Molnupiravir: A Versatile Prodrug against SARS-CoV-2 Variants
Abstract
1. Introduction
2. Mechanism of Action of Molnupiravir
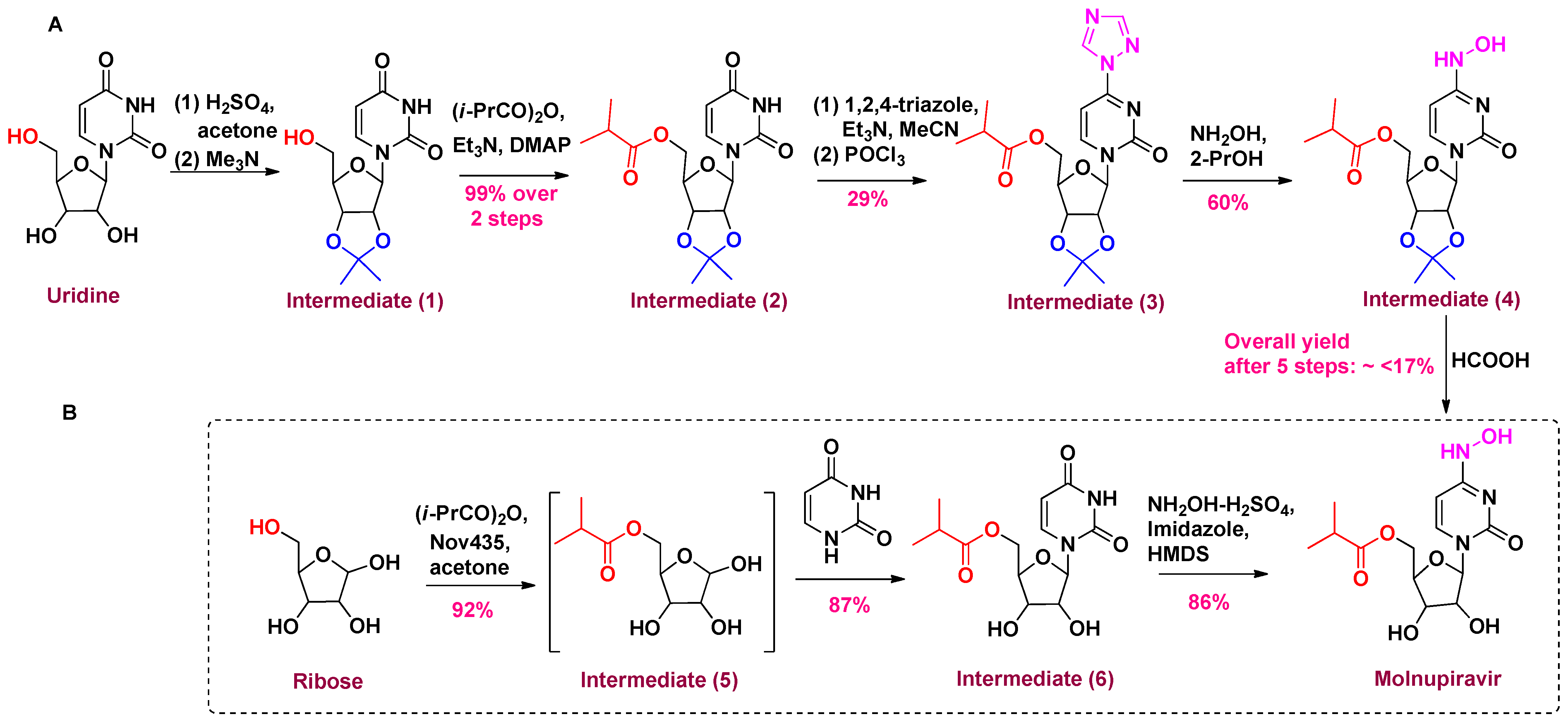
3. Chemistry of Molnupiravir
4. Molecular Docking Study
5. Impact of Molnupiravir on SARS-CoV-2 Variants
5.1. Preclinical Studies of Molnupiravir
5.2. Clinical Studies of Molnupiravir
6. Pharmacovigilance Profile of Molnupiravir
6.1. Adverse Effects of Molnupiravir
6.2. Cases of Molnupiravir in Patients with Comorbidity
6.3. Study of Molnupiravir in Vaccinated and Unvaccinated Patients
6.4. Pharmacokinetic Studies of Molnupiravir
6.5. WHO Indications for Molnupiravir
7. Conclusions and Future Perspectives
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Chavda, V.P.; Vora, L.K.; Gajjar, N.; Apostolopoulos, V.; Shah, N.; Chen, Z.S. 2-Deoxy-D-Glucose and Its Derivatives for the COVID-19 Treatment: An Update. Front. Pharmacol. 2022, 13, 899633. [Google Scholar] [CrossRef] [PubMed]
- Chavda, V.P.; Vora, L.K.; Apostolopoulos, V. Inhalable Vaccines: Can They Help Control Pandemics? Vaccines 2022, 10, 1309. [Google Scholar] [CrossRef] [PubMed]
- Chavda, V.P.; Soni, S.; Vora, L.K.; Soni, S.; Khadela, A.; Ajabiya, J. MRNA-Based Vaccines and Therapeutics for COVID-19 and Future Pandemics. Vaccines 2022, 10, 2150. [Google Scholar] [CrossRef] [PubMed]
- Chavda, V.P.; Balar, P.; Vaghela, D.; Solanki, H.K.; Vaishnav, A.; Hala, V.; Vora, L. Omicron Variant of SARS-CoV-2: An Indian Perspective of Vaccination and Management. Vaccines 2023, 11, 160. [Google Scholar] [CrossRef] [PubMed]
- Chavda, V.P.; Patel, A.B.; Pandya, A.; Vora, L.K.; Patravale, V.; Tambuwala, Z.M.; Aljabali, A.A.; Serrano-Aroca, Á.; Mishra, V.; Tambuwala, M.M. Co-Infection Associated with SARS-CoV-2 and Their Management. Future Sci. OA 2022, 8, FSO819. [Google Scholar] [CrossRef] [PubMed]
- Bezbaruah, R.; Chavda, V.P.; Nongrang, L.; Alom, S.; Deka, K.; Kalita, T.; Ali, F.; Bhattacharjee, B.; Vora, L. Nanoparticle-Based Delivery Systems for Vaccines. Vaccines 2022, 10, 1946. [Google Scholar] [CrossRef] [PubMed]
- Chavda, V.P.; Yao, Q.; Vora, L.K.; Apostolopoulos, V.; Patel, C.A.; Bezbaruah, R.; Patel, A.B.; Chen, Z.-S. Fast-Track Development of Vaccines for SARS-CoV-2: The Shots That Saved the World. Front. Immunol. 2022, 13, 961198. [Google Scholar] [CrossRef]
- WHO. Coronavirus (COVID-19) Dashboard. Available online: https://Covid19.Who.Int/ (accessed on 28 November 2022).
