Placenta Extracellular Vesicles: Messengers Connecting Maternal and Fetal Systems
Abstract
:1. Introduction
2. Extracellular Vesicles, Cargo Contents, and Critical Tools for EV Analysis
3. Effects of Placental Extracellular Vesicles on Maternal Systems
3.1. Effects of Placental EV on Maternal Cardiovascular Responses
3.2. Effects of Placenta EV on Maternal Immune System Responses
3.3. Effects of Placental EV on the Uterus and Other Maternal Organs
3.4. Effects of MicroRNAs (miRs) and Other Small RNAs Contain within Placental-Derived Extracellular Vesicles on Maternal Systems
4. Effects of Placental Extracellular Vesicles on the Fetal Brain and Other Fetal Tissues
5. Effects of Maternal Diseases on Placental Extracellular Vesicles
5.1. Maternal Non-Communicable Diseases and Effects on Placental Extracellular Vesicles
5.2. Maternal Infectious Diseases and Effects on Placental Extracellular Vesicles
6. Usage of Placental Extracellular Vesicles for Early Diagnostic and Therapeutic Strategies to Mitigate Offspring Diseases
7. Conclusions and Future Directions
Funding
Conflicts of Interest
References
- Bidarimath, M.; Khalaj, K.; Kridli, R.T.; Kan, F.W.; Koti, M.; Tayade, C. Extracellular vesicle mediated intercellular communication at the porcine maternal-fetal interface: A new paradigm for conceptus-endometrial cross-talk. Sci. Rep. 2017, 7, 40476. [Google Scholar] [CrossRef] [PubMed]
- Kshirsagar, S.K.; Alam, S.M.; Jasti, S.; Hodes, H.; Nauser, T.; Gilliam, M.; Billstrand, C.; Hunt, J.S.; Petroff, M.G. Immunomodulatory molecules are released from the first trimester and term placenta via exosomes. Placenta 2012, 33, 982–990. [Google Scholar] [CrossRef] [PubMed]
- Southcombe, J.; Tannetta, D.; Redman, C.; Sargent, I. The immunomodulatory role of syncytiotrophoblast microvesicles. PLoS ONE 2011, 6, e20245. [Google Scholar] [CrossRef] [PubMed]
- Messerli, M.; May, K.; Hansson, S.R.; Schneider, H.; Holzgreve, W.; Hahn, S.; Rusterholz, C. Feto-maternal interactions in pregnancies: Placental microparticles activate peripheral blood monocytes. Placenta 2010, 31, 106–112. [Google Scholar] [CrossRef]
- Gupta, A.K.; Hasler, P.; Holzgreve, W.; Gebhardt, S.; Hahn, S. Induction of neutrophil extracellular DNA lattices by placental microparticles and IL-8 and their presence in preeclampsia. Hum. Immunol. 2005, 66, 1146–1154. [Google Scholar] [CrossRef] [PubMed]
- Song, P.; Anna, B.; Scott, G.E.; Chamley, L.W. The interaction of placental micro-EVs with immune cells in vivo and in vitro. Am. J. Reprod. Immunol. 2023, 90, e13766. [Google Scholar] [CrossRef] [PubMed]
- Bai, K.; Li, J.; Lin, L.; Zhang, Q.; Zhong, J.; Liu, X.; Cao, D.; Duan, Y.G.; Yao, Y.; Li, R.H.W.; et al. Placenta exosomal miRNA-30d-5p facilitates decidual macrophage polarization by targeting HDAC9. J. Leukoc. Biol. 2023, 113, 434–444. [Google Scholar] [CrossRef] [PubMed]
- Bai, K.; Lee, C.L.; Liu, X.; Li, J.; Cao, D.; Zhang, L.; Hu, D.; Li, H.; Hou, Y.; Xu, Y.; et al. Human placental exosomes induce maternal systemic immune tolerance by reprogramming circulating monocytes. J. Nanobiotechnol. 2022, 20, 86. [Google Scholar] [CrossRef] [PubMed]
- Kovács, Á.F.; Fekete, N.; Turiák, L.; Ács, A.; Kőhidai, L.; Buzás, E.I.; Pállinger, É. Unravelling the Role of Trophoblastic-Derived Extracellular Vesicles in Regulatory T Cell Differentiation. Int. J. Mol. Sci. 2019, 20, 3457. [Google Scholar] [CrossRef]
- Cooke, W.R.; Jiang, P.; Ji, L.; Bai, J.; Jones, G.D.; Lo, Y.M.D.; Redman, C.; Vatish, M. Differential 5’-tRNA Fragment Expression in Circulating Preeclampsia Syncytiotrophoblast Vesicles Drives Macrophage Inflammation. Hypertension 2024, 81, 876–886. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Kusama, K.; Bai, R.; Sakurai, T.; Isuzugawa, K.; Godkin, J.D.; Suda, Y.; Imakawa, K. Induction of IFNT-Stimulated Genes by Conceptus-Derived Exosomes during the Attachment Period. PLoS ONE 2016, 11, e0158278. [Google Scholar] [CrossRef] [PubMed]
- Muhandiram, S.; Dissanayake, K.; Orro, T.; Godakumara, K.; Kodithuwakku, S.; Fazeli, A. Secretory Proteomic Responses of Endometrial Epithelial Cells to Trophoblast-Derived Extracellular Vesicles. Int. J. Mol. Sci. 2023, 24, 11924. [Google Scholar] [CrossRef] [PubMed]
- Godakumara, K.; Heath, P.R.; Fazeli, A. Rhythm of the First Language: Dynamics of Extracellular Vesicle-Based Embryo-Maternal Communication in the Pre-Implantation Microenvironment. Int. J. Mol. Sci. 2023, 24, 6811. [Google Scholar] [CrossRef] [PubMed]
