Healing of Experimental Periodontal Defects Following Treatment with Fibroblast Growth Factor-2 and Deproteinized Bovine Bone Mineral
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Biomolecules and Materials
2.3. In Vivo Experimental Design and Surgical Procedures
2.4. Microcomputed Tomography Analysis
2.5. Histological Analysis
2.6. Histomorphometric Analysis
2.7. Immunohistochemistry
2.8. In Vitro Cell Culture
2.9. Enzyme-Linked Immunosorbent Assay and Confocal Laser Scanning Microscopy
2.10. Cell Viability/Proliferation Assay
2.11. Assessment of Cell Morphology and Spreading
2.12. Alkaline Phosphatase (ALP) and Alizarin Red Staining
2.13. Statistical Analysis
3. Results
3.1. Micro-CT Analysis
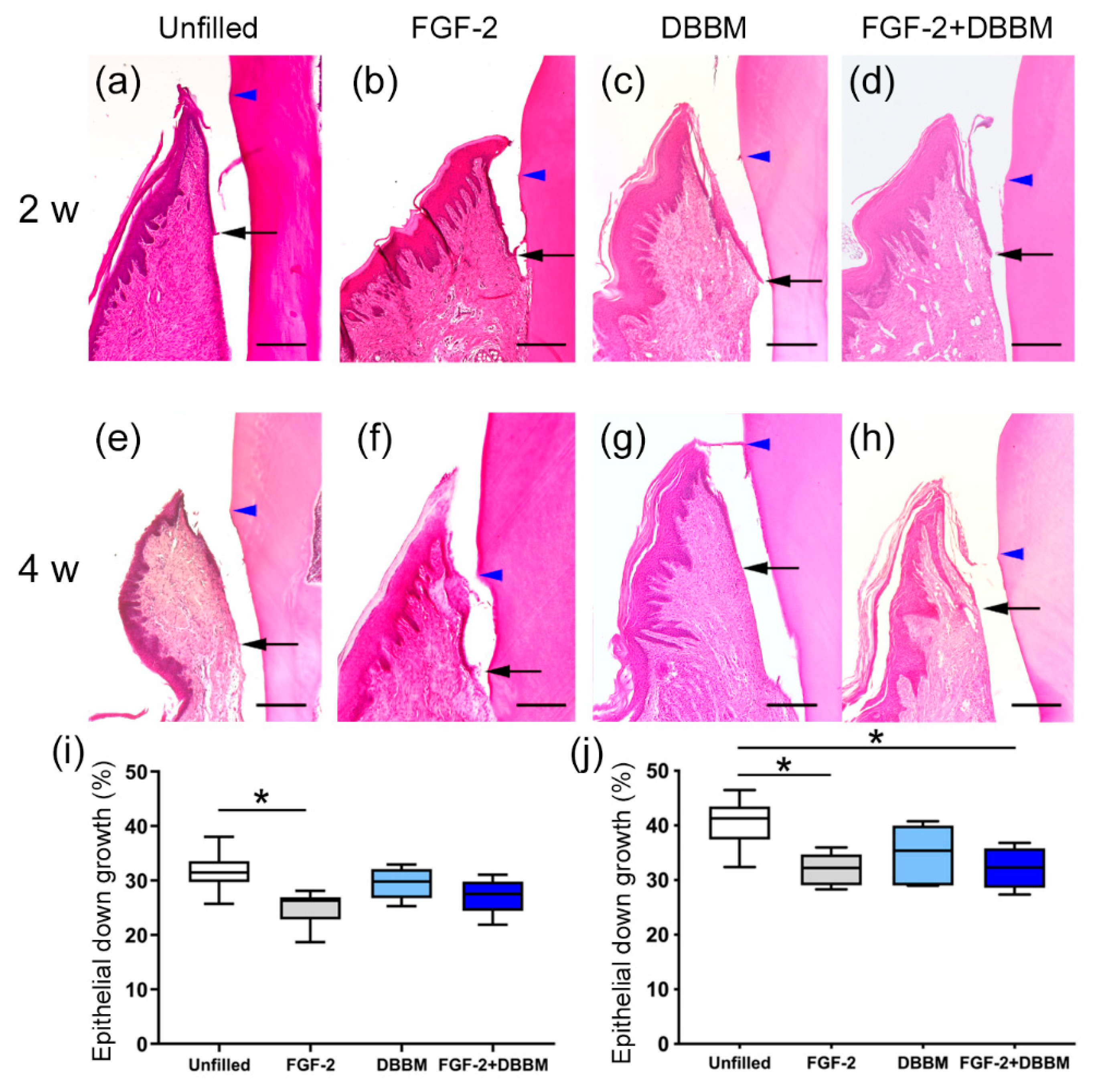
3.2. Histological Analysis
3.3. Histomorphometric Analysis
3.4. Immunohistochemical Analyses
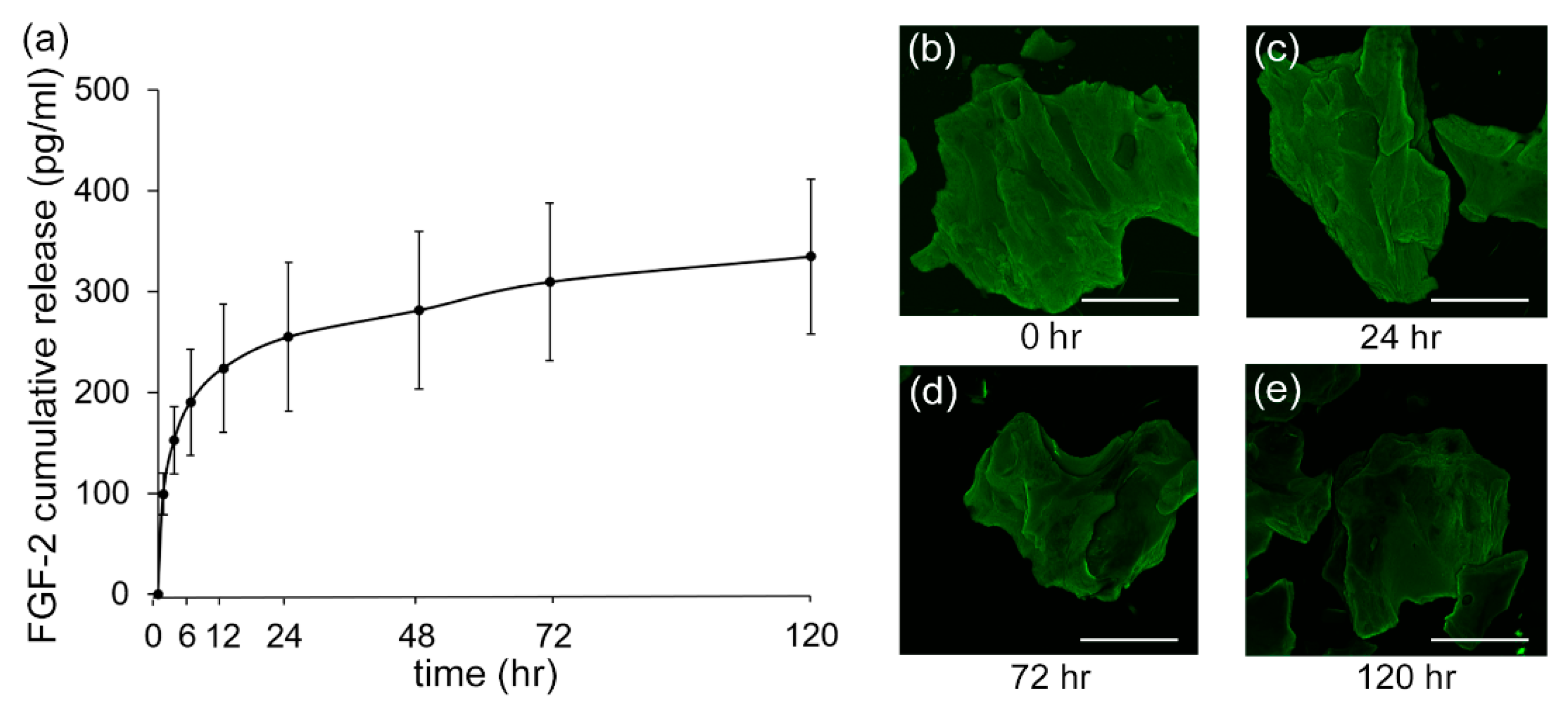
3.5. Release Kinetics of FGF-2
3.6. Cell Viability/Proliferation
3.7. Cell Morphology and Behavior
3.8. ALP Activity and Alizarin Red Staining
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bartold, P.M.; Gronthos, S.; Ivanovski, S.; Fisher, A.; Hutmacher, D.W. Tissue engineered periodontal products. J. Periodontal Res. 2016, 51, 1–15. [Google Scholar] [CrossRef]
- Seo, B.M.; Miura, M.; Gronthos, S.; Bartold, P.M.; Batouli, S.; Brahim, J.; Young, M.; Robey, P.G.; Wang, C.; Shi, S. Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet 2004, 364, 149–155. [Google Scholar] [CrossRef]
- Shimono, M.; Ishikawa, T.; Ishikawa, H.; Matsuzaki, H.; Hashimoto, S.; Muramatsu, T.; Shima, K.; Matsuzaka, K.; Inoue, T. Regulatory mechanisms of periodontal regeneration. Microsc. Res. Tech. 2003, 60, 491–502. [Google Scholar] [CrossRef]
- Shimabukuro, Y.; Terashima, H.; Takedachi, M.; Maeda, K.; Nakamura, T.; Sawada, K.; Kobashi, M.; Awata, T.; Oohara, H.; Kawahara, T.; et al. Fibroblast growth factor-2 stimulates directed migration of periodontal ligament cells via PI3K/AKT signaling and CD44/hyaluronan interaction. J. Cell. Physiol. 2011, 226, 809–821. [Google Scholar] [CrossRef]
- Murakami, S. Periodontal tissue regeneration by signaling molecule(s): What role does basic fibroblast growth factor (FGF-2) have in periodontal therapy? Periodontol. 2000 2011, 56, 188–208. [Google Scholar] [CrossRef] [PubMed]
- Takayama, S.; Murakami, S.; Shimabukuro, Y.; Kitamura, M.; Okada, H. Periodontal regeneration by FGF-2 (bFGF) in primate models. J. Dent. Res. 2001, 80, 2075–2079. [Google Scholar] [CrossRef] [PubMed]
