Serum Irisin, Myostatin, and Myonectin Correlate with Metabolic Health Markers, Liver Disease Progression, and Blood Pressure in Patients with Metabolic Dysfunction-Associated Fatty Liver Disease and Hypertension
Abstract
1. Background
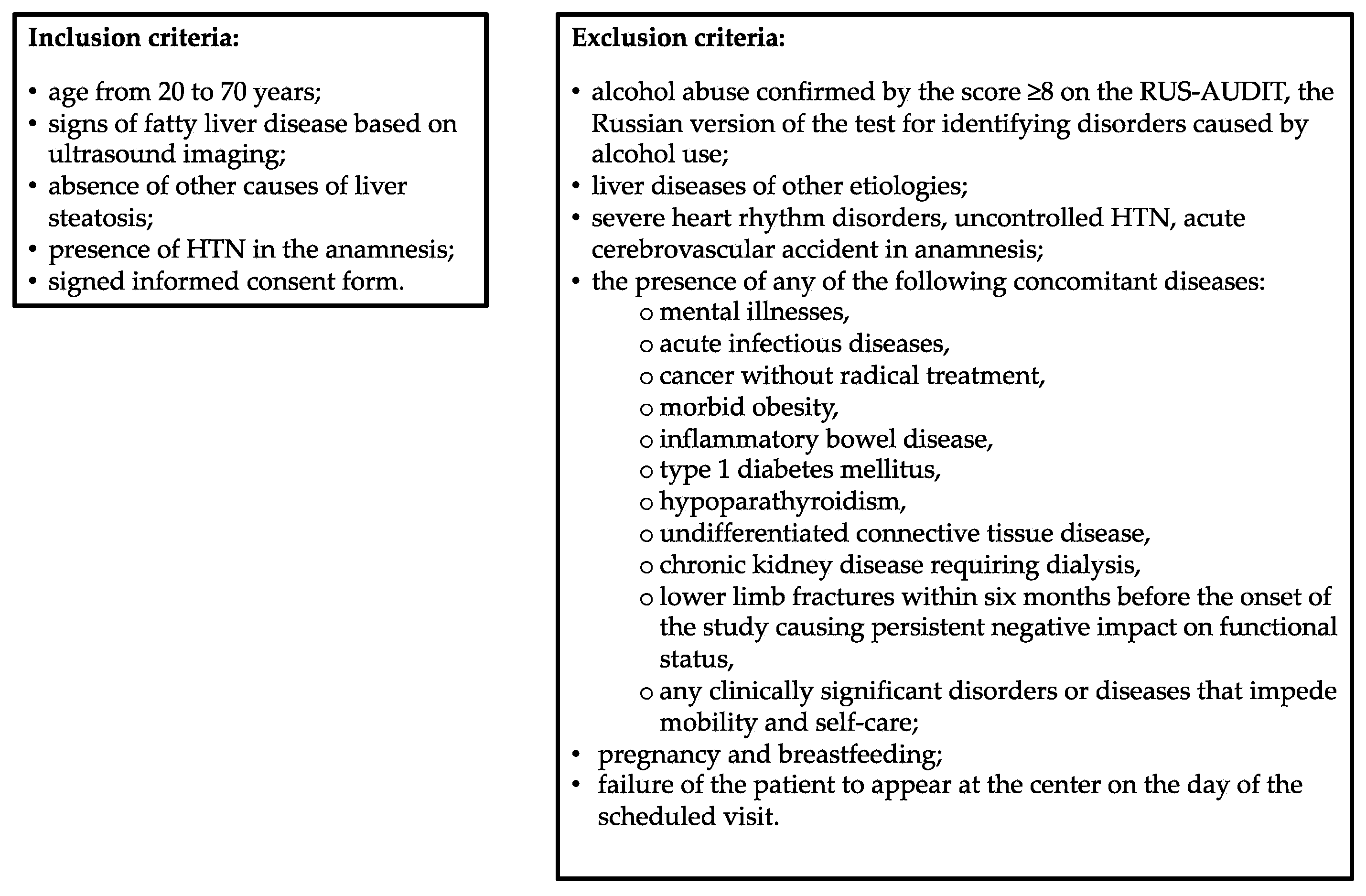
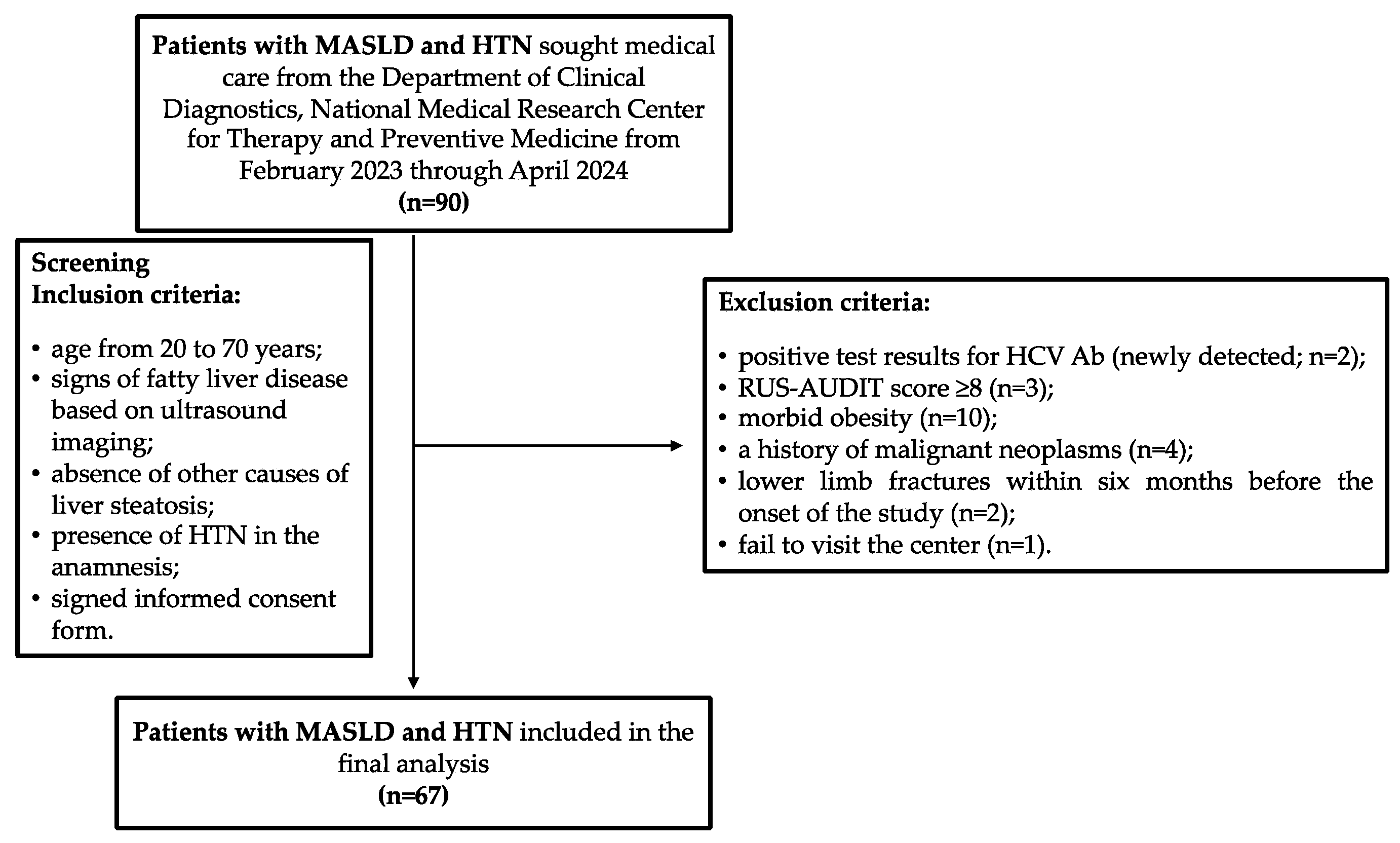
2. Materials and Methods
2.1. Patients
2.2. Diagnoses of Metabolic Dysfunction-Associated Steatotic Liver Disease and Hypertension
2.3. Assessment of Anthropometric Indicators
2.4. Blood Myokine Profile Study
2.5. Statistical Analyses
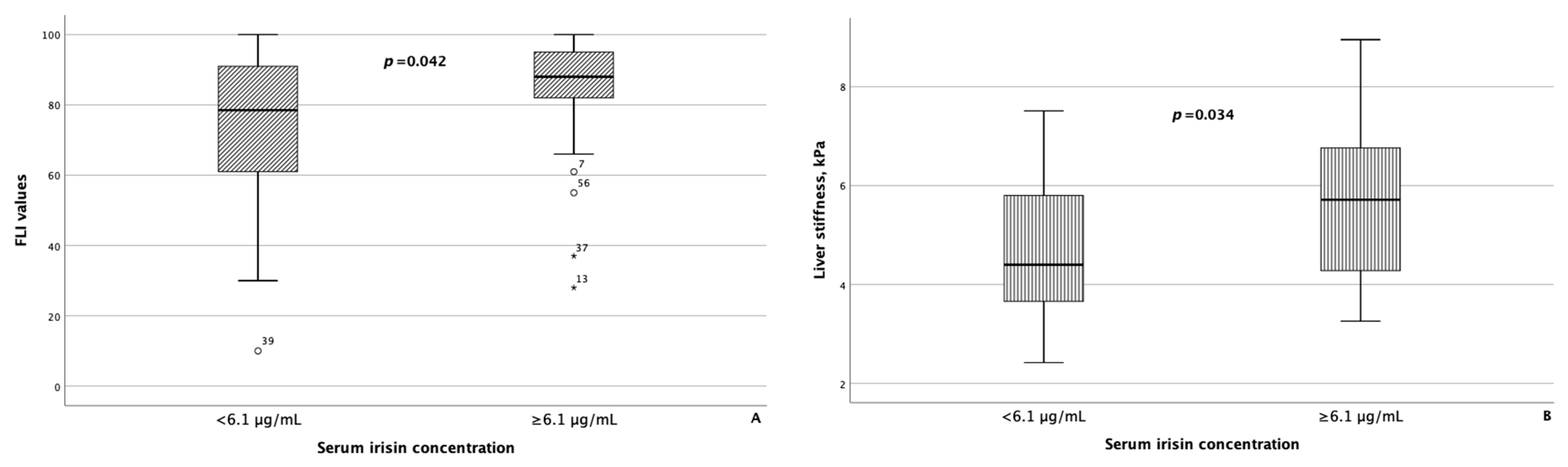
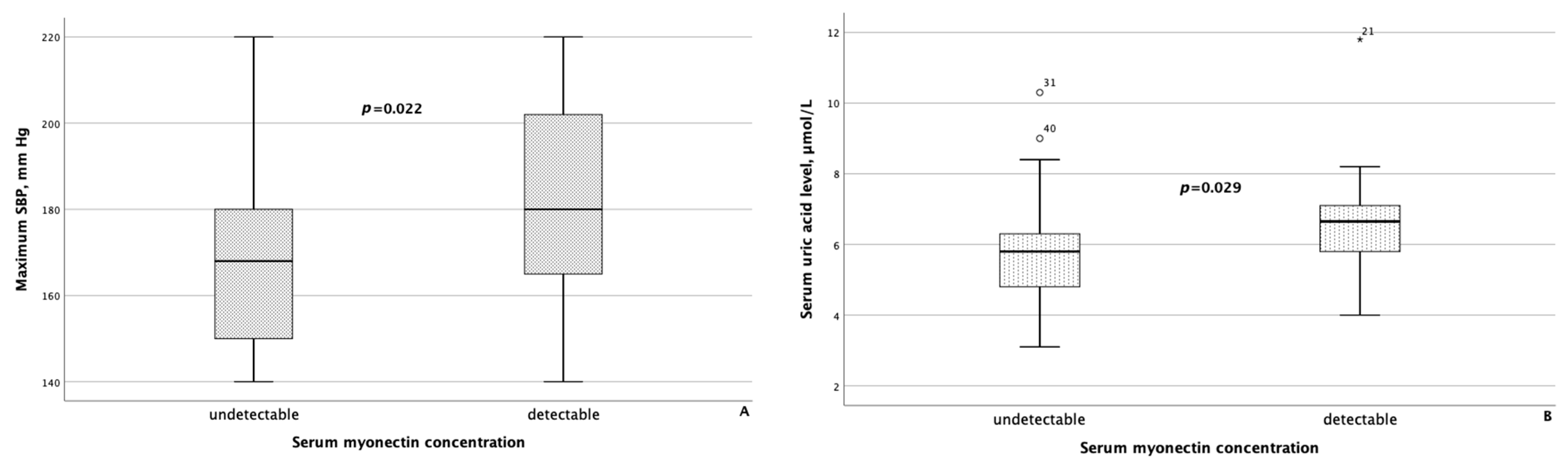
3. Results
3.1. General Characteristics of Patients
3.2. Assessment of Myokine Concentrations in the Blood Serum of Patients with Metabolic Dysfunction-Associated Steatotic Liver Disease and Hypertension
4. Discussion
5. Limitations of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global Epidemiology of Nonalcoholic Fatty Liver Disease-Meta-Analytic Assessment of Prevalence, Incidence, and Outcomes. Hepatol. Baltim. Md. 2016, 64, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Golabi, P.; Paik, J.M.; Henry, A.; Van Dongen, C.; Henry, L. The Global Epidemiology of Nonalcoholic Fatty Liver Disease (NAFLD) and Nonalcoholic Steatohepatitis (NASH): A Systematic Review. Hepatol. Baltim. Md. 2023, 77, 1335–1347. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, G.; Dashti, F.; Banini, B.A. Nonalcoholic Liver Disease: Epidemiology, Risk Factors, Natural History, and Management Strategies. Ann. N. Y. Acad. Sci. 2023, 1526, 16–29. [Google Scholar] [CrossRef] [PubMed]
- Tkachev, A.V.; Tarasova, G.N.; Groshilin, V.S.; Vasilchenkov, D.A.; Ushakova, T.I.; Blinov, D.V. Prevalence of nonalcoholic fatty liver disease in outpatients in Rostov-on-Don: Regional results of the DIREG-2 study. Ter. Arkh. 2016, 88, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Kanwal, F.; Kramer, J.R.; Li, L.; Dai, J.; Natarajan, Y.; Yu, X.; Asch, S.M.; El-Serag, H.B. Effect of Metabolic Traits on the Risk of Cirrhosis and Hepatocellular Cancer in Nonalcoholic Fatty Liver Disease. Hepatol. Baltim. Md. 2020, 71, 808–819. [Google Scholar] [CrossRef]
- Song, Q.; Liu, S.; Ling, Q.-H.; Gao, Q.-N.; Yang, R.-X.; Chen, S.-H.; Wu, S.; Chen, M.-L.; Cai, J. Severity of Nonalcoholic Fatty Liver Disease Is Associated With Cardiovascular Outcomes in Patients With Prehypertension or Hypertension: A Community–Based Cohort Study. Front. Endocrinol. 2022, 13, 942647. [Google Scholar] [CrossRef]
