanding of the treatment’s efficacy and safety profiles.
From a methodological viewpoint, no authoritative reference documents were specifically available for dark spot evaluation, hence the selection of previously published protocols. While guidelines such as the “Guidelines for the Evaluation of the Efficacy of Cosmetic Products” from Cosmetics Europe or ISO standards (i.e., only applicable to sunscreen products) exist, specific efficacy evaluation methodologies were adapted herein. For further investigation of the effects of the products on facial dark spots, additional analytical tools (e.g., dermoscopy, Mexameter, DermaSpectrometer, VISIA, Antera 3D) may be used to provide complementary quantitative datasets in future studies.
Finally, the absence of a control group using a well-established depigmenting agent, such as hydroquinone or other tyrosinase inhibitors, limited the comparative evaluation of the tested products. Including such a control group in future studies would provide a benchmark against which to gauge the relative efficacy of the investigational formulas. Furthermore, future studies may benefit from methodological design adaptations aiming to elucidate which component and/or which formula (i.e., of the cream or serum) procures the best effects or a synergistic effect. In this respect, an alternative approach would be to utilize the serum as a concentrated formulation, in conjunction with a simple occlusive treatment. Such enhanced methodological elements will be implemented following this pilot study.
5. Conclusions
The present in-use test under dermatological control demonstrated that cream and serum formulations containing 3% TXA, 5% niacinamide, and 2% vitamin C, combined with HAs of different molecular weights, are effective in managing facial hyperpigmentation over an 8-week period. Clinical and colorimetric evaluations showed significant reductions in both the intensity and size of hyperpigmented facial spots, leading to locally improved skin tone and appearance. The investigated cosmetic formulations were well-tolerated, with no serious adverse skin reactions reported, resulting in high reported user satisfaction. Overall, the presented findings support the use of TXA, niacinamide, and vitamin C as a safe and functional combination for managing facial hyperpigmentation, offering multiple skin health benefits and a better safety profile compared to traditional topical care. This study confirmed the potential of these active ingredients in cosmeceutical products for safe and effective management of facial hyperpigmentation and improving overall skin appearance attributes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cosmetics11050168/s1, Figure S1: Modalities of application of the investigated cosmetic formulations; Figure S2: Illustration of the effects of external aggressions in skin coloration; Figure S3: Mechanistic description of tranexamic acid’s lightening action; Figure S4: Mechanistic description of niacinamide’s lightening action; Figure S5: Mechanistic description of L-ascorbic acid’s functional attributes; Figure S6: Description of the various HA molecular weight classes present in the investigated cosmetic formulations; Table S1: Summary of patient related characteristics; Table S2: Raw data for the colorimetric measurement of the spots; Table S3: Results of participant-reported assessments for the investigated formulations; Table S4: Raw data for the clinical scoring of the size of the spots; Table S5: Raw data for the clinical scoring of the color intensity of the spots.
Author Contributions
Conceptualization, S.H., K.L., A.P., C.M., C.R., L.A.A. and A.L.; methodology, S.H., K.L., A.P., C.M., L.A.A. and A.L.; software, S.H., K.L., A.P. and A.L.; validation, S.H., K.L., A.P., C.M., C.R., W.R., C.S., P.A.-S., B.H., L.A.A. and A.L.; formal analysis, S.H., K.L., A.P., C.M., C.R., B.H., L.A.A. and A.L.; investigation, S.H., K.L., A.P., C.M. and A.L.; resources, A.P., L.A.A. and A.L.; data curation, S.H., K.L., A.P., C.M., C.R., L.A.A. and A.L.; writing—original draft preparation, S.H., K.L., A.P. and A.L.; writing—review and editing, S.H., K.L., A.P., C.M., C.R., W.R., C.S., P.A.-S., B.H., L.A.A. and A.L.; visualization, S.H., K.L., A.P. and A.L.; supervision A.P., L.A.A. and A.L.; project administration, A.P. and A.L.; funding acquisition, A.P. and A.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki [76]. The clinical section of this study was conducted following the principles of Good Clinical Practices (GCP), published by the ICH (International Recommendations ICH Topic E6, CPMP/ICH/135/95 of 1 May 1996, European Parliament and Council Guideline 2001/20/CE DOCE of 1 May 2001).
