Poorly Investigated Ecuadorian Medicinal Plants
Abstract
:1. Introduction
2. Research Strategies and Literature Sources
3. Ethnobotanical and Ethnopharmacological Data
| No. | Botanical Name | Vernacular Name | Phytochemical and Pharmacological Data b | Used Part(s) of the Plant | Traditional Uses |
|---|---|---|---|---|---|
| ACANTHACEAE | |||||
| 1 | Justicia pectoralis Jacq. | Saucillo, tigrecillo | No information is reported in literature. | Branches | It is used orally to treat general disorders of nervous and dermatological systems, and culture-related syndromes [4,16,20,21,22]. |
| AMARANTHACEAE | |||||
| 2 | Alternanthera porrigens (Jacq.) Kunze | Moradilla | No information is reported in literature. | Branches, flowers | It is used orally and in baths to treat general disorders of the gynecological system [20,21]. |
| 3 | Amaranthus caudatus L. | Amaranto, ataco morado | No information is reported in literature. | Inflorescences | It is used orally and in baths to treat disorders of the circulatory, gynecological, and respiratory systems [20,21]. |
| 4 | Amaranthus cruentus L. | Ataco, sangorache | No information is reported in literature. | Inflorescences, leaves | Anti-inflammatory, astringent, anti-flu, antihemorrhagic, diuretic and tonic, carminative, emmenagogue, hepatic, stimulant, to enhance blood circulation, and to treat abdominal pain related to menstruation [4,16,20]. |
| 5 | Amaranthus hybridus L. | Bledo, ataco | No information is reported in literature. | Inflorescences | It is used orally to treat general disorders of the circulatory, gynecological, respiratory, and urinary systems [21]. |
| 6 | Amaranthus quitensis Kunth | Ataco | No information is reported in literature. | Leaves, roots | Pain relief (at joints, head, throat), and to treat gastrointestinal and respiratory problems [18]. |
| 7 | Iresine diffusa Humb. & Bonp. Ex Willd | Tigrecillo, velo de novia, chulco, escancel | No information is reported in literature. | Branches | In topical applications, oral poultices, and washings to heal disorders of the dermatological, digestive, gynecological, urinary, nervous, and respiratory systems [21]. |
| 8 | Iresine herbstii Hook. | Escancel, lancetilla, tigrecillo | The isoflavanone 2′,2,5-trimethoxy-6,7-methylenedioxyisoflavanone, together with the isoflavone tlatlancuayin (2′,5-dimethoxy-6,7-methylenedioxyisoflavone) were isolated from the aerial parts [27]. | Leaves, stalks, whole plant, stems, branches | Anti-inflammatory, anti-flu, analgesic, diuretic, sedative, and tonic. To treat intestinal, uterus, and vaginal infections, injuries, liver and kidney problems, general disorders of the gynecological, nervous, urinary, respiratory, dermatological, and digestive systems, mal aire (bad air) d, and culture-related syndromes [4,16,20,21,22]. |
| 9 | Marchantia polymorpha L. | Sapo yuyu | No information is reported in literature. | Whole plant | To heal body malaise [4]. |
| APIACEAE | |||||
| 10 | Arracacia xanthorrhiza Bancr. c | Zanahoria blanca | This species is well known as food. | Leaves | To eliminate the cattle placenta [4]. |
| 11 | Eryngium foetidum L. | Culantro extranjero | Phytochemical analysis of the leaves indicated the presence of flavonoids, tannins, a saponin and several triterpenoids, as well as the absence of alkaloids. A significant constituent of the EO of the plant is (E)-2-dodecenal (“eryngial”), accompanied by minor amounts of trimethylbenzaldehyde isomers. Pharmacological studies of the aerial parts have demonstrated anthelmintic activity due to eryngial, anti-inflammatory action due to the phytosterol fractions, anti-convulsant activity, and selective antibacterial activity against Salmonella and Erwinia species [28]. | Whole plant | It is used to treat stomach pain [22]. |
| APOCYNACEAE | |||||
| 12 | Lacmellea spaciosa Woodson | Chicle | No information is reported in literature. | Fruits | Huaorani eat fruits. The latex from the trunk is used to clean teeth and as chewing gum [19]. |
| 13 | Marsdenia condurango Rchb. f | Condurango | Pregnane glycosides isolated from the bark of M. cundurango were evaluated for their cytotoxic activity against human HL-60 leukemia cells, A549 lung adenocarcinoma cells, and TIG-3 normal lung cells. Moreover, a representative pregnane glycoside induced apoptosis in HL-60 cells [29]. | Bark | It is used orally to treat general disorders of the digestive system [21]. |
| ARECACEAE | |||||
| 14 | Ceroxylon parvifrons (Engel) H. Wendl. | Palma de ramos | No information is reported in literature. | Leaves | The aerial parts are used as incense [4]. |
| ASCLEPIADACEAE | |||||
| 15 | Orthosia ellemannii (Morillo) Liede & Meve | Cola de caballo | No information is reported in literature. | Branches | It is used orally to treat general disorders of the urinary system [21]. |
| ASTERACEAE | |||||
| 16 | Aequatorium jamesonii (S.F. Blake) C. Jeffrey | Guangalo | No information is reported in literature. | Branches | Branches are rubbed to treat culture-related syndromes [21]. |
| 17 | Achyrocline hallii Hieron | Sacha algodón, lechugilla | No information is reported in literature. | Leaves, whole plant | To treat disorders of the digestive system and injuries [4,21]. |
| 18 | Ambrosia arborescens Mill. | Marco, altamiso | Sotillo et al. investigated the anticancer activity of sesquiterpene lactones isolated from the plant and a few synthetic derivatives against breast cancer cell lines, especially against cancer stem cells (CSCs) [30]. | Leaves, branches | Pain relief (joints, head, throat), and to treat gastrointestinal, respiratory, and muscular problems. Topical applications and rubbings are also used to treat disorders of the dermatological system and culture-related syndromes [18,21]. |
| 19 | Ambrosia artemisioides Meyen & Walpers ex Meyen | Marco | Compounds derived from allantolactone, as well as epieudesmane and oplopanone sesquiterpenes have been isolated from samples of A. artemisioides collected in the Tacna region of southern Peru [31]. | Branches | To cure the fever or the cold caused by cold air or strong winds (locally known as mal aire in Spanish) d [4]. |
| 20 | Aristeguietia persicifolia (Kunth) R.M. King & H. Rob | Ishpingo, monte de culebra | No information is reported in literature. | Branches | Branches are rubbed to treat culture-related syndromes [21]. |
| 21 | Artemisia sodiroi Hieron | Ajenjo, alcanfor | A specimen collected in Ecuador gave a volatile fraction which contained sabinyl acetate (65.8%) as the main constituent [32]. | Branches | Branches are rubbed to treat culture-related syndromes [21]. and gargles are used to heal disorders of the respiratory system [21]. |
| 22 | Baccharis oblongifolia (Ruiz & Pav.) Pers. | Chilca | The flavonoids oblongifoliosides A and B have been isolated from the leaves [33]. | Branches | To cure a restless and confused child, and in postpartum baths [4]. |
| 23 | Baccharis latifolia (Ruiz & Pav.) Pers. | Chilca larga | A specimen collected in Ecuador afforded an essential oil, whose main components were limonene (33.72%), β-phellandrene (10.32%), sabinene (10.28%), β-pinene (6.99%), and α-pinene (5.44%). The essential oil exhibited moderate activity against Trichophyton rubrum (ATCC 28188) and Trichophyton mentagrophytes (ATCC 28185) [34]. | Leaves, stalks | Pain relief (joints, head, throat) and to treat gastrointestinal, skin (inflammation, bruises), renal-urological, and neurological problems. Rubbings are used to treat culture-related syndromes [18,22]. |
| 24 | Bidens andicola Kunth. | Ñachic, nachag | A new glycosyl chalcone ester, together with 7-O-glycosyl derivatives of flavonoids quercetin and quercetin 3-O-methyl ether have been isolated from the aerial parts. The sugar chains contained three or four sugar units, including β-D-glucopyranose, α-L-rhamnopyranose, and β-D-xylopyranose [35]. | Whole plant, leaves | To decrease disease relapses after recovery (locally known as recaída in Spanish) and pain relief (joints, head, throat) [4,18]. |
| 25 | Bidens pilosa L. | Pacunga, amor seco, huichingue | The isolation of sterols, terpenoids, phenylpropanoids and hydrocarbons were reported [36]. | Whole plant, flowers | To decrease disease relapses after recovery (locally known as recaída), pain relief (at joints, head, throat), and as an anti-inflammatory [4,16]. |
| 26 | Bidens triplinervia Kunth | Ñachig | No information is reported in literature. | Whole plant without roots | It is used orally to treat disorders of the gynecological system [21]. |
| 27 | Diplostephium oblanceolatum S. F. Blake | Chuquiragua | No information is reported in literature. | Leaves | To heal body malaise [4]. |
| 28 | Gamochaeta americana (Mill.) Wedd. | Rabo de danta, lechuguilla, lancetilla | No information is reported in literature. | Whole plant | To cure the cold [4]. |
| 29 | Loricaria thuyoides (Lam.) Sch. Bip. | Ushcu chaqui, pata de gallinazo, trensilla | No information is reported in literature. | Branches | To cure a restless and confused child and used as a tonic and in energy baths [4]. |
| 30 | Oritrophium peruvianum (Lam.) Cuatrec. | Uña kushma | No information is reported in literature. | Whole plant | To heal liver and kidney inflammations [4]. |
| 31 | Vernonanthura patens (Kunth) H. Rob. | Jujumba | Lupeol was identified in the callus extract [37]. | Leaves | It is used orally to treat disorders of the dermatological system [22]. |
| BASELLACEAE | |||||
| 32 | Anredera ramosa (Moq.) Eliasson. | Lutuyuyu | No information is reported in literature. | Whole plant | In baths for children, and to cure fever and headache [4]. |
| BEGONIACEAE | |||||
| 33 | Begonia x tuberhybrida Voss | Begonia rosada | No information is reported in literature. | Flowers, petals | To treat constipation [16]., and used as a sedative and tonic [20]. |
| BETULACEAE | |||||
| 34 | Alnus acuminata Kunth | Aliso | No information is reported in literature. | Leaves, buds | To cure headaches, and to treat bone fractures, sprains, and dislocations [4]. |
| BRASSICACEAE | |||||
| 35 | Cardamine bonariensis Pers. | Berro | No information is reported in literature. | Whole plant | It is used orally to cure disorders of the circulatory system [21]. |
| 36 | Lepidium chichicara Desv. | Chichira negra | No information is reported in literature. | Whole plant | To decrease disease relapses after recovery (locally known as recaída in Spanish), to cure the fever or the cold caused by cold air or strong winds (locally known as mal aire (bad air) d [4]. |
| 37 | Lepidium thurberi Wooton | Chichira | No information is reported in literature. | Plant without roots | It is used orally to treat gynecological disorders [21]. |
| BROMELIACEAE | |||||
| 38 | Tillandsia straminea Kunth | Flor de cristo, clavel del aire | No information is reported in literature. | Flowers | It is used to treat neurological disorders [21]. |
| CACTACEAE | |||||
| 39 | Cumulopuntia corotilla (K.Schum. ex Vaupel) E.F.Anderson | Corotilla | No information is reported in literature. | Whole plant | Pain relief (joints, head, throat), and to treat skin (inflammation, bruises) and neurological problems [18]. |
| CAMPANULACEAE | |||||