- Murakami, S.; Takayama, S.; Kitamura, M.; Shimabukuro, Y.; Yanagi, K.; Ikezawa, K.; Okada, H. Recombinant human basic fibroblast growth factor (bFGF) stimulates periodontal regeneration in class II furcation defects created in beagle dogs. J. Periodontal Res. 2003, 38, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Nagayasu-Tanaka, T.; Anzai, J.; Takaki, S.; Shiraishi, N.; Terashima, A.; Asano, T.; Nozaki, T.; Kitamura, M.; Murakami, S. Action mechanism of fibroblast growth factor-2 (FGF-2) in the promotion of periodontal regeneration in beagle dogs. PLoS ONE 2015, 10, e0131870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitamura, M.; Akamatsu, M.; Kawanami, M.; Furuichi, Y.; Fujii, T.; Mori, M.; Kunimatsu, K.; Shimauchi, H.; Ogata, Y.; Yamamoto, M.; et al. Randomized placebo-controlled and controlled non-inferiority Phase III trials comparing trafermin, a recombinant human fibroblast growth factor 2, and enamel matrix derivative in periodontal regeneration in intrabony defects. J. Bone Miner. Res. 2016, 31, 806–814. [Google Scholar] [CrossRef]
- Kitamura, M.; Akamatsu, M.; Machigashira, M.; Hara, Y.; Sakagami, R.; Hirofuji, T.; Hamachi, T.; Maeda, K.; Yokota, M.; Kido, J.; et al. FGF-2 stimulates periodontal regeneration: Results of a multi-center randomized clinical trial. J. Dent. Res. 2011, 90, 35–40. [Google Scholar] [CrossRef]
- Kitamura, M.; Nakashima, K.; Kowashi, Y.; Fujii, T.; Shimauchi, H.; Sasano, T.; Furuuchi, T.; Fukuda, M.; Noguchi, T.; Shibutani, Y.; et al. Periodontal tissue regeneration using fibroblast growth factor -2: Randomized controlled phase II clinical trial. PLoS ONE 2008, 3, e2611. [Google Scholar] [CrossRef]
- Saito, A.; Bizenjima, T.; Takeuchi, T.; Suzuki, E.; Sato, M.; Yoshikawa, K.; Kitamura, Y.; Matsugami, D.; Aoki, H.; Kita, D.; et al. Treatment of intrabony periodontal defects using rhFGF-2 in combination with deproteinized bovine bone mineral or rhFGF-2 alone: A 6-month randomized controlled trial. J. Clin. Periodontol. 2019, 46, 332–341. [Google Scholar] [CrossRef] [PubMed]