Informed Consent Statement
Informed consent was obtained from all participants of the study for use of the gathered and anonymized data.
Data Availability Statement
The data presented in this study are freely available within the article files.
Acknowledgments
We would like to thank the participants to the clinical portion of the presented study.
Conflicts of Interest
Authors S.H., K.L., A.P., C.M. and C.R. were employed by LOUNA REGENERATIVE SA (Geneva, Switzerland) during this study. Author A.L. was employed by LAM Biotechnologies SA (Epalinges, Switzerland) and by TEC-PHARMA SA (Bercher, Switzerland) during this study. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The funders had no role in the design of the study; in the collection, analyses or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
List of Abbreviations
| AGE | advanced glycation end-products |
| CHUV | Lausanne University Hospital |
| CRO | contract research organization |
| DNA | deoxyribonucleic acid |
| ECHA | European Chemicals Agency |
| FDA | US Food and Drug Administration |
| HA | hyaluronic acid |
| kDA | kiloDalton |
| MDa | megaDalton |
| MMP | matrix metalloproteinase |
| mRNA | messenger ribonucleic acid |
| NAD | nicotinamide adenine dinucleotide |
| NADP | nicotinamide adenine dinucleotide phosphate |
| NIA | niacinamide |
| Ph. Eur. | European Pharmacopoeia |
| PIH | post-inflammatory hyperpigmentation |
| ROS | reactive oxygen species |
| TXA | tranexamic acid |
| USA | United States of America |
| UV | ultraviolet |
| VEGFR | vascular endothelial growth factor receptor |
References
- Thawabteh, A.M.; Jibreen, A.; Karaman, D.; Thawabteh, A.; Karaman, R. Skin pigmentation types, causes and treatment-A review. Molecules 2023, 28, 4839. [Google Scholar] [CrossRef] [PubMed]
- Plensdorf, S.; Livieratos, M.; Dada, N. Pigmentation disorders: Diagnosis and management. Am. Fam. Physician 2017, 96, 797–804. [Google Scholar] [PubMed]
- Dalgard, F.J.; Gieler, U.; Tomas-Aragones, L.; Lien, L.; Poot, F.; Jemec, G.B.E.; Misery, L.; Szabo, C.; Linder, D.; Sampogna, F.; et al. The psychological burden of skin diseases: A cross-sectional multicenter study among dermatological out-patients in 13 European countries. J. Investig. Dermatol. 2015, 135, 984–991. [Google Scholar] [CrossRef]
- Dabas, G.; Vinay, K.; Parsad, D.; Kumar, A.; Kumaran, M.S. Psychological disturbances in patients with pigmentary disorders: A cross-sectional study. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 392–399. [Google Scholar] [CrossRef]
- Moolla, S.; Miller-Monthrope, Y. Dermatology: How to manage facial hyperpigmentation in skin of colour. Drugs Context 2022, 11, 2021-11-2. [Google Scholar] [CrossRef]
- Sarkar, R.; Arora, P.; Garg, K.V. Cosmeceuticals for hyperpigmentation: What is available? J. Cutan. Aesthet. Surg. 2013, 6, 4–11. [Google Scholar] [CrossRef]
- Clark, A.; Sivamani, R. Phytochemicals in the treatment of hyperpigmentation. Bot. Targets Ther. 2016, 6, 89–96. [Google Scholar] [CrossRef]