- Bian, L.; Gao, F.; Zhang, J.; He, Q.; Mao, Q.; Xu, M.; Liang, Z. Effects of SARS-CoV-2 Variants on Vaccine Efficacy and Response Strategies. Expert Rev. Vaccines 2021, 20, 365–373. [Google Scholar] [CrossRef]
- Maurya, R.; Mishra, P.; Swaminathan, A.; Ravi, V.; Saifi, S.; Kanakan, A.; Mehta, P.; Devi, P.; Praveen, S.; Budhiraja, S.; et al. SARS-CoV-2 Mutations and COVID-19 Clinical Outcome: Mutation Global Frequency Dynamics and Structural Modulation Hold the Key. Front. Cell. Infect. Microbiol. 2022, 12, 868414. [Google Scholar] [CrossRef]
- Akkiz, H. Implications of the Novel Mutations in the SARS-CoV-2 Genome for Transmission, Disease Severity and the Vaccine Development. J. Transl. Sci. 2021, 7, 636532. [Google Scholar] [CrossRef]
- Chavda, V.P.; Patel, A.B.; Vaghasiya, D.D. SARS-CoV-2 Variants and Vulnerability at the Global Level. J. Med. Virol. 2022, 94, 2986–3005. [Google Scholar] [CrossRef] [PubMed]
- Chavda, V.P.; Vuppu, S.; Mishra, T.; Kamaraj, S.; Patel, A.B.; Sharma, N.; Chen, Z.-S. Recent Review of COVID-19 Management: Diagnosis, Treatment and Vaccination. Pharmacol. Rep. 2022, 74, 1120–1148. [Google Scholar] [CrossRef] [PubMed]
- Scovino, A.M.; Dahab, E.C.; Vieira, G.F.; Freire-de-Lima, L.; Freire-de-Lima, C.G.; Morrot, A. SARS-CoV-2’s Variants of Concern: A Brief Characterization. Front. Immunol. 2022, 13, 834098. [Google Scholar] [CrossRef]
- Hirabara, S.M.; Serdan, T.D.A.; Gorjao, R.; Masi, L.N.; Pithon-Curi, T.C.; Covas, D.T.; Curi, R.; Durigon, E.L. SARS-CoV-2 Variants: Differences and Potential of Immune Evasion. Front. Cell. Infect. Microbiol. 2022, 11, 781429. [Google Scholar] [CrossRef]
- Aleem, A.; Akbar Samad, A.B.; Slenker, A.K. Emerging Variants of SARS-CoV-2 and Novel Therapeutics against Coronavirus (COVID-19); Bookshelf ID: NBK570580; StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Chavda, V.P.; Apostolopoulos, V. Omicron Variant (B.1.1.529) of SARS-CoV-2: Threat for the Elderly? Maturitas 2022, 158, 78–81. [Google Scholar] [CrossRef]
- Harvey, W.T.; Carabelli, A.M.; Jackson, B.; Gupta, R.K.; Thomson, E.C.; Harrison, E.M.; Ludden, C.; Reeve, R.; Rambaut, A.; Peacock, S.J.; et al. SARS-CoV-2 Variants, Spike Mutations and Immune Escape. Nat. Rev. Microbiol. 2021, 19, 409–424. [Google Scholar] [CrossRef]
- Sanyaolu, A.; Okorie, C.; Marinkovic, A.; Haider, N.; Abbasi, A.F.; Jaferi, U.; Prakash, S.; Balendra, V. The Emerging SARS-CoV-2 Variants of Concern. Ther. Adv. Infect. Dis. 2021, 8, 20499361211024372. [Google Scholar] [CrossRef]
- Ison, M.G.; Wolfe, C.; Boucher, H.W. Emergency Use Authorization of Remdesivir. JAMA 2020, 323, 2365–2366. [Google Scholar] [CrossRef]
- Teli, D.M.; Patel, B.; Chhabria, M.T. Fragment-Based Design of SARS-CoV-2 Mpro Inhibitors. Struct. Chem. 2022, 33, 2155–2168. [Google Scholar] [CrossRef]
- COVID-19 Vaccines with WHO Emergency Use Listing. Available online: Https://Extranet.Who.Int/Pqweb/Vaccines/Vaccinescovid-19-Vaccine-Eul-Issued (accessed on 28 November 2022).
- Chavda, V.P.; Vihol, D.R.; Solanki, H.K.; Apostolopoulos, V. The Vaccine World of COVID-19: India’s Contribution. Vaccines 2022, 10, 1943. [Google Scholar] [CrossRef] [PubMed]
- Chavda, V.P.; Chen, Y.; Dave, J.; Chen, Z.-S.; Chauhan, S.C.; Yallapu, M.M.; Uversky, V.N.; Bezbaruah, R.; Patel, S.; Apostolopoulos, V. COVID-19 and Vaccination: Myths Vs Science. Expert Rev. Vaccines 2022, 21, 1603–1620. [Google Scholar] [CrossRef] [PubMed]
- Jornada, D.H.; Dos Santos Fernandes, G.F.; Chiba, D.E.; De Melo, T.R.F.; Dos Santos, J.L.; Chung, M.C. The Prodrug Approach: A Successful Tool for Improving Drug Solubility. Molecules 2016, 21, 42. [Google Scholar] [CrossRef] [PubMed]
- Markovic, M.; Ben-Shabat, S.; Dahan, A. Prodrugs for Improved Drug Delivery: Lessons Learned from Recently Developed and Marketed Products. Pharmaceutics 2020, 12, 1031. [Google Scholar] [CrossRef]
- Mahato, R.; Tai, W.; Cheng, K. Prodrugs for Improving Tumor Targetability and Efficiency. Adv. Drug Deliv. Rev. 2011, 63, 659–670. [Google Scholar] [CrossRef]
- Sanches, B.M.A.; Ferreira, E.I. Is Prodrug Design an Approach to Increase Water Solubility? Int. J. Pharm. 2019, 568, 118498. [Google Scholar] [CrossRef]
- Müller, C.E. Prodrug Approaches for Enhancing the Bioavailability of Drugs with Low Solubility. Chem. Biodivers. 2009, 6, 2071–2083. [Google Scholar] [CrossRef]
- Najjar, A.; Karaman, R. The Prodrug Approach in the Era of Drug Design. Expert Opin. Drug Deliv. 2019, 16, 1–5. [Google Scholar] [CrossRef]
- Zhang, X.Y.; Elfarra, A.A. Toxicity Mechanism-Based Prodrugs: Glutathione-Dependent Bioactivation as a Strategy for Anticancer Prodrug Design. Expert Opin. Drug Discov. 2018, 13, 815–824. [Google Scholar] [CrossRef]
- Mihiretie, M.; Tebelay, D.; Tengchuan, J. Structural Basis of Potential Inhibitors Targeting SARS-CoV-2 Main Protease. Front. Chem. 2021, 9, 622898. [Google Scholar] [CrossRef]
- Kumari, M.; Lu, R.M.; Li, M.C.; Huang, J.L.; Hsu, F.F.; Ko, S.H.; Ke, F.Y.; Su, S.C.; Liang, K.H.; Yuan, J.P.Y.; et al. A Critical Overview of Current Progress for COVID-19: Development of Vaccines, Antiviral Drugs, and Therapeutic Antibodies. J. Biomed. Sci. 2022, 29, 68. [Google Scholar] [CrossRef]
- Wu, C.R.; Yin, W.C.; Jiang, Y.; Xu, H.E. Structure Genomics of SARS-CoV-2 and Its Omicron Variant: Drug Design Templates for COVID-19. Acta Pharmacol. Sin. 2022, 43, 3021–3033. [Google Scholar] [CrossRef] [PubMed]
- FDA. FDA Approves First Treatment for COVID-19. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-covid-19 (accessed on 26 November 2022).
