Current and Novel Therapeutic Approaches for Treatment of Neovascular Age-Related Macular Degeneration
Abstract
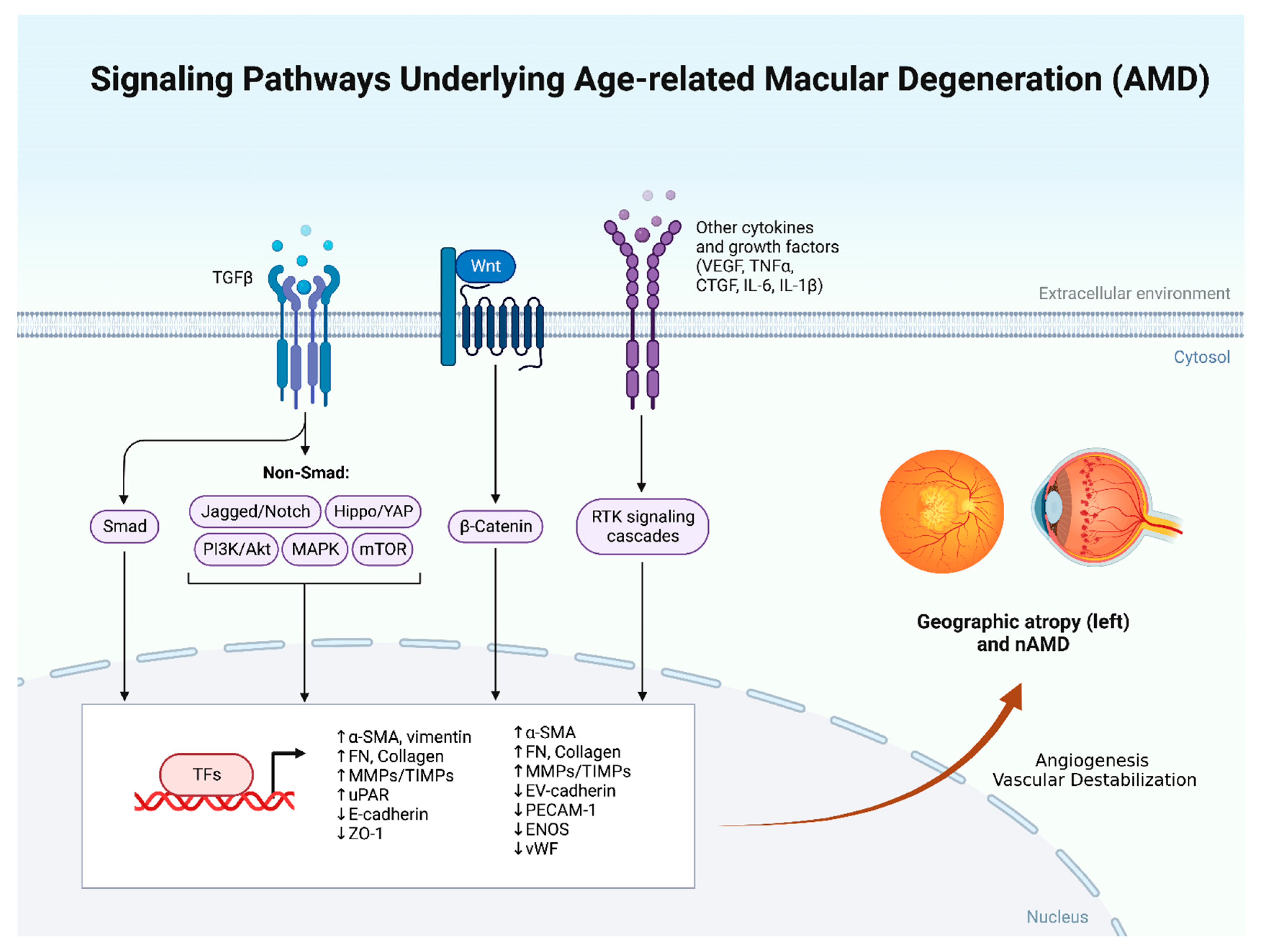
:1. Introduction
2. Laser Therapy
3. Photodynamic Therapy
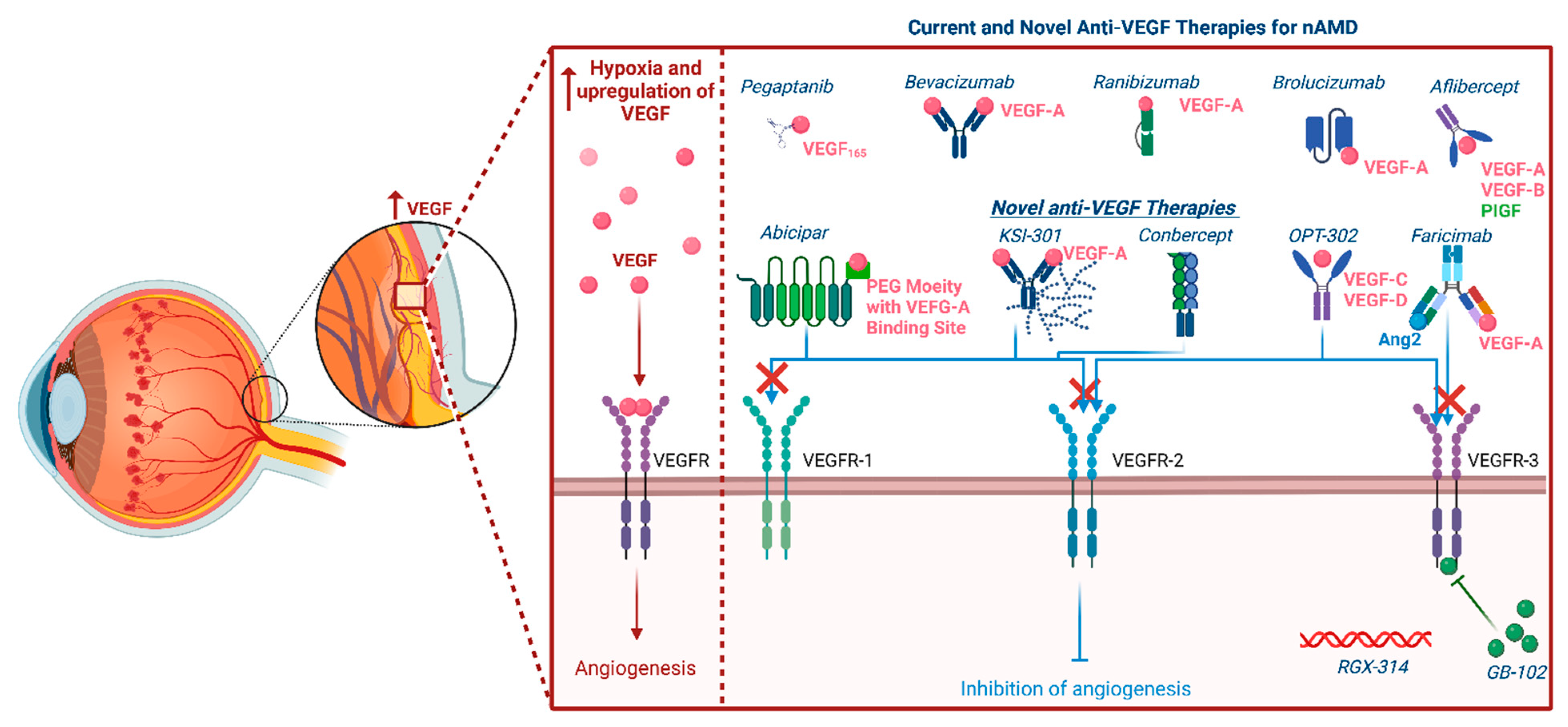
4. Pegaptanib
5. Bevacizumab
6. Ranibizumab
7. Aflibercept
8. Brolucizumab
9. Newer Anti-VEGF Medications
10. Ranibizumab Portal Delivery System
11. Abicipar Pegol
12. Faricimab
13. KSI-301
14. OPT-302
15. GB-102
16. RGX-314
17. PAN-90806
18. ICON-1
19. Conbercept
20. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smith, W.; Assink, J.; Klein, R.; Mitchell, P.; Klaver, C.C.; Klein, B.E.; Hofman, A.; Jensen, S.; Wang, J.J.; T de Jong, P. Risk factors for age-related macular degeneration: Pooled findings from three continents. Ophthalmology 2001, 108, 697–704. [Google Scholar] [CrossRef]
- Brown, G.C.; Brown, M.M.; Sharma, S.; Stein, J.D.; Roth, Z.; Campanella, J.; Beauchamp, G.R. The burden of age-related macular degeneration: A value-based medicine analysis. Trans. Am. Ophthalmol. Soc. 2005, 103, 173-84; discussion 184-6. [Google Scholar] [CrossRef]
- Bakri, S.J.; Thorne, J.E.; Ho, A.C.; Ehlers, J.P.; Schoenberger, S.D.; Yeh, S.; Kim, S.J. Safety and Efficacy of Anti-Vascular Endothelial Growth Factor Therapies for Neovascular Age-Related Macular Degeneration: A Report by the American Academy of Ophthalmology. Ophthalmology 2019, 126, 55–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shao, J.; Choudhary, M.M.; Schachat, A.P. Neovascular Age-Related Macular Degeneration. Dev. Ophthalmol. 2016, 55, 125–136. [Google Scholar] [CrossRef]
- Olsson, A.K.; Dimberg, A.; Kreuger, J.; Claesson-Welsh, L. VEGF receptor signalling—In control of vascular function. Nat. Rev. Mol. Cell Biol. 2006, 7, 359–371. [Google Scholar] [CrossRef] [PubMed]
- Breen, E.C. VEGF in biological control. J. Cell Biochem. 2007, 102, 1358–1367. [Google Scholar] [CrossRef]
- Handa, J.T.; Bowes Rickman, C.; Dick, A.D.; Gorin, A.B.; Miller, J.W.; Toth, C.A.; Ueffing, M.; Zarbin, M.; Farrer, L.A. A systems biology approach towards understanding and treating non-neovascular age-related macular degeneration. Nat. Commun. 2019, 10, 3347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cabral, T.; Lima, L.H.; Mello, L.G.M.; Pollido, J.; Correra, A.P.; Oshima, A.; Duong, J.; Serracarbassa, P.; Regatiere, C.V.; Mahajan, V.B.; et al. Bevacizumab Injection in Patients with Neovascular Age-Related Macular Degeneration Increases Angiogenic Biomarkers. Ophthalmol. Retin. 2018, 2, 31–37. [Google Scholar] [CrossRef] [Green Version]
- Fiedler, U.; Reiss, Y.; Scharpfenecker, M.; Grunow, V.; Koidl, S.; Thurston, G.; Gale, N.W.; Witzenrath, M.; Rosseau, S.; Suttorp, N.; et al. Angiopoietin-2 sensitizes endothelial cells to TNF-alpha and has a crucial role in the induction of inflammation. Nat. Med. 2006, 12, 235–239. [Google Scholar] [CrossRef]
- Shen, J.; Frye, M.; Lee, B.L.; Reinardy, J.L.; McClung, J.M.; Ding, K.; Kojima, M.; Xia, H.; Seidel, C.; Lima e Silva, R.; et al. Targeting VE-PTP activates TIE2 and stabilizes the ocular vasculature. J. Clin. Investig. 2014, 124, 4564–4576. [Google Scholar] [CrossRef]
- Martin, D.F.; Maguire, M.G.; Ying, G.S.; Grunwald, J.E.; Fine, S.L.; Jaffe, G.J. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N. Engl. J. Med. 2011, 364, 1897–1908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cox, J.T.; Eliott, D.; Sobrin, L. Inflammatory Complications of Intravitreal Anti-VEGF Injections. J. Clin. Med. 2021, 10, 981. [Google Scholar] [CrossRef] [PubMed]
- Wallsh, J.O.; Gallemore, R.P. Anti-VEGF-Resistant Retinal Diseases: A Review of the Latest Treatment Options. Cells 2021, 10, 1049. [Google Scholar] [CrossRef] [PubMed]
- Day, S.; Acquah, K.; Lee, P.P.; Mruthyunjaya, P.; Sloan, F.A. Medicare costs for neovascular age-related macular degeneration, 1994–2007. Am. J. Ophthalmol. 2011, 152, 1014–1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmidt-Erfurth, U.; Chong, V.; Loewenstein, A.; Larsen, M.; Souied, E.; Schlingemann, R.; Eldem, B.; Mones, J.; Richard, G.; Bandello, F.; et al. Guidelines for the management of neovascular age-related macular degeneration by the European Society of Retina Specialists (EURETINA). Br. J. Ophthalmol. 2014, 98, 1144–1167. [Google Scholar] [CrossRef] [PubMed]
- Van der Reis, M.I.; La Heij, E.C.; De Jong-Hesse, Y.; Ringens, P.J.; Hendrikse, F.; Schouten, J.S. A systematic review of the adverse events of intravitreal anti-vascular endothelial growth factor injections. Retina 2011, 31, 1449–1469. [Google Scholar] [CrossRef]
- Macular Photocoagulation Study Group. Argon laser photocoagulation for neovascular maculopathy. Three-year results from randomized clinical trials. Arch. Ophthalmol. 1986, 104, 694–701. [Google Scholar] [CrossRef]