- González-Molina, V.; Martí-Pineda, A.; González, N. Topical treatments for melasma and their mechanism of action. J. Clin. Aesthet. Dermatol. 2022, 15, 19–28. [Google Scholar] [PubMed]
- Gaćina, K.; Krstanović Ćosić, A. The use of tranexamic acid in dermatology. Acta Clin. Croat. 2023, 62, 368–372. [Google Scholar] [CrossRef]
- Kim, S.J.; Park, J.Y.; Shibata, T.; Fujiwara, R.; Kang, H.Y. Efficacy and possible mechanisms of topical tranexamic acid in melasma. Clin. Exp. Dermatol. 2016, 41, 480–485. [Google Scholar] [CrossRef]
- Ebrahimi, B.; Naeini, F.F. Topical tranexamic acid as a promising treatment for melasma. J. Res. Med. Sci. 2014, 19, 753–757. [Google Scholar] [PubMed]
- Atefi, N.; Dalvand, B.; Ghassemi, M.; Mehran, G.; Heydarian, A. Therapeutic effects of topical tranexamic acid in comparison with hydroquinone in treatment of women with melasma. Dermatol. Ther. 2017, 7, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.M.; Lim, H.W. The uses of tranexamic acid in dermatology: A review. Int. J. Dermatol. 2023, 62, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Otte, N.; Borelli, C.; Korting, H.C. Nicotinamide-Biologic actions of an emerging cosmetic ingredient. Int. J. Cos. Sci. 2005, 27, 255–261. [Google Scholar] [CrossRef]
- Bissett, D.L.; Miyamoto, K.; Sun, P.; Li, J.; Berge, C.A. Topical niacinamide reduces yellowing, wrinkling, red blotchiness, and hyperpigmented spots in aging facial skin. Int. J. Cos. Sci. 2004, 26, 231–238. [Google Scholar] [CrossRef]
- Hakozaki, T.; Minwalla, L.; Zhuang, J.; Chhoa, M.; Matsubara, A.; Miyamoto, K.; Greatens, A.; Hillebrand, G.G.; Bissett, D.L.; Boissy, R.E. The effect of niacinamide on reducing cutaneous pigmentation and suppression of melanosome transfer. Br. J. Dermatol. 2002, 147, 20–31. [Google Scholar] [CrossRef]
- Couteau, C.; Alvarez Rueda, N.; Breton, B.; Coiffard, L. A review of homemade cosmetics based on a study of 150 blogs and their authors. Int. J. Cos. Sci. 2023, 45, 539–547. [Google Scholar] [CrossRef]
- Wu, Y.; Tanaka, T.; Akimoto, M. Utilization of individual typology angle (ITA) and hue angle in the measurement of skin color on images. Bioimages 2020, 28, 1–8. [Google Scholar]
- Alaluf, S.; Atkins, D.; Barrett, K.; Blount, M.; Carter, N.; Heath, A. The impact of epidermal melanin on objective measurements of human skin colour. Pigment Cell Res. 2002, 15, 119–126. [Google Scholar] [CrossRef]
- Jdid, R.; Pedrazzani, M.; Lejeune, F.; Fischman, S.; Cazorla, G.; Forestier, S.; Khalifa, Y.B. Skin dark spot mapping and evaluation of brightening product efficacy using Line-field Confocal Optical Coherence Tomography (LC-OCT). Ski. Res. Technol. 2024, 30, e13623. [Google Scholar] [CrossRef]
- Makino, E.T.; Huang, P.; Cheng, T.; Acevedo, S.F.; de Oliveira, C.; Mehta, R.C. 12-Week, single-center study of a targeted pigment-correcting dark spot treatment for post-inflammatory hyperpigmentation and solar lentigines. Clin. Cosmet. Investig. Dermatol. 2023, 16, 2677–2686. [Google Scholar] [CrossRef] [PubMed]