- Godakumara, K.; Ord, J.; Lättekivi, F.; Dissanayake, K.; Viil, J.; Boggavarapu, N.R.; Faridani, O.R.; Jääger, K.; Velthut-Meikas, A.; Jaakma, Ü.; et al. Trophoblast derived extracellular vesicles specifically alter the transcriptome of endometrial cells and may constitute a critical component of embryo-maternal communication. Reprod. Biol. Endocrinol. 2021, 19, 115. [Google Scholar] [CrossRef]
- Jiang, L.; Fei, H.; Jin, X.; Liu, X.; Yang, C.; Li, C.; Chen, J.; Yang, A.; Zhu, J.; Wang, H.; et al. Extracellular Vesicle-Mediated Secretion of HLA-E by Trophoblasts Maintains Pregnancy by Regulating the Metabolism of Decidual NK Cells. Int. J. Biol. Sci. 2021, 17, 4377–4395. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.K.; Houshdaran, S.; Robinson, J.F.; Gormley, M.J.; Kwan, E.Y.; Kapidzic, M.; Schilling, B.; Giudice, L.C.; Fisher, S.J. Cytotrophoblast extracellular vesicles enhance decidual cell secretion of immune modulators via TNFα. Development 2020, 147, dev187013. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Li, Q.; Zhang, Q.; Li, Z.; Yao, X.; Guo, Y.; Xiao, L.; Wang, X.; Ni, H. Exosomes derived from placental trophoblast cells regulate endometrial epithelial receptivity in dairy cows during pregnancy. J. Reprod. Dev. 2022, 68, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Tersigni, C.; Furqan Bari, M.; Cai, S.; Zhang, W.; Kandzija, N.; Buchan, A.; Miranda, F.; Di Simone, N.; Redman, C.W.; Bastie, C.; et al. Syncytiotrophoblast-derived extracellular vesicles carry apolipoprotein-E and affect lipid synthesis of liver cells in vitro. J. Cell. Mol. Med. 2022, 26, 123–132. [Google Scholar] [CrossRef]
- Luo, S.S.; Ishibashi, O.; Ishikawa, G.; Ishikawa, T.; Katayama, A.; Mishima, T.; Takizawa, T.; Shigihara, T.; Goto, T.; Izumi, A.; et al. Human villous trophoblasts express and secrete placenta-specific microRNAs into maternal circulation via exosomes. Biol. Reprod. 2009, 81, 717–729. [Google Scholar] [CrossRef]
- Tiozzo, C.; Bustoros, M.; Lin, X.; Manzano De Mejia, C.; Gurzenda, E.; Chavez, M.; Hanna, I.; Aguiari, P.; Perin, L.; Hanna, N. Placental extracellular vesicles-associated microRNA-519c mediates endotoxin adaptation in pregnancy. Am. J. Obstet. Gynecol. 2021, 225, 681.e1–681.e620. [Google Scholar] [CrossRef]
- Chaiwangyen, W.; Murrieta-Coxca, J.M.; Favaro, R.R.; Photini, S.M.; Gutiérrez-Samudio, R.N.; Schleussner, E.; Markert, U.R.; Morales-Prieto, D.M. MiR-519d-3p in Trophoblastic Cells: Effects, Targets and Transfer to Allogeneic Immune Cells via Extracellular Vesicles. Int. J. Mol. Sci. 2020, 21, 3458. [Google Scholar] [CrossRef]
- Latos, P.A.; Hemberger, M. From the stem of the placental tree: Trophoblast stem cells and their progeny. Development 2016, 143, 3650–3660. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Tan, Q.; Liang, J.; Cao, D.; Wang, S.; Liang, J.; Chen, K.; Wang, Z. Placental trophoblast cell-derived exosomal microRNA-1290 promotes the interaction between endometrium and embryo by targeting LHX6. Mol. Ther. Nucleic Acids 2021, 26, 760–772. [Google Scholar] [CrossRef] [PubMed]
- Vu, H.T.H.; Kaur, H.; Kies, K.R.; Starks, R.R.; Tuteja, G. Identifying novel regulators of placental development using time-series transcriptome data. Life Sci. Alliance 2023, 6, e202201788. [Google Scholar] [CrossRef] [PubMed]
- Hu, D.; Cross, J.C. Development and function of trophoblast giant cells in the rodent placenta. Int. J. Dev. Biol. 2010, 54, 341–354. [Google Scholar] [CrossRef] [PubMed]
- Natale, B.V.; Schweitzer, C.; Hughes, M.; Globisch, M.A.; Kotadia, R.; Tremblay, E.; Vu, P.; Cross, J.C.; Natale, D.R.C. Sca-1 identifies a trophoblast population with multipotent potential in the mid-gestation mouse placenta. Sci. Rep. 2017, 7, 5575. [Google Scholar] [CrossRef] [PubMed]
- Simmons, D.G.; Fortier, A.L.; Cross, J.C. Diverse subtypes and developmental origins of trophoblast giant cells in the mouse placenta. Dev. Biol. 2007, 304, 567–578. [Google Scholar] [CrossRef] [PubMed]
- Lackinger, M.; Sungur, A.; Daswani, R.; Soutschek, M.; Bicker, S.; Stemmler, L.; Wüst, T.; Fiore, R.; Dieterich, C.; Schwarting, R.K.; et al. A placental mammal-specific microRNA cluster acts as a natural brake for sociability in mice. EMBO Rep. 2019, 20, e46429. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, R.; Zhang, J.; Wang, P.; Wang, Z.; Gao, J.; Liu, X. Role of Extracellular Vesicles in Placental Inflammation and Local Immune Balance. Mediat. Inflamm. 2021, 2021, 5558048. [Google Scholar] [CrossRef]
