ORAI Ca2+ Channels in Cancers and Therapeutic Interventions
Abstract
:1. Introduction
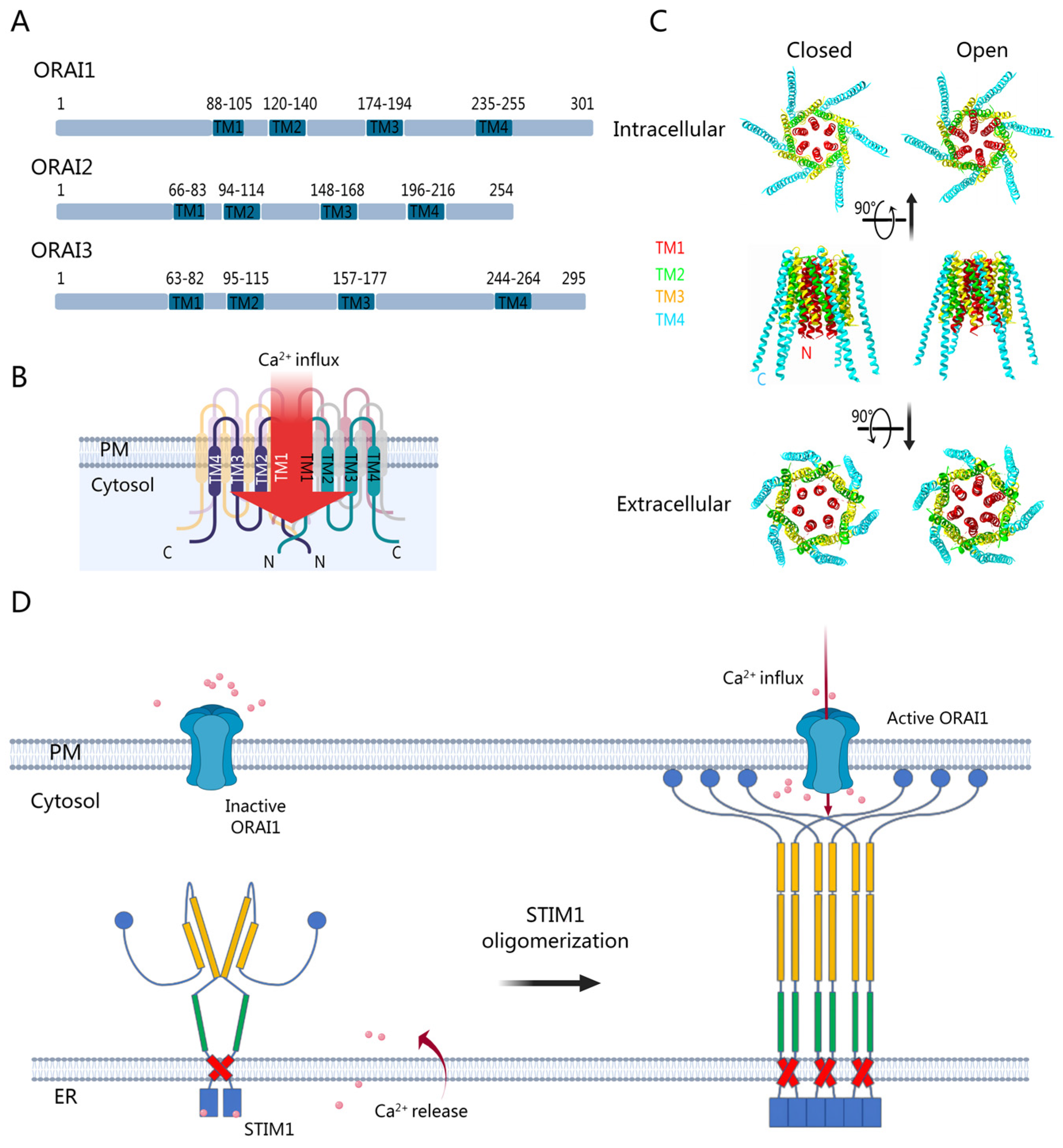
2. ORAI Activation and Modulation
2.1. The Mechanism of ORAI Channel Activation and Inactivation
2.2. Mutations and Post-Translational Modifications of ORAI in Diseases
2.3. Techniques to Modulate ORAI Channel Function
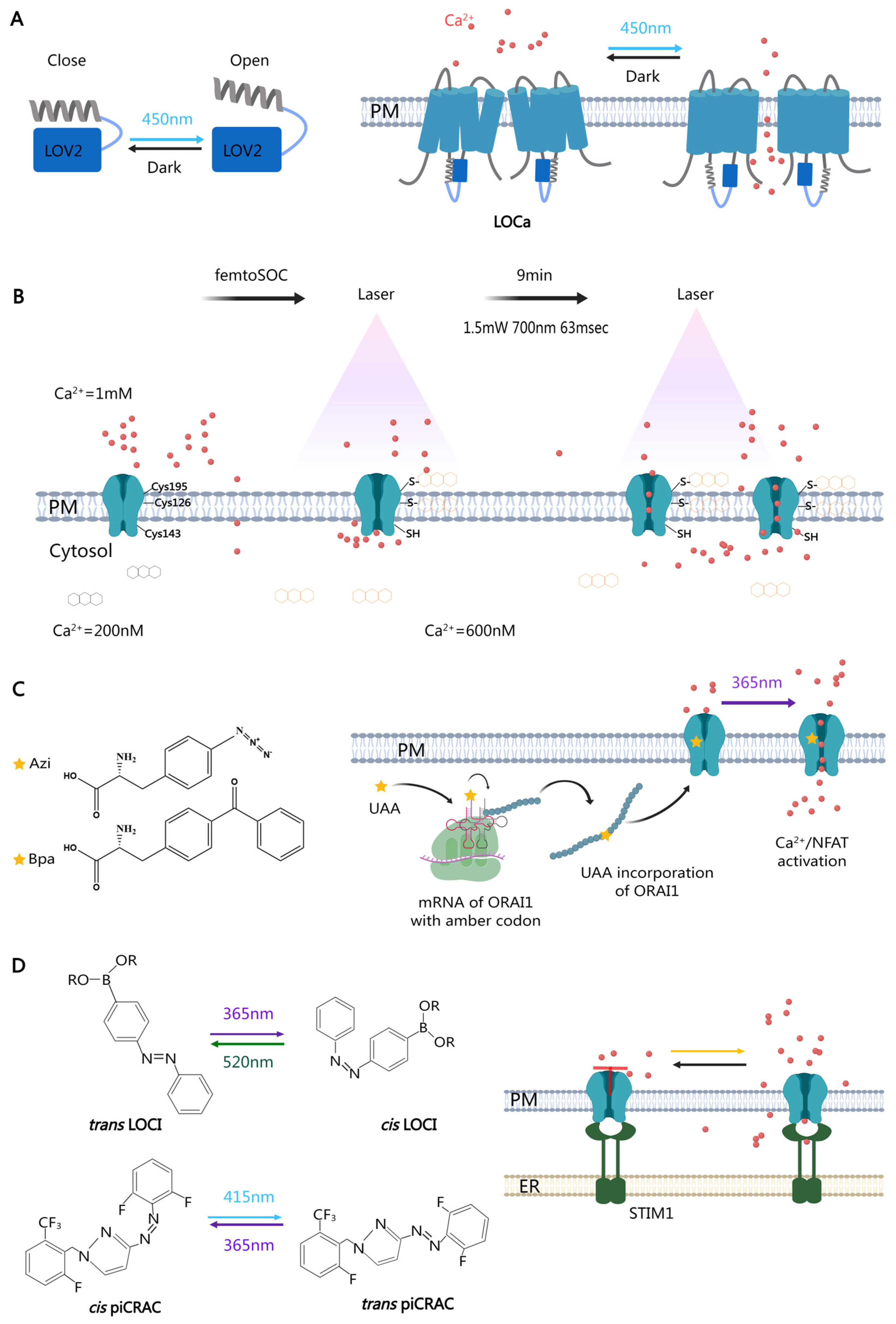
2.3.1. Optical Tools in ORAI Regulation
2.3.2. Novel Pharmacological Inhibitors for the ORAI Channel
2.3.3. ORAI1-Targeted Antibodies
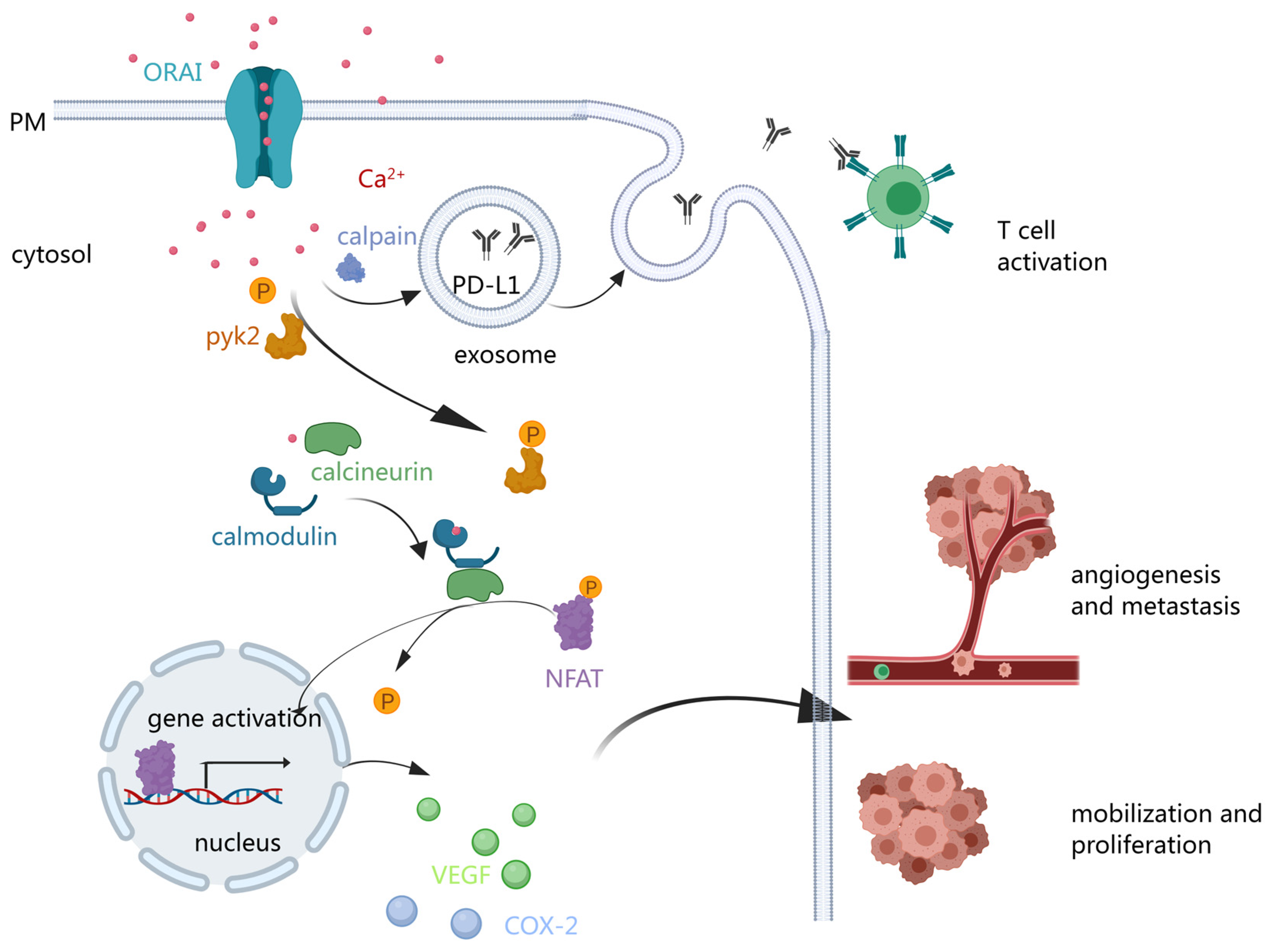
3. ORAI and Cancers
3.1. ORAI Expression and Its Role in Various Cancers
3.2. ORAI-Mediated Cancer Cell Epithelial-to-Mesenchymal Transition and Invasion
3.3. ORAI in Tumor Angiogenesis and Metastasis
3.4. ORAI and Carcinoma Immunity
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gao, X.H.; Di, X.H.; Li, J.J.; Kang, Y.T.; Xie, W.J.; Sun, L.J.; Zhang, J.B. Extracellular Calcium-Induced Calcium Transient Regulating the Proliferation of Osteoblasts through Glycolysis Metabolism Pathways. Int. J. Mol. Sci. 2023, 24, 4991. [Google Scholar] [CrossRef]
- Hammad, A.S.; Machaca, K. Store Operated Calcium Entry in Cell Migration and Cancer Metastasis. Cells 2021, 10, 1246. [Google Scholar] [CrossRef] [PubMed]
- Estacion, M.; Mordan, L.J. PDGF-stimulated calcium influx changes during in vitro cell transformation. Cell. Signal. 1997, 9, 363–366. [Google Scholar] [CrossRef]
- Perrone, M.; Patergnani, S.; Di Mambro, T.; Palumbo, L.; Wieckowski, M.R.; Giorgi, C.; Pinton, P. Calcium Homeostasis in the Control of Mitophagy. Antioxid. Redox Sign. 2023, 38, 581–598. [Google Scholar] [CrossRef]
- Putney, J.W. A Model for Receptor-Regulated Calcium Entry. Cell Calcium 1986, 7, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Krizova, A.; Maltan, L.; Derler, I. Critical parameters maintaining authentic CRAC channel hallmarks. Eur. Biophys. J. 2019, 48, 425–445. [Google Scholar] [CrossRef]
- Fahrner, M.; Pandey, S.K.; Muik, M.; Traxler, L.; Butorac, C.; Stadlbauer, M.; Zayats, V.; Krizova, A.; Plenk, P.; Frischauf, I.; et al. Communication between N terminus and loop2 tunes Orai activation. J. Biol. Chem. 2018, 293, 1271–1285. [Google Scholar] [CrossRef] [PubMed]
- Frischauf, I.; Muik, M.; Derler, I.; Bergsmann, J.; Fahrner, M.; Schindl, R.; Groschner, K.; Romanin, C. Molecular determinants of the coupling between STIM1 and Orai channels: Differential activation of Orai1-3 channels by a STIM1 coiled-coil mutant. J. Biol. Chem. 2009, 284, 21696–21706. [Google Scholar] [CrossRef]
- Derler, I.; Butorac, C.; Krizova, A.; Stadlbauer, M.; Muik, M.; Fahrner, M.; Frischauf, I.; Romanin, C. Authentic CRAC channel activity requires STIM1 and the conserved portion of the Orai N terminus. J. Biol. Chem. 2018, 293, 1259–1270. [Google Scholar] [CrossRef]
- Zhang, X.; Xin, P.; Yoast, R.E.; Emrich, S.M.; Johnson, M.T.; Pathak, T.; Benson, J.C.; Azimi, I.; Gill, D.L.; Monteith, G.R.; et al. Distinct pharmacological profiles of ORAI1, ORAI2, and ORAI3 channels. Cell Calcium 2020, 91, 102281. [Google Scholar] [CrossRef]
- Yoast, R.E.; Emrich, S.M.; Zhang, X.; Xin, P.; Johnson, M.T.; Fike, A.J.; Walter, V.; Hempel, N.; Yule, D.I.; Sneyd, J.; et al. The native ORAI channel trio underlies the diversity of Ca(2+) signaling events. Nat. Commun. 2020, 11, 2444. [Google Scholar] [CrossRef] [PubMed]
- Yoast, R.E.; Emrich, S.M.; Trebak, M. The anatomy of native CRAC channel(s). Curr. Opin. Physiol. 2020, 17, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Feske, S.; Gwack, Y.; Prakriya, M.; Srikanth, S.; Puppel, S.H.; Tanasa, B.; Hogan, P.G.; Lewis, R.S.; Daly, M.; Rao, A. A mutation in Orai1 causes immune deficiency by abrogating CRAC channel function. Nature 2006, 441, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.B.; Ramachandran, S.; Oh-hora, M.; Rao, A.; Hogan, P.G. Pore architecture of the ORAI1 store-operated calcium channel. Proc. Natl. Acad. Sci. USA 2010, 107, 4896–4901. [Google Scholar] [CrossRef]
- Hou, X.W.; Pedi, L.; Diver, M.M.; Long, S.B. Crystal Structure of the Calcium Release-Activated Calcium Channel Orai. Science 2012, 338, 1308–1313. [Google Scholar] [CrossRef] [PubMed]
- Hou, X.W.; Burstein, S.R.; Long, S.B. Structures Reveal Opening of the Store-Operated Calcium Channel ORAI. Biophys. J. 2019, 116, 302a. [Google Scholar] [CrossRef]
- Cai, X.Y.; Zhou, Y.D.; Nwokonko, R.M.; Loktionova, N.A.; Wang, X.M.; Xin, P.; Trebak, M.; Wang, Y.J.; Gill, D.L. The Orai1 Store-operated Calcium Channel Functions as a Hexamer. J. Biol. Chem. 2016, 291, 25764–25775. [Google Scholar] [CrossRef] [PubMed]
- Yen, M.; Lokteva, L.A.; Lewis, R.S. Functional Analysis of Orai1 Concatemers Supports a Hexameric Stoichiometry for the CRAC Channel. Biophys. J. 2016, 111, 1897–1907. [Google Scholar] [CrossRef] [PubMed]
- Cendula, R.; Dragún, M.; Gazová, A.; Kyselovic, J.; Hulman, M.; Mátus, M. Changes in STIM Isoforms Expression and Gender-Specific Alterations in Orai Expression in Human Heart Failure. Physiol. Res. 2019, 68, S165–S172. [Google Scholar] [CrossRef]
