Oxidative Stability and Protective Effect of the Mixture between Helianthus annuus L. and Oenothera biennis L. Oils on 3D Tissue Models of Skin Irritation and Phototoxicity
Abstract
:1. Introduction
2. Results
2.1. Fatty Acids Composition
2.2. Thiobarbituric Acid-Reactive Substances Assay (TBA)
2.3. EpiDerm Models
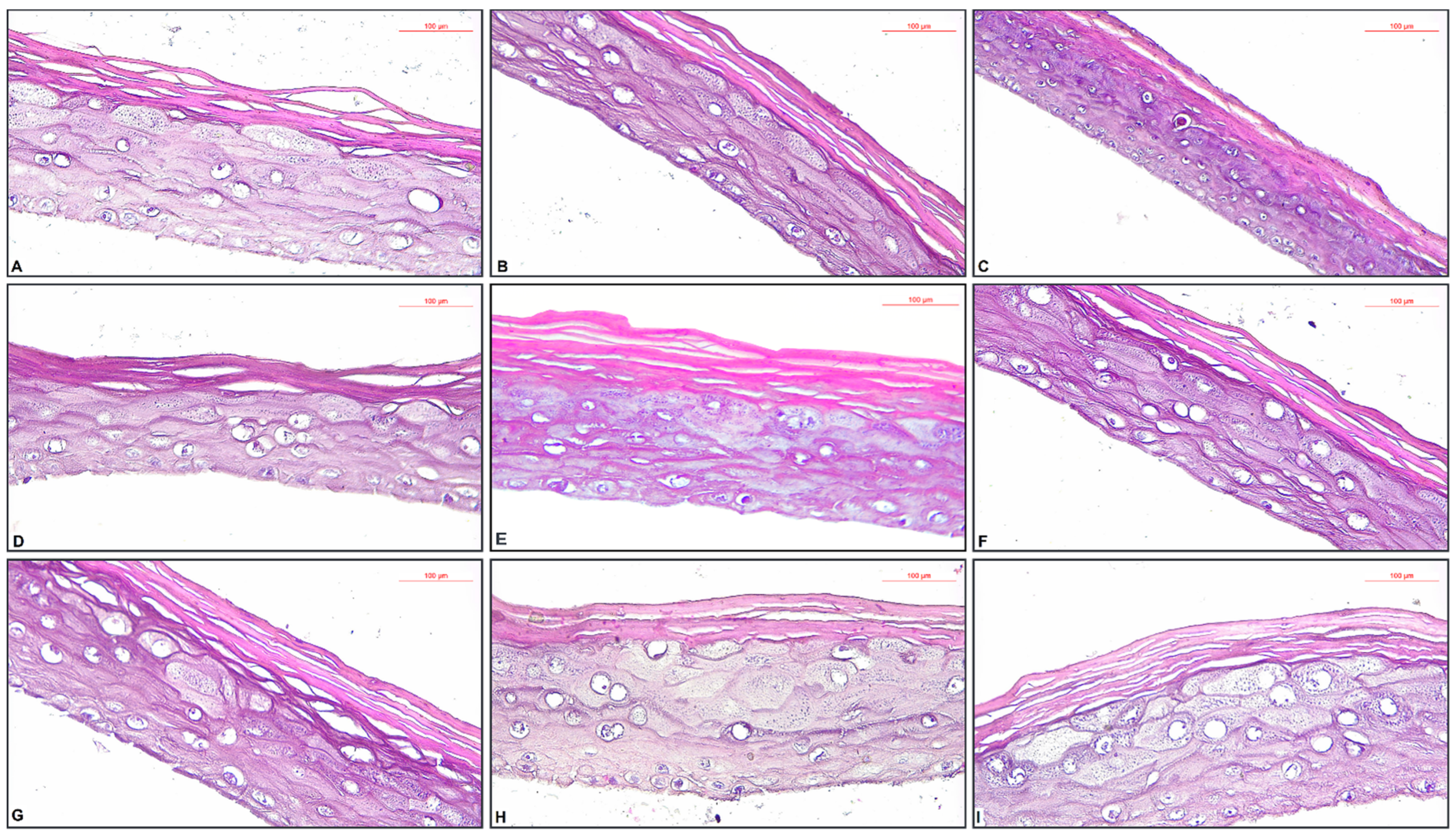
2.4. Histopathological Assessment of EpiDerm Skin Irritation Models with the Tested Oil Samples
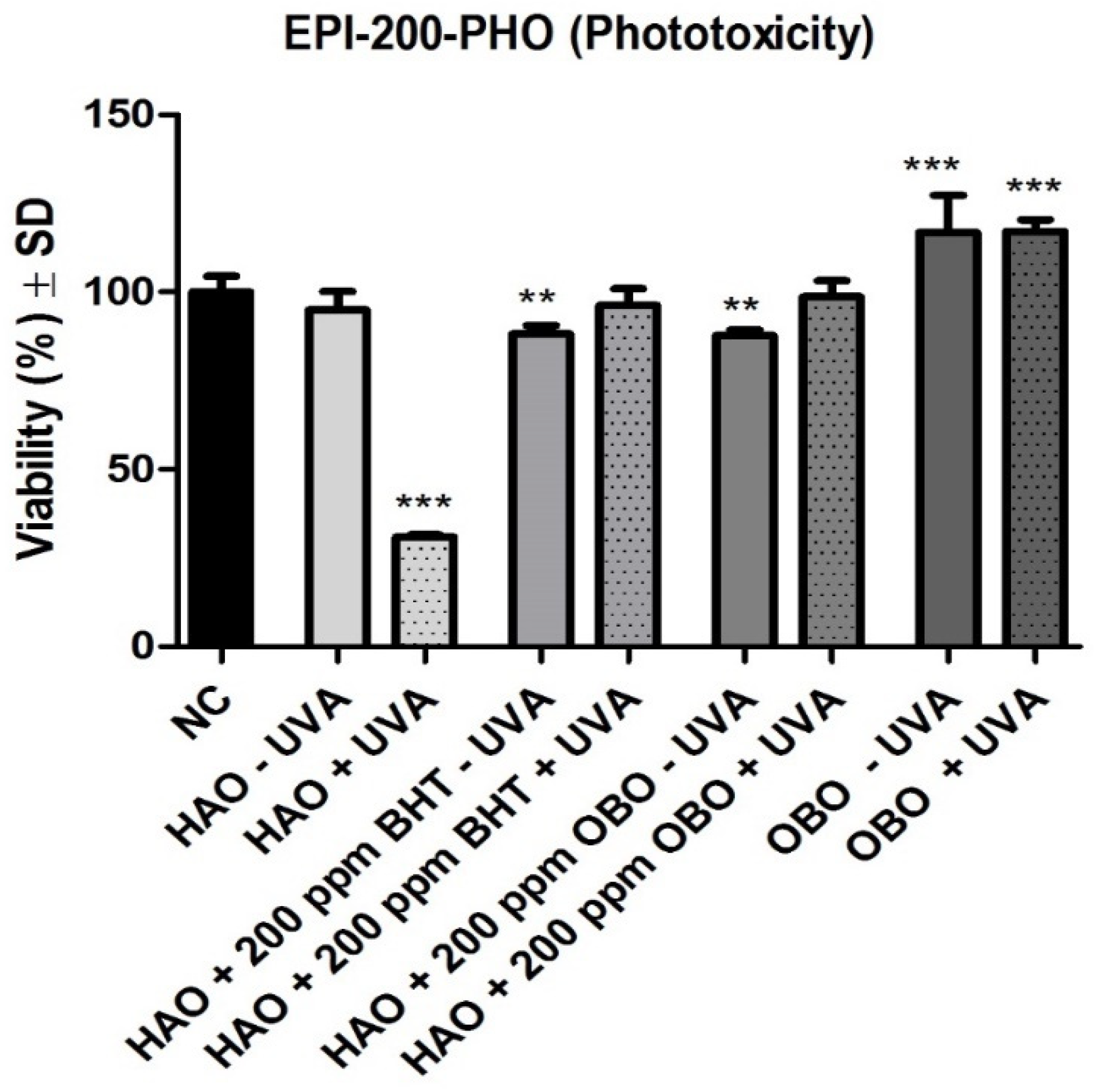
2.5. Histopathological Assessment of EpiDerm Phototoxicity Models with the Tested Oil Samples ± UVA Treatment
3. Discussion
4. Materials and Methods
4.1. Preparation of Oil Samples
4.2. Application of OBO to HAO
4.3. Assessment of Fatty Acid Composition
MUFAs = sum of C16:1 ω9 + C18:1 tr ω9 + C18:1 cis ω9 + C20:1 ω9 + C22:1 ω9 and
PUFAs = sum of C18:2 ω6 + C18:2 cis ω6 + C20:4 ω3 + C18:3 ω3 + C20:5 ω3 + C20:2 ω7
4.4. Thiobarbituric Acid-Reactive Substances Assay
4.5. EpiDerm Skin Irritation Test (OECD TG 439)
Relative viability NC (%) = [ODNC/Mean of ODNC] × 100
Relative viability PC (%) = [ODPC/Mean of ODNC] × 100
4.6. EpiDerm Phototoxicity Test (OECD TG 498)
RTV Control (%) = [OD(vehicle control)/OD(vehicle control)] × 100
4.7. Histopathological Assessment of 3D Tissue Models
4.8. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Bhusnure, O.G.; Shinde, M.C.; Vijayendra, S.S.; Gholve, S.B.; Giram, P.S.; Birajdar, M.J. Phytopharmaceuticals: An Emerging Platform for Innovation and Development of New Drugs from Botanicals. J. Drug Deliv. Ther. 2019, 9, 1046–1057. [Google Scholar]
- Blaak, J.; Staib, P. An Updated Review on Efficacy and Benefits of Sweet Almond, Evening Primrose and Jojoba Oils in Skin Care Applications. Int. J. Cosmet. Sci. 2022, 44, 1–9. [Google Scholar] [CrossRef]
- Danby, S.G.; Alenezi, T.; Sultan, A.; Lavender, T.; Chittock, J.; Brown, K.; Cork, M.J. Effect of Olive and Sunflower Seed Oil on the Adult Skin Barrier: Implications for Neonatal Skin Care. Pediatr. Dermatol. 2013, 30, 42–50. [Google Scholar] [CrossRef]
- Bashir, T.; Zia-Ur-Rehman Mashwani, K.Z.; Haider, S.; Shaista Tabassum, M. 02. Chemistry, Pharmacology and Ethnomedicinal Uses of Helianthus annuus (Sunflower): A Review. Pure Appl. Biol. 2021, 4, 226–235. [Google Scholar] [CrossRef]
- Andrianasolo, F.N.; Debaeke, P.; Champolivier, L.; Maury, P. Analysis and Modelling of the Factors Controlling Seed Oil Concentration in Sunflower: A Review. OCL-Oilseeds Fats Crop. Lipids 2016, 23, D206. [Google Scholar] [CrossRef] [Green Version]
- Spring, O. Sesquiterpene Lactones in Sunflower Oil. LWT-Food Sci. Technol. 2021, 142, 1–5. [Google Scholar] [CrossRef]
- Flagella, Z.; Rotunno, T.; Tarantino, E.; Di Caterina, R.; De Caro, A. Changes in Seed Yield and Oil Fatty Acid Composition of High Oleic Sunflower (Helianthus annuus L.) Hybrids in Relation to the Sowing Date and the Water Regime. Eur. J. Agron. 2002, 17, 221–230. [Google Scholar] [CrossRef]
- Radanović, A.; Miladinović, D.; Cvejić, S.; Jocković, M.; Jocić, S. Sunflower Genetics from Ancestors to Modern Hybrids—A Review. Genes 2018, 9, 528. [Google Scholar] [CrossRef] [Green Version]