- Zarbin, M.; Szirth, B. Current treatment of age-related macular degeneration. Optom. Vis. Sci. 2007, 84, 559–572. [Google Scholar] [CrossRef]
- Awan, M.A.; Tarin, S.A. Review of photodynamic therapy. Surgeon 2006, 4, 231–236. [Google Scholar] [CrossRef]
- Bressler, N.M. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: Two-year results of 2 randomized clinical trials-tap report 2. Arch. Ophthalmol. 2001, 119, 198–207. [Google Scholar]
- Arnold, J.; Barbezetto, I.; Birngruber, R.; Bressler, N.M.; Bressler, S.B.; Donati, G.; Fish, G.E.; Flaxel, C.J.; Gragoudas, E.S.; Harvey, P.; et al. Verteporfin in Photodynamic Therapy Study Group. Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: Two-year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization—Verteporfin in photodynamic therapy report 2. Am. J. Ophthalmol. 2001, 131, 541–560. [Google Scholar] [CrossRef]
- Azab, M.; Boyer, D.S.; Bressler, N.M.; Bressler, S.B.; Cihelkova, I.; Hao, Y.; Immonen, I.; Lim, J.I.; Menchini, U.; Naor, J.; et al. Verteporfin therapy of subfoveal minimally classic choroidal neovascularization in age-related macular degeneration: 2-year results of a randomized clinical trial. Arch. Ophthalmol. 2005, 123, 448–457. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, P.K. Verteporfin PDT for subfoveal occult CNV in AMD: Two-year results of a randomized trial. Curr. Med. Res. Opin. 2009, 25, 1853–1860. [Google Scholar] [CrossRef] [PubMed]
- Blinder, K.J.; Bradley, S.; Bressler, N.M.; Bressler, S.; Donati, G.; Hao, Y.; Ma, C.; Menchini, U.; Miller, J.; Potter, M.J.; et al. Effect of lesion size, visual acuity, and lesion composition on visual acuity change with and without verteporfin therapy for choroidal neovascularization secondary to age-related macular degeneration: TAP and VIP report no. 1. Am. J. Ophthalmol. 2003, 136, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.K. Photodynamic therapy: Current role in the treatment of chorioretinal conditions. Eye 2016, 30, 202–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gragoudas, E.S.; Adamis, A.P.; Cunningham, E.T., Jr.; Feinsod, M.; Guyer, D.R. Pegaptanib for neovascular age-related macular degeneration. N. Engl. J. Med. 2004, 351, 2805–2816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fish, G.; Haller, J.A.; Ho, A.C.; Klein, M.; Loewenstein, J.; Martin, D.; Orth, D.; Rosen, R.B.; Sanislo, S.; Schwartz, S.D.; et al. The Eyetech Study Group. Anti-vascular endothelial growth factor therapy for subfoveal choroidal neovascularization secondary to age-related macular degeneration: Phase II study results. Ophthalmology 2003, 110, 979–986. [Google Scholar] [CrossRef]
- Ferrara, N.; Hillan, K.J.; Gerber, H.P.; Novotny, W. Discovery and development of bevacizumab, an anti-VEGF antibody for treating cancer. Nat. Rev. Drug Discov. 2004, 3, 391–400. [Google Scholar] [CrossRef]
- Moshfeghi, A.A.; Rosenfeld, P.J.; Puliafito, C.A.; Michels, S.; Marcus, E.N.; Lenchus, J.D.; Venkatraman, A.S. Systemic bevacizumab (Avastin) therapy for neovascular age-related macular degeneration: Twenty-four-week results of an uncontrolled open-label clinical study. Ophthalmology 2006, 113, e1–e12. [Google Scholar] [CrossRef]
- Rosenfeld, P.J.; Moshfeghi, A.A.; Puliafito, C.A. Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for neovascular age-related macular degeneration. Ophthalmic Surg. Lasers Imaging Retin. 2005, 36, 331–335. [Google Scholar] [CrossRef]
- Spaide, R.F.; Laud, K.; Fine, H.F.; Klancnik, J.M.; Meyerle, B.C.; Yannuzzi, L.A.; Sorenson, J.; Slakter, J.; Fisher, Y.L.; Cooney, M.J. Intravitreal bevacizumab treatment of choroidal neovascularization secondary to age-related macular degeneration. Retina 2006, 26, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Chakravarthy, U.; Harding, S.P.; Rogers, C.A.; Downes, S.M.; Lotery, A.J.; Culliford, A.J.; Reeves, B.C. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial. Lancet 2013, 382, 1258–1267. [Google Scholar] [CrossRef]
- Martin, D.F.; Maguire, M.G.; Fine, S.L.; Klancnik Jr, J.M.; Meyerle, C.B.; Yannuzzi, L.A.; Sorenson, J.; Slakter, J.; Fisher, Y.L.; Cooney, M.J. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: Two-year results. Ophthalmology 2012, 119, 1388–1398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schauwvlieghe, A.M.; Dijkman, G.; Hooymans, J.M.; Verbraak, F.D.; Hoyng, C.B.; Dijkgraaf, M.G.W.; Peto, T.; Vingerling, J.R.; Schlingemann, R.O. Comparing the Effectiveness of Bevacizumab to Ranibizumab in Patients with Exudative Age-Related Macular Degeneration. The BRAMD Study. PLoS ONE 2016, 11, e0153052. [Google Scholar] [CrossRef] [Green Version]
