Exploration of Potential Breath Biomarkers of Chronic Kidney Disease through Thermal Desorption–Gas Chromatography/Mass Spectrometry
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Breath Sample Collection and Preparation
2.3. VOC Analysis Using TD–GCMS
2.4. Statistical Analyses
3. Results
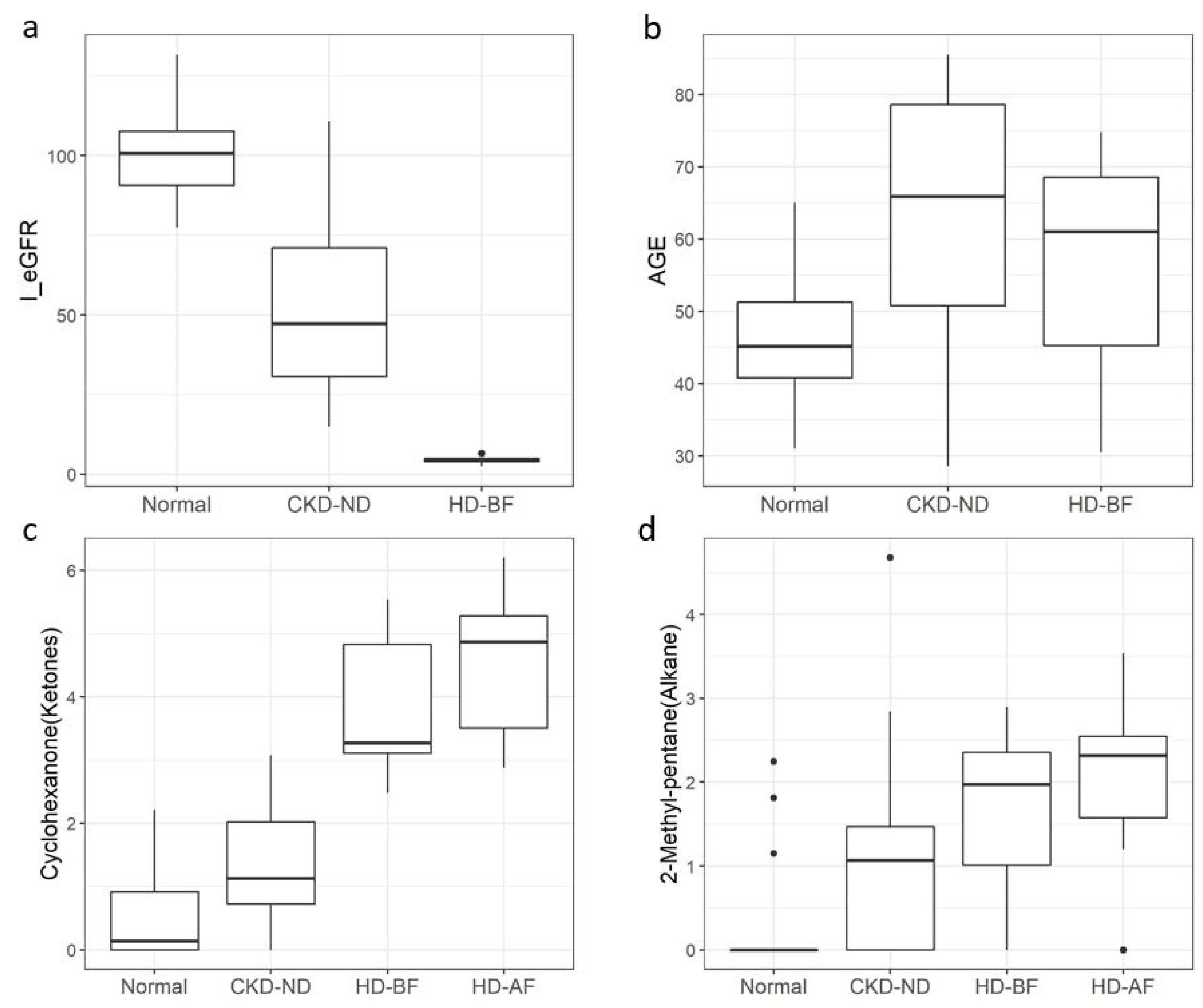
3.1. Characteristics of Study Participants
3.2. Overview of Breath VOCs
3.3. Potential Breath Markers for CKD
3.3.1. Selection of Significant Breath VOCs and Clinical Variables
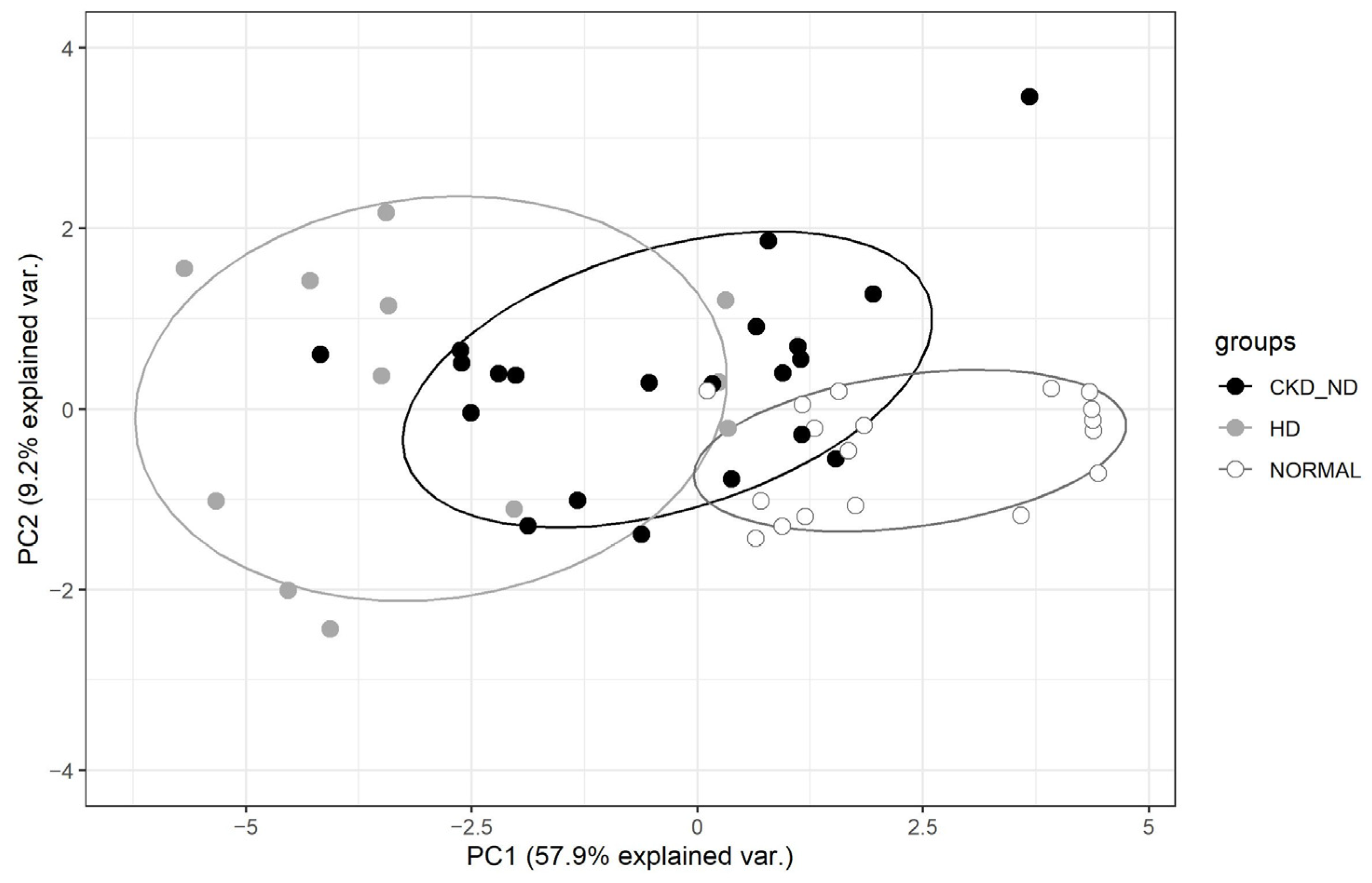
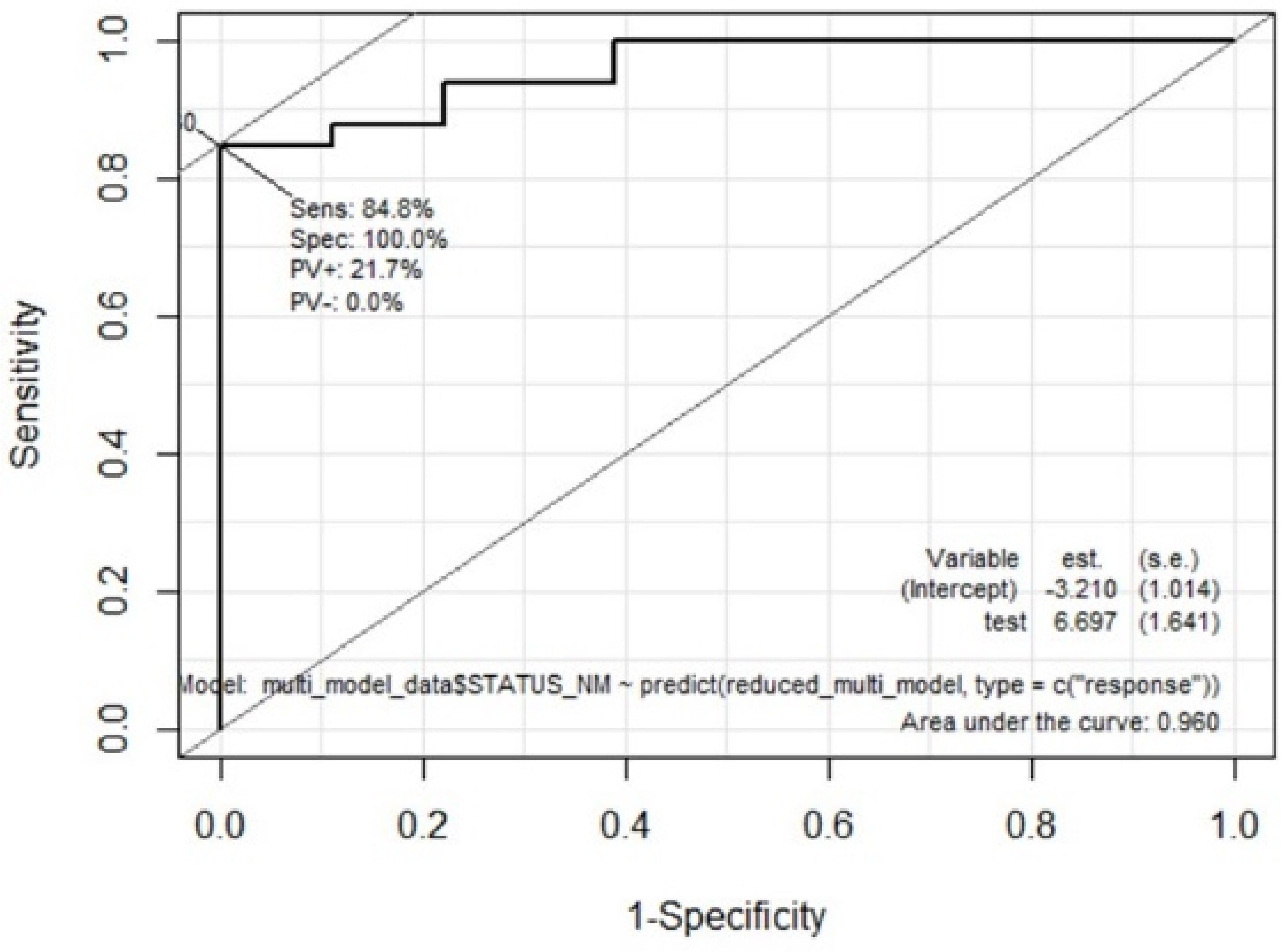
3.3.2. Multivariate Analysis to Extract Prediction Model of Discriminating Patients with CKD from Normal Controls
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Das, S.; Pal, M. Review—Non-Invasive Monitoring of Human Health by Exhaled Breath Analysis: A Comprehensive Review. J. Electrochem. Soc. 2020, 167, 037562. [Google Scholar] [CrossRef]
- Jendrny, P.; Schulz, C.; Twele, F.; Meller, S.; von Köckritz-Blickwede, M.; Osterhaus, A.D.M.E.; Ebbers, J.; Pilchová, V.; Pink, I.; Welte, T.; et al. Scent dog identification of samples from COVID-19 patients—A pilot study. BMC Infect. Dis. 2020, 20, 536. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, R.C.; Rodríguez, M.; de Romero, N.J.; Bruins, M.; Gómez, R.; Yntema, J.B.; Abente, G.C.; Gerritsen, J.W.; Wiegerinck, W.; Bejerano, D.P.; et al. The potential of a portable, point-of-care electronic nose to diagnose tuberculosis. J. Infect. 2017, 75, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Duranton, F.; Cohen, G.; De Smet, R.; Rodriguez, M.; Jankowski, J.; Vanholder, R.; Argiles, A.; European Uremic Toxin Work Group. Normal and Pathologic Concentrations of Uremic Toxins. J. Am. Soc. Nephrol. 2012, 23, 1258–1270. [Google Scholar] [CrossRef] [Green Version]
- Rosner, M.H.; Reis, T.; Husain-Syed, F.; Vanholder, R.; Hutchison, C.; Stenvinkel, P.; Blankestijn, P.J.; Cozzolino, M.; Juillard, L.; Kashani, K.; et al. Classification of Uremic Toxins and Their Role in Kidney Failure. Clin. J. Am. Soc. Nephrol. 2021, 16, 1918–1928. [Google Scholar] [CrossRef]
- Demirjian, S.; Paschke, K.M.; Wang, X.; Grove, D.; Heyka, R.J.; Dweik, R.A. Molecular breath analysis identifies the breathprint of renal failure. J. Breath Res. 2017, 11, 026009. [Google Scholar] [CrossRef]
- Pagonas, N.; Vautz, W.; Seifert, L.; Slodzinski, R.; Jankowski, J.; Zidek, W.; Westhoff, T.H. Volatile Organic Compounds in Uremia. PLoS ONE 2012, 7, e46258. [Google Scholar] [CrossRef] [Green Version]