- Dubois, C.; Vanden Abeele, F.; Lehen’kyi, V.; Gkika, D.; Guarmit, B.; Lepage, G.; Slomianny, C.; Borowiec, A.S.; Bidaux, G.; Benahmed, M.; et al. Remodeling of Channel-Forming ORAI Proteins Determines an Oncogenic Switch in Prostate Cancer. Cancer Cell 2014, 26, 19–32. [Google Scholar] [CrossRef]
- Li, S.; Yao, M.L.; Niu, C.Q.; Liu, D.; Tang, Z.M.; Gu, C.M.; Zhao, H.Y.; Ke, J.; Wu, S.Y.; Wang, X.; et al. Inhibition of MCF-7 breast cancer cell proliferation by a synthetic peptide derived from the C-terminal sequence of Orai channel. Biochem. Biophys. Res. Commun. 2019, 516, 1066–1072. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, N.; Lindemann, O.; Schwab, A. TRP channels and STIM/ORAI proteins: Sensors and effectors of cancer and stroma cell migration. Br. J. Pharmacol. 2014, 171, 5524–5540. [Google Scholar] [CrossRef] [PubMed]
- Baraniak, J.H.; Zhou, Y.D.; Nwokonko, R.M.; Jennette, M.R.; Kazzaz, S.A.; Stenson, J.M.; Whitsell, A.L.; Wang, Y.J.; Trebak, M.; Gill, D.L. Orai channel C-terminal peptides are key modulators of STIM-Orai coupling and calcium signal generation. Cell Rep. 2021, 35, 109322. [Google Scholar] [CrossRef] [PubMed]
- Palty, R.; Stanley, C.; Isacoff, E.Y. Critical role for Orai1 C-terminal domain and TM4 in CRAC channel gating. Cell Res. 2015, 25, 963–980. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.F.; Wu, G.Y.; Yu, Y.; Chen, X.Z.; Ji, R.C.; Lu, J.; Li, X.; Zhang, X.; Yang, X.; Shen, Y.Q. Molecular understanding of calcium permeation through the open Orai channel. PLoS Biol. 2019, 17, e3000096. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.; Han, W.D.; Cao, W.M.; Wang, Y.J.; Wen, S.F.; Huang, Y.; Li, M.Y.; Du, L.P.; Zhou, Y.B. Store-Operated Calcium Entry Mediated by ORAI and STIM. Compr. Physiol. 2018, 8, 981–1002. [Google Scholar] [CrossRef] [PubMed]
- Yeung, P.S.W.; Yamashita, M.; Prakriya, M. A pathogenic human Orai1 mutation unmasks STIM1-independent rapid inactivation of Orai1 channels. eLife 2023, 12, e82281. [Google Scholar] [CrossRef] [PubMed]
- Tiffner, A.; Schober, R.; Höglinger, C.; Bonhenry, D.; Pandey, S.; Lunz, V.; Sallinger, M.; Frischauf, I.; Fahrner, M.; Lindinger, S.; et al. CRAC channel opening is determined by a series of Orai1 gating checkpoints in the transmembrane and cytosolic regions. J. Biol. Chem. 2021, 296, 100224. [Google Scholar] [CrossRef]
- McCarl, C.A.; Picard, C.; Khalil, S.; Kawasaki, T.; Röther, J.; Papolos, A.; Kutok, J.; Hivroz, C.; LeDeist, F.; Plogmann, K.; et al. ORAI1 deficiency and lack of store-operated Ca2+ entry cause immunodeficiency, myopathy, and ectodermal dysplasia. J. Allergy Clin. Immun. 2009, 124, 1311–1318. [Google Scholar] [CrossRef]
- Partiseti, M.; Ledeist, F.; Hivroz, C.; Fischer, A.; Korn, H.; Choquet, D. The Calcium Current Activated by T-Cell Receptor and Store Depletion in Human-Lymphocytes Is Absent in a Primary Immunodeficiency. J. Biol. Chem. 1994, 269, 32327–32335. [Google Scholar] [CrossRef]
- Feske, S.; Prakriya, M.; Lewis, R.S.; Rao, A. Defect in CRAC Ca2+ channel function associated with altered K+ channel gating properties in T cells from immunodeficient patients. FASEB J. 2005, 19, A1163. [Google Scholar]
- Garibaldi, M.; Fattori, F.; Riva, B.; Labasse, C.; Brochier, G.; Ottaviani, P.; Sacconi, S.; Vizzaccaro, E.; Laschena, F.; Romero, N.B.; et al. A novel gain-of-function mutation in ORAI1 causes late-onset tubular aggregate myopathy and congenital miosis. Clin. Genet. 2017, 91, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Böhm, J.; Bulla, M.; Urquhart, J.E.; Malfatti, E.; Williams, S.G.; O’Sullivan, J.; Szlauer, A.; Koch, C.; Baranello, G.; Mora, M.; et al. ORAI1 Mutations with Distinct Channel Gating Defects in Tubular Aggregate Myopathy. Hum. Mutat. 2017, 38, 426–438. [Google Scholar] [CrossRef]
- Lian, J.; Cuk, M.; Kahlfuss, S.; Kozhaya, L.; Vaeth, M.; Rieux-Laucat, F.; Picard, C.; Benson, M.J.; Jakovcevic, A.; Bilic, K.; et al. ORAI1 mutations abolishing store-operated Ca2+ entry cause anhidrotic ectodermal dysplasia with immunodeficiency. J. Allergy Clin. Immun. 2018, 142, 1297–1310.e11. [Google Scholar] [CrossRef]
- Ledeist, F.; Hivroz, C.; Partiseti, M.; Thomas, C.; Buc, H.A.; Oleastro, M.; Belohradsky, B.; Choquet, D.; Fischer, A. A Primary T-Cell Immunodeficiency Associated with Defective Transmembrane Calcium Influx. Blood 1995, 85, 1053–1062. [Google Scholar] [CrossRef]
- Bulla, M.; Gyimesi, G.; Kim, J.H.; Bhardwaj, R.; Hediger, M.A.; Frieden, M.; Demaurex, N. ORAI1 channel gating and selectivity is differentially altered by natural mutations in the first or third transmembrane domain. J. Physiol. 2019, 597, 561–582. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.; Agrebi, N.; Mackeh, R.; Abouhazima, K.; KhudaBakhsh, K.; Adeli, M.; Lo, B.; Hassan, A.; Machaca, K. Novel ORAI1 Mutation Disrupts Channel Trafficking Resulting in Combined Immunodeficiency. J. Clin. Immunol. 2021, 41, 1004–1015. [Google Scholar] [CrossRef]
- Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature 2012, 487, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Endo, Y.; Noguchi, S.; Hara, Y.; Hayashi, Y.K.; Motomura, K.; Miyatake, S.; Murakami, N.; Tanaka, S.; Yamashita, S.; Kizu, R.; et al. Dominant mutations in ORAI1 cause tubular aggregate myopathy with hypocalcemia via constitutive activation of store-operated Ca2+ channels. Hum. Mol. Genet. 2015, 24, 637–648. [Google Scholar] [CrossRef]
- The Cancer Genome Atlas Research Network, Comprehensive molecular characterization of gastric adenocarcinoma. Nature 2014, 513, 202–209. [CrossRef]
- Getz, G.; Gabriel, S.B.; Cibulskis, K.; Lander, E.; Sivachenko, A.; Sougnez, C.; Lawrence, M.; Kandoth, C.; Dooling, D.; Fulton, R.; et al. Integrated genomic characterization of endometrial carcinoma. Nature 2013, 497, 67–73. [Google Scholar] [CrossRef]
- Chou, J.; Badran, Y.R.; Yee, C.S.K.; Bainter, W.; Ohsumi, T.K.; Al-Hammadi, S.; Pai, S.Y.; Feske, S.; Geha, R.S. A novel mutation in ORAI1 presenting with combined immunodeficiency and residual T-cell function. J. Allergy Clin. Immun. 2015, 136, 479–482.e1. [Google Scholar] [CrossRef] [PubMed]
- Gwack, Y.; Srikanth, S.; Feske, S.; Cruz-Guilloty, F.; Oh-hora, M.; Neems, D.S.; Hogan, P.G.; Rao, A. Biochemical and functional characterization of Orai proteins. J. Biol. Chem. 2007, 282, 16232–16243. [Google Scholar] [CrossRef] [PubMed]
- Nesin, V.; Wiley, G.; Kousi, M.; Ong, E.C.; Lehmann, T.; Nicholl, D.J.; Suri, M.; Shahrizaila, N.; Katsanis, N.; Gaffney, P.M.; et al. Activating mutations in STIM1 and ORAI1 cause overlapping syndromes of tubular myopathy and congenital miosis. Proc. Natl. Acad. Sci. USA 2014, 111, 4197–4202. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, M.S.; Sougnez, C.; Lichtenstein, L.; Cibulskisl, K.; Lander, E.; Gabriel, S.B.; Getz, G.; Ally, A.; Balasundaram, M.; Birol, I.; et al. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 2015, 517, 576–582. [Google Scholar] [CrossRef]
- Feske, S.; Picard, C.; Fischer, A. Immunodeficiency due to mutations in ORAI1 and STIM1. Clin. Immunol. 2010, 135, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Bergmeier, W.; Weidinger, C.; Zee, I.; Feske, S. Emerging roles of store-operated Ca entry through STIM and ORAI proteins in immunity, hemostasis and cancer. Channels 2013, 7, 379–391. [Google Scholar] [CrossRef]
- Lacruz, R.S.; Feske, S. Diseases caused by mutations in ORAI1 and STIM1. Ann. N. Y. Acad. Sci. 2015, 1356, 45–79. [Google Scholar] [CrossRef]
- Didier, M.B.; Frieden, M.; Demaurex, N. Orai1 Mutations with Distinct Channel Gating Defects cause Tubular Aggregate Myopathy. Biophys. J. 2017, 112, 538a. [Google Scholar]
- Johnson, J.; Blackman, R.; Gross, S.; Soboloff, J. Control of STIM and Orai function by post-translational modifications. Cell Calcium 2022, 103, 102544. [Google Scholar] [CrossRef]
- Lin, J.; Xie, Z.; Zhu, H.; Qian, J. Understanding protein phosphorylation on a systems level. Brief. Funct. Genomics 2010, 9, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Kawasaki, T.; Ueyama, T.; Lange, I.; Feske, S.; Saito, N. Protein Kinase C-induced Phosphorylation of Orai1 Regulates the Intracellular Ca2+ Level via the Store-operated Ca2+ Channel. J. Biol. Chem. 2010, 285, 25720–25730. [Google Scholar] [CrossRef] [PubMed]
- Hooper, R.; Zhang, X.X.; Webster, M.; Go, C.; Kedra, J.; Marchbank, K.; Gill, D.L.; Weeraratna, A.T.; Trebak, M.; Soboloff, J. Novel Protein Kinase C-Mediated Control of Orai1 Function in Invasive Melanoma. Mol. Cell Biol. 2015, 35, 2790–2798. [Google Scholar] [CrossRef] [PubMed]
- Dörr, K.; Kilch, T.; Kappel, S.; Alansary, D.; Schwär, G.; Niemeyer, B.A.; Peinelt, C. Cell type-specific glycosylation of Orai1 modulates store-operated Ca entry. Sci. Signal. 2016, 9, ra25. [Google Scholar] [CrossRef] [PubMed]
- Kilch, T.; Alansary, D.; Peglow, M.; Dörr, K.; Rychkov, G.; Rieger, H.; Peinelt, C.; Niemeyer, B.A. Mutations of the Ca2+-sensing Stromal Interaction Molecule STIM1 Regulate Ca2+ Influx by Altered Oligomerization of STIM1 and by Destabilization of the Ca2+ Channel Orai1. J. Biol. Chem. 2013, 288, 1653–1664. [Google Scholar] [CrossRef] [PubMed]
- West, S.J.; Kodakandla, G.; Wang, Q.C.; Tewari, R.; Zhu, M.X.; Boehning, D.; Akimzhanov, A.M. S-acylation of Orai1 regulates store-operated Ca2+ entry. J. Cell Sci. 2022, 135, jcs258579. [Google Scholar] [CrossRef] [PubMed]
- Ma, G.L.; Zhang, Q.; He, L.; Nguyen, N.T.; Liu, S.Z.; Gong, Z.J.; Huang, Y.; Zhou, Y.B. Genetically encoded tags for real time dissection of protein assembly in living cells. Chem. Sci. 2018, 9, 5551–5555. [Google Scholar] [CrossRef] [PubMed]
- Tan, P.; He, L.; Huang, Y.; Zhou, Y.B. Optophysiology: Illuminating Cell Physiology with Optogenetics. Physiol. Rev. 2022, 102, 1263–1325. [Google Scholar] [CrossRef]
