Dipeptidyl Peptidase-4 Inhibitor Sitagliptin Phosphate Accelerates Cellular Cholesterol Efflux in THP-1 Cells
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Cell Culture
2.3. Cellular Cholesterol Efflux
2.4. RNA Isolation and Quantitative, Real-Time Polymerase Chain Reaction (PCR)
2.5. Western Blot Analysis
2.6. Statistical Analysis
3. Results
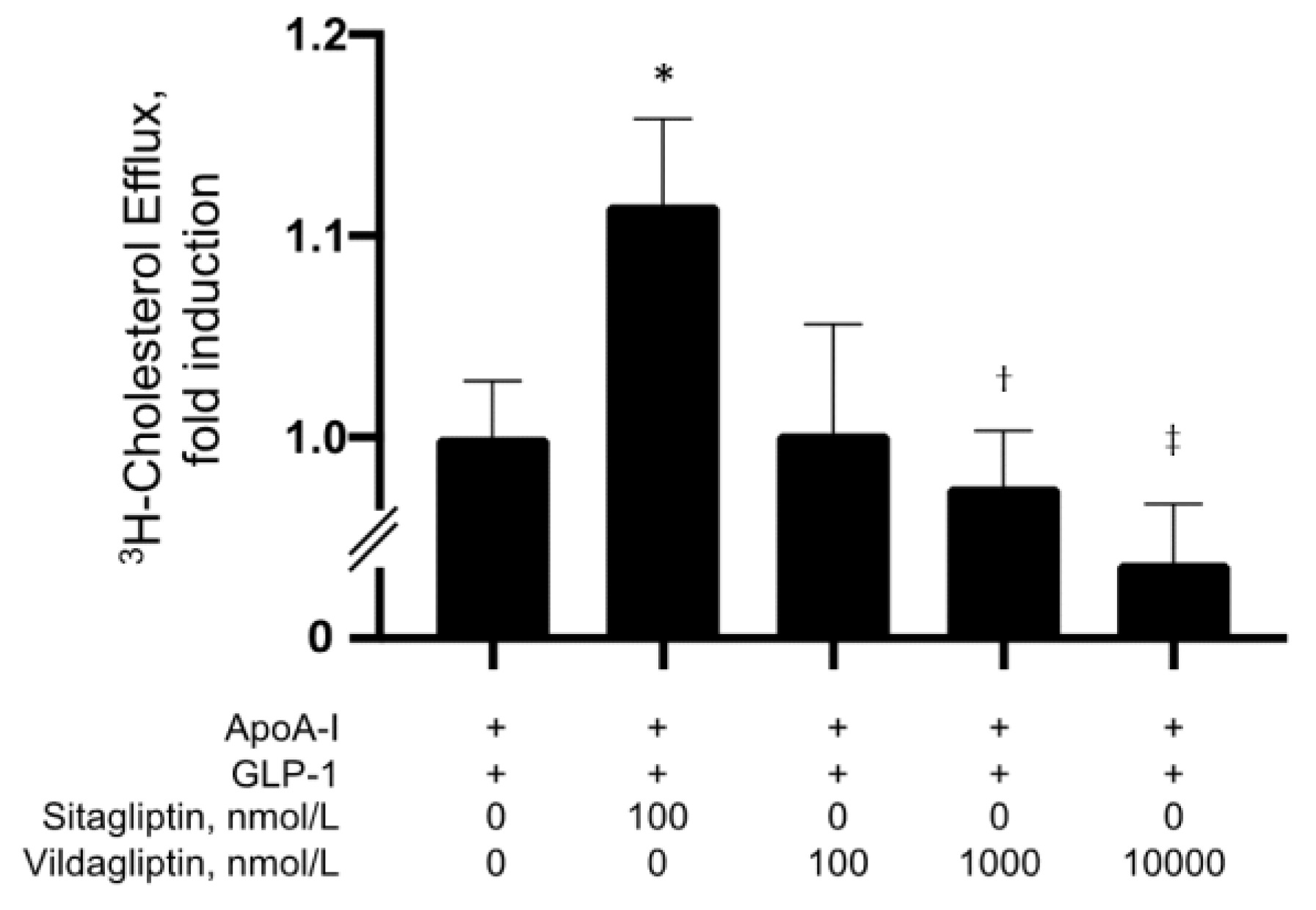
3.1. Sitagliptin Together with GLP-1 Significantly Increased Apoa1-Mediated Cholesterol Efflux
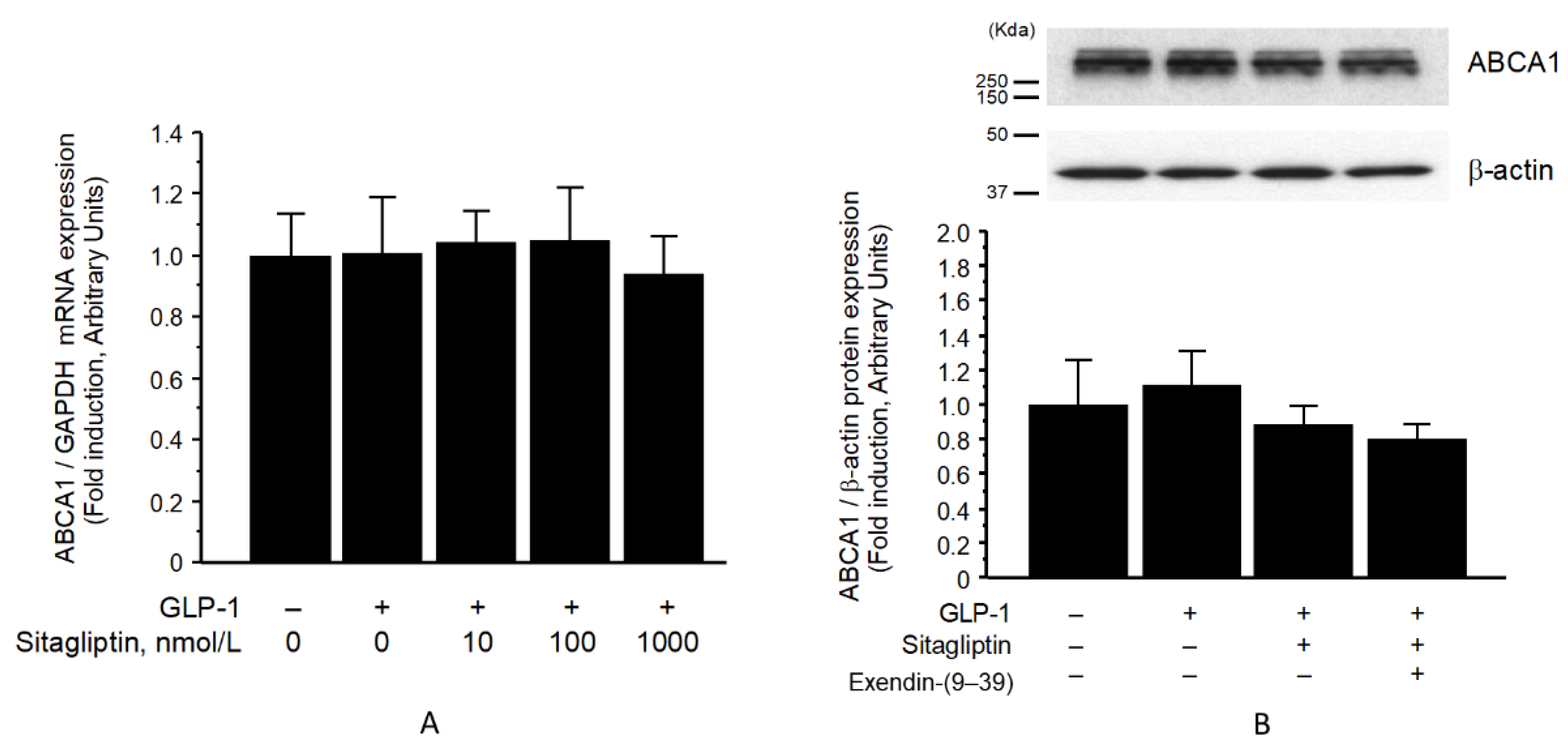
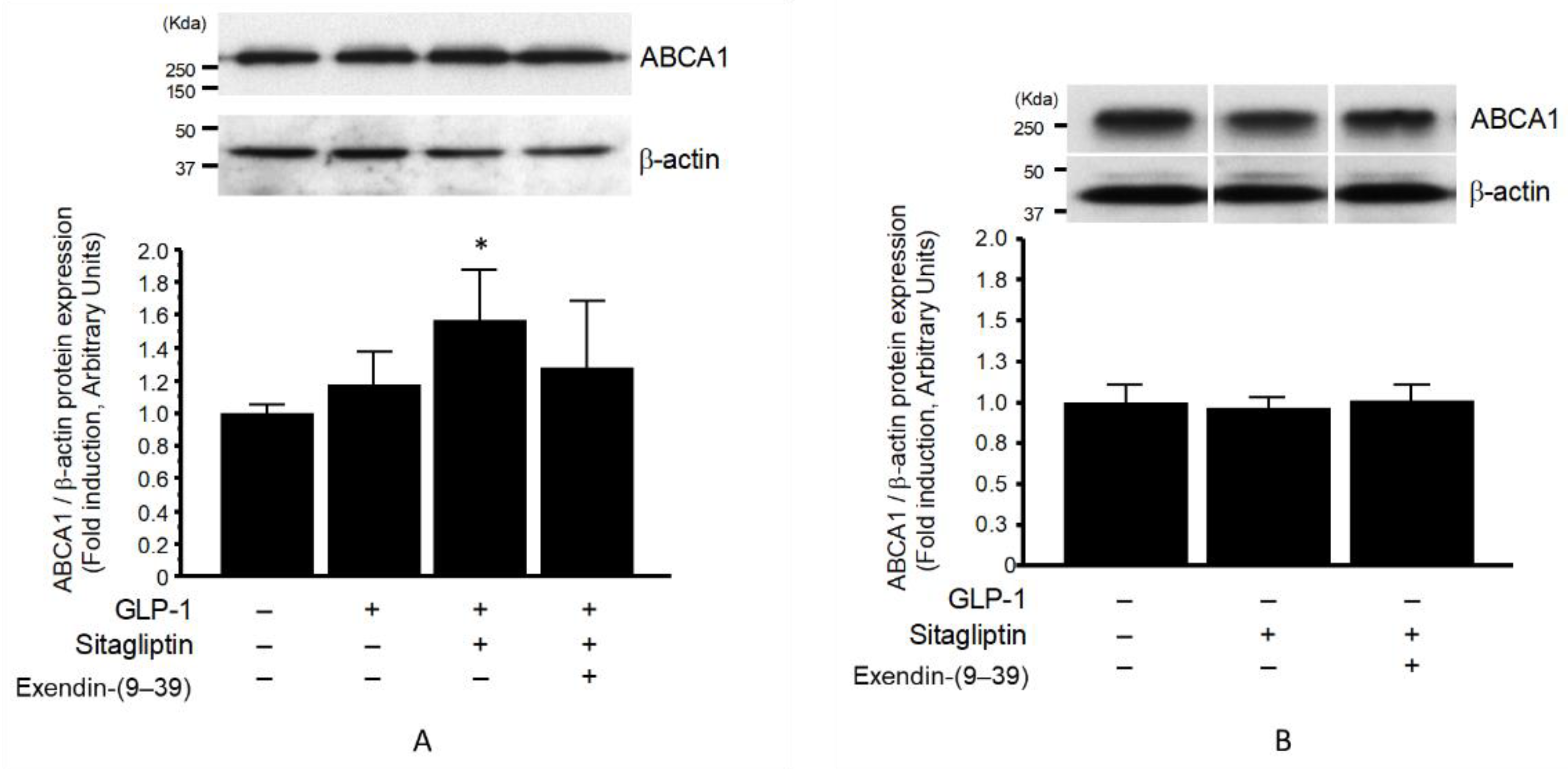
3.2. ABCA1 Protein in Membrane Fraction, but Not Whole-Cell Fraction, Was Significantly Increased by Sitagliptin Phosphate
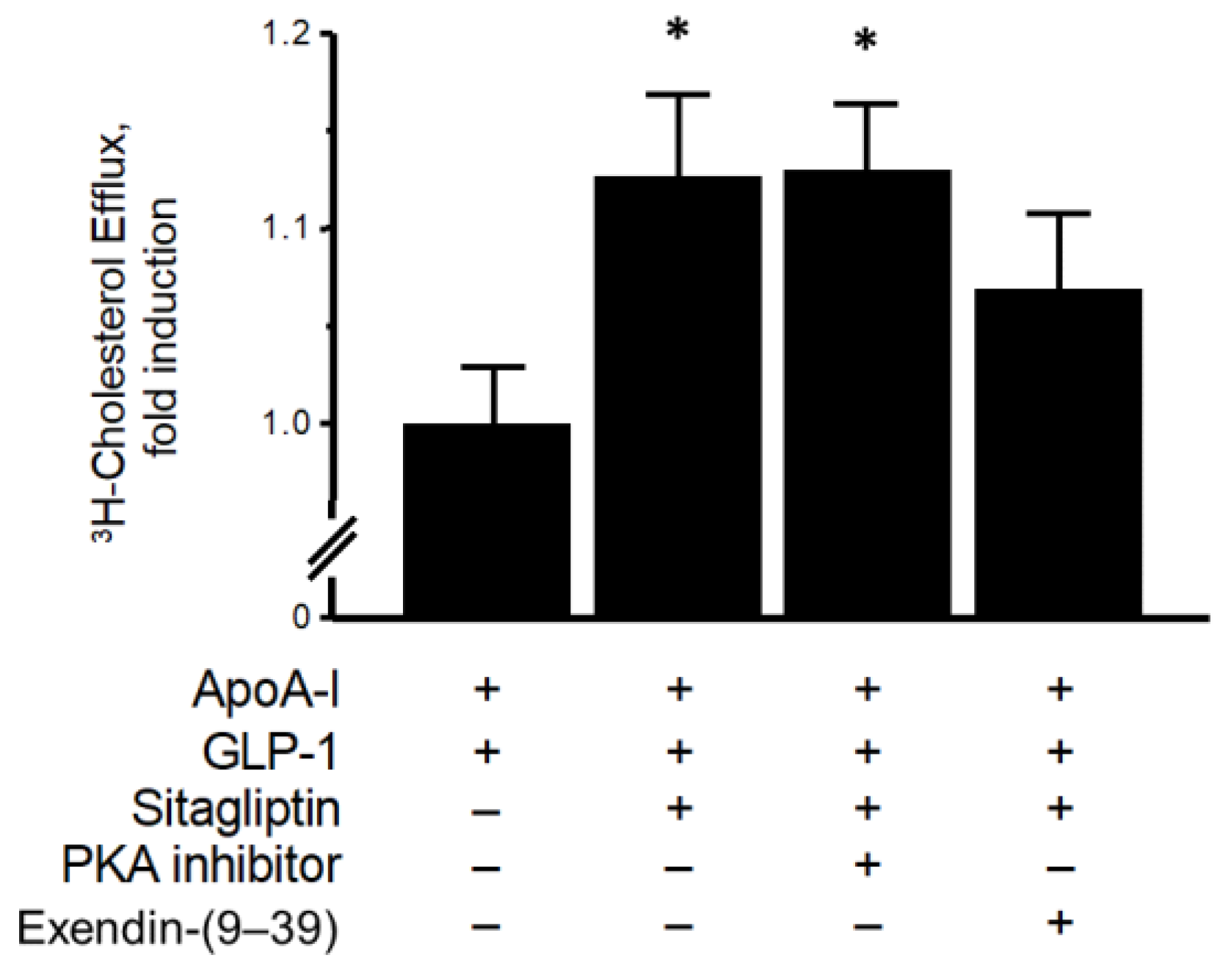
3.3. ApoA1-Mediated Cholesterol Efflux Was Mediated via GLP-1R Pathway
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lewis, G.F.; Rader, D.J. New insights into the regulation of HDL metabolism and reverse cholesterol transport. Circ. Res. 2005, 96, 1221–1232. [Google Scholar] [CrossRef] [PubMed]
- Rosenson, R.S.; Brewer, H.B., Jr.; Davidson, W.S.; Fayad, Z.A.; Fuster, V.; Goldstein, J.; Hellerstein, M.; Jiang, X.C.; Phillips, M.C.; Rader, D.J.; et al. Cholesterol efflux and atheroprotection: Advancing the concept of reverse cholesterol transport. Circulation 2012, 125, 1905–1919. [Google Scholar] [CrossRef] [PubMed]
- Oram, J.F.; Lawn, R.M. ABCA1. The gatekeeper for eliminating excess tissue cholesterol. J. Lipid Res. 2001, 42, 1173–1179. [Google Scholar] [CrossRef] [PubMed]
- Yvan-Charvet, L.; Ranalletta, M.; Wang, N.; Han, S.; Terasaka, N.; Li, R.; Welch, C.; Tall, A.R. Combined deficiency of ABCA1 and ABCG1 promotes foam cell accumulation and accelerates atherosclerosis in mice. J. Clin. J. Clin. Investig. 2007, 117, 3900–3908. [Google Scholar] [CrossRef] [PubMed]
- Vaisman, B.L.; Lambert, G.; Amar, M.; Joyce, C.; Ito, T.; Shamburek, R.D.; Cain, W.J.; Fruchart-Najib, J.; Neufeld, E.D.; Remaley, A.T.; et al. ABCA1 overexpression leads to hyperalphalipoproteinemia and increased biliary cholesterol excretion in transgenic mice. J. Clin. Investig. 2001, 108, 303–309. [Google Scholar] [CrossRef]