- Spinner, C.D.; Gottlieb, R.L.; Criner, G.J.; Arribas López, J.R.; Cattelan, A.M.; Soriano Viladomiu, A.; Ogbuagu, O.; Malhotra, P.; Mullane, K.M.; Castagna, A.; et al. Effect of Remdesivir vs Standard Care on Clinical Status at 11 Days in Patients With Moderate COVID-19: A Randomized Clinical Trial. JAMA 2020, 324, 1048. [Google Scholar] [CrossRef] [PubMed]
- Beigel, J.H.; Tomashek, K.M.; Dodd, L.E.; Mehta, A.K.; Zingman, B.S.; Kalil, A.C.; Hohmann, E.; Chu, H.Y.; Luetkemeyer, A.; Kline, S.; et al. Remdesivir for the Treatment of COVID-19—Final Report. N. Engl. J. Med. 2020, 383, 1813–1826. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, D.; Du, G.; Du, R.; Zhao, J.; Jin, Y.; Fu, S.; Gao, L.; Cheng, Z.; Lu, Q.; et al. Remdesivir in Adults with Severe COVID-19: A Randomised, Double-Blind, Placebo-Controlled, Multicentre Trial. Lancet 2020, 395, 1569–1578. [Google Scholar] [CrossRef] [PubMed]
- Larkin, H.D. Paxlovid Drug Interaction Screening Checklist Updated. JAMA 2022, 328, 1290. [Google Scholar] [CrossRef] [PubMed]
- Fischer, W.A.; Eron, J.J.; Holman, W.; Cohen, M.S.; Fang, L.; Szewczyk, L.J.; Sheahan, T.P.; Baric, R.; Mollan, K.R.; Wolfe, C.R.; et al. A Phase 2a Clinical Trial of Molnupiravir in Patients with COVID-19 Shows Accelerated SARS-CoV-2 RNA Clearance and Elimination of Infectious Virus. Sci. Transl. Med. 2022, 14, eabl7430. [Google Scholar] [CrossRef]
- Li, G.; Jing, X.; Zhang, P.; De Clercq, E. Antiviral Classification. In Encyclopedia of Virology; Elsevier: Amsterdam, The Netherlands, 2021; pp. 121–130. ISBN 978-0-12-814516-6. [Google Scholar]
- Kausar, S.; Said Khan, F.; Ishaq Mujeeb Ur Rehman, M.; Akram, M.; Riaz, M.; Rasool, G.; Hamid Khan, A.; Saleem, I.; Shamim, S.; Malik, A. A Review: Mechanism of Action of Antiviral Drugs. Int. J. Immunopathol. Pharmacol. 2021, 35, 205873842110026. [Google Scholar] [CrossRef]
- Coronavirus (COVID-19)|Drugs. Available online: https://www.fda.gov/drugs/emergency-preparedness-drugs/coronavirus-covid-19-drugs (accessed on 4 January 2023).
- Chaijamorn, W.; Rungkitwattanakul, D.; Nuchtavorn, N.; Charoensareerat, T.; Pattharachayakul, S.; Sirikun, W.; Srisawat, N. Antiviral Dosing Modification for Coronavirus Disease 2019–Infected Patients Receiving Extracorporeal Therapy. Crit. Care Explor. 2020, 2, e0242. [Google Scholar] [CrossRef]
- Durbin, R.P. Letter: Acid Secretion by Gastric Mucous Membrane. Am. J. Physiol. 1975, 229, 1726. [Google Scholar] [CrossRef]
- Liverpool COVID-19 Interactions. Available online: https://www.covid19-druginteractions.org/home (accessed on 4 January 2023).
- Liu, D.; Zeng, X.; Ding, Z.; Lv, F.; Mehta, J.L.; Wang, X. Adverse Cardiovascular Effects of Anti-COVID-19 Drugs. Front. Pharmacol. 2021, 12, 699949. [Google Scholar] [CrossRef] [PubMed]
- Corritori, S.; Savchuk, N.; Pauza, C.D. Risk/Benefit Profiles of Currently Approved Oral Antivirals for Treatment of COVID-19: Similarities and Differences. COVID 2022, 2, 1057–1076. [Google Scholar] [CrossRef]
- Favipiravir Terminated Phase 3 Trials for Coronavirus Disease 2019 (COVID-19) Treatment|DrugBank Online. Available online: https://go.drugbank.com/drugs/DB12466/clinical_trials?conditions=DBCOND0129755&phase=3&purpose=treatment&status=terminated (accessed on 4 January 2023).