- Gall, A.R.; Amoah, S.; Kitase, Y.; Jantzie, L.L. Placental mediated mechanisms of perinatal brain injury: Evolving inflammation and exosomes. Exp. Neurol. 2022, 347, 113914. [Google Scholar] [CrossRef]
- León, J.; Acurio, J.; Bergman, L.; López, J.; Karin Wikström, A.; Torres-Vergara, P.; Troncoso, F.; Castro, F.O.; Vatish, M.; Escudero, C. Disruption of the Blood-Brain Barrier by Extracellular Vesicles From Preeclampsia Plasma and Hypoxic Placentae: Attenuation by Magnesium Sulfate. Hypertension 2021, 78, 1423–1433. [Google Scholar] [CrossRef]
- Stefanski, A.L.; Martinez, N.; Peterson, L.K.; Callahan, T.J.; Treacy, E.; Luck, M.; Friend, S.F.; Hermesch, A.; Maltepe, E.; Phang, T.; et al. Murine trophoblast-derived and pregnancy-associated exosome-enriched extracellular vesicle microRNAs: Implications for placenta driven effects on maternal physiology. PLoS ONE 2019, 14, e0210675. [Google Scholar] [CrossRef] [PubMed]
- Neckles, V.N.; Morton, M.C.; Holmberg, J.C.; Sokolov, A.M.; Nottoli, T.; Liu, D.; Feliciano, D.M. A transgenic inducible GFP extracellular-vesicle reporter (TIGER) mouse illuminates neonatal cortical astrocytes as a source of immunomodulatory extracellular vesicles. Sci. Rep. 2019, 9, 3094. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, P.L.; Leone, G. Expression of Cre recombinase in early diploid trophoblast cells of the mouse placenta. Genesis 2007, 45, 129–134. [Google Scholar] [CrossRef]
- Tersigni, C.; Di Simone, N.; Lucchetti, D.; Colella, F.; Onori, M.; Perossini, S.; Vidiri, A.; Franco, R.; Sgambato, A.; Vatish, M.; et al. Shedding of Syncytiotrophoblast-Derived Extracellular Vesicles Is Increased in Placenta Previa and Accreta Spectrum. Reprod. Sci. 2024, 31, 2043–2048. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.; Subedi, R.; Kundu, I.; Idicula-Thomas, S.; Shinde, U.; Bansal, V.; Balsarkar, G.; Mayadeo, N.; Das, D.K.; Balasinor, N.; et al. Differential proteomics of circulating extracellular vesicles of placental origin isolated from women with early-onset preeclampsia reveal aberrant innate immune and hemostasis processes. Am. J. Reprod. Immunol. 2024, 91, e13860. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.R.; Cheng, L.; Wang, Y.P. Prediction of severe preeclampsia and intrauterine growth restriction based on serum placental exosome miR-520a-5p levels during the first-trimester. Medicine 2024, 103, e38188. [Google Scholar] [CrossRef] [PubMed]
- Awoyemi, T.; Jiang, S.; Rahbar, M.; Logentherian, P.; Collett, G.; Zhang, W.; Cribbs, A.; Cerdeira, S.; Vatish, M. MicroRNA analysis of medium/large placenta extracellular vesicles in normal and preeclampsia pregnancies. Front. Cardiovasc. Med. 2024, 11, 1371168. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Li, Q.; Liu, X.; Huang, H.; Wang, G.; Zhang, C.; Meng, Y.; Yang, W. Placental exosomal miR-125b triggered endothelial barrier injury in preeclampsia. Placenta 2023, 137, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Dutta, S.; Lai, A.; Scholz-Romero, K.; Shiddiky, M.J.A.; Yamauchi, Y.; Mishra, J.S.; Rice, G.E.; Hyett, J.; Kumar, S.; Salomon, C. Hypoxia-induced small extracellular vesicle proteins regulate proinflammatory cytokines and systemic blood pressure in pregnant rats. Clin. Sci. 2020, 134, 593–607. [Google Scholar] [CrossRef]
- Cheung, S.; Barrett, C.; Chen, Q.; Groom, K.; Chamley, L.; Lau, S.Y. First trimester placental extracellular vesicles likely contribute to the vasodilation of maternal resistance arteries in normal pregnancy. Placenta 2022, 129, 84–86. [Google Scholar] [CrossRef] [PubMed]
- Erlandsson, L.; Ohlsson, L.; Masoumi, Z.; Rehnström, M.; Cronqvist, T.; Edvinsson, L.; Hansson, S.R. Preliminary evidence that blocking the uptake of placenta-derived preeclamptic extracellular vesicles protects the vascular endothelium and prevents vasoconstriction. Sci. Rep. 2023, 13, 18425. [Google Scholar] [CrossRef] [PubMed]
- Gu, M.; Chen, P.; Zeng, D.; Jiang, X.; Lv, Q.; Li, Y.; Zhang, F.; Wan, S.; Zhou, Q.; Lu, Y.; et al. Preeclampsia impedes foetal kidney development by delivering placenta-derived exosomes to glomerular endothelial cells. Cell Commun. Signal 2023, 21, 336. [Google Scholar] [CrossRef]