- Simenhoff, M.L.; Burke, J.F.; Saukkonen, J.J.; Ordinario, A.T.; Doty, R.; Dunn, S. Biochemical Profile of Uremic Breath. N. Engl. J. Med. 1977, 297, 132–135. [Google Scholar] [CrossRef]
- Grabowska-Polanowska, B.; Faber, J.; Skowron, M.; Miarka, P.; Pietrzycka, A.; Śliwka, I.; Amann, A. Detection of potential chronic kidney disease markers in breath using gas chromatography with mass-spectral detection coupled with thermal desorption method. J. Chromatogr. A 2013, 1301, 179–189. [Google Scholar] [CrossRef]
- Narasimhan, L.R.; Goodman, W.; Patel, C.K.N. Correlation of breath ammonia with blood urea nitrogen and creatinine during hemodialysis. Proc. Natl. Acad. Sci. USA 2001, 98, 4617–4621. [Google Scholar] [CrossRef]
- Levin, A.; Stevens, P.E.; Bilous, R.W.; Coresh, J.; De Francisco, A.L.; De Jong, P.E.; Griffith, K.E.; Hemmelgarn, B.R.; Iseki, K.; Lamb, E.J.; et al. Kidney disease: Improving global outcomes (KDIGO) CKD work group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. Suppl. 2013, 3, 1–150. [Google Scholar]
- Westphal, K.; Dudzik, D.; Waszczuk-Jankowska, M.; Graff, B.; Narkiewicz, K.; Markuszewski, M.J. Common Strategies and Factors Affecting Off-Line Breath Sampling and Volatile Organic Compounds Analysis Using Thermal Desorption-Gas Chromatography-Mass Spectrometry (TD-GC-MS). Metabolites 2022, 13, 8. [Google Scholar] [CrossRef] [PubMed]