- Pourkarim, F.; Pourtaghi-Anvarian, S.; Rezaee, H. Molnupiravir: A New Candidate for COVID-19 Treatment. Pharmacol. Res. Perspect. 2022, 10, e00909. [Google Scholar] [CrossRef] [PubMed]
- Malone, B.; Campbell, E.A. Molnupiravir: Coding for Catastrophe. Nat. Struct. Mol. Biol. 2021, 28, 706–708. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.C.; Hsieh, C.C.; Ko, W.C. Molnupiravir—A Novel Oral Anti-SARS-CoV-2 Agent. Antibiotics 2021, 10, 1294. [Google Scholar] [CrossRef] [PubMed]
- Yip, A.J.W.; Low, Z.Y.; Chow, V.T.K.; Lal, S.K. Repurposing Molnupiravir for COVID-19: The Mechanisms of Antiviral Activity. Viruses 2022, 14, 1345. [Google Scholar] [CrossRef] [PubMed]
- Kayali, F.; Leung, M.S.T.; Wong, W.; Morgan, K.P.; Harky, A. What Impact Can Molnupiravir Have on the Treatment of SARS-CoV-2 Infection? Expert Opin. Pharmacother. 2022, 23, 865–868. [Google Scholar] [CrossRef]
- Zhou, S.; Hill, C.S.; Sarkar, S.; Tse, L.V.; Woodburn, B.M.D.; Schinazi, R.F.; Sheahan, T.P.; Baric, R.S.; Heise, M.T.; Swanstrom, R. β-d-N4-Hydroxycytidine Inhibits SARS-CoV-2 through Lethal Mutagenesis but Is Also Mutagenic to Mammalian Cells. J. Infect. Dis. 2021, 224, 415–419. [Google Scholar] [CrossRef]
- Toots, M.; Yoon, J.J.; Hart, M.; Natchus, M.G.; Painter, G.R.; Plemper, R.K. Quantitative Efficacy Paradigms of the Influenza Clinical Drug Candidate EIDD-2801 in the Ferret Model. Transl. Res. 2020, 218, 16–28. [Google Scholar] [CrossRef]
- Painter, G.R.; Bowen, R.A.; Bluemling, G.R.; DeBergh, J.; Edpuganti, V.; Gruddanti, P.R.; Guthrie, D.B.; Hager, M.; Kuiper, D.L.; Lockwood, M.A.; et al. The Prophylactic and Therapeutic Activity of a Broadly Active Ribonucleoside Analog in a Murine Model of Intranasal Venezuelan Equine Encephalitis Virus Infection. Antivir. Res. 2019, 171, 104597. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, L. Broad-Spectrum Prodrugs with Anti-SARS-CoV-2 Activities: Strategies, Benefits, and Challenges. J. Med. Virol. 2022, 94, 1373–1390. [Google Scholar] [CrossRef]
- Zarenezhad, E.; Marzi, M. Review on Molnupiravir as a Promising Oral Drug for the Treatment of COVID-19. Med. Chem. Res. 2022, 31, 232–243. [Google Scholar] [CrossRef] [PubMed]
- Parra-Lucares, A.; Segura, P.; Rojas, V.; Pumarino, C.; Saint-Pierre, G.; Toro, L. Emergence of SARS-CoV-2 Variants in the World: How Could This Happen? Life 2022, 12, 194. [Google Scholar] [CrossRef] [PubMed]
- Clancy, S. Chemical Structure of RNA. Nat. Educ. 2008, 7, 60. [Google Scholar]
- Menéndez-Arias, L. Decoding Molnupiravir-Induced Mutagenesis in SARS-CoV-2. J. Biol. Chem. 2021, 297, 100867. [Google Scholar] [CrossRef] [PubMed]
- Sheahan, T.P.; Sims, A.C.; Zhou, S.; Graham, R.L.; Pruijssers, A.J.; Agostini, M.L.; Leist, S.R.; Schafer, A.; Dinnon, K.H.; Stevens, L.J.; et al. An Orally Bioavailable Broad-Spectrum Antiviral Inhibits SARS-CoV-2 in Human Airway Epithelial Cell Cultures and Multiple Coronaviruses in Mice. Sci. Transl. Med. 2020, 12, eabb5883. [Google Scholar] [CrossRef] [PubMed]
- Agostini, M.L.; Pruijssers, A.J.; Chappell, J.D.; Gribble, J.; Lu, X.; Andres, E.L.; Bluemling, G.R.; Lockwood, M.A.; Sheahan, T.P.; Sims, A.C.; et al. Small-Molecule Antiviral β-d-N4-Hydroxycytidine Inhibits a Proofreading-Intact Coronavirus with a High Genetic Barrier to Resistance. J. Virol. 2019, 93, e01348-19. [Google Scholar] [CrossRef]
- Gordon, C.J.; Tchesnokov, E.P.; Schinazi, R.F.; Götte, M. Molnupiravir Promotes SARS-CoV-2 Mutagenesis via the RNA Template. J. Biol. Chem. 2021, 297, 100770. [Google Scholar] [CrossRef]
- Painter, G.R.; Bluemling, G.R.; Natchus, M.G.; Guthrie, D. N4-hydroxycytidine and Derivatives and Anti-viral Uses Related Thereto. WO Patent 20191134622018, 12 June 2019. [Google Scholar]
- Steiner, A.; Znidar, D.; Ötvös, S.B.; Snead, D.R.; Dallinger, D.; Kappe, C.O. A High-Yielding Synthesis of EIDD-2801 from Uridine. Eur. J. Org. Chem. 2020, 2020, 6736–6739. [Google Scholar] [CrossRef]
- Vasudevan, N.; Ahlqvist, G.P.; McGeough, C.P.; Paymode, D.J.; Cardoso, F.S.P.; Lucas, T.; Dietz, J.P.; Opatz, T.; Jamison, T.F.; Gupton, F.B.; et al. A Concise Route to MK-4482 (EIDD-2801) from Cytidine. Chem. Commun. 2020, 56, 13363–13364. [Google Scholar] [CrossRef]
- Paymode, D.J.; Vasudevan, N.; Ahmad, S.; Kadam, A.L.; Cardoso, F.S.P.; Burns, J.M.; Cook, D.W.; Stringham, R.W.; Snead, D.R. Toward a Practical, Two-Step Process for Molnupiravir: Direct Hydroxamination of Cytidine Followed by Selective Esterification. Org. Process Res. Dev. 2021, 25, 1822–1830. [Google Scholar] [CrossRef]
- Ahlqvist, G.P.; McGeough, C.P.; Senanayake, C.; Armstrong, J.D.; Yadaw, A.; Roy, S.; Ahmad, S.; Snead, D.R.; Jamison, T.F. Progress Toward a Large-Scale Synthesis of Molnupiravir (MK-4482, EIDD-2801) from Cytidine. ACS Omega 2021, 6, 10396–10402. [Google Scholar] [CrossRef]
- Benkovics, T.; McIntosh, J.A.; Silverman, S.M.; Kong, J.; Maligres, P.; Itoh, T.; Yang, H.; Huffman, M.A.; Verma, D.; Pan, W.; et al. Evolving to an Ideal Synthesis of Molnupiravir, an Investigational Treatment for COVID-19. ChemRxiv 2020. [CrossRef]
- Yin, W.; Mao, C.; Luan, X.; Shen, D.D.; Shen, Q.; Su, H.; Wang, X.; Zhou, F.; Zhao, W.; Gao, M.; et al. Structural Basis for Inhibition of the RNA-Dependent RNA Polymerase from SARS-CoV-2 by Remdesivir. Science 2020, 368, 1499–1504. [Google Scholar] [CrossRef] [PubMed]
- Sharov, A.; Burkhanova, T.; Taskın Tok, T.; Babashkina, M.; Safin, D. Computational Analysis of Molnupiravir. Int. J. Mol. Sci. 2022, 23, 1508. [Google Scholar] [CrossRef]
- Celik, I.; Tallei, T.E. A Computational Comparative Analysis of the Binding Mechanism of Molnupiravir’s Active Metabolite to RNA-dependent RNA Polymerase of Wild-type and Delta Subvariant AY.4 of SARS-CoV-2. J. Cell. Biochem. 2022, 123, 807–818. [Google Scholar] [CrossRef]