- Marques, C.; Hadjab, F.; Porcello, A.; Lourenço, K.; Scaletta, C.; Abdel-Sayed, P.; Hirt-Burri, N.; Applegate, L.A.; Laurent, A. Mechanistic insights into the multiple functions of niacinamide: Therapeutic implications and cosmeceutical applications in functional skincare products. Antioxidants 2024, 13, 425. [Google Scholar] [CrossRef] [PubMed]
- Pandey, A.; Jatana, G.K.; Sonthalia, S. Cosmeceuticals. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar] [PubMed]
- Ali, A.; Skedung, L.; Burleigh, S.; Lavant, E.; Ringstad, L.; Anderson, C.D.; Wahlgren, M.; Engblom, J. Relationship between sensorial and physical characteristics of topical creams: A comparative study on effects of excipients. Int. J. Pharm. 2022, 613, 121370. [Google Scholar] [CrossRef]
- Nebogina, N.A.; Prozorova, I.V.; Yudina, N.V. The influence of the temperature of formation of water-oil emulsions on their dispersion. AIP Conf. Proc. 2020, 2310, 020221. [Google Scholar] [CrossRef]
- Kim, K.M.; Oh, H.M.; Lee, J.H. Controlling the emulsion stability of cosmetics through shear mixing process. Korea-Aust. Rheol. J. 2020, 32, 243–249. [Google Scholar] [CrossRef]
- Maeda, K.; Tomita, Y. Mechanism of the inhibitory effect of tranexamic acid on melanogenesis in cultured human melanocytes in the presence of keratinocyte-conditioned medium. J. Health Sci. 2007, 53, 389–396. [Google Scholar] [CrossRef]
- Zhu, J.W.; Ni, Y.J.; Tong, X.Y.; Guo, X.; Wu, X.P. Activation of VEGF receptors in response to UVB promotes cell proliferation and melanogenesis of normal human melanocytes. Exp. Cell Res. 2020, 387, 111798. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.W.; Ni, Y.J.; Tong, X.Y.; Guo, X.; Wu, X.P.; Lu, Z.F. Tranexamic acid inhibits angiogenesis and melanogenesis in vitro by targeting VEGF receptors. Int. J. Med. Sci. 2020, 17, 903–911. [Google Scholar] [CrossRef]
- Kim, H.J.; Moon, S.H.; Cho, S.H.; Lee, J.D.; Kim, H.S. Efficacy and safety of tranexamic acid in melasma: A meta-analysis and systematic review. Acta Derm. Venereol. 2017, 97, 776–781. [Google Scholar] [CrossRef]
- Walocko, F.M.; Eber, A.E.; Keri, J.E.; Al-Harbi, M.A.; Nouri, K. The role of nicotinamide in acne treatment. Dermatol. Ther. 2017, 30, e12481. [Google Scholar] [CrossRef]
- Cho, Y.H.; Park, J.E.; Lim, D.S.; Lee, J.S. Tranexamic acid inhibits melanogenesis by activating the autophagy system in cultured melanoma cells. J. Dermatol. Sci. 2017, 88, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Bang, S.H.; Kim, J.H.; Shin, H.J.; Choi, J.H.; Chang, S.E. Tranexamic acid diminishes laser-induced melanogenesis. Ann. Dermatol. 2015, 27, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Kimball, A.B.; Kaczvinsky, J.R.; Li, J.; Robinson, L.R.; Matts, P.J.; Berge, C.A.; Miyamoto, K.; Bissett, D.L. Reduction in the appearance of facial hyperpigmentation after use of moisturizers with a combination of topical niacinamide and N-acetyl glucosamine: Results of a randomized, double-blind, vehicle-controlled trial. Br. J. Dermatol. 2010, 162, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Boo, Y.C. Mechanistic basis and clinical evidence for the applications of nicotinamide (niacinamide) to control skin aging and pigmentation. Antioxidants 2021, 10, 1315. [Google Scholar] [CrossRef]