- He, L.; Zhang, Q.; Huang, Y.; Zhou, Y.B. Optogenetic Approaches to Control Calcium Entry in Non-Excitable Cells. In Calcium Entry Channels in Non-Excitable Cells; Kozak, J.A., Putney, J.W., Jr., Eds.; CRC Press/Taylor & Francis: Boca Raton, FL, USA, 2018; Volume 8, pp. 145–160. [Google Scholar]
- He, L.; Zhang, Y.W.; Ma, G.L.; Tan, P.; Li, Z.J.; Zang, S.B.; Wu, X.; Jing, J.; Fang, S.H.; Zhou, L.J.; et al. Near-infrared photoactivatable control of Ca signaling and optogenetic immunomodulation. eLife 2015, 4, e10024. [Google Scholar] [CrossRef]
- Ma, G.L.; Wen, S.F.; Huang, Y.; Zhou, Y.B. The STIM-Orai Pathway: Light-Operated Ca2+ Entry Through Engineered CRAC Channels. Adv. Exp. Med. Biol. 2017, 993, 117–138. [Google Scholar] [CrossRef]
- Nguyen, N.T.; Ma, G.L.; Lin, E.N.; D’Souza, B.; Jing, J.; He, L.; Huang, Y.; Zhou, Y.B. CRAC channel-based optogenetics. Cell Calcium 2018, 75, 79–88. [Google Scholar] [CrossRef]
- Ishii, T.; Sato, K.; Kakumoto, T.; Miura, S.; Touhara, K.; Takeuchi, S.; Nakata, T. Light generation of intracellular Ca2+ signals by a genetically encoded protein BACCS. Nat. Commun. 2015, 6, 8021. [Google Scholar] [CrossRef]
- He, L.; Wang, L.Q.; Zeng, H.X.; Tan, P.; Ma, G.L.; Zheng, S.S.; Li, Y.X.; Sun, L.; Dou, F.; Siwko, S.; et al. Engineering of a bona fide light-operated calcium channel. Nat. Commun. 2021, 12, 164. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Tian, X.Y.; Tang, W.Y.; Cheng, J.; Bao, J.; Wang, H.P.; Zheng, S.S.; Wang, Y.J.; Wei, X.B.; Chen, T.N.; et al. Direct control of store-operated calcium channels by ultrafast laser. Cell Res. 2021, 31, 758–772. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.Q.; Sun, X.W.; Lu, L.J.; Marie, A.; Carrel, D.; Zhao, S.; Mille, C.; Song, Q.; Zhang, Y.; Ye, S.X. Optoproteomics elucidates the interactome of L-type amino acid transporter 3 (LAT3). Chem. Commun. 2021, 57, 4734–4737. [Google Scholar] [CrossRef]
- Chen, Y.T.; Lu, L.J.; Ye, S.X. Genetic Code Expansion and Optoproteomics. Yale J. Biol. Med. 2017, 90, 599–610. [Google Scholar]
- Maltan, L.; Weiss, S.; Najjar, H.; Leopold, M.; Lindinger, S.; Höglinger, C.; Höbarth, L.; Sallinger, M.; Grabmayr, H.; Berlansky, S.; et al. Photocrosslinking-induced CRAC channel-like Orai1 activation independent of STIM1. Nat. Commun. 2023, 14, 1286. [Google Scholar] [CrossRef]
- Nödling, A.R.; Spear, L.A.; Williams, T.L.; Luk, L.Y.P.; Tsai, Y.H. Using genetically incorporated unnatural amino acids to control protein functions in mammalian cells. Essays Biochem. 2019, 63, 237–266. [Google Scholar] [CrossRef] [PubMed]
- Coin, I. Application of non-canonical crosslinking amino acids to study protein-protein interactions in live cells. Curr. Opin. Chem. Biol. 2018, 46, 156–163. [Google Scholar] [CrossRef]
- Shawer, H.; Norman, K.; Cheng, C.W.; Foster, R.; Beech, D.J.; Bailey, M.A. ORAI1 Ca2+ Channel as a Therapeutic Target in Pathological Vascular Remodelling. Front. Cell Dev. Biol. 2021, 9, 653812. [Google Scholar] [CrossRef]
- Stauderman, K.A. CRAC channels as targets for drug discovery and development. Cell Calcium 2018, 74, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Gerasimenko, O.V.; Gerasimenko, J.V. CRAC channel inhibitors in pancreatic pathologies. J. Physiol. 2022, 600, 1597–1598. [Google Scholar] [CrossRef] [PubMed]
- Tian, C.S.; Du, L.P.; Zhou, Y.B.; Li, M.Y. Store-operated CRAC channel inhibitors: Opportunities and challenges. Future Med. Chem. 2016, 8, 817–832. [Google Scholar] [CrossRef] [PubMed]
- Viswanadha, S.; Nyayapathy, S.; Veeraraghavan, S.; Vakkalanka, S. Antitumor activity of RP4010, a novel small-molecule inhibitor of the calcium release-activated calcium (CRAC) channel pathway. Mol. Cancer Ther. 2018, 17, B127. [Google Scholar] [CrossRef]
- Miller, J.; Bruen, C.; Schnaus, M.; Zhang, J.; Ali, S.; Lind, A.; Stoecker, Z.; Stauderman, K.; Hebbar, S. Auxora versus standard of care for the treatment of severe or critical COVID-19 pneumonia: Results from a randomized controlled trial. Crit. Care 2020, 24, 502. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Wrennall, J.A.; Goriounova, A.S.; Sekhri, M.; Iskarpatyoti, J.A.; Ghosh, A.; Abdelwahab, S.H.; Voeller, A.; Rai, M.; Mahida, R.Y.; et al. Specific Inhibition of Orai1-mediated Calcium Signalling Resolves Inflammation and Clears Bacteria in an ARDS Model. Am. J. Respir. Crit. Care Med. 2023, 209, 703–715. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.J.; Wang, F.F.; Chen, Y.; Liang, X.Y.; Yin, Y.; Liu, H.; Luo, G.Q.; Li, Y.P.; Liang, S.P.; Wang, Y.J.; et al. Molecular action mechanisms of two novel and selective calcium release-activated calcium channel antagonists. Int. J. Biol. Macromol. 2023, 253, 126937. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.M.; Tang, B.; Chen, Y.L.; Zhou, L.J.; Deng, J.W.; Han, L.; Zhai, Y.G.; Zhou, Y.D.; Gill, D.L.; Lu, C.J.; et al. Celastrol inhibits store operated calcium entry and suppresses psoriasis. Front. Pharmacol. 2023, 14, 1111798. [Google Scholar] [CrossRef] [PubMed]