- Eskridge, W.; Cryer, D.R.; Schattenberg, J.M.; Gastaldelli, A.; Malhi, H.; Allen, A.M.; Noureddin, M.; Sanyal, A.J. Metabolic Dysfunction-Associated Steatotic Liver Disease and Metabolic Dysfunction-Associated Steatohepatitis: The Patient and Physician Perspective. J. Clin. Med. 2023, 12, 6216. [Google Scholar] [CrossRef]
- Ding, Y.; Deng, Q.; Yang, M.; Niu, H.; Wang, Z.; Xia, S. Clinical Classification of Obesity and Implications for Metabolic Dysfunction-Associated Fatty Liver Disease and Treatment. Diabetes Metab. Syndr. Obes. 2023, 16, 3303–3329. [Google Scholar] [CrossRef]
- Francque, S.M.A.; Dirinck, E. NAFLD Prevalence and Severity in Overweight and Obese Populations. Lancet Gastroenterol. Hepatol. 2023, 8, 2–3. [Google Scholar] [CrossRef]
- Altajar, S.; Baffy, G. Skeletal Muscle Dysfunction in the Development and Progression of Nonalcoholic Fatty Liver Disease. J. Clin. Transl. Hepatol. 2020, 8, 414–423. [Google Scholar] [CrossRef]
- Peiseler, M.; Schwabe, R.; Hampe, J.; Kubes, P.; Heikenwälder, M.; Tacke, F. Immune Mechanisms Linking Metabolic Injury to Inflammation and Fibrosis in Fatty Liver Disease—Novel Insights into Cellular Communication Circuits. J. Hepatol. 2022, 77, 1136–1160. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, N.; Maruyama, T.; Yoshikawa, N.; Matsumiya, R.; Ma, Y.; Ito, N.; Tasaka, Y.; Kuribara-Souta, A.; Miyata, K.; Oike, Y.; et al. A Muscle-Liver-Fat Signalling Axis Is Essential for Central Control of Adaptive Adipose Remodelling. Nat. Commun. 2015, 6, 6693. [Google Scholar] [CrossRef] [PubMed]
- Chakravarthy, M.V.; Siddiqui, M.S.; Forsgren, M.F.; Sanyal, A.J. Harnessing Muscle-Liver Crosstalk to Treat Nonalcoholic Steatohepatitis. Front. Endocrinol. 2020, 11, 592373. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Wang, L.; You, W.; Shan, T. Myokines Mediate the Cross Talk between Skeletal Muscle and Other Organs. J. Cell. Physiol. 2021, 236, 2393–2412. [Google Scholar] [CrossRef] [PubMed]
- Severinsen, M.C.K.; Pedersen, B.K. Muscle–Organ Crosstalk: The Emerging Roles of Myokines. Endocr. Rev. 2020, 41, 594–609. [Google Scholar] [CrossRef]
- Pourranjbar, M.; Arabnejad, N.; Naderipour, K.; Rafie, F. Effects of Aerobic Exercises on Serum Levels of Myonectin and Insulin Resistance in Obese and Overweight Women. J. Med. Life 2018, 11, 381–386. [Google Scholar] [CrossRef]
- Balakrishnan, R.; Thurmond, D.C. Mechanisms by Which Skeletal Muscle Myokines Ameliorate Insulin Resistance. Int. J. Mol. Sci. 2022, 23, 4636. [Google Scholar] [CrossRef]