- Richardson, C.R.; Mellonig, J.T.; Brunsvold, M.A.; McDonnell, H.T.; Cochran, D.L. Clinical evaluation of Bio-Oss: A bovine-derived xenograft for the treatment of periodontal osseous defects in humans. J. Clin. Periodontol. 1999, 26, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, A.; Karring, T. Five-year results of guided tissue regeneration in combination with deproteinized bovine bone (Bio-Oss) in the treatment of intrabony periodontal defects: A case series report. Clin. Oral Investig. 2005, 9, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Jensen, T.; Schou, S.; Stavropoulos, A.; Terheyden, H.; Holmstrup, P. Maxillary sinus floor augmentation with Bio-Oss or Bio-Oss mixed with autogenous bone as graft in animals: A systematic review. Clin. Oral Implant. Res. 2012, 23, 263–273. [Google Scholar] [CrossRef]
- Yamamoto, S.; Masuda, H.; Shibukawa, Y.; Yamada, S. Combination of bovinederived xenografts and enamel matrix derivative in the treatment of intrabony periodontal defects in dogs. Int. J. Periodontics Restor. Dent. 2007, 27, 471–479. [Google Scholar]
- Shahriari, S.; Houshmand, B.; Razavian, H.; Khazaei, S.; Abbas, F.M. Effect of the combination of enamel matrix derivatives and deproteinized bovine bone materials on bone formation in rabbits’ calvarial defects. J. Dent. Res. 2012, 9, 422–426. [Google Scholar]
- Miron, R.J.; Wei, L.; Bosshardt, D.D.; Buser, D.; Sculean, A.; Zhang, Y. Effects of enamel matrix proteins in combination with a bovine-derived natural bone mineral for the repair of bone defects. Clin. Oral Investig. 2014, 18, 471–478. [Google Scholar] [CrossRef]
- Oi, Y.; Ota, M.; Yamamoto, S.; Shibukawa, Y.; Yamada, S. Beta-tricalcium phosphate and basic fibroblast growth factor combination enhances periodontal regeneration in intrabony defects in dogs. Dent. Mater. J. 2009, 28, 162–169. [Google Scholar] [CrossRef]
- Anzai, J.; Kitamura, M.; Nozaki, T.; Nagayasu, T.; Terashima, A.; Asano, T.; Murakami, S. Effects of concomitant use of fibroblast growth factor (FGF)-2 with beta-tricalcium phosphate (β-TCP) on the beagle dog 1-wall periodontal defect model. Biochem. Biophys. Res. Commun. 2010, 403, 345–350. [Google Scholar] [CrossRef]
- Aoki, H.; Bizenjima, T.; Seshima, F.; Sato, M.; Irokawa, D.; Yoshikawa, K.; Yoshida, Y.; Imamura, K.; Matsugami, D.; Kitamura, Y.; et al. Periodontal surgery using rhFGF-2 with deproteinized bovine bone mineral or rhFGF-2 alone: 2-year follow-up of a randomized controlled trial. J. Clin. Periodontol. 2021, 48, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Klein, Y.; Fleissig, O.; Stabholz, A.; Chaushu, S.; Polak, D. Bone regeneration with bovine bone impairs orthodontic tooth movement despite proper osseous wound healing in a novel mouse model. J. Periodontol. 