- De Vietro, N.; Aresta, A.M.; Picciariello, A.; Altomare, D.F.; Lucarelli, G.; Di Gilio, A.; Palmisani, J.; De Gennaro, G.; Zambonin, C. Optimization of a Breath Analysis Methodology to Potentially Diagnose Transplanted Kidney Rejection: A Preclinic Study. Appl. Sci. 2023, 13, 2852. [Google Scholar] [CrossRef]
- Phillips, M.; Herrera, J.; Krishnan, S.; Zain, M.; Greenberg, J.; Cataneo, R.N. Variation in volatile organic compounds in the breath of normal humans. J. Chromatogr. B Biomed. Sci. Appl. 1999, 729, 75–88. [Google Scholar] [CrossRef] [PubMed]
- Vinaixa, M.; Schymanski, E.L.; Neumann, S.; Navarro, M.; Salek, R.M.; Yanes, O. Mass spectral databases for LC/MS- and GC/MS-based metabolomics: State of the field and future prospects. TrAC Trends Anal. Chem. 2016, 78, 23–35. [Google Scholar] [CrossRef] [Green Version]
- Doran, S.L.F.; Romano, A.; Hanna, G.B. Optimisation of sampling parameters for standardised exhaled breath sampling. J. Breath Res. 2017, 12, 016007. [Google Scholar] [CrossRef] [PubMed]
- Davies, R. The metabolomic quest for a biomarker in chronic kidney disease. Clin. Kidney J. 2018, 11, 694–703. [Google Scholar] [CrossRef]
