COVID-Vaccines in Pregnancy: Maternal and Neonatal Response over the First 9 Months after Delivery
Abstract
:1. Introduction
2. Materials and Methods
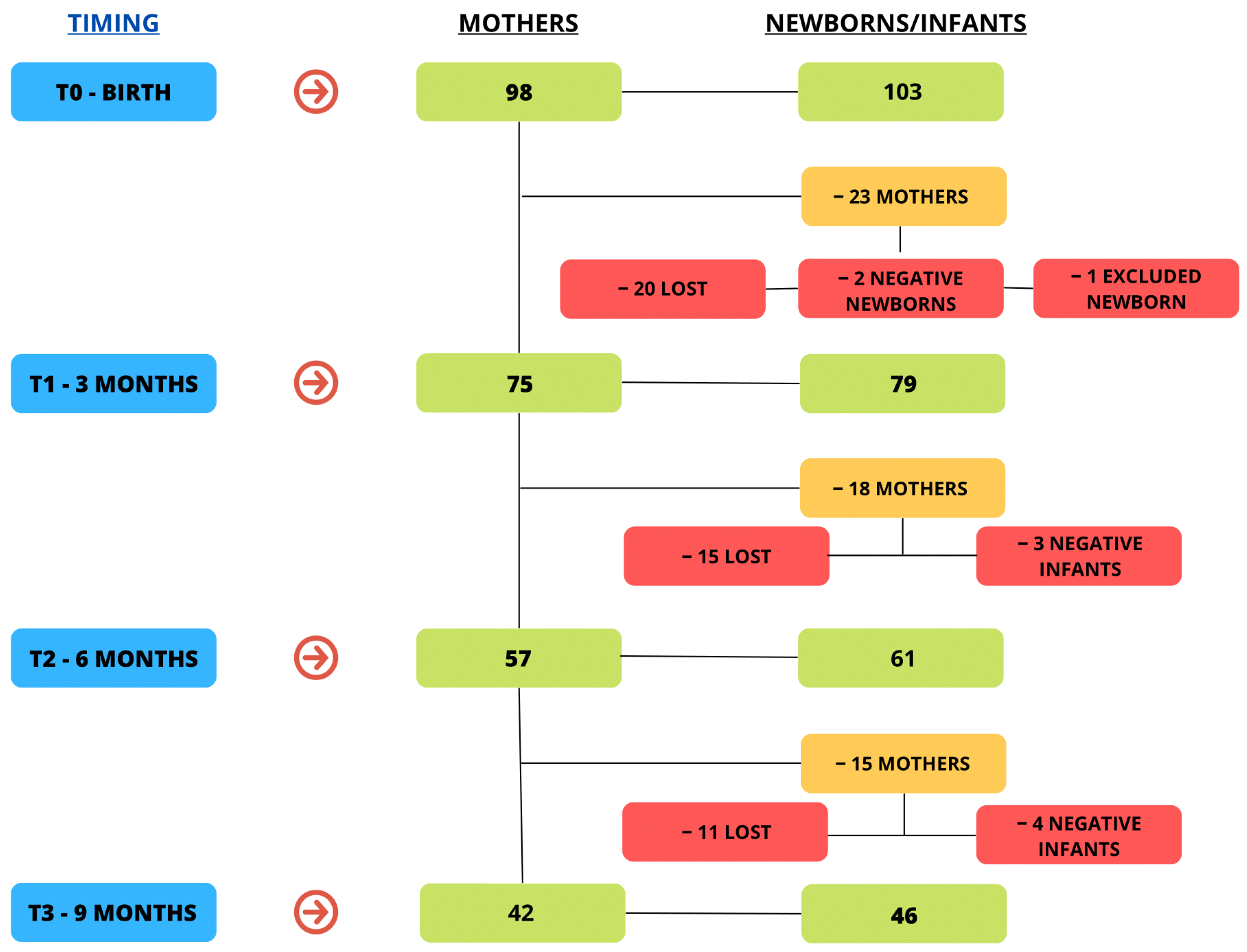
2.1. Participants Recruitment
2.2. Study Design and Sample Collection
2.3. Statistical Analyses
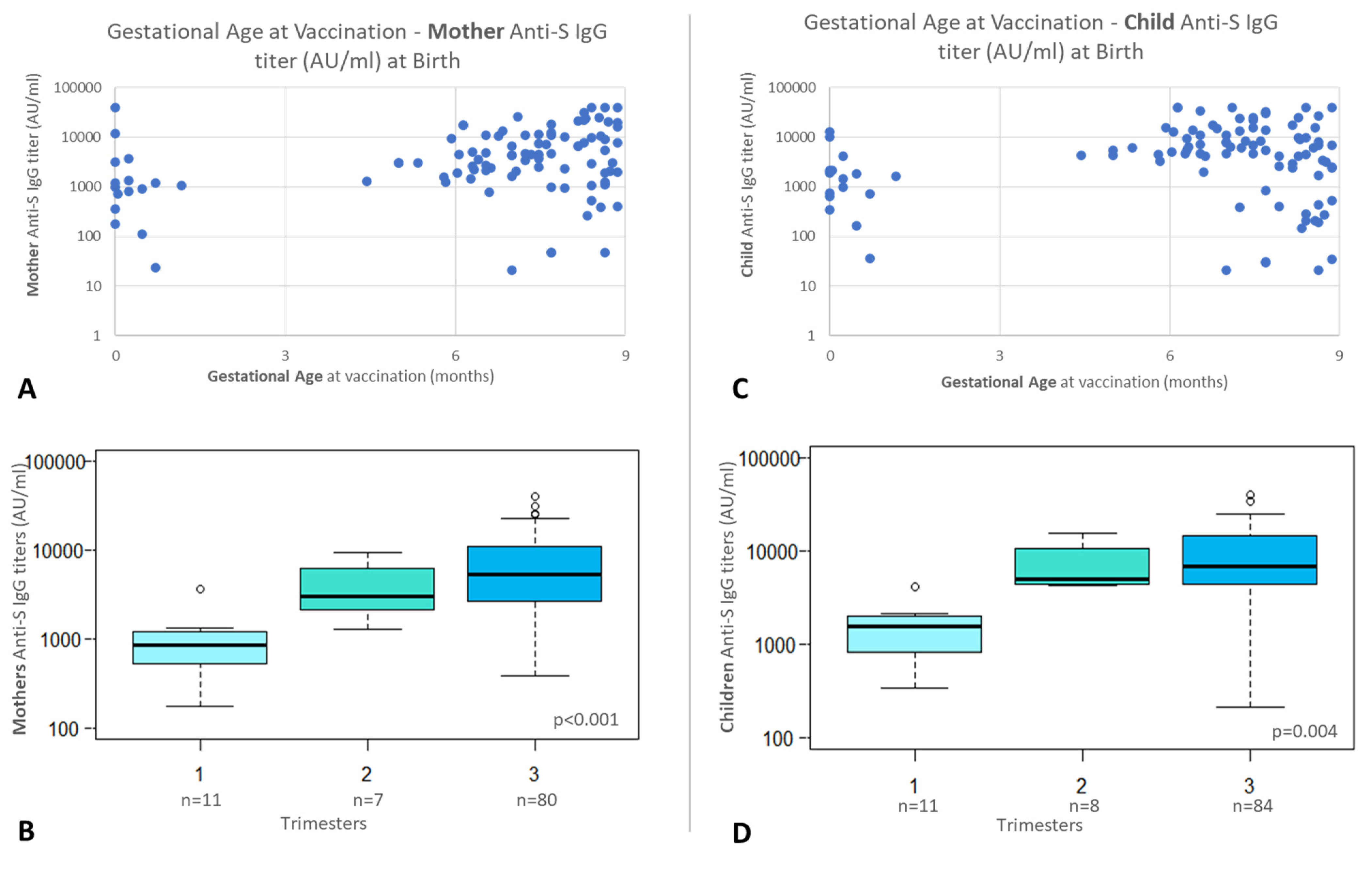
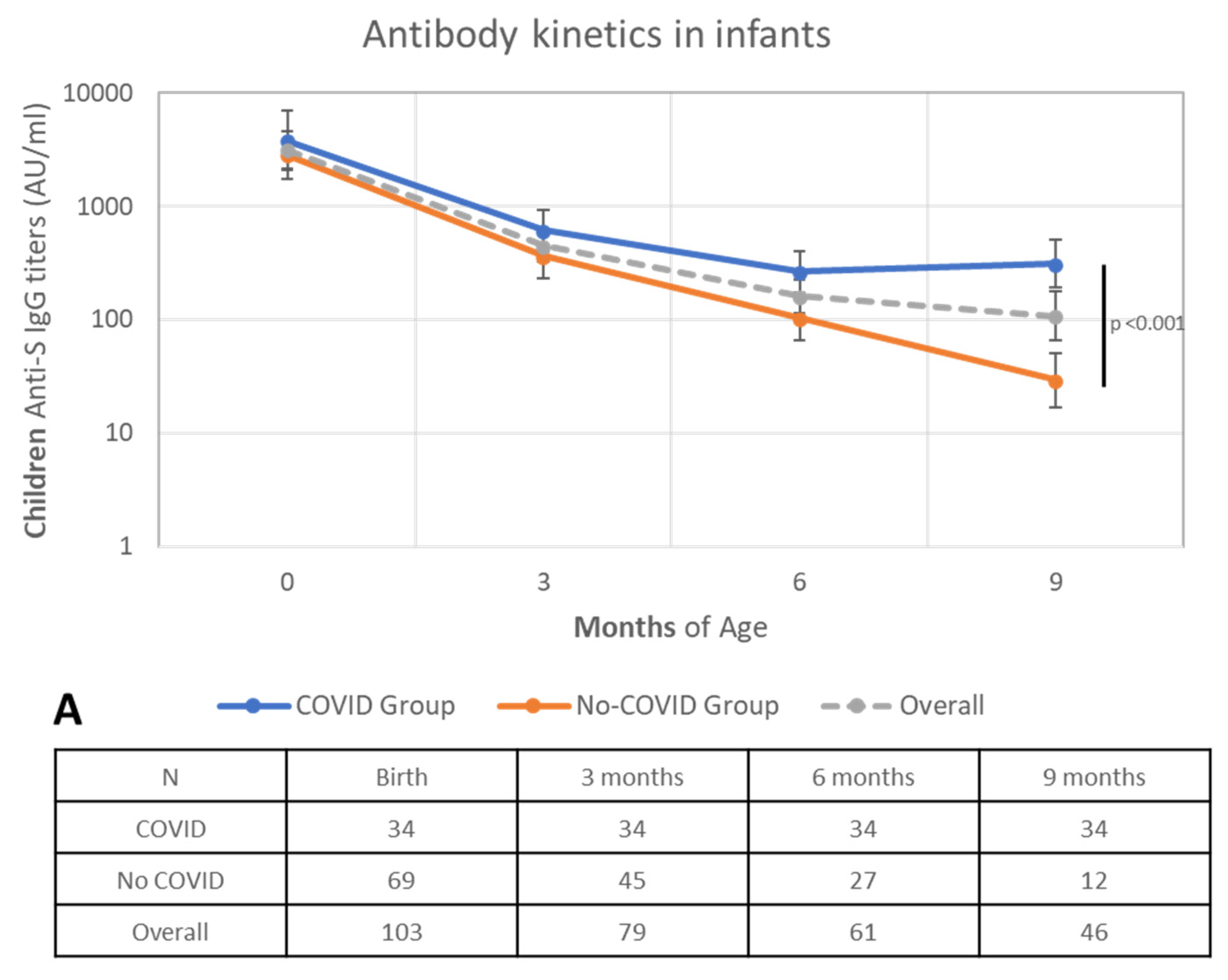
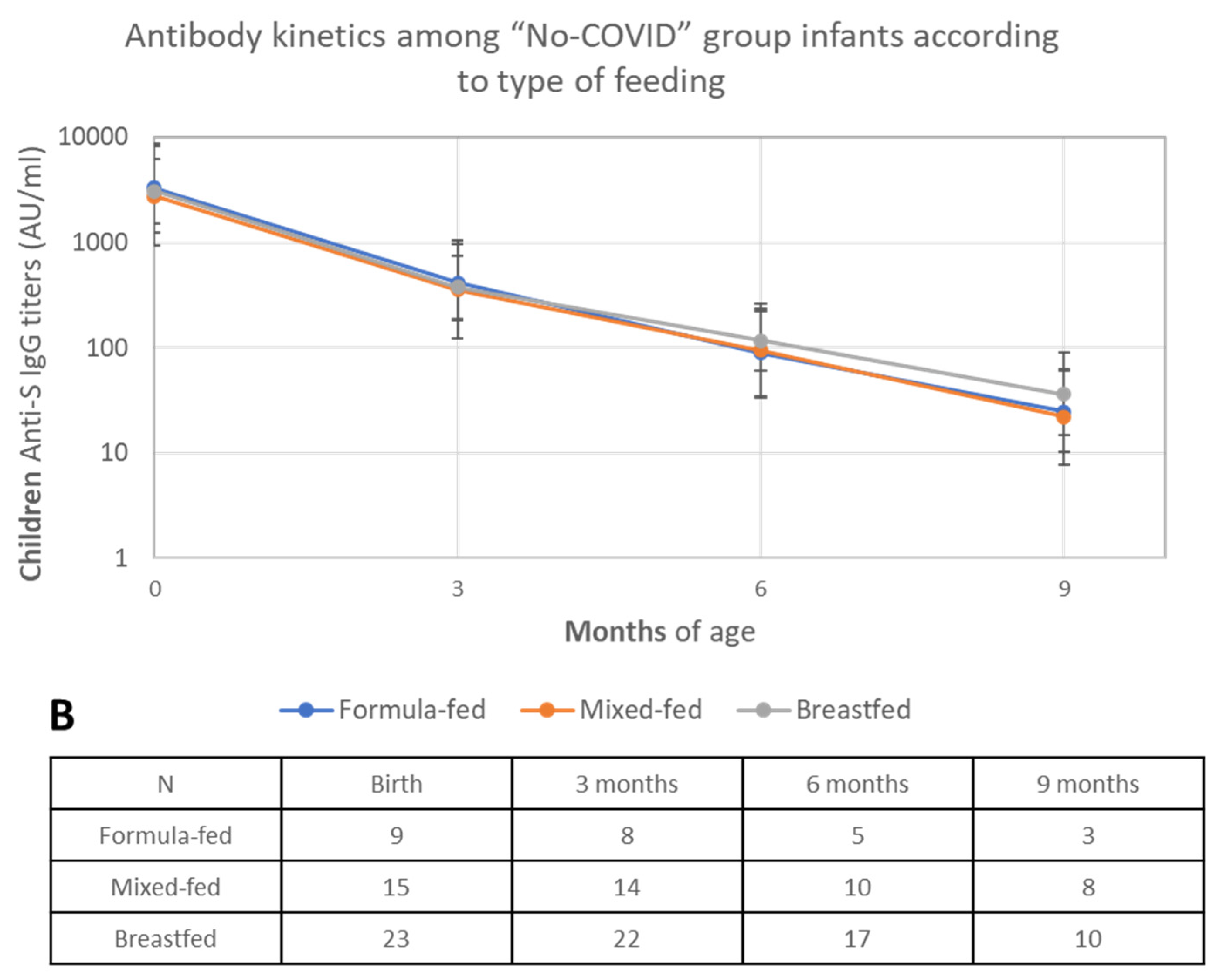
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- 2019-nCoV Outbreak Is an Emergency of International Concern—World|ReliefWeb. Available online: https://reliefweb.int/report/world/2019-ncov-outbreak-emergency-international-concern (accessed on 8 February 2024).
- Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV). Available online: https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (accessed on 8 February 2024).
- Mangat, C.; Milosavljevic, N. BNT162b2 Vaccination during Pregnancy Protects Both the Mother and Infant: Anti-SARS-CoV-2 S Antibodies Persistently Positive in an Infant at 6 Months of Age. Case Rep. Pediatr. 2021, 2021, 6901131. [Google Scholar] [CrossRef] [PubMed]
- Rathberger, K.; Häusler, S.; Wellmann, S.; Weigl, M.; Langhammer, F.; Bazzano, M.V.; Ambrosch, A.; Fill Malfertheiner, S. SARS-CoV-2 in pregnancy and possible transfer of immunity: Assessment of peripartal maternal and neonatal antibody levels and a longitudinal follow-up. J. Perinat. Med. 2021, 49, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Popescu, D.-E.; Cîtu, C.; Jura, A.M.C.; Lungu, N.; Navolan, D.; Craina, M.; Semenescu, A.; Gorun, F.; Jura, M.-A.; Belengeanu, V.; et al. The Benefits of Vaccination against SARS-CoV-2 during Pregnancy in Favor of the Mother/Newborn Dyad. Vaccines 2022, 10, 848. [Google Scholar] [CrossRef] [PubMed]