- Ahima, R.S.; Park, H.-K. Connecting Myokines and Metabolism. Endocrinol. Metab. 2015, 30, 235–245. [Google Scholar] [CrossRef]
- Delogu, W.; Caligiuri, A.; Provenzano, A.; Rosso, C.; Bugianesi, E.; Coratti, A.; Macias-Barragan, J.; Galastri, S.; Di Maira, G.; Marra, F. Myostatin Regulates the Fibrogenic Phenotype of Hepatic Stellate Cells via C-Jun N-Terminal Kinase Activation. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2019, 51, 1400–1408. [Google Scholar] [CrossRef]
- Dong, H.N.; Park, S.Y.; Le, C.T.; Choi, D.-H.; Cho, E.-H. Irisin Regulates the Functions of Hepatic Stellate Cells. Endocrinol. Metab. 2020, 35, 647–655. [Google Scholar] [CrossRef]
- Schneider, C.V.; Zandvakili, I.; Thaiss, C.A.; Schneider, K.M. Physical Activity Is Associated with Reduced Risk of Liver Disease in the Prospective UK Biobank Cohort. JHEP Rep. 2021, 3, 100263. [Google Scholar] [CrossRef] [PubMed]
- Zunner, B.E.M.; Wachsmuth, N.B.; Eckstein, M.L.; Scherl, L.; Schierbauer, J.R.; Haupt, S.; Stumpf, C.; Reusch, L.; Moser, O. Myokines and Resistance Training: A Narrative Review. Int. J. Mol. Sci. 2022, 23, 3501. [Google Scholar] [CrossRef] [PubMed]
- Pucci, G.; Ministrini, S.; Nulli Migliola, E.; Nunziangeli, L.; Battista, F.; D’Abbondanza, M.; Anastasio, F.; Crapa, M.E.; Sanesi, L.; Carbone, F.; et al. Relationship between Serum Myostatin Levels and Carotid-Femoral Pulse Wave Velocity in Healthy Young Male Adolescents: The MACISTE Study. J. Appl. Physiol. Bethesda Md. 1985 2021, 130, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Xiang, G.; Liu, M.; Mei, W.; Xiang, L.; Dong, J. Irisin Protects against Endothelial Injury and Ameliorates Atherosclerosis in Apolipoprotein E-Null Diabetic Mice. Atherosclerosis 2015, 243, 438–448. [Google Scholar] [CrossRef] [PubMed]
- Maciorkowska, M.; Musiałowska, D.; Małyszko, J. Adropin and Irisin in Arterial Hypertension, Diabetes Mellitus and Chronic Kidney Disease. Adv. Clin. Exp. Med. Off. Organ. Wroc. Med. Univ. 2019, 28, 1571–1575. [Google Scholar] [CrossRef]
- Leiherer, A.; Muendlein, A.; Geiger, K.; Saely, C.H.; Grabher, V.; Fraunberger, P.; Drexel, H. The New Myokine Myonectin Is Significantly Associated with Type 2 Diabetes in Elderly Cardiovascular Disease Patients. Atherosclerosis 2022, 355, 167. [Google Scholar] [CrossRef]
- Rinella, M.E.; Lazarus, J.V.; Ratziu, V.; Francque, S.M.; Sanyal, A.J.; Kanwal, F.; Romero, D.; Abdelmalek, M.F.; Anstee, Q.M.; Arab, J.P.; et al. A Multisociety Delphi Consensus Statement on New Fatty Liver Disease Nomenclature. Hepatol. Baltim. Md. 2023, 78, 1966–1986. [Google Scholar] [CrossRef]
