The Role and Function of TRPM8 in the Digestive System
Abstract
1. The Structure, Functions, and Distribution of TRPM8
2. The Role of TRPM8 in the Esophagus
3. The Role of TRPM8 in the Stomach
4. The Role of TRPM8 in the Small Intestine and Colon
5. The Role of TRPM8 in the Liver
6. The Role of TRPM8 in the Pancreas
7. Conclusions and Outlook
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wu, F.; Bu, S.; Wang, H. Role of TRP Channels in Metabolism-Related Diseases. Int. J. Mol. Sci. 2024, 25, 692. [Google Scholar] [CrossRef] [PubMed]
- McKemy, D.D.; Neuhausser, W.M.; Julius, D. Identification of a cold receptor reveals a general role for TRP channels in thermosensation. Nature 2002, 416, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Ochoa, S.V.; Casas, Z.; Albarracin, S.L.; Sutachan, J.J.; Torres, Y.P. Therapeutic potential of TRPM8 channels in cancer treatment. Front. Pharmacol. 2023, 14, 1098448. [Google Scholar] [CrossRef] [PubMed]
- Janssens, A.; Voets, T. Ligand stoichiometry of the cold- and menthol-activated channel TRPM8. J. Physiol. 2011, 589, 4827–4835. [Google Scholar] [CrossRef] [PubMed]
- Chuang, H.H.; Neuhausser, W.M.; Julius, D. The super-cooling agent icilin reveals a mechanism of coincidence detection by a temperature-sensitive TRP channel. Neuron 2004, 43, 859–869. [Google Scholar] [CrossRef] [PubMed]
- Voets, T.; Owsianik, G.; Janssens, A.; Talavera, K.; Nilius, B. TRPM8 voltage sensor mutants reveal a mechanism for integrating thermal and chemical stimuli. Nat. Chem. Biol. 2007, 3, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Voets, T.; Owsianik, G.; Nilius, B. TRPM8. In Transient Receptor Potential (TRP) Channels; Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany, 2007; pp. 329–344. [Google Scholar] [CrossRef]
- Izquierdo, C.; Martin-Martinez, M.; Gomez-Monterrey, I.; Gonzalez-Muniz, R. TRPM8 Channels: Advances in Structural Studies and Pharmacological Modulation. Int. J. Mol. Sci. 2021, 22, 8502. [Google Scholar] [CrossRef] [PubMed]
- Yee, N.S.; Brown, R.D.; Lee, M.S.; Zhou, W.; Jensen, C.; Gerke, H.; Yee, R.K. TRPM8 ion channel is aberrantly expressed and required for preventing replicative senescence in pancreatic adenocarcinoma: Potential role of TRPM8 as a biomarker and target. Cancer Biol. Ther. 2012, 13, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Tsavaler, L.; Shapero, M.H.; Morkowski, S.; Laus, R. Trp-p8, a novel prostate-specific gene, is up-regulated in prostate cancer and other malignancies and shares high homology with transient receptor potential calcium channel proteins. Cancer Res. 2001, 61, 3760–3769. [Google Scholar]
- Grolez, G.P.; Gkika, D. TRPM8 Puts the Chill on Prostate Cancer. Pharmaceuticals 2016, 9, 44. [Google Scholar] [CrossRef]
- Zhang, L.; Barritt, G.J. TRPM8 in prostate cancer cells: A potential diagnostic and prognostic marker with a secretory function? Endocr. -Relat. Cancer 2006, 13, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Mikrani, R.; He, Y.; Faran, A.B.M.; Abbas, M.; Naveed, M.; Tang, M.; Zhang, Q.; Li, C.; Zhou, X. TRPM8 channels: A review of distribution and clinical role. Eur. J. Pharmacol. 2020, 882, 173312. [Google Scholar] [CrossRef]
- Yee, N.S. Roles of TRPM8 Ion Channels in Cancer: Proliferation, Survival, and Invasion. Cancers 2015, 7, 2134–2146. [Google Scholar] [CrossRef] [PubMed]