- Thompson-Torgerson, C.S.; Champion, H.C.; Santhanam, L.; Harris, Z.L.; Shoukas, A.A. Cyclohexanone contamination from extracorporeal circuits impairs cardiovascular function. Am. J. Physiol. Circ. Physiol. 2009, 296, H1926–H1932. [Google Scholar] [CrossRef] [Green Version]
- Mochalski, P.; King, J.; Haas, M.; Unterkofler, K.; Amann, A.; Mayer, G. Blood and breath profiles of volatile organic compounds in patients with end-stage renal disease. BMC Nephrol. 2014, 15, 43. [Google Scholar] [CrossRef]
- Wikipedia; Cyclohexanone. Available online: https://en.wikipedia.org/wiki/Cyclohexanone (accessed on 28 January 2023).
- International Agency for Research on Cancer (IARC). Cyclohexanone. Some Organic Solvents, Resin Monomers and Related Compounds, Pigments and Occupational Exposures in Paint Manufacture and Painting; World Health Organiztion: Geneva, Switzerland, 1989; Volume 47, pp. 157–169. [Google Scholar]
- Martis, L.; Tolhurst, T.; Koeferl, M.T.; Miller, T.R.; Darby, T.D. Disposition kinetics of cyclohexanone in beagle dogs*1. Toxicol. Appl. Pharmacol. 1980, 55, 545–553. [Google Scholar] [CrossRef]
- Human Metabolome DataBase (HMDB); Cyclohexanone. Available online: https://hmdb.ca/metabolites/HMDB0003315 (accessed on 29 January 2023).