- Martire, S.; Montarolo, F.; Spadaro, M.; Perga, S.; Sforza, M.L.; Marozio, L.; Frezet, F.; Bruno, S.; Chiabotto, G.; Deregibus, M.C.; et al. A First Phenotypic and Functional Characterization of Placental Extracellular Vesicles from Women with Multiple Sclerosis. Int. J. Mol. Sci. 2021, 22, 2875. [Google Scholar] [CrossRef] [PubMed]
- Kandzija, N.; Zhang, W.; Motta-Mejia, C.; Mhlomi, V.; McGowan-Downey, J.; James, T.; Cerdeira, A.S.; Tannetta, D.; Sargent, I.; Redman, C.W.; et al. Placental extracellular vesicles express active dipeptidyl peptidase IV; levels are increased in gestational diabetes mellitus. J. Extracell. Vesicles 2019, 8, 1617000. [Google Scholar] [CrossRef]
- Kandzija, N.; Payne, S.; Cooke, W.R.; Seedat, F.; Fischer, R.; Vatish, M. Protein Profiling of Placental Extracellular Vesicles in Gestational Diabetes Mellitus. Int. J. Mol. Sci. 2024, 25, 1947. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Van Oostdam, A.S.; Toro-Ortíz, J.C.; López, J.A.; Noyola, D.E.; García-López, D.A.; Durán-Figueroa, N.V.; Martínez-Martínez, E.; Portales-Pérez, D.P.; Salgado-Bustamante, M.; López-Hernández, Y. Placental exosomes isolated from urine of patients with gestational diabetes exhibit a differential profile expression of microRNAs across gestation. Int. J. Mol. Med. 2020, 46, 546–560. [Google Scholar] [CrossRef]
- Nair, S.; Jayabalan, N.; Guanzon, D.; Palma, C.; Scholz-Romero, K.; Elfeky, O.; Zuñiga, F.; Ormazabal, V.; Diaz, E.; Rice, G.E.; et al. Human placental exosomes in gestational diabetes mellitus carry a specific set of miRNAs associated with skeletal muscle insulin sensitivity. Clin. Sci. 2018, 132, 2451–2467. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yuan, Y.; Shen, S.; Ge, Z.; Zhu, D.; Bi, Y. Placenta-derived exosomes exacerbate beta cell dysfunction in gestational diabetes mellitus through delivery of miR-320b. Front. Endocrinol. (Lausanne) 2023, 14, 1282075. [Google Scholar] [CrossRef]
- Salomon, C.; Scholz-Romero, K.; Sarker, S.; Sweeney, E.; Kobayashi, M.; Correa, P.; Longo, S.; Duncombe, G.; Mitchell, M.D.; Rice, G.E.; et al. Gestational Diabetes Mellitus Is Associated With Changes in the Concentration and Bioactivity of Placenta-Derived Exosomes in Maternal Circulation Across Gestation. Diabetes 2016, 65, 598–609. [Google Scholar] [CrossRef]
- Moro, L.; Bardají, A.; Macete, E.; Barrios, D.; Morales-Prieto, D.M.; España, C.; Mandomando, I.; Sigaúque, B.; Dobaño, C.; Markert, U.R.; et al. Placental Microparticles and MicroRNAs in Pregnant Women with Plasmodium falciparum or HIV Infection. PLoS ONE 2016, 11, e0146361. [Google Scholar] [CrossRef] [PubMed]
- Block, L.N.; Schmidt, J.K.; Keuler, N.S.; McKeon, M.C.; Bowman, B.D.; Wiepz, G.J.; Golos, T.G. Zika virus impacts extracellular vesicle composition and cellular gene expression in macaque early gestation trophoblasts. Sci. Rep. 2022, 12, 7348. [Google Scholar] [CrossRef] [PubMed]
- Tolosa, J.M.; Schjenken, J.E.; Clifton, V.L.; Vargas, A.; Barbeau, B.; Lowry, P.; Maiti, K.; Smith, R. The endogenous retroviral envelope protein syncytin-1 inhibits LPS/PHA-stimulated cytokine responses in human blood and is sorted into placental exosomes. Placenta 2012, 33, 933–941. [Google Scholar] [CrossRef] [PubMed]
- Mi, S.; Lee, X.; Li, X.; Veldman, G.M.; Finnerty, H.; Racie, L.; LaVallie, E.; Tang, X.Y.; Edouard, P.; Howes, S.; et al. Syncytin is a captive retroviral envelope protein involved in human placental morphogenesis. Nature 2000, 403, 785–789. [Google Scholar] [CrossRef]
- Galli, J.; Almiñana, C.; Wiesendanger, M.; Schuler, G.; Kowalewski, M.P.; Klisch, K. Bovine placental extracellular vesicles carry the fusogenic syncytin BERV-K1. Theriogenology 2024, 223, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Delorme-Axford, E.; Donker, R.B.; Mouillet, J.F.; Chu, T.; Bayer, A.; Ouyang, Y.; Wang, T.; Stolz, D.B.; Sarkar, S.N.; Morelli, A.E.; et al. Human placental trophoblasts confer viral resistance to recipient cells. Proc. Natl. Acad. Sci. USA 2013, 110, 12048–12053. [Google Scholar] [CrossRef]