- Udasin, R.; Sil, A.; Zomot, E.; Cohen, H.A.; Haj, J.; Engelmayer, N.; Lev, S.; Binshtok, A.M.; Shaked, Y.; Kienzler, M.A.; et al. Photopharmacological modulation of native CRAC channels using azoboronate photoswitches. Proc. Natl. Acad. Sci. USA 2022, 119, e2118160119. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.Y.; Ma, G.L.; Zheng, S.S.; Qin, X.J.; Li, X.; Du, L.P.; Wang, Y.J.; Zhou, Y.B.; Li, M.Y. Optical Control of CRAC Channels Using Photoswitchable Azopyrazoles. J. Am. Chem. Soc. 2020, 142, 9460–9470. [Google Scholar] [CrossRef]
- Tscherrig, D.; Bhardwaj, R.; Biner, D.; Dernič, J.; Ross-Kaschitza, D.; Peinelt, C.; Hediger, M.A.; Lochner, M. Development of chemical tools based on GSK-7975A to study store-operated calcium entry in cells. Cell Calcium 2024, 117, 102834. [Google Scholar] [CrossRef] [PubMed]
- Jardin, I.; Lopez, J.J.; Salido, G.M.; Rosado, J.A. Orai1 mediates the interaction between STIM1 and hTRPC1 and regulates the mode of activation of hTRPC1-forming Ca channels. J. Biol. Chem. 2008, 283, 25296–25304. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.F.; Elliott, R.; Colombero, A.; Gaida, K.; Kelley, L.; Moksa, A.; Ho, S.Y.; Bykova, E.; Wong, M.; Rathanaswami, P.; et al. Generation and Characterization of Fully Human Monoclonal Antibodies Against Human Orai1 for Autoimmune Disease. J. Pharmacol. Exp. Ther. 2013, 345, 225–238. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.H.; Hussell, S.; Sondergaard, H.; Roepstorff, K.; Bui, J.V.; Deer, J.R.; Zhang, J.; Li, Z.G.; Lamberth, K.; Kvist, P.H.; et al. Antibody-Mediated Targeting of the Orai1 Calcium Channel Inhibits T Cell Function. PLoS ONE 2013, 8, e82944. [Google Scholar] [CrossRef] [PubMed]
- Gaida, K.; Salimi-Moosavi, H.; Subramanian, R.; Almon, V.; Knize, A.; Zhang, M.; Lin, F.F.; Nguyen, H.Q.; Zhou, L.; Sullivan, J.K.; et al. Inhibition of CRAC with a human anti-ORAI1 monoclonal antibody inhibits T-cell-derived cytokine production but fails to inhibit a T-cell-dependent antibody response in the cynomolgus monkey. J. Immunotoxicol. 2015, 12, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, I.A.D.; Ferreira, S.R.D.; Fernandes, J.M.; Silva, B.A.D.; Vasconcelos, L.H.C.; Cavalcante, F.A. A review of the pathophysiology and the role of ion channels on bronchial asthma. Front. Pharmacol. 2023, 14, 1236550. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.H.; Gao, H.W.; Gao, D.D.; Yang, W.Y.; Zhao, M.K.; Shen, B.; Hu, M. Exercise Reduces Airway Smooth Muscle Contraction in Asthmatic Rats via Inhibition of IL-4 Secretion and Store-Operated Ca2+ Entry Pathway. Allergy Asthma Immunol. Res. 2023, 15, 361–373. [Google Scholar] [CrossRef] [PubMed]
- Howard, E.; Hurrell, B.P.; Helou, D.G.; Shafiei-Jahani, P.; Hasiakos, S.; Painter, J.; Srikanth, S.; Gwack, Y.; Akbari, O. Orai inhibition modulates pulmonary ILC2 metabolism and alleviates airway hyperreactivity in murine and humanized models. Nat. Commun. 2023, 14, 5989. [Google Scholar] [CrossRef] [PubMed]
- Angulo, J.; Fernandez, A.; Sevilleja-Ortiz, A.; Sanchez-Ferrer, A.; Rodriguez-Manas, L.; El Assar, M. Upregulation of Orai Channels Contributes to Aging-Related Vascular Alterations in Rat Coronary Arteries. Int. J. Mol. Sci. 2023, 24, 13402. [Google Scholar] [CrossRef]
- El Assar, M.; Garcia-Rojo, E.; Sevilleja-Ortiz, A.; Sanchez-Ferrer, A.; Fernandez, A.; Garcia-Gomez, B.; Romero-Otero, J.; Rodriguez-Manas, L.; Angulo, J. Functional Role of STIM-1 and Orai1 in Human Microvascular Aging. Cells 2022, 11, 3675. [Google Scholar] [CrossRef]
- Cendula, R.; Chomanicova, N.; Adamickova, A.; Gazova, A.; Kyselovic, J.; Matus, M. Altered Expression of ORAI and STIM Isoforms in Activated Human Cardiac Fibroblasts. Physiol. Res. 2021, 70, S21–S30. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Zhang, W.; He, Y.; Ma, X.; Li, M.; Jiang, Q.; Loor, J.J.; Lv, X.; Yang, W.; Xu, C. Store-operated Ca2+ entry-sensitive glycolysis regulates neutrophil adhesion and phagocytosis in dairy cows with subclinical hypocalcemia. J. Dairy Sci. 2023, 106, 7131–7146. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Fang, Y.; Huang, X.; Zheng, F.; Ma, S.; Zhang, X.; Han, T.; Gao, H.; Shen, B. Role of Orai3-Mediated Store-Operated Calcium Entry in Radiation-Induced Brain Microvascular Endothelial Cell Injury. Int. J. Mol. Sci. 2023, 24, 6818. [Google Scholar] [CrossRef] [PubMed]
- Buijs, T.J.; Vilar, B.; Tan, C.H.; McNaughton, P.A. STIM1 and ORAI1 form a novel cold transduction mechanism in sensory and sympathetic neurons. EMBO J. 2023, 42, e111348. [Google Scholar] [CrossRef] [PubMed]
- Mitra, R.; Hasan, G. Store-operated Ca2+ entry regulates neuronal gene expression and function. Curr. Opin. Neurobiol. 2022, 73, 102520. [Google Scholar] [CrossRef] [PubMed]