- Berg, K.; Pedersen, T.R.; Sandvik, L.; Bragadóttir, R. Comparison of ranibizumab and bevacizumab for neovascular age-related macular degeneration according to LUCAS treat-and-extend protocol. Ophthalmology 2015, 122, 146–152. [Google Scholar] [CrossRef]
- Van Asten, F.; Michels, C.T.J.; Hoyng, C.B.; Jan van der Wilt, G.; Klevering, B.J.; Rovers, M.M.; Grutters, J.P.C. The cost-effectiveness of bevacizumab, ranibizumab and aflibercept for the treatment of age-related macular degeneration-A cost-effectiveness analysis from a societal perspective. PLoS ONE 2018, 13, e0197670. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Wiesmann, C.; Fuh, G.; Li, B.; Christinger, H.W.; McKay, P.; M de Vos, A.; Lowman, H.B. Selection and analysis of an optimized anti-VEGF antibody: Crystal structure of an affinity-matured Fab in complex with antigen. J. Mol. Biol. 1999, 293, 865–881. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrara, N.; Damico, L.; Shams, N.; Lowman, H.; Kim, R. Development of ranibizumab, an anti-vascular endothelial growth factor antigen binding fragment, as therapy for neovascular age-related macular degeneration. Retina 2006, 26, 859–870. [Google Scholar] [CrossRef]
- Rosenfeld, P.J.; Brown, D.M.; Heier, J.S.; Boyer, D.S.; Kaiser, P.K.; Chung, C.Y.; Kim, R.Y. Ranibizumab for neovascular age-related macular degeneration. N. Engl. J. Med. 2006, 355, 1419–1431. [Google Scholar] [CrossRef] [Green Version]
- Brown, D.M.; Kaiser, P.K.; Michels, M.; Soubrane, G.; Heier, J.S.; Kim, R.Y.; Sy, J.P.; Schneider, S. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N. Engl. J. Med. 2006, 355, 1432–1444. [Google Scholar] [CrossRef] [Green Version]
- Schmidt-Erfurth, U.; Eldem, B.; Guymer, R.; Korobelink, J.F.; Schlingemann, R.O.; Axer-Siegel, R.; Wiedemann, P.; Simader, C.; Gekkieva, M.; Weichselberger, A. Efficacy and safety of monthly versus quarterly ranibizumab treatment in neovascular age-related macular degeneration: The EXCITE study. Ophthalmology 2011, 118, 831–839. [Google Scholar] [CrossRef] [PubMed]
- Lalwani, G.A.; Rosenfeld, P.J.; Fung, A.E.; Dubvoy, S.R.; Michels, S.; Feuer, W.; Davis, J.L.; Flynn, H.W., Jr.; Esquiarbo, M. A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: Year 2 of the PrONTO Study. Am. J. Ophthalmol. 2009, 148, 43–58.e1. [Google Scholar] [CrossRef] [PubMed]
- Boyer, D.S.; Heier, J.S.; Brown, D.M.; Francom, S.F.; Ianchulev, T.; Rubio, R.G. A Phase IIIb study to evaluate the safety of ranibizumab in subjects with neovascular age-related macular degeneration. Ophthalmology 2009, 116, 1731–1739. [Google Scholar] [CrossRef] [PubMed]
- Holz, F.G.; Amoaku, W.; Donate, J.; Guymer, R.H.; Kellner, U.; Schlingemann, R.O.; Weichselberger, A.; Staurenghi, G. Safety and efficacy of a flexible dosing regimen of ranibizumab in neovascular age-related macular degeneration: The SUSTAIN study. Ophthalmology 2011, 118, 663–671. [Google Scholar] [CrossRef]
- Eldem, B.M.; Muftuoglu, G.; Topbaş, S.; Cakir, M.; Kadayifcilar, S.; Ozmert, E.; Bahcecioglu, H.; Sahin, F.; Sevgi, S. A randomized trial to compare the safety and efficacy of two ranibizumab dosing regimens in a Turkish cohort of patients with choroidal neovascularization secondary to AMD. Acta Ophthalmol. 2015, 93, e458–e464. [Google Scholar] [CrossRef] [PubMed]
- Wykoff, C.C.; Croft, D.E.; Brown, D.M.; Wang, R.; Payne, J.F.; Clark, L.; Abdelfattah, N.S.; Sadda, S.R.; TREX-AMD Group. Prospective Trial of Treat-and-Extend versus Monthly Dosing for Neovascular Age-Related Macular Degeneration: TREX-AMD 1-Year Results. Ophthalmology 2015, 122, 2514–2522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmidt-Erfurth, U.; Schlötzer-Schrehard, U.; Cursiefen, C.; Michels, S.; Beckendorf, A.; Naumann, G.O. Influence of photodynamic therapy on expression of vascular endothelial growth factor (VEGF), VEGF receptor 3, and pigment epithelium-derived factor. Investig. Ophthalmol. Vis. Sci. 2003, 44, 4473–4480. [Google Scholar] [CrossRef] [Green Version]
- Antoszyk, A.N.; Tuomi, L.; Chung, C.Y.; Singh, A. Ranibizumab combined with verteporfin photodynamic therapy in neovascular age-related macular degeneration (FOCUS): Year 2 results. Am. J. Ophthalmol. 2008, 145, 862–874. [Google Scholar] [CrossRef]
- Holz, F.G.; PROTECT Study Group. Nine Month Safety and Efficacy Results from an Open-Label, Multicenter, Phase II Study of Same-Day Verteporfin and Ranibizumab 0.5mg (PROTECT Study). Investig. Ophthalmol. Vis. Sci. 2007, 48, 4566. [Google Scholar]
- Kais, P.K.; Boyer, D.S.; Cruess, A.F.; Slakter, J.S.; Pilz, S.; Weisberger, A. Verteporfin plus ranibizumab for choroidal neovascularization in age-related macular degeneration: Twelve-month results of the DENALI study. Ophthalmology 2012, 119, 1001–1010. [Google Scholar] [CrossRef]