- McCance, R.A.; Widdowson, E.M. McCance and Widdowson’s the Composition of Foods; Royal Society of Chemistry: London, UK, 2014. [Google Scholar]
- Blicharska, E.; Komsta, Ł.; Kocjan, R.; Gumieniczek, A.; Kloc, A.; Kaźmierczak, J. Determination of Microelements in Sprouts Grown on Metal-Enriched Solutions by Ion Chromatography. Acta Chromatogr. 2014, 26, 739–747. [Google Scholar]
- Kamal, J. Quantification of Alkaloids, Phenols and Flavonoids in Sunflower (Helianthus annuus L.). African J. Biotechnol. 2011, 10, 3149–3151. [Google Scholar]
- Weisz, G.M.; Kammerer, D.R.; Carle, R. Identification and Quantification of Phenolic Compounds from Sunflower (Helianthus annuus L.) Kernels and Shells by HPLC-DAD/ESI-MSn. Food Chem. 2009, 115, 758–765. [Google Scholar] [CrossRef]
- Amakura, Y.; Yoshimura, M.; Yamakami, S.; Yoshida, T. Isolation of Phenolic Constituents and Characterization of Antioxidant Markers from Sunflower (Helianthus annuus) Seed Extract. Phytochem. Lett. 2013, 6, 302–305. [Google Scholar] [CrossRef]
- Aboki, M.A.; Mohammed, M.; Musa, S.H.; Zuru, B.S.; Aliyu, H.M.; Gero, M.; Alibe, I.M.; Inuwa, B. Physicochemical and Anti-Microbial Properties of Sunflower (Helianthus annuus L.) Seed Oil. Int. J. Sci. Technol. 2012, 2, 151–194. [Google Scholar]
- Anjum, F.M.; Nadeem, M.; Khan, M.I.; Hussain, S. Nutritional and Therapeutic Potential of Sunflower Seeds: A Review. Br. Food J. 2010, 114, 544–552. [Google Scholar] [CrossRef]
- Adeleke, B.S.; Babalola, O.O. Oilseed Crop Sunflower (Helianthus annuus) as a Source of Food: Nutritional and Health Benefits. Food Sci. Nutr. 2020, 8, 4666–4684. [Google Scholar] [CrossRef]
- Vijayakumar, M.; Vasudevan, D.M.; Sundaram, K.R.; Krishnan, S.; Vaidyanathan, K.; Nandakumar, S.; Chandrasekhar, R.; Mathew, N. A Randomized Study of Coconut Oil versus Sunflower Oil on Cardiovascular Risk Factors in Patients with Stable Coronary Heart Disease. Indian Heart J. 2015, 68, 498–506. [Google Scholar] [CrossRef] [Green Version]
- Pal, D. Sunflower (Helianthus annuus L.) Seeds in Health and Nutrition; Elsevier Inc.: Amsterdam, The Netherlands, 2011. [Google Scholar] [CrossRef]
- Stănescu, U.; Hăncianu, M.; Cioancă, O.; Aprotosoaie, A.C.; Miron, A. Plante Medicinale de La A La Z. Monogr. Ale Prod. Interes Ter. 2014, 1, 2. [Google Scholar]
- Montserrat-De La Paz, S.; Fernández-Arche, M.A.; Ángel-Martín, M.; García-Giménez, M.D. Phytochemical Characterization of Potential Nutraceutical Ingredients from Evening Primrose Oil (Oenothera biennis L.). Phytochem. Lett. 2014, 8, 158–162. [Google Scholar] [CrossRef]
- Hudson, B.J.F. Evening Primrose (Oenothera Spp.) Oil and Seed. J. Am. Oil Chem. Soc. 1984, 61, 540–543. [Google Scholar] [CrossRef]
- Ratz-Lyko, A.; Arct, J.; Pytkowska, K.; Majewski, S. In Vivo and Ex Vivo Evaluation of Cosmetic Properties of Seedcakes. J. Cosmet. Laser Ther. 2014, 17, 109–115. [Google Scholar] [CrossRef]
- Mahboubi, M. Evening Primrose (Oenothera biennis) Oil in Management of Female Ailments. J. Menopausal Med. 2019, 25, 74–82. [Google Scholar] [CrossRef]
- Cameron, M.; Gagnier, J.; Chrubasik, S. Herbal Therapy for Treating Rheumatoid Arthritis. Cochrane Database Syst. Rev. 2011, 2, CD002948. [Google Scholar] [CrossRef]