- Vangeel, L.; Chiu, W.; De Jonghe, S.; Maes, P.; Slechten, B.; Raymenants, J.; André, E.; Leyssen, P.; Neyts, J.; Jochmans, D. Remdesivir, Molnupiravir and Nirmatrelvir Remain Active against SARS-CoV-2 Omicron and Other Variants of Concern. Antivir. Res. 2022, 198, 105252. [Google Scholar] [CrossRef]
- Wahl, A.; Gralinski, L.E.; Johnson, C.E.; Yao, W.; Kovarova, M.; Dinnon, K.H.; Liu, H.; Madden, V.J.; Krzystek, H.M.; De, C.; et al. SARS-CoV-2 Infection Is Effectively Treated and Prevented by EIDD-2801. Nature 2021, 591, 451–457. [Google Scholar] [CrossRef]
- Lieber, C.M.; Cox, R.M.; Sourimant, J.; Wolf, J.D.; Juergens, K.; Phung, Q.; Saindane, M.T.; Smith, M.K.; Sticher, Z.M.; Kalykhalov, A.A.; et al. SARS-CoV-2 VOC Type and Biological Sex Affect Molnupiravir Efficacy in Severe COVID-19 Dwarf Hamster Model. Nat. Commun. 2022, 13, 4416. [Google Scholar] [CrossRef]
- Rosenke, K.; Lewis, M.; Feldmann, F.; Feldmann, H. Combined Molnupiravir and Nirmatrelvir Treatment Improves the Inhibitory Effect on SARS-CoV-2 in Rhesus Macaques. bioRxiv 2022. [Google Scholar] [CrossRef]
- Jeong, J.H.; Chokkakula, S.; Min, S.C.; Kim, B.K.; Choi, W.-S.; Oh, S.; Yun, Y.S.; Kang, D.H.; Lee, O.-J.; Kim, E.-G.; et al. Combination Therapy with Nirmatrelvir and Molnupiravir Improves the Survival of SARS-CoV-2 Infected Mice. Antiviral Res. 2022, 208, 105430. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Singh, A.; Singh, R.; Misra, A. Molnupiravir in COVID-19: A Systematic Review of Literature. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 102329. [Google Scholar] [CrossRef] [PubMed]
- Painter, W.P.; Holman, W.; Bush, J.A.; Almazedi, F.; Malik, H.; Eraut, N.C.J.E.; Morin, M.J.; Szewczyk, L.J.; Painter, G.R. Human Safety, Tolerability, and Pharmacokinetics of Molnupiravir, a Novel Broad-Spectrum Oral Antiviral Agent with Activity against SARS-CoV-2. Antimicrob. Agents Chemother. 2021, 65, e02428-20. [Google Scholar] [CrossRef] [PubMed]
- Arribas, J.R.; Bhagani, S.; Lobo, S.M.; Khaertynova, I.; Mateu, L.; Fishchuk, R.; Park, W.Y.; Hussein, K.; Kim, S.W.; Ghosn, J.; et al. Randomized Trial of Molnupiravir or Placebo in Patients Hospitalized with COVID-19. NEJM Evid. 2022, 1, EVIDoa2100044. [Google Scholar] [CrossRef]
- Amani, B.; Zareei, S.; Amani, B. Rapid Review and Meta-Analysis of Adverse Events Associated with Molnupiravir in Patients with COVID-19. Br. J. Clin. Pharmacol. 2022, 88, 4403–4411. [Google Scholar] [CrossRef]
- Wong, C.K.H.; Au, I.C.H.; Lau, K.T.K.; Lau, E.H.Y.; Cowling, B.J.; Leung, G.M. Real-World Effectiveness of Early Molnupiravir or Nirmatrelvir–Ritonavir in Hospitalised Patients with COVID-19 without Supplemental Oxygen Requirement on Admission during Hong Kong’s Omicron BA.2 Wave: A Retrospective Cohort Study. Lancet Infect. Dis. 2022, 22, 1681–1693. [Google Scholar] [CrossRef]
- Zou, R.; Peng, L.; Shu, D.; Zhao, L.; Lan, J.; Tan, G.; Peng, J.; Yang, X.; Liu, M.; Zhang, C.; et al. Antiviral Efficacy and Safety of Molnupiravir Against Omicron Variant Infection: A Randomized Controlled Clinical Trial. Front. Pharmacol. 2022, 13, 939573. [Google Scholar] [CrossRef]
- Tiseo, G.; Barbieri, C.; Galfo, V.; Occhineri, S.; Matucci, T.; Almerigogna, F.; Kalo, J.; Sponga, P.; Cesaretti, M.; Marchetti, G.; et al. Efficacy and Safety of Nirmatrelvir/Ritonavir, Molnupiravir, and Remdesivir in a Real-World Cohort of Outpatients with COVID-19 at High Risk of Progression: The PISA Outpatient Clinic Experience. Infect. Dis. Ther. 2022, 12, 257–271. [Google Scholar] [CrossRef]
- Streinu-Cercel, A.; Miron, V.D.; Oană, A.A.; Irimia, M.; Popescu, R.Ș.; Dărămuș, I.A.; Moțoi, M.M.; Ceapraga, G.J.; Săndulescu, O. Real-World Use of Molnupiravir in the Treatment of Outpatients with SARS-CoV-2 Infection—A Patient Profile Based on the Experience of a Tertiary Infectious Disease Center. Pharmaceuticals 2022, 15, 1065. [Google Scholar] [CrossRef]
- Wong, C.K.H.; Au, I.C.H.; Lau, K.T.K.; Lau, E.H.Y.; Cowling, B.J.; Leung, G.M. Real-World Effectiveness of Molnupiravir and Nirmatrelvir plus Ritonavir against Mortality, Hospitalisation, and in-Hospital Outcomes among Community-Dwelling, Ambulatory Patients with Confirmed SARS-CoV-2 Infection during the Omicron Wave in Hong Kong: An Observational Study. Lancet 2022, 400, 1213–1222. [Google Scholar] [CrossRef]
- Kannan, S.R.; Spratt, A.N.; Cohen, A.R.; Naqvi, S.H.; Chand, H.S.; Quinn, T.P.; Lorson, C.L.; Byrareddy, S.N.; Singh, K. Evolutionary Analysis of the Delta and Delta Plus Variants of the SARS-CoV-2 Viruses. J. Autoimmun. 2021, 124, 102715. [Google Scholar] [CrossRef] [PubMed]
- Dhawan, M.; Saied, A.R.A.; Mitra, S.; Alhumaydhi, F.A.; Emran, T.B.; Wilairatana, P. Omicron Variant (B.1.1.529) and Its Sublineages: What Do We Know so Far amid the Emergence of Recombinant Variants of SARS-CoV-2? Biomed. Pharmacother. 2022, 154, 113522. [Google Scholar] [CrossRef] [PubMed]
- Takashita, E.; Kinoshita, N.; Yamayoshi, S.; Sakai-Tagawa, Y.; Fujisaki, S.; Ito, M.; Iwatsuki-Horimoto, K.; Chiba, S.; Halfmann, P.; Nagai, H.; et al. Efficacy of Antibodies and Antiviral Drugs against COVID-19 Omicron Variant. N. Engl. J. Med. 2022, 386, 995–998. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Karuppanan, K.; Subramaniam, G. Omicron (BA.1) and Sub-Variants (BA.1, BA.2 and BA.3) of SARS-CoV-2 Spike Infectivity and Pathogenicity: A Comparative Sequence and Structural-Based Computational Assessment. J. Med. Virol. 2022, 94, 4780–4791. [Google Scholar] [CrossRef]
- Wang, Q.; Guo, Y.; Iketani, S.; Nair, M.S.; Li, Z.; Mohri, H.; Wang, M.; Yu, J.; Bowen, A.D.; Chang, J.Y.; et al. Antibody Evasion by SARS-CoV-2 Omicron Subvariants BA.2.12.1, BA.4 and BA.5. Nature 2022, 608, 603–608. [Google Scholar] [CrossRef]
- Study Shows 3 Japan-Approved Drugs Effective against Omicron BA.5. Available online: https://english.kyodonews.net/news/2022/07/ab41d4f7ed44-study-shows-3-japan-approved-drugs-effective-against-omicron-ba5.html (accessed on 3 December 2022).