- Letizia, M.; Wang, Y.H.; Kaufmann, U.; Gerbeth, L.; Sand, A.; Brunkhorst, M.; Weidner, P.; Ziegler, J.F.; Bottcher, C.; Schlickeiser, S.; et al. Store-operated calcium entry controls innate and adaptive immune cell function in inflammatory bowel disease. EMBO Mol. Med. 2022, 14, e15687. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.Y.; Wang, W.C.; Su, C.W.; Hsu, C.W.; Yuan, S.S.; Chen, Y.K. Expression of Orai1 and STIM1 in human oral squamous cell carcinogenesis. J. Dent. Sci. 2022, 17, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Umemura, M.; Nakakaji, R.; Ishikawa, Y. Physiological functions of calcium signaling via Orai1 in cancer. J. Physiol. Sci. 2023, 73, 21. [Google Scholar] [CrossRef] [PubMed]
- Daba, M.Y.; Fan, Z.J.; Li, Q.Y.; Yuan, X.L.; Liu, B. The role of calcium channels in prostate cancer progression and potential as a druggable target for prostate cancer treatment. Crit. Rev. Oncol. Hemat. 2023, 186, 104014. [Google Scholar] [CrossRef]
- Kouba, S.; Buscaglia, P.; Guéguinou, M.; Ibrahim, S.; Félix, R.; Guibon, R.; Fromont, G.; Pigat, N.; Capiod, T.; Vandier, C.; et al. Pivotal role of the ORAI3-STIM2 complex in the control of mitotic death and prostate cancer cell cycle progression. Cell Calcium 2023, 115, 102794. [Google Scholar] [CrossRef]
- Chalmers, S.B.; Monteith, G.R. ORAI channels and cancer. Cell Calcium 2018, 74, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Barretina, J.; Caponigro, G.; Stransky, N.; Venkatesan, K.; Margolin, A.A.; Kim, S.; Wilson, C.J.; Lehar, J.; Kryukov, G.V.; Sonkin, D.; et al. The Cancer Cell Line Encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature 2012, 483, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Perrouin Verbe, M.A.; Bruyere, F.; Rozet, F.; Vandier, C.; Fromont, G. Expression of store-operated channel components in prostate cancer: The prognostic paradox. Hum. Pathol. 2016, 49, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Collado, J.; Jardin, I.; Lopez, J.J.; Ronco, V.; Salido, G.M.; Dubois, C.; Prevarskaya, N.; Rosado, J.A. Role of Orai3 in the Pathophysiology of Cancer. Int. J. Mol. Sci. 2021, 22, 11426. [Google Scholar] [CrossRef]
- Zhang, X.; Gonzalez-Cobos, J.C.; Schindl, R.; Muik, M.; Ruhle, B.; Motiani, R.K.; Bisaillon, J.M.; Zhang, W.; Fahrner, M.; Barroso, M.; et al. Mechanisms of STIM1 activation of store-independent leukotriene C4-regulated Ca2+ channels. Mol. Cell. Biol. 2013, 33, 3715–3723. [Google Scholar] [CrossRef] [PubMed]
- Tanwar, J.; Arora, S.; Motiani, R.K. Orai3: Oncochannel with therapeutic potential. Cell Calcium 2020, 90, 102247. [Google Scholar] [CrossRef] [PubMed]
- Perrouin-Verbe, M.A.; Schoentgen, N.; Talagas, M.; Garlantezec, R.; Uguen, A.; Doucet, L.; Rosec, S.; Marcorelles, P.; Potier-Cartereau, M.; Vandier, C.; et al. Overexpression of certain transient receptor potential and Orai channels in prostate cancer is associated with decreased risk of systemic recurrence after radical prostatectomy. Prostate 2019, 79, 1793–1804. [Google Scholar] [CrossRef] [PubMed]
- Holzmann, C.; Kilch, T.; Kappel, S.; Armbruster, A.; Jung, V.; Stockle, M.; Bogeski, I.; Schwarz, E.C.; Peinelt, C. ICRAC controls the rapid androgen response in human primary prostate epithelial cells and is altered in prostate cancer. Oncotarget 2013, 4, 2096–2107. [Google Scholar] [CrossRef]
- Flourakis, M.; Lehen’kyi, V.; Beck, B.; Raphael, M.; Vandenberghe, M.; Abeele, F.V.; Roudbaraki, M.; Lepage, G.; Mauroy, B.; Romanin, C.; et al. Orai1 contributes to the establishment of an apoptosis-resistant phenotype in prostate cancer cells. Cell Death Dis. 2010, 1, e75. [Google Scholar] [CrossRef]
- Denmeade, S.R.; Lin, X.S.; Isaacs, J.T. Role of programmed (apoptotic) cell death during the progression and therapy for prostate cancer. Prostate 1996, 28, 251–265. [Google Scholar] [CrossRef]
- Motiani, R.K.; Abdullaev, I.F.; Trebak, M. A novel native store-operated calcium channel encoded by Orai3: Selective requirement of Orai3 versus Orai1 in estrogen receptor-positive versus estrogen receptor-negative breast cancer cells. J. Biol. Chem. 2010, 285, 19173–19183. [Google Scholar] [CrossRef] [PubMed]
- Vashisht, A.; Tanwar, J.; Motiani, R.K. Regulation of proto-oncogene Orai3 by miR18a/b and miR34a. Cell Calcium 2018, 75, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Hasna, J.; Hague, F.; Rodat-Despoix, L.; Geerts, D.; Leroy, C.; Tulasne, D.; Ouadid-Ahidouch, H.; Kischel, P. Orai3 calcium channel and resistance to chemotherapy in breast cancer cells: The p53 connection. Cell Death Differ. 2018, 25, 693–707. [Google Scholar] [CrossRef] [PubMed]
- Jardin, I.; Alvarado, S.; Jimenez-Velarde, V.; Nieto-Felipe, J.; Lopez, J.J.; Salido, G.M.; Smani, T.; Rosado, J.A. Orai1alpha and Orai1beta support calcium entry and mammosphere formation in breast cancer stem cells. Sci. Rep. 2023, 13, 19471. [Google Scholar] [CrossRef]