- Smith, J.D.; Miyata, M.; Ginsberg, M.; Grigaux, C.; Shmookler, E.; Plump, A.S. Cyclic AMP induces apolipoprotein E binding activity and promotes cholesterol efflux from a macrophage cell line to apolipoprotein acceptors. J. Biol. Chem. 1996, 271, 30647–30655. [Google Scholar] [CrossRef] [PubMed]
- Oram, J.F.; Lawn, R.M.; Garvin, M.R.; Wade, D.P. ABCA1 is the cAMP-inducible apolipoprotein receptor that mediates cholesterol secretion from macrophages. J. Biol. Chem. 2000, 275, 34508–34511. [Google Scholar] [CrossRef]
- Haidar, B.; Denis, M.; Krimbou, L.; Marcil, M.; Genest, J., Jr. cAMP induces ABCA1 phosphorylation activity and promotes cholesterol efflux from fibroblasts. J. Lipid Res. 2002, 43, 2087–2094. [Google Scholar] [CrossRef]
- Després, J.P.; Marette, A. Relation of components of insulin resistance syndrome to coronary disease risk. Curr. Opin. Lipidol. 1994, 5, 274–289. [Google Scholar] [CrossRef]
- Hergenç, G.; Schulte, H.; Assmann, G.; von Eckardstein, A. Associations of obesity markers, insulin, and sex hormones with HDL-cholesterol levels in Turkish and German individuals. Atherosclerosis 1999, 145, 147–156. [Google Scholar] [CrossRef]
- Karhapaa, P.; Malkki, M.; Laakso, M. Isolated low HDL cholesterol. An insulin-resistant state. Diabetes 1994, 43, 411–417. [Google Scholar] [CrossRef] [PubMed]
- von Eckardstein, A.; Schulte, H.; Assmann, G. Risk for diabetes mellitus in middle-aged Caucasian male participants of the PROCAM study: Implications for the definition of impaired fasting glucose by the american diabetes association. prospective cardiovascular munster. J. Clin. Endocrinol. Metab. 2000, 85, 3101–3108. [Google Scholar] [CrossRef] [PubMed]
- Holst, J.J.; Vilsbøll, T.; Deacon, C.F. The incretin system and its role in type 2 diabetes mellitus. Mol. Cell Endocrinol. 2009, 297, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Göke, R.; Fehmann, H.C.; Richter, G.; Trautmann, M.; Göke, B. Interaction of glucagon-like peptide-1(7-36)amide and somatostatin-14 in RINm5F cells and in the perfused rat pancreas. Pancreas 1989, 4, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Göke, R.; Kolligs, F.; Richter, G.; Lankat-Buttgereit, B.; Goke, B. Solubilization of active receptors for glucagon-like peptide-1(7-36)amide from rat lung membranes. Am. J. Physiol. 1993, 264, L146–L152. [Google Scholar] [CrossRef] [PubMed]