- Polyzos, S.A.; Kountouras, J.; Anastasilakis, A.D.; Geladari, E.V.; Mantzoros, C.S. Irisin in Patients with Nonalcoholic Fatty Liver Disease. Metabolism 2014, 63, 207–217. [Google Scholar] [CrossRef]
- Petta, S.; Valenti, L.; Svegliati-Baroni, G.; Ruscica, M.; Pipitone, R.M.; Dongiovanni, P.; Rychlicki, C.; Ferri, N.; Cammà, C.; Fracanzani, A.L.; et al. Fibronectin Type III Domain-Containing Protein 5 Rs3480 A>G Polymorphism, Irisin, and Liver Fibrosis in Patients With Nonalcoholic Fatty Liver Disease. J. Clin. Endocrinol. Metab. 2017, 102, 2660–2669. [Google Scholar] [CrossRef]
- Kakino, S.; Ohki, T.; Nakayama, H.; Yuan, X.; Otabe, S.; Hashinaga, T.; Wada, N.; Kurita, Y.; Tanaka, K.; Hara, K.; et al. Pivotal Role of TNF-α in the Development and Progression of Nonalcoholic Fatty Liver Disease in a Murine Model. Horm. Metab. Res. 2018, 50, 80–87. [Google Scholar] [CrossRef]
- Wilkes, J.J.; Lloyd, D.J.; Gekakis, N. Loss-of-Function Mutation in Myostatin Reduces Tumor Necrosis Factor α Production and Protects Liver Against Obesity-Induced Insulin Resistance. Diabetes 2009, 58, 1133–1143. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Rinella, M.E.; Sanyal, A.J.; Harrison, S.A.; Brunt, E.M.; Goodman, Z.; Cohen, D.E.; Loomba, R. From NAFLD to MAFLD: Implications of a Premature Change in Terminology. Hepatology 2021, 73, 1194–1198. [Google Scholar] [CrossRef] [PubMed]
- Bedogni, G.; Bellentani, S.; Miglioli, L.; Masutti, F.; Passalacqua, M.; Castiglione, A.; Tiribelli, C. The Fatty Liver Index: A Simple and Accurate Predictor of Hepatic Steatosis in the General Population. BMC Gastroenterol. 2006, 6, 33. [Google Scholar] [CrossRef] [PubMed]
- Boursier, J.; Zarski, J.-P.; de Ledinghen, V.; Rousselet, M.-C.; Sturm, N.; Lebail, B.; Fouchard-Hubert, I.; Gallois, Y.; Oberti, F.; Bertrais, S.; et al. Determination of Reliability Criteria for Liver Stiffness Evaluation by Transient Elastography. Hepatol. Baltim. Md. 2013, 57, 1182–1191. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.; Sidhu, P.S. Ultrasound-Based Liver Elastography: Current Results and Future Perspectives. Abdom. Radiol. N. Y. 2020, 45, 3463–3472. [Google Scholar] [CrossRef]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef]
- Bland, M. An Introduction to Medical Statistics; Oxford University Press: Oxford, UK, 2015; ISBN 978-0-19-958992-0. [Google Scholar]