- Silva, R.M.; Faria de Abreu, J.R.; Travassos, A.; Cunha-Vaz, J.G. Stabilization of visual acuity with photodynamic therapy in eyes with chorioretinal anastomoses. Graefes Arch. Clin. Exp. Ophthalmol. 2004, 242, 368–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koh, A.; Lee, W.K.; Chen, L.J.; Chen, S.J.; Hashad, Y.; Kim, H.; Lai, T.Y.; Pilz, S.; Ruamviboonsuk, P.; Tokaji, E.; et al. EVEREST study: Efficacy and safety of verteporfin photodynamic therapy in combination with ranibizumab or alone versus ranibizumab monotherapy in patients with symptomatic macular polypoidal choroidal vasculopathy. Retina 2012, 32, 1453–1464. [Google Scholar] [CrossRef] [PubMed]
- Lim, T.H.; Lai, T.Y.Y.; Takahashi, K.; Wong, T.Y.; Chen, L.J.; Ruamviboonsuk, P.; Tan, C.S.; Lee, W.K.; Cheung, C.M.G.; Ngah, N.F.; et al. Comparison of Ranibizumab with or without Verteporfin Photodynamic Therapy for Polypoidal Choroidal Vasculopathy: The EVEREST II Randomized Clinical Trial. JAMA Ophthalmol. 2020, 138, 935–942. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.H.; Holz, F.G. Preclinical aspects of anti-VEGF agents for the treatment of wet AMD: Ranibizumab and bevacizumab. Eye 2011, 25, 661–672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chong, V. Ranibizumab for the treatment of wet AMD: A summary of real-world studies. Eye 2016, 30, 270–286. [Google Scholar] [CrossRef]
- Chavan, R.; Panneerselvam, S.; Adhana, P.; Narendran, N.; Yang, Y. Bilateral visual outcomes and service utilization of patients treated for 3 years with ranibizumab for neovascular age-related macular degeneration. Clin. Ophthalmol. 2014, 8, 717–723. [Google Scholar] [CrossRef] [Green Version]
- Cohen, S.Y.; Mimoun, G.; Oubraham, H.; Zourdani, A.; Malbrel, C.; Quere, S.; Schneider, V.; LUMIERE Study Group. Changes in visual acuity in patients with wet age-related macular degeneration treated with intravitreal ranibizumab in daily clinical practice: The LUMIERE study. Retina 2013, 33, 474–481. [Google Scholar] [CrossRef]
- Finger, R.P.; Wiedemann, P.; Blumhagen, F.; Pohl, K.; Holz, F.G. Treatment patterns, visual acuity and quality-of-life outcomes of the WAVE study—A noninterventional study of ranibizumab treatment for neovascular age-related macular degeneration in Germany. Acta Ophthalmol. 2013, 91, 540–546. [Google Scholar] [CrossRef]
- Frennesson, C.I.; Nilsson, S.E. A three-year follow-up of ranibizumab treatment of exudative AMD: Impact on the outcome of carrying forward the last acuity observation in drop-outs. Acta Ophthalmol. 2014, 92, 216–220. [Google Scholar] [CrossRef]
- Gabai, A.; Veritti, D.; Lanzetta, P. One-year outcome of ranibizumab for neovascular age-related macular degeneration: A thorough analysis in a real-world clinical setting. Eur. J. Ophthalmol. 2014, 24, 396–401. [Google Scholar] [CrossRef]
- Hjelmqvist, L.; Lindberg, C.; Kanulf, P.; Dahlgren, H.; Johansson, I.; Siewert, A. One-year outcomes using ranibizumab for neovascular age-related macular degeneration: Results of a prospective and retrospective observational multicentre study. J. Ophthalmol. 2011, 2011, 405724. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holz, F.G.; Tadayoni, R.; Beatty, S.; Berger, A.; Cereda, M.G.; Cortez, R.; Hoyng, C.B.; Hykin, P.; Staurenghi, G.; Heldner, S. Multi-country real-life experience of anti-vascular endothelial growth factor therapy for wet age-related macular degeneration. Br. J. Ophthalmol. 2015, 99, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Sahni, J.N.; Stangos, A.N.; Campa, C.; Harding, S.P. Effectiveness of ranibizumab for neovascular age-related macular degeneration using clinician-determined retreatment strategy. Br. J. Ophthalmol. 2011, 95, 530–533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsumiya, W.; Honda, S.; Kusuhara, S.; Tsukahara, Y.; Negi, A. Effectiveness of intravitreal ranibizumab in exudative age-related macular degeneration (AMD): Comparison between typical neovascular AMD and polypoidal choroidal vasculopathy over a 1 year follow-up. BMC Ophthalmol. 2013, 13, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muether, P.S.; Hoerster, R.; Hermann, M.M.; Kirchhof, B.; Fauser, S. Long-term effects of ranibizumab treatment delay in neovascular age-related macular degeneration. Graefes Arch. Clin. Exp. Ophthalmol. 2013, 251, 453–458. [Google Scholar] [CrossRef]
- Nomura, Y.; Takahashi, H.; Tan, X.; Fujimura, S.; Obata, R.; Yanagi, Y. Effects of vitreomacular adhesion on ranibizumab treatment in Japanese patients with age-related macular degeneration. Jpn. J. Ophthalmol. 2014, 58, 443–447. [Google Scholar] [CrossRef]