| 40 | Siphocampylus scandens (Kunth) G. Don | Pena roja de monte | No information is reported in literature. | Flowers | To treat neurological problems [4]. |
| CANNACEAE | |||||
| 41 | Canna indica L. | Achira | The phytochemical analysis showed the presence of alkaloids, carbohydrates, proteins, flavonoids, terpenoids, cardiac glycosides, oils, steroids, tannins, saponins, anthocyanin pigments, phlobatinins, and other chemical compounds. The pharmacological studies showed that this plant exerted antibacterial, antiviral, anthelmintic, molluscicidal, anti-inflammatory, analgesic immunomodulatory, antioxidant, cytotoxic, hemostatic, hepatoprotective, anti-diarrheal, and other effects [38]. | Leaves | It is used to treat general neurological and respiratory problems [21,22]. |
| 42 | Canna coccinea Mill. | Platanillo | No information is reported in literature. | Leaves, flowers | Pain relief (joints, head, throat) [18]. |
| CAPPARACEAE | |||||
| 43 | Cleome longifolia C. Presl. | Sacha yuca | No information is reported in literature. | Leaves | Antirheumatic [4]. |
| CARICACEAE | |||||
| 44 | Carica pubescens Lenn’e & C. Koch c | Chihualcán, chamburo | Ethyl 3-O-β-D-glucopyranosyloxybutanoate, butyl 3-O-β-D-glucopyranosyloxybutanoate, and 3-oxo-octyl 1-O-β-D-glucopyranoside were isolated from fruit pulp by liquid chromatography on XAD [39]. | Fruits, leaves | To cure nerves, diarrhea, and dislocations [4]. |
| COMBRETACEAE | |||||
| 45 | Conocarpus erectus L. | Botoncillo | The extracts of leaves, shoot, bark, and fruit showed high antibacterial, antioxidant, and hepta-protective activities due to phenolic content. Tannins and flavonoids were the main constituents. Tannins exhibited high antibacterial activity [40]. | Flowers | Pain relief (joints, head, throat) [18]. |
| COMMELINACEAE | |||||
| 46 | Callisia gracilis (Kunth) R. D. Hunt | Cachorillo, cachurillo, calcec, calcha verde, calsug | No information is reported in literature. | Leaves | To cure general gynecological disorders [21,22]. |
| 47 | Callisia repens (Jacq.) L. | Calsi, calcha, calcec pequeño | No information is reported in literature. | Leaves | To prevent postpartum relapse [4,21]. |
| CLUSIACEAE | |||||
| 48 | Vismia baccifera (L.) Triana & Planch. | Achotillo, sangre de gallina, ushca | Triprenylated anthranoids ferruginins A and B, together with ferruantrone and harunganin, were isolated from the taxon V. baccifera var. ferruginea [41]. | Leaves | To treat skin conditions and fainting spells [19]. |
| CUCURBITACEAE | |||||
| 49 | Cyclanthera pedata (L.) Schrad. c | Achoccha, achogcha, caigua | From a methanolic extract of the fruits flavonoid glycosides were separated by HPLC and identified [42]. | Fruits | To cure earache and to decrease disease relapses after recovery (locally known as recaída in Spanish) [4]. |
| EQUISETACEAE | |||||
| 50 | Equisetum bogotense Kunth. | Cola de caballo, caballo chupa | No information is reported in literature. | Leaves, stalks, whole plant | Anti-inflammatory, antiseptic, depurative, diuretic, hepatic, febrifuge, anticancer, anticough, anti-parasite, and to cure kidney problems and liver inflammation [4,16,20,21]. |
| 51 | Equisetum giganteum L. | Chupa caballo, cola de caballo | Caffeic acid derivatives, flavonoids, and styrilpyrones were identified. The most abundant glycosylated flavonoids were kaempferol derivatives [43]. | Leaves, stalks | Pain relief (joints, head, throat), anti-inflammatory, and to treat gastrointestinal, respiratory, skin (inflammation, bruises), and renal-urological problems [9,21]. |
| ERICACEAE | |||||
| 52 | Bejaria aestuans L. | Payana, payamo, payamo | No information is reported in literature. | Flowers | To treat abdominal pain related to menstruation [4,21]. |
| 53 | Bejaria subsessilis Benth. | Pena de cerro, joyapa | No information is reported in literature. | Flowers | To treat neurological problems [4]. |
| 54 | Cavendishia bracteata (Ruiz & Pav. ex J. St.-Hil.) Hoerold | Joyapa, salapa | No information is reported in literature. | Fruits | Feed [4]. |
| 55 | Disterigma alaternoides (Kunth) Nied. | Perlillas o joyapilla | No information is reported in literature. | Fruits | To treat physical exhaustion [4]. |
| 56 | Gaultheria erecta Vent. | Monte blanco | No information is reported in literature. | Fruits | To treat physical exhaustion [4]. |
| 57 | Macleania rupestris (Kunth) A. C. Sm. | Joyapa, salapa verde | No information is reported in literature. | Fruits | Antidiarrheal and to treat general physical malaise [4]. |
| ERIOCAULACEAE | |||||
| 58 | Paepalanthus ensifolius (Kunth) Kunth. | Cucharillo | No information is reported in literature. | Leaves | To cure nerves [4]. |
| 59 | Eriocaulon microcephalum Kunth | Monte de seguro | No information is reported in literature. | Whole plant | To wish good luck [4]. |
| EUPHORBIACEAE | |||||
| 60 | Cnidoscolus aconitifolius (Mill.) I.M. Johnst | Chaya | Kaempferol, quercetin, and myricetin were the most abundant phenolic compounds found in an extract [44]. | Leaves | To treat general digestive and circulatory problems [21]. |
| 61 | Sapium glandulosum (L.) Morong | Caucho | LC-MS analysis of the latex revealed the presence of tigliane-type diterpenoids, especially 12-deoxyphorbol esters. Considering that 12-deoxytigliane diterpenes are described as antitumor and antiviral agents, these results indicated that this plant has pharmacological potential [45]. | Leaves | An infusion of burnt leaves is used to remove pimples from the skin. The leaves are used to cure fainting [19]. |
| FABACEAE | |||||
| 62 | Acacia macracantha Humb. & Bonpl. ex Willd. | Uña de gato | The sugars identified in gum exudates of eight specimens of A. macracantha collected in Venezuela were galactose, arabinose, glucuronic acid, 4-O-methylglucuronic acid, and rhamnose [46]. | Leaves, flowers | Pain relief (joints, head, throat), anti-inflammatory, and to treat gastrointestinal, skin (inflammation, bruises), and renal-urological problems [18]. |
| 63 | Amicia glandulosa Kunth | Nona, urusus, orozús | No information is reported in literature. | Flowers | To treat respiratory disorders [21]. |
| 64 | Desmodium molliculum (Kunth) DC. | San Antonio, hierba de san Antonio, hierba del ángel | No information is reported in literature. | Plant without roots | To treat gynecological disorders [21]. |
| 65 | Myroxylon balsamum (L) Harms | Chaquino | (±)-7-Hydroxy-4′-methoxyisoflavanone, (±)-7,3′-dihydroxy-4′-methoxyisoflavanone, and 2-(2′,4′-dihydroxyphenyl)-5,6-dimethoxybenzofuran were isolated from this species [47]. | Bark | To treat digestive disorders [21]. |
| 66 | Myroxylon peruiferum L. f. | Chaquino | Two flavonoids, 2′-hydroxy-7,3′,4′-trimethoxyisoflavanone, and 2′-hydroxy-7,3′,4′-trimethoxyisoflavone were isolated from this species [48]. | Bark | To treat general respiratory disorders [22]. |
| GENTIANACEAE | |||||
| 67 | Halenia weddelliana Gilg | Taruka cacho, cacho de venado | No information is reported in literature. | Whole plant | It helps maintain milk production in cattle [4]. |
| 68 | Macrocarpaea lenae J. R. Grant | Tabaco de cerro | No information is reported in literature. | Leaves | To cure the fever or the cold caused by cold air or strong winds (locally known as mal aire (bad air) d [4]. |
| GERANIACEAE | |||||
| 69 | Geranium diffusum Kunth. | Cáncer | No information is reported in literature. | Whole plant | To cure gangrene and infections after birth [4]. |
| JUGLANDACEAE | |||||
| 70 | Juglans neotropica Diels. c | Nogal, tocte | No information is reported in literature. | Leaves | In postpartum baths, and to treat disorders of the circulatory system [4,21,22]. |
| LAMIACEAE | |||||
| 71 | Hyptis purdiei Benth. | Poleo de cerro, poleo negro | No information is reported in literature. | Branches | The plant is rubbed to treat culture-related syndromes [21]. |
| 72 | Minthostachys mollis (Kunth) Griseb. | Poleo blanco, tipo | This aromatic shrub grows wild in the Andes above 1500 m of altitude from Venezuela to Argentina. Apparently, the composition of the essential oil of the plant grown in different geographical locations is not the same. A specimen from Argentina contained (-)-menthone as the main component; the oil from M. mollis collected in Ecuador contained neomenthol, (-)-menthone and menthol as the main constituents, while pulegone (75.2–79.3%) predominated among 28 components identified in the oil from Venezuela [49]. | Branches | To cure the fever or the cold caused by cold air or strong winds (locally known as mal aire (bad air) d, for pain relief (joints, head, throat), anti-inflammatory, and to cure respiratory problems [4,18,21]. |
| 73 | Salvia leucocephala Kunth. | Espliego, lavanda | No information is reported in literature. | Whole plant | In postpartum baths [4]. |
| 74 | Salvia scutellarioides Kunth.(syn. S. palaefolia) | Matico grande, salvia flor azul | Alkaloids, triterpenes, and lignans were isolated this species [50]. | Flowers | Vaho de agua (supernatural disease caused by exposure to water-vapors from rivers, lakes, etc.) d [4,21]. |
| LAURACEAE | |||||
| 75 | Persea americana Mill. | Aguacate, palta | Juglanin and (+)-lyoniresinol were isolated from the leaves. Both compounds showed significant cell regeneration in neomycin-damaged hair cell without cellular toxicity [51]. | Seeds | To treat coups and hematomas [4]. |
| LYCOPODIACEAE | |||||
| 76 | Huperzia sellifolia B. Øllg. | Wuaminga colorado | No information is reported in literature. | Whole plant | Amulet against evil eye and sorcery d [4]. |
| 77 | Lycopodium weberbaueri (Nessel). | Wuaminga suco or gris | No information is reported in literature. | Whole plant | Amulet against evil eye and sorcery d [4]. |
| 78 | Huperzia austroecuadorica B. Øllg | Wuaminga verde (pequeña) | No information is reported in literature. | Whole plant | Amulet against evil eye and sorcery d [4]. |
| MELASTOMATACEAE | |||||
| 79 | Aciotis rubricaulis (Mart. ex DC.) Triana | Chulco | No information is reported in literature. | Leaves, stalks | Pain relief (joints, head, throat), and to treat gastrointestinal and renal-urological problems [18]. |
| 80 | Brachyotum confertum (Bonpl.) Triana. | Sacha zarcillo | No information is reported in literature. | Branches | Against allergies [4]. |
| 81 | Tibouchina laxa (Desr.) Cogn. | Dumaricgri, dumarín, chininingue, garra del diablo | No information is reported in literature. | Flowers | To treat eye infections of guinea pigs (it has not been used for man) [4]. |
| MELIACEAE | |||||
| 82 | Cedrela montana Moritz ex Turcz. | Cedro andino, cedro blanco | Two oleanane-type triterpenes, 3-oxo-11a,12a-epoxy-oleanan-28,13b-olide and 3-oxo-olean-11-en-28,13b-olide, were isolated from the fruits and seeds. In addition, the known compounds oleanonic acid, a mixture of b-sitosterol and stigmasterol, and the limonoid photogedunin were isolated [52]. | Leaves | In postpartum baths and to relieve bone pain [4]. |
| MORACEAE | |||||
| 83 | Ficus yoponensis Desv. | Saumerio | No information is reported in literature. | Latex | The latex has medicinal and technological uses and serves as an adhesive to bandage wounds. To treat kidney diseases and rheumatic pain, stomach pain and ulcers, varicose veins, hepatic inflammatory processes, and used as a vermifuge [19]. |