- Yanez, M.; Jhanji, M.; Murphy, K.; Gower, R.M.; Sajish, M.; Jabbarzadeh, E. Nicotinamide augments the anti-inflammatory properties of resveratrol through PARP1 activation. Sci. Rep. 2019, 9, 10219. [Google Scholar] [CrossRef]
- Biedroń, R.; Ciszek, M.; Tokarczyk, M.; Bobek, M.; Kurnyta, M.; Słominska, E.M.; Smoleński, R.T.; Marcinkiewicz, J. 1-Methylnicotinamide and nicotinamide: Two related anti-inflammatory agents that differentially affect the functions of activated macrophages. Arch. Immunol. Ther. Exp. 2008, 56, 127–134. [Google Scholar] [CrossRef]
- Ong, R.R.; Goh, C.F. Niacinamide: A review on dermal delivery strategies and clinical evidence. Drug Del. Transl. Res. 2024, 1–37. [Google Scholar] [CrossRef]
- Minoretti, P.; Emanuele, E. Clinically actionable topical strategies for addressing the hallmarks of skin aging: A primer for aesthetic medicine practitioners. Cureus 2024, 16, e52548. [Google Scholar] [CrossRef]
- Huber, R.; Wong, A. Nicotinamide: An update and review of safety & differences from niacin. Ski. Ther. Let. 2020, 25, 7–11. [Google Scholar]
- Schalka, S. New data on hyperpigmentation disorders. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 18–21. [Google Scholar] [CrossRef]
- Qian, H.; Shan, Y.; Gong, R.; Lin, D.; Zhang, M.; Wang, C.; Wang, L. Mechanism of action and therapeutic effects of oxidative stress and stem cell-based materials in skin aging: Current evidence and future perspectives. Front. Bioeng. Biotechnol. 2023, 10, 1082403. [Google Scholar] [CrossRef] [PubMed]
- Porcello, A.; Chemali, M.; Marques, C.; Scaletta, C.; Lourenço, K.; Abdel-Sayed, P.; Raffoul, W.; Hirt-Burri, N.; Applegate, L.A.; Laurent, A. Dual functionalization of hyaluronan dermal fillers with vitamin B3: Efficient combination of bio-stimulation properties with hydrogel system resilience enhancement. Gels 2024, 10, 361. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, Y.; Kim, J.; Lee, S.; Park, J. The synergistic effect of hyaluronic acid and vitamin C in hydrating and brightening the skin. Int. J. Cosmet. Sci. 2018, 40, 325–331. [Google Scholar]
- Boo, Y.C. Ascorbic acid (vitamin C) as a cosmeceutical to increase dermal collagen for skin antiaging purposes: Emerging combination therapies. Antioxidants 2022, 11, 1663. [Google Scholar] [CrossRef] [PubMed]
- Al-Niaimi, F.; Chiang, N.Y.Z. Topical vitamin C and the skin: Mechanisms of action and clinical applications. J. Clin. Aesthet. Dermatol. 2017, 10, 14–17. [Google Scholar]
- Maione-Silva, L.; de Castro, E.G.; Nascimento, T.L.; Cintra, E.R.; Moreira, L.C.; Cintra, B.A.S.; Valadares, M.C.; Lima, E.M. Ascorbic acid encapsulated into negatively charged liposomes exhibits increased skin permeation, retention and enhances collagen synthesis by fibroblasts. Sci. Rep. 2019, 9, 522. [Google Scholar] [CrossRef]
- Pullar, J.M.; Carr, A.C.; Vissers, M.C.M. The roles of vitamin C in skin health. Nutrients 2017, 9, 866. [Google Scholar] [CrossRef]