- Xia, J.; Wang, H.; Huang, H.; Sun, L.; Dong, S.; Huang, N.; Shi, M.; Bin, J.; Liao, Y.; Liao, W. Elevated Orai1 and STIM1 expressions upregulate MACC1 expression to promote tumor cell proliferation, metabolism, migration, and invasion in human gastric cancer. Cancer Lett. 2016, 381, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Mignen, O.; Vannier, J.P.; Schneider, P.; Renaudineau, Y.; Abdoul-Azize, S. Orai1 Ca2+ channel modulators as therapeutic tools for treating cancer: Emerging evidence! Biochem. Pharmacol. 2024, 219, 115955. [Google Scholar] [CrossRef] [PubMed]
- Son, G.Y.; Tu, N.H.; Santi, M.D.; Lopez, S.L.; Bomfim, G.H.S.; Vinu, M.; Zhou, F.; Chaloemtoem, A.; Alhariri, R.; Idaghdour, Y.; et al. The Ca2+ channel ORAI1 is a regulator of oral cancer growth and nociceptive pain. Sci. Signal. 2023, 16, eadf9535. [Google Scholar] [CrossRef]
- McCarl, C.A.; Khalil, S.; Ma, J.A.; Oh-Hora, M.; Yamashita, M.; Roether, J.; Kawasaki, T.; Jairaman, A.; Sasaki, Y.; Prakriya, M.; et al. Store-Operated Ca2+ Entry through ORAI1 Is Critical for T Cell-Mediated Autoimmunity and Allograft Rejection. J. Immunol. 2010, 185, 5845–5858. [Google Scholar] [CrossRef] [PubMed]
- Berry, C.T.; May, M.J.; Freedman, B.D. STIM- and Orai-mediated calcium entry controls NF-kappaB activity and function in lymphocytes. Cell Calcium 2018, 74, 131–143. [Google Scholar] [CrossRef]
- Kim, J.H.; Lkhagvadorj, S.; Lee, M.R.; Hwang, K.H.; Chung, H.C.; Jung, J.H.; Cha, S.K.; Eom, M. Orai1 and STIM1 are critical for cell migration and proliferation of clear cell renal cell carcinoma. Biochem. Biophys. Res. Commun. 2014, 448, 76–82. [Google Scholar] [CrossRef]
- Pan, Y.; Huang, J.; Liu, K.; Xie, C.; Chen, H.; Guo, Z.; Guo, S.; Chen, Y. Orai1-mediated store-operated Ca2+ entry promotes cervical cancer progression through IL-6 signaling. Front. Mol. Biosci. 2022, 9, 1041674. [Google Scholar] [CrossRef] [PubMed]
- Azimi, I.; Bong, A.H.; Poo, G.X.H.; Armitage, K.; Lok, D.; Roberts-Thomson, S.J.; Monteith, G.R. Pharmacological inhibition of store-operated calcium entry in MDA-MB-468 basal A breast cancer cells: Consequences on calcium signalling, cell migration and proliferation. Cell. Mol. Life Sci. 2018, 75, 4525–4537. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Hughes, J.D.; Rollins, S.; Chen, B.; Perkins, E. Calcium entry via ORAI1 regulates glioblastoma cell proliferation and apoptosis. Exp. Mol. Pathol. 2011, 91, 753–760. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Zhang, J.J.; Huang, X.Y. Orai1 and STIM1 are critical for breast tumor cell migration and metastasis. Cancer Cell 2009, 15, 124–134. [Google Scholar] [CrossRef]
- Moccia, F.; Zuccolo, E.; Poletto, V.; Turin, I.; Guerra, G.; Pedrazzoli, P.; Rosti, V.; Porta, C.; Montagna, D. Targeting Stim and Orai Proteins as an Alternative Approach in Anticancer Therapy. Curr. Med. Chem. 2016, 23, 3450–3480. [Google Scholar] [CrossRef]
- Zhu, M.; Lv, B.; Ge, W.; Cui, Z.; Zhao, K.; Feng, Y.; Yang, X. Suppression of store-operated Ca2+ entry regulated by silencing Orai1 inhibits C6 glioma cell motility via decreasing Pyk2 activity and promoting focal adhesion. Cell Cycle 2020, 19, 3468–3479. [Google Scholar] [CrossRef]
- Yang, J.; Antin, P.; Berx, G.; Blanpain, C.; Brabletz, T.; Bronner, M.; Campbell, K.; Cano, A.; Casanova, J.; Christofori, G.; et al. Guidelines and definitions for research on epithelial-mesenchymal transition. Nat. Rev. Mol. Cell. Biol. 2020, 21, 341–352. [Google Scholar] [CrossRef]
- Miettinen, P.J.; Ebner, R.; Lopez, A.R.; Derynck, R. TGF-beta induced transdifferentiation of mammary epithelial cells to mesenchymal cells: Involvement of type I receptors. J. Cell Biol. 1994, 127, 2021–2036. [Google Scholar] [CrossRef]
- Hu, J.; Qin, K.; Zhang, Y.; Gong, J.; Li, N.; Lv, D.; Xiang, R.; Tan, X. Downregulation of transcription factor Oct4 induces an epithelial-to-mesenchymal transition via enhancement of Ca2+ influx in breast cancer cells. Biochem. Biophys. Res. Commun. 2011, 411, 786–791. [Google Scholar] [CrossRef]
- Liu, X.Y.; Wang, T.; Wang, Y.; Chen, Z.; Hua, D.; Yao, X.Q.; Ma, X.; Zhang, P. Orail is critical for Notch-driven aggressiveness under hypoxic conditions in triple-negative breast cancers. BBA Mol. Basis Dis. 2018, 1864, 975–986. [Google Scholar] [CrossRef]
- Liu, X.Y.; Wan, X.; Kan, H.; Wang, Y.; Yu, F.; Feng, L.; Jin, J.; Zhang, P.; Ma, X. Hypoxia-induced upregulation of Orai1 drives colon cancer invasiveness and angiogenesis. Eur. J. Pharmacol. 2018, 832, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; Chen, L.; Zhao, P.; Zhou, H.; Zhang, C.; Yu, S.; Lin, Y.; Yang, X. Store-operated Ca2+ entry regulates glioma cell migration and invasion via modulation of Pyk2 phosphorylation. J. Exp. Clin. Cancer Res. 2014, 33, 98. [Google Scholar] [CrossRef] [PubMed]
- Kang, Q.J.; Peng, X.D.; Li, X.S.; Hu, D.H.; Wen, G.X.; Wei, Z.Q.; Yuan, B.H. Calcium Channel Protein ORAI1 Mediates TGF-β Induced Epithelial-to-Mesenchymal Transition in Colorectal Cancer Cells. Front. Oncol. 2021, 11, 649476. [Google Scholar] [CrossRef] [PubMed]