- Pagliarini, S.; Beatty, S.; Lipkova, B.; Garcia, E.P.S.; Reynders, S.; Gekkieva, M.; Bouazza, A.; Pilz, S. A 2-Year, Phase IV, Multicentre, Observational Study of Ranibizumab 0.5 mg in Patients with Neovascular Age-Related Macular Degeneration in Routine Clinical Practice: The EPICOHORT Study. J. Ophthalmol. 2014, 2014, 857148. [Google Scholar] [CrossRef]
- Piermarocchi, S.; Miotto, S.; Colavito, D.; Leon, A.; Segato, T. Combined effects of genetic and non-genetic risk factors affect response to ranibizumab in exudative age-related macular degeneration. Acta Ophthalmol. 2015, 93, e451–e457. [Google Scholar] [CrossRef]
- Rakic, J.M.; Leys, A.; Brié, H.; Denhaerynck, K.; Pacheco, C.; Vancayzeele, S.; Hermans, C.; Macdonald, K.; Abraham, I. Real-world variability in ranibizumab treatment and associated clinical, quality of life, and safety outcomes over 24 months in patients with neovascular age-related macular degeneration: The HELIOS study. Clin. Ophthalmol. 2013, 7, 1849–1858. [Google Scholar] [CrossRef] [Green Version]
- Zhu, M.; Chew, J.K.; Broadhead, G.K.; Luo, K.; Joachim, N.; Hong, T.; Syed, A.; Chang, A.A. Intravitreal Ranibizumab for neovascular Age-related macular degeneration in clinical practice: Five-year treatment outcomes. Graefes Arch. Clin. Exp. Ophthalmol. 2015, 253, 1217–1225. [Google Scholar] [CrossRef]
- Chan, C.K.; Lalezary, M.; Abraham, P.; Elman, M.; Beaulieu, W.T.; Lin, S.G.; Khurana, R.N.; Bansal, A.S.; Wieland, M.R.; Palmer, J.D. Prophylactic Ranibizumab to Prevent Neovascular Age-Related Macular Degeneration in Vulnerable Fellow Eyes: A Randomized Clinical Trial. Ophthalmol. Retin. 2022, 6, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Hussain, R.M.; Ciulla, T.A. Emerging vascular endothelial growth factor antagonists to treat neovascular age-related macular degeneration. Expert Opin. Emerg. Drugs 2017, 22, 235–246. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.M.; Heier, J.S.; Ciulla, T.; Benz, M.; Abraham, P.; Yancopoulos, G.; Stahl, N.; Ingerman, A.; Vitti, R.; Berliner, A.J. Primary endpoint results of a phase II study of vascular endothelial growth factor trap-eye in wet age-related macular degeneration. Ophthalmology 2011, 118, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
- Heier, J.S.; Brown, D.M.; Chong, V.; Korobrlinik, J.; Kaiser, P.K.; Nguyen, Q.D.; Kirchhof, B.; Ho, A.; Ogura, Y.; Yancopoulos, G.D.; et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology 2012, 119, 2537–2548. [Google Scholar] [CrossRef] [PubMed]
- Providência, J.; Rodrigues, T.M.; Oliveira, M.; Bernardes, J.; Marques, J.P.; Murta, J.; Silva, R. Real-World Results of Aflibercept versus Ranibizumab for the Treatment of Exudative AMD Using a Fixed Regimen. Biomed. Res. Int. 2018, 2018, 9276580. [Google Scholar] [CrossRef] [Green Version]
- Luksa, D.; Heinke, A.; Michalska-Małecka, K. Two Year Study of Aflibercept and Ranibizumab Intravitreal Therapy in Patients with Wet AMD. Medicina 2021, 57, 1293. [Google Scholar] [CrossRef]
- Ishibashi, K.; Haruta, M.; Ishibashi, Y.; Noda, R.; Dake, S.; Yoshida, S. Four-year outcomes of intravitreal aflibercept treatment for neovascular age-related macular degeneration using a treat-and-extend regimen in Japanese patients. Ther. Adv. Ophthalmol. 2021, 13, 2515841420984586. [Google Scholar] [CrossRef]
- Lee, J.; Kim, Y.N.; Kim, J.G. Monthly Alternating Injections of Aflibercept and Bevacizumab for Neovascular Age-Related Macular Degeneration. J. Clin. Med. 2022, 11, 1543. [Google Scholar] [CrossRef]
- Hamid, M.A.; Abdelfattah, N.S.; Salamzadeh, J.; Abdelaziz, S.T.A.; Sabry, A.M.; Mourad, K.M.; Shehab, A.A.; Kuppermann, B.D. Aflibercept therapy for exudative age-related macular degeneration resistant to bevacizumab and ranibizumab. Int. J. Retin. Vitr. 2021, 7, 26. [Google Scholar] [CrossRef]
- Heier, J.S.; Brown, D.M.; Shah, S.P.; Saroj, N.; Dang, S.; Waheed, N.K.; Wykoff, C.C.; Prenner, J.L.; Boyer, D.S. Intravitreal Aflibercept Injection vs Sham as Prophylaxis against Conversion to Exudative Age-Related Macular Degeneration in High-risk Eyes: A Randomized Clinical Trial. JAMA Ophthalmol. 2021, 139, 542–547. [Google Scholar] [CrossRef]
- Dugel, P.U.; Koh, A.; Ogura, Y.; Jaffe, G.J.; Schmidt-Erfurth, U.; Brown, D.M.; Gomes, A.V.; Warburton, J.; Weicheselberger, A.; Holz, F.G.; et al. HAWK and HARRIER: Phase 3, Multicenter, Randomized, Double-Masked Trials of Brolucizumab for Neovascular Age-Related Macular Degeneration. Ophthalmology 2020, 127, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Bulirsch, L.M.; Saßmannshausen, M.; Nadal, J.; Liegl, R.; Thiele, S.; Holz, F.G. Short-term real-world outcomes following intravitreal brolucizumab for neovascular AMD: SHIFT study. Br. J. Ophthalmol. 2021, 106, 1288–1294. [Google Scholar] [CrossRef] [PubMed]