- Pietrasanta, C.; Artieri, G.; Ronchi, A.; Crippa, B.; Ballerini, C.; Crimi, R.; Mosca, F.; Pugni, L. SARS-CoV-2 infection and neonates: Evidence-based data after 18 months of the pandemic. Pediatr. Allergy Immunol. 2022, 33 (Suppl. 27), 96–98. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.-J.; Fu, Y.-C.; Lin, Y.-P.; Shen, C.-F.; Sun, D.-J.; Chen, H.-Y.; Cheng, C.-M. Evaluation of Transplacental Antibody Transfer in SARS-CoV-2-Immunized Pregnant Women. Vaccines 2022, 10, 101. [Google Scholar] [CrossRef]
- Favre, G.; Maisonneuve, E.; Pomar, L.; Winterfeld, U.; Daire, C.; Martinez de Tejada, B.; Delecraz, D.; Campelo, S.; Moser, M.; Todesco-Bernasconi, M.; et al. COVID-19 mRNA vaccine in pregnancy: Results of the Swiss COVI-PREG registry, an observational prospective cohort study. Lancet Reg. Health Eur. 2022, 18, 100410. [Google Scholar] [CrossRef] [PubMed]
- Atyeo, C.G.; Shook, L.L.; Brigida, S.; De Guzman, R.M.; Demidkin, S.; Muir, C.; Akinwunmi, B.; Baez, A.M.; Sheehan, M.L.; McSweeney, E.; et al. Maternal immune response and placental antibody transfer after COVID-19 vaccination across trimester and platforms. Nat. Commun. 2022, 13, 3571. [Google Scholar] [CrossRef]
- Gray, K.J.; Bordt, E.A.; Atyeo, C.; Deriso, E.; Akinwunmi, B.; Young, N.; Baez, A.M.; Shook, L.L.; Cvrk, D.; James, K.; et al. Coronavirus disease 2019 vaccine response in pregnant and lactating women: A cohort study. Am. J. Obstet. Gynecol. 2021, 225, 303.e1–303.e17. [Google Scholar] [CrossRef]
- Atyeo, C.; DeRiso, E.A.; Davis, C.; Bordt, E.A.; De Guzman, R.M.; Shook, L.L.; Yonker, L.M.; Fasano, A.; Akinwunmi, B.; Lauffenburger, D.A.; et al. COVID-19 mRNA vaccines drive differential antibody Fc-functional profiles in pregnant, lactating, and nonpregnant women. Sci. Transl. Med. 2021, 13, eabi8631. [Google Scholar] [CrossRef] [PubMed]
- Collier, A.-R.Y.; McMahan, K.; Yu, J.; Tostanoski, L.H.; Aguayo, R.; Ansel, J.; Chandrashekar, A.; Patel, S.; Apraku Bondzie, E.; Sellers, D.; et al. Immunogenicity of COVID-19 mRNA Vaccines in Pregnant and Lactating Women. JAMA 2021, 325, 2370–2380. [Google Scholar] [CrossRef] [PubMed]
