Development Status and Multilevel Classification Strategy of Medical Robots
Abstract
:1. Introduction
1.1. Exploration in Medical Institutions
1.2. Progress in Home Care
1.3. Novel Materials and Appearances
1.4. Difficulties in Diversified Development of Medical Robots
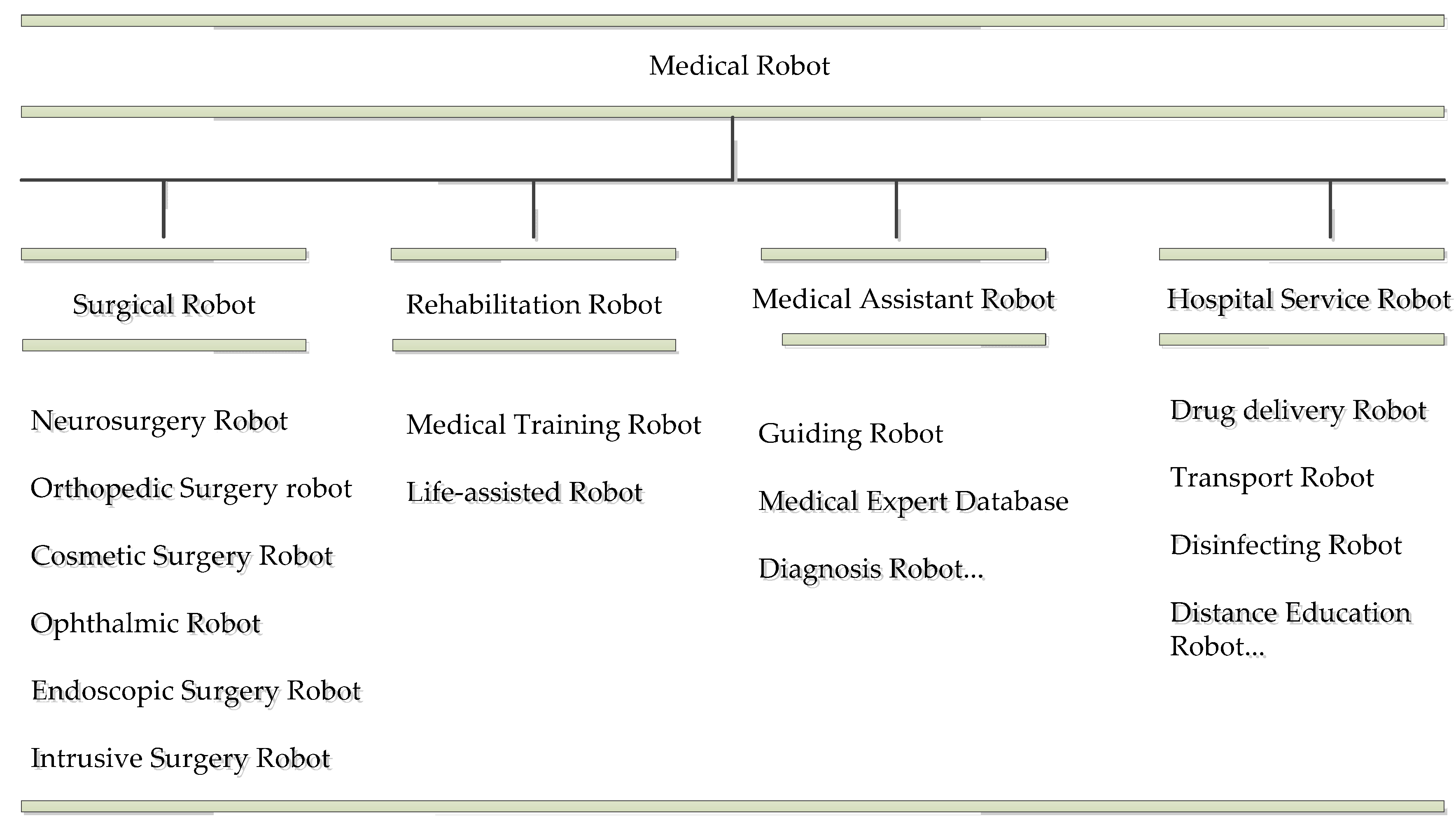
2. Classification Strategies and Characteristics Analysis of Each Medical Robots
2.1. The Status of Classification
2.2. Establishing the Principle of Classification
2.2.1. Principle of Easy Identification
2.2.2. Principle of Excellent Application Ability
2.2.3. Principle of a Stable Classification System
2.3. Proposed Classification Strategy
3. Definition and Characteristics of the Main Types of Medical Robot
3.1. Surgical Robots
3.2. Rehabilitation Robots
3.3. Medical Assistant Robots
3.4. Hospital Service Robots
4. Development Status and Secondary Classification Strategy of Surgical Robots
4.1. Development Status of Surgical Robots
4.1.1. Neurosurgery
4.1.2. Orthopedics
4.1.3. Endoscope
4.1.4. Intrusive Surgery
4.2. The Necessity of Secondary Classification of Surgical Robots
4.3. Secondary Classification Strategy for Surgical Robots
5. Development Status and Secondary Classification Strategy of Rehabilitation Robots
5.1. Development Status of Rehabilitation Robots
5.1.1. Rehabilitation Training Scene
5.1.2. Life Assisted Scenes
5.2. Secondary Classification Strategy for Rehabilitation Robots
6. Expectations and Outlook
6.1. Security
6.2. Low Cost
6.3. Clinical Needs
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Veiga, T.D.; Chandler, J.H.; Lloyd, P.; Pittiglio, G.; Valdastri, P. Challenges of continuum robots in clinical context: A review. Prog. Biomed. Eng. 2020, 2, 032003. [Google Scholar] [CrossRef]
- Schiavina, R.; Bianchi, L.; Borghesi, M.; Dababneh, H.; Chessa, F.; Pultrone, C.V.; Angiolini, A.; Gaudiano, C.; Porreca, A.; Fiorentino, M.; et al. Mri displays the prostatic cancer anatomy and improves the bundles management before robot-assisted radical prostatectomy. J. Endourol. 2018, 32, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Park, H.S.; Lee, J.; Lee, H.; Lee, K.; Song, S.Y.; Toesca, A. Development of robotic mastectomy using a single-port surgical robot system. J. Breast Cancer 2020, 23, 107–112. [Google Scholar] [CrossRef]
- Wang, D.; Wang, Y.; Zi, B.; Cao, Z.; Ding, H. Development of an active and passive finger rehabilitation robot using pneumatic muscle and magnetorheological damper. Mech. Mach. Theory 2020, 147, 103762. [Google Scholar] [CrossRef]
- Ogata, K.; Matsumoto, Y. Estimating road surface and gradient using internal sensors for robot assist walker. In Proceedings of the 2020 IEEE/SICE International Symposium on System Integration (SII), Honolulu, HI, USA, 12–15 January 2020; pp. 826–831. [Google Scholar]
- Nüesch, R.; Alt, R.; Puschmann, T. Hybrid customer interation. Bus. Inf. Syst. Eng. 2015, 57, 73–78. [Google Scholar] [CrossRef]
- Hung, C.-L. The research of factors influencing advanced medical robot use. Qual. Quant. 2021, 55, 385–393. [Google Scholar] [CrossRef]
- Kwoh, Y.S.; Hou, J.; Jonckheere, E.A.; Hayati, S. A robot with improved absolute positioning accuracy for ct guided stereo-tactic brain surgery. IEEE Trans. Biomed. Eng. 1988, 35, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Kucuk, S. Introductory chapter: Medical robots in surgery and rehabilitation. In Medical Robotics-New Achievements; I-Tech Education and Publishing: London, UK, 2020. [Google Scholar]
- Pransky, J. Robodoc-surgical robot success story. Ind. Robot Int. J. 1997, 24, 231–233. [Google Scholar] [CrossRef]
- Shah, K.; Abaza, R. Comparison of intraoperative outcomes using the new and old generation da vinci® robot for robot-assisted laparoscopic prostatectomy. BJU Int. 2011, 108, 1642–1645. [Google Scholar] [CrossRef] [PubMed]
- Brandao, L.F.; Autorino, R.; Laydner, H.; Haber, G.P.; Ouzaid, I.; De Sio, M.; Perdonà, S.; Stein, R.J.; Porpiglia, F.; Kaouk, J.H. Robotic versus laparoscopic adrenalectomy: A systematic review and meta-analysis. Eur. Urol. 2014, 65, 1154–1161. [Google Scholar] [CrossRef]
- Ginhoux, R.; Gangloff, J.; de Mathelin, M.; Soler, L.; Sanchez MM, A.; Marescaux, J. Active filtering of physiological motion in robotized surgery using predictive control. IEEE Trans. Robot. 2005, 21, 67–79. [Google Scholar] [CrossRef] [Green Version]
- Zhou, H.X.; Guo, Y.H.; Yu, X.F.; Bao, S.Y.; Liu, J.L.; Zhang, Y.; Ren, Y.G. Zeus robot-assisted laparoscopic cholecystectomy in comparison with conventional laparoscopic cholecystectomy. Hepatobiliary Pancreat. Dis. Int. 2006, 5, 115–118. [Google Scholar] [PubMed]
- Hannaford, B.; Rosen, J.; Friedman, D.W.; King, H.; Roan, P.; Cheng, L.; Glozman, D.; Ma, J.; Kosari, S.N.; White, L. Raven-ii: An open platform for surgical robotics research. IEEE Trans. Biomed. Eng. 2012, 60, 954–959. [Google Scholar] [CrossRef]
- Lewis, A.; Hannaford, B. Dynamically evaluated gravity compensation for the raven surgical robot. In Proceedings of the 2014 IEEE International Conference on Robotics and Automation (ICRA), Hong Kong, China, 31 May–7 June 2014; pp. 2534–2539. [Google Scholar]
- Velasquez, C.A.; King, H.H.; Hannaford, B.; Yoon, W.J. Development of a flexible imaging probe integrated to a surgical telerobot system: Preliminary remote control test and probe design. In Proceedings of the 2012 4th IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), Rome, Italy, 24–27 June 2012; pp. 894–898. [Google Scholar]
- Bodner, J.; Wykypiel, H.; Wetscher, G.; Schmid, T. First experiences with the da vinci™ operating robot in thoracic surgery. Eur. J. Cardio-Thorac. Surg. 2004, 25, 844–851. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Latif, A.A.; Nizamani, M.A.; Shoro, G.M.; Abassi, F.; Memon, B.R. Design and control of autonomous robot using gesture based intuitive interaction. Int. J. Adv. Comput. Syst. Softw. Eng. 2020, 1, 18–22. [Google Scholar]
- Orozco-Magdaleno, E.C.; Cafolla, D.; Castañeda, E.C.; Carbone, G. A hybrid legged-wheeled obstacle avoidance strategy for service operations. SN Appl. Sci. 2020, 2, 329. [Google Scholar] [CrossRef] [Green Version]
- Jia, Y.; Ma, S. A Coach-Based Bayesian Reinforcement Learning Method for Snake Robot Control. IEEE Robot. Autom. Lett. 2021, 6, 2319–2326. [Google Scholar] [CrossRef]
- Rydgren, M. Humanoid Robots in Healthcare: A Quantitative Study about Students’ Attitudes. Master’s Thesis, Åbo Akademi University, Turku, Finland, May 2020. [Google Scholar]
- Hudson, J.; Orviska, M.; Hunady, J. People’s attitudes to robots in caring for the elderly. Int. J. Soc. Robot. 2017, 9, 199–210. [Google Scholar] [CrossRef]
- Wu, Y.-H.; Fassert, C.; Rigaud, A.-S. Designing robots for the elderly: Appearance issue and beyond. Arch. Gerontol. Geriatr. 2012, 54, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Johansson-Pajala, R.-M.; Thommes, K.; Hoppe, J.A.; Tuisku, O.; Hennala, L.; Pekkarinen, S.; Melkas, H.; Gustafsson, C. Care robot orientation: What, who and how? Potential users’ perceptions. Int. J. Soc. Robot. 2020, 12, 1103–1117. [Google Scholar] [CrossRef] [Green Version]
- Graf, B.; Reiser, U.; Hägele, M.; Mauz, K.; Klein, P. Robotic home assistant care-o-bot® 3-product vision and innovation platform. In Proceedings of the 2009 IEEE Workshop on Advanced Robotics and Its Social Impacts, Tokyo, Japan, 23–25 November 2009; pp. 139–144. [Google Scholar]
- Cavallo, F.; Limosani, R.; Manzi, A.; Bonac-corsi, M.; Esposito, R.; di Rocco, M.; Pecora, F.; Teti, G.; Saffiotti, A.; Dario, P. Development of a socially believable multi-robot solution from town to home. Cogn. Comput. 2014, 6, 954–967. [Google Scholar] [CrossRef] [Green Version]
- Di Nuovo, A.; Broz, F.; Wang, N.; Belpaeme, T.; Cangelosi, A.; Jones, R.; Esposito, R.; Cavallo, F.; Dario, P. The multi-modal interface of Robot-Era multi-robot services tailored for the elderly. Intell. Serv. Robot. 2018, 11, 109–126. [Google Scholar] [CrossRef] [Green Version]
- Gustafsson, C.; Svanberg, C.; Müllersdorf, M. Using a robotic cat in dementia care: A pilot study. J. Gerontol. Nurs. 2015, 41, 46–56. [Google Scholar] [CrossRef]
- Wada, K.; Shibata, T.; Musha, T.; Kimura, S. Effects of robot therapy for demented patients evaluated by eeg. In Proceedings of the 2005 IEEE/RSJ International Conference on Intelligent Robots and Systems, Edmonton, AB, Canada, 2–6 August 2005; pp. 1552–1557. [Google Scholar]
- Martinez-Martin, E.; del Pobil, A.P. Personal robot assistants for elderly care: An overview. In Personal Assistants: Emerging Computational Technologies; Springer: Berlin/Heidelberg, Germany, 11 August 2018; pp. 77–91. [Google Scholar]
- Li, D.; Rau, P.L.P.; Li, Y. A cross-cultural study: Effect of robot appearance and task. Int. J. Soc. Robot. 2010, 2, 175–186. [Google Scholar] [CrossRef]
- Jiang, A.; Secco, E.; Wurdemann, H.; Nanayakkara, T.; Dasgupta, P.; Athoefer, K. Stiffness-controllable octopus-like robot arm for minimally invasive surgery. In Proceedings of the 3rd Joint Workshop on New Technologies for Computer/Robot Assisted Surgery, Verona, Italy, 11–13 September 2013. [Google Scholar]
- Sareh, S.; Jiang, A.; Faragasso, A.; Noh, Y.; Nanayakkara, T.; Dasgupta, P.; Seneviratne, L.D.; Wurdemann, H.A.; Althoefer, K. Bio-inspired tactile sensor sleeve for surgical soft manipulators. In Proceedings of the 2014 IEEE International Conference on Robotics and Automation (ICRA), Hong Kong, China, 31 May–7 June 2014; pp. 1454–1459. [Google Scholar]
- Potnuru, A.; Jafarzadeh, M.; Tadesse, Y. 3d printed dancing humanoid robot “buddy” for homecare. In Proceedings of the 2016 IEEE International Conference on Automation Science and Engineering (CASE), Fort Worth, TX, USA, 21–24 August 2016; pp. 733–738. [Google Scholar]
- Pino, O.; Palestra, G.; Trevino, R.; de Carolis, B. The humanoid robot nao as trainer in a memory program for elderly people with mild cognitive impairment. Int. J. Soc. Robot. 2020, 12, 21–33. [Google Scholar] [CrossRef]
- Dario, P.; Guglielmelli, E.; Allotta, B. Robotics in medicine. In Proceedings of the IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS’94), Munich, Germany, 12–16 September 1994; Volume 2, pp. 739–752. [Google Scholar]
- ISO 8373: 2012. Robots and Robotic Devices-Vocabulary. In International Standards Organization; Vernier: Geneva, Switzerland, March 2012; p. 38.
- The Official Website of the International Federation of Robotics. Available online: https://ifr.org/ (accessed on 3 January 2019).
- Antipina, E.V.; Ivshin, K.S. Classification system of shaping characteristics of personal service robots. Int. Trans. J. Eng. Manag. Appl. Sci. Technol. 2019, 10, 1014. [Google Scholar]
- Entsfellner, K.; Schuermann, J.; Coy, J.A.; Strauss, G.; Lueth, T.C. A modular micro-macro robot system for instrument guiding in middle ear surgery. In Proceedings of the 2015 IEEE International Conference on Robotics and Biomimetics (ROBIO), Zhuhai, China, 6–9 December 2015; pp. 374–379. [Google Scholar]
- Kim, S.M.; Yi, B.; Chung, J.; Cheong, J.; Kim, W. Development of a new neurosurgical 5-dof parallel robot for stereotactic dbs operations. Int. J. Precis. Eng. Manuf. 2017, 18, 333–343. [Google Scholar] [CrossRef]
- Du, Z.; Sun, L.; Fu, L. Overview of the development of medical robots. Robotics 2003, 25, 182–187. [Google Scholar]
- Wang, T.; Zhang, D.; Liu, D. A perspective on medical robotics. Chin. J. Med. Instrum. 2008, 32, 235–238. [Google Scholar]
- Zhang, X.; Ma, X.; Zhou, J.; Zhou, Q. Summary of medical robot technology development. In Proceedings of the 2018 IEEE International Conference on Mechatronics and Automation (ICMA), Changchun, China, 5–8 August 2018; pp. 443–448. [Google Scholar]
- Lou, Y. A review of medical robot technology development and research. China Strateg. Emerg. Ind. 2017, 48. [Google Scholar]
- Khan, A.; Anwar, Y. Robots in healthcare: A survey. In Science and Information Conference; Springer: Las Vegas, NV, USA, 2019; pp. 280–292. [Google Scholar]
- Okamura, A.M.; Mataric’, M.J.; Christensen, H.I. Medical and health-care robotics. IEEE Robot. Autom. Mag. 2010, 17, 26–37. [Google Scholar] [CrossRef]
- Radice, L. Challenge in surgical robot development. In Clinical Engineering Handbook; Elsevier Academic Press: Salt Lake City, UT, USA, 2020; pp. 469–472. [Google Scholar]
- Tarawneh, A.M.; Salem, K.M.I. A systematic review and meta-analysis of randomized controlled trials comparing the accuracy and clinical outcome of pedicle screw placement using robot-assisted technology and conventional freehand technique. Glob. Spine J. 2020. [Google Scholar] [CrossRef]
- Kamarajah, S.K.; Bundred, J.R.; Marc, O.S.; Jiao, L.R.; Hilal, M.A.; Manas, D.M.; White, S.A. A systematic review and network meta-analysis of different surgical approaches for pancreaticoduodenectomy. HPB 2020, 22, 329–339. [Google Scholar] [CrossRef]
- Zhou, Y.; Wang, N. Overview of rehabilitation robot. Chin. J. Rehabil. Med. 2015, 30, 400–403. [Google Scholar]
- Nawrat, Z. MIS AI-artificial intelligence application in minimally invasive surgery. Mini-Invasive Surg. 2020, 4. [Google Scholar] [CrossRef]
- Li, B.; Li, G.; Sun, Y.; Jiang, G.; Kong, J.; Jiang, D. A review of rehabilitation robot. In Proceedings of the 2017 32nd Youth Academic Annual Conference of Chinese Association of Automation (YAC), Hefei, China, 19–21 May 2017; pp. 907–911. [Google Scholar]
- Ching, H.L.; Hale, M.F.; Sidhu, R.; McAlindon, M.E. Pth-050 robot magnet-controlled upper gi capsule endoscopy using the ankon navi-cam® system: First reported experience outside china. BMJ J. 2017, 66, A230. [Google Scholar]
- Son, D.; Gilbert, H.; Sitti, M. Magnetically actuated soft capsule endoscope for fine-needle biopsy. Soft Robot. 2020, 7, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Bao, Z.; Fu, Q.; Guo, S. Design and implementation of a novel wireless modular capsule robotic system in pipe. Med. Biol. Eng. Comput. 2020, 58, 2305–2324. [Google Scholar] [CrossRef]
- Shubha, P.; Meenakshi, M. Design and implementation of healthcare assistive robot. In Proceedings of the 2019 5th International Conference on Advanced Computing & Communication Systems (ICACCS), Coimbatore, India, 15–16 March 2019; pp. 61–65. [Google Scholar]
- Ramesh, C.R. Intelligent prescription delivery mobile robot. Stud. Indian Place Names 2020, 40, 260–265. [Google Scholar]
- Qureshi, D.; Salim, M.; Singh, P.; Swarnkar, P.; Goud, H. Robotics solutions to combat novel corona virus disease-2019 (covid-19). In Pushpendra and Swarnkar, Pankaj and Goud, Harsh, Robotics Solutions to Combat Novel Corona Virus Disease-2019 (COVID-19); Elsevier: Amsterdam, The Netherlands, 8 June 2020. [Google Scholar]
- Deng, Y. Timrobot: Remove the crown from the pyramid. Pudong Dev. 2017, 6, 20–21. [Google Scholar]
- Smith, J.A.; Jivraj, J.; Wong, R.; Yang, V. 30 Years of Neurosurgical Robots: Review and Trends for Manipulators and Associated Navigational Systems. Ann. Biomed. Eng. 2016, 44, 836–846. [Google Scholar] [CrossRef]
- Bertelsen, A.; Melo, J.; Sánchez, E.; Borro, D. A review of surgical robots for spinal interventions. Int. J. Med. Robot. Comput. Assist. Surg. 2013, 9, 407–422. [Google Scholar] [CrossRef]
- Yasin, H.; Hoff, H.-J.; Blümcke, I.; Simon, M. Experience with 102 Frameless Stereotactic Biopsies Using the neuromate Robotic Device. World Neurosurg. 2019, 123, e450–e456. [Google Scholar] [CrossRef]
- Dawes, W.; Marcus, H.J.; Tisdall, M.; Aquilina, K. Robot-assisted stereotactic brainstem biopsy in children: Prospective cohort study. J. Robot. Surg. 2019, 13, 575–579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Candela, S.; Vanegas, M.I.; Darling, A.; Ortigoza-Escobar, J.D.; Alamar, M.; Muchart, J.; Pérez-Dueñas, B. Frameless robot-assisted pallidal deep brain stimulation surgery in pediatric patients with movement disorders: Precision and short-term clinical results. J. Neurosurg. Pediatr. 2018, 22, 416–425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takács, A.; Nagy, D.A.; Rudas, I.; Haidegger, T. Origins of surgical robotics: From space to the operating room. Acta Polytech. Hung. 2016, 13, 13–30. [Google Scholar]
- Du, Z.; Sun, L. Review of surgical robotics and key techniques analysis. In Proceedings of the IEEE International Conference on Robotics, Intelligent Systems and Signal Processing, Changsha, Shanghai, 8–13 October 2003; Volume 2, pp. 1041–1046. [Google Scholar]
- Villotte, N.; Glauser, D.; Flury, P.; Burckardt, C.W. Conception of stereotactic instruments for the neurosurgical robot minerva. In Proceedings of the 1992 14th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Paris, France, 29 October–1 November 1992; Volume 3, pp. 1089–1090. [Google Scholar]
- Sutherland, G.R.; Lama, S.; Gan, L.S.; Wolfsberger, S.; Zareinia, K. Merging machines with microsurgery: Clinical experience with neuroarm. J. Neurosurg. 2013, 118, 521–529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- González-Martínez, J.; Bulacio, J.; Thompson, S.; Gale, J.; Smithason, S.; Najm, I.; Bingaman, W. Technique, results, and complications related to robot-assisted stereoelectroen-cephalography. Neurosurgery 2016, 78, 169–180. [Google Scholar] [CrossRef] [Green Version]
- Lefranc, M.; Capel, C.; Pruvot-Occean, A.-S.; Fichten, A.; Desenclos, C.; Toussaint, P.; Le Gars, D.; Peltier, J. Frameless robotic stereotactic biopsies: A consecutive series of 100 cases. J. Neurosurg. 2015, 122, 342–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brandmeir, N.; Acharya, V.; Sather, M. Robot Assisted Stereotactic Laser Ablation for a Radiosurgery Resistant Hypothalamic Hamartoma. Cureus 2016, 8. [Google Scholar] [CrossRef] [Green Version]
- Bekelis, K.; Radwan, T.A.; Desai, A.; Roberts, D.W. Frameless robotically targeted stereotactic brain biopsy: Feasibility, diagnostic yield, and safety. J. Neurosurg. 2012, 116, 1002–1006. [Google Scholar] [CrossRef] [PubMed]
- Burgner, J.; Swaney, P.J.; Lathrop, R.A.; Weaver, K.D.; Webster, R.J. Debulking From Within: A Robotic Steerable Cannula for Intracerebral Hemorrhage Evacuation. IEEE Trans. Biomed. Eng. 2013, 60, 2567–2575. [Google Scholar] [CrossRef]
- Liu, J.; Zhang, Y.; Wang, T.; Xing, H.; Tian, Z. Neuromaster: A robot system for neurosurgery. In Proceedings of the IEEE International Conference on Robotics and Automation, New Orleans, LA, USA, 26 April–1 May 2004; Volume 1, pp. 824–828. [Google Scholar]
- Liu, J.; Zhang, Y.; Li, Z. The application accuracy of neuromaster: A robot system for stereotactic neurosurgery. In Proceedings of the 2006 2nd IEEE/ASME International Conference on Mechatronics and Embedded Systems and Applications, Beijing, China, 13–16 August 2006; pp. 1–5. [Google Scholar]
- Yang, X.; Li, Z.; Xu, W. Research status and progress of surgical robot. J. Hebei Union Univ. Med. Ed. 2012, 14, 176–177. [Google Scholar]
- Wang, Z.; Qin, Z.; Wang, H.; Yang, H.; Zheng, H.; Zhang, J.; Liu, X.; Wang, Z.; Wang, Y. Model cas-r-2 frameless stereodirected instrument assisted stereotactic aspiration and drainage for small supratentorial hematomas from hypertensive intracerebral hemorrhage. Clin. J. Med. Off. 2007, 6, 41. [Google Scholar]
- Han, X.; Liu, Y.; Fan, M.; Tian, W. Development and clinical application of orthopedic surgical robot technology. Tech. Rev. 2017, 35, 19–25. [Google Scholar]
- Wang, N.; Zhang, Z.; Zhang, X. Stabilization control for acrobot based on siso stabilization method. J. Hunan Inst. Sci. Technol. 2018. [Google Scholar] [CrossRef]
- Kant, A.J.; Klein, M.D.; Langenburg, S.E. Robotics in pediatric surgery: Perspectives for imaging. Pediatr. Radiol. 2004, 34, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Craven, M.P.; Davey, S.M.; Martin, J.L. Factors Influencing Wider Acceptance of Computer Assisted Orthopaedic Surgery (caos) Technologies for Total Joint Arthroplasty; University of Nottingham: Nottingham, UK, 12 November 2020. [Google Scholar]
- Simon, D.A.; Jaramaz, B.; Blackwell, M.; Morgan, F.; DiGioia, A.M.; Kischell, E.; Colgan, B.; Kanade, T. Development and validation of a navigational guidance system for acetabular implant placement. In CVRMed-MRCAS’97; Springer: Berlin/Heidelberg, Germany, 1997; pp. 583–592. [Google Scholar]
- Ahmadian, R.; Lorke, C.; Mai, S.; Siebert, W. 5 years of results with the operation robot system caspar in knee tep implants. Z. Orthop. 2006, 144, 124–126. [Google Scholar]
- Grimm, F.; Naros, G.; Gutenberg, A.; Keric, N.; Giese, A.; Gharabaghi, A. Blurring the boundaries between frame-based and frameless stereotaxy: Feasibility study for brain biopsies performed with the use of a head-mounted robot. J. Neurosurg. 2015, 123, 737–742. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Minchev, G.; Kronreif, G.; Martínez-Moreno, M.; Dorfer, C.; Micko, A.; Mert, A.; Kiesel, B.; Widhalm, G.; Knosp, E.; Wolfsberger, S. A novel miniature robotic guidance device for stereotactic neurosurgical interventions: Preliminary experience with the iSYS1 robot. J. Neurosurg. 2017, 126, 985–996. [Google Scholar] [CrossRef]
- Lefranc, M.; Peltier, J. Evaluation of the ROSA™ Spine robot for minimally invasive surgical procedures. Expert Rev. Med. Devices 2016, 13, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Seidenstein, A.; Birmingham, M.; Foran, J.; Ogden, S. Better accuracy and reproducibility of a new robotically-assisted system for total knee arthroplasty compared to conventional instrumentation: A cadaveric study. Knee Surg. Sports Traumatol. Arthrosc. 2020, 29, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tian, W.; Wei, Y.; Han, X. The history and development of robot-assisted orthopedic surgery. In Navigation Assisted Robotics in Spine and Trauma Surgery; Springer: Berlin/Heidelberg, Germany, 2020; pp. 1–3. [Google Scholar]
- Long, T.; Li, K.; Gao, J.; Liu, T.; Mu, J.; Wang, X.; Peng, C.; He, Z. Comparative Study of Percutaneous Sacroiliac Screw with or without TiRobot Assistance for Treating Pelvic Posterior Ring Fractures. Orthop. Surg. 2019, 11, 386–396. [Google Scholar] [CrossRef]
- Ni, Z.; Wang, T.; Liu, D. Overview of medical robotics technology development. J. Mech. Eng. 2015, 51, 45–52. [Google Scholar] [CrossRef]
- Mettler, L.; Ibrahim, M.; Jonat, W. One year of experience working with the aid of a robotic assistant (the voice-controlled optic holder AESOP) in gynaecological endoscopic surgery. Hum. Reprod. 1998, 13, 2748–2750. [Google Scholar] [CrossRef] [Green Version]
- Sah, C.; Kuzgunbay, B. Does Robot-assisted Surgery in Urology Has Benefits? The Current Status. Bull Urooncol. 2019, 18, 117–119. [Google Scholar] [CrossRef]
- Lee, C.-H.; Kim, J.B.; Jung, S.-H.; Choo, S.J.; Chung, C.H.; Lee, J.W. Left Atrial Appendage Resection Versus Preservation During the Surgical Ablation of Atrial Fibrillation. Ann. Thorac. Surg. 2014, 97, 124–132. [Google Scholar] [CrossRef]
- Fujie, M.G.; Zhang, B. State-of-the-art of intelligent minimally invasive surgical robots. Front. Med. 2020, 14, 404–416. [Google Scholar] [CrossRef]
- Hung, A.J.; Chen, J.; Shah, A.; Gill, I.S. Telementoring and telesurgery for minimally invasive procedures. J. Urol. 2018, 199, 355–369. [Google Scholar] [CrossRef] [PubMed]
- Peters, B.S.; Armijo, P.R.; Krause, C.; Choudhury, S.A.; Oleynikov, D. Review of emerging surgical robotic technology. Surg. Endosc. 2018, 32, 1636–1655. [Google Scholar] [CrossRef]
- Harichane, A.; Chauvet, D.; Hans, S. Nasopharynx access by minimally invasive transoral robotic surgery: Anatomical study. J. Robot. Surg. 2018, 12, 687–692. [Google Scholar] [CrossRef]
- Kuo, C.-H.; Dai, J.S. Robotics for minimally invasive surgery: A historical review from the perspective of kinematics. In International Symposium on History of Machines and Mechanisms; Springer: Berlin/Heidelberg, Germany, 2009; pp. 337–354. [Google Scholar]
- Simaan, N.; Taylor, R.; Flint, P. A dexterous system for laryngeal surgery. In Proceedings of the IEEE International Conference on Robotics and Automation, New Orleans, LA, USA, 26 April–1 May 2004; Volume 1, pp. 351–357. [Google Scholar]
- Ding, J.; Xu, K.; Goldman, R.; Allen, P.; Fowler, D.; Simaan, N. Design, simulation and evaluation of kinematic alternatives for insertable robotic effectors platforms in single port access surgery. In Proceedings of the 2010 IEEE International Conference on Robotics and Automation, Anchorage, AK, USA, 3–8 May 2010; pp. 1053–1058. [Google Scholar]
- Wang, W.; Wang, W.; Yan, Z.; Du, Z.; He, S.; Chen, G.; Zhou, D. A review of the development of robotic laparoscopic surgery. Chin. Med. Equip. 2014, 29, 5–10. [Google Scholar]
- Wang, Z.; Zi, B.; Wang, D.; Qian, J.; You, W.; Yu, L. External Force Self-Sensing Based on Cable-Tension Disturbance Observer for Surgical Robot End-Effector. IEEE Sens. J. 2019, 19, 5274–5284. [Google Scholar] [CrossRef]
- Jing, Y.; Lingyan, J.; Xinge, S.; Deming, Z.; Ming, H.; Jin, L.; Shi, X.; Zhao, D.; Hu, M. Dimensional Optimization for Minimally Invasive Surgery Robot Based on Double Space and Kinematic Accuracy Reliability Index. J. Eng. Sci. Med. Diagn. Ther. 2020, 3. [Google Scholar] [CrossRef]
- Simorov, A.; Otte, R.S.; Kopietz, C.M.; Oleynikov, D. Review of surgical robotics user interface: What is the best way to control robotic surgery? Surg. Endosc. 2012, 26, 2117–2125. [Google Scholar] [CrossRef]
- Ram, W.; Meyer, H. Heart catheterization in a neonate by interacting magnetic fields: A new and simple method of catheter guidance. Catheter. Cardiovasc. Diagn. 1991, 22, 317–319. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zhang, Z.; Wang, Y.; Wang, Q. Applications of high magnetic field in interventional medical treatment. Chin. Sci. Bull. 2019, 64, 854–868. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, B.L.; Merino, J.L.; Shachar, Y.; Estrada, A.; Doiny, D.; Castrejon, S.; Marx, B.; Johnson, D.; Marfori, W.; Gang, E.S. Non-Fluoroscopic Transseptal Catheterization During Electrophysiology Procedures using a Remote Magnetic Navigation System. J. Atr. Fibrillation 2013, 6. [Google Scholar]
- Kim, Y.; Parada, G.A.; Liu, S.; Zhao, X. Ferromagnetic soft continuum robots. Sci. Robot. 2019, 4, eaax7329. [Google Scholar] [CrossRef]
- Picard, F.; Deakin, A.H.; Riches, P.E.; Deep, K.; Baines, J. Computer assisted orthopaedic surgery: Past, present and future. Med. Eng. Phys. 2019, 72, 55–65. [Google Scholar] [CrossRef]
- Lane, T. A short history of robotic surgery. Ann. R. Coll. Surg. Engl. 2018, 100, 5–7. [Google Scholar] [CrossRef]
- Kong, X. Minimally invasive surgical robots have been around for a long time. Robot. Ind. 2015, 5, 103. [Google Scholar]
- Friel, K.M.; Lee, P.; Soles, L.V.; Smorenburg, A.R.; Kuo, H.-C.; Gupta, D.; Edwards, D.J. Combined transcranial direct current stimulation and robotic upper limb therapy improves upper limb function in an adult with cerebral palsy. Neurorehabilitation 2017, 41, 41–50. [Google Scholar] [CrossRef] [Green Version]
- Jezernik, S.; Colombo, G.; Keller, T.; Frueh, H.; Morari, M. Robotic orthosis lokomat: A rehabilitation and research tool. Neuromodulation. Technol. Neural Interface 2003, 6, 108–115. [Google Scholar] [CrossRef]
- Lum, P.S.; Burgar, C.G.; Van Der Loos, M.; Shor, P.C.; Majmundar, M.; Yap, R. MIME robotic device for upper-limb neurorehabilitation in subacute stroke subjects: A follow-up study. J. Rehabilit. Res. Dev. 2006, 43, 631–642. [Google Scholar] [CrossRef]
- Shahbazi, M.; Atashzar, S.F.; Patel, R.V. A framework for supervised robotics-assisted mirror rehabilitation therapy. In Proceedings of the 2014 IEEE/RSJ International Conference on Intelligent Robots and Systems, Chicago, IL, USA, 14–18 September 2014; pp. 3567–3572. [Google Scholar]
- Germanotta, M.; Vasco, G.; Petrarca, M.; Rossi, S.; Carniel, S.; Bertini, E.; Cappa, P.; Castelli, E. Robotic and clinical evaluation of upper limb motor performance in patients with friedreich’s ataxia: An observational study. J. Neuroeng. Rehabilit. 2015, 12, 41. [Google Scholar] [CrossRef] [Green Version]
- El-Shamy, S. Efficacy of Armeo® Robotic Therapy Versus Conventional Therapy on Upper Limb Function in Children With Hemiplegic Cerebral Palsy. Am. J. Phys. Med. Rehabilit. 2018, 97, 164–169. [Google Scholar] [CrossRef]
- Faran, S.; Einav, O.; Yoeli, D.; Kerzhner, M.; Geva, D.; Magnazi, G.; van Kaick, S.; Mauritz, K.H. Reo assessment to guide the reogo therapy: Reliability and validity of novel robotic scores. In Proceedings of the 2009 Virtual Rehabilitation International Conference, Haifa, Israel, 29 June–2 July 2009; p. 209. [Google Scholar]
- Topping, M. An Overview of the Development of Handy 1, a Rehabilitation Robot to Assist the Severely Disabled. J. Intell. Robot. Syst. 2002, 34, 253–263. [Google Scholar] [CrossRef]
- De Ruiter, H.-P. Lifting devices revisited: Safer for nurses-but what about the patients? Am. J. Nurs. 2006, 106, 13. [Google Scholar] [CrossRef]
- Ganesan, V.; Gu, E.Y.L. Fall Protection Framework of Lower Extremity Exoskeleton Walking System Based on Differential Motion Planning. Int. J. Soc. Robot. 2020, 1–12. [Google Scholar] [CrossRef]
- Kex, X.; Chen, Y.; Tang, W. An overview of the research on the human lower extremity exoskeletons and its key technological analysis. Robot Tech. Appl. 2009, 6, 28–32. [Google Scholar]
- Li, X.; Sun, K.; Guo, C.; Liu, T.; Liu, H. Enhanced static modeling of commercial pneumatic artificial muscles. Assem. Autom. 2020, 40, 407–417. [Google Scholar] [CrossRef]
- Kai, X.; Zhao, X.; Chen, W. Research situation and development trend of robot exoskeleton. Chin. Med. Equip. J. 2015, 36, 104–107. [Google Scholar]
- Ouyang, X.P.; Fan, B.Q.; Ding, S. Current situation and prospect of the power assisted lower extremity external skeleton robot. Sci. Technol. Rev. 2015, 33, 92–99. [Google Scholar]
- Liu, B.; Wang, X.M.; Wang, H.Y. Research progress of gait rehabilitation robot. Chin. J. Trauma Disabil. Med. 2014, 122, 280–282. [Google Scholar]





| Classification Principe | Classification Method | Advantages | Disadvantages |
|---|---|---|---|
| Sizes and shapes | Macro-robot Micro-robot Biological robot |
|
|
| Application scenarios and functions | Surgical Robot Rehabilitation Robot Hospital-service Robot |
|
|
| Application scenarios | Surgical Robot Rehabilitation Robot Assistance Robot Medical service Robot |
|
|
| Functions/ Departments | Neurosurgery robot Cosmetic surgery robot Orthopedic robot Laparoscopic robot Vascular intrusive robot Auxiliary and Rehabilitation robot Capsule robot… |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, Y.; Yang, Y.; Liu, Y.; Li, Q.; Cao, F.; Feng, M.; Wu, H.; Li, W.; Kang, Y. Development Status and Multilevel Classification Strategy of Medical Robots. Electronics 2021, 10, 1278. https://doi.org/10.3390/electronics10111278
Guo Y, Yang Y, Liu Y, Li Q, Cao F, Feng M, Wu H, Li W, Kang Y. Development Status and Multilevel Classification Strategy of Medical Robots. Electronics. 2021; 10(11):1278. https://doi.org/10.3390/electronics10111278
Chicago/Turabian StyleGuo, Yingwei, Yingjian Yang, Yang Liu, Qiang Li, Fengqiu Cao, Mengting Feng, Hanhui Wu, Wei Li, and Yan Kang. 2021. "Development Status and Multilevel Classification Strategy of Medical Robots" Electronics 10, no. 11: 1278. https://doi.org/10.3390/electronics10111278
APA StyleGuo, Y., Yang, Y., Liu, Y., Li, Q., Cao, F., Feng, M., Wu, H., Li, W., & Kang, Y. (2021). Development Status and Multilevel Classification Strategy of Medical Robots. Electronics, 10(11), 1278. https://doi.org/10.3390/electronics10111278