- Jack, A.M.; Keegan, A.; Cotter, M.A.; Cameron, N.E. Effects of Diabetes and Evening Primrose Oil Treatment on Responses of Aorta, Corpus Cavernosum and Mesenteric Vasculature in Rats. Life Sci. 2002, 71, 1863–1877. [Google Scholar] [CrossRef]
- Salaga, M.; Lewandowska, U.; Sosnowska, D.; Zakrzewski, P.; Cygankiewicz, A.; Piechota-Polanczyk, A.; Sobczak, M.; Mosinska, P.; Chen, C.; Krajewska, W.; et al. Polyphenol Extract from Evening Primrose Pomace Alleviates Experimental Colitis after Intracolonic and Oral Administration in Mice. Naunyn-Schmiedeberg’s Arch Pharm. 2014, 387, 1069–1078. [Google Scholar] [CrossRef]
- Singh, S.; Dubey, V.; Singh, D.K.; Fatima, K.; Ahmad, A.; Luqman, S. Antiproliferative and Antimicrobial Efficacy of the Compounds Isolated from the Roots of Oenothera biennis L. J. Pharm. Pharmacol. 2017, 69, 1230–1243. [Google Scholar] [CrossRef]
- Dalla, C.; Padovani, G.; Mainente, F.; Zoccatelli, G.; Bissoli, G.; Mosconi, S.; Veneri, G.; Peruffo, A.; Andrighetto, G.; Rizzi, C.; et al. Anti-Tumour Potential of a Gallic Acid-Containing Phenolic Fraction from Oenothera biennis. Cancer Lett. 2005, 226, 17–25. [Google Scholar] [CrossRef]
- Timoszuk, M.; Bielawska, K.; Skrzydlewska, E. Evening Primrose (Oenothera biennis) Biological Activity Dependent on Chemical Composition. Antioxidants 2018, 7, 108. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Wang, Q.; Li, S.; Xu, Y.; Wang, X.; Wang, C. Carvacrol Methyl Ether, a Compound from the Essential Oil of Gardenia Jasminoides Fruits, Exhibits Antioxidant Effects in the Deep-Frying of Chinese Youmotou Using Sunflower Oil. LWT-Food Sci. Technol. 2020, 128, 109502. [Google Scholar] [CrossRef]
- Jianu, C.; Stoin, D.; Cocan, I.; David, I.; Pop, G.; Lukinich-Gruia, A.T.; Mioc, M.; Mioc, A.; Șoica, C.; Muntean, D.; et al. In Silico and in Vitro Evaluation of the Antimicrobial and Antioxidant Potential of Mentha × Smithiana r. Graham Essential Oil from Western Romania. Foods 2021, 10, 815. [Google Scholar] [CrossRef]
- Pinzaru, I.; Tanase, A.; Enatescu, V.; Coricovac, D.; Bociort, F.; Marcovici, I.; Watz, C.; Vlaia, L.; Soica, C.; Dehelean, C. Proniosomal Gel for Topical Delivery of Rutin: Preparation, Physicochemical Characterization and in Vitro Toxicological Profile Using 3d Reconstructed Human Epidermis Tissue and 2d Cells. Antioxidants 2021, 10, 85. [Google Scholar] [CrossRef]
- Rosa, P.M.; Antoniassi, R.; Freitas, S.C.; Bizzo, H.R.; Zanotto, D.L.; Oliveira, M.F.; Castiglioni, V.B.R. Chemical Composition of Brazilian Sunflower Varieties/Composición Química de Las Variedades de Girasol Brasileñas/Composition Chimique de Sortes de Tournesol Brésiliennes. Helia 2009, 32, 145–156. [Google Scholar] [CrossRef] [Green Version]
- Akkaya, M.R. Fatty Acid Compositions of Sunflowers (Helianthus annuus L.) Grown in East Mediterranean Region. Riv. Ital. delle Sostanze Grasse 2018, 95, 239–247. [Google Scholar]
- Pérez, G.L.; Altamirano, M.T. Indication of Sulflower Oil Concentrated in the Treatment of Atopic Dermatitis. Rev. Alerg. Mex. 2006, 53, 217–225. [Google Scholar]