- Lee, Y.-H.; Chung, Y.H.; Kim, H.-Y.; Shin, S.H.; Lee, S.B. Subacute Inhalation Toxicity of Cyclohexanone in B6C3F1 Mice. Toxicol. Res. 2018, 34, 49–53. [Google Scholar] [CrossRef] [Green Version]
- Bernard, A.M.; de Russis, R.; Normand, J.-C.; Lauwerys, R.R. Evaluation of the subacute nephrotoxicity of cyclohexane and other industrial solvents in the female Sprague-Dawley rat. Toxicol. Lett. 1989, 45, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Ong, C.; Chia, S.; Phoon, W.H.; Tan, K.T.; Kok, P.W. Monitoring of exposure to cyclohexanone through the analysis of breath and urine. Scand. J. Work. Environ. Health 1991, 17, 430–435. [Google Scholar] [CrossRef] [Green Version]
- Brugnone, F.; Perbellini, L.; Grigolini, L.; Apostoli, P. Solvent exposure in a shoe upper factory: II. Methylcyclopentane, 2-methylpentane, and 3-methylpentane concentration in alveolar and in environmental air and in blood. Int. Arch. Occup. Environ. Health 1979, 42, 355–363. [Google Scholar] [CrossRef] [PubMed]
- National Center for Biotechnology Information: PubChem; 2-Methylpentane. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/2-Methylpentane (accessed on 29 January 2023).
- Human Metabolome DataBase (HMDB). 2-Methylpentane. Available online: https://hmdb.ca/metabolites/HMDB0061884#spectra (accessed on 29 January 2023).
- de Lacy Costello, B.; Amann, A.; Al-Kateb, H.; Flynn, C.; Filipiak, W.; Khalid, T.; Osborne, D.; Ratcliffe, N.M. A review of the volatiles from the healthy human body. J. Breath Res. 2014, 8, 14001. [Google Scholar] [CrossRef]
- Garner, C.E.; Smith, S.; de Lacy Costello, B.; White, P.; Spencer, R.; Probert, C.S.J.; Ratcliffem, N.M. Volatile organic compounds from feces and their potential for diagnosis of gastrointestinal disease. FASEB J. 2007, 21, 1675–1688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smolinska, A.; Klaassen, E.M.M.; Dallinga, J.W.; Van De Kant, K.D.G.; Jobsis, Q.; Moonen, E.J.C.; Van Schayck, O.C.P.; Dompeling, E.; Van Schooten, F.J. Profiling of Volatile Organic Compounds in Exhaled Breath As a Strategy to Find Early Predictive Signatures of Asthma in Children. PLoS ONE 2014, 9, e95668. [Google Scholar] [CrossRef]


| Total n = 51 | Normal Healthy Control Group (n = 18) | CKD Group | ||
|---|---|---|---|---|
| Non-Dialysis CKD Patients (n = 21) | Hemodialysis Patients (n = 12) | p-Value | ||
| Age | 46.0 ± 8.9 (31.0–65.0) | 63.3 ± 16.4 (28.6–85.5) | 56.1 ± 16.0 (30.5–74.8) | 0.0001 |
| Sex (M:F) | 10:8 | 13:8 | 6:6 | 0.8893 |
| Physical Examination (mean ± SD) | ||||
| Body weight | 67.5 ± 14.6 | 71.9 ± 14.5 | 59.2 ± 10.3 | 0.962 |