- Knowlton, W.M.; McKemy, D.D. TRPM8: From cold to cancer, peppermint to pain. Curr. Pharm. Biotechnol. 2011, 12, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Wu, H.; Wei, Z.; Wang, X.; Shen, P.; Wang, S.; Wang, A.; Chen, W.; Lu, Y. TRPM8: A potential target for cancer treatment. J. Cancer Res. Clin. 2016, 142, 1871–1881. [Google Scholar] [CrossRef]
- Yu, X.; Hu, Y.; Ru, F.; Kollarik, M.; Undem, B.J.; Yu, S. TRPM8 function and expression in vagal sensory neurons and afferent nerves innervating guinea pig esophagus. Am. J. Physiol.-Gastrointest. Liver Physiol. 2015, 308, G489–G496. [Google Scholar] [CrossRef]
- Lan, X.; Zhao, J.; Song, C.; Yuan, Q.; Liu, X. TRPM8 facilitates proliferation and immune evasion of esophageal cancer cells. Biosci. Rep. 2019, 39, BSR20191878. [Google Scholar] [CrossRef]
- Xu, Q.; Kong, N.; Zhang, J.; Bai, N.; Bi, J.; Li, W. Expression of transient receptor potential cation channel subfamily M member 8 in gastric cancer and its clinical significance. Exp. Ther. Med. 2021, 21, 377. [Google Scholar] [CrossRef]
- Kong, N.; Li, W.; Zhang, J.; Wang, X.; Hu, L.; Xu, Q. TRPM8 as a Potential Biomarker and Therapeutic Target for Gastric Cancer Identified by a Combination of Text Mining and RNA Sequencing. Curr. Gene Ther. 2023, 23, 391–399. [Google Scholar] [CrossRef]
- Fouad, A.; Matsumoto, K.; Amagase, K.; Yasuda, H.; Tominaga, M.; Kato, S. Protective Effect of TRPM8 against Indomethacin-Induced Small Intestinal Injury via the Release of Calcitonin Gene-Related Peptide in Mice. Biol. Pharm. Bull. 2021, 44, 947–957. [Google Scholar] [CrossRef]
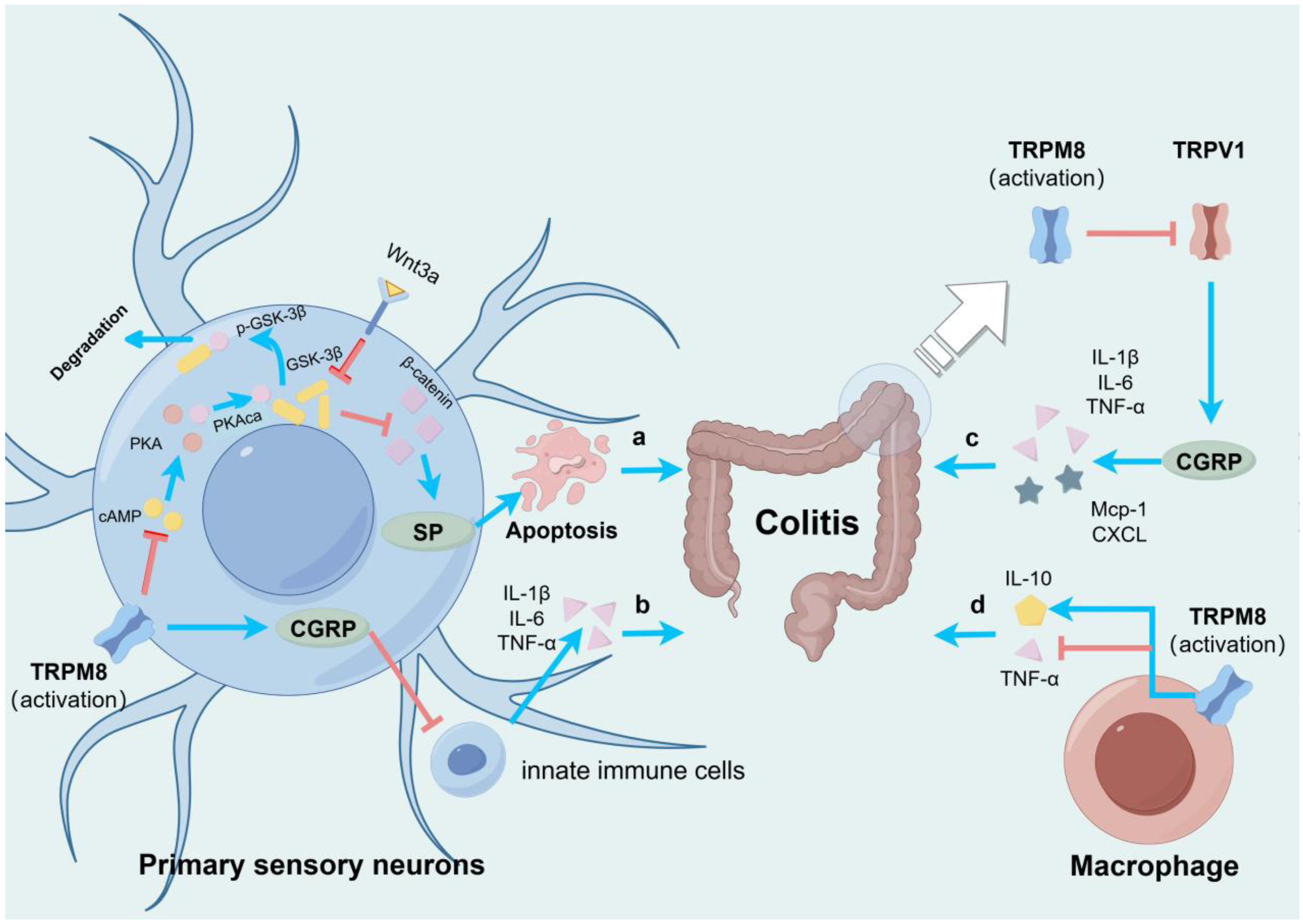
- Zhang, Z.; Yan, X.; Kang, L.; Leng, Z.; Ji, Y.; Yang, S.; Du, X.; Fang, K.; Wang, Z.; Li, Z.; et al. TRPM8 inhibits substance P release from primary sensory neurons via PKA/GSK-3beta to protect colonic epithelium in colitis. Cell Death Dis. 2024, 15, 91. [Google Scholar] [CrossRef]
- de Jong, P.R.; Takahashi, N.; Peiris, M.; Bertin, S.; Lee, J.; Gareau, M.G.; Paniagua, A.; Harris, A.R.; Herdman, D.S.; Corr, M.; et al. TRPM8 on mucosal sensory nerves regulates colitogenic responses by innate immune cells via CGRP. Mucosal Immunol. 2015, 8, 491–504. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, R.; Hyun, E.; Zhao, L.; Lapointe, T.K.; Chapman, K.; Hirota, C.L.; Ghosh, S.; McKemy, D.D.; Vergnolle, N.; Beck, P.L.; et al. TRPM8 activation attenuates inflammatory responses in mouse models of colitis. Proc. Natl. Acad. Sci. USA 2013, 110, 7476–7481. [Google Scholar] [CrossRef] [PubMed]
- Khalil, M.; Babes, A.; Lakra, R.; Forsch, S.; Reeh, P.W.; Wirtz, S.; Becker, C.; Neurath, M.F.; Engel, M.A. Transient receptor potential melastatin 8 ion channel in macrophages modulates colitis through a balance-shift in TNF-alpha and interleukin-10 production. Mucosal Immunol. 2016, 9, 1500–1513. [Google Scholar] [CrossRef]
- Borrelli, F.; Pagano, E.; Romano, B.; Panzera, S.; Maiello, F.; Coppola, D.; De Petrocellis, L.; Buono, L.; Orlando, P.; Izzo, A.A. Colon carcinogenesis is inhibited by the TRPM8 antagonist cannabigerol, a Cannabis-derived non-psychotropic cannabinoid. Carcinogenesis 2014, 35, 2787–2797. [Google Scholar] [CrossRef]