- Targher, G.; Tilg, H.; Byrne, C.D. Non-Alcoholic Fatty Liver Disease: A Multisystem Disease Requiring a Multidisciplinary and Holistic Approach. Lancet Gastroenterol. Hepatol. 2021, 6, 578–588. [Google Scholar] [CrossRef]
- Santos, J.P.M.D.; Maio, M.C.D.; Lemes, M.A.; Laurindo, L.F.; Haber, J.F.D.S.; Bechara, M.D.; Prado Jr, P.S.D.; Rauen, E.C.; Costa, F.; Pereira, B.C.D.A.; et al. Non-Alcoholic Steatohepatitis (NASH) and Organokines: What Is Now and What Will Be in the Future. Int. J. Mol. Sci. 2022, 23, 498. [Google Scholar] [CrossRef]
- Sanyal, A.J.; Shankar, S.S.; Yates, K.P.; Bolognese, J.; Daly, E.; Dehn, C.A.; Neuschwander-Tetri, B.; Kowdley, K.; Vuppalanchi, R.; Behling, C.; et al. Diagnostic Performance of Circulating Biomarkers for Non-Alcoholic Steatohepatitis. Nat. Med. 2023, 29, 2656–2664. [Google Scholar] [CrossRef]
- Tariq, T.; Desai, A.P. Nonalcoholic Fatty Liver Disease: Making the Diagnosis. Clin. Liver Dis. 2020, 16, 53–57. [Google Scholar] [CrossRef]
- Chang, J.S.; Kim, T.H.; Nguyen, T.T.; Park, K.-S.; Kim, N.; Kong, I.D. Circulating Irisin Levels as a Predictive Biomarker for Sarcopenia: A Cross-Sectional Community-Based Study. Geriatr. Gerontol. Int. 2017, 17, 2266–2273. [Google Scholar] [CrossRef] [PubMed]
- Carli, F.; Sabatini, S.; Gaggini, M.; Sironi, A.M.; Bedogni, G.; Gastaldelli, A. Fatty Liver Index (FLI) Identifies Not Only Individuals with Liver Steatosis but Also at High Cardiometabolic Risk. Int. J. Mol. Sci. 2023, 24, 14651. [Google Scholar] [CrossRef] [PubMed]
- Roh, J.-H.; Park, J.-H.; Lee, H.; Yoon, Y.-H.; Kim, M.; Kim, Y.-G.; Park, G.-M.; Lee, J.-H.; Seong, I.-W. A Close Relationship between Non-Alcoholic Fatty Liver Disease Marker and New-Onset Hypertension in Healthy Korean Adults. Korean Circ. J. 2020, 50, 695–705. [Google Scholar] [CrossRef] [PubMed]
- Pinho-Jr, J.D.S.; Camacho, F.A.; Cavararo, C.D.S.; Baião, P.F.; Medeiros, R.F.; Barroso, S.G.; Matos, A.C.D. Irisin and Cardiometabolic Disorders in Obesity: A Systematic Review. Int. J. Inflamm. 2023, 2023, 5810157. [Google Scholar] [CrossRef] [PubMed]
- Stengel, A.; Hofmann, T.; Goebel-Stengel, M.; Elbelt, U.; Kobelt, P.; Klapp, B.F. Circulating Levels of Irisin in Patients with Anorexia Nervosa and Different Stages of Obesity--Correlation with Body Mass Index. Peptides 2013, 39, 125–130. [Google Scholar] [CrossRef]
- Leung, W.K.C.; Yu, A.P.; Lai, C.W.K.; Siu, P.M. Association of Markers of Proinflammatory Phenotype and Beige Adipogenesis with Metabolic Syndrome in Chinese Centrally Obese Adults. J. Diabetes Res. 2018, 2018, 8956509. [Google Scholar] [CrossRef]