- Lipkind, H.S.; Vazquez-Benitez, G.; DeSilva, M.; Vesco, K.K.; Ackerman-Banks, C.; Zhu, J.; Boyce, T.G.; Daley, M.F.; Fuller, C.C.; Getahun, D.; et al. Receipt of COVID-19 Vaccine During Pregnancy and Preterm or Small-for-Gestational-Age at Birth—Eight Integrated Health Care Organizations, United States, December 15, 2020–July 22, 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 26–30. [Google Scholar] [CrossRef] [PubMed]
- SARS-CoV-2 Immunoassay|Core Laboratory at Abbott. Available online: https://www.corelaboratory.abbott/int/en/offerings/segments/infectious-disease/sars-cov-2.html (accessed on 8 February 2024).
- Jorgensen, S.C.J.; Burry, L.; Tabbara, N. Role of maternal COVID-19 vaccination in providing immunological protection to the newborn. Pharmacotherapy 2022, 42, 58–70. [Google Scholar] [CrossRef] [PubMed]
- Rottenstreich, A.; Zarbiv, G.; Oiknine-Djian, E.; Zigron, R.; Wolf, D.G.; Porat, S. Efficient Maternofetal Transplacental Transfer of Anti-Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Spike Antibodies after Antenatal SARS-CoV-2 BNT162b2 Messenger RNA Vaccination. Clin. Infect. Dis. 2021, 73, 1909–1912. [Google Scholar] [CrossRef] [PubMed]
- Paul, G.; Chad, R. Newborn antibodies to SARS-CoV-2 detected in cord blood after maternal vaccination—A case report. BMC Pediatr. 2021, 21, 138. [Google Scholar] [CrossRef] [PubMed]
- Nir, O.; Schwartz, A.; Toussia-Cohen, S.; Leibovitch, L.; Strauss, T.; Asraf, K.; Doolman, R.; Sharabi, S.; Cohen, C.; Lustig, Y.; et al. Maternal-neonatal transfer of SARS-CoV-2 immunoglobulin G antibodies among parturient women treated with BNT162b2 messenger RNA vaccine during pregnancy. Am. J. Obstet. Gynecol. MFM 2022, 4, 100492. [Google Scholar] [CrossRef] [PubMed]