| MYRICACEAE | |||||
| 84 | Morella parvifolia (Benth.) C.Parra | Laurel, laurel de cera, laurel de monte | The main constituents of the essential oil analyzed by GC-MS were α-bisabolol (50.6–58.9%) and α-pinene (12.9–16.8%). No antibacterial activity was detected [53]. | Branches | To treat general gynecological disorders [21]. |
| 85 | Morella pubescens (Humb. & Bonpl. Ex Willd.) Wilbur | Laurel, laurel de cera | No information is reported in literature. | Branches | To treat general gynecological disorders [21]. |
| 86 | Myrica parvifolia Benth. | Laurel | No information is reported in literature. | Branches, buds | To treat the fever or the cold caused by cold air or strong winds (locally known as mal aire (bad air) d, used against stomach colic, and to treat fainting during childbirth [4]. |
| 87 | Myrica pubescens Humb. & Bonpl. ex Willd. | Millma laure (laurel lanudo) | No information is reported in literature. | Leaves | To treat the fever or the cold caused by cold air or strong winds (locally known as mal aire (bad air) d [4]. |
| MYRTACEAE | |||||
| 88 | Psidium guajava L. | Guayaba | Meroterpenoids, a triterpenoid, terpenoid derivatives, and aromatic compounds, were isolated from the leaves. Meroterpenoids were evaluated for their antitumor and antifungal activities. Meroterpenoids psiguajadial D, guapsidial A, 4,5-diepipsidial A, guadial A, and guadial B were cytotoxic against five human tumor cell lines (HL-60, A-549, SMMC-7721, MCF-7, and SW-480). Guapsidial A was the most effective with an IC50 of 3.21–9.94 μmol·L−1 [54]. | Fruits | It is used orally to treat disorders of the digestive system [21]. |
| ONAGRACEAE | |||||
| 89 | Fuchsia harlingii Munz | Pena, pena de cerro | No information is reported in literature. | Flowers | Anti-inflammatory and sedative remedy [20]. It is used orally to treat neurological disorders [21]. |
| 90 | Fuchsia hypoleuca I. M. Johnst | Sacha pena | No information is reported in literature. | Flowers | To treat neurological disorders [4]. |
| 91 | Fuchsia loxensis Kunth | Pena, pena rosada | No information is reported in literature. | Flowers | Cardiotonic, febrifuge and sedative remedy [20]. It is used orally to treat neurological disorders [21]. |
| 92 | Ludwigia nervosa (Poir.) H. Hara | Flor de reina, mejorana de huerta | No information is reported in literature. | Flowers | Anti-inflammatory and sedative remedy [20]. It is used orally to treat gynecological, nervous, and dermatological disorders [21]. |
| 93 | Oenothera rosea L’Her. ex Aiton | Shullo, shullu colorado | The flavonoids: quercetrin and quercetin 3-O-β-D-allopyraNoside-3″,6″-diacetate were isolated from this plant [55]. | Flowers, leaves, stalks | Anti-inflammatory, digestive, diuretic remedy, and to treat hepatic and kidney problems [16,21,22]. |
| ORCHIDACEAE | |||||
| 94 | Epidendrum cochlidium Lindl. | Flor de cristo anaranjada | No information is reported in literature. | Flowers | To treat neurological disorders [4]. |
| 95 | Epidendrum fimbriatum Kunth | Flor de cristo blanca, espíritu | No information is reported in literature. | Flowers | To treat internal tumors [4]. |
| 96 | Epidendrum jamiesonis Rchb.f. | Flor de cristo violeta, maywa | No information is reported in literature. | Flowers | Used as an anti-inflammatory, sedative, diuretic, and hepatic remedy [20]. It is used orally to treat dermatological disorders [21]. |
| OXALIDACEAE | |||||
| 97 | Oxalis corniculata L. | Chulco, trebol, trebol de huerta | Corniculatin A was isolated from an EtOAc extract of the whole plant, together with luteolin, luteolin-7-O-β-D-glucoside, and β-sitosterol-3-O-β-D-glucoside [56]. | Whole plant | Against scurvy (scorbutic tongue) [4]. |
| 98 | Oxalis peduncularis Kunth. | Chulco amarillo | No information is reported in literature. | Whole plant | To cure infection of the throat [4]. |
| 99 | Oxalis spiralis Ruiz & Pav. ex G. Don | Chulco, cañitas, trigonella | No information is reported in literature. | Whole plant | To cure infection of the throat [4]. |
| PHYTOLACCACEAE | |||||
| 100 | Phytolacca americana L. | Atuczara, hatun sara | No information is reported in literature. | Fruits | Against dandruff [4]. |
| PIPERACEAE | |||||
| 101 | Peperomia blanda (Jacq.) Kunth | Sacha congona | Tetrahydrofuran lignans and flavones were isolated from the aerial parts. Some lignans exhibited high in vitro trypanocidal activity against epimastigotes of Trypanosoma cruzi strain Y. [57]. | Plant roots | It is used orally to treat neurological disorders [21]. |
| 102 | Peperomia congona Sodiro | Congona, congona olorosa | No information is reported in literature. | Leaves, flowers, stalks | Anti-parasitic, antiperspirant, analgesic, cardiotonic, diuretic, hepatic, sedative, and to treat headache and insomnia [4]. |
| 103 | Peperomia galioides Kunth | Tigresillo, sacha congona, congona de cerro | Eighty-four constituents were identified in the leaf essential oil analyzed by GC and GC-MS, which constituted more than 99% of the oil. The main components were safrole (42.3%) and epi-α-bisabolol (29.2%) [58]. | Whole plant | Against aire de agua o vaho de agua (a supernatural disease caused by exposure to water-vapors from, for example, rivers, lakes, etc.) d [4,21]. |
| 104 | Peperomia ilaloensis Sodiro | Congona de castilla, congona negra | No information is reported in literature. | Plant without roots | As an analgesic and sedative remedy [20]. It is used orally to treat neurological and sensorial disorders [21]. |
| 105 | Peperomia peltigera C. DC. c | Pata conguyo, condorcol | No information is reported in literature. | Fruit, leaves | To treat headache, respiratory, and neurological problems [4,18]. |
| 106 | Piper aduncum L. | Cordoncillo, matico de monte, monte del soldado | Bioactivity-guided fractionation of a leaf ethanolic extract afforded the dihydrochalcone adunchalcone, which was evaluated against promastigote forms of Leishmania amazonensis, L. braziliensis, L. shawi, and L. chagasi. The compound displayed EC50 values of 11.03, 26.70, and 11.26 μM, respectively, as well as selective indexes of 4.86, 2.01, 4.76, and 0.50, respectively. In contrast, adunchalcone exhibited weak activity against intracellular forms of L. amazonensis, compared to amphotericin B [59]. | Leaves, stalks | To treat infections of external wounds, gastrointestinal, respiratory, and skin (inflammation, bruises) problems, and an anti-inflammatory [4,18,21,22]. |
| 107 | Piper crassinervium Kunth | Guabiduca dulce | Bioactivity-guided fractionation of a leaf extract afforded three antifungal prenylated hydroquinones, together with two antifungal flavanones [60]. | Leaves | As an analgesic and antiseptic remedy, and against stomachache [20]. It is used orally to treat hormonal and respiratory disorders [21]. |
| POLYGALACEAE | |||||
| 108 | Polygala paniculata L. | Mentol, poligaga flores violetas | The xanthones 1-hydroxy-5-methoxy-2,3-methylenedioxy-xanthone and 1,5-dihydroxy-2,3-dimethoxyxanthone, together with the coumarin murragatin and the flavonol rutin were isolated from this plant [61]. | Whole plant | It is used orally to treat musculoskeletal disorders [21]. |
| POLYGONACEAE | |||||
| 109 | Rumex tolimensis Wedd | Turu | No information is reported in literature. | Stems, leaves | To promote hair growth and against dandruff [4]. |
| POLYPODIACEAE | |||||
| 110 | Niphidium crassifolium (L) Lellinger | Calaguala, calawala | No information is reported in literature. | Roots | It is used orally to treat digestive and urological disorders [21]. |
| PTERIADACEAE | |||||
| 111 | Adiantum poiretii Wikstr. | Culantrillo pata negra | No information is reported in literature. | Whole plant, leaves | To treat the cold [4]. It is used orally to treat gynecological disorders [21]. |
| 112 | Adiantum raddianum C. Presl. | Culantrillo | No information is reported in literature. | Leaves | It is used orally to treat gynecological and urological disorders [21]. |
| 113 | Cheilanthes bonariensis (Willd.) Proctor. | Helecho congona | No information is reported in literature. | Leaves | It is used orally to treat gynecological disorders [21]. |
| 114 | Notholaena sulphurea (Cav.) J. Sm. | Grano de oro | The main constituent of the yellow frond exudate of this fern was identified as 3,5,2′-trihydroxy-7-methoxy-8-acetoxy flavone. The 5,2′-dihydroxy-7,8-dimethoxy flavone was also found, along with some common flavonoids. The white form of the fern produced three dihydrochalcones that were accompanied by some kaempferol methyl ethers and apigenin-7-methyl ether. The 3-acetoxy as well as the 3-butyryloxy and the 4′-butyryloxy derivatives of 7-methyl aromadendrin were also identified [62]. | Leaves | It is used orally to treat gynecological disorders [21]. |
| 115 | Pityrogramma ebenea (L) Proctor. | Doradilla plateada, luna plateada | 2′,6′-Dihydroxy-4,3′-dimethoxy-4′,5′-dioxymethylenedihydrochalcone was identified in the leaves [63]. | Leaves | It is used orally to treat gynecological disorders [21]. |
| 116 | Pityrogramma calomelanos (L.) Link | Doradilla del sol | An isolated new pigment was assigned the structure of an 8- or 6-dihydrocinnamoyl-5,7-dihydroxy-4-phenyl-2H-1-benzopyran-2-one. From the same fern, two other phenyl-benzopyran-2-one-derivatives and a 2-phenyl-γ-pyron (ol)-ring derivative were isolated [64]. | Leaves | It is used orally to treat gynecological disorders [21]. |
| 117 | Trachypteris induta (Maxon) R.M. Tryon & A.F. Tryon | Pata de gallina | No information is reported in literature. | Leaves | It is used orally to treat gynecological disorders [21]. |
| RANUNCULACEAE | |||||
| 118 | Clematis haenkeana C. Presl. | Zarzaparrilla roja | No information is reported in literature. | Buds | To cure sore teeth [4]. |
| ROSACEAE | |||||
| 119 | Alchemilla aphanoides Mutis ex L f. | Saucillo | No information is reported in literature. | Branches | It is used orally to treat neurological disorders [21]. |
| 120 | Hesperomeles obtusifolia (Pers.) Lindl | Quique, cerote | No information is reported in literature. | Leaves | Pain relief (joints, head, throat), and to cure gastrointestinal, respiratory, and renal-urological disorders [18]. |
| 121 | Margyricarpus pinnatus (Lam.) Kuntze | Perlilla, nigua | The main constituents of the leaf essential oil were limonene (57.8%) and α-pinene (9.7%), whereas sabinene (24.2%), limonene (9.1%), and pinocarvone (9.7%) were the main components of the fruit oil [65]. | Plant without roots | It is used orally to treat respiratory and dermatological disorders [21]. |
| 122 | Prunus serotina Ehrh. | Capulí | Bio-guided fractionation of a methanolic extract afforded 2,3-dihydro-5,7-dihydroxy-2-(4-hydroxyphenyl)-4H-1-benzopyran-4-one (naringenin, NGN), 3,4,5-trimethoxybenzoic acid, and 1,3,5-trimethoxybenzene. NGN exhibited in vitro activity, in a time-concentration-dependent manner (EC50 = 89.3 μM]. Furthermore, NGN at a dose of 376.1 μmol/kg, displayed in vivo efficacy against Taenia crassiceps cysts similar to albendazole at 188.4 μmol/kg [66]. | Leaves | In postpartum baths and to cure bone pain [4]. |