- Göke, R.; Oltmer, B.; Sheikh, S.P.; Goke, B. Solubilization of active GLP-1 (7-36)amide receptors from RINm5F plasma membranes. FEBS Lett. 1992, 300, 232–236. [Google Scholar] [CrossRef]
- Göke, R.; Trautmann, M.E.; Haus, E.; Richter, G.; Fehmann, H.C.; Arnold, R.; Göke, B. Signal transmission after GLP-1(7-36)amide binding in RINm5F cells. Am. J. Physiol. 1989, 257, G397–G401. [Google Scholar] [CrossRef]
- van Eyll, B.; Lankat-Buttgereit, B.; Bode, H.P.; Goke, R.; Goke, B. Signal transduction of the GLP-1-receptor cloned from a human insulinoma. FEBS Lett. 1994, 348, 7–13. [Google Scholar] [CrossRef]
- Dillon, J.S.; Tanizawa, Y.; Wheeler, M.B.; Leng, X.H.; Ligon, B.B.; Rabin, D.U.; Yoo-Warren, H.; Permutt, M.A.; Boyd, A.E., III. Cloning and functional expression of the human glucagon-like peptide-1 (GLP-1) receptor. Endocrinology 1993, 133, 1907–1910. [Google Scholar] [CrossRef]
- Thorens, B.; Porret, A.; Bühler, L.; Deng, S.P.; Morel, P.; Widmann, C. Cloning and functional expression of the human islet GLP-1 receptor. Demonstration that exendin-4 is an agonist and exendin-(9-39) an antagonist of the receptor. Diabetes 1993, 42, 1678–1682. [Google Scholar] [CrossRef]
- Graziano, M.P.; Hey, P.J.; Borkowski, D.; Chicchi, G.G.; Strader, C.D. Cloning and functional expression of a human glucagon-like peptide-1 receptor. Biochem. Biophys. Res. Commun. 1993, 196, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Mojsov, S. Tissue-specific expression of the human receptor for glucagon-like peptide-I: Brain, heart and pancreatic forms have the same deduced amino acid sequences. FEBS Lett. 1995, 358, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, M.; Mita, T.; Azuma, K.; Ebato, C.; Goto, H.; Nomiyama, T.; Fujitani, Y.; Hirose, T.; Kawamori, R.; Watada, H. Inhibition of monocyte adhesion to endothelial cells and attenuation of atherosclerotic lesion by a glucagon-like peptide-1 receptor agonist, exendin-4. Diabetes 2010, 59, 1030–1037. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, J.; Sugiyama, S.; Sugamura, K.; Nakamura, T.; Fujiwara, Y.; Akiyama, E.; Kurokawa, H.; Nozaki, T.; Ohba, K.; Konishi, M.; et al. A dipeptidyl peptidase-4 inhibitor, des-fluoro-sitagliptin, improves endothelial function and reduces atherosclerotic lesion formation in apolipoprotein E-deficient mice. J. Am. Coll. Cardiol. 2012, 59, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.; Li, C.; Guan, M.; Zheng, Z.; Li, J.; Xu, W.; Wang, L.; He, F.; Xue, Y. The DPP-4 inhibitor sitagliptin attenuates the progress of atherosclerosis in apolipoprotein-E-knockout mice via AMPK- and MAPK-dependent mechanisms. Cardiovasc. Diabetol. 2014, 13, 32. [Google Scholar] [CrossRef]
- Terasaki, M.; Nagashima, M.; Nohtomi, K.; Kohashi, K.; Tomoyasu, M.; Sinmura, K.; Nogi, Y.; Katayama, Y.; Sato, K.; Itoh, F.; et al. Preventive effect of dipeptidyl peptidase-4 inhibitor on atherosclerosis is mainly attributable to incretin’s actions in nondiabetic and diabetic apolipoprotein E-null mice. PLoS ONE 2013, 8, e70933. [Google Scholar] [CrossRef]
- Vittone, F.; Liberman, A.; Vasic, D.; Ostertag, R.; Esser, M.; Walcher, D.; Ludwig, A.; Marx, N.; Burgmaier, M. Sitagliptin reduces plaque macrophage content and stabilises arteriosclerotic lesions in Apoe (-/-) mice. Diabetologia 2012, 55, 2267–2275. [Google Scholar] [CrossRef]
- Zheng, S.L.; Roddick, A.J.; Aghar-Jaffar, R.; Shun-Shin, M.J.; Francis, D.; Oliver, N.; Meeran, K. Association between use of sodium-glucose cotransporter 2 inhibitors, glucagon-like peptide 1 agonists, and dipeptidyl peptidase 4 inhibitors with all-cause mortality in patients with type 2 diabetes: A systematic review and meta-analysis. JAMA 2018, 319, 1580–1591. [Google Scholar] [CrossRef]
- Drucker, D.J. The role of gut hormones in glucose homeostasis. J. Clin. Investig. 2007, 117, 24–32. [Google Scholar] [CrossRef]
- Ervinna, N.; Mita, T.; Yasunari, E.; Azuma, K.; Tanaka, R.; Fujimura, S.; Sukmawati, D.; Nomiyama, T.; Kanazawa, A.; Kawamori, R.; et al. Anagliptin, a DPP-4 inhibitor, suppresses proliferation of vascular smooth muscles and monocyte inflammatory reaction and attenuates atherosclerosis in male apo E-deficient mice. Endocrinology 2013, 154, 1260–1270. [Google Scholar] [CrossRef]