- Bayer, A.; Lennemann, N.J.; Ouyang, Y.; Sadovsky, E.; Sheridan, M.A.; Roberts, R.M.; Coyne, C.B.; Sadovsky, Y. Chromosome 19 microRNAs exert antiviral activity independent from type III interferon signaling. Placenta 2018, 61, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, Y.; Bayer, A.; Chu, T.; Tyurin, V.A.; Kagan, V.E.; Morelli, A.E.; Coyne, C.B.; Sadovsky, Y. Isolation of human trophoblastic extracellular vesicles and characterization of their cargo and antiviral activity. Placenta 2016, 47, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, M.I.; Khalil, M.; Ben-Dov, I.Z.; Alverez-Perez, J.; Illsley, N.P.; Zamudio, S.; Al-Khan, A.; Loudig, O. Customizing EV-CATCHER to Purify Placental Extracellular Vesicles from Maternal Plasma to Detect Placental Pathologies. Int. J. Mol. Sci. 2024, 25, 5102. [Google Scholar] [CrossRef]
- Salomon, C.; Guanzon, D.; Scholz-Romero, K.; Longo, S.; Correa, P.; Illanes, S.E.; Rice, G.E. Placental Exosomes as Early Biomarker of Preeclampsia: Potential Role of Exosomal MicroRNAs Across Gestation. J. Clin. Endocrinol. Metab. 2017, 102, 3182–3194. [Google Scholar] [CrossRef]
- Levine, L.; Habertheuer, A.; Ram, C.; Korutla, L.; Schwartz, N.; Hu, R.W.; Reddy, S.; Freas, A.; Zielinski, P.D.; Harmon, J.; et al. Syncytiotrophoblast extracellular microvesicle profiles in maternal circulation for noninvasive diagnosis of preeclampsia. Sci. Rep. 2020, 10, 6398. [Google Scholar] [CrossRef] [PubMed]
- Gill, M.; Motta-Mejia, C.; Kandzija, N.; Cooke, W.; Zhang, W.; Cerdeira, A.S.; Bastie, C.; Redman, C.; Vatish, M. Placental Syncytiotrophoblast-Derived Extracellular Vesicles Carry Active NEP (Neprilysin) and Are Increased in Preeclampsia. Hypertension 2019, 73, 1112–1119. [Google Scholar] [CrossRef] [PubMed]
- Mazahir, F.; Yadav, A.K. Recent progress in engineered extracellular vesicles and their biomedical applications. Life Sci. 2024, 350, 122747. [Google Scholar] [CrossRef] [PubMed]
- Kugeratski, F.G.; McAndrews, K.M.; Kalluri, R. Multifunctional Applications of Engineered Extracellular Vesicles in the Treatment of Cancer. Endocrinology 2021, 162, bqaa250. [Google Scholar] [CrossRef] [PubMed]
- Loomes, R.; Hull, L.; Mandy, W.P.L. What Is the Male-to-Female Ratio in Autism Spectrum Disorder? A Systematic Review and Meta-Analysis. J. Am. Acad. Child. Adolesc. Psychiatry 2017, 56, 466–474. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, C.S. The placenta-brain-axis. J. Neurosci. Res. 2020, 99, 271–283. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, C.S. Placental serotonin signaling, pregnancy outcomes, and regulation of fetal brain developmentdagger. Biol. Reprod. 2020, 102, 532–538. [Google Scholar] [CrossRef]
- Carter, A.M. Evolution of Placental Hormones: Implications for Animal Models. Front. Endocrinol. (Lausanne) 2022, 13, 891927. [Google Scholar] [CrossRef]
- Leaman, D.W.; Roberts, R.M. Genes for the trophoblast interferons in sheep, goat, and musk ox and distribution of related genes among mammals. J. Interferon Res. 1992, 12, 1–11. [Google Scholar] [CrossRef]
- Roberts, R.M. Conceptus interferons and maternal recognition of pregnancy. Biol. Reprod. 1989, 40, 449–452. [Google Scholar] [CrossRef]
- Roberts, R.M. Interferon-tau, a Type 1 interferon involved in maternal recognition of pregnancy. Cytokine Growth Factor Rev. 2007, 18, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Roberts, R.M. 30 years on from the molecular cloning of interferon-tau. Reproduction 2017, 154, E1–E2. [Google Scholar] [CrossRef] [PubMed]
- Roberts, R.M.; Chen, Y.; Ezashi, T.; Walker, A.M. Interferons and the maternal-conceptus dialog in mammals. Semin. Cell Dev. Biol. 2008, 19, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Chubakov, A.R.; Gromova, E.A.; Konovalov, G.V.; Sarkisova, E.F.; Chumasov, E.I. The effects of serotonin on the morpho-functional development of rat cerebral neocortex in tissue culture. Brain Res. 1986, 369, 285–297. [Google Scholar] [CrossRef] [PubMed]
- Chumasov, E.I.; Chubakov, A.R.; Konovalov, G.V.; Gromova, E.A. Effect of serotonin on growth and differentiation of hippocampal cells in culture. Neurosci. Behav. Physiol. 1980, 10, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Gromova, H.A.; Chubakov, A.R.; Chumasov, E.I.; Konovalov, H.V. Serotonin as a stimulator of hippocampal cell differentiation in tissue culture. Int. J. Dev. Neurosci. 1983, 1, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Koren, Z.; Pfeifer, Y.; Sulman, F.G. Serotonin Content of Human Placenta and Fetus during Pregnancy. Am. J. Obstet. Gynecol. 1965, 93, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Laurent, L.; Deroy, K.; St-Pierre, J.; Côté, F.; Sanderson, J.T.; Vaillancourt, C. Human placenta expresses both peripheral and neuronal isoform of tryptophan hydroxylase. Biochimie 2017, 140, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Kliman, H.J.; Quaratella, S.B.; Setaro, A.C.; Siegman, E.C.; Subha, Z.T.; Tal, R.; Milano, K.M.; Steck, T.L. Pathway of Maternal Serotonin to the Human Embryo and Fetus. Endocrinology 2018, 159, 1609–1629. [Google Scholar] [CrossRef] [PubMed]