| Height | 168.0 ± 9.5 | 163.6 ± 10.5 | 162.5 ± 10.0 | 0.119 |
| Body Mass Index (BMI) | 23.7 ± 3.2 | 26.7 ± 4.1 | 22.3 ± 2.6 | 0.230 |
| Systolic BP (SBP) | 122.4 ± 13.7 | 133.1 ± 13.9 | 148.3 ± 21.7 | 0.003 |
| Diastolic BP (DBP) | 76.3 ± 9.7 | 74.9 ± 10.2 | 78.3 ± 14.0 | 0.955 |
| Comorbidity (number (%)) | ||||
| Diabetes | 0 (0%) | 10 (47.6%) | 7 (58.3%) | 0.0000 |
| Hypertension | 0 (0%) | 17 (81.0%) | 11 (91.7%) | 0.0000 |
| Dyslipidemia | 0 (0%) | 17 (81.0%) | 3 (25.0%) | 0.0000 |
| Cerebrovascular accident (CVA) | 0 (0%) | 2 (9.5%) | 1 (8.3%) | 0.0995 |
| Coronary heart disease (CHD) | 0 (0%) | 1 (4.8%) | 7 (58.3%) | 0.0053 |
| Lung disease | 0 (0%) | 0 (0.0%) | 0 (0.0%) | |
| History of cancer | 1 (5.6%) | 5 (23.8%) | 0 (0.0%) | |
| Lab data (mean ± SD) | ||||
| BUN | 11.0 ± 3.9 | 23.6 ± 8.6 | 62.4 ± 20.0 | |
| Serum creatinine | 0.80 ± 0.16 | 1.56 ± 0.55 | 10.49 ± 1.87 | |
| eGFR (CKD-EPI) | 100.4 ± 12.0 | 50.8 ± 26.9 | 4.4 ± 1.0 | |
| Hemoglobin | 14.2 ± 1.3 | 13.2 ± 2.3 | 10.8 ± 1.0 | |
| Glucose | 101.4 ± 10.0 | 118.2 ± 26.9 | 150.8 ± 55.3 | |
| Calcium | 9.6 ± 0.4 | 9.4 ± 0.8 | 8.9 ± 0.5 | |
| Phosphorus | 3.6 ± 0.4 | 3.6 ± 0.5 | 5.1 ± 1.0 | |
| Uric acid | 4.7 ± 1.7 | 7.1 ± 1.5 | 6.3 ± 1.1 | |
| Total cholesterol | 201.8 ± 18.6 | 161.3 ± 48.8 | 107.8 ± 17.9 | |
| Triglycerides | 111.8 ± 56.8 | 125.1 ± 51.3 | 100.0 ± 55.3 | |
| HDL-cholesterol | 63.5 ± 13.4 | 48.4 ± 9.3 | 47.2 ± 7.9 | |
| LDL-cholesterol | 122.7 ± 19.4 | 90.6 ± 36.4 | 55.0 ± 12.3 | |
| Protein | 7.5 ± 0.5 | 7.1 ± 0.6 | 6.6 ± 0.4 | |
| Albumin | 4.7 ± 0.4 | 4.2 ± 0.6 | 3.9 ± 0.3 | |
| Name of VOC or Clinical Variable | VOC Group | OR | 95% CI | p_Value | DEP_VAR |
|---|---|---|---|---|---|
| Decane | Alkane | 2.79 | 1.67–5.44 | 0.0005 | A_152 |
| Heptane | Alkane | 5.85 | 2.47–20.09 | 0.0006 | A_134 |
| Acetophenone | Ketones | 10.04 | 3.15–50.01 | 0.0008 | A_35 |
| m-Xylene | Aromatics | 2.27 | 1.5–4.13 | 0.0010 | A_222 |
| Trichloroethene | Halo-Hydrocarbons | 4.00 | 1.88–10.48 | 0.0013 | A_100 |
| Cyclohexanone | Ketones | 3.60 | 1.83–9.04 | 0.0014 | A_31 |
| Acetic acid ethyl ester | Acetate | 3.63 | 1.86–9.5 | 0.0014 | A_239 |
| n-Nonane | Alkane | 2.69 | 1.52–5.68 | 0.0025 | A_147 |
| Age | 1.08 | 1.03–1.14 | 0.0035 | AGE | |
| 1,2-Dichloro- ethane | Halo-Hydrocarbons | 16.48 | 3.27–169.2 | 0.0043 | A_93 |
| 2-Butanone | Ketones | 2.07 | 1.29–3.77 | 0.0069 | A_23 |
| Systolic BP | 1.07 | 1.02–1.13 | 0.0085 | PE_SBP | |
| Sulfur dioxide | VSC | 3.03 | 1.45–7.84 | 0.0085 | A_4 |
| 2-Methyl pentane | Alkane | 2.92 | 1.42–7.54 | 0.0099 | A_130 |
| Phenol | Alcohol | 0.78 | 0.61–0.91 | 0.0105 | A_62 |
| 3-Heptanone | Ketones | 5.56 | 1.63–26.17 | 0.0135 | A_25 |