- Beharier, O.; Plitman Mayo, R.; Raz, T.; Nahum Sacks, K.; Schreiber, L.; Suissa-Cohen, Y.; Chen, R.; Gomez-Tolub, R.; Hadar, E.; Gabbay-Benziv, R.; et al. Efficient maternal to neonatal transfer of antibodies against SARS-CoV-2 and BNT162b2 mRNA COVID-19 vaccine. J. Clin. Investig. 2021, 131, e154834. [Google Scholar] [CrossRef]
- Kugelman, N.; Nahshon, C.; Shaked-Mishan, P.; Kleifeld, S.; Cohen, N.; Sher, M.L.; Zahran, H.; Barsha, H.; Assaf, W.; Shalabna, E.; et al. Maternal and Neonatal Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Immunoglobulin G Levels After the Pfizer-BioNTech Booster Dose for Coronavirus Disease 2019 (COVID-19) Vaccination During the Second Trimester of Pregnancy. Obstet. Gynecol. 2022, 140, 187–193. [Google Scholar] [CrossRef]
- Rottenstreich, A.; Zarbiv, G.; Oiknine-Djian, E.; Vorontsov, O.; Zigron, R.; Kleinstern, G.; Porat, S.; Wolf, D.G. Kinetics of Maternally Derived Anti-Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Antibodies in Infants in Relation to the Timing of Antenatal Vaccination. Clin. Infect. Dis. 2023, 76, e274–e279. [Google Scholar] [CrossRef]
- Kugelman, N.; Nahshon, C.; Shaked-Mishan, P.; Cohen, N.; Lahav Sher, M.; Barsha, H.; Shalabna, E.; Zolotarevsky, A.; Lavie, O.; Kedar, R.; et al. Third trimester messenger RNA COVID-19 booster vaccination upsurge maternal and neonatal SARS-CoV-2 immunoglobulin G antibody levels at birth. Eur. J. Obstet. Gynecol. Reprod. Biol. 2022, 274, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Nevo, L.; Cahen-Peretz, A.; Vorontsov, O.; Frenkel, R.; Kabessa, M.; Cohen, S.M.; Hamrani, A.; Oiknine-Djian, E.; Lipschuetz, M.; Goldman-Wohl, D.; et al. Boosting maternal and neonatal humoral immunity following SARS-CoV-2 infection using a single messenger RNA vaccine dose. Am. J. Obstet. Gynecol. 2022, 227, 486.e1–486.e10. [Google Scholar] [CrossRef] [PubMed]
- Shook, L.L.; Atyeo, C.G.; Yonker, L.M.; Fasano, A.; Gray, K.J.; Alter, G.; Edlow, A.G. Durability of Anti-Spike Antibodies in Infants After Maternal COVID-19 Vaccination or Natural Infection. JAMA 2022, 327, 1087–1089. [Google Scholar] [CrossRef] [PubMed]