- Uehara, Y.; Miura, S.; von Eckardstein, A.; Abe, S.; Fujii, A.; Matsuo, Y.; Rust, S.; Lorkowski, S.; Assmann, G.; Yamada, T.; et al. Unsaturated fatty acids suppress the expression of the ATP-binding cassette transporter G1 (ABCG1) and ABCA1 genes via an LXR/RXR responsive element. Atherosclerosis 2007, 191, 11–21. [Google Scholar] [CrossRef] [PubMed]
- De Nigris, V.; Prattichizzo, F.; Iijima, H.; Ceriello, A. DPP-4 inhibitors have different effects on endothelial low-grade inflammation and on the M1-M2 macrophage polarization under hyperglycemic conditions. Diabetes Metab. Syndr. Obes. 2021, 14, 1519–1531. [Google Scholar] [CrossRef]
- Tanaka, M.; Matsuo, Y.; Yamakage, H.; Masuda, S.; Terada, Y.; Muranaka, K.; Wada, H.; Hasegawa, K.; Shimatsu, A.; Satoh-Asahara, N. Differential effects of GLP-1 receptor agonist on foam cell formation in monocytes between non-obese and obese subjects. Metabolism 2016, 65, 1–11. [Google Scholar] [CrossRef]
- Uehara, Y.; Engel, T.; Li, Z.; Goepfert, C.; Rust, S.; Zhou, X.; Langer, C.; Schachtrup, C.; Wiekowski, J.; Lorkowski, S.; et al. Polyunsaturated fatty acids and acetoacetate downregulate the expression of the ATP-binding cassette transporter A1. Diabetes 2002, 51, 2922–2928. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, R.; Yokoyama, S. Helical apolipoproteins stabilize ATP-binding cassette transporter A1 by protecting it from thiol protease-mediated degradation. J. Biol. Chem. 2002, 277, 22426–22429. [Google Scholar] [CrossRef] [PubMed]
- Uehara, Y.; Yamada, T.; Baba, Y.; Miura, S.; Abe, S.; Kitajima, K.; Higuchi, M.A.; Iwamoto, T.; Saku, K. ATP-binding cassette transporter G4 is highly expressed in microglia in Alzheimer’s brain. Brain Res. 2008, 1217, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Baggio, L.L.; Drucker, D.J. Biology of incretins: GLP-1 and GIP. Gastroenterology 2007, 132, 2131–2157. [Google Scholar] [CrossRef] [PubMed]
- Phillips, M.C. Molecular mechanisms of cellular cholesterol efflux. J. Biol. Chem. 2014, 289, 24020–24029. [Google Scholar] [CrossRef]