- Jamialahamdi, T.; Mirhadi, E.; Almahmeed, W.; Eid, A.H.; Al-Rasadi, K.; Nguyen, N.T.; Gadde, K.M.; Sahebkar, A. Impact of Bariatric Surgery on Circulating Irisin Levels: A Systematic Review and Meta-analysis. Updat. Surg. 2024, 76, 1–10. [Google Scholar] [CrossRef]
- Maak, S.; Norheim, F.; Drevon, C.A.; Erickson, H.P. Progress and Challenges in the Biology of FNDC5 and Irisin. Endocr. Rev. 2021, 42, 436–456. [Google Scholar] [CrossRef]
- Moreno-Navarrete, J.M.; Ortega, F.; Serrano, M.; Guerra, E.; Pardo, G.; Tinahones, F.; Ricart, W.; Fernández-Real, J.M. Irisin Is Expressed and Produced by Human Muscle and Adipose Tissue in Association with Obesity and Insulin Resistance. J. Clin. Endocrinol. Metab. 2013, 98, E769–E778. [Google Scholar] [CrossRef]
- Nilofer Sagana, M.K.; Arul Senghor, K.A.; Vinodhini, V.M.; Renuka, P. Irisin and Triglyceride Glucose Index as Markers of Dyslipidemia in Young Adults. Indian. J. Clin. Biochem. IJCB 2024, 39, 136–141. [Google Scholar] [CrossRef]
- Ismail, Z.M.; Al-Fartusie, F.S.; Tahir, N.T.; Ismail, A.H. Investigation the Relationship Between Myonectin Levels and Both Lipid Profiles and Liver Function Tests in Diabetic Nephropathy Patients. J. Port. Sci. Res. 2024, 7, 30–35. [Google Scholar] [CrossRef]
- Li, Z.; Yang, Y.-L.; Zhu, Y.-J.; Li, C.-G.; Tang, Y.-Z.; Ni, C.-L.; Chen, L.-M.; Niu, W.-Y. Circulating Serum Myonectin Levels in Obesity and Type 2 Diabetes Mellitus. Exp. Clin. Endocrinol. Diabetes 2021, 129, 528–534. [Google Scholar] [CrossRef] [PubMed]
- McKay, B.R.; Ogborn, D.I.; Bellamy, L.M.; Tarnopolsky, M.A.; Parise, G. Myostatin Is Associated with Age-Related Human Muscle Stem Cell Dysfunction. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2012, 26, 2509–2521. [Google Scholar] [CrossRef] [PubMed]
- Yasar, E.; Tek, N.A.; Tekbudak, M.Y.; Yurtdaş, G.; Gülbahar, Ö.; Uyar, G.Ö.; Ural, Z.; Çelik, Ö.M.; Erten, Y. The Relationship Between Myostatin, Inflammatory Markers, and Sarcopenia in Patients With Chronic Kidney Disease. J. Ren. Nutr. 2022, 32, 677–684. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, T.; Vasilieva, L.; Kontogianni, M.D.; Tenta, R.; Georgiou, A.; Stroumpouli, E.; Mani, I.; Alexopoulou, A. Myostatin in Combination with Creatine Phosphokinase or Albumin May Differentiate Patients with Cirrhosis and Sarcopenia. Am. J. Physiol. Gastrointest. Liver Physiol. 2021, 321, G543–G551. [Google Scholar] [CrossRef]