2018, 90, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Oortgiesen, D.A.; Plachokova, A.S.; Geenen, C.; Meijer, G.J.; Walboomers, X.F.; Van den Beucken, J.J.; Jansen, J.A. Alkaline phosphatase immobilization onto Bio-Gide® and Bio-Oss® for periodontal and bone regeneration. J. Clin. Periodontol. 2012, 39, 546–555. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, W.; Matsugami, D.; Murakami, T.; Bizenjima, T.; Imamura, K.; Seshima, F.; Saito, A. Combined effects of systemic parathyroid hormone (1-34) and locally delivered neutral self-assembling peptide hydrogel in the treatment of periodontal defects: An experimental in vivo investigation. J. Clin. Periodontol. 2019, 46, 1030–1040. [Google Scholar] [CrossRef] [PubMed]
- Arima, Y.; Uemura, N.; Hashimoto, Y.; Baba, S.; Matsumoto, N. Evaluation of bone regeneration by porous alpha-tricalcium phosphate/atelocollagen sponge composite in rat calvarial defects. J. Hard. Tissue Biol. 2013, 25, 35–40. [Google Scholar] [CrossRef]
- Zhang, P.; Ding, L.; Kasugai, S. Effect of doxycycline doped bone substitute on vertical bone augmentation on rat calvaria. Dent. Mater. J. 2019, 38, 211–217. [Google Scholar] [CrossRef] [Green Version]
- Takeda, Y.; Honda, Y.; Kakinoki, S.; Yamaoka, T.; Baba, S. Surface modification of porous alpha-tricalcium phosphate granules with heparin enhanced their early osteogenic capability in a rat calvarial defect model. Dent. Mater. J. 2018, 37, 575–581. [Google Scholar] [CrossRef] [Green Version]
- Takeuchi, T.; Bizenjima, T.; Ishii, Y.; Imamura, K.; Suzuki, E.; Seshima, F.; Saito, A. Enhanced healing of surgical periodontal defects in rats following application of a self-assembling peptide nanofibre hydrogel. J. Clin. Periodontol. 2016, 43, 279–288. [Google Scholar] [CrossRef]
- Bizenjima, T.; Seshima, F.; Ishizuka, Y.; Takeuchi, T.; Kinumatsu, T.; Saito, A. Fibroblast growth factor-2 promotes healing of surgically created periodontal defects in rats with early, streptozotocin-induced diabetes via increasing cell proliferation and regulating angiogenesis. J. Clin. Periodontol. 2015, 42, 62–71. [Google Scholar] [CrossRef]
- Park, C.H.; Rios, H.F.; Jin, Q.; Sugai, J.V.; Padial-Molina, M.; Taut, A.D.; Flanagan, C.L.; Hollister, S.J.; Giannobile, W.V. Tissue engineering bone-ligament complexes using fiber-guiding scaffolds. Biomaterials 2012, 33, 137–145. [Google Scholar] [CrossRef] [Green Version]