| 123 | Rubus urticifolius Poir | Mora silvestre | No information is reported in literature. | Bud and flowers | To cure gangrene [4]. |
| RUBIACEAE | |||||
| 124 | Cinchona pubescens Vahl | Cascarilla, cascarilla roja | Seven known anthraquinones, alizarin-2-methylether, anthragallol-1,2-dimethylether, purpurin, purpurin-1-methylether, 1-hydroxy-2-hydroxymethylanthraquinone, 2-hydroxy-1,3,4-trimethoxyanthraquinone, and 2,5-(or 3,5-)dihydroxy-1,3,4-(or 1,2,4-)trimethoxyanthraquinone, together with five new anthraquinones, 2-hydroxy-1,3,4,6-(or 1,3,4,7-)tetramethoxyanthraquinone, 1,6-(or 1,7-)dihydroxy-2-methylanthraquinone, 5-hydroxypurpurin-1-methyl ether, 4,6-(or 4,7-)dihydroxy-2,7-(or 2,6-)dimethoxyanthraquinone, and 6,7-dihydroxy-1-methoxy-2-methylanthraquinone were isolated from callus cultures [67]. | Bark | It is used orally to treat respiratory problems [21,22]. |
| SAPOTACEAE | |||||
| 125 | Pouteria caimito (Ruiz & Pav.) radlk | Caimito | Three triterpenoids, Δ14–taraxene–3β–ol acetate, Δ14–taraxene–3–one, and Δ14–taraxene–3β–ol, together with β–sitosterol, were isolated from the bark [68]. | Leaves | The latex is used to remove subcutaneous larvae. The leaf infusion is used to treat skin infections [19]. |
| SCROPHULARIACEAE | |||||
| 126 | Pedicularis incurva Benth. | Pimpinela del cerro | No information is reported in literature. | Branches | To treat the cold [4]. |
| SOLANACEAE | |||||
| 127 | Brugmansia candida Pers. | Floripondio blanco, guando, guando blanco | The alkaloids, scopolamine and anisodamine, were produced in a modified bioreactor culture system [69]. | Flowers, leaves | To cure the fever or the cold caused by cold air or strong winds (locally known as mal aire (bad air) d [4,21,22]. |
| 128 | Brugmansia sanguinea (Ruiz & Pav.) D. Don | Floripòndio rojo, guando rojo | No information is reported in literature. | Flowers, leaves | The plant is rubbed to treat culture-related syndromes [21]. |
| 129 | Cestrum mariquitense Kunth | Sauco negro | No information is reported in literature. | Branches | It is used to treat general disorders of the circulatory system [21]. |
| 130 | Cestrum racemosum Ruiz & Pav | Sauco blanco | No information is reported in literature. | Branches | It is used to treat general culture-related syndromes [21,22]. |
| 131 | Cestrum sendtnerianum C. Mart. | Sauco negro | No information is reported in literature. | Leaves and flowers | To cure fever, headache, and postpartum relapses [4]. |
| 132 | Cyphomandra betacea (Cav.) | Tomate de árbol | No information is reported in literature. | Fruits | To cure throat infection [4]. |
| 133 | Lycopersicon hirsutum Dunal | Monte de guishco, monte de gallinazo, monte de ushco | No information is reported in literature. | Branches, leaves | It is used to treat general culture-related syndromes [22]. |
| 134 | Physalis peruviana L. c | Uvilla, uchuva, uvilla lanuda | The UPLC-ESI-MS/MS metabolic profile of an EtOAc extract of fruits cultivated in Egypt allowed the identification of several phenolic compounds. Moreover, the EtOAc extract showed remarkable α-amylase, β-glucosidase, and lipase inhibitory effects. In an in vivo antihyperglycemic test with streptozotocin (STZ)-induced diabetic rats, the EtOAc extract decreased the blood glucose level, prevented the reduction of body weight, and improved serum indicators of kidney injury [70]. | Fruits | To lower cholesterol [4]. |
| 135 | Solanum americanum Mill. | Mortiño, hierba mora | No information is reported in literature. | Leaves, fruits | Anti-inflammatory, analgesic, digestive, febrifuge, sedative, to treat respiratory diseases, the fever, the cold, pneumonia, internal infections, and kidney problems [4,16,21,22]. |
| 136 | Solanum juglandifolium Dunal | Matico | No information is reported in literature. | Flowers | Against air wáter d [4]. |
| 137 | Solanum nigrescens M. | Hierba mora | The antifungal activity of the extracts was attributed to the presence of a spirostanol glycoside, cantalasaponin-3 [71]. | Leaves | Pain relief (joints, head, throat), and to cure fever, gastrointestinal, respiratory, skin (inflammation, bruises), renal-urological, and anti-inflammatory diseases [4,21]. |
| 138 | Solanum oblongifolium Dunal, Solan. | Turpe, tululuche, mata perro | No information is reported in literature. | Branches, leaves | To cure the fever or the cold caused by cold air or strong winds (locally known as mal aire (bad air) d, and dislocation [4]. |
| 139 | Solanum pimpinellifolium L. | Monte de gallinazo | No information is reported in literature. | Branches | To treat general culture-related syndromes [21]. |
| TILIACEAE | |||||
| 140 | Triumfetta althaeoides Lam. | Abrojo, achotillo, cadillo | No information is reported in literature. | Leaves | To treat liver and kidney inflammations [4,22]. |
| 141 | Triumfetta semitriloba Jacq. | Abrojo, cadillo, monstrante | No information is reported in literature. | Leaves | To treat general urological diseases [21]. |
| VALERIANACEAE | |||||
| 142 | Valeriana pyramidalis Kunth | Valeriana | No information is reported in literature. | Roots | It is used orally to treat neurological problems [21]. |
| 143 | Valeriana microphylla Kunth | Valeriana de cerro | Five valepotriates, i.e., valtrate, isovaltrate, diavaltrate, acevaltrate, and didrovaltrate, together with nardostaquine, and two lignans, (+)-1-hydroxypiNoresiNol and pinoresinol were isolated and identified [72]. | Roots | To cure nerves [4]. |
| VERBENACEAE | |||||
| 144 | Aloysia citriodora Paláu | Cedrón | The effect of continuous and pulsed ultrasound pre-treatments (15, 30, and 45 min), followed by conventional hydrodistillation, on the characteristics of isolated essential oils (EOs) from dried leaves of A. citriodora was evaluated for the first time. Moreover, the chemical composition, the antibacterial and antioxidant activities, as well as the contents in heavy metals (iron, copper, lead, arsenic, and cadmium) of the Eos were determined [73]. | Leaves | Pain relief (joints, head, throat), anti-inflammatory, and to treat gastrointestinal and respiratory problems [4]. |
| 145 | Aloysia triphylla (L’Hér.) Britton. * | Cedrón | The EO contained myrcenone (36.50%), α-thujone (13.10%), lippifoli-1(6)-en-5-one (8.87%), and limonene (6.87%) as the main components [74]. | Leaves, flowers, stalks | Anti-inflammatory, antispasmodic, anti-neuralgic, analgesic, cardiotonic, digestive, stomach tonic, diuretic, and to cure the fever, headache, the cold, and colic [4,21,22]. |
| 146 | Phyla strigulosa (M. Martens & Galeotti) Moldenke | Sistalgina/novalgina | No information is reported in literature. | Whole plant | To treat stomachache [22]. |
| 147 | Verbena litoralis Kunth | Verbena | Phytochemical tests revealed the presence of iridoid glycosides, flavonoids, phenylpropanoid derivatives, phenylethanoid derivatives, cinnamic acid derivatives, and triterpenes. The extract was classified ‘safe’ (category 5), according to the OECD guidelines, in acute treatments [75]. | Flowers | To cure plagues and headache, body malaise, infection of the throat, respiratory and skin diseases (inflammation, bruises), flu, and pain relief (joints, head, throat) [4,18,21,22]. |
| VIOLACEAE | |||||
| 148 | Viola arguta Willd. & Schult. ex Roem. | Violeta de campo flor roja, pucango | No information is reported in literature. | Flowers | To cure nerve problems [4]. |
| 149 | Viola dombeyana DC. | Violeta de campo | No information is reported in literature. | Flowers | To cure nerve problems [4]. |
| VISCACEAE | |||||
| 150 | Dendrophthora fastigiata Kuijt. | Suelda pequeña | No information is reported in literature. | Whole plant | To treat fractured and dislocated bones [4]. |
| 151 | Phoradendron parietarioides Trel. | Suelda grande, matapalo, solda-solda, suelda | No information is reported in literature. | Whole plant | To treat fractured and dislocated bones [4]. |
| WINTERACEAE | |||||
| 152 | Drimys granadensis L. f. | Cascarilla | A total of 85 components were identified in the leaf EO analyzed by GC and GC-MS. Germacrene D (14.7%), sclarene (9.5%), α-cadinol (7.3%), longiborneol acetate (6.3%), drimenol (4.2%), (Z)-β-ocimene (3, 4.2%), α-pinene (3.2%), and β-elemene (2.7%) were the main components of the oil. The EO was also tested against eight bacteria strains using the Kirby–Bauer disk-diffusion method. Most of the tested Gram-positive bacteria were susceptible to the oil, while the Gram-negative bacteria were not [76]. | Bark | To cure sore teeth [4]. |
| No. | Botanical Name | Vernacular Name | Used Part(s) of the Plant | Traditional Uses |
|---|---|---|---|---|
| AGAVACEAE | ||||
| 1 | Agave americana L. a,b | Cabuya, penco, chaguarquero | Stems | To heal bone fractures and dislocations [4]. |
| AIZOACEAE | ||||
| 2 | Mesembryanthemum elegans L. | Condorcoles pequeño | Leaves | To treat nerves and headache [4]. |
| AMARANTHACEAE | ||||
| 3 | Aerva sanguinolenta (L.) Blume a,b | Escancel | Whole plant without roots | It is used in topical applications, orally, and in poultices and washings to treat general disorders of the dermatological, digestive, gynecological, urinary, and nervous systems, and to cure renal problems and culture-related syndromes [18,21]. |
| 4 | Dysphania ambrosioides (L) Mosyakin & Clemants a,b | Paico | Branches | Branches are rubbed to treat disorders of the digestive system and culture-related syndromes [21,22]. |
| APIACEAE | ||||
| 5 | Anethum graveolens L. a,b | Eneldo | Whole plant | Pain relief (joints, head, throat), and to treat gastrointestinal, respiratory, skin (inflammation, bruises), and renal-urological problems [18]. |
| 6 | Apium graveolens L. a,b | Apio | Leaves, stalks | Pain relief (joints, head, throat), and to treat gastrointestinal, respiratory, and anti-inflammatory problems [18]. |
| 7 | Apium leptophyllum (Pers.) F. Muell. b | Culantrillo blanco | Whole plant | It is used to treat the cold [4]. |
| 8 | Coriandrum sativum L. a,b | Cilantro, culantro | Whole plant | To treat the abdominal pain related to menstruation [4]. |
| 9 | Cyclospermum leptophyllum (Pers.) Sprague ex Britton & P. Wilson b | Culantrillo, cominillo | Branches | It is used orally to treat disorders of the digestive system [21]. |
| 10 | Daucus carota L. a,b | Zanahoria | Leaves | The juice is used to treat gastritis [4]. |
| 11 | Foeniculum vulgare Mill. a,b | Hinojo, eneldo | Leaves, whole plant | It is used orally to treat disorders of the digestive system, and as an anti-inflammatory, a relaxant, against conjunctivitis, indigestion, gastritis, menstrual colic, diabetes, anticancer, and to increase the breast milk [4,16,21]. |
| 12 | Petroselinum crispum (Mill.) Fuss a,b | Perejil | Whole plant, leaves, stalks | Pain relief (joints, head, throat), and to treat gastrointestinal, respiratory, and neurological disorders [4,18]. |
| 13 | Pimpinella anisum L. b | Anís | Seeds | Pain relief (joints, head, throat), to treat gastrointestinal problems, and as a febrifuge [18]. |
| ASPHODELACEAE | ||||
| 14 | Aloe vera (L.) Burm. f. b | Sábila | Leaves | Pain relief (joints, head, throat), and to treat gastrointestinal, respiratory, and renal-urological problems. Topical applications are used to treat skin problems [18,21,22]. |
| ASTERACEAE | ||||
| 15 | Ageratum conyzoides L. b | Canayuyo, pedorrera, hierba de chivo | Whole plant | To heal gangrene and infections. It is also used orally to treat disorders of the digestive system [4,21]. |
| 16 | Cotula australis (Sieber ex Spreng.) Hook.f. | Chichira sombrerito | Whole plant | To decrease disease relapses after recovery (locally known as recaída in Spanish) [4]. |
| 17 | Cynara cardunculus L. a,b | Alcachofa | Fruits | It is used orally to treat disorders of the hormonal system [21]. |
| 18 | Matricaria chamomilla L. a,b | Manzanilla | Whole plant | Pain relief (joints, head, throat), anti-inflammatory, to treat gastritis, gastrointestinal and respiratory problems, skin inflammation, and bruises [4,18,22]. |
| 19 | Matricaria recutita L. a,b | Manzanilla | Flowers, leaves, stalks | Anti-inflammatory, sedative, anti-flatulence, anthelmintic, analgesic, carminative, digestive, febrifuge, and used against cramps, insomnia, wounds, stomach pain, and burns. Used as a stimulant tonic. It is also used in gargles to treat disorders of the respiratory system [16,21]. |
| 20 | Sigesbeckia mandoni Schult. Bip. | Sacha jícama | Leaves | To treat diarrhea in children from 1 to 6 months of age [4]. |
| 21 | Sonchus oleraceus L. a,b | Cerraja, serraja, Cachicerraja | Whole plant | To heal body malaise, pain relief (joints, head, throat), and to treat gastrointestinal, respiratory, and renal-urological problems, skin inflammation, and bruises [4,18]. |
| 22 | Tagetes erecta L. a,b | Killo rosa, flor de muerto, calendula | Branches, flowers | Against vaho de agua c (a supernatural disease, presumed to be due to exposure to water-vapors). The plant is rubbed to heal culture-related syndromes [4,21]. |
| 23 | Tagetes patula L. a,b | Arrayosa | Flowers | The plant is rubbed to heal culture-related syndromes [22]. |
| 24 | Tanacetum parthenium (L.) Sch. Bip. b | Santa María | Whole plant | To cure fear in children [4,21,22]. |
| 25 | Taraxacum officinale F. H. Wigg. b | Diente de león, taraxaco | Whole plant | To cure gastritis and ulcer, and for pain relief (joints, head, throat). To treat gastrointestinal, respiratory, and renal-urological problems, skin inflammation, and bruises [4,18,21]. |
| BALSAMINACEAE | ||||
| 26 | Impatiens balsamina L. a,b | Amor constante, begonia | Flowers | In postpartum relapse [4]. |
| BORAGINACEAE | ||||
| 27 | Borago officinalis L. a,b | Borraja | Flowers, leaves, stalks | Anti-inflammatory, anti-flu, expectorant, febrifuge, to enhance blood circulation, sudorific, astringent, diuretic, anti-hypercholesterolemic, analgesic, antidiarrheal, antitussive and emmenagogue; to treat hepatic pain, conjunctivitis, burnings, headache, and coughs; to decrease disease relapses after recovery (locally known as recaída in Spanish); to cure gastrointestinal, respiratory, and renal-urological problems [16,18,20,21,22]. |
| 28 | Symphytum officinale L. b | Consuelda, suelda | Leaves | It is used to treat musculoskeletal disorders [21]. |
| BRASSICACEAE | ||||
| 29 | Brassica oleracea ‘Acephala’ a,b | Col silvestre | Stems | To cure liver and kidney inflammations and infections, and postpartum infections [4]. |
| 30 | Matthiola incana (L.) R. Br. a,b | Alhelí, alelí | Flowers | It is used orally to treat neurological disorders [21]. |
| 31 | Nasturtium officinale R. Br. a,b | Berro chico, berro negro | Leaves, whole plant | To cure body malaise, headache, flu, and pneumonia [4]. |
| 32 | Rorippa nasturtium-aquaticum (L.) Hayek | Berro | Plant without roots | It is used orally to cure disorders of the circulatory system [21]. |
| CACTACEAE | ||||
| 33 | Echinopsis pachanoi (Britton & Rose) Friedrich & G. D. Rowley | San pedrillo, san Pedro, aguacolla | Stems | In sorcery rituals c [4,22]. |
| 34 | Trichocereus macrogonus (Salm-Dyck) Riccob. | San pedrillo | Wood | To treat culture-related syndromes [21]. |
| CAMPANULACEAE | ||||
| 35 | Lobelia cf. decurrens Cav. a | Cholo valiente, cararango | Branches | To treat culture-related syndromes [21,22]. |
| CAPRIFOLIACEAE | ||||
| 36 | Sambucus nigra L. a,b | Tilo, sauco tilo | Flowers | Anti-flu, to treat bronchitis, febrifuge, antidiarrheal, sedative, antitussive, to cure nerves, colds, coughs, and headaches [16,20,21,22]. |
| CARYOPHYLLACEAE | ||||
| 37 | Dianthus caryophyllus L. a,b | Clavel | Flowers | Anti-inflammatory, anti-flu, analgesic, anticough, sedative, cardiotonic, and to cure nerves and stomach pain [4,16,20,21]. |
| CHENOPODIACEAE | ||||
| 38 | Chenopodium album L. b | Paico, palitaria, palitaria blanca | Branches or buds | To treat blows, dislocations, and sprains [4,21]. |
| 39 | Chenopodium ambrosioides L. b | Paico | Whole plant | To treat gallbladder stones and gastrointestinal problems [4,18]. |
| 40 | Tradescantia zebrina Hort. Ex Bosse b | Hoja de la plata, lazo de amor, oreja de tigre, zebrina, calcha | Whole plant | To prevent postpartum relapse [4,21]. |
| CRASSULACEAE | ||||
| 41 | Kalanchoe gastonis Bonnieri b | Dulcamara, mala madre | Leaves | To treat general digestive disorders [21]. |
| CUCURBITACEAE | ||||
| 42 | Cucurbita ficifolia Bouchè, Verh. a,b | Alcayata, zambo | Whole plant | To treat blows [4]. |
| 43 | Cucurbita maxima D’uchense ex Lam. a,b | Zapallo | Leaves | To cure diarrhea in children from 1 to 6 months of age [4]. |
| 44 | Cucurbita pepo L. a,b | Sambo | Latex | To treat general dermatological disorders [21]. |
| CUPRESSACEAE | ||||
| 45 | Cupressus lusitanica Mill. a,b | Ciprés | Fruits | To control baldness [4]. |
| FABACEAE | ||||
| 46 | Medicago sativa L. a,b | Alfalfa | Leaves | To treat circulatory problems, especially lack of sensitivity at the body extremities (e.g., hands, feet, and/or toes) [4]. |
| 47 | Vicia faba L. a,b | Haba | Leaves | To treat headache [4]. |
| GENTIANACEAE | ||||
| 48 | Centaurium erythraea Rafr. b | Pedorrera, canchalagua | Whole plant | To cure body malaise [4,21,22]. |
| GERANIACEAE | ||||
| 49 | Erodium cf. cicutarium (L) L’Hér. Ex Aiton b | Agujilla, aujilla | Branches | It is used orally to treat general disorders and culture-related syndromes [21]. |
| 50 | Pelargonium graveolens L’Hér. ex Aiton. a,b | Esencia de rosa | Flowers, leaves, stalks | Anti-inflammatory, analgesic, febrifuge, antidiabetic, antidiarrheal, to treat gallbladder and liver problems, a digestive, to cure gastric ulcers, wounds, burns, respiratory diseases, jaundice, infertility, and urinary stones. It is also used to cure vaginal infections before and after childbirth [4,16,21,22]. |
| 51 | Pelargonium odoratissimum (L.) L’ Hér. a,b | Malva olorosa | Flowers, leaves, stalks, branches | Anti-inflammatory, analgesic, carminative and tonic, diuretic, antidiarrheal, and to cure colic, neurological and heart problems, and children’s colds [4,16,20,21,22]. |
| 52 | Pelargonium zonale (L.) L’Hér. a | Geranio | Flowers | To cure vaginal infections before and after childbirth [4,22]. |
| JUGLANDACEAE | ||||
| 53 | Juglans nigra L. a,b | Nogal | Leaves | To cure gastrointestinal and renal-urological problems [18]. |
| LAMIACEAE | ||||
| 54 | Mentha piperita L. a,b | Menta, menta negra | Leaves, stalks, branches | Analgesic, antidiarrheal, anti-flu, anti-inflammatory, antitussive, carminative, digestive, tonic, and against stomach pain, stomach colic, to cure indigestion and the cold; pain relief (joints, head, throat); to treat gastrointestinal, respiratory, skin (inflammation, bruises), and neurological problems [4,18,20,21,22]. |
| 55 | Mentha pulegium L. a,b | Menta de castilla | Branches | To treat stomach colic, indigestion, and the cold [4]. |
| 56 | Mentha spicata L. a,b | Hierba buena, menta, menta negra | Leaves | Anti-inflammatory, anti-flu, analgesic, digestive, antitussive, carminative, febrifuge, to cure stomach colic and the cold; pain relief (joints, head, throat); to treat gastrointestinal, respiratory, and renal-urological problems [4,18,20,21,22]. |
| 57 | Ocimum basilicum L. a,b | Albahaca, albahaca blanca | Flower, leaves | Anti-inflammatory, antispasmodic, anti-flatulence, analgesic, febrifuge, digestive, stimulant of lactation, relaxant, to treat headache, coughs, heart problems, nerves, gastritis, high blood pressure, internal infections, pain relief (joints, head, throat); to treat gastrointestinal and skin (inflammation, bruises) problems [16,18,21]. |
| 58 | Origanum majorana L. a,b | Mejorana | Leaves | Pain relief (joints, head, throat) [18,22]. |
| 59 | Origanum x majoricum Camb. a,b | Orégano, oregano de castilla | Whole plant without roots | To treat digestive problems [21]. |
| 60 | Origanum vulgare L. a,b | Orégano | Whole plant | Pain relief (joints, head, throat), and to treat gastrointestinal and renal-urological problems [4,22]. |
| 61 | Plectranthus unguentarius Codd | Oreganón, orégano grande | Leaves | It is used orally to treat digestive problems [21]. |
| 62 | Rosmarinus officinalis L. a,b | Romero | Branches, whole plant | To cure the fever or the cold caused by cold air or strong winds (locally known as mal aire (bad air) c. Pain relief (joints, head, throat); to cure gastrointestinal, skin (inflammation, bruises), and neurological problems [4,18,21,22]. |
| 63 | Salvia tiliifolia Vahl. b | Santa María | Whole plant without roots | The plant is rubbed to treat culture-related syndromes [21]. |
| 64 | Thymus vulgaris L. a,b | Tomillo | Branches, leaves | To cure indigestion, gastrointestinal, and renal-urological problems; pain relief (joints, head, throat) [4,18,21]. |
| LAURACEAE | ||||
| 65 | Cinnamomum verum J. Presl b | Canela | Bark | Pain relief (joints, head, throat), and to treat gastrointestinal and respiratory problems [18]. |
| LILIACEAE (AMARYLLIDACEAE) | ||||
| 66 | Allium sativum L. a,b | Ajo | Garlic, bulbs | To cure coughs; pain relief (joints, head, throat), and to treat gastrointestinal and respiratory problems [4,18]. |
| LINACEAE | ||||
| 67 | Linum usitatissimum L. a,b | Linaza | Seeds, leaves, stalk | It is used to treat general disorders of the digestive and urological systems [15,22]. Anti–inflammatory, digestive, hepatic, diuretic, to treat stomachache and kidney problems, inflammation of liver and kidney, and gastrointestinal and respiratory problems [4,16,18,20]. |
| MALVACEAE | ||||
| 68 | Alcea rosea L. a,b | Malva goma, malva rosa | Flowers, bark | To treat liver and kidney pain, and used as a diuretic, analgesic, and depurative [4,20,21]. |
| 69 | Corchorus siliquosus L | Té | Whole plant | To treat general digestive disorders [22]. |
| 70 | Lavatera arborea L. a | Malva, puka malva | Flowers | To treat liver and kidney inflammations [4]. |
| 71 | Malva arborea (L.) Webb & Berthel. a | Malva altea, malva blanca, malva alta | Flowers | Anti-inflammatory, antidiarrheal, febrifuge, depurative, diuretic, tonic, digestive, to treat obesity, constipation, and insect bites [4,21]. |
| 72 | Malva parviflora L. a,b | Malva blanca | Branches, flowers | To treat general gynecological and urological disorders [21]. |
| MORACEAE | ||||
| 73 | Ficus carica L. a,b | Higo, breva, higuera | Leaves | It is used orally to treat gynecological disorders [21]. |
| MYRTACEAE | ||||