- Chakraborty, C.; Bhattacharya, M.; Sharma, A.R.; Dhama, K. Recombinant SARS-CoV-2 Variants XD, XE, and XF: The Emergence of Recombinant Variants Requires an Urgent Call for Research–Correspondence. Int. J. Surg. 2022, 102, 106670. [Google Scholar] [CrossRef]
- Whitley, R. Molnupiravir—A Step toward Orally Bioavailable Therapies for COVID-19. N. Engl. J. Med. 2022, 386, 592–593. [Google Scholar] [CrossRef]
- Tian, L.; Pang, Z.; Li, M.; Lou, F.; An, X.; Zhu, S.; Song, L.; Tong, Y.; Fan, H.; Fan, J. Molnupiravir and Its Antiviral Activity Against COVID-19. Front. Immunol. 2022, 13, 855496. [Google Scholar] [CrossRef]
- Gwadz, M.; Campos, S.; Freeman, R.; Cleland, C.M.; Wilton, L.; Sherpa, D.; Ritchie, A.S.; Hawkins, R.L.; Allen, J.Y.; Martinez, B.Y.; et al. Black and Latino Persons Living with HIV Evidence Risk and Resilience in the Context of COVID-19: A Mixed-Methods Study of the Early Phase of the Pandemic. AIDS Behav. 2021, 25, 1340–1360. [Google Scholar] [CrossRef]
- Jayk Bernal, A.; da Gomes Silva, M.M.; Musungaie, D.B.; Kovalchuk, E.; Gonzalez, A.; Delos Reyes, V.; Martín-Quirós, A.; Caraco, Y.; Williams-Diaz, A.; Brown, M.L.; et al. Molnupiravir for Oral Treatment of COVID-19 in Nonhospitalized Patients. N. Engl. J. Med. 2022, 386, 509–520. [Google Scholar] [CrossRef]
- Nakamura, K.; Fujimoto, K.; Hasegawa, C.; Aoki, I.; Yoshitsugu, H.; Ugai, H.; Yatsuzuka, N.; Tanaka, Y.; Furihata, K.; Maas, B.M.; et al. A Phase I, Randomized, Placebo-Controlled Study of Molnupiravir in Healthy Japanese to Support Special Approval in Japan to Treat COVID-19. Clin. Transl. Sci. 2022, 15, 2697–2708. [Google Scholar] [CrossRef] [PubMed]
- Merck and Ridgeback’s Molnupiravir, an Investigational Oral Antiviral COVID-19 Treatment, Receives Special Approval for Emergency in Japan-Merck.Com. Available online: https://www.merck.com/news/merck-and-ridgebacks-molnupiravir-an-investigational-oral-antiviral-covid-19-treatment-receives-special-approval-for-emergency-in-japan/ (accessed on 3 December 2022).
- Vitiello, A.; Ferrara, F.; Zovi, A.; Trama, U.; Boccellino, M. Pregnancy and COVID-19, Focus on Vaccine and Pharmacological Treatment. J. Reprod. Immunol. 2022, 151, 103630. [Google Scholar] [CrossRef] [PubMed]
- Villamarín, M.; Márquez-Algaba, E.; Esperalba, J.; Perelló, M.; Los Arcos, I.; Campany, D.; Moreso, F.; Len, O. Preliminary Clinical Experience of Molnupiravir to Prevent Progression of COVID-19 in Kidney Transplant Recipients. Transplantation 2022, 106, 2200–2204. [Google Scholar] [CrossRef]
- Czarnecka, K.; Czarnecka, P.; Tronina, O.; Durlik, M. Molnupiravir Outpatient Treatment for Adults with COVID-19 in a Real-World Setting—A Single Center Experience. J. Clin. Med. 2022, 11, 6464. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Shibata, Y.; Minemura, H.; Nikaido, T.; Tanino, Y.; Fukuhara, A.; Kanno, R.; Saito, H.; Suzuki, S.; Inokoshi, Y.; et al. Real-World Clinical Outcomes of Treatment with Molnupiravir for Patients with Mild-to-Moderate Coronavirus Disease 2019 during the Omicron Variant Pandemic. Clin. Exp. Med. 2022, 1–9. [Google Scholar] [CrossRef]
- Haddad, F.; Dokmak, G.; Karaman, R. A Comprehensive Review on the Efficacy of Several Pharmacologic Agents for the Treatment of COVID-19. Life 2022, 12, 1758. [Google Scholar] [CrossRef]
- Huang, Z.; Xu, S.; Liu, J.; Wu, L.; Qiu, J.; Wang, N.; Ren, J.; Li, Z.; Guo, X.; Tao, F.; et al. Effectiveness of Inactivated and Ad5-NCoV COVID-19 Vaccines against SARS-CoV-2 Omicron BA. 2 Variant Infection, Severe Illness, and Death. BMC Med. 2022, 20, 400. [Google Scholar] [CrossRef]
- Khoo, S.H.; FitzGerald, R.; Saunders, G.; Middleton, C.; Ahmad, S.; Edwards, C.J.; Hadjiyiannakis, D.; Walker, L.; Lyon, R.; Shaw, V.; et al. Molnupiravir versus Placebo in Unvaccinated and Vaccinated Patients with Early SARS-CoV-2 Infection in the UK (AGILE CST-2): A Randomised, Placebo-Controlled, Double-Blind, Phase 2 Trial. Lancet Infect. Dis. 2022, 23, 183. [Google Scholar] [CrossRef]
- Thorlund, K.; Sheldrick, K.; Meyerowitz-Katz, G.; Singh, S.; Hill, A. Making Statistical Sense of the Molnupiravir MOVe-OUT Clinical Trial. Am. J. Trop. Med. Hyg. 2022, 106, 1301–1304. [Google Scholar] [CrossRef]
- Reichel, A.; Lienau, P. Pharmacokinetics in Drug Discovery: An Exposure-Centred Approach to Optimising and Predicting Drug Efficacy and Safety. Handb. Exp. Pharmacol. 2016, 232, 235–260. [Google Scholar] [CrossRef]
- Butler, C.C.; Hobbs, F.D.R.; Gbinigie, O.A.; Rahman, N.M.; Hayward, G.; Richards, D.B.; Dorward, J.; Lowe, D.M.; Standing, J.F.; Breuer, J.; et al. Molnupiravir plus Usual Care versus Usual Care Alone as Early Treatment for Adults with COVID-19 at Increased Risk of Adverse Outcomes (PANORAMIC): An Open-Label, Platform-Adaptive Randomised Controlled Trial. Lancet 2023, 401, 281–293. [Google Scholar] [CrossRef] [PubMed]
- EMA Article 5(3) Opinions. Available online: https://www.ema.europa.eu/en/human-regulatory/post-authorisation/referral-procedures/article-53-opinions (accessed on 4 January 2023).