- Lucarini, G.; Zizzi, A.; Aspriello, S.D.; Ferrante, L.; Tosco, E.; Muzio, L.L.; Foglini, P.; Mattioli-Belmonte, M.; Primio, R.D.; Piemontese, M. Involvement of vascular endothelial growth factor, CD44 and CD133 in periodontal disease and diabetes: An immunohistochemical study. J. Clin. Periodontol. 2009, 36, 3–10. [Google Scholar] [CrossRef]
- Matsugami, D.; Murakami, T.; Yoshida, Y.; Imamura, K.; Bizenjima, T.; Seshima, F.; Saito, A. Treatment with functionalized designer self-assembling peptide hydrogels promotes healing of experimental periodontal defects. J. Periodontal Res. 2021, 56, 162–172. [Google Scholar] [CrossRef] [PubMed]
- Inoue, T.; Deporter, D.A.; Melcher, A.H. Induction of chondrogenesis in muscle, skin, bone marrow, and periodontal ligament by demineralized dentin and bone matrix in vivo and in vitro. J. Dent. Res. 1986, 65, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, I.; Sawada, R.; Kato, Y.; Tsuji, K.; Shao, J.; Yamada, T.; Kato, R.; Tsuchiya, T. Effectivity of the novel serum-free medium STK2 for proliferating human mesenchymal stem cells. Yakugaku Zasshi. 2009, 129, 381–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Draenert, F.G.; Nonnenmacher, A.L.; Kämmerer, P.W.; Goldschmitt, J.; Wagner, W. BMP-2 and bFGF release and in vitro effect on human osteoblasts after adsorption to bone grafts and biomaterials. Clin. Oral Implant. Res. 2013, 24, 750–757. [Google Scholar] [CrossRef]
- Huh, J.B.; Yang, J.J.; Choi, K.H.; Bae, J.H.; Lee, J.Y.; Kim, S.E.; Shin, S.W. Effect of rhBMP-2 immobilized anorganic bovine bone matrix on bone regeneration. Int. J. Mol. Sci. 2015, 16, 16034–16052. [Google Scholar] [CrossRef] [Green Version]
- Fujioka-Kobayashi, M.; Sawada, K.; Kobayashi, E.; Schaller, B.; Zhang, Y.; Miron, R.J. Osteogenic potential of rhBMP9 combined with a bovine-derived natural bone mineral scaffold compared to rhBMP2. Clin. Oral Implant. Res. 2017, 28, 381–387. [Google Scholar] [CrossRef]
- Park, J.W.; Ko, H.J.; Jang, J.H.; Kang, H.; Suh, J.Y. Increased new bone formation with a surface magnesium-incorporated deproteinized porcine bone substitute in rabbit calvarial defects. J. Biomed. Mater. Res. A 2012, 100, 834–840. [Google Scholar] [CrossRef] [PubMed]
- Klinge, B.; Alberius, P.; Isaksson, S.; Jönsson, J. Osseous response to implanted natural bone mineral and synthetic hydroxylapatite ceramic in the repair of experimental skull bone defects. J. Oral Maxillofac. Surg. 1992, 50, 241–249. [Google Scholar] [CrossRef]