- Eichenfield, L.F.; McCollum, A.; Msika, P. The Benefits of Sunflower Oleodistillate (SOD) in Pediatric Dermatology. Pediatr. Dermatol. 2009, 26, 669–675. [Google Scholar] [CrossRef]
- Leprán, I.; Szekeres, L. Effect of Dietary Sunflower Seed Oil on the Severity of Reperfusion-Induced Arrhythmias in Anesthetized Rats. J. Cardiovasc. Pharmacol. 1992, 19, 40–44. [Google Scholar] [CrossRef]
- Bester, D.; Esterhuyse, A.J.; Truter, E.J.; Van Rooyen, J. Cardiovascular Effects of Edible Oils: A Comparison between Four Popular Edible Oils. Nutr. Res. Rev. 2010, 23, 334–348. [Google Scholar] [CrossRef]
- Dutta, A.; Dutta, S.K. Vitamin E and Its Role in the Prevention of Atherosclerosis and Carcinogenesis: A Review. J. Am. Coll. Nutr. 2003, 22, 258–268. [Google Scholar] [CrossRef]
- Singh, U.; Devaraj, S.; Jialal, I. Vitamin E, Oxidative Stress, and Inflammation. Annu. Rev. Nutr. 2005, 25, 151. [Google Scholar] [CrossRef]
- Darmstadt, G.L.; Badrawi, N.; Law, P.A.; Alam, A.; Ahmed, S.; Husein, M.H.; Winch, P.; Santosham, M.; Gipson, R. Topical Therapy with Sunflower Seed Oil Prevents Nosocomial Infections and Mortality in Premature Babies in Egypt: A Randomized, Controlled Clinical Trial. Pediatr. Infect. Dis. J. 2004, 23, 719. [Google Scholar] [CrossRef]
- Balch, S.A.; McKenney, C.B.; Auld, D.L. Evaluation of Gamma-Linolenic Acid Composition of Evening Primrose (Oenothera) Species Native to Texas. HortScience 2003, 38, 595–598. [Google Scholar] [CrossRef] [Green Version]
- Chiofalo, B.; Presti, V.L.; Chiofalo, V.; Gresta, F. The Productive Traits, Fatty Acid Profile and Nutritional Indices of Three Lupin (Lupinus Spp.) Species Cultivated in a Mediterranean Environment for the Livestock. Anim. Feed Sci. Technol. 2012, 171, 230–239. [Google Scholar] [CrossRef]
- Belitz, H.-D.; Grosch, W. Legumes. In Food Chemistry; Springer: Berlin/Heidelberg, Germany, 1999; pp. 693–715. [Google Scholar] [CrossRef]
- Simopoulos, A.P. Importance of the Ratio of Omega-6/Omega-3 Essential Fatty Acids: Evolutionary Aspects. In Omega-6/Omega-3 Essential Fatty Acid Ratio: The Scientific Evidence; The Scientific Evidence: Basel, Switzerland, 2003; Volume 92, pp. 1–22. [Google Scholar]
- Cocan, I.; Negrea, M.; Cozma, A.; Alexa, E.; Poiana, M.; Raba, D.; Danciu, C.; Popescu, I.; Cadariu, A.I.; Obistioiu, D.; et al. Chili and Sweet Pepper Seed Oil Used as a Natural Antioxidant to Improve the Thermo-Oxidative Stability of Sunflower Oil. Agronomy 2021, 11, 2579. [Google Scholar] [CrossRef]
- Wang, D.; Fan, W.; Guan, Y.; Huang, H.; Yi, T.; Ji, J. Oxidative Stability of Sunflower Oil Flavored by Essential Oil from Coriandrum Sativum L. during Accelerated Storage. LWT-Food Sci. Technol. 2018, 98, 268–275. [Google Scholar] [CrossRef] [Green Version]
- Iqbal, S.; Haleem, S.; Akhtar, M.; Zia-ul-Haq, M.; Akbar, J. Efficiency of Pomegranate Peel Extracts in Stabilization of Sunflower Oil under Accelerated Conditions. Food Res. Int. 2008, 41, 194–200. [Google Scholar] [CrossRef]
- Wang, Z.; Wu, Z.; Zuo, G.; Lim, S.S.; Yan, H. Defatted Seeds of Oenothera Biennis as a Potential Functional Food Ingredient for Diabetes. Foods 2021, 10, 538. [Google Scholar] [CrossRef]