| 74 | Corymbia citriodora (Hook.) K.D. Hill & LAS. Johnson a,b | Eucalipto oloroso, eucalipto aromático | Branches | It is used for inhalations to treat disorders of the respiratory system [21]. |
| 75 | Myrtus communis L. b | Arrayán | Leaves, fruits | To treat fever, gastrointestinal, respiratory, and skin (inflammation, bruises) problems [18]. |
| 76 | Syzygium aromaticum L. a,b | Clavo de olor | Flower buds, peduncles | Pain relief (joints, head, throat), and to cure gastrointestinal problems [18]. |
| OLEACEAE | ||||
| 77 | Jasminum grandiflorum L. a,b | Jazmín | Flowers | To treat neurological disorders [22]. |
| ONAGRACEAE | ||||
| 78 | Fuchsia magellanica Lam. a,b | Pena-pena, pena, pena morada, zarcillo | Flowers | Sedative, disinfectant, wound healer, and relaxant [19,20,21]. |
| PINACEAE | ||||
| 79 | Pinus radiata D. Don a,b | Pino | Fruits | Against asthma [4]. |
| PLANTAGINACEAE | ||||
| 80 | Plantago major L. a,b | Llantén | Whole plant, leaves | Anti-inflammatory, antihemorrhagic, digestive, wound healer, diuretic, to treat liver problems, insomnia, insect bites, liver and kidney inflammation; pain relief (joints, head, throat), and for gastrointestinal, respiratory, skin (inflammation, bruises), renal-urological, and neurological problems [4,18,21,22]. |
| POACEAE | ||||
| 81 | Cynodon dactylon (L.) Pers. b | Grama dulce, paja | Whole plant without roots | It is used orally to treat urological and gynecological disorders [21]. |
| 82 | Cymbopogon citratus (DC.) Stapf. a,b | Hierba Luisa, limonaria | Leaves | Anti-flatulence, analgesic, digestive, sedative, expectorant, spasmolytic, relaxant and diuretic, anti-inflammatory, to treat high pressure, nerves, gastritis, diarrhea, jaundice, insomnia and the cold, gastrointestinal, respiratory, skin (inflammation, bruises), and neurological problems; pain relief (joints, head, throat) [14,21,22]. |
| 83 | Zea mays L. a,b | Maíz (pelo de choclo) | Hair of dried maize, flowers | Against diarrhea and general malaise; pain relief (joints, head, throat), anti-inflammatory; to treat gastrointestinal, respiratory, renal-urological, and neurological problems, skin inflammation, and bruises [4,18,21,22]. |
| POLYGONACEAE | ||||
| 84 | Rumex obtusifolius L. b | Lengua de vaca, sacha-gula | Leaves, flowers | Pain relief (joints, head, throat), and to cure skin inflammation and bruises; anti-inflammatory [18]. |
| ROSACEAE | ||||
| 85 | Eriobotrya japonica (Thunb.) Lindl. a,b | Níspero, míspero, níspero del japón | Leaves | It is used orally to treat urinary disorders [21,22]. |
| 86 | Poterium sanguisorba L. b | Pimpinela | Whole plant | To treat neurological problems [4]. |
| 87 | Rosa x alba L. a,b | Rosa blanca | Flowers | To treat infections and flu [22]. |
| 88 | Rosa centifolia L. | Rosa roja | Flowers | To treat neurological problems [4,22]. |
| 89 | Rosa cymosa Tratt. a,b | Rosa | Flowers | It is used orally to treat gynecological and urological disorders [21]. |
| 90 | Sanguisorba minor subsp. Muricata (Bonnier & Layens) Briq a,b | Pimpinela | Leaves | It is used orally to treat neurological problems [21]. |
| RUTACEAE | ||||
| 91 | Citrus x junos Siebold ex Tanaka a,b | Naranja agria | Fruits | It is used orally to treat dermatological problems [21]. |
| 92 | Citrus limetta Risso a,b | Lima dulce | Fruits | To prevent high blood pressure [22]. |
| 93 | Citrus x limonum Risso a,b | Limón | Seeds | It is used orally to treat dental pain [22]. |
| 94 | Citrus sinensis (L.) Osbeck. a,b | Hojas de naranja | Leaves | Antispasmodic, relaxant, antidiarrheal; used as hair tonic; used to treat insomnia, the cold and kidney problems [16]. |
| 95 | Ruta graveolens L. a,b | Ruda | Branches, flowers, whole plant | To treat headaches, bad air c, fainting during childbirth, gastrointestinal and neurological problems; pain relief (joints, head, throat) [4,18,21,22]. |
| SIMAROUBACEAE | ||||
| 96 | Castela tortuosa Liebm. b | Hierba de perro | Leaves, flowers | Pain relief (joints, head, throat), and to treat gastrointestinal problems [18]. |
| TILIACEAE | ||||
| 97 | Tilia platyphyllos Scop. a | Tilo | Leaves, flowers | To cure respiratory, neurological, and reproductive diseases; anti-inflammatory [18]. |
| URTICACEAE | ||||
| 98 | Urtica dioica L. b | Ortiga, ortiga de monte | Whole plant | Pain relief (joints, head, throat), and to cure gastrointestinal, neurological diseases [18,21]. |
| 99 | Urtica urens L. b | Chine, chini, ortiga común | Whole plant | To treat intestinal infection and blows [4,21]. |
| VALERIANACEAE | ||||
| 100 | Valeriana officinalis L. b | Valeriana, guasilla | Leaves | To cure gastrointestinal and neurological diseases [4]. |
| VERBENACEAE | ||||
| 101 | Phyla dulcis (Trevir.) Moldenke a,b | Buscapina | Whole plant | To treat stomachache [22]. |
| 102 | Phyla scaberrima (A. Juss. Ex Pers.) Moldenke b | Buscapina, novalgina | Whole plant without roots | It is used orally to treat digestive problems [4,21]. |
| VIOLACEAE | ||||
| 103 | Viola odorata L. a,b | Violeta, violeta de huerta, violeta de jardín | Flowers | To cure coughs [4,21,22]. |
| 104 | Viola tricolor L. b | Pensamiento | Flowers | Analgesic, antidiarrheal, anti-flu, anti-inflammatory, antiseptic, diuretic, febrifuge; to cure the hoarseness and headache; to treat kidney, skin, heart, and nerve problems [4,18,21]. |
| ZINGIBERACEAE | ||||
| 105 | Hedychium coronarium J.Köning a,b | Jazmín de río, caña agria | Stems | It is used orally to treat problems of the urinary system [21,22]. |
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tene, V.; Malagón, O.; Finzi, P.V.; Vidari, G.; Armijos, C.; Zaragoza, T. An ethnobotanical survey of medicinal plants used in Loja and Zamora-Chinchipe, Ecuador. J. Ethnopharmacol. 2007, 111, 63–81. [Google Scholar] [CrossRef] [PubMed]
- Malagón, O.; Ramírez, J.; Andrade, J.M.; Morocho, V.; Armijos, C.; Gilardoni, G. Phytochemistry and Ethnopharmacology of the Ecuadorian Flora. A Review. Nat. Prod. Commun. 2016, 11, 297–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armijos, C.; Gilardoni, G.; Amay, L.; Lozano, A.; Bracco, F.; Ramírez, J.; Bec, N.; Larroque, C.; Finzi, P.V.; Vidari, G. Phytochemical and ethnomedicinal study of Huperzia species used in the traditional medicine of Saraguros in Southern Ecuador; AChE and MAO inhibitory activity. J. Ethnopharmacol. 2016, 193, 546–554. [Google Scholar] [CrossRef] [PubMed]
- Andrade, J.M.; Mosquera, H.L.; Armijos, C. Ethnobotany of indigenous Saraguros: Medicinal plants used by community healers “Hampiyachakkuna” in the San Lucas Parish, Southern Ecuador. BioMed Res. Int. 2017, 2017, 9343724. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Traditional medicine. In Proceedings of the Fifty-Sixth World Health Assembly, Geneva, Switzerland, 31 March 2003. A56/18. [Google Scholar]
- Mittermeier, R.A.; Gil, P.R.; Mittermeier, C.G. Megadiversity: Earth’s biologically wealthiest nations. In Conservation International; Cemex: San Pedro Garza Garcia, Mexico, 1997. [Google Scholar]
- Jørgensen, P.M.; León-Yanez, S. (Eds.) Catalogue of Vascular Plants of Ecuador; Monographs in Systematic Botany; Missouri Botanical Garden Press: St. Louis, MO, USA, 1999. [Google Scholar]
- De la Torre, L.; Navarrete, H.; Muriel, P.; Macía, M.J.; Balslev, H. Enciclopedia de las Plantas Utiles del Ecuador, 1st ed.; Herbario QCA de la Escuela de Ciencias Biológicas de la Pontificia Universidad Católica del Ecuador & Herbario AAU del Departamento de Ciencias Biológicas de la Universidad de Aarhus: Quito, Ecuador, 2008. [Google Scholar]
- Ulloa, C.U.; Acevedo-Rodríguez, P.; Beck, S.; Belgrano, M.J.; Bernal, R.; Berry, P.E.; Gradstein, S.R. An integrated assessment of the vascular plant species of the Americas. Science 2017, 358, 1614–1617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- León-Yánez, S.; Valencia, R.; Pitmam, N.; Endara, L.; Ulloa, C.; Navarrete, H. Libro Rojo de plantas endémicas del Ecuador, 2nd ed.; Publicaciones del Herbario QCA; Pontificia Universidad Católica del Ecuador: Quito, Ecuador, 2011; pp. 367–369. [Google Scholar]
- Neill, D.A. Cuantas especies nativas de plantas vasculares hay en Ecuador. In Revista amazónica: Ciencia y Tecnología; Universidad Estatal Amazónica: Puyo, Ecuador, 2012; Available online: https://biblat.unam.mx/es/revista/revista-amazonica-ciencia-y-tecnologia/articulo/cuantas-especies-nativas-de-plantas-vasculares-hay-en-ecuador (accessed on 14 December 2021).
- WHO Traditional Medicine Strategy 2014–2023. Available online: https://www.who.int/publications/i/item/9789241506096 (accessed on 2 March 2022).
- Newman, D.J.; Cragg, G.M. Drugs and Drug Candidates from marine sources: An assessment of the current “state of play”. Planta Med. 2016, 82, 775–789. [Google Scholar] [CrossRef] [Green Version]
- Newman, D.J.; Cragg, G.M. Natural products as sources of new drugs from 1981 to 2014. J. Nat. Prod. 2016, 79, 629–661. [Google Scholar] [CrossRef] [Green Version]
- Armijos, C.; Ramírez, J.; Salinas, M.; Vidari, G.; Suárez, A. Pharmacology and phytochemistry of Ecuadorian medicinal plants: An update and perspectives. Pharmaceuticals 2021, 14, 1145. [Google Scholar] [CrossRef]
- Armijos, C.; Matailo, A.; Bec, N.; Salinas, M.; Aguilar, G.; Solano, N.; Calva, J.; Ludeña, C.; Larroque, C.; Vidari, G. Chemical composition and selective BuChE inhibitory activity of the essential oils from aromatic plants used to prepare the traditional Ecuadorian beverage horchata lojana. J. Ethnopharmacol. 2020, 263, 113162. [Google Scholar] [CrossRef]
- Radice, M.; Cossio, N.; Scalvenzi, L. Ilex guayusa: A systematic review of its traditional uses, chemical constituents, biological activities and biotrade opportunities. In Mol2net: From Molecules to Networks, Proceedings of the MOL2NET 2016, International Conference on Multidisciplinary Sciences, Basel, Switzerland, 15 January–15 December 2016, 2nd ed.; MDPI: Basel, Switzerland, 2017; pp. 1–7. [Google Scholar]
- Fernández-Cusimamani, E.; Espinel-Jara, V.; Gordillo-Alarcón, S.; Castillo-Andrade, R.; Žiarovská, J.; Zepeda-Del Valle, J.M. Estudio etnobotánico de plantas medicinales utilizadas en tres cantones de la provincia Imbabura, Ecuador. Agrociencia 2019, 53, 797–810. [Google Scholar]
- Navas-Flores, V.; Chiriboga-Pazmiño, X.; Miño-Cisneros, P.; Luzuriaga-Quichimbo, C. Estudio fitoquímico y toxicológico de plantas nativas del oriente ecuatoriano. Cienc. Unemi 2021, 14, 26–36. [Google Scholar] [CrossRef]
- Rios, M.; Tinitana, F.; Jarrín, P.; Donoso, N.; Romero, J. “Horchata” drink in Southern Ecuador: Medicinal plants and people’s wellbeing. J. Ethnobiol. Ethnomed. 2017, 13, 18. [Google Scholar] [CrossRef] [Green Version]
- Tinitana, F.; Rios, M.; Romero-Benavides, J.; De la Cruz Rot, M.; Pardo-De-Santaya, M. Medicinal plants sold at traditional markets in southern Ecuador. J. Ethnobiol. Ethnomed. 2016, 12, 12–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maza, D.; Abad, S.; Malagón, O.; Armijos, C. Productos forestales no maderables de la comunidad El Tundo: Un remanente boscoso de biodiversidad y conocimiento ancestral del sur del Ecuador. Rev. Bionatura. 2021, 6, 2161–2174. [Google Scholar] [CrossRef]
- World Flora Online. Available online: http://www.worldfloraonline.org (accessed on 23 December 2021).