- Tashiro, Y.; Sato, K.; Watanabe, T.; Nohtomi, K.; Terasaki, M.; Nagashima, M.; Hirano, T. A glucagon-like peptide-1 analog liraglutide suppresses macrophage foam cell formation and atherosclerosis. Peptides 2014, 54, 19–26. [Google Scholar] [CrossRef]
- Nagashima, M.; Watanabe, T.; Terasaki, M.; Tomoyasu, M.; Nohtomi, K.; Kim-Kaneyama, J.; Miyazaki, A.; Hirano, T. Native incretins prevent the development of atherosclerotic lesions in apolipoprotein E knockout mice. Diabetologia 2011, 54, 2649–2659. [Google Scholar] [CrossRef]
- Marso, S.P.; Bain, S.C.; Consoli, A.; Eliaschewitz, F.G.; Jódar, E.; Leiter, L.A.; Lingvay, I.; Rosenstock, J.; Seufert, J.; Warren, M.L.; et al. Investigators semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 2016, 375, 1834–1844. [Google Scholar] [CrossRef]
- Diaz-Jimenez, D.; Petrillo, M.G.; Busada, J.T.; Hermoso, M.A.; Cidlowski, J.A. Glucocorticoids mobilize macrophages by transcriptionally up-regulating the exopeptidase DPP4. J. Biol. Chem. 2020, 295, 3213–3227. [Google Scholar] [CrossRef] [PubMed]
- Dullaart, R.P.; De Vries, R.; Scheek, L.; Borggreve, S.E.; Van Gent, T.; Dallinga-Thie, G.M.; Ito, M.; Nagano, M.; Sluiter, W.J.; Hattori, H.; et al. Type 2 diabetes mellitus is associated with differential effects on plasma cholesteryl ester transfer protein and phospholipid transfer protein activities and concentrations. Scand. J. Clin. Lab. Investig. 2004, 64, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Borggreve, S.E.; De Vries, R.; Dullaart, R.P. Alterations in high-density lipoprotein metabolism and reverse cholesterol transport in insulin resistance and type 2 diabetes mellitus: Role of lipolytic enzymes, lecithin:cholesterol acyltransferase and lipid transfer proteins. Eur. J. Clin. Investig. 2003, 33, 1051–1069. [Google Scholar] [CrossRef]
- Hu, Y.W.; Yang, J.Y.; Ma, X.; Chen, Z.P.; Hu, Y.R.; Zhao, J.Y.; Li, S.F.; Qiu, Y.R.; Lu, J.B.; Wang, Y.C.; et al. A lincRNA-DYNLRB2-2/GPR119/GLP-1R/ABCA1-dependent signal transduction pathway is essential for the regulation of cholesterol homeostasis. J. Lipid Res. 2014, 55, 681–697. [Google Scholar] [CrossRef]