- Kashani-Ligumsky, L.; Lopian, M.; Cohen, R.; Senderovich, H.; Czeiger, S.; Halperin, A.; Chaim, A.B.; Kremer, I.; Lessing, J.B.; Somekh, E.; et al. Titers of SARS CoV-2 antibodies in cord blood of neonates whose mothers contracted SARS CoV-2 (COVID-19) during pregnancy and in those whose mothers were vaccinated with mRNA to SARS CoV-2 during pregnancy. J. Perinatol. 2021, 41, 2621–2624. [Google Scholar] [CrossRef] [PubMed]
- Kugelman, N.; Nahshon, C.; Shaked-Mishan, P.; Lavie, O.; Stein, N.; Kedar, R.; Waisman, D. SARS-CoV-2 immunoglobulin G antibody levels in infants following messenger RNA COVID-19 vaccination during pregnancy. Am. J. Obstet. Gynecol. 2022, 227, 911–913. [Google Scholar] [CrossRef] [PubMed]
- Halasa, N.B.; Olson, S.M.; Staat, M.A.; Newhams, M.M.; Price, A.M.; Boom, J.A.; Sahni, L.C.; Cameron, M.A.; Pannaraj, P.S.; Bline, K.E.; et al. Effectiveness of Maternal Vaccination with mRNA COVID-19 Vaccine During Pregnancy Against COVID-19-Associated Hospitalization in Infants Aged <6 Months—17 States, July 2021–January 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Lopez, P.A.; Nziza, N.; Chen, T.; Shook, L.L.; Burns, M.D.; Demidkin, S.; Jasset, O.; Akinwunmi, B.; Yonker, L.M.; Gray, K.J.; et al. Placental transfer dynamics and durability of maternal COVID-19 vaccine-induced antibodies in infants. iScience 2024, 27, 109273. [Google Scholar] [CrossRef] [PubMed]
- Elahi, S.; Thompson, D.R.; Van Kessel, J.; Babiuk, L.A.; Gerdts, V. Protective Role of Passively Transferred Maternal Cytokines against Bordetella pertussis Infection in Newborn Piglets. Infect. Immun. 2017, 85, e01063-16. [Google Scholar] [CrossRef] [PubMed]
- Cinicola, B.; Conti, M.G.; Terrin, G.; Sgrulletti, M.; Elfeky, R.; Carsetti, R.; Fernandez Salinas, A.; Piano Mortari, E.; Brindisi, G.; De Curtis, M.; et al. The Protective Role of Maternal Immunization in Early Life. Front. Pediatr. 2021, 9, 638871. [Google Scholar] [CrossRef]
