Abstract
Skin disorders are a worldwide health problem that normally affect human life. A traditional healer is an important expert in researching notable medicinal plants for skin disease treatment. This study aimed to determine the traditional knowledge and the use of medicinal plants for the treatment of skin diseases among traditional healers in the Songkhla province, Thailand. The ethnobotanical information was collected from experienced traditional healers by semi-structured interviews and participant observations. Plant specimens were also collected and identified using the standard taxonomic method. The data were analyzed by interpretation and descriptive statistics. Twenty-five polyherbal formulations for the treatment of skin diseases were obtained from traditional healers with at least 10 years of experience. A total of 66 plant species in 38 families were documented. Leaves and trees were the most commonly employed plant parts and plant habits included in the herbal remedies, respectively. Fabaceