Comparison of Neck Pain and Posture with Spine Angle Tracking System between Static and Dynamic Computer Monitor Use
Abstract
1. Introduction
2. Materials and Methods
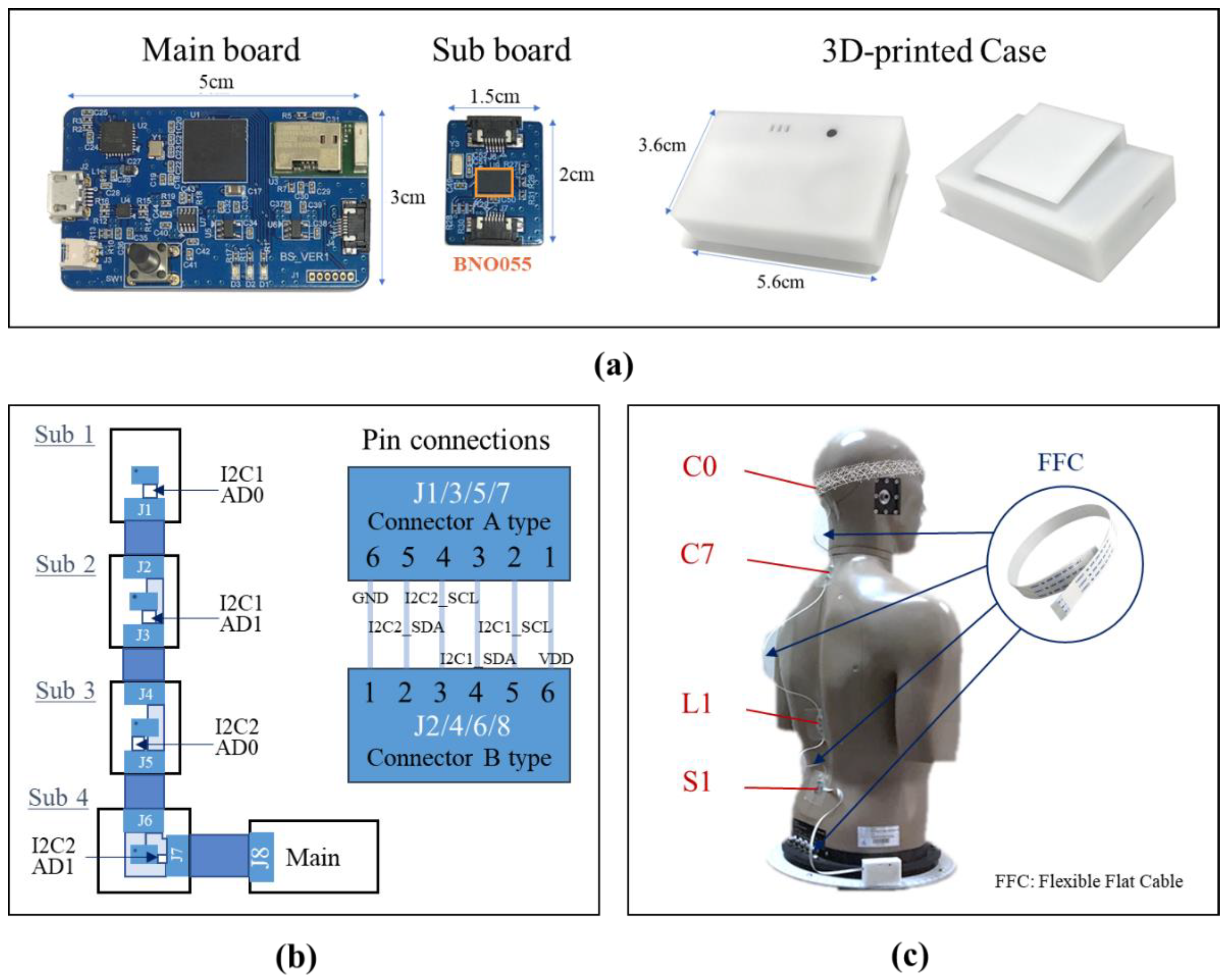
2.1. Spine Angle Tracking System
2.1.1. IMU-Embedded Wearable Device
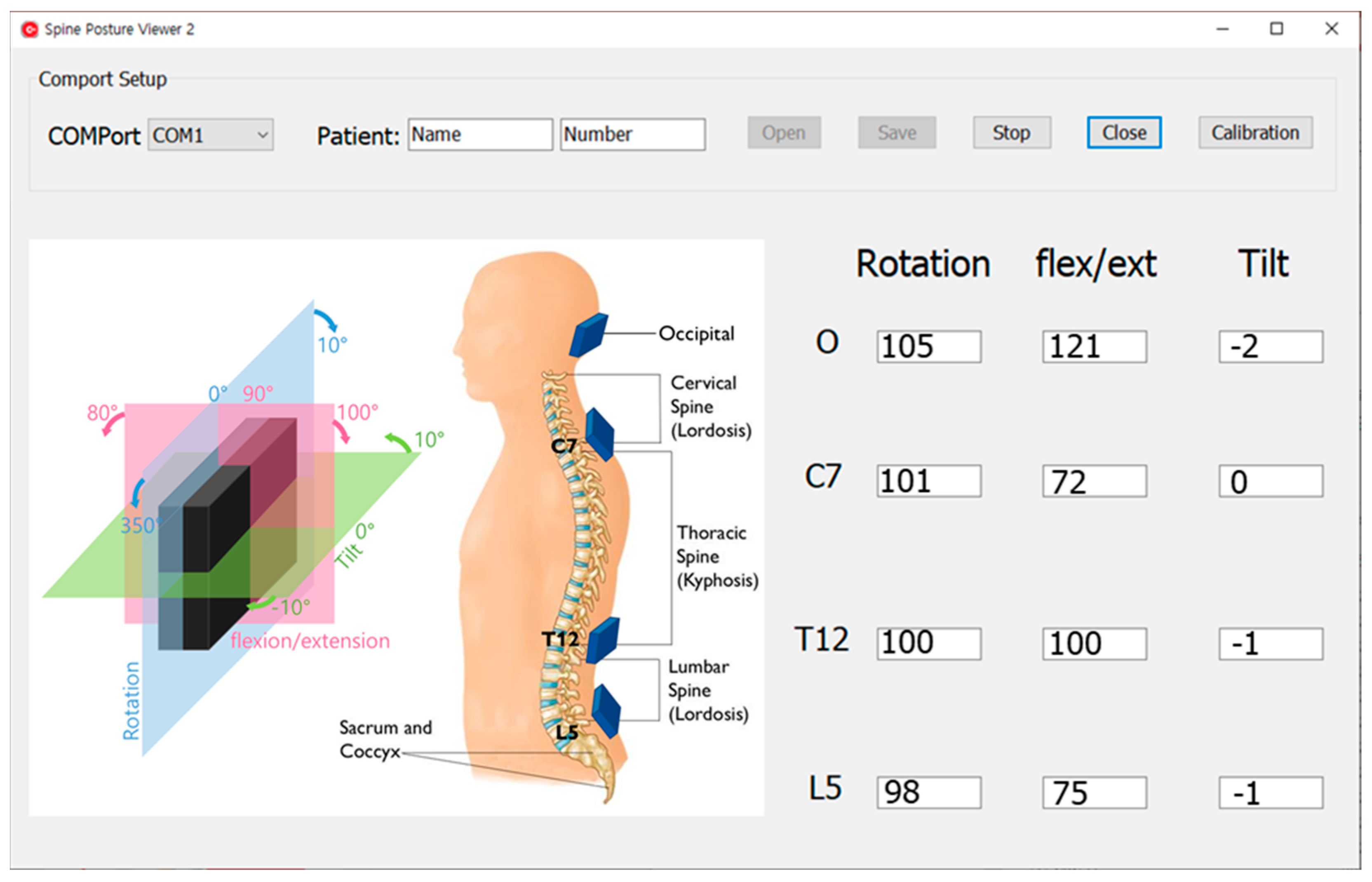
2.1.2. Data Acquisition and User Interface Viewer
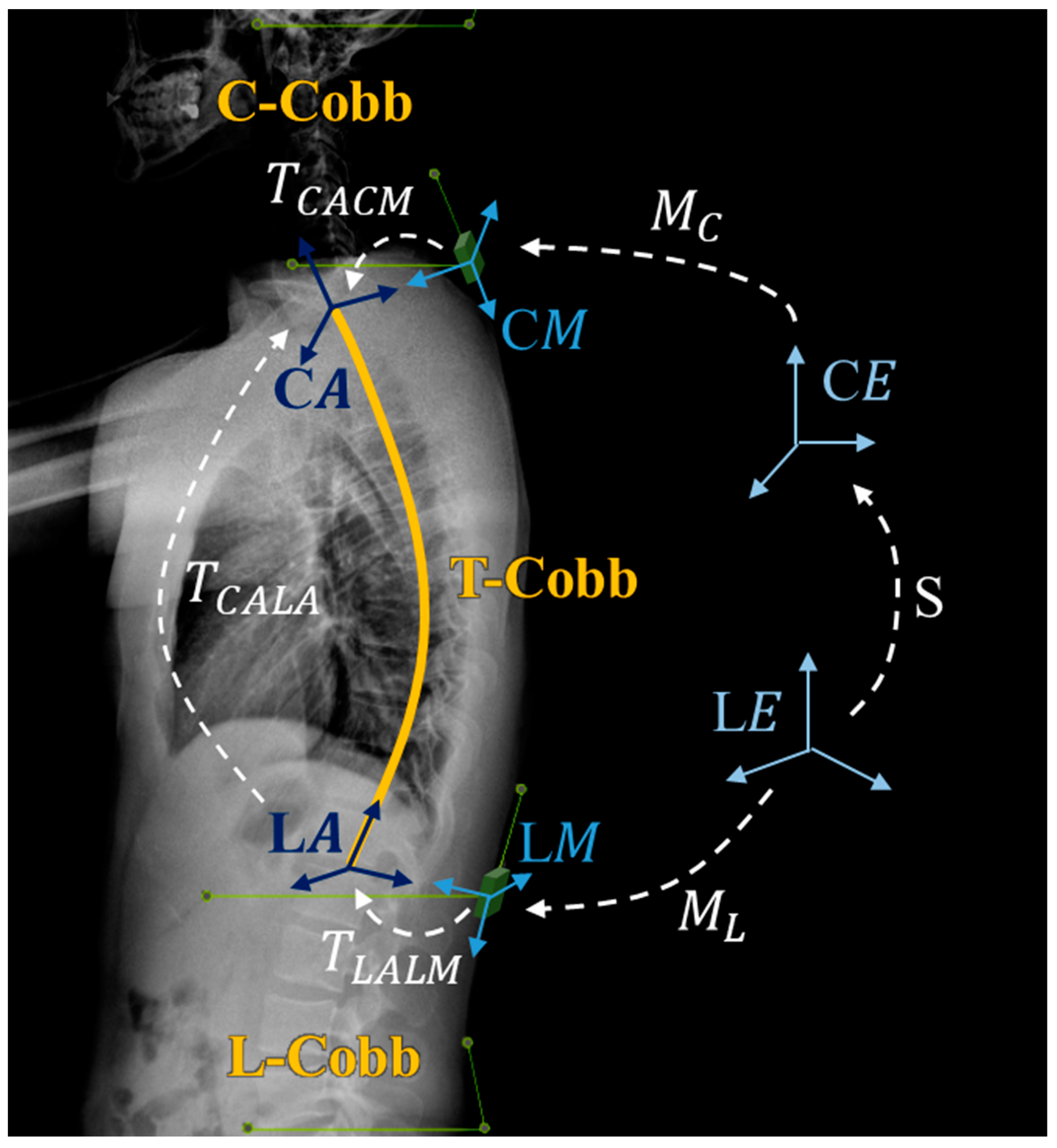
2.1.3. System Algorithms
2.2. Evaluation of Sensor Accuracy and Concordance between Sensor Estimates and X-ray Measurements
2.3. Experimental Design
2.3.1. Static Monitor and Dynamic Monitor
2.3.2. Measurements
2.4. Statistical Analysis
3. Results
3.1. Evaluation of Sensor Accuracy and Concordance between Sensor Estimates and X-ray Measurements
3.1.1. Sensor Accuracy
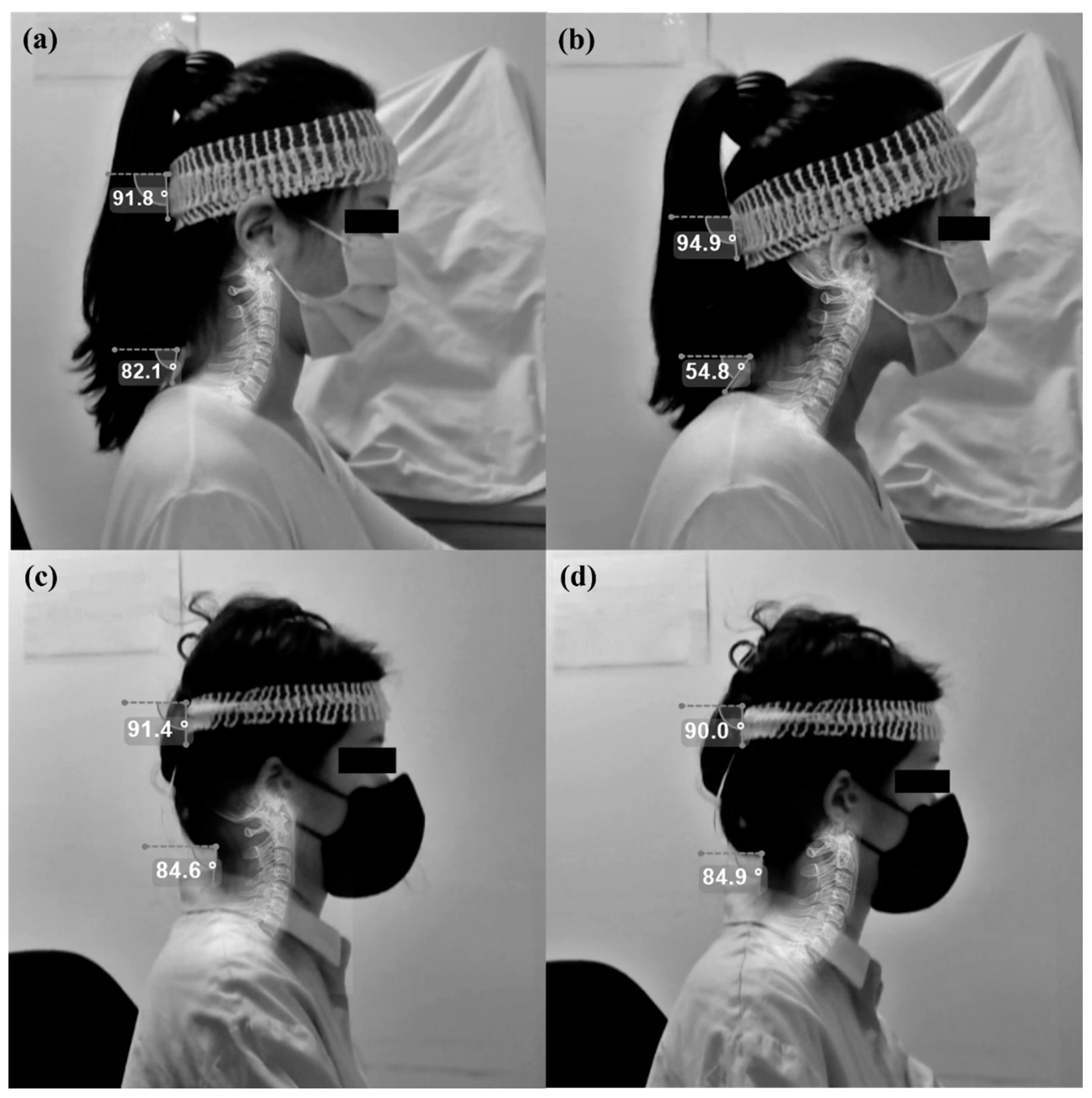
3.1.2. Concordance between Sensor Estimates and X-ray Measurements
3.2. Baseline Characteristics
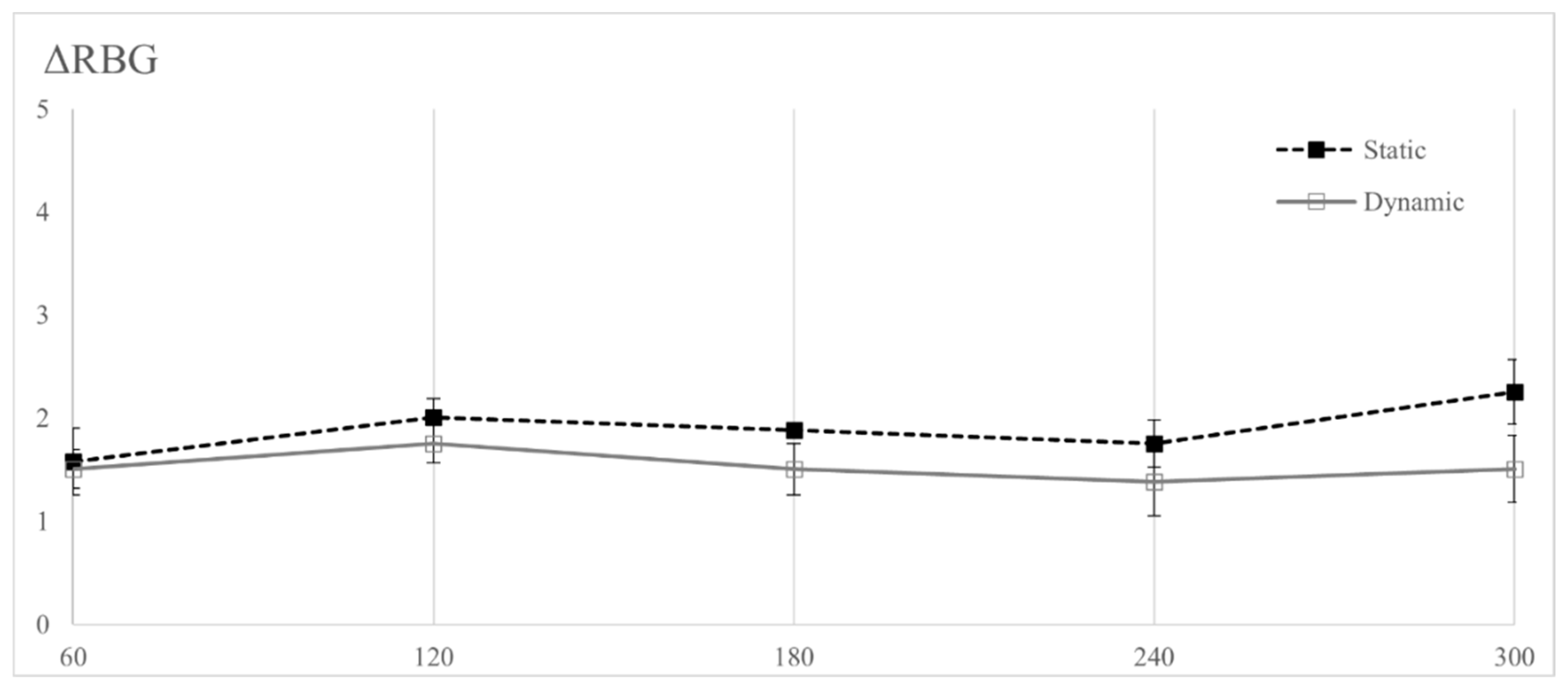
3.3. Neck Pain Change in Static and Dynamic Monitor Environment
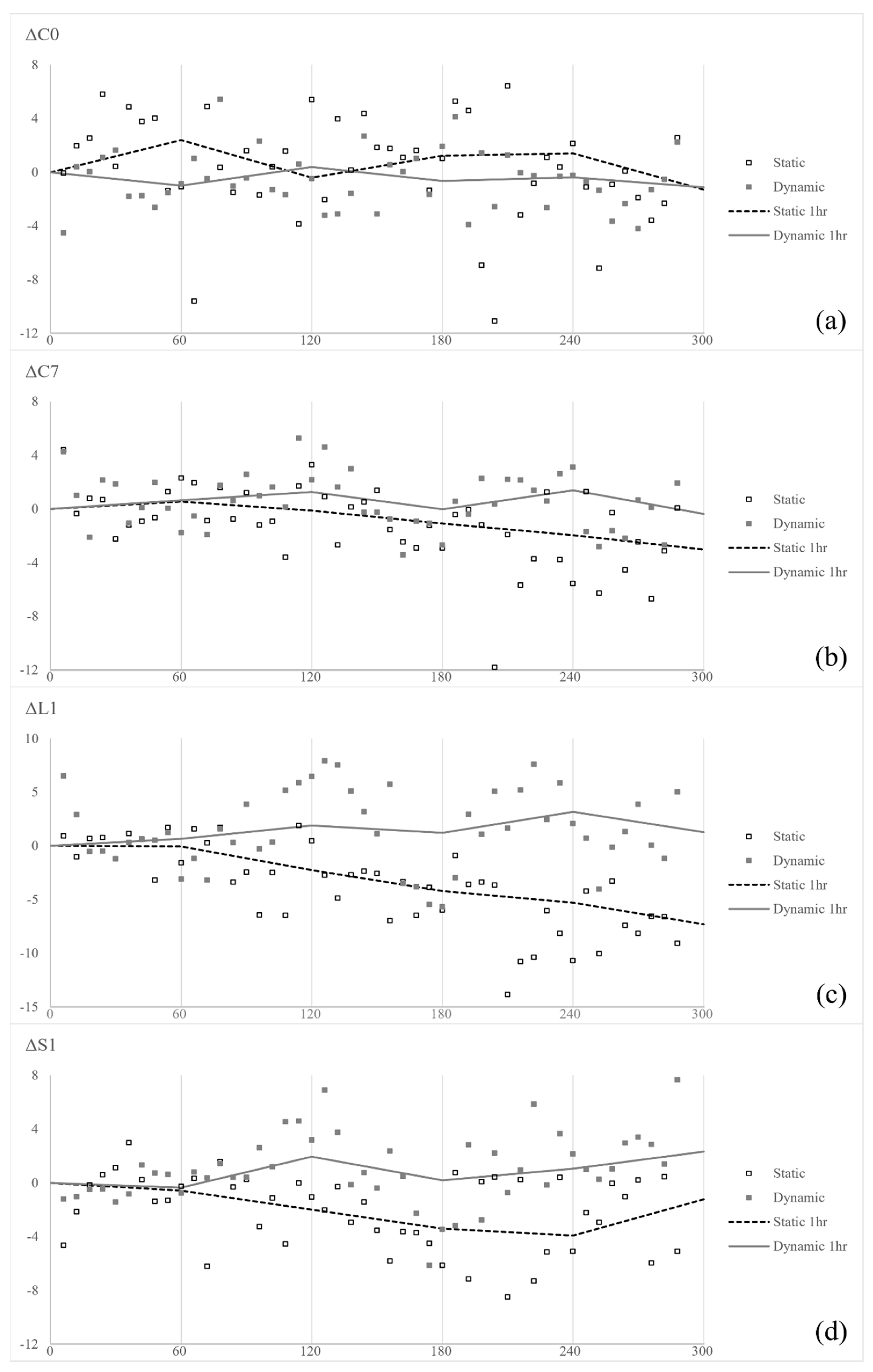
3.4. Spine Angle Change in Static and Dynamic Monitor Environment
3.5. Association between Neck Pain and Spine Angle or Monitor Setting
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Hoy, D.; March, L.; Woolf, A.; Blyth, F.; Brooks, P.; Smith, E.; Vos, T.; Barendregt, J.; Blore, J.; Murray, C.; et al. The global burden of neck pain: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014, 73, 1309–1315. [Google Scholar] [CrossRef] [PubMed]
- Hoy, D.G.; Protani, M.; De, R.; Buchbinder, R. The epidemiology of neck pain. Best Pract. Res. Clin. Rheumatol. 2010, 24, 783–792. [Google Scholar] [CrossRef] [PubMed]
- Yip, C.H.; Chiu, T.T.; Poon, A.T. The relationship between head posture and severity and disability of patients with neck pain. Man. Ther. 2008, 13, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Shaghayegh Fard, B.; Ahmadi, A.; Maroufi, N.; Sarrafzadeh, J. Evaluation of forward head posture in sitting and standing positions. Eur. Spine J. 2016, 25, 3577–3582. [Google Scholar] [CrossRef] [PubMed]
- Braun, B.L.; Amundson, L.R. Quantitative assessment of head and shoulder posture. Arch. Phys. Med. Rehabil. 1989, 70, 322–329. [Google Scholar] [PubMed]
- Nejati, P.; Lotfian, S.; Moezy, A.; Nejati, M. The study of correlation between forward head posture and neck pain in Iranian office workers. Int. J. Occup. Med. Environ. Health 2015, 28, 295–303. [Google Scholar] [CrossRef]
- Mahmoud, N.F.; Hassan, K.A.; Abdelmajeed, S.F.; Moustafa, I.M.; Silva, A.G. The Relationship Between Forward Head Posture and Neck Pain: A Systematic Review and Meta-Analysis. Curr. Rev. Musculoskelet. Med. 2019, 12, 562–577. [Google Scholar] [CrossRef] [PubMed]
- Falla, D.; Jull, G.; Hodges, P.W. Feedforward activity of the cervical flexor muscles during voluntary arm movements is delayed in chronic neck pain. Exp. Brain Res. 2004, 157, 43–48. [Google Scholar] [CrossRef]
- Schomacher, J.; Falla, D. Function and structure of the deep cervical extensor muscles in patients with neck pain. Man. Ther. 2013, 18, 360–366. [Google Scholar] [CrossRef]
- Kumar, S. Theories of musculoskeletal injury causation. Ergonomics 2001, 44, 17–47. [Google Scholar] [CrossRef]
- Ariens, G.A.; Bongers, P.M.; Douwes, M.; Miedema, M.C.; Hoogendoorn, W.E.; van der Wal, G.; Bouter, L.M.; van Mechelen, W. Are neck flexion, neck rotation, and sitting at work risk factors for neck pain? Results of a prospective cohort study. Occup. Environ. Med. 2001, 58, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Sikka, I.; Chawla, C.; Seth, S.; Alghadir, A.H.; Khan, M. Effects of Deep Cervical Flexor Training on Forward Head Posture, Neck Pain, and Functional Status in Adolescents Using Computer Regularly. Biomed. Res. Int. 2020, 2020, 8327565. [Google Scholar] [CrossRef]
- Cote, P.; van der Velde, G.; Cassidy, J.D.; Carroll, L.J.; Hogg-Johnson, S.; Holm, L.W.; Carragee, E.J.; Haldeman, S.; Nordin, M.; Hurwitz, E.L.; et al. The burden and determinants of neck pain in workers: Results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008, 33 (Suppl. S4), S60–S74. [Google Scholar] [CrossRef] [PubMed]
- Hakala, P.T.; Rimpela, A.H.; Saarni, L.A.; Salminen, J.J. Frequent computer-related activities increase the risk of neck-shoulder and low back pain in adolescents. Eur. J. Public Health 2006, 16, 536–541. [Google Scholar] [CrossRef] [PubMed]
- Auvinen, J.; Tammelin, T.; Taimela, S.; Zitting, P.; Karppinen, J. Neck and shoulder pains in relation to physical activity and sedentary activities in adolescence. Spine 2007, 32, 1038–1044. [Google Scholar] [CrossRef] [PubMed]
- Briggs, A.M.; Straker, L.M.; Bear, N.L.; Smith, A.J. Neck/shoulder pain in adolescents is not related to the level or nature of self-reported physical activity or type of sedentary activity in an Australian pregnancy cohort. BMC Musculoskelet. Disord. 2009, 10, 87. [Google Scholar] [CrossRef] [PubMed]
- Kothiyal, K.; Bjornerem, A.M. Effects of computer monitor setting on muscular activity, user comfort and acceptability in office work. Work 2009, 32, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Burgess-Limerick, R.; Plooy, A.; Ankrum, D.R. The effect of imposed and self-selected computer monitor height on posture and gaze angle. Clin Biomech. 1998, 13, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Chiou, W.K.; Chou, W.Y.; Chen, B.H. Notebook computer use with different monitor tilt angle: Effects on posture, muscle activity and discomfort of neck pain users. Work 2012, 41 (Suppl. S1), 2591–2595. [Google Scholar] [CrossRef]
- Jensen, C. Development of neck and hand-wrist symptoms in relation to duration of computer use at work. Scand. J. Work Environ. Health 2003, 29, 197–205. [Google Scholar] [CrossRef]
- Lau, K.T.; Cheung, K.Y.; Chan, M.H.; Lo, K.Y.; Chiu, T.T.W. Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity and disability. Man. Ther. 2010, 15, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Mascret, Q.; Bielmann, M.; Fall, C.-L.; Bouyer, L.J.; Gosselin, B. (Eds.) Real-time human physical activity recognition with low latency prediction feedback using raw IMU data. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018. [Google Scholar]
- Kobsar, D.; Charlton, J.M.; Tse, C.T.; Esculier, J.-F.; Graffos, A.; Krowchuk, N.M.; Thatcher, D.; Hunt, M.A. Validity and reliability of wearable inertial sensors in healthy adult walking: A systematic review and meta-analysis. J. Neuroeng. Rehabil. 2020, 17, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Jebelli, H.; Ahn, C.R.; Stentz, T.L. Comprehensive fall-risk assessment of construction workers using inertial measurement units: Validation of the gait-stability metric to assess the fall risk of iron workers. J. Comput. Civ. Eng. 2016, 30, 04015034. [Google Scholar] [CrossRef]
- Han, H.; Jang, H.; Yoon, S.W. Novel wearable monitoring system of forward head posture assisted by magnet-magnetometer pair and machine learning. IEEE Sens. J. 2019, 20, 3838–3848. [Google Scholar] [CrossRef]
- Lin, Z.R.; Xiong, Y.S.; Dai, H.D.; Xia, X.K. An Experimental Performance Evaluation of the Orientation Accuracy of Four Nine-Axis MEMS Motion Sensors. In Proceedings of the 2017 5th International Conference on Enterprise Systems (ES), Beijing, China, 22–24 September 2017; pp. 185–189. [Google Scholar]
- Yoon, S.D.; Lee, C.H.; Lee, J.; Choi, J.Y.; Min, W.K. Occipitocervical inclination: New radiographic parameter of neutral occipitocervical position. Eur. Spine J. 2017, 26, 2297–2302. [Google Scholar] [CrossRef] [PubMed]
- Horng, M.-H.; Kuok, C.-P.; Fu, M.-J.; Lin, C.-J.; Sun, Y.-N. Cobb angle measurement of spine from X-ray images using convolutional neural network. Comput. Math. Methods Med. 2019, 2019, 6357171. [Google Scholar] [CrossRef] [PubMed]
- Brennan, A.; Zhang, J.; Deluzio, K.; Li, Q. Quantification of inertial sensor-based 3D joint angle measurement accuracy using an instrumented gimbal. Gait Posture 2011, 34, 320–323. [Google Scholar] [CrossRef] [PubMed]
- Keown, G.A.; Tuchin, P.A. Workplace factors associated with neck pain experienced by computer users: A systematic review. J. Manip. Physiol. Ther. 2018, 41, 508–529. [Google Scholar] [CrossRef]
- Balasubramanian, V.; Jagannath, M.; Adalarasu, K. Muscle fatigue based evaluation of bicycle design. Appl. Ergon. 2014, 45, 339–345. [Google Scholar] [CrossRef]
- Choi, K.H.; Cho, M.U.; Park, C.W.; Kim, S.Y.; Kim, M.J.; Hong, B.; Kong, Y.K. A Comparison Study of Posture and Fatigue of Neck According to Monitor Types (Moving and Fixed Monitor) by Using Flexion Relaxation Phenomenon (FRP) and Craniovertebral Angle (CVA). Int. J. Environ. Res. Public Health 2020, 17, 6345. [Google Scholar] [CrossRef]
- Patwardhan, A.G.; Havey, R.M.; Khayatzadeh, S.; Muriuki, M.G.; Voronov, L.I.; Carandang, G.; Nguyen, N.L.; Ghanayem, A.J.; Schuit, D.; Patel, A.A.; et al. Postural Consequences of Cervical Sagittal Imbalance: A Novel Laboratory Model. Spine 2015, 40, 783–792. [Google Scholar] [CrossRef] [PubMed]
- Hansraj, K.K. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg. Technol. Int. 2014, 25, 277–279. [Google Scholar] [PubMed]

| Grade | Pain Scale Criteria |
|---|---|
| 0 | No pain |
| 1 | Very minor, barely felt |
| 2 | Minor pain not interfering with the work routine |
| 3 | Moderate pain |
| 4 | Continuous pain affecting routine cycling |
| 5 | Unbearable/severe pain |
| Sagittal (°) | Transverse (°) | Frontal (°) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 30 | 60 | 90 | 30 | 60 | 90 | 30 | 60 | 90 | |
| Average | 29.93 | 59.92 | 89.88 | 30.04 | 59.96 | 89.93 | 29.29 | 59.25 | 88.54 |
| Mean error | 0.09 | 0.05 | 0.81 | ||||||
| ICC * | 95% CI * | p-Value | |
|---|---|---|---|
| C0 | 0.993 | 0.987, 0.996 | <0.001 |
| C7 | 0.876 | 0.804, 0.923 | <0.001 |
| Factor | Static | Dynamic | p-Value | ||
|---|---|---|---|---|---|
| Mean ± SD | Median [Min, Max] | Mean ± SD | Median [Min, Max] | ||
| RBG | 0.63 ± 0.92 | 0 [0, 2] | 0.5 ± 0.53 | 0.5 [0, 1] | 0.705 |
| C0, ° | −9.14 ± 7.11 | −9.17 [−19.77, 0.26] | −8.23 ± 4.12 | −9.16 [−12.94, −2.09] | 0.889 |
| C7, ° | −26.94 ± 6.62 | −26.85 [−36.73, −16.53] | −28.01 ± 6.83 | −26.62 [−39.82, −17.51] | 0.575 |
| L1, ° | 3.52 ± 11.91 | −0.78 [−8.24, 28.35] | 1.54 ± 7.97 | −1.18 [−4.32, 19.4] | 0.674 |
| S1, ° | −24.59 ± 18.35 | −28.13 [−56.53, 5.7] | −22.72 ± 10.02 | −23.7 [−39.57, −5.72] | 0.484 |
| C-Cobb, ° | 17.81 ± 6.76 | 17.5 [9.6, 29.92] | 19.31 ± 7.61 | 21.25 [6.83, 31.37] | 0.575 |
| T-Cobb, ° | −30.11 ± 9.36 | −30.85 [−41.22, −18.01] | −29.59 ± 11.21 | −28.77 [−50.68, −13.42] | 0.779 |
| L-Cobb, ° | 27.81 ± 11.2 | 24.15 [18.27, 51.53] | 24.33 ± 12.03 | 23.85 [9.21, 43.86] | 0.889 |
| Monitor setting | |||||
| Eye-level, cm | 48.19 ± 3.81 | 48.55 [41.6, 53.6] | 47.38 ± 3.78 | 46.70 [40.3, 54.0] | 0.294 |
| Distance, cm | 56.04 ± 5.41 | 56.65 [48.4, 64.0] | 54.13 ± 6.08 | 55.55 [42.9, 63.2] | 0.290 |
| Height, cm | 37.65 ± 1.68 | 37.55 [35.4, 40.8] | 37.86 ± 3.80 | 38.45 [29.0, 44.6] | 0.186 |
| Tilt, ° | 0.30 ± 1.43 | 0.24 [−2.12, 2.50] | 0.32 ± 3.58 | 0.65 [−7.80, 6.42] | 0.943 |
| Factor | Estimate | 95% CI * | p-Value | |
|---|---|---|---|---|
| C0, ° | 0.0329 | 0.0044 | 0.0613 | 0.024 |
| C7, ° | ||||
| static | −0.0076 | −0.0435 | 0.0283 | 0.674 |
| dynamic | −0.0498 | −0.0802 | −0.0194 | 0.002 |
| L1, ° | −0.013 | −0.0328 | 0.0069 | 0.197 |
| S1, ° | 0.0059 | −0.0069 | 0.0188 | 0.359 |
| C-Cobb, ° | 0.0345 | 0.0124 | 0.0566 | 0.003 |
| T-Cobb, ° | −0.0024 | −0.0244 | 0.0196 | 0.829 |
| L-Cobb, ° | −0.0103 | −0.023 | 0.0025 | 0.114 |
| ΔC0, ° | −0.02914 | −0.0669 | 0.00863 | 0.128 |
| ΔC7, ° | −0.01038 | −0.0416 | 0.02078 | 0.508 |
| ΔL1, ° | −0.01035 | −0.0263 | 0.00555 | 0.198 |
| ΔS1, ° | ||||
| static | 0.002103 | −0.0258 | 0.02999 | 0.881 |
| dynamic | −0.08655 | −0.1361 | −0.037 | 0.001 |
| ΔC-Cobb, ° | −0.011 | −0.0449 | 0.02291 | 0.520 |
| ΔT-Cobb, ° | 0.01523 | −0.0126 | 0.04304 | 0.278 |
| ΔL-Cobb, ° | −0.00103 | −0.0207 | 0.0186 | 0.917 |
| Monitor height, cm | −0.0063 | −0.0938 | 0.0811 | 0.885 |
| Monitor tilt, ° | 0.0018 | −0.0711 | 0.0746 | 0.961 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.; Won, Y.I.; Kang, S.; Choi, Y.; Park, J.H.; Lee, J.; Kim, I.Y.; Chung, C.K. Comparison of Neck Pain and Posture with Spine Angle Tracking System between Static and Dynamic Computer Monitor Use. Electronics 2024, 13, 1363. https://doi.org/10.3390/electronics13071363
Kim H, Won YI, Kang S, Choi Y, Park JH, Lee J, Kim IY, Chung CK. Comparison of Neck Pain and Posture with Spine Angle Tracking System between Static and Dynamic Computer Monitor Use. Electronics. 2024; 13(7):1363. https://doi.org/10.3390/electronics13071363
Chicago/Turabian StyleKim, Hayoung, Young Il Won, Soohee Kang, Yunhee Choi, Jin Ho Park, Jongshill Lee, In Young Kim, and Chun Kee Chung. 2024. "Comparison of Neck Pain and Posture with Spine Angle Tracking System between Static and Dynamic Computer Monitor Use" Electronics 13, no. 7: 1363. https://doi.org/10.3390/electronics13071363
APA StyleKim, H., Won, Y. I., Kang, S., Choi, Y., Park, J. H., Lee, J., Kim, I. Y., & Chung, C. K. (2024). Comparison of Neck Pain and Posture with Spine Angle Tracking System between Static and Dynamic Computer Monitor Use. Electronics, 13(7), 1363. https://doi.org/10.3390/electronics13071363