- Nishikawa, H.; Enomoto, H.; Ishii, A.; Iwata, Y.; Miyamoto, Y.; Ishii, N.; Yuri, Y.; Hasegawa, K.; Nakano, C.; Nishimura, T.; et al. Elevated Serum Myostatin Level Is Associated with Worse Survival in Patients with Liver Cirrhosis. J. Cachexia Sarcopenia Muscle 2017, 8, 915–925. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO) EASL-EASD-EASO Clinical Practice Guidelines for the Management of Non-Alcoholic Fatty Liver Disease. J. Hepatol. 2016, 64, 1388–1402. [CrossRef]
| Parameter | Patients with MASLD and HTN (n = 67) |
|---|---|
| Gender: female, n% | 43 (64.2) |
| Age, years | 58 (51–65) |
| BMI, kg/m2 | 33.2 (30.4–36.9) |
| Normal weight (18.5 ≤ BMI < 25 kg/m2), n (%) | 2 (2.9) |
| Overweight (25 ≤ BMI < 30 kg/m2) | 13 (19.4) |
| Obesity (BMI ≥ 30 kg/m2) | 52 (77.6) |
| Waist circumference (all subjects), cm | 106.5 (102–113.2) |
| Waist circumference (male), cm | 108 (106–116.5) |
| Waist circumference (female), cm | 106 (100–112.3) |
| Hip circumference, cm | 114 (109–119) |
| Parameter | Patients with MASLD and HTN (n = 67) |
|---|---|
| Erythrocytes, 1012/L | 4.7 (4.41–4.9) |
| Hemoglobin, g/L | 145 (133–151) |
| ESR, mm/h | 9 (4–14) |
| Platelets, 109/L | 245 (210–286) |
| Leukocytes, 109/L | 6.1 (5.3–7.2) |
| ALT, IU/L | 23 (17–38) |
| AST, IU/L | 22 (18–26) |
| GGT, IU/L | 31.5 (21–46.3) |
| Albumin, g/dL | 4.5 (4.4–4.7) |
| Total bilirubin, μmol/L | 12 (9–15) |
| Uric acid, μmol/L | 6 (5.3–7) |
| CRP, mg/L | 2.7 (1.4–5.5) |
| Total cholesterol, mmol/L | 5.8 (5.1–6.2) |
| Triglycerides, mmol/L | 1.43 (1.04–2.04) |
| Creatinine, μmol/L | 74 (68–88) |
| Glucose, mmol/L | 5.7 (5.4–6.1) |
| HOMA-IR > 2.7, n (%) | 47 (70.1) |
| Liver stiffness, kPa (pSWE) | 5.1 (4.1–6.3) |
| Category of Pharmaceutical Drugs | Number of Patients with MASLD and HTN, n (%) |
|---|---|
| Calcium channel blockers | 1 (1.5) |
| Beta blockers | 4 (5.9) |
| Angiotensin receptor blockers | 8 (11.8) |
| ACE inhibitors | 5 (7.4) |
| Combination antihypertensive therapy | 31 (45.6) |
| Myokine | Median Concentration | IQR |
|---|---|---|
| Irisin (all patients), µg/mL | 6.04 | 5.1–7.3 |
| Irisin (men), µg/mL | 6.1 | 5.7–8.1 |
| Irisin (women), µg/mL | 6.0 | 4.49–7.2 |
| Myonectin (all patients), pg/mL | 0.0 | 0.0–78.5 |
| Myonectin (men), pg/mL | 0.0 | 0.0–82.8 |
| Myonectin (women), pg/mL | 0.0 | 0.0–75.3 |
| Myostatin (all patients), ng/mL | 4.6 | 3.4–5.8 |
| Myostatin (men), ng/mL | 4.2 | 2.9–5.7 |
| Myostatin (women), ng/mL | 4.9 | 3.6–5.9 |
| Parameter | Serum Irisin Concentration in Patients with MASLD and HTN, μg/mL | Serum Myostatin Concentration in Patients with MASLD and HTN, ng/mL | ||||