- Machado, B.H.B.; Frame, J.; Zhang, J.; Najlah, M. Comparative study on the outcome of periorbital wrinkles treated with laser-assisted delivery of vitamin C or vitamin C plus growth factors: A randomized, double-blind, clinical trial. Aesthet. Plast. Surg. 2021, 45, 1020–1032. [Google Scholar] [CrossRef]
- Mainville, L.; Smilga, A.S.; Fortin, P.R. Effect of nicotinamide in skin cancer and actinic keratoses chemoprophylaxis, and adverse effects related to nicotinamide: A systematic review and meta-analysis. J. Cutan. Med. Surg. 2022, 26, 297–308. [Google Scholar] [CrossRef]
- Lee, D.H.; Oh, I.Y.; Koo, K.T.; Suk, J.M.; Jung, S.W.; Park, J.O.; Kim, B.J.; Choi, Y.M. Reduction in facial hyperpigmentation after treatment with a combination of topical niacinamide and tranexamic acid: A randomized, double-blind, vehicle-controlled trial. Ski. Res. Technol. 2014, 20, 208–212. [Google Scholar] [CrossRef]
- Telang, P.S. Vitamin C in dermatology. Indian Dermatol. Online J. 2013, 4, 143–146. [Google Scholar] [CrossRef] [PubMed]
- Farris, P.K. Topical vitamin C: A useful agent for treating photoaging and other dermatologic conditions. Dermatol. Surg. 2005, 31, 814–818. [Google Scholar] [CrossRef]
- Jacques, C.; Genies, C.; Bacqueville, D.; Tourette, A.; Borotra, N.; Chaves, F.; Sanches, F.; Gaudry, A.L.; Bessou-Touya, S.; Duplan, H. Ascorbic acid 2-glucoside: An ascorbic acid pro-drug with longer-term antioxidant efficacy in skin. Int. J. Cosmet. Sci. 2021, 43, 691–702. [Google Scholar] [CrossRef]
- Stamford, N.P. Stability, transdermal penetration, and cutaneous effects of ascorbic acid and its derivatives. J. Cosmet. Dermatol. 2012, 11, 310–317. [Google Scholar] [CrossRef]
- Starr, N.J.; Abdul Hamid, K.; Wibawa, J.; Marlow, I.; Bell, M.; Pérez-García, L.; Barrett, D.A.; Scurr, D.J. Enhanced vitamin C skin permeation from supramolecular hydrogels, illustrated using in situ ToF-SIMS 3D chemical profiling. Int. J. Pharm. 2019, 563, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.Y.; Lee, P.C.; Huang, L.K.; Lu, L.P.; Liao, W.C. Stability studies of ascorbic acid 2-glucoside in cosmetic lotion using surface response methodology. Bioorgan. Med. Chem. Let. 2013, 23, 1583–1587. [Google Scholar] [CrossRef] [PubMed]
- Proksch, E. pH in nature, humans and skin. J. Dermatol. 2018, 45, 1044–1052. [Google Scholar] [CrossRef] [PubMed]
- Gęgotek, A.; Skrzydlewska, E. Antioxidative and anti-inflammatory activity of ascorbic acid. Antioxidants 2022, 11, 1993. [Google Scholar] [CrossRef]
- Bravo, B.; Correia, P.; Gonçalves Junior, J.E.; Sant’Anna, B.; Kerob, D. Benefits of topical hyaluronic acid for skin quality and signs of skin aging: From literature review to clinical evidence. Dermatol. Ther. 2022, 35, e15903. [Google Scholar] [CrossRef]
- Kim, J.H.; Park, E.S.; Nam, S.M.; Choi, C.Y. Comparison of effectiveness and safety of a botulinum toxin monotherapy and a combination therapy with hyaluronic acid filler for improving glabellar frown. Aesthet. Plast. Surg. 2022, 46, 1872–1880. [Google Scholar] [CrossRef]
- Juncan, A.M.; Moisă, D.G.; Santini, A.; Morgovan, C.; Rus, L.L.; Vonica-Țincu, A.L.; Loghin, F. Advantages of hyaluronic acid and its combination with other bioactive ingredients in cosmeceuticals. Molecules 2021, 26, 4429. [Google Scholar] [CrossRef] [PubMed]