- Pagano, E.; Romano, B.; Cicia, D.; Iannotti, F.A.; Venneri, T.; Lucariello, G.; Nani, M.F.; Cattaneo, F.; De Cicco, P.; D’Armiento, M.; et al. TRPM8 indicates poor prognosis in colorectal cancer patients and its pharmacological targeting reduces tumour growth in mice by inhibiting Wnt/beta-catenin signalling. Br. J. Pharmacol. 2023, 180, 235–251. [Google Scholar] [CrossRef]
- Liu, J.J.; Li, L.Z.; Xu, P. Upregulation of TRPM8 can promote the colon cancer liver metastasis through mediating Akt/GSK-3 signal pathway. Biotechnol. Appl. Biochem. 2022, 69, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Qi, Q.; Li, Y.; Miao, Q.; Yin, W.; Pan, J.; Zhao, Z.; Chen, X.; Yang, F.; Zhou, X.; et al. TCAF2 in Pericytes Promotes Colorectal Cancer Liver Metastasis via Inhibiting Cold-Sensing TRPM8 Channel. Adv. Sci. 2023, 10, e2302717. [Google Scholar] [CrossRef]
- Sugino, S.; Inoue, K.; Kobayashi, R.; Hirose, R.; Doi, T.; Harusato, A.; Dohi, O.; Yoshida, N.; Uchiyama, K.; Ishikawa, T.; et al. Association Between the Cool Temperature-dependent Suppression of Colonic Peristalsis and Transient Receptor Potential Melastatin 8 Activation in Both a Randomized Clinical Trial and an Animal Model. J. Neurogastroenterol. 2022, 28, 693–705. [Google Scholar] [CrossRef]
- Amato, A.; Terzo, S.; Lentini, L.; Marchesa, P.; Mule, F. TRPM8 Channel Activation Reduces the Spontaneous Contractions in Human Distal Colon. Int. J. Mol. Sci. 2020, 21, 5403. [Google Scholar] [CrossRef]
- Peiris, M.; Weerts, Z.; Aktar, R.; Masclee, A.; Blackshaw, A.; Keszthelyi, D. A putative anti-inflammatory role for TRPM8 in irritable bowel syndrome-An exploratory study. Neurogastroenterol. Motil. 2021, 33, e14170. [Google Scholar] [CrossRef]
- Harrington, A.M.; Hughes, P.A.; Martin, C.M.; Yang, J.; Castro, J.; Isaacs, N.J.; Blackshaw, A.L.; Brierley, S.M. A novel role for TRPM8 in visceral afferent function. Pain 2011, 152, 1459–1468. [Google Scholar] [CrossRef]
- Hosoya, T.; Matsumoto, K.; Tashima, K.; Nakamura, H.; Fujino, H.; Murayama, T.; Horie, S. TRPM8 has a key role in experimental colitis-induced visceral hyperalgesia in mice. Neurogastroenterol. Motil. 2014, 26, 1112–1121. [Google Scholar] [CrossRef]
- Fu, J.; Liu, G.; Zhang, X.; Lei, X.; Liu, Q.; Qian, K.; Tong, Q.; Qin, W.; Li, Z.; Cao, Z.; et al. TRPM8 promotes hepatocellular carcinoma progression by inducing SNORA55 mediated nuclear-mitochondrial communication. Cancer Gene Ther. 2023, 30, 738–751. [Google Scholar] [CrossRef]
- Lei, X.; Liu, Q.; Qin, W.; Tong, Q.; Li, Z.; Xu, W.; Liu, G.; Fu, J.; Zhang, J.; Kuang, T.; et al. TRPM8 contributes to liver regeneration via mitochondrial energy metabolism mediated by PGC1alpha. Cell Death Dis. 2022, 13, 1050. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Lei, X.; Cao, Z.; Zhang, J.; Yan, L.; Fu, J.; Tong, Q.; Qin, W.; Shao, Y.; Liu, C.; et al. TRPM8 deficiency attenuates liver fibrosis through S100A9-HNF4alpha signaling. Cell Biosci. 2022, 12, 58. [Google Scholar] [CrossRef] [PubMed]
- Yee, N.S.; Chan, A.S.; Yee, J.D.; Yee, R.K. TRPM7 and TRPM8 Ion Channels in Pancreatic Adenocarcinoma: Potential Roles as Cancer Biomarkers and Targets. Scientifica 2012, 2012, 415158. [Google Scholar] [CrossRef] [PubMed]