- Tovar, N.; Jimbo, R.; Gangolli, R.; Perez, L.; Manne, L.; Yoo, D.; Lorenzoni, F.; Witek, L.; Coelho, P.G. Evaluation of bone response to various anorganic bovine bone xenografts: An experimental calvaria defect study. Int. J. Oral Maxillofac. Surg. 2014, 43, 251–260. [Google Scholar] [CrossRef]
- Dvorak, H.F.; Brown, L.F.; Detmar, M.; Dvorak, A.M. Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am. J. Pathol. 1995, 146, 1029–1039. [Google Scholar]
- Takayama, S.; Yoshida, J.; Hirano, H.; Okada, H.; Murakami, S. Effects of basic fibroblast growth factor on human gingival epithelial cells. J. Clin. Periodontol. 2002, 73, 1467–1473. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, K.; Zhou, X.; Kunkel, G.; Zhang, Z.; Deng, J.M.; Behringer, R.R.; Crombrugghe, B.D. The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell 2002, 108, 17–29. [Google Scholar] [CrossRef] [Green Version]
- Murakami, Y.; Kojima, T.; Nagasawa, T.; Kobayashi, H.; Ishikawa, I. Novel isolation of alkaline phosphatase-positive subpopulation from periodontal ligament fibroblasts. J. Periodontol. 2003, 74, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Barbeck, M.; Udeabor, S.E.; Lorenz, J.; Kubesch, A.; Choukroun, J.; Sader, R.A.; Kirkpatrick, C.J.; Ghanaati, S. Induction of multinucleated giant cells in response to small sized bovine bone substitute (Bio-Oss™) results in an enhanced early implantation bed vascularization. Ann. Maxillofac. Surg. 2014, 4, 150–157. [Google Scholar] [PubMed] [Green Version]
- Kangwannarongkul, T.; Subbalekha, K.; Vivatbutsiri, P.; Suwanwela, J. Gene expression and microcomputed tomography analysis of grafted bone using deproteinized bovine bone and freeze-dried human bone. Int. J. Oral Maxillofac Implant. 2018, 33, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Takayama, S.; Murakami, S.; Miki, Y.; Ikezawa, K.; Tasaka, S.; Terashima, A.; Asano, T.; Okada, H. Effects of basic fibroblast growth factor on human periodontal ligament cells. J. Periodontal Res. 1997, 32, 667–675. [Google Scholar] [CrossRef]
- Marković, D.; Karadzic, I.; Jokanović, V.; Vukovic, A. Biological aspects of application of nanomaterials in tissue engineering. Chem. Ind. Chem. Eng. Q. 2016, 22, 145–153. [Google Scholar] [CrossRef]
- Lozano, D.; Feito, M.J.; Sergio, P.N.; Lozano, R.M.; Matesanz, M.C.; Serrano, M.C.; María, V.; Portolés, M.T.; Esbrit, P. Osteostatin improves the osteogenic activity of fibroblast growth factor-2 immobilized in Si-doped hydroxyapatite in osteoblastic cells. Acta Biomater. 2012, 8, 2770–2777. [Google Scholar] [CrossRef] [PubMed]