- Yao, Y.; Li, Q.; Gao, P.; Wang, W.; Chen, L.; Zhang, J.; Xu, Y. Glucagon-like peptide-1 contributes to increases ABCA1 expression by downregulating miR-758 to regulate cholesterol homeostasis. Biochem. Biophys. Res. Commun. 2018, 497, 652–658. [Google Scholar] [CrossRef]
- Osto, E.; Doytcheva, P.; Corteville, C.; Bueter, M.; Dörig, C.; Stivala, S.; Buhmann, H.; Colin, S.; Rohrer, L.; Hasballa, R.; et al. Rapid and body weight-independent improvement of endothelial and high-density lipoprotein function after Roux-en-Y gastric bypass: Role of glucagon-like peptide-1. Circulation 2015, 131, 871–881. [Google Scholar] [CrossRef] [PubMed]
- Venkateswaran, A.; Laffitte, B.A.; Joseph, S.B.; Mak, P.A.; Wilpitz, D.C.; Edwards, P.A.; Tontonoz, P. Control of cellular cholesterol efflux by the nuclear oxysterol receptor LXR alpha. Proc. Natl. Acad. Sci. USA 2000, 97, 12097–12102. [Google Scholar] [CrossRef]
- Brubaker, P.L.; Drucker, D.J. Minireview: Glucagon-like peptides regulate cell proliferation and apoptosis in the pancreas, gut, and central nervous system. Endocrinology 2004, 145, 2653–2659. [Google Scholar] [CrossRef]
- See, R.H.; Caday-Malcolm, R.A.; Singaraja, R.R.; Zhou, S.; Silverston, A.; Huber, M.T.; Moran, J.; James, E.R.; Janoo, R.; Savill, J.M.; et al. Protein kinase A site-specific phosphorylation regulates ATP-binding cassette A1 (ABCA1)-mediated phospholipid efflux. J. Biol. Chem. 2002, 277, 41835–41842. [Google Scholar] [CrossRef]
- Wu, Y.R.; Shi, X.Y.; Ma, C.Y.; Zhang, Y.; Xu, R.X.; Li, J.J. Liraglutide improves lipid metabolism by enhancing cholesterol efflux associated with ABCA1 and ERK1/2 pathway. Cardiovasc. Diabetol. 2019, 18, 146. [Google Scholar] [CrossRef] [PubMed]
- Yin, Q.H.; Zhang, R.; Li, L.; Wang, Y.T.; Liu, J.P.; Zhang, J.; Bai, L.; Cheng, J.Q.; Fu, P.; Liu, F. Exendin-4 Ameliorates lipotoxicity-induced glomerular endothelial cell injury by improving ABC transporter A1-mediated cholesterol efflux in diabetic apoE knockout Mice. J. Biol. Chem. 2016, 291, 26487–26501. [Google Scholar] [CrossRef]
- Robichaux, W.G., III; Mei, F.C.; Yang, W.; Wang, H.; Sun, H.; Zhou, Z.; Milewicz, D.M.; Teng, B.B.; Cheng, X. Epac1 (Exchange protein directly activated by cAMP 1) upregulates LOX-1 (Oxidized low-density lipoprotein receptor 1) to promote foam cell formation and atherosclerosis development. Arterioscler. Thromb. Vasc. Biol. 2020, 40, e322–e335. [Google Scholar] [PubMed]