- Essendoubi, M.; Gobinet, C.; Reynaud, R.; Angiboust, J.F.; Manfait, M.; Piot, O.J.S.R. Human skin penetration of hyaluronic acid of different molecular weights as probed by Raman spectroscopy. Ski. Res. Technol. 2016, 22, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Zolghadri, S.; Beygi, M.; Mohammad, T.F.; Alijanianzadeh, M.; Pillaiyar, T.; Garcia-Molina, P.; Garcia-Canovas, F.; Munoz-Munoz, J.; Saboury, A.A. Targeting tyrosinase in hyperpigmentation: Current status, limitations and future promises. Biochem. Pharmacol. 2023, 212, 115574. [Google Scholar] [CrossRef] [PubMed]
- Zolghadri, S.; Bahrami, A.; Hassan Khan, M.T.; Munoz-Munoz, J.; Garcia-Molina, F.; Garcia-Canovas, F.; Saboury, A.A. A comprehensive review on tyrosinase inhibitors. J. Enz. Inhib. Med. Chem. 2019, 34, 279–309. [Google Scholar] [CrossRef] [PubMed]
- Ko, D.; Wang, R.F.; Ozog, D.; Lim, H.W.; Mohammad, T.F. Disorders of hyperpigmentation. Part II. Review of management and treatment options for hyperpigmentation. J. Am. Acad. Dermatol. 2023, 88, 291–320. [Google Scholar] [CrossRef]
- Nautiyal, A.; Wairkar, S. Management of hyperpigmentation: Current treatments and emerging therapies. Pigment Cell Melan. Res. 2021, 34, 1000–1014. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, J.; Jiang, L.; Mu, Y. The application of skin care product in melasma treatment. Clin. Cosmet. Investig. Dermatol. 2021, 14, 1165–1171. [Google Scholar] [CrossRef]
- Steiner, M.; Peppelman, M.; Houben, E.; van Erp, P.; van de Kerkhof, P.; Luttge, R. The effectiveness of tranexamic acid in combination with laser treatments for melasma. Lasers Med. Sci. 2019, 34, 1237–1243. [Google Scholar]
- Maeda, K. New method of measurement of epidermal turnover in humans. Cosmetics 2017, 4, 47. [Google Scholar] [CrossRef]
- Collier, A.E.; Wek, R.C.; Spandau, D.F. Human keratinocyte differentiation requires translational control by the eIF2α kinase GCN2. J. Invest. Dermatol. 2017, 137, 1924–1934. [Google Scholar] [CrossRef]
- Feng, X.; Su, H.; Xie, J. Efficacy and safety of tranexamic acid in the treatment of adult melasma: An updated meta-analysis of randomized controlled trials. J. Clin. Pharm. Therap. 2021, 46, 1263–1273. [Google Scholar] [CrossRef] [PubMed]
- Koch, L.; Michael, S.; Reimers, K.; Strauß, S.; Vogt, P.M.; Chichkov, B. Bioprinting for skin. In 3D Bioprinting and Nanotechnology in Tissue Engineering and Regenerative Medicine; Academic Press: Cambridge, MA, USA, 2022; pp. 397–425. [Google Scholar]
- Austin, E.; Nguyen, J.K.; Jagdeo, J. Topical treatments for melasma: A systematic review of randomized controlled trials. J. Drugs Dermatol. 2019, 18, S1545961619P1156X. [Google Scholar] [PubMed]
- Desai, S.; Ayres, E.; Bak, H.; Manco, M.; Lynch, S.; Raab, S.; Du, A.; Green, D.; Skobowiat, C.; Wangari-Talbot, J.; et al. Effect of a tranexamic acid, kojic acid, and niacinamide containing serum on facial dyschromia: A clinical evaluation. J. Drugs Dermatol. 2019, 18, 454–459. [Google Scholar]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).