- Yee, N.S.; Li, Q.; Kazi, A.A.; Yang, Z.; Berg, A.; Yee, R.K. Aberrantly Over-Expressed TRPM8 Channels in Pancreatic Adenocarcinoma: Correlation with Tumor Size/Stage and Requirement for Cancer Cells Invasion. Cells 2014, 3, 500–516. [Google Scholar] [CrossRef]
- Du, J.D.; Zheng, X.; Chen, Y.L.; Huang, Z.Q.; Cai, S.W.; Jiao, H.B.; Zhu, Z.M.; Hu, B. Elevated Transient Receptor Potential Melastatin 8 (TRPM8) Expression Is Correlated with Poor Prognosis in Pancreatic Cancer. Med. Sci. Monit. 2018, 24, 3720–3725. [Google Scholar] [CrossRef] [PubMed]
- Yee, N.S.; Zhou, W.; Lee, M. Transient receptor potential channel TRPM8 is over-expressed and required for cellular proliferation in pancreatic adenocarcinoma. Cancer Lett. 2010, 297, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Ulareanu, R.; Chiritoiu, G.; Cojocaru, F.; Deftu, A.; Ristoiu, V.; Stanica, L.; Mihailescu, D.F.; Cucu, D. N-glycosylation of the transient receptor potential melastatin 8 channel is altered in pancreatic cancer cells. Tumor Biol. 2017, 39, 1393368724. [Google Scholar] [CrossRef] [PubMed]
- Cucu, D.; Chiritoiu, G.; Petrescu, S.; Babes, A.; Stanica, L.; Duda, D.G.; Horii, A.; Dima, S.O.; Popescu, I. Characterization of functional transient receptor potential melastatin 8 channels in human pancreatic ductal adenocarcinoma cells. Pancreas 2014, 43, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Chen, J.; Liu, A.A.; Chen, L.; Liang, X.; Peng, J.F.; Zheng, M.H.; Li, J.D.; Cao, Y.B.; Shao, C.H. Identifying Liver Metastasis-Related Genes Through a Coexpression Network to Construct a 5-Gene Model for Predicting Pancreatic Ductal Adenocarcinoma Patient Prognosis. Pancreas 2023, 52, e151–e162. [Google Scholar] [CrossRef]
- Taylor, D.; Hamid, S.M.; Andres, A.M.; Saadaeijahromi, H.; Piplani, H.; Germano, J.F.; Song, Y.; Sawaged, S.; Feuer, R.; Pandol, S.J.; et al. Antiviral Effects of Menthol on Coxsackievirus B. Viruses 2020, 12, 373. [Google Scholar] [CrossRef]
- Yu, S.; Undem, B.J.; Kollarik, M. Vagal afferent nerves with nociceptive properties in guinea-pig oesophagus. J. Physiol. 2005, 563, 831–842. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Jones, S.; Brody, K.; Costa, M.; Brookes, S.J. Thermosensitive transient receptor potential channels in vagal afferent neurons of the mouse. Am. J. Physiol.-Gastrointest. Liver Physiol. 2004, 286, G983–G991. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, S.; Kato, K.; Ono, Y.; Yano, K.; Kurosaka, H.; Takahashi, A.; Abeta, H.; Kushiro, T.; Miyamoto, S.; Kurihara, R.; et al. Oral peppermint oil is a useful antispasmodic for double-contrast barium meal examination. J. Gastroenterol. Hepatol. 2006, 21, 1297–1301. [Google Scholar] [CrossRef]
- Choi, Y.J.; Park, M.I.; Park, S.J.; Moon, W.; Kim, S.E.; Kwon, H.J.; Kim, J.H.; Jeon, W.S. The effect of water bolus temperature on esophageal motor function as measured by high-resolution manometry. Neurogastroenterol. Motil. 2014, 26, 1628–1634. [Google Scholar] [CrossRef]
- Lei, W.Y.; Liang, S.W.; Hung, J.S.; Wong, M.W.; Liu, T.T.; Yi, C.H.; Lin, L.; Orr, W.C.; Chen, C.L. Effects of menthol on esophageal motility in humans: Studies using high-resolution manometry. Neurogastroenterol. Motil. 2022, 34, e14267. [Google Scholar] [CrossRef]