- Sielicka, M.; Małecka, M.; Purłan, M. Comparison of the Antioxidant Capacity of Lipid-soluble Compounds in Selected Cold-pressed Oils Using Photochemiluminescence Assay (PCL) and DPPH Method. Eur. J. Lipid Sci. Technol. 2014, 116, 388–394. [Google Scholar] [CrossRef]
- Rhazi, L.; Depeint, F.; Ayerdi Gotor, A. Loss in the Intrinsic Quality and the Antioxidant Activity of Sunflower (Helianthus annuus L.) Oil during an Industrial Refining Process. Molecules 2022, 27, 916. [Google Scholar] [CrossRef]
- Granica, S.; Czerwińska, M.E.; Piwowarski, J.P.; Ziaja, M.; Kiss, A.K. Chemical Composition, Antioxidative and Anti-Inflammatory Activity of Extracts Prepared from Aerial Parts of Oenothera biennis L. and Oenothera Paradoxa Hudziok Obtained after Seeds Cultivation. J. Agric. Food Chem. 2013, 61, 801–810. [Google Scholar] [CrossRef]
- Mescher, A.L. Junqueira’s Basic Histology: Text and Atlas, 14th ed.; McGraw-Hill Medical: New York, NY, USA, 2016. [Google Scholar]
- Bamford, J.; Ray, S.; Musekiwa, A.; van Gool, C.; Humphreys, R.; Ernst, E. Oral Evening Primrose Oil and Borage Oil for Eczema. Cochrane Database Syst. Rev. 2013, 2020, CD004416. [Google Scholar] [CrossRef]
- Schlichte, M.; Vandersall, A.; Katta, R. Diet and Eczema: A Review of Dietary Supplements for the Treatment of Atopic Dermatitis. Dermatol. Pract. Concept. 2016, 6, 23–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chung, B.Y.; Kim, J.H.; Cho, S.I.; Ahn, I.S.; Kim, H.O.; Park, C.W.; Lee, C.H. Dose-Dependent Effects of Evening Primrose Oil in Children and Adolescents with Atopic Dermatitis. Ann. Dermatol. 2013, 25, 285–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, T.H.; Kim, W.J.; Park, S.Y.; Kim, H.; Chung, D.K. In Vitro Anti-Wrinkle and Skin-Moisturizing Effects of Evening Primrose (Oenothera biennis) Sprout and Identification of Its Active Components. Processes 2021, 9, 145. [Google Scholar] [CrossRef]
- Karagounis, T.K.; Gittler, J.K.; Rotemberg, V.; Morel, K.D. Use of “Natural” Oils for Moisturization: Review of Olive, Coconut, and Sunflower Seed Oil. Pediatr. Dermatol. 2019, 36, 9–15. [Google Scholar] [CrossRef] [Green Version]
- Blaess, M.; Deigner, H.P. Derailed Ceramide Metabolism in Atopic Dermatitis (AD): A Causal Starting Point for a Personalized (Basic) Therapy. Int. J. Mol. Sci. 2019, 20, 3967. [Google Scholar] [CrossRef] [Green Version]
- Liu, M.; Li, X.; Chen, X.Y.; Xue, F.; Zheng, J. Topical Application of a Linoleic Acid-Ceramide Containing Moisturizer Exhibit Therapeutic and Preventive Benefits for Psoriasis Vulgaris: A Randomized Controlled Trial. Dermatol. Ther. 2015, 28, 373–382. [Google Scholar] [CrossRef]
- Cho, K.H.; Kang, D.J.; Nam, H.S.; Kim, J.H.; Kim, S.Y.; Lee, J.O.; Kim, B.J. Ozonated Sunflower Oil Exerted Protective Effect for Embryo and Cell Survival via Potent Reduction Power and Antioxidant Activity in HDL with Strong Antimicrobial Activity. Antioxidants 2021, 10, 1651. [Google Scholar] [CrossRef]