- Tropicos.org. Missouri Botanical Garden. Available online: https://www.tropicos.org/home (accessed on 23 December 2021).
- Global Biodiversity Information Facility GBIF, Ecuador. Available online: https://www.gbif.org/es/country/EC/summary (accessed on 29 December 2021).
- Hart, G.; Gaoue, O.G.; De la Torre, L.; Navarrete, H.; Muriel, P.; Macía, M.J.; Balslev, H.; León-Yánez, S.; Jørgensen, P.; Duffy, D.C. Availability, diversification and versatility explain human selection of introduced plants in Ecuadorian traditional medicine. PLoS ONE 2017, 12, e0184369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valentová, M.; Marek, R.; Švajdlenka, E.; Kubínová, R.; Suchý, V. A new isoflavanone from Iresine herbstii. Fitoterapia 2011, 82, 272–275. [Google Scholar] [CrossRef] [PubMed]
- Paul, J.H.A.; Seaforth, C.E.; Tikasingh, T. Eryngium foetidum L.: A review. Fitoterapia 2011, 82, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Tatsuno, S.; Yokosuka, A.; Hatsuma, F.; Mashiko, Y.; Mimaki, Y. Pregnane glycosides from the bark of Marsdenia cundurango and their cytotoxic activity. J. Nat. Med. 2019, 73, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Sotillo, W.S.; Villagomez, R.; Smiljanic, S.; Huang, X.; Malakpour, A.; Kempengren, S.; Rodrigo, G.; Almanza, G.; Sterner, O.; Oredsson, S. Anti-cancer stem cell activity of a sesquiterpene lactone isolated from Ambrosia arborescens and of a synthetic derivative. PLoS ONE 2017, 12, e0184304. [Google Scholar] [CrossRef] [Green Version]
- Jakupovic, J.; Jaensch, M.; Bohlmann, F.; Dillon, M.O. Eudesmanolides, 5,10-bis-epi-eudesmanes and oplopanone derivatives from Ambrosia artemisioides. Phytochemistry 1998, 27, 3551–3556. [Google Scholar] [CrossRef]
- Ruiz, S.; Malagón, O.; Zaragoza, T.; Valarezo, E. Composition of the essential oils of Artemisia sodiroi Hieron., Siparuna eggersii Hieron., Tagetes filifolia Lag. and Clinopodium nubigenum (Kunth) Kuntze from Loja Ecuador. J. Essent. Oil Bear. Plants 2010, 13, 676–691. [Google Scholar] [CrossRef]
- Zampieri, P.R.F.; Tamayose, C.I.; Fávero, O.A.; Romoff, P.; Ferreira, M.J.P. Two New Flavonoids from the leaves of Baccharis oblongifolia (Ruiz and Pav.) Pers. (Asteraceae). Molecules 2019, 24, 3198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valarezo, E.; Rosillo, M.; Cartuche, L.; Malagón, O.; Meneses, M.; Morocho, V. Chemical composition, antifungal and antibacterial activity of the essential oil from Baccharis latifolia (Ruiz\&Pav.) Pers. (Asteraceae) from Loja, Ecuador. J. Essent. Oil Res. 2013, 25, 233–238. [Google Scholar] [CrossRef]
- De Tommasi, N.; Piacente, S.; Pizza, C. Flavonol and chalcone ester glycosides from Bidens andicola. J. Nat. Prod. 1998, 61, 973–977. [Google Scholar] [CrossRef]
- Lima Silva, F.; Fischer, D.C.H.; Fechine Tavares, J.; Sobral Silva, M.; Filgueiras de Athayde-Filho, P.; Barbosa-Filho, J.M. Compilation of secondary metabolites from Bidens pilosa L. Molecules 2011, 16, 1070–1102. [Google Scholar] [CrossRef] [Green Version]
- Chóez-Guaranda, I.; García, J.; Sánchez, C.; Pesantes, C.; Flores, J.; Manzano, P. Identification of lupeol produced by Vernonanthura patens (Kunth) H. Rob. leaf callus culture. Nat. Prod. Res. 2021, 35, 503–507. [Google Scholar] [CrossRef]
- Al-Snafi, A.E. Bioactive components and pharmacological effects of Canna indica: An overview. Int. J. Pharmacol. Toxicol. 2015, 5, 71–75. [Google Scholar]
- Krajewski, D.; Duque, C.; Schrejer, P. Aliphatic β-D-glucosides from fruits of Carica pubescens. Phytochemistry 1997, 45, 1627–1631. [Google Scholar] [CrossRef]
- Khalil, R.; Ali, Q.; Hafeez, M.; Malik, A. Phytochemical activities of Conocarpus erectus: An overview. Biol. Clin. Sci. Res. J. 2020, 2020, e008. [Google Scholar] [CrossRef]
- Monache, F.D.; Mc Quhae, M.M.; Ferrari, F.; Marini-Bettolo, G.B. Ferruginin A and B and ferruanthrone, new triprenylated anthranoids from Vismia baccifera var. ferruginea. Tetrahedron 1979, 35, 2143–2149. [Google Scholar] [CrossRef]
- Carbone, V.; Montoro, P.; de Tommasi, N.; Pizza, C. Analysis of flavonoids from Cyclanthera pedata fruits by liquid chromatography/electrospray mass spectrometry. J. Pharm. Biomed. Anal. 2004, 34, 295–304. [Google Scholar] [CrossRef]
- Francescato, L.N.; Debenedetti, S.L.; Schwanz, T.G.; Bassani, V.L.; Henriques, A.T. Identification of phenolic compounds in Equisetum giganteum by LC–ESI-MS/MS and a new approach to total flavonoid quantification. Talanta 2013, 105, 192–203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodrigues, L.G.; Mazzutti, S.; Siddique, I.; Da Silva, M.; Vitali, L.; Salvador, S.R. Subcritical water extraction and microwave-assisted extraction applied for the recovery of bioactive components from Chaya (Cnidoscolus aconitifolius Mill.). J. Supercrit. Fluids 2020, 165, 104976. [Google Scholar] [CrossRef]
- Sobottka, A.M.; Görick, C.; Melzig, M.F. Analysis of diterpenoid compounds from the latex of two Euphorbiaceae by liquid chromatography-electrospray ionisation mass spectrometry. Nat. Prod. Res. 2016, 30, 1941–1944. [Google Scholar] [CrossRef] [PubMed]
- Martínez, M.C.; De Pinto, G.L.; Rivas, C. Composition of Acacia macracantha gum exudates. Phytochemistry 1992, 31, 535–536. [Google Scholar] [CrossRef]
- De Oliveira, A.B.; Iracema, M.; Madruga, L.M.; Gottlieb, O.R. Isoflavonoids from Myroxylon balsamum. Phytochemistry 1978, 17, 593–595. [Google Scholar] [CrossRef]
- Maranduba, A.; De Oliveira, A.B.; De Oliveira, G.G.; de Reis, J.E.; Gottlieb, O.R. Isoflavonoids from Myroxylon peruiferum. Phytochemistry 1979, 18, 815–817. [Google Scholar] [CrossRef]
- Rojas, L.B.; Usubillaga, A.N. Essential Oil of Minthostachys mollis Grisebach from Venezuela. J. Essent. Oil Res. 1995, 7, 211–213. [Google Scholar] [CrossRef]
- González, A.G.; Grillo, T.A.; Luis, J.G.; Vázquez, J.T.; Rodríguez, M.L.; Ravelo, J.L.; Calle, J.; Rivera, A. Sesquiterpene lactones from Salvia palaefolia. Phytochemistry 1990, 29, 3581–3585. [Google Scholar] [CrossRef]
- Park, S.; Nam, Y.H.; Rodriguez, I.; Park, J.H.; Kwak, H.J.; Oh, Y.; Oh, M.; Park, M.S.; Lee, K.W.; Lee, J.S.; et al. Chemical constituents of leaves of Persea americana (avocado) and their protective effects against neomycin-induced hair cell damage. Rev. Bras. Farmacogn. 2019, 29, 739–743. [Google Scholar] [CrossRef]
- Castellano, L.; de Correa, R.S.; Martínez, E.; Calderon, J.S. Oleanane Triterpenoids from Cedrela montana (Meliaceae). Z. Naturforsch. C J. Biosci. 2002, 57, 575–578. [Google Scholar] [CrossRef]
- Mora, F.; Silva, B.; Hernandez, V.; Rojas, L.; Carmona, J. Chemical composition of the essential oil of Morella parvifolia (Benth.) Parra-O. from the Venezuelan Andes. Emir. J. Food Agric. 2017, 28, 288–290. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.-C.; Lin, D.-M.; Liu, M.; Zhang, M.; Li, Q.; Wang, J.; Xu, L.-L.; Gao, Y.; Yang, J. Chemical constituents of Psidium guajava and their antitumor and antifungal activities. J. Chin. Mater. Med. 2021, 46, 3877–3885. [Google Scholar] [CrossRef]
- Munir, R.; Semmar, N.; Farman, M.; Ahmad, N.S. An updated review on pharmacological activities and phytochemical constituents of evening primrose (genus Oenothera). Asian Pac. J. Trop. Biomed. 2017, 7, 1046–1054. [Google Scholar] [CrossRef]
- Ibrahim, M.; Hussain, I.; Imran, M.; Hussain, N.; Hussain, A.; Mahboob, T.; Corniculatin, A. A new flavonoidal glucoside from Oxalis corniculata. Rev. Bras. Farmacogn. 2013, 23, 630–634. [Google Scholar] [CrossRef] [Green Version]