- Masuoka, K.; Ishihara, M.; Asazuma, T.; Hattori, H.; Matsui, T.; Takase, B.; Kanatani, Y.; Fujita, M.; Saito, Y.; Yura, H.; et al. The interaction of chitosan with fibroblast growth factor-2 and its protection from inactivation. Biomaterials 2005, 26, 3277–3284. [Google Scholar] [CrossRef]
- Kawaguchi, H.; Kurokawa, T.; Hanada, K.; Hiyama, Y.; Tamura, M.; Ogata, E.; Matsumoto, T. Stimulation of fracture repair by recombinant human basic fibroblast growth factor in normal and streptozotocin-diabetic rats. Endocrinology 1994, 135, 774–781. [Google Scholar] [CrossRef]
- Santana, R.B.; Trackman, P.C. Controlled release of fibroblast growth factor 2 stimulates bone healing in an animal model of diabetes mellitus. Int. J. Oral Maxillofac Implant. 2006, 21, 711–718. [Google Scholar]
- Miron, R.J.; Caluseru, O.M.; Guillemette, V.; Zhang, Y.; Buser, D.; Chandad, F.; Sculean, A. Effect of bone graft density on in vitro cell behavior with enamel matrix derivative. Clin. Oral Investig. 2015, 19, 1643–1651. [Google Scholar] [CrossRef] [PubMed]
- Miron, R.J.; Bosshardt, D.D.; Buser, D.; Zhang, Y.; Tugulu, S.; Gemperli, A.; Dard, M.; Caluseru, O.M.; Chandad, F.; Sculean, A. Comparison of the capacity of enamel matrix derivative gel and enamel matrix derivative in liquid formulation to adsorb to bone grafting materials. J. Periodontol. 2015, 86, 578–587. [Google Scholar] [CrossRef] [PubMed]
- Protivínský, J.; Appleford, M.; Strnad, J.; Helebrant, A. Effect of chemically modified titanium surfaces on protein adsorption and osteoblast precursor cell Behavior. Int. J. Oral Maxillofac. Implant. 2007, 22, 542–550. [Google Scholar]
- Cortellini, P.; Tonetti, M.S. Focus on intrabony defects: Guided tissue regeneration. Periodontol. 2000 2000, 22, 104–132. [Google Scholar] [CrossRef]
- Reynolds, M.A.; Kao, R.T.; Nares, S.; Camargo, P.M.; Caton, J.G.; Clem, D.S.; Fiorellini, J.P.; Geisinger, M.L.; Mills, M.P.; Nevins, M.P.; et al. Periodontal regeneration—Intrabony defects: Practical applications from the AAP Regeneration Workshop. Clin. Adv. Periodontics 2015, 5, 21–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]





| Area/Group | Unfilled | FGF-2 | DBBM | FGF-2 + DBBM | ||
|---|---|---|---|---|---|---|
| PCNA | 2 w | Root side | 20.5 ± 3.1 * | 44.9 ± 9.7 a | 29.6 ± 6.6 | 46.1 ± 6.5 a |
| Bone side | 18.6 ± 3.0 | 33.1 ± 5.8 a | 27.2 ± 5.0 | 34.5 ± 4.3 a | ||