- Mukherjee, S.; Yang, L.; Vincent, C.; Lei, X.; Ottaviani, M.F.; Ananthapadmanabhan, K.P. A Comparison between Interactions of Triglyceride Oil and Mineral Oil with Proteins and Their Ability to Reduce Cleanser Surfactant- Induced Irritation. Int. J. Cosmet. Sci. 2015, 37, 371–378. [Google Scholar] [CrossRef]
- Freitas, L.M.; Antunes, F.T.T.; Obach, E.S.; Correa, A.P.; Wiiland, E.; de Mello Feliciano, L.; Reinicke, A.; Amado, G.J.V.; Grivicich, I.; Fialho, M.F.P.; et al. Anti-Inflammatory Effects of a Topical Emulsion Containing Helianthus annuus Oil, Glycerin, and Vitamin B3 in Mice. J. Pharm. Investig. 2021, 51, 223–232. [Google Scholar] [CrossRef]
- Tamara, N.; Angkasa, C.; Ginting, C.N.; Chiuman, L.; Lister, I.N.E. Determination Sunscreen Potential Based on Sunflower Seed Oil (Helianthus annuus) in Cream Preparation With Combination of Oxybenzone and Octyl Methoxycinnamate by in Vitro Method. Am. Sci. Res. J. Eng. Technol. Sci. 2019, 60, 33–39. [Google Scholar]
- Kawamura, A.; Ooyama, K.; Kojima, K.; Kachi, H.; Abe, T.; Amano, K.; Aoyama, T. Dietary Supplementation of Gamma-Linolenic Acid Improves Skin Parameters in Subjects with Dry Skin and Mild Atopic Dermatitis. J. Oleo Sci. 2011, 607, 597–607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Senapati, S.; Banerjee, S.; Gangopadhyay, D.N. Evening Primrose Oil Is Effective in Atopic Dermatitis: A Randomized Placebo-Controlled Trial. Indian J. Dermatol. Venereol. Leprol. 2008, 74, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Muggli, R. Systemic Evening Primrose Oil Improves the Biophysical Skin Parameters of Healthy Adults. Int. J. Cosmet. Sci. 2005, 27, 243–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, K.Y.; Ko, E.J.; Kim, I.S.; Li, K.; Kim, B.J.; Seo, S.J.; Kim, M.N.; Hong, C.K. The Effect of Evening Primrose Oil for the Prevention of Xerotic Cheilitis in Acne Patients Being Treated with Isotretinoin: A Pilot Study. Ann. Dermatol. 2014, 26, 706–712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fecker, R.; Buda, V.; Alexa, E.; Avram, S.; Pavel, I.Z.; Muntean, D.; Cocan, I.; Watz, C.; Minda, D.; Dehelean, C.A.; et al. Phytochemical and Biological Screening of Oenothera biennis L. Hydroalcoholic Extract. Biomolecules 2020, 10, 818. [Google Scholar] [CrossRef]
- Cho, H.; Lee, M.; Lee, J.; No, K.; Park, S.; Lee, H.; Kang, S.; Cho, W.; Park, H.; Oh, K.; et al. Anti-Wrinkling Effects of the Mixture of Vitamin C, Vitamin E, Pycnogenol and Evening Primrose Oil, and Molecular Mechanisms on Hairless Mouse Skin Caused by Chronic Ultraviolet B Irradiation. Photodermatol. Photoimmunol. Photomed. 2007, 23, 155–162. [Google Scholar] [CrossRef]
- Koo, J.H.; Lee, I.; Yun, S.K.; Kim, H.U.; Park, B.H.; Park, J.W. Saponified Evening Primrose Oil Reduces Melanogenesis in B16 Melanoma Cells and Reduces UV-Induced Skin Pigmentation in Humans. Lipids 2010, 45, 401–407. [Google Scholar] [CrossRef]
- Poșta, D.S.; Radulov, I.; Cocan, I.; Berbecea, A.A.; Alexa, E.; Hotea, I.; Iordănescu, O.A.; Băla, M.; Cântar, I.C.; Rózsa, S. Hazelnuts (Corylus avellana L.) from Spontaneous Flora of the West Part of Romania: A Source of Nutrients for Locals. Agronomy 2022, 12, 214. [Google Scholar] [CrossRef]
- Ulbricht, T.L.V.; Southgate, D.A.T. Coronary Heart Disease: Seven Dietary Factors. Lancet 1991, 338, 985–992. [Google Scholar]