- Yamauchi, Y.; Hayashi, M.; Abe-Dohmae, S.; Yokoyama, S. Apolipoprotein A-I activates protein kinase C alpha signaling to phosphorylate and stabilize ATP binding cassette transporter A1 for the high density lipoprotein assembly. J. Biol. Chem. 2003, 278, 47890–47897. [Google Scholar] [PubMed]
- Tang, C.; Vaughan, A.M.; Oram, J.F. Janus kinase 2 modulates the apolipoprotein interactions with ABCA1 required for removing cellular cholesterol. J. Biol. Chem. 2004, 279, 7622–7628. [Google Scholar]
- Ogura, M.; Ayaori, M.; Terao, Y.; Hisada, T.; Iizuka, M.; Takiguchi, S.; Uto-Kondo, H.; Yakushiji, E.; Nakaya, K.; Sasaki, M.; et al. Proteasomal inhibition promotes ATP-binding cassette transporter A1 (ABCA1) and ABCG1 expression and cholesterol efflux from macrophages in vitro and in vivo. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 1980–1987. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Komatsu, T.; Abe, S.; Nakashima, S.; Sasaki, K.; Higaki, Y.; Saku, K.; Miura, S.-i.; Uehara, Y. Dipeptidyl Peptidase-4 Inhibitor Sitagliptin Phosphate Accelerates Cellular Cholesterol Efflux in THP-1 Cells. Biomolecules 2023, 13, 228. https://doi.org/10.3390/biom13020228
Komatsu T, Abe S, Nakashima S, Sasaki K, Higaki Y, Saku K, Miura S-i, Uehara Y. Dipeptidyl Peptidase-4 Inhibitor Sitagliptin Phosphate Accelerates Cellular Cholesterol Efflux in THP-1 Cells. Biomolecules. 2023; 13(2):228. https://doi.org/10.3390/biom13020228
Chicago/Turabian StyleKomatsu, Tomohiro, Satomi Abe, Shihoko Nakashima, Kei Sasaki, Yasuki Higaki, Keijiro Saku, Shin-ichiro Miura, and Yoshinari Uehara. 2023. "Dipeptidyl Peptidase-4 Inhibitor Sitagliptin Phosphate Accelerates Cellular Cholesterol Efflux in THP-1 Cells" Biomolecules 13, no. 2: 228. https://doi.org/10.3390/biom13020228
APA StyleKomatsu, T., Abe, S., Nakashima, S., Sasaki, K., Higaki, Y., Saku, K., Miura, S.-i., & Uehara, Y. (2023). Dipeptidyl Peptidase-4 Inhibitor Sitagliptin Phosphate Accelerates Cellular Cholesterol Efflux in THP-1 Cells. Biomolecules, 13(2), 228. https://doi.org/10.3390/biom13020228