- Albrecht, M.; Arck, P.C. Vertically Transferred Immunity in Neonates: Mothers, Mechanisms and Mediators. Front. Immunol. 2020, 11, 555. [Google Scholar] [CrossRef]
- Calvert, A.; Jones, C.E. Placental transfer of antibody and its relationship to vaccination in pregnancy. Curr. Opin. Infect. Dis. 2017, 30, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Shahbaz, S.; Bozorgmehr, N.; Lu, J.; Osman, M.; Sligl, W.; Tyrrell, D.L.; Elahi, S. Analysis of SARS-CoV-2 isolates, namely the Wuhan strain, Delta variant, and Omicron variant, identifies differential immune profiles. Microbiol. Spectr. 2023, 11, e0125623. [Google Scholar] [CrossRef] [PubMed]
- Trougakos, I.P.; Terpos, E.; Alexopoulos, H.; Politou, M.; Paraskevis, D.; Scorilas, A.; Kastritis, E.; Andreakos, E.; Dimopoulos, M.A. Adverse effects of COVID-19 mRNA vaccines: The spike hypothesis. Trends Mol. Med. 2022, 28, 542–554. [Google Scholar] [CrossRef] [PubMed]
- Giannotta, G.; Murrone, A.; Giannotta, N. COVID-19 mRNA Vaccines: The Molecular Basis of Some Adverse Events. Vaccines 2023, 11, 747. [Google Scholar] [CrossRef]
- Atyeo, C.; Shook, L.L.; Nziza, N.; Deriso, E.A.; Muir, C.; Baez, A.M.; Lima, R.S.; Demidkin, S.; Brigida, S.; De Guzman, R.M.; et al. COVID-19 booster dose induces robust antibody response in pregnant, lactating, and nonpregnant women. Am. J. Obstet. Gynecol. 2023, 228, 68.e1–68.e12. [Google Scholar] [CrossRef] [PubMed]
- Nicolaidou, V.; Georgiou, R.; Christofidou, M.; Felekkis, K.; Pieri, M.; Papaneophytou, C. Detection of SARS-CoV-2-Specific Antibodies in Human Breast Milk and Their Neutralizing Capacity after COVID-19 Vaccination: A Systematic Review. Int. J. Mol. Sci. 2023, 24, 2957. [Google Scholar] [CrossRef]