- Wasowicz, E.; Gramza, A.; Hes, M.; Jelen, H.; Korczak, J.; Malecka, M.; Mildner-Szkudlarz, S.; Rudzinska, M.; Samotyja, U.; Zawirska-Wojtasiak, R. Oxidation of Lipids in Food. Polish J. Food Nutr. Sci. 2004, 13/54, 87–100. [Google Scholar]
- Gordon, M.H. Measuring Antioxidant Activity. In Antioxidants in Food; Woodhead Publishing: Cambridge, UK, 2001; pp. 71–80. [Google Scholar]
- Kikuzaki, H.; Nakatani, N. Antioxidant Effects of Some Ginger Constituents. J. Food Sci. 1993, 58, 1407–1410. [Google Scholar] [CrossRef]
- Tarladgis, B.G.; Watts, B.M.; Margaret, Y.T. A Distillation Method for the Quantitative Determination of Malonaldehyde in Rancid Foods. J. Am. Oil Chem. Soc. 1960, 37, 44–48. [Google Scholar] [CrossRef]
- Skin Irritation Test (SIT) OECD TG 439|MatTek Corporation. Available online: https://www.mattek.com/application/skin-irritation-test-oecd-439/ (accessed on 28 September 2022).
- Phototoxicity|MatTek Corporation. Available online: https://www.mattek.com/application/phototoxicity/ (accessed on 28 September 2022).


| Shorthand Nomenclature | Type of Fatty Acid | Fatty Acids Systematic Names | Fatty Acids TRIVIAL Name | Retention Time | HAO g/100 g Total Fatty Acids | OBO g/100 g Total Fatty Acids |
|---|---|---|---|---|---|---|
| C12:0 | - | Dodecanoic acid, methyl ester | Lauric acid | 23.156 | nd | 0.154 ± 0.003 |
| C13:0 | - | Tridecanoic acid, methyl ester | Ginkgolic acid | 27.001 | nd | 0.147 ± 0.004 |
| C14:0 | - | Methyl tetradecanoate | Myristic acid | 30.343 | nd | 0.325 ± 0.007 |
| C15:0 | - | Pentadecanoic acid, 14-methyl-, methyl ester | Pentadecylic acid | 35.994 | nd | ω0.281 ± 0.008 |
| C16:0 | - | Hexadecanoic acid, methyl ester | Palmitic acid | 36.473 | 7.179 ± 0.123 a | 6.205 ± 0.156 b |
| C17:0 | - | Heptadecanoic acid, methyl ester | Margaric acid | 38.719 | nd | 0.033 ± 0.001 |
| C18:0 | - | Octadecanoic acid, methyl ester | Stearic acid | 40.969 | 3.586 ± 0.110 a | 2.039 ± 0.057 b |
| C20:0 | - | Eicosanoic acid, methyl ester | Arachidic acid | 45.004 | 0.138 ± 0.001 a | 0.275 ± 0.008 b |
| C22:0 | - | Docosanoic acid, methyl ester | Acid behenic | 48.767 | 0.548 ± 0.003 a | 0.069 ± 0.002 b |
| C24:0 | - | Tetracosanoic acid, methyl ester | Lignoceric acid | 52.275 | nd | 0.030 ± 0.001 |
| C16:1 | ω9 | 9-Hexadecenoic acid, methyl ester, (Z)- | Palmitoleic acid | 38.014 | 0.158 ± 0.001 a | 0.094 ± 0.004 b |
| C18:1 tr | ω9 | 9-Octadecenoic acid, methyl ester, € | Elaidic acid | 42.054 | nd | 0.119 ± 0.006 |
| C18:1 cis | ω9 | 9-Octadecenoic acid (Z)-, methyl ester | Oleic acid, cis | 42.251 | 28.249 ± 1.322 a | 7.175 ± 0.141 b |
| C20:1 | ω9 | 11-Eicosenoic acid, methyl ester | 11-Eicosenoic acid | 46.201 | nd | 0.210 ± 0.007 |
| C22:1 | ω9 | 13-Docosenoic acid, methyl ester, (Z)- | Acid erucic | 49.901 | nd | 0.040 ± 0.002 |
| C18:2n6 trans | ω6 | 9,12-Octadecadienoic acid, methyl ester | Linoleic acid | 44.045 | nd | 0.050 ± 0.003 |
| C18:2n6 cis | ω6 | 9,12-Octadecadienoic acid (Z,Z)-, methyl ester | Linoleic acid, cis | 44.324 | 59.941 ± 4.511 a | 72.093 ± 1.414 b |
| C20:4 | ω3 | Methyl (Z)-5,11,14,17-eicosatetraenoate | Arachidonic acid | 45.623 | nd | 9.812 ± 0.156 |