- Bilgic, A.; Kodjikian, L.; Srivastava, S.; Dwivedi, S.; Banker, A.S.; Abukashabah, A.; Sudhalkar, A.; Mathis, T. Initial Pro Re Nata Brolucizumab for Exudative AMD: The PROBE Study. J. Clin. Med. 2021, 10, 4153. [Google Scholar] [CrossRef]
- Bilgic, A.; Kodjikian, L.; March de Ribot, F.; Vasavada, V.; Gonzalez-Cortes, J.H.; Abukashabah, A.; Sudhalkar, A.; Mathis, T. Real-World Experience with Brolucizumab in Wet Age-Related Macular Degeneration: The REBA Study. J. Clin. Med. 2021, 10, 2758. [Google Scholar] [CrossRef] [PubMed]
- Pearce, I.; Amoaku, W.; Bailey, C.; Dowenet, L.; Gale, R.; Ghanchi, F.; Hamilton, R.; Mahmood, S.; Menon, G.; Nosek, J.; et al. The changing landscape for the management of patients with neovascular AMD: Brolucizumab in clinical practice. Eye 2022, 36, 1725–1734. [Google Scholar] [CrossRef] [PubMed]
- Campochiaro, P.A.; Marcus, D.M.; Awh, C.C.; Regillo, C.; Adamis, A.P.; Bantseev, V.; Chiang, Y.; Ehrlich, J.S.; Erickson, S.; Hanley, W.D.; et al. The Port Delivery System with Ranibizumab for Neovascular Age-Related Macular Degeneration: Results from the Randomized Phase 2 Ladder Clinical Trial. Ophthalmology 2019, 126, 1141–1154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loewenstein, A.; Laganovska, G.; Bressler, N.M.; Vanags, J.; Alster, Y.; De Juan, E.; Stewart, J.M.; Kardatzke, D.; Singh, N.; Erickson, S. Phase 1 Clinical Study of the Port Delivery System with ranibizumab for continuous treatment of neovascular age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2020, 61, 4201. [Google Scholar]
- Khanani, A.M.; Callanan, D.; Dreyer, R.; Chen, S.; Howard, J.G.; Hopkins, J.J.; Lin, C.-Y.; Lorenz-Candlin, M.; Makadia, S.; Patel, S. End-of-Study Results for the Ladder Phase 2 Trial of the Port Delivery System with Ranibizumab for Neovascular Age-Related Macular Degeneration. Ophthalmol. Retin. 2021, 5, 775–787. [Google Scholar] [CrossRef]
- Holekamp, N.M.; Campochiaro, P.A.; Chang, M.A.; Barteselli, G.; Regillo, C. Archway Randomized Phase 3 Trial of the Port Delivery System with Ranibizumab for Neovascular Age-Related Macular Degeneration. Ophthalmology 2022, 129, 295–307. [Google Scholar] [CrossRef]
- Extension Study for the Port Delivery System with Ranibizumab (Portal). Available online: https://clinicaltrials.gov/ct2/show/NCT03683251 (accessed on 8 January 2022).
- Rao, P.; Lum, F.; Wood, K.; Salman, C.; Burugapalli, B.; Hall, R.; Singh, S.; Parke 2nd, D.W.; Williams, G.A. Real-World Vision in Age-Related Macular Degeneration Patients Treated with Single Anti-VEGF Drug Type for 1 Year in the IRIS Registry. Ophthalmology 2018, 125, 522–528. [Google Scholar] [CrossRef]
- Chang, M.A.; Kapre, A.; Kaufman, D.; Kardatzke, D.R.; Rabena, M.; Patel, S.; Bobbala, A.; Gune, S.; Fung, A.; Wallenstein, G. Patient Preference and Treatment Satisfaction with a Port Delivery System for Ranibizumab vs Intravitreal Injections in Patients with Neovascular Age-Related Macular Degeneration: A Randomized Clinical Trial. JAMA Ophthalmol. 2022, 140, 771–778. [Google Scholar] [CrossRef] [PubMed]
- Callanan, D.; Kunimoto, D.; Maturi, R.K.; Patel, S.S.; Staurenghi, G.; Wolf, S.; Cheetham, J.K.; Hohman, T.C.; Kim, K.; Lopez, F.J.; et al. Double-Masked, Randomized, Phase 2 Evaluation of Abicipar Pegol (an Anti-VEGF DARPin Therapeutic) in Neovascular Age-Related Macular Degeneration. J. Ocul. Pharmacol. Ther. 2018, 34, 700–709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Souied, E.H.; Devin, F.; Mauget-Faÿsse, M.; Kolar, P.; Wolf-Schnurrbusch, U.; Framme, C.; Gaucher, D.; Querques, G.; Stumpp, M.T.; Wolf, S. Treatment of exudative age-related macular degeneration with a designed ankyrin repeat protein that binds vascular endothelial growth factor: A phase I/II study. Am. J. Ophthalmol. 2014, 158, 724–732.e2. [Google Scholar] [CrossRef] [PubMed]
- Kunimoto, D.; Yoon, Y.H.; Wykoff, C.C.; Chang, A.; Khurana, R.N.; Maturi, R.K.; Agostini, H.; Souied, E.; Chow, D.R.; Lotery, A.J.; et al. Efficacy and Safety of Abicipar in Neovascular Age-Related Macular Degeneration: 52-Week Results of Phase 3 Randomized Controlled Study. Ophthalmology 2020, 127, 1331–1344. [Google Scholar] [CrossRef] [PubMed]
- Khurana, R.N.; Kunimoto, D.; Yoon, Y.H.; Wykoff, C.C.; Chang, A.; Maturi, R.K.; Agostini, H.; Souied, E.; Chow, D.R.; Lotery, A.J.; et al. Two-Year Results of the Phase 3 Randomized Controlled Study of Abicipar in Neovascular Age-Related Macular Degeneration. Ophthalmology 2021, 128, 1027–1038. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://investors.molecularpartners.com/news-releases/news-release-details/allergan-and-molecular-partners-present-late-breaking-data-phase (accessed on 8 January 2022).