- Yoon, J.-J.; Toots, M.; Lee, S.; Lee, M.-E.; Ludeke, B.; Luczo, J.M.; Ganti, K.; Cox, R.M.; Sticher, Z.M.; Edpuganti, V.; et al. Orally Efficacious Broad-Spectrum Ribonucleoside Analog Inhibitor of Influenza and Respiratory Syncytial Viruses. Antimicrob. Agents Chemother. 2018, 62, e00766-18. [Google Scholar] [CrossRef] [PubMed]
- Toots, M.; Yoon, J.-J.; Cox, R.M.; Hart, M.; Sticher, Z.M.; Makhsous, N.; Plesker, R.; Barrena, A.H.; Reddy, P.G.; Mitchell, D.G.; et al. Characterization of Orally Efficacious Influenza Drug with High Resistance Barrier in Ferrets and Human Airway Epithelia. Sci. Transl. Med. 2019, 11, eaax5866. [Google Scholar] [CrossRef] [PubMed]
- EMA. EMA Issues Advice on Use of Lagevrio (Molnupiravir) for the Treatment COVID-19. Available online: https://www.ema.europa.eu/en/news/ema-issues-advice-use-lagevrio-molnupiravir-treatment-covid-19 (accessed on 4 January 2023).
- Amara, A.; Penchala, S.D.; Else, L.; Hale, C.; FitzGerald, R.; Walker, L.; Lyons, R.; Fletcher, T.; Khoo, S. The Development and Validation of a Novel LC-MS/MS Method for the Simultaneous Quantification of Molnupiravir and Its Metabolite ß-d-N4-Hydroxycytidine in Human Plasma and Saliva. J. Pharm. Biomed. Anal. 2021, 206, 114356. [Google Scholar] [CrossRef] [PubMed]
- WHO. Updates Its Treatment Guidelines to Include Molnupiravir. Available online: Https://Www.Who.Int/News/Item/03-03-2022-Molnupiravir (accessed on 30 December 2022).
- Merck and Ridgeback’s Molnupiravir Receives U.S. FDA Emergency Use Authorization for the Treatment of High-Risk Adults with Mild to Moderate COVID-19. Available online: https://www.merck.com/news/merck-and-ridgebacks-molnupiravir-receives-u-s-fda-emergency-use-authorization-for-the-treatment-of-high-risk-adults-with-mild-to-moderate-covid-19/ (accessed on 4 January 2023).
- Moon, S.; Armstrong, J.; Hutler, B.; Upshur, R.; Katz, R.; Atuire, C.; Bhan, A.; Emanuel, E.; Faden, R.; Ghimire, P.; et al. Governing the Access to COVID-19 Tools Accelerator: Towards Greater Participation, Transparency, and Accountability. Lancet 2022, 399, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Imran, M.; Kumar Arora, M.; Asdaq, S.M.B.; Khan, S.A.; Alaqel, S.I.; Alshammari, M.K.; Alshehri, M.M.; Alshrari, A.S.; Mateq Ali, A.; Al-Shammeri, A.M.; et al. Discovery, Development, and Patent Trends on Molnupiravir: A Prospective Oral Treatment for COVID-19. Molecules 2021, 26, 5795. [Google Scholar] [CrossRef] [PubMed]
- Hui, K.P.Y.; Ho, J.C.W.; Cheung, M.; Ng, K.; Ching, R.H.H.; Lai, K.; Kam, T.T.; Gu, H.; Sit, K.-Y.; Hsin, M.K.Y.; et al. SARS-CoV-2 Omicron Variant Replication in Human Bronchus and Lung Ex Vivo. Nature 2022, 603, 715–720. [Google Scholar] [CrossRef]
- Wolter, N.; Jassat, W.; Walaza, S.; Welch, R.; Moultrie, H.; Groome, M.; Amoako, D.G.; Everatt, J.; Bhiman, J.N.; Scheepers, C.; et al. Early Assessment of the Clinical Severity of the SARS-CoV-2 Omicron Variant in South Africa: A Data Linkage Study. Lancet 2022, 399, 437–446. [Google Scholar] [CrossRef]
- Goh, G.K.-M.; Dunker, A.K.; Foster, J.A.; Uversky, V.N. Shell Disorder Models Detect That Omicron Has Harder Shells with Attenuation but Is Not a Descendant of the Wuhan-Hu-1 SARS-CoV-2. Biomolecules 2022, 12, 631. [Google Scholar] [CrossRef]
- Wang, Y.; Li, P.; Solanki, K.; Li, Y.; Ma, Z.; Peppelenbosch, M.P.; Baig, M.S.; Pan, Q. Viral Polymerase Binding and Broad-Spectrum Antiviral Activity of Molnupiravir against Human Seasonal Coronaviruses. Virology 2021, 564, 33–38. [Google Scholar] [CrossRef]


| Drug | Molnupiravir | Paxlovid (Nirmatrelvir/Ritonavir) | Remdesivir | Favipiravir | References | |
|---|---|---|---|---|---|---|
| Criteria | ||||||
| Developed by | Merck & Ridgeback | Pfizer | Gilead Sciences | Toyama Chemical Co., Ltd. (Tokyo, Japan) | ||
| Chemical class | Nucleotide analog, prodrug | Peptidomimetic, active drug | Nucleotide analog, prodrug | Nucleotide analog, prodrug | [42] | |
| Mechanism | RdRp inhibitor | Protease inhibitor | RdRp inhibitor | RdRp inhibitor | [43] | |
| Indication | Mild to moderate to severe nonhospitalized high-risk COVID-19 patients | Mild to moderate nonhospitalized adult and pediatric COVID-19 patients | Mild to moderate to severe hospitalized high-risk COVID-19 patients | Mild to moderate hospitalized COVID-19 patients | [43] | |
| Approval status | EUA by US-FDA | EUA by US-FDA | Approved by US-FDA | Approved by Russian Health Ministry and National Medical Products Administration of China, not approved by US-FDA | [44] | |
| Dose | 800 mg, twice a day for 5 days | 300 mg Nirmatrelvir + 100 mg Ritonavir, twice a day for 5 days | 100 mg, once a day for 5 days | 1600 mg, twice a day for first day, followed by 600 mg, twice a day for second to fifth days | [45] | |
| Administration route in the body | Oral | Oral | Parenteral | Oral | [46] | |