- Stuckelberger, S.; Favre, G.; Ceulemans, M.; Nordeng, H.; Gerbier, E.; Lambelet, V.; Stojanov, M.; Winterfeld, U.; Baud, D.; Panchaud, A.; et al. SARS-CoV-2 Vaccine Willingness among Pregnant and Breastfeeding Women during the First Pandemic Wave: A Cross-Sectional Study in Switzerland. Viruses 2021, 13, 1199. [Google Scholar] [CrossRef]

| Mothers | ||||
| T0 | n = 98 | |||
| Age | (mean, sd) | 35.23 | 5.41 | |
| (median, Q1–Q3) | 35.50 | 32–39 | ||
| Race | (n, %) | Caucasian | 93 | 94.90 |
| Asian | 1 | 1.02 | ||
| Hispanic | 2 | 2.04 | ||
| North African | 2 | 2.04 | ||
| Number of doses | (n, %) | 1 | 24 | 24.49 |
| 2 | 74 | 75.51 | ||
| GA 1st dose (days) 1 | (mean, sd) | 175.91 | 80.04 | |
| (median, Q1–Q3) | 196 | 153–238 | ||
| GA 2nd dose (days) 2 | (mean, sd) | 203.93 | 66.80 | |
| (median, Q1–Q3) | 218 | 189–248 | ||
| GA at childbirth | (mean, sd) | 272.91 | 11.93 | |
| (median, Q1–Q3) | 275 | 268–280 | ||
| 2nd dose post-partum | (n, %) | 23 | 23.47 | |
| Type of delivery | (n, %) | ED | 73 | 74.49 |
| CS | 21 | 21.43 | ||
| OVD | 4 | 4.08 | ||
| COVID | (n, %) | 34 | 34.69 | |
| 3rd dose | (n, %) | After childbirth | 56 | 57.14 |
| Comorbidity | (n, %) | 13 | 13.27 | |
| Maternal diseases | (n, %) | 13 | 13.27 | |
| Adverse Events to vaccination | (n, %) | No | 81 | 82.02 |
| Yes | 17 | 19.10 | ||
| Admitted to follow-up | (%) | n = 75 (73.5) | ||
| SARS-CoV-2 cases among followed-up | (n, %) | 34 | 25.5 | |
| n = 34 | ||||
| Period of Infection | ||||
| (n, %) | 0–3 months | 10 | 29.41 | |
| 3–6 moths | 15 | 44.12 | ||
| 6–9 months | 9 | 26.47 | ||
| (n, %) | Before 3rd dose | 12 | 35.29 | |
| After 3rd dose | 22 | 64.71 | ||
| Babies | ||||
| T0 | n = 103 | |||
| Sex | (n, %) | Male | 61 | 59.22 |
| Female | 42 | 40.78 | ||
| Weight (g) | (mean, sd) | Birth | 3056.21 | 512.48 |
| (median, Q1–Q3) | 3080 | 2780–3400 | ||
| 3 months 3 | 5785.41 | 841.75 | ||
| 5950 | 5000–6450 | |||
| 6 months 4 | 7485.56 | 906.59 | ||
| 7400 | 6800–8000 | |||