|---|---|---|---|---|---|---|
| <6.1 (n = 31) | ≥6.1 (n = 30) | p | <4.98 (n = 37) | ≥4.98 (n = 30) | p | |
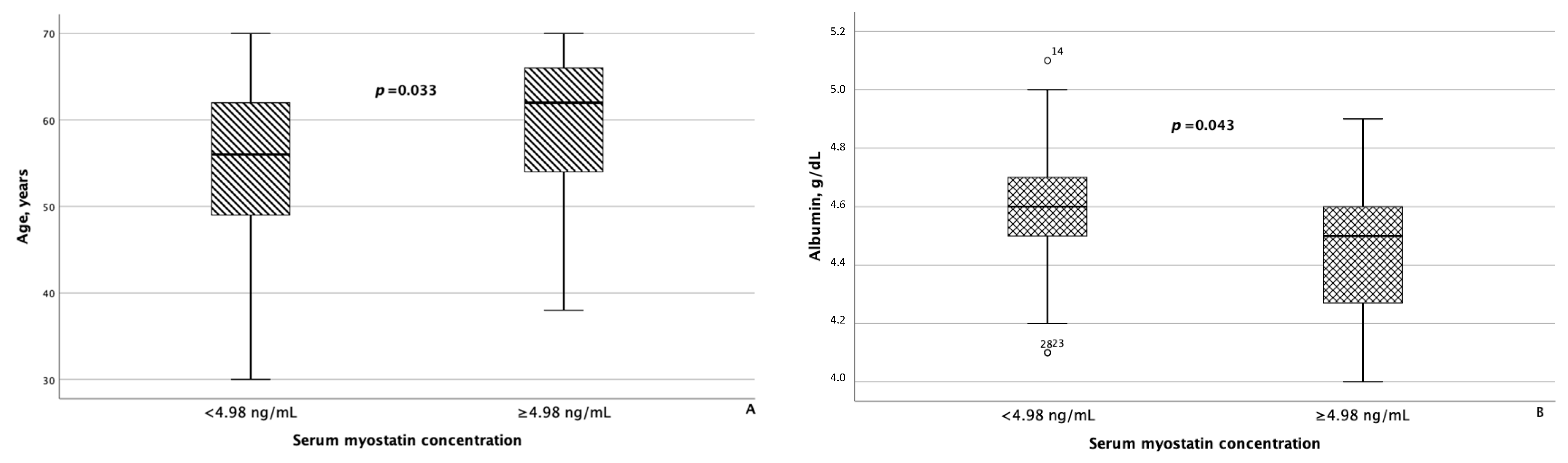
| Age, years | 59 (53–64) | 60 (49–66) | n/s | 56 (47.5–62.5) | 62 (53.5–66) | 0.033 |
| Gender: female, n (%) | 22 (70.9) | 18 (60) | n/s | 22 (59.5) | 20 (66.7) | n/s |
| BMI, kg/m2 | 33 (30.8–36.9) | 33.9 (29.5–37.2) | n/s | 33.1 (30.8–36.7) | 33.6 (30.1–36.9) | n/s |
| HTN, n (%): | n/s | n/s | ||||
| Grade 1 | 11 (35.5) | 8 (26.7) | 11 (29.7) | 10 (33.3) | ||
| Grade 2 | 11 (35.5) | 9 (30) | 13 (35.1) | 9 (30) | ||
| Grade 3 | 9 (29) | 13 (43.3) | 13 (35.1) | 11 (36.7) | ||
| T2D, n (%) | 5 (16.1) | 2 (6.7) | n/s | 5 (13.5) | 2 (6.7) | n/s |
| IFG, n (%) | 7 (22.6) | 2 (6.7) | n/s | 4 (10.8) | 5 (16.7) | n/s |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheptulina, A.F.; Mamutova, E.M.; Elkina, A.Y.; Timofeev, Y.S.; Metelskaya, V.A.; Kiselev, A.R.; Drapkina, O.M. Serum Irisin, Myostatin, and Myonectin Correlate with Metabolic Health Markers, Liver Disease Progression, and Blood Pressure in Patients with Metabolic Dysfunction-Associated Fatty Liver Disease and Hypertension. Metabolites 2024, 14, 584. https://doi.org/10.3390/metabo14110584
Sheptulina AF, Mamutova EM, Elkina AY, Timofeev YS, Metelskaya VA, Kiselev AR, Drapkina OM. Serum Irisin, Myostatin, and Myonectin Correlate with Metabolic Health Markers, Liver Disease Progression, and Blood Pressure in Patients with Metabolic Dysfunction-Associated Fatty Liver Disease and Hypertension. Metabolites. 2024; 14(11):584. https://doi.org/10.3390/metabo14110584
Chicago/Turabian StyleSheptulina, Anna F., Elvira M. Mamutova, Anastasia Yu. Elkina, Yuriy S. Timofeev, Victoria A. Metelskaya, Anton R. Kiselev, and Oxana M. Drapkina. 2024. "Serum Irisin, Myostatin, and Myonectin Correlate with Metabolic Health Markers, Liver Disease Progression, and Blood Pressure in Patients with Metabolic Dysfunction-Associated Fatty Liver Disease and Hypertension" Metabolites 14, no. 11: 584. https://doi.org/10.3390/metabo14110584
APA StyleSheptulina, A. F., Mamutova, E. M., Elkina, A. Y., Timofeev, Y. S., Metelskaya, V. A., Kiselev, A. R., & Drapkina, O. M. (2024). Serum Irisin, Myostatin, and Myonectin Correlate with Metabolic Health Markers, Liver Disease Progression, and Blood Pressure in Patients with Metabolic Dysfunction-Associated Fatty Liver Disease and Hypertension. Metabolites, 14(11), 584. https://doi.org/10.3390/metabo14110584