- Vaillancourt, C.; Petit, A.; Gallo-Payet, N.; Bellabarba, D.; Lehoux, J.G.; Belisle, S. Labelling of D2-dopaminergic and 5-HT2-serotonergic binding sites inhuman trophoblastic cells using [3H]-spiperone. J. Recept. Res. 1994, 14, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Salomon, C.; Torres, M.J.; Kobayashi, M.; Scholz-Romero, K.; Sobrevia, L.; Dobierzewska, A.; Illanes, S.E.; Mitchell, M.D.; Rice, G.E. Agestational profile ofplacental exosomes inmaternal plasma andtheir effects on endothelial cellmigration. PLoS ONE 2014, 9, e98667. [Google Scholar] [CrossRef]
- Huang, W.Q.; Zhang, C.L.; Di, X.Y.; Zhang, R.Q. Studies on the localization of 5-hydroxytryptamine and its receptors in human placenta. Placenta 1998, 19, 655–661. [Google Scholar] [CrossRef] [PubMed]
- Viau, M.; Lafond, J.; Vaillancourt, C. Expression of placental serotonin transporter and 5-HT 2A receptor in normal and gestational diabetes mellitus pregnancies. Reprod. Biomed. Online 2009, 19, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Hadden, C.; Fahmi, T.; Cooper, A.; Savenka, A.V.; Lupashin, V.V.; Roberts, D.J.; Maroteaux, L.; Hauguel-de Mouzon, S.; Kilic, F. Serotonin transporter protects the placental cells against apoptosis in caspase 3-independent pathway. J. Cell. Physiol. 2017, 232, 3520–3529. [Google Scholar] [CrossRef]
- Wu, H.H.; Choi, S.; Levitt, P. Differential patterning of genes involved in serotonin metabolism and transport in extra-embryonic tissues of the mouse. Placenta 2016, 42, 74–83. [Google Scholar] [CrossRef]
- Yavarone, M.S.; Shuey, D.L.; Sadler, T.W.; Lauder, J.M. Serotonin uptake in the ectoplacental cone and placenta of the mouse. Placenta 1993, 14, 149–161. [Google Scholar] [CrossRef]
- Bonnin, A.; Goeden, N.; Chen, K.; Wilson, M.L.; King, J.; Shih, J.C.; Blakely, R.D.; Deneris, E.S.; Levitt, P. A transient placental source of serotonin for the fetal forebrain. Nature 2011, 472, 347–350. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Wu, M.; Huang, H.; Tao, H.; Zou, L.; Luo, Q. Plasma Exosomal miR-199a-5p Derived from Preeclampsia with Severe Features Impairs Endothelial Cell Function via Targeting SIRT1. Reprod. Sci. 2022, 29, 3413–3424. [Google Scholar] [CrossRef]
- Li, L.; Li, X.; Zhu, Y.; Li, L.; Wu, Y.; Ying, J.; Li, Y.; Chen, J. Human Trophoblast Cell-Derived Extracellular Vesicles Facilitate Preeclampsia by Transmitting miR-1273d, miR-4492, and miR-4417 to Target HLA-G. Reprod. Sci. 2022, 29, 2685–2696. [Google Scholar] [CrossRef]
- Zou, G.; Ji, Q.; Geng, Z.; Du, X.; Jiang, L.; Liu, T. miR-31-5p from placental and peripheral blood exosomes is a potential biomarker to diagnose preeclampsia. Hereditas 2022, 159, 35. [Google Scholar] [CrossRef]
- Fudono, A.; Imai, C.; Takimoto, H.; Tarui, I.; Aoyama, T.; Yago, S.; Okamitsu, M.; Muramatsu, M.; Sato, N.; Miyasaka, N. Trimester-specific associations between extracellular vesicle microRNAs and fetal growth. J. Matern. Fetal Neonatal Med. 2022, 35, 8728–8734. [Google Scholar] [CrossRef] [PubMed]
- Santos, H.P., Jr.; Bhattacharya, A.; Joseph, R.M.; Smeester, L.; Kuban, K.C.K.; Marsit, C.J.; O‘Shea, T.M.; Fry, R.C. Evidence for the placenta-brain axis: Multi-omic kernel aggregation predicts intellectual and social impairment in children born extremely preterm. Mol. Autism 2020, 11, 97. [Google Scholar] [CrossRef] [PubMed]
- Cote, F.; Fligny, C.; Bayard, E.; Launay, J.M.; Gershon, M.D.; Mallet, J.; Vodjdani, G. Maternal serotonin is crucial for murine embryonic development. Proc. Natl. Acad. Sci. USA 2007, 104, 329–334. [Google Scholar] [CrossRef]