| Middle area | 15.7 ± 2.4 | 31.3 ± 7.0 | 37.3 ± 2.8 a,† | 39.3 ± 9.8 a | ||
| 4 w | Root side | 18.3 ± 7.0 | 16.2 ± 4.6 | 16.3 ± 4.7 | 17.6 ± 5.3 | |
| Bone side | 15.6 ± 5.2 | 14.1 ± 8.8 | 16.6 ± 4.6 | 13.6 ± 2.7 | ||
| Middle area | 14.0 ± 3.1 | 10.1 ± 3.9 | 16.1 ± 4.1 | 16.9 ± 5.3 | ||
| VEGF | 2 w | Root side | 7.7 ± 1.9 | 18.2 ± 3.7 a | 13.9 ± 4.6 | 19.0 ± 4.2 a |
| Bone side | 6.7 ± 2.9 | 17.3 ± 3.0 a | 12.5 ± 5.0 | 18.0 ± 3.4 a | ||
| Middle area | 7.1 ± 2.2 | 15.3 ± 3.6 a | 16.0 ± 4.0 a | 19.0 ± 6.1 a | ||
| 4 w | Root side | 8.8 ± 3.1 | 11.7 ± 5.3 | 9.9 ± 3.2 | 11.1 ± 3.5 | |
| Bone side | 8.3 ± 2.9 | 7.4 ± 3.3 | 9.5 ± 2.3 | 11.0 ± 3.6 | ||
| Middle area | 9.2 ± 3.0 | 8.3 ± 4.6 | 12.3 ± 2.0 | 13.7 ± 3.4 | ||
| Osx | 2 w | Root side | 8.4 ± 2.7 * | 18.8 ± 5.4 a,* | 13.3 ± 3.6 * | 19.6 ± 7.9 a,* |
| Bone side | 4.8 ± 1.9 | 9.8 ± 2.7 a | 7.8 ± 1.4 | 9.4 ± 1.0 a | ||
| Middle area | 0.2 ± 0.2 | 0.6 ± 0.8 | 7.1 ± 2.9 a,b | 8.0 ± 2.4 a,b | ||
| 4 w | Root side | 19.6 ± 5.9 * | 14.6 ± 4.4 * | 19.7 ± 4.6 *,† | 17.2 ± 4.7 * | |
| Bone side | 8.6 ± 5.2 | 8.8 ± 3.4 | 9.1 ± 4.1 | 9.4 ± 2.9 | ||
| Middle area | 0.1 ± 0.2 | 0.6 ± 1.1 | 7.4 ± 4.2 a,b | 6.6 ± 2.3 a,b | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murakami, T.; Matsugami, D.; Yoshida, W.; Imamura, K.; Bizenjima, T.; Seshima, F.; Saito, A. Healing of Experimental Periodontal Defects Following Treatment with Fibroblast Growth Factor-2 and Deproteinized Bovine Bone Mineral. Biomolecules 2021, 11, 805. https://doi.org/10.3390/biom11060805
Murakami T, Matsugami D, Yoshida W, Imamura K, Bizenjima T, Seshima F, Saito A. Healing of Experimental Periodontal Defects Following Treatment with Fibroblast Growth Factor-2 and Deproteinized Bovine Bone Mineral. Biomolecules. 2021; 11(6):805. https://doi.org/10.3390/biom11060805
Chicago/Turabian StyleMurakami, Tasuku, Daisuke Matsugami, Wataru Yoshida, Kentaro Imamura, Takahiro Bizenjima, Fumi Seshima, and Atsushi Saito. 2021. "Healing of Experimental Periodontal Defects Following Treatment with Fibroblast Growth Factor-2 and Deproteinized Bovine Bone Mineral" Biomolecules 11, no. 6: 805. https://doi.org/10.3390/biom11060805
APA StyleMurakami, T., Matsugami, D., Yoshida, W., Imamura, K., Bizenjima, T., Seshima, F., & Saito, A. (2021). Healing of Experimental Periodontal Defects Following Treatment with Fibroblast Growth Factor-2 and Deproteinized Bovine Bone Mineral. Biomolecules, 11(6), 805. https://doi.org/10.3390/biom11060805