- Felippe, L.G.; Baldoqui, D.C.; Kato, M.J.; da Silva Bolzani, V.; Guimarães, E.F.; Cicarelli, R.M.B.; Furlan, M. Trypanocidal tetrahydrofuran lignans from Peperomia blanda. Phytochemistry 2008, 69, 445–450. [Google Scholar] [CrossRef]
- Robayo-Gama, P.A.; Quijano, C.E.; Morales, G.; Pino, J.A. Composition of the essential oil from leaves of Peperomia galioides HBK grown in Colombia. J. Essent. Oil Res. 2010, 22, 307–309. [Google Scholar] [CrossRef]
- Dal Picolo, C.R.; Bezerra, M.P.; Gomes, K.S.; Passero, L.F.D.; Laurenti, M.D.; Martins, E.G.A.; Sartorelli, P.; Lago, J.H.G. Antileishmanial activity evaluation of adunchalcone, a new prenylated dihydrochalcone from Piper aduncum L. Fitoterapia 2014, 97, 28–33. [Google Scholar] [CrossRef]
- Danelutte, A.P.; Lago, J.H.G.; Young, M.C.M.; Kato, M.J. Antifungal flavanones and prenylated hydroquinones from Piper crassinervium Kunth. Phytochemistry 2003, 64, 555–559. [Google Scholar] [CrossRef]
- Cristiano, R.; Pizzolatti, M.G.; Monache, F.D.; Rezende, C.M.; Branco, A. Two Xanthones from Polygala paniculata and confirmation of the 1-hydroxy- 2,3,5-trimethoxy-xanthone at trace level by HRGC-MS. Z. Naturforsch. C J. Biosci. 2003, 58, 490–494. [Google Scholar] [CrossRef]
- Arriaga-Giner, F.J.; Mizuno, M.; Iinuma, M.; Tanaka, T.; Scheele, C.; Wollenweber, E. Novel Flavonoids from the Fern Notholaena sulphurea. Z. Naturforsch. C J. Biosci. 1987, 42, 1063–1069. [Google Scholar] [CrossRef]
- Miraglia, M.D.C.M.; De Pádua, A.P.; Mesquita, A.A.L.; Gottlieb, O.R. Flavonoids from the ferns Blechnum regnellianum and Pityrogramma ebenea. Phytochemistry 1985, 24, 1120. [Google Scholar] [CrossRef]
- Wagner, H.; Seligmann, O.; Chari, M.V.; Wollenweber, E.; Dietz, V.H.; Donnelly, D.M.X.; Meegan, M.J.; O’Donnell, B. Strukurell neuartige 4-phenyl-benzopyran-2-one aus Pityrogramma calomelanos (L.) link. Tetrahedron Lett. 1979, 20, 4269–4272. [Google Scholar] [CrossRef]
- García-Roja, A.; Quijano, C.E.Q.; Morales, G.; Pino, J.A. Composition of the essential oil from leaves and fruits of Margyricarpus pinnatus (L.) O. Kuntze grown in Colombia. J. Essent. Oil Res. 2009, 21, 547–549. [Google Scholar] [CrossRef]
- Palomares-Alonso, F.; Rojas-Tomé, I.S.; Palencia Hernández, G.; Jiménez-Arellanes, M.A.; Macías-Rubalcava, M.L.; González-Maciel, A.; Ramos-Morales, A.; Santiago-Reyes, R.; Castro, N.; González-Hernández, I.; et al. In vitro and in vivo cysticidal activity of extracts and isolated flavanone from the bark of Prunus serotina: A bio-guided study. Acta Trop. 2017, 170, 1–7. [Google Scholar] [CrossRef]
- Wijnsma, R.; Go, J.T.K.A.; Harkes, P.A.A.; Verpoorte, R.; Svendsen, A.B. Anthraquinones in callus cultures of Cinchona pubescens. Phytochemistry 1986, 25, 1123–1126. [Google Scholar] [CrossRef]
- Ardon, A.; Nakano, T. Triterpenes from the bark of Pouteria caimito. Planta Med. 1973, 23, 348–352. [Google Scholar] [CrossRef]
- Cardillo, A.B.; Otálvaro, A.Á.M.; Busto, V.D.; Talou, J.R.; Velásquez, L.M.E.; Giulietti, A.M. Scopolamine, anisodamine and hyoscyamine production by Brugmansia candida hairy root cultures in bioreactors. Process Biochem. 2010, 45, 1577–1581. [Google Scholar] [CrossRef]
- Ezzat, S.M.; Abdallah, H.M.I.; Yassen, N.N.; Radwan, R.A.; Mostafa, E.S.; Salama, M.M.; Salem, M.A. Phenolics from Physalis peruviana fruits ameliorate streptozotocin-induced diabetes and diabetic nephropathy in rats via induction of autophagy and apoptosis regression. Biomed. Pharmacother. 2021, 142, 111948. [Google Scholar] [CrossRef]
- He, X.; Mocek, U.; Floss, H.G.; Cáceres, A.; Girón, L.; Buckley, H.; Cooney, G.; Manns, J.; Wilson, B.W. An antifungal compound from Solanum nigrescens. J. Ethnopharmacol. 1994, 43, 173–177. [Google Scholar] [CrossRef]
- Bach, K.; Ghia, F.; Torssell, K. Valtrates and Lignans in Valeriana microphylla. Planta Med. 1993, 59, 478–479. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, S.M.B.; Mousavi Khaneghah, A.; Koubaa, M.; Barba, F.J.; Abedi, E.; Niakousari, M.; Tavakoli, J. Extraction of essential oil from Aloysia citriodora Palau leaves using continuous and pulsed ultrasound: Kinetics, antioxidant activity and antimicrobial properties. Process Biochem. 2018, 65, 197–204. [Google Scholar] [CrossRef]
- Zygadlo, J.A.; Lamarque, A.L.; Maestri, D.M.; Guzmán, C.A.; Lucini, E.I.; Grosso, N.R.; Ariza-Espinar, L. Volatile constituents of Aloysia triphylla (L’Herit.) Britton. Britton. J. Essent. Oil Res. 1994, 6, 407–409. [Google Scholar] [CrossRef]
- De Lima, R.; Guex, C.G.; da Silva, A.R.H.; Lhamas, C.L.; dos Santos Moreira, K.L.; Casoti, R.; Dornelles, R.C.; da Rocha, M.I.U.M.; da Veiga, M.L.; de Freitas Bauermann, L.; et al. Acute and subacute toxicity and chemical constituents of the hydroethanolic extract of Verbena litoralis Kunth. J. Ethnopharmacol. 2018, 224, 76–84. [Google Scholar] [CrossRef]
- Gaviria, M.; Quijano, C.; Pino, J.; Madriñan, S. Chemical composition and antibacterial activity of the essential oil of Drimys granadensis L.f. leaves from Colombia. Chem. Biodivers. 2011, 8, 532–539. [Google Scholar] [CrossRef]
- Dewick, P.M. Medicinal Natural Products: A Biosynthetic Approach, 3rd ed.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2009; ISBN 978-0-470-74168-9. [Google Scholar]
- Armijos, C.; Cota, I.; González, S. Traditional medicine applied by the Saraguro yachakkuna: A preliminary approach to the use of sacred and psychoactive plant species in the Southern region of Ecuador. J. Ethnobiol. Ethnomed. 2014, 10, 26. [Google Scholar] [CrossRef] [Green Version]
- Tuzimski, T.; Petruczynik, A. Determination of anti-Alzheimer’s disease activity of selected plant ingredients. Molecules 2022, 27, 3222. [Google Scholar] [CrossRef]
- Jimoh, M.O.; Okaiyeto, K.; Oguntibeju, O.O.; Laubscher, C.P. A Systematic Review on Amaranthus-Related Research. Horticulturae 2022, 8, 239. [Google Scholar] [CrossRef]
- Ramírez, J.; Suarez, A.I.; Bec, N.; Armijos, C.; Gilardoni, G.; Larroque, C.; Vidari, G. Carnosol from Lepechinia mutica and tiliroside from Vallea stipularis: Two promising inhibitors of BuChE. Rev. Bras. Farmacogn. 2018, 28, 559–563. [Google Scholar] [CrossRef]
- Malagón, O.; Cartuche, P.; Montaño, A.; Cumbicus, N.; Gilardoni, G. A new essential oil from the leaves of the endemic Andean species Gynoxys miniphylla Cuatrec. (Asteraceae): Chemical and enantioselective analyses. Plants 2022, 11, 398. [Google Scholar] [CrossRef]
- Tubon, I.; Bernardini, C.; Antognoni, F.; Mandrioli, R.; Potente, G.; Bertocchi, M.; Vaca, G.; Zannoni, A.; Salaroli, R.; Forni, M. Clinopodium tomentosum (Kunth) Govaerts leaf extract influences in vitro cell proliferation and angiogenesis on primary cultures of porcine aortic endothelial cells. Oxidat. Med. Cell. Longev. 2020, 2020, 2984613. [Google Scholar] [CrossRef] [PubMed]
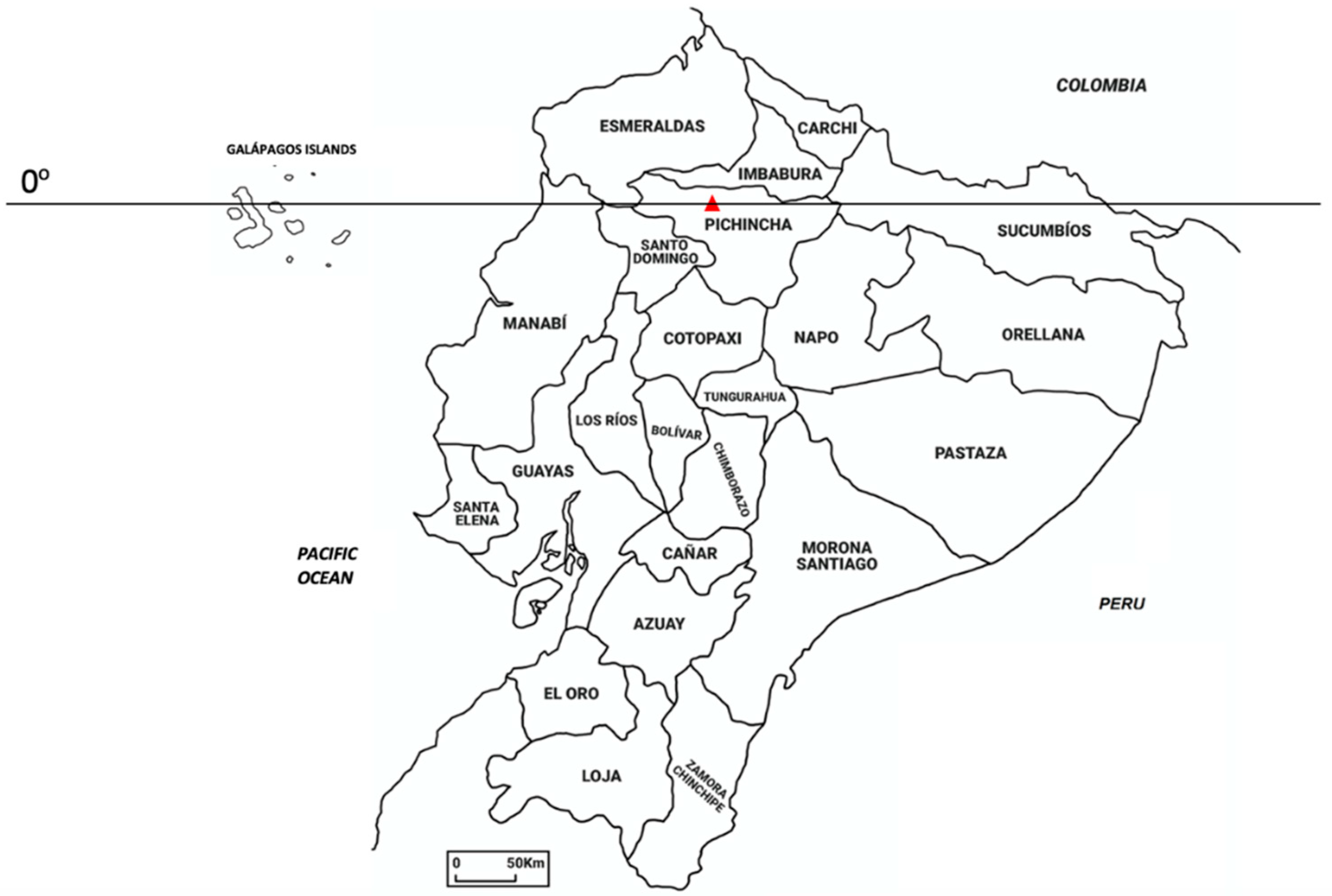
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Armijos, C.; Ramírez, J.; Vidari, G. Poorly Investigated Ecuadorian Medicinal Plants. Plants 2022, 11, 1590. https://doi.org/10.3390/plants11121590
Armijos C, Ramírez J, Vidari G. Poorly Investigated Ecuadorian Medicinal Plants. Plants. 2022; 11(12):1590. https://doi.org/10.3390/plants11121590
Chicago/Turabian StyleArmijos, Chabaco, Jorge Ramírez, and Giovanni Vidari. 2022. "Poorly Investigated Ecuadorian Medicinal Plants" Plants 11, no. 12: 1590. https://doi.org/10.3390/plants11121590
APA StyleArmijos, C., Ramírez, J., & Vidari, G. (2022). Poorly Investigated Ecuadorian Medicinal Plants. Plants, 11(12), 1590. https://doi.org/10.3390/plants11121590