| Interaction potential | Not the inhibitors or inducers of major drug metabolizing enzymes | Nirmatrelvir is a substrate for CYP3A and P-gp. Ritonavir is a potent CYP3A inhibitor, and is given with nirmatrelvir to increase plasma levels and half-life of nirmatrelvir. | It is an inducer of CYP1A2 and potentially CYP3A4 in vitro. | Weak inhibitor of CYPs 1A2, 2C9, 2D6, 2EA, and 3A4; Showed little of no induction of CYPs 1A2, 2C9, 2D6, 2EA, and 3A4 | [47] | |
| Cardiac effects | The effect on QT interval yet to be accessed | No effect was observed on QT interval | A possible risk of QT prolongation | The risk of QT elongation is considered low. | [48] | |
| Adverse effects | Diarrhea, nausea, and dizziness | Dysgeusia, diarrhea, hypertension, myalgia, anaphylaxis, and other hypersensitivity reactions | Nausea, hypersensitivity, increase prothrombin time | Diarrhea, liver toxicity, hyperuricemia | [49] | |
| Drug–drug interaction | Not found | Significant drug–drug interaction | No drug–drug interaction studies conducted clinically | Interaction observed with some drugs like chlorpromazine and quetiapine | [47] | |
| Important clinical trial | MOVe-OUT | EPIC-HR | PINETREE | NCT04434248, NCT04529499 | [50] | |
| Major concern | Safety concern | Multiple drug–drug interactions | Expensive and parenteral route of administration | High dose required | [51] | |
| Variants | Sub Variants | Major Mutations in Spike Protein | Impact of Molnupiravir | References |
|---|---|---|---|---|
| Delta | B.1.617.2 | T19R, G142D, FR156⁃157del, R158G, L452R, T478K, D614G, P681R, D950N | Studies shows that molnupiravir and its metabolite (EIDD-1931) inhibited the VeroE6-GFP cells in the SARS-CoV assay. | [76] |
| B.1.617.2 | The in vivo study for the efficacy of molnupiravir in ferrets and dwarf hamster model indicate that it reduced the lung viral load and prevented transmission. | [78] | ||
| B.1.617.2 | The early treatment of mild to moderately infected SARS-CoV-2 unvaccinated adult patient with molnupiravir decreases hospitalization and probability of death by 7.3%. | [79] | ||
| B.1.617.2.1 OR AY.1 | K417N, A1146T, V70F, and W258L | Although molnupiravir is recommended by USFDA, specific study related to B.1.617.2.1 is required to prove its efficacy and safety. | [90] | |
| Omicron | B. A1 | P681H, A67V, H655Y, S371L, and N679K | The susceptibility of molnupiravir was found to be 0.43 ± 0.08(IC50). This proves its effectiveness against B. A1. | [91,92] |
| B. A2 | S371F, D405N | A lower mortality rate, lower risk of SARS-CoV-2 progression, and redundancy in oxygen therapy was reported in molnupiravir-treated groups compared to the matched controls. | [85] | |
| B. A2 | S371F, D405N | The overall viral RNA clearance was decrease in molnupiravir group. | [86] | |
| B. A2 | P132H, S371F, D405N | The therapeutic results indicate that molnupiravir and its metabolite (EIDD-1931) inhibit the cytopathogenicity in VeroE6-GFP cells. | [93] | |
| B. A3 | A67V, H69del, V70del, T95I, V143del, Y144del, Y145del, N211I, L212del, S371F, D405N and G446S | Although molnupiravir is recommended by USFDA, specific study related to BA.3 is required to prove its efficacy and safety. | [94] | |
| B. A4 | Del69-70, 44 L452R, F486V, and R493Q | Use of molnupiravir is recommended by Japan government along with two other drugs, but clinical trials are not performed to support the data. | [95,96] | |
| B. A5 | Del69-70, 44 L452R, F486V, and R493Q | Use of molnupiravir is recommended by Japan government along with two other drugs, but clinical trials are not performed to support the data. | [95,96] | |
| Hybrid Variant | XD | E172D | A detailed study is required to prove the efficacy of molnupiravir against XD hybrid variant. | [97] |
| XE | A detailed study is required to prove the efficacy of molnupiravir against XD hybrid variant. | [97] | ||
| XF | A detailed study is required to prove the efficacy of molnupiravir against XD hybrid variant. | [97] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teli, D.; Balar, P.; Patel, K.; Sharma, A.; Chavda, V.; Vora, L. Molnupiravir: A Versatile Prodrug against SARS-CoV-2 Variants. Metabolites 2023, 13, 309. https://doi.org/10.3390/metabo13020309
Teli D, Balar P, Patel K, Sharma A, Chavda V, Vora L. Molnupiravir: A Versatile Prodrug against SARS-CoV-2 Variants. Metabolites. 2023; 13(2):309. https://doi.org/10.3390/metabo13020309
Chicago/Turabian StyleTeli, Divya, Pankti Balar, Kishan Patel, Anu Sharma, Vivek Chavda, and Lalit Vora. 2023. "Molnupiravir: A Versatile Prodrug against SARS-CoV-2 Variants" Metabolites 13, no. 2: 309. https://doi.org/10.3390/metabo13020309
APA StyleTeli, D., Balar, P., Patel, K., Sharma, A., Chavda, V., & Vora, L. (2023). Molnupiravir: A Versatile Prodrug against SARS-CoV-2 Variants. Metabolites, 13(2), 309. https://doi.org/10.3390/metabo13020309