- Silva, R.O.; Bingana, R.D.; Sales, T.; Moreira, R.; Costa, D.; Sales, K.; Brito, G.; Santos, A.A.; Souza, M.; Soares, P.; et al. Role of TRPV1 receptor in inflammation and impairment of esophageal mucosal integrity in a murine model of nonerosive reflux disease. Neurogastroenterol. Motil. 2018, 30, e13340. [Google Scholar] [CrossRef]
- Banerjee, B.; Medda, B.K.; Lazarova, Z.; Bansal, N.; Shaker, R.; Sengupta, J.N. Effect of reflux-induced inflammation on transient receptor potential vanilloid one (TRPV1) expression in primary sensory neurons innervating the oesophagus of rats. NNeurogastroenterol. Motil. 2007, 19, 681–691. [Google Scholar] [CrossRef] [PubMed]
- Guarino, M.P.; Cheng, L.; Ma, J.; Harnett, K.; Biancani, P.; Altomare, A.; Panzera, F.; Behar, J.; Cicala, M. Increased TRPV1 gene expression in esophageal mucosa of patients with non-erosive and erosive reflux disease. Neurogastroenterol. Motil. 2010, 22, 746-e219. [Google Scholar] [CrossRef] [PubMed]
- Rozza, A.L.; Hiruma-Lima, C.A.; Takahira, R.K.; Padovani, C.R.; Pellizzon, C.H. Effect of menthol in experimentally induced ulcers: Pathways of gastroprotection. Chem.-Biol. Interact. 2013, 206, 272–278. [Google Scholar] [CrossRef]
- Takaishi, M.; Uchida, K.; Suzuki, Y.; Matsui, H.; Shimada, T.; Fujita, F.; Tominaga, M. Reciprocal effects of capsaicin and menthol on thermosensation through regulated activities of TRPV1 and TRPM8. J. Physiol. Sci. 2016, 66, 143–155. [Google Scholar] [CrossRef]
- Zhang, Z.; Wu, X.; Zhang, L.; Mao, A.; Ma, X.; He, D. Menthol relieves acid reflux inflammation by regulating TRPV1 in esophageal epithelial cells. Biochem. Biophys. Res. Commun. 2020, 525, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA-Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Schizas, D.; Lazaridis, I.I.; Moris, D.; Mastoraki, A.; Lazaridis, L.D.; Tsilimigras, D.I.; Charalampakis, N.; Liakakos, T. The role of surgical treatment in isolated organ recurrence of esophageal cancer-a systematic review of the literature. World J. Surg. Oncol. 2018, 16, 55. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, H.; Seto, Y.; Takenaka, R.; Okuma, K.; Kiritooshi, T.; Mori, K.; Yamada, K.; Fukuda, T.; Kaminishi, M.; Abe, O.; et al. Survival comparison between radical surgery and definitive chemoradiation in 267 esophageal squamous cell carcinomas in a single institution: A propensity-matched study. PLoS ONE 2017, 12, e177133. [Google Scholar] [CrossRef] [PubMed]
- Yudin, Y.; Rohacs, T. Regulation of TRPM8 channel activity. Mol. Cell. Endocrinol. 2012, 353, 68–74. [Google Scholar] [CrossRef]
- Yamamura, H.; Ugawa, S.; Ueda, T.; Morita, A.; Shimada, S. TRPM8 activation suppresses cellular viability in human melanoma. Am. J. Physiol.-Cell Physiol. 2008, 295, C296–C301. [Google Scholar] [CrossRef]
- Matsuoka, T.; Yashiro, M. Biomarkers of gastric cancer: Current topics and future perspective. World J. Gastroenterol. 2018, 24, 2818–2832. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.; Cunningham, D.; Oliveira, J. Gastric cancer: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann. Oncol. 2009, 20 (Suppl. S4), 34–36. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, N.; Yasuda, K.; Kitano, S. Laparoscopic gastrectomy with lymph node dissection for gastric cancer. Gastric Cancer 2006, 9, 167–176. [Google Scholar] [CrossRef]