- Ye, J.; Huang, J.; He, Q.; Zhao, W.; Zhou, X.; Zhang, Z.; Li, Y.; Wei, J.; Zhang, J. Blockage of store-operated Ca2+ entry antagonizes Epstein-Barr virus-promoted angiogenesis by inhibiting Ca2+ signaling-regulated VEGF production in nasopharyngeal carcinoma. Cancer Manag. Res. 2018, 10, 1115–1124. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.M.; Minter, L.M.; Cho, O.H.; Gottipati, S.; Fauq, A.H.; Golde, T.E.; Sonenshein, G.E.; Osborne, B.A. Notch1 augments NF-kappaB activity by facilitating its nuclear retention. EMBO J. 2006, 25, 129–138. [Google Scholar] [CrossRef]
- Eylenstein, A.; Schmidt, S.; Gu, S.; Yang, W.; Schmid, E.; Schmidt, E.M.; Alesutan, I.; Szteyn, K.; Regel, I.; Shumilina, E.; et al. Transcription factor NF-kappaB regulates expression of pore-forming Ca2+ channel unit, Orai1, and its activator, STIM1, to control Ca2+ entry and affect cellular functions. J. Biol. Chem. 2012, 287, 2719–2730. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.H.; Xu, P.; Lv, J.L.; Ge, H.; Yan, Z.Y.; Huang, S.S.; Li, B.W.; Xu, H.; Yang, L.; Xu, Z.K.; et al. Peritoneal high-fat environment promotes peritoneal metastasis of gastric cancer cells through activation of NSUN2-mediated ORAI2 m5C modification. Oncogene 2023, 42, 1980–1993. [Google Scholar] [CrossRef] [PubMed]
- Brahmer, J.R.; Tykodi, S.S.; Chow, L.Q.M.; Hwu, W.J.; Topalian, S.L.; Hwu, P.; Drake, C.G.; Camacho, L.H.; Kauh, J.; Odunsi, K.; et al. Safety and Activity of Anti-PD-L1 Antibody in Patients with Advanced Cancer. N. Engl. J. Med. 2012, 366, 2455–2465. [Google Scholar] [CrossRef] [PubMed]
- Apolo, A.B.; Infante, J.R.; Hamid, O.; Patel, M.R.; Wang, D.; Kelly, K.; Mega, A.E.; Britten, C.D.; Mita, A.C.; Ravaud, A.; et al. Safety, clinical activity, and PD-L1 expression of avelumab (MSB0010718C), an anti-PD-L1 antibody, in patients with metastatic urothelial carcinoma from the JAVELIN Solid Tumor phase Ib trial. J. Clin. Oncol. 2016, 34, 367. [Google Scholar] [CrossRef]
- Desai, J.; Voskoboynik, M.; Markman, B.; Hou, J.; Zeng, D.; Meniawy, T. Phase I/II study investigating safety, tolerability, pharmacokinetics, and preliminary antitumor activity of anti-PD-L1 monoclonal antibody BGB-A333 alone and in combination with anti-PD-1 monoclonal antibody tislelizumab in patients with advanced solid tumors. Ann. Oncol. 2018, 29, 146. [Google Scholar]
- Barros, F.M.; Carneiro, F.; Machado, J.C.; Melo, S.A. Exosomes and Immune Response in Cancer: Friends or Foes? Front. Immunol. 2018, 9, 730. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Li, J.Q.; Zhang, R.; Zhang, Y.; Wang, X.X.; Leung, E.L.H.; Ma, L.J.; Wong, V.K.W.; Liu, L.; Neher, E.; et al. Suppression of PD-L1 release from small extracellular vesicles promotes systemic anti-tumor immunity by targeting ORAI1 calcium channels. J. Extracell. Vesicles. 2022, 11, e12279. [Google Scholar] [CrossRef] [PubMed]
- Rubaiy, H.N. ORAI Calcium Channels: Regulation, Function, Pharmacology, and Therapeutic Targets. Pharmaceuticals 2023, 16, 162. [Google Scholar] [CrossRef] [PubMed]
| Regions | Mutations | Effects on ORAI | Related Diseases | Ref. |
|---|---|---|---|---|
| TM1 | A88SfsX25 | Loss-of-function | Neutropenia and thrombocytopenia, congenital muscular hypotonia, and encephalopathy | [29,30] |
| R91W | Loss-of-function | SCID and hypocalcified amelogenesis imperfecta | [13,31] | |
| S97C | Gain-of-function | TAM and congenital miosis | [32] | |
| G98S | Gain-of-function | TAM | [33] | |
| G98R | Loss-of-function | CID, autoimmunity, ectodermal dysplasia with anhidrosis, and muscular dysplasia | [34] | |
| A103E/L194P | Loss-of-function | Congenital muscular hypotonia, eczema, and neovascularization of cornea | [29,35] | |
| Loop1 | V107M | Gain-of-function | TAM | [33,36] |
| TM2 | C126R | Loss-of-function | CID | [37] |
| L135R | Loss-of-function | CID | [37] | |
| A137V | Gain-of-function | Colorectal adenocarcinoma | [38] | |
| L138F | Gain-of-function | TAM | [27,39] | |
| M139V | Gain-of-function | Stomach carcinoma | [40] | |
| Loop2 | S159L | Gain-of-function | Uterine carcinoma | [41] |
| H165PfsX1 | Loss-of-function | CID | [42] | |
| TM3 | T184M | Gain-of-function | TAM | [36] |
| V181SfsX8 | Loss-of-function | CID, autoimmunity, ectodermal dysplasia with anhidrosis, and muscular dysplasia | [34] | |
| L194P | Loss-of-function | CID, autoimmunity, ectodermal dysplasia with anhidrosis, and muscular dysplasia | [34] | |
| Loop3 | N233A | Loss-of-function | SCID | [43] |
| TM4 | P245L | Gain-of-function | TAM | [36,44] |
| G247S | Gain-of-function | Neck carcinoma | [45] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Q.; Wang, C.; He, L. ORAI Ca2+ Channels in Cancers and Therapeutic Interventions. Biomolecules 2024, 14, 417. https://doi.org/10.3390/biom14040417
Zhang Q, Wang C, He L. ORAI Ca2+ Channels in Cancers and Therapeutic Interventions. Biomolecules. 2024; 14(4):417. https://doi.org/10.3390/biom14040417
Chicago/Turabian StyleZhang, Qian, Chen Wang, and Lian He. 2024. "ORAI Ca2+ Channels in Cancers and Therapeutic Interventions" Biomolecules 14, no. 4: 417. https://doi.org/10.3390/biom14040417