| C18:3 | ω3 | 9,12,15-Octadecatrienoic acid, methyl ester | Acid linolenic | 46.371 | 0.208 ± 0.002 a | 0.233 ± 0.014 a |
| C20:5 | ω3 | Methyl eicosa-5,8,11,14,17-pentaenoate | cis-5,8,11,14,17-Eicosapentaenoic acid | 47.800 | nd | 0.033 ± 0.001 |
| C20:2 | ω7 | 11,13-Eicosadienoic acid, methyl ester | 11,13-Eicosadienoic acid | 48.034 | nd | 0.026 ± 0.001 |
| * Until 100% other compounds | * Until 100% other compounds |
| Sample | SFAs g/100 g Total Fatty Acids | MUFAs g/100 g Total Fatty Acids | PUFAs ω6 g/100 g Total Fatty Acids | PUFAs ω3 g/100 g Total Fatty Acids | UFA/SFA | PUFA/SFA | PUFA ω3/ ω6 | AI | TI |
|---|---|---|---|---|---|---|---|---|---|
| HAO | 11.451 | 28.407 | 59.941 | 0.208 | 7.733 | 5.252 | 0.003 | 0.087 | 0.240 |
| OBO | 9.49 | 8.196 | 72.143 | 10.078 | 9.530 | 8.664 | 0.140 | 0.085 | 0.188 |
| TBA (μg MDA/g) | Day 1 | Day 5 | Day 10 | Day 15 | Day 20 | Day 25 | Day 30 |
|---|---|---|---|---|---|---|---|
| HAO | 2.500 ± 0.105 a | 9.387 ± 0.276 a | 11.117 ± 0.241 a | 15.310 ± 0.376 a | 19.393 ± 0.382 a | 26.373 ± 0.396 a | 30.097 ± 0.630 a |
| HAO + 200 ppm BHT | 2.373 ± 0.168 a | 4.937 ± 0.195 b | 7.997 ± 0.175 b | 9.907 ± 0.570 b | 14.827 ± 0.403 b | 20.460 ± 0.901 b | 24.517 ± 0.411 b |
| HAO + 100 ppm OBO | 2.477 ± 0.085 a | 8.607 ± 0.253 c | 10.600 ± 0.335 a | 14.533 ± 0.387 a | 18.770 ± 0.575 a | 26.200 ± 0.383 a | 29.103 ± 0.523 a |
| HAO + 200 ppm OBO | 2.460 ± 0.061 a | 7.497 ± 0.313 d | 9.573 ± 0.182 c | 13.313 ± 0.409 c | 16.350 ± 0.342 c | 24.713 ± 0.421 c | 27.107 ± 0.329 c |
| HAO + 300 ppm OBO | 2.440 ± 0.070 a | 6.593 ± 0.268 e | 8.967 ± 0.289 d | 11.557 ± 0.280 d | 15.370 ± 0.223 d | 23.500 ± 0.471 d | 26.590 ± 0.334 c |
| HAO + 500 ppm OBO | 2.400 ± 0.195 a | 5.543 ± 0.214 b | 8.527 ± 0.278 b,d | 9.830 ± 0.255 b | 14.647 ± 0.320 b | 21.027 ± 0.523 b | 24.583 ± 0.511 b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fecker, R.; Magyari-Pavel, I.Z.; Cocan, I.; Alexa, E.; Popescu, I.M.; Lombrea, A.; Bora, L.; Dehelean, C.A.; Buda, V.; Folescu, R.; et al. Oxidative Stability and Protective Effect of the Mixture between Helianthus annuus L. and Oenothera biennis L. Oils on 3D Tissue Models of Skin Irritation and Phototoxicity. Plants 2022, 11, 2977. https://doi.org/10.3390/plants11212977
Fecker R, Magyari-Pavel IZ, Cocan I, Alexa E, Popescu IM, Lombrea A, Bora L, Dehelean CA, Buda V, Folescu R, et al. Oxidative Stability and Protective Effect of the Mixture between Helianthus annuus L. and Oenothera biennis L. Oils on 3D Tissue Models of Skin Irritation and Phototoxicity. Plants. 2022; 11(21):2977. https://doi.org/10.3390/plants11212977
Chicago/Turabian StyleFecker, Ramona, Ioana Zinuca Magyari-Pavel, Ileana Cocan, Ersilia Alexa, Iuliana Maria Popescu, Adelina Lombrea, Larisa Bora, Cristina Adriana Dehelean, Valentina Buda, Roxana Folescu, and et al. 2022. "Oxidative Stability and Protective Effect of the Mixture between Helianthus annuus L. and Oenothera biennis L. Oils on 3D Tissue Models of Skin Irritation and Phototoxicity" Plants 11, no. 21: 2977. https://doi.org/10.3390/plants11212977