- Rozza, A.L.; Meira, D.F.F.; Souza, B.A.; Pellizzon, C.H. The gastroprotective effect of menthol: Involvement of anti-apoptotic, antioxidant and anti-inflammatory activities. PLoS ONE 2014, 9, e86686. [Google Scholar] [CrossRef]
- Weinstock, J.V. Substance P and the regulation of inflammation in infections and inflammatory bowel disease. Acta Physiol. 2015, 213, 453–461. [Google Scholar] [CrossRef]
- Holzmann, B. Modulation of immune responses by the neuropeptide CGRP. Amino Acids 2013, 45, 1–7. [Google Scholar] [CrossRef]
- Wu, W.; Feng, B.; Liu, J.; Li, Y.; Liao, Y.; Wang, S.; Tao, S.; Hu, S.; He, W.; Shu, Q.; et al. The CGRP/macrophage axis signal facilitates inflammation recovery in the intestine. Clin. Immunol. 2022, 245, 109154. [Google Scholar] [CrossRef] [PubMed]
- Armulik, A.; Genove, G.; Betsholtz, C. Pericytes: Developmental, physiological, and pathological perspectives, problems, and promises. Dev. Cell 2011, 21, 193–215. [Google Scholar] [CrossRef]
- Gkika, D.; Lemonnier, L.; Shapovalov, G.; Gordienko, D.; Poux, C.; Bernardini, M.; Bokhobza, A.; Bidaux, G.; Degerny, C.; Verreman, K.; et al. TRP channel-associated factors are a novel protein family that regulates TRPM8 trafficking and activity. J. Cell Biol. 2015, 208, 89–107. [Google Scholar] [CrossRef]
- Pittler, M.H.; Ernst, E. Peppermint oil for irritable bowel syndrome: A critical review and metaanalysis. Am. J. Gastroenterol. 1998, 93, 1131–1135. [Google Scholar] [CrossRef]
- Khanna, R.; MacDonald, J.K.; Levesque, B.G. Peppermint oil for the treatment of irritable bowel syndrome: A systematic review and meta-analysis. J. Clin. Gastroenterol. 2014, 48, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Inoue, K.; Dohi, O.; Gen, Y.; Jo, M.; Mazaki, T.; Tokita, K.; Yoshida, N.; Okayama, T.; Kamada, K.; Katada, K.; et al. L-menthol improves adenoma detection rate during colonoscopy: A randomized trial. Endoscopy 2014, 46, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Inoue, K.; Okuda, T.; Oka, K.; Sugino, S.; Endo, Y.; Ota, T.; Minagawa, Y.; Yasue, C.; Tsuji, T.; Katayama, T.; et al. Effects of L-Menthol and Carbon Dioxide on the Adenoma Detection Rate during Colonoscopy: L-Menthol and Carbon Dioxide on Colonoscopy. Digestion 2020, 101, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Klein, A.H.; Sawyer, C.M.; Carstens, M.I.; Tsagareli, M.G.; Tsiklauri, N.; Carstens, E. Topical application of L-menthol induces heat analgesia, mechanical allodynia, and a biphasic effect on cold sensitivity in rats. Behav. Brain Res. 2010, 212, 179–186. [Google Scholar] [CrossRef]
- Green, B.G.; McAuliffe, B.L. Menthol desensitization of capsaicin irritation. Evidence of a short-term anti-nociceptive effect. Physiol. Behav. 2000, 68, 631–639. [Google Scholar] [CrossRef]
- Fonfria, E.; Murdock, P.R.; Cusdin, F.S.; Benham, C.D.; Kelsell, R.E.; McNulty, S. Tissue distribution profiles of the human TRPM cation channel family. J. Recept. Signal Transduct. 2006, 26, 159–178. [Google Scholar] [CrossRef]
- Tracy, S.; Hofling, K.; Pirruccello, S.; Lane, P.H.; Reyna, S.M.; Gauntt, C.J. Group B coxsackievirus myocarditis and pancreatitis: Connection between viral virulence phenotypes in mice. J. Med. Virol. 2000, 62, 70–81. [Google Scholar] [CrossRef]