- Bonnin, A.; Levitt, P. Fetal, maternal, and placental sources of serotonin and new implications for developmental programming of the brain. Neuroscience 2011, 197, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Tuteja, G.; Chung, T.; Bejerano, G. Changes in the enhancer landscape during early placental development uncover a trophoblast invasion gene-enhancer network. Placenta 2016, 37, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Muller, C.L.; Anacker, A.M.; Rogers, T.D.; Goeden, N.; Keller, E.H.; Forsberg, C.G.; Kerr, T.M.; Wender, C.; Anderson, G.M.; Stanwood, G.D.; et al. Impact of Maternal Serotonin Transporter Genotype on Placental Serotonin, Fetal Forebrain Serotonin, and Neurodevelopment. Neuropsychopharmacology 2017, 42, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.; Jain, A.; Denslow, N.D.; Nouri, M.Z.; Chen, S.; Wang, T.; Zhu, N.; Koh, J.; Sarma, S.J.; Sumner, B.W.; et al. Bisphenol A and bisphenol S disruptions of the mouse placenta and potential effects on the placenta-brain axis. Proc. Natl. Acad. Sci. USA 2020, 117, 4642–4652. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.; Kinkade, J.A.; Bivens, N.J.; Rosenfeld, C.S. miRNA changes in the mouse placenta due to bisphenol A exposure. Epigenomics 2021, 13, 1909–1919. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Tuteja, G. TissueEnrich: Tissue-specific gene enrichment analysis. Bioinformatics 2019, 35, 1966–1967. [Google Scholar] [CrossRef]
- Shen, Y.; Yue, F.; McCleary, D.F.; Ye, Z.; Edsall, L.; Kuan, S.; Wagner, U.; Dixon, J.; Lee, L.; Lobanenkov, V.V.; et al. A map of the cis-regulatory sequences in the mouse genome. Nature 2012, 488, 116–120. [Google Scholar] [CrossRef]
- Jasarevic, E.; Sieli, P.T.; Twellman, E.E.; Welsh, T.H., Jr.; Schachtman, T.R.; Roberts, R.M.; Geary, D.C.; Rosenfeld, C.S. Disruption of adult expression of sexually selected traits by developmental exposure to bisphenol A. Proc. Natl. Acad. Sci. USA 2011, 108, 11715–11720. [Google Scholar] [CrossRef] [PubMed]
- Jasarevic, E.; Williams, S.A.; Vandas, G.M.; Ellersieck, M.R.; Liao, C.; Kannan, K.; Roberts, R.M.; Geary, D.C.; Rosenfeld, C.S. Sex and dose-dependent effects of developmental exposure to bisphenol A on anxiety and spatial learning in deer mice (Peromyscus maniculatus bairdii) offspring. Horm. Behav. 2013, 63, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.A.; Jasarevic, E.; Vandas, G.M.; Warzak, D.A.; Geary, D.C.; Ellersieck, M.R.; Roberts, R.M.; Rosenfeld, C.S. Effects of developmental bisphenol A exposure on reproductive-related behaviors in California mice (Peromyscus californicus): A monogamous animal model. PLoS ONE 2013, 8, e55698. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.A.; Javurek, A.B.; Painter, M.S.; Ellersieck, M.R.; Welsh, T.H., Jr.; Camacho, L.; Lewis, S.M.; Vanlandingham, M.M.; Ferguson, S.A.; Rosenfeld, C.S. Effects of developmental exposure to bisphenol A on spatial navigational learning and memory in rats: A CLARITY-BPA study. Horm. Behav. 2016, 80, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Strawn, M.; Samal, A.; Sarker, M.B.; Dhakal, P.; Behura, S.K. Relevance of microRNAs to the regulation of the brain-placental axis in mice. Placenta 2021, 112, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Mashouri, L.; Yousefi, H.; Aref, A.R.; Ahadi, A.m.; Molaei, F.; Alahari, S.K. Exosomes: Composition, biogenesis, and mechanisms in cancer metastasis and drug resistance. Mol. Cancer 2019, 18, 75. [Google Scholar] [CrossRef] [PubMed]
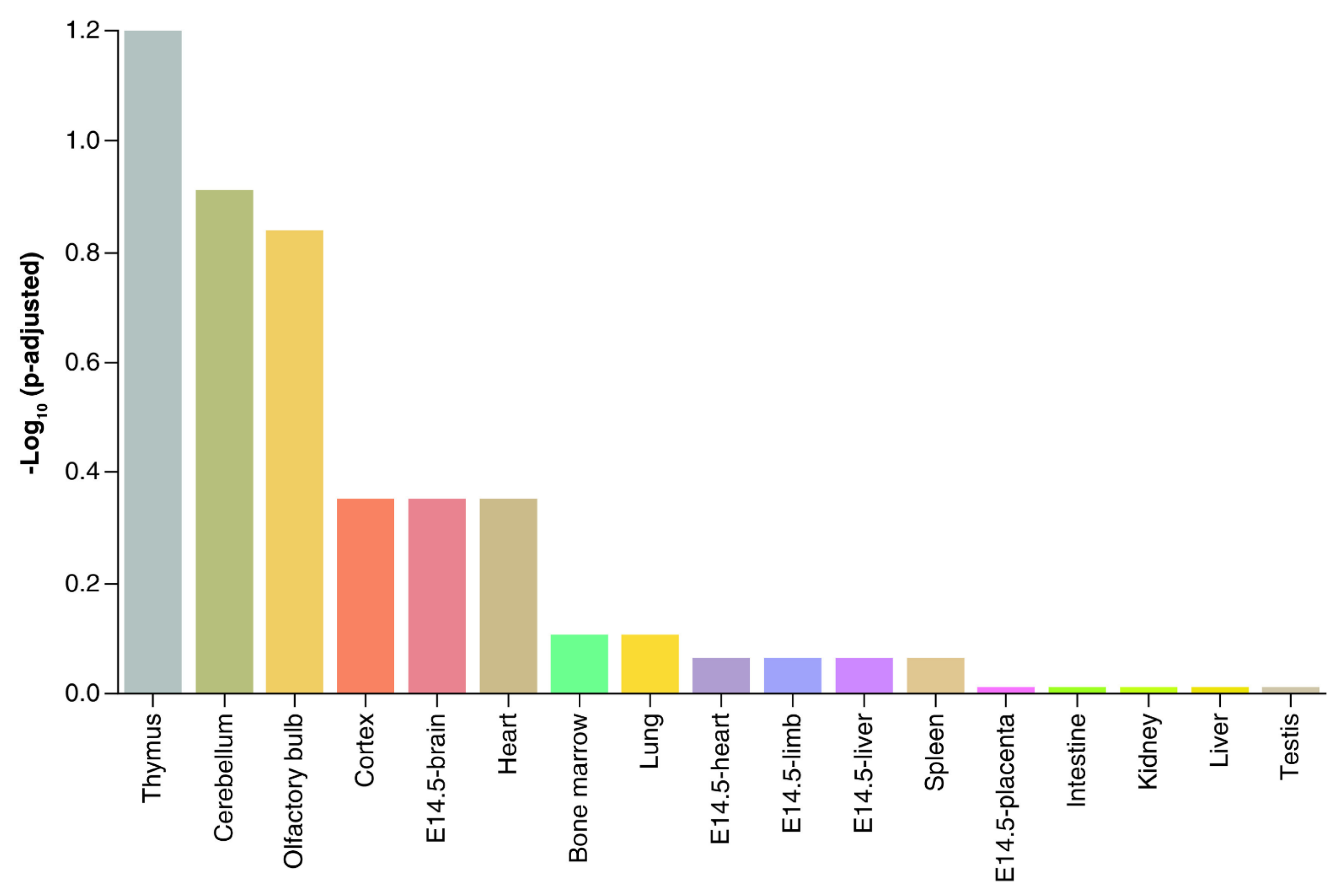
- Kinkade, J.A.; Seetharam, A.S.; Sachdev, S.; Bivens, N.J.; Phinney, B.S.; Grigorean, G.; Roberts, R.M.; Tuteja, G.; Rosenfeld, C.S. Extracellular vesicles from mouse trophoblast cells: Effects on neural progenitor cells and potential participants in the placenta-brain axis†. Biol. Reprod. 2024, 110, 310–328. [Google Scholar] [CrossRef]
- Ayala-Ramírez, P.; Machuca-Acevedo, C.; Gámez, T.; Quijano, S.; Barreto, A.; Silva, J.L.; Olaya, C.M.; García-Robles, R. Assessment of Placental Extracellular Vesicles-Associated Fas Ligand and TNF-Related Apoptosis-Inducing Ligand in Pregnancies Complicated by Early and Late Onset Preeclampsia. Front. Physiol. 2021, 12, 708824. [Google Scholar] [CrossRef]
- Buca, D.; Bologna, G.; D’Amico, A.; Cugini, S.; Musca, F.; Febbo, M.; D’Arcangelo, D.; Buca, D.; Simeone, P.; Liberati, M.; et al. Extracellular Vesicles in Feto-Maternal Crosstalk and Pregnancy Disorders. Int. J. Mol. Sci. 2020, 21, 2120. [Google Scholar] [CrossRef]
- Czernek, L.; Düchler, M. Exosomes as Messengers Between Mother and Fetus in Pregnancy. Int. J. Mol. Sci. 2020, 21, 4264. [Google Scholar] [CrossRef]