- Joussen, A.M.; Ricci, F.; Paris, L.P.; Korn, C.; Quezada-Ruiz, C.; Zarbin, M. Angiopoietin/Tie2 signalling and its role in retinal and choroidal vascular diseases: A review of preclinical data. Eye 2021, 35, 1305–1316. [Google Scholar] [CrossRef]
- Heier, J.S.; Singh, R.P.; Wykoff, C.C.; Csaky, K.G.; Lai, T.Y.; Loewenstein, A.; Schlottmann, P.G.; Paris, L.P.; Westenskow, P.D.; Quezada-Ruiz, C. The Angiopoietin/Tie Pathway in Retinal Vascular Diseases: A Review. Retina 2021, 41, 1–19. [Google Scholar] [CrossRef]
- Heier, J.S.; Khanani, A.M.; Quezada Ruiz, C.; Basu, K.; Ferrone, P.J.; Brittain, C.; Figueroa, M.S.; Lin, H.; Holz, F.G.; Patel, V.; et al. Efficacy, durability, and safety of intravitreal faricimab up to every 16 weeks for neovascular age-related macular degeneration (TENAYA and LUCERNE): Two randomised, double-masked, phase 3, non-inferiority trials. Lancet 2022, 399, 729–740. [Google Scholar] [CrossRef]
- Patel, S.S.; Janer, D.; Miller, B.; Ehrlich, J.S.; Perlroth, V.; Velazquez-Martin, J.P. Updated Results of Phase 1b Study of KSI-301, an Anti-VEGF Antibody Biopolymer Conjugate with Extended Durability, in wAMD, DME, and RVO. Investig. Ophthalmol. Vis. Sci. 2020, 61, 4286. [Google Scholar]
- Regillo, C.; Ehrlich, J.S.; Janer, D.; Do, D.V.; Velazquez-Martin, P.; Zawadzki, R.; Perlroth, V. Efficacy, durability and safety of KSI-301 antibody biopolymer conjugate in wet AMD – Year 1 primary endpoint results from the pivotal DAZZLE study. Investig. Ophthalmol. Vis. Sci. 2022, 63, 3122. [Google Scholar]
- Dugel, P.U.; Boyer, D.S.; Antoszyk, A.N.; Steinle, N.C.; Varenhorst, M.P.; Pearlman, J.A.; Gillies, M.C.; Finger, R.P.; Baldwin, M.E.; Leitch, I.A. Phase 1 Study of OPT-302 Inhibition of Vascular Endothelial Growth Factors C and D for Neovascular Age-Related Macular Degeneration. Ophthalmol. Retin. 2020, 4, 250–263. [Google Scholar] [CrossRef] [PubMed]
- Arepalli, S.; Kaiser, P.K. Pipeline therapies for neovascular age related macular degeneration. Int. J. Retin. Vitr. 2021, 7, 55. [Google Scholar] [CrossRef] [PubMed]
- Khanani, A.M. Suprachoroidal Delivery of RGX-314 Gene Therapy for Neovascular AMD: The Phase II AAVIATE™ Study. Investig. Ophthalmol. Vis. Sci. 2022, 63, 1497. [Google Scholar]
- Chaney, P. PAN-90806: Once-daily topical anti-VEGF eye drop for wet AMD and other neovascular eye disease. In Proceedings of the Ophthamology Innovation Summit, San Francisco, CA, USA, 10 October 2019; Available online: https://www.panopticapharma.com/wp-content/uploads/2019/10/PAN-90806-Data-at-OIS@AAO.pdf (accessed on 8 January 2022).
- Wells, J.A.; Gonzales, C.R.; Berger, B.B.; Gonzalez, V.H.; Sippy, B.D.; Burian, G. A Phase 1, Open-Label, Dose-Escalation Trial to Investigate Safety and Tolerability of Single Intravitreous Injections of ICON-1 Targeting Tissue Factor in Wet AMD. Ophthalmic Surg. Lasers Imaging Retin. 2018, 49, 336–345. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, C.R.; Burian, G. A Phase 2 Study (EMERGE) Evaluating Repeated Intravitreal Administration of ICON-1 in Patients with Choroidal Neovascularization (CNV) Secondary to Age-related Macular Degeneration (AMD). Investig. Ophthalmol. Vis. Sci. 2017, 58, 3766. [Google Scholar]
- Available online: https://clinicaltrials.gov/ct2/show/NCT03452527 (accessed on 8 January 2022).
| Study | Main Study Objective | Study Design | Interventions | Results |
|---|---|---|---|---|
| Treatment of AMD with PDT (TAP studies) [20] | Evaluation of efficacy of PDT in nAMD patients | Two multicenter, double-masked, randomized, controlled studies, in Europe and the United States of America | Patients were randomized to receive either PDT or placebo | The primary endpoint was the percentage of eyes that lost less than 15 ETDRS letters from baseline at 12 and 24 months. PDT was significantly better than placebo at 12 months (61% versus 46%) And 24 months (53% versus 38%) (p < 0.001) |
| Verteporfin in PDT (VIP) studies [21] | Evaluation of the safety and efficacy of PDT in patients with occult lesions. | Multicenter, randomized, double-masked, controlled clinical trial | Patients were randomized to receive either verteporfin or a placebo | Results at 12 months were disappointing but efficacy was noted at 24 months. At 24 months verteporfin-treated eyes were less likely to have a moderate or severe visual loss, 30% versus 47 % verteporfin-treateded eyes and placebo-treated eyes, respectively, lost at least 30 letters (p = 0.001) |
| Verteporfin in Minimally Classic Choroidal Neovascularization (CNV) (VIM studies) [22] | Evaluation of the efficacy of PDT in minimally classic membranes below six-disc areas in size | Phase 2 Multicenter, randomized, double-masked, controlled clinical trial | Patients were randomized to receive verteporfin with reduced fluence (RF) or standard fluence (SF) or a placebo infusion with either RF or SF | At 24 months, the loss of at least three-lines occurred in 26% of the RF group (p = 0.003), 53% of the SF group (p = 0.54), and 62% of the placebo group (p = 0.03) At 24 months, progression to minimally classic CNV was more common in the placebo group 28%, versus the RF group (5%) (p = 0.007) and versus the SF group (3% with p = 0.002) |
| Visudyne in Occult Classic Choroidal Neovascularization (VIO study) [23] | Evaluation of the role of PDT in patients with an occult lesion (lacking any classic component) | Multicenter, randomized, double-masked, controlled clinical trial | Patients were randomized to receive either verteporfin PDT or placebo | There were no statistically significant differences in the degree of vision loss in both the PDT and the placebo groups at 12 and 24 months. |
| Study | Number of Patients/Country | Duration | Objective | Study Design | Treatment | Prior Treatments | Visual Acuity |
|---|---|---|---|---|---|---|---|
| Chavan et al. [56] | 123 eyes in 120 patients United Kingdom | 3 years | To describe bilateral visual outcomes after treatment, and the effects of incomplete follow up | Retrospective data collected over 36 months from consecutive patients over 9 months | 3 monthly injections of ranibizumab 0.5 mg followed by a pro re nata (PRN) dosing regimen | Naïve patients | Mean change in visual acuity (VA) from Baseline ETDRS letters −1.68 ± 17.76 |