- Huber, S.; Ramsingh, A.I. Coxsackievirus-induced pancreatitis. Viral Immunol. 2004, 17, 358–369. [Google Scholar] [CrossRef]
- Amato, A.; Serio, R.; Mule, F. Involvement of cholinergic nicotinic receptors in the menthol-induced gastric relaxation. Eur. J. Pharmacol. 2014, 745, 129–134. [Google Scholar] [CrossRef]
- Sherkheli, M.A.; Vogt-Eisele, A.K.; Bura, D.; Beltran, M.L.; Gisselmann, G.; Hatt, H. Characterization of selective TRPM8 ligands and their structure activity response (S.A.R) relationship. J. Pharm. Pharm. Sci. 2010, 13, 242–253. [Google Scholar] [CrossRef]
- Macpherson, L.J.; Hwang, S.W.; Miyamoto, T.; Dubin, A.E.; Patapoutian, A.; Story, G.M. More than cool: Promiscuous relationships of menthol and other sensory compounds. Mol. Cell. Neurosci. 2006, 32, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; G, G.; Ak, V.E.; Jf, D.; H, H. Menthol derivative WS-12 selectively activates transient receptor potential melastatin-8 (TRPM8) ion channels. Pak. J. Pharm. Sci. 2008, 21, 370–378. [Google Scholar] [PubMed]
- DeFalco, J.; Duncton, M.A.; Emerling, D. TRPM8 biology and medicinal chemistry. Curr. Top. Med. Chem. 2011, 11, 2237–2252. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Muniz, R.; Bonache, M.A.; Martin-Escura, C.; Gomez-Monterrey, I. Recent Progress in TRPM8 Modulation: An Update. Int. J. Mol. Sci. 2019, 20, 2618. [Google Scholar] [CrossRef]
- Pergolizzi, J.J.; Taylor, R.J.; LeQuang, J.A.; Raffa, R.B. The role and mechanism of action of menthol in topical analgesic products. J. Clin. Pharm. Ther. 2018, 43, 313–319. [Google Scholar] [CrossRef]
- Li, Z.; Zhang, H.; Wang, Y.; Li, Y.; Li, Q.; Zhang, L. The distinctive role of menthol in pain and analgesia: Mechanisms, practices, and advances. Front. Mol. Neurosci. 2022, 15, 1006908. [Google Scholar] [CrossRef]
| Organs Distributed by TRPM8 | Functions | Related Disorders | References |
|---|---|---|---|
| Esophagus | Participating in esophageal sensory transduction | Esophageal sensation and nociception | Yu et al. (2015) [17] |
| Esophagus | Leading to immune evasion of esophageal cancer cells | Esophageal cancer | Lan et al. (2019) [18] |
| Stomach | Promoting gastric cancer cell proliferation and metastasis in vivo | Gastric cancer | Xu et al. (2021) [19] |
| Stomach | As candidates for novel biomarkers in gastric cancer | Gastric cancer | Kong et al. (2023) [20] |
| Small intestine | Relieving indomethacin-induced small intestinal injury by promoting the expression of calcitonin gene-related peptide (CGRP) | Small intestinal injury | Fouad et al. (2021) [21] |
| Colon | Inhibiting the role of substance P (SP) in promoting colonic epithelial apoptosis and relieving colitis | Colitis | Zhang et al. (2024) [22] |
| Colon | Relieving innate inflammatory responses by promoting the expression of CGRP | Colitis | De Jong et al. (2015) [23] |
| Colon | Suppressing the pro-inflammatory effect of TRPV1 by inhibiting the expression of CGRP | Colitis | Ramachandran et al. (2013) [24] |
| Colon | Regulating tumor necrosis factor-α (TNF-α) and interleukin (IL)-10 production | Colitis | Khalil et al. (2016) [25] |
| Colon | Regulating the growth of colorectal cancer cells | Colorectal cancer | Borrelli et al. (2014) [26] |
| Colon | Regulating tumor development via inhibition of oncogenic Wnt/β-catenin signaling | Colorectal cancer | Pagano et al. (2023) [27] |