| Acetone | Ketones | 1.05 | 1.01–1.11 | 0.0159 | A_21 |
| p-Xylene | Aromatics | 2.14 | 1.26–4.54 | 0.0166 | A_219 |
| Dihydro-2(3H)-furanone | Ketones | 2.59 | 1.26–6.17 | 0.0171 | A_27 |
| Nonadecane | Alkane | 0.80 | 0.62–0.91 | 0.0175 | A_178 |
| 2-Pentanone | Ketones | 0.72 | 0.53–0.92 | 0.0176 | A_28 |
| Isoprene | Terpenes | 0.96 | 0.91–0.99 | 0.0188 | A_187 |
| Octadecane | Alkane | 0.51 | 0.26–0.82 | 0.0241 | A_177 |
| 2-Ethyl-1-Hexanol | Alcohol | 2.64 | 1.34–8.7 | 0.0264 | A_67 |
| Ethylene oxide | Other | 1.49 | 1.06–2.17 | 0.0269 | A_294 |
| 3-Carene | Terpenes | 0.65 | 0.42–0.91 | 0.0271 | A_197 |
| o-Xylene | Aromatics | 0.79 | 0.63–0.96 | 0.0282 | A_221 |
| Myrcene | Terpenes | 0.73 | 0.54–0.93 | 0.0293 | A_196 |
| Octanal | Aldehyde | 3.03 | 1.31–10.64 | 0.0309 | A_281 |
| 2-Methylpropyl methyl ketone | Ketones | 2.74 | 1.14–7.4 | 0.0327 | A_33 |
| Azulene | Aromatics | 4.71 | 1.52–37.23 | 0.0351 | A_228 |
| Acetaldehyde | Aldehyde | 0.85 | 0.7–0.97 | 0.0353 | A_273 |
| 1,8-Cineol | Other | 0.85 | 0.69–0.96 | 0.0378 | A_297 |
| γ-Terpinene | Terpenes | 0.72 | 0.5–0.95 | 0.0387 | A_192 |
| Ethyl cyclohexane | Alkane | 5.99 | 1.48–61.03 | 0.0444 | A_139 |
| Pentadecane | Alkane | 0.71 | 0.45–0.91 | 0.0450 | A_169 |
| (1-Methylethyl)-benzene | Aromatics | 2.41 | 1.11–6.59 | 0.0468 | A_223 |
| Dimethyl selenide | Other | 0.69 | 0.46–0.98 | 0.0481 | A_285 |
| DEP_VAR | OR | 2.50% | 97.50% | p-Value |
|---|---|---|---|---|
| (Intercept) | −12.92 | 4.80 | −2.69 | 0.007 |
| Age | 0.18 | 0.07 | 2.49 | 0.013 |
| 2-Methyl-pentane (A_130) | 2.10 | 0.94 | 2.24 | 0.025 |
| Cyclohexanone (A_31) | 2.31 | 0.88 | 2.64 | 0.008 |
| STATUS_NM | 0 | 1 | ||
| 0 | 15 | 3 | ||
| 1 | 4 | 29 | Accuracy = 86.3% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seong, S.-H.; Kim, H.S.; Lee, Y.-M.; Kim, J.-S.; Park, S.; Oh, J. Exploration of Potential Breath Biomarkers of Chronic Kidney Disease through Thermal Desorption–Gas Chromatography/Mass Spectrometry. Metabolites 2023, 13, 837. https://doi.org/10.3390/metabo13070837
Seong S-H, Kim HS, Lee Y-M, Kim J-S, Park S, Oh J. Exploration of Potential Breath Biomarkers of Chronic Kidney Disease through Thermal Desorption–Gas Chromatography/Mass Spectrometry. Metabolites. 2023; 13(7):837. https://doi.org/10.3390/metabo13070837
Chicago/Turabian StyleSeong, Si-Hyun, Hyun Sik Kim, Yong-Moon Lee, Jae-Seok Kim, Sangwoo Park, and Jieun Oh. 2023. "Exploration of Potential Breath Biomarkers of Chronic Kidney Disease through Thermal Desorption–Gas Chromatography/Mass Spectrometry" Metabolites 13, no. 7: 837. https://doi.org/10.3390/metabo13070837