| Cohen et al. [57] (LUMIERE) | 551 eyes in 551 patients France | 1 year | To survey compliance with recommended intravitreal ranibizumab treatment protocols in daily clinical practice in France, with reference to outcomes. | Retrospective, descriptive observational study. Data on patients were collected after 12 months of treatment with ranibizumab | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Naïve patients | Mean change in VA from Baseline ETDRS letters +3.2 ± 14.8 |
| Finger et al. (WAVE) [58] | 3470 patients Germany | 1 year | Evaluation of efficacy and safety of repeated ranibizumab 0.5 mg injections | Prospective non interventional study including AMD patients from 274 practices over a defined period | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Both naïve and previously treated were included | Mean change in BCVA +0.02 ± 0.01 SEM (LogMAR Snellen Values) |
| Frennesson and Nilson [59] | 312 eyes in 268 patients Sweden | 3 years | Evaluation of the effect of carrying forward the last VA of dropouts to the first evaluation point (to get more accurate results) | Retrospective data on patients treated with ranibizumab and followed up for 36 months | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Both naïve and previously treated were included | Change in BCVA ETDRS: at 36 months +0.1 letter. However, if the last available acuity of dropouts was carried forward, VA decreased by 4.1 letters (p = 0.003) at 36 months |
| Gabai et al. [60] | 100 eyes in 92 patients Italy | 1 year | Evaluation of efficacy and safety profile of ranibizumab | Retrospective data was collected on patients with Ranibizumab treatment and follow-up for neovascular AMD for > 12 months | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Naïve patients | Mean change in VA from Baseline ETDRS letters −2.0 ± 17.6 |
| Hjelmqvist et al. (Swedish Lucentis Quality Registry) [61] | 471 patients (272 retrospectively and 199 prospectively) Sweden | 1 year | Evaluation of efficacy of Ranibizumab | 12-month, open-label, observational, prospective, and retrospective study of ranibizumab administration for wet AMD | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Not Mentioned | Mean change in VA from Baseline ETDRS letters +1.0 ± 13.6 |
| Holz et al. (AURA) [62] | 2227 patients, multicenter in Canada and Europe | 2 years | Evaluation of efficacy ranibizumab in management of wet AMD in a real-life setting | Retrospective non-interventional observational study | Treatment as prescribed by a physician (not all patients received 3 months loading dose) | Not mentioned. | Mean change in VA from Baseline ETDRS letters at 2 years +0.6 letters |
| Kumar et al. [63] | 81 eyes in 81 patients UK | 1 year | Evaluation of efficacy ranibizumab in management of wet AMD in a real-life setting | Prospective study following patients starting ranibizumab for wet AMD | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Naïve patients | Mean change in VA from Baseline ETDRS letters +3.7 ± 10.8 |
| Matsumiya et al. [64] | 54 patients, 24 with wet AMD and 30 with PCV Japan | 1 year | Evaluation of the efficacy of ranibizumab in management of two types of AMD | Retrospective cohort study | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Both naïve and previously treated were included | Change in BCVA at 12 months (log MAR values) PCV: −0.04 Typical AMD: −0.16 |
| Muether et al. [65] | 102 patients Germany | 1 year | Evaluation of the effect of latency and delay in initiation of treatment | Prospective study following patients with wet AMD | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen. The German Health System caused a delay of 23.5 ± 10.4 days Between the decision to treat and initiation of treatment | Naïve Patients | Mean change in VA from Baseline ETDRS letters +0.66 ± 16.82 |
| Nomura et al. [66] | 123 patients Japan | 1 year | Evaluation of the effect of Vitreomacular adhesions VMA during treatment with ranibizumab in patients with wet AMD | Retrospective study | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Naïve patients | Mean change in VA from Baseline ETDRS letters Absent VMA: +6 letters VMA: +1.5 letters |
| Pagliarini et al. (EPICOHORT) [67] | 755 patients, 133 of which had bilateral treatment Europe | 2 years | Evaluation of the efficacy and safety profile of Ranibizumab in a real-life setting | Prospective, Phase 4 observational trial | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Both naïve and previously treated were included | Mean change in VA from Baseline ETDRS letters At 12 months: +1.5 ± 0.61 (SEM) |
| Piermarocchi et al [68] | 94 eyes of 94 patients Italy | 1 year | Evaluation of the effect of genetic and non-genetic factors in treatment response to ranibizumab in wet AMD | Prospective study | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Naïve Patients | Mean change in VA from Baseline ETDRS letters At 12 months 0.97 ± 9.1 |
| Rakic et al. (HELIOS) [69] | 309 eyes in 267 paients Belgium | 2 years | Prospective multicenter observational study | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Both naïve and previously treated were included | Mean change in VA from Baseline ETDRS letters At 24 months −2.4 ± 17.4 | |
| Zhu et al. [70] | 886 patients 208 eyes of 208 patients completed the study Australia | 5 years | Evaluation of the efficacy and safety profile of Ranibizumab in a real-life setting | Retrospective study | 3 monthly injections of ranibizumab 0.5 mg followed by a PRN dosing regimen | Both naïve and previously treated were included | Mean change in VA from Baseline ETDRS letters At 5 years: −2.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
ElSheikh, R.H.; Chauhan, M.Z.; Sallam, A.B. Current and Novel Therapeutic Approaches for Treatment of Neovascular Age-Related Macular Degeneration. Biomolecules 2022, 12, 1629. https://doi.org/10.3390/biom12111629
ElSheikh RH, Chauhan MZ, Sallam AB. Current and Novel Therapeutic Approaches for Treatment of Neovascular Age-Related Macular Degeneration. Biomolecules. 2022; 12(11):1629. https://doi.org/10.3390/biom12111629
Chicago/Turabian StyleElSheikh, Reem H., Muhammad Z. Chauhan, and Ahmed B. Sallam. 2022. "Current and Novel Therapeutic Approaches for Treatment of Neovascular Age-Related Macular Degeneration" Biomolecules 12, no. 11: 1629. https://doi.org/10.3390/biom12111629
APA StyleElSheikh, R. H., Chauhan, M. Z., & Sallam, A. B. (2022). Current and Novel Therapeutic Approaches for Treatment of Neovascular Age-Related Macular Degeneration. Biomolecules, 12(11), 1629. https://doi.org/10.3390/biom12111629