| Colon | Promoting the progression and epithelial–mesenchymal transition (EMT) of colon cancer cells | Colon cancer liver metastasis | Liu et al. (2022) [28] |
| Colon | Suppressing the EMT of colon cancer cells | Colon cancer liver metastasis | Li et al. (2023) [29] |
| Colon | Suppressing colonic peristalsis | Irritable bowel syndrome (IBS) | Sugino et al. (2022) [30] |
| Colon | Reducing colonic spontaneous motility | IBS | Amato et al. (2020) [31] |
| Colon | Reducing release of inflammatory cytokines IL-1β, IL-6, and TNF-α | IBS | Peiris et al. (2021) [32] |
| Colon | Desensitizing afferents to mechanical stimulation | Colonic sensation | Harrington et al. (2011) [33] |
| Colon | Contributing to the visceral hyperalgesia of experimental colitis | Colitis | Hosoya et al. (2014) [34] |
| Liver | Promoting hepatocellular carcinoma progression | Hepatocellular carcinoma | Fu et al. (2023) [35] |
| Liver | Contributing to liver regeneration | Hepatectomy | Lei et al. (2022) [36] |
| Liver | Regulating S100A9 (commonly known as calgranulin B)-hepatocyte nuclear factor 4α (HNF4α) signaling | Inflammation; liver fibrosis | Liu et al. (2022) [37] |
| Pancreas | As a cancer biomarker and target | Pancreatic adenocarcinoma | Yee et al. (2012) [38] |
| Pancreas | Related to tumor size/stage and requirement for cancer cell invasion | Pancreatic adenocarcinoma | Yee et al. (2014) [39] |
| Pancreas | Might be a useful prognostic factor for patients with pancreatic adenocarcinoma | Pancreatic adenocarcinoma | Du et al. (2018) [40] |
| Pancreas | Being required for cellular proliferation in pancreatic adenocarcinoma | Pancreatic adenocarcinoma | Yee et al. (2010) [41] |
| Pancreas | Preventing replicative senescence in pancreatic adenocarcinoma | Pancreatic adenocarcinoma | Yee et al. (2012) [9] |
| Pancreas | Affecting cell proliferation, cell migration, and calcium uptake | Pancreatic adenocarcinoma | Roxana et al. (2017) [42] |
| Pancreas | Inhibiting pancreatic ductal adenocarcinoma (PDA) cell motility | PDA | Cucu et al. (2014) [43] |
| Pancreas | Constructing a 5-Gene Model for predicting PDA patient prognosis | PDA | Liu et al. (2023) [44] |
| Pancreas | Blocking TRPV1-mediated mitochondrial fragmentation following Coxsackie virus B (CVB) exposure and attenuates infection | Pancreatitis | Taylor et al. (2020) [45] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Z.; Peng, S.; Huang, W.; Zhang, Y.; Liu, Y.; Yu, X.; Shen, L. The Role and Function of TRPM8 in the Digestive System. Biomolecules 2024, 14, 877. https://doi.org/10.3390/biom14070877
Wu Z, Peng S, Huang W, Zhang Y, Liu Y, Yu X, Shen L. The Role and Function of TRPM8 in the Digestive System. Biomolecules. 2024; 14(7):877. https://doi.org/10.3390/biom14070877
Chicago/Turabian StyleWu, Zunan, Shuai Peng, Wensha Huang, Yuling Zhang, Yashi Liu, Xiaoyun Yu, and Lei Shen. 2024. "The Role and Function of TRPM8 in the Digestive System" Biomolecules 14, no. 7: 877. https://doi.org/10.3390/biom14070877
APA StyleWu, Z., Peng, S., Huang, W., Zhang, Y., Liu, Y., Yu, X., & Shen, L. (2024). The Role and Function of TRPM8 in the Digestive System. Biomolecules, 14(7), 877. https://doi.org/10.3390/biom14070877