- Gebara, N.; Correia, Y.; Wang, K.; Bussolati, B. Angiogenic Properties of Placenta-Derived Extracellular Vesicles in Normal Pregnancy and in Preeclampsia. Int. J. Mol. Sci. 2021, 22, 5402. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, A.; Sugiura, K.; Hoshino, A. Impact of exosome-mediated feto-maternal interactions on pregnancy maintenance and development of obstetric complications. J. Biochem. 2021, 169, 163–171. [Google Scholar] [CrossRef] [PubMed]
- James-Allan, L.B.; Devaskar, S.U. Extracellular vesicles and their role in gestational diabetes mellitus. Placenta 2021, 113, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Kupper, N.; Huppertz, B. The endogenous exposome of the pregnant mother: Placental extracellular vesicles and their effect on the maternal system. Mol. Asp. Med. 2021, 87, 100955. [Google Scholar] [CrossRef] [PubMed]
- Morales-Prieto, D.M.; Favaro, R.R.; Markert, U.R. Placental miRNAs in feto-maternal communication mediated by extracellular vesicles. Placenta 2020, 102, 27–33. [Google Scholar] [CrossRef]
- Nair, S.; Guanzon, D.; Jayabalan, N.; Lai, A.; Scholz-Romero, K.; Kalita de Croft, P.; Ormazabal, V.; Palma, C.; Diaz, E.; McCarthy, E.A.; et al. Extracellular vesicle-associated miRNAs are an adaptive response to gestational diabetes mellitus. J. Transl. Med. 2021, 19, 360. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.; Salomon, C. Extracellular vesicles as critical mediators of maternal-fetal communication during pregnancy and their potential role in maternal metabolism. Placenta 2020, 98, 60–68. [Google Scholar] [CrossRef]
- Palma, C.; Jellins, J.; Lai, A.; Salas, A.; Campos, A.; Sharma, S.; Duncombe, G.; Hyett, J.; Salomon, C. Extracellular Vesicles and Preeclampsia: Current Knowledge and Future Research Directions. Subcell. Biochem. 2021, 97, 455–482. [Google Scholar] [CrossRef]
- Rajaratnam, N.; Ditlevsen, N.E.; Sloth, J.K.; Bæk, R.; Jørgensen, M.M.; Christiansen, O.B. Extracellular Vesicles: An Important Biomarker in Recurrent Pregnancy Loss? J. Clin. Med. 2021, 10, 2549. [Google Scholar] [CrossRef]
- Tang, Y.; Groom, K.; Chamley, L.; Chen, Q. Melatonin, a Potential Therapeutic Agent for Preeclampsia, Reduces the Extrusion of Toxic Extracellular Vesicles from Preeclamptic Placentae. Cells 2021, 10, 1904. [Google Scholar] [CrossRef]
- Tersigni, C.; Lucchetti, D.; Franco, R.; Colella, F.; Neri, C.; Crispino, L.; Sgambato, A.; Lanzone, A.; Scambia, G.; Vatish, M.; et al. Circulating Placental Vesicles Carry HLA-DR in Pre-Eclampsia: A New Potential Marker of the Syndrome. Front. Immunol. 2021, 12, 717879. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhang, W.; Zou, N.; Zhang, L. Trophoblasts Modulate the Ca(2+) Oscillation and Contraction of Myometrial Smooth Muscle Cells by Small Extracellular Vesicle- (sEV-) Mediated Exporting of miR-25-3p during Premature Labor. Oxid. Med. Cell Longev. 2021, 2021, 8140667. [Google Scholar] [CrossRef] [PubMed]
- Block, L.N.; Bowman, B.D.; Schmidt, J.K.; Keding, L.T.; Stanic, A.K.; Golos, T.G. The promise of placental extracellular vesicles: Models and challenges for diagnosing placental dysfunction in utero†. Biol. Reprod. 2021, 104, 27–57. [Google Scholar] [CrossRef]
- Pethe, P.; Kale, V. Placenta: A gold mine for translational research and regenerative medicine. Reprod. Biol. 2021, 21, 100508. [Google Scholar] [CrossRef]
- Villalobos-Labra, R.; Liu, R.; Spaans, F.; Sáez, T.; Quon, A.; Wong, M.; Pink, D.; Lewis, J.; Vatish, M.; Davidge, S.T.; et al. Placenta-derived extracellular vesicles from preeclamptic and healthy pregnancies impair ex vivo vascular endothelial function. Biosci. Rep. 2022, 42, BSR20222185. [Google Scholar] [CrossRef] [PubMed]
- Murugesan, S.; Hussey, H.; Saravanakumar, L.; Sinkey, R.G.; Sturdivant, A.B.; Powell, M.F.; Berkowitz, D.E. Extracellular Vesicles From Women with Severe Preeclampsia Impair Vascular Endothelial Function. Anesth. Analg. 2022, 134, 713–723. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosenfeld, C.S. Placenta Extracellular Vesicles: Messengers Connecting Maternal and Fetal Systems. Biomolecules 2024, 14, 995. https://doi.org/10.3390/biom14080995
Rosenfeld CS. Placenta Extracellular Vesicles: Messengers Connecting Maternal and Fetal Systems. Biomolecules. 2024; 14(8):995. https://doi.org/10.3390/biom14080995
Chicago/Turabian StyleRosenfeld, Cheryl S. 2024. "Placenta Extracellular Vesicles: Messengers Connecting Maternal and Fetal Systems" Biomolecules 14, no. 8: 995. https://doi.org/10.3390/biom14080995