| 9 months 5 | 8530.00 | 940.51 | ||
| 8050 | 7900–9000 | |||
| Lenght at birth (cm) | (mean, sd) | 48.61 | 2.73 | |
| (median, Q1–Q3) | 49 | 48–50 | ||
| Head circumference at birth (cm) | (mean, sd) | 33.82 | 1.48 | |
| (median, Q1–Q3) | 34 | 33–35 | ||
| Weight at birth (cent) | (mean, sd) | 38.74 | 28.07 | |
| (median, Q1–Q3) | 33 | 14–60 | ||
| Lenght at birth (cent) | (mean, sd) | 36.95 | 27.18 | |
| (median, Q1–Q3) | 33 | 13–53 | ||
| Head circumference at birth (cent) | (mean, sd) | 43.06 | 27.92 | |
| (median, Q1–Q3) | 37 | 20–69 | ||
| APGAR 1′ | (n, %) | 10 | 30 | 29.13 |
| 9 | 58 | 56.31 | ||
| 8 | 11 | 10.68 | ||
| ≤7 | 4 | 3.88 | ||
| APGAR 5′ | (n, %) | 10 | 85 | 82.52 |
| 9 | 15 | 14.56 | ||
| 8 | 3 | 2.91 | ||
| Feeding (T0) | (n, %) | Formula-fed | 15 | 16.13 |
| Mixed-fed | 23 | 24.73 | ||
| Breastfed | 55 | 59.14 | ||
| Admitted to follow-up | (%) | n = 79 (81.5) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Proto, A.; Agliardi, S.; Pani, A.; Renica, S.; Gazzaniga, G.; Giossi, R.; Senatore, M.; Di Ruscio, F.; Campisi, D.; Vismara, C.; et al. COVID-Vaccines in Pregnancy: Maternal and Neonatal Response over the First 9 Months after Delivery. Biomolecules 2024, 14, 435. https://doi.org/10.3390/biom14040435
Proto A, Agliardi S, Pani A, Renica S, Gazzaniga G, Giossi R, Senatore M, Di Ruscio F, Campisi D, Vismara C, et al. COVID-Vaccines in Pregnancy: Maternal and Neonatal Response over the First 9 Months after Delivery. Biomolecules. 2024; 14(4):435. https://doi.org/10.3390/biom14040435
Chicago/Turabian StyleProto, Alice, Stefano Agliardi, Arianna Pani, Silvia Renica, Gianluca Gazzaniga, Riccardo Giossi, Michele Senatore, Federica Di Ruscio, Daniela Campisi, Chiara Vismara, and et al. 2024. "COVID-Vaccines in Pregnancy: Maternal and Neonatal Response over the First 9 Months after Delivery" Biomolecules 14, no. 4: 435. https://doi.org/10.3390/biom14040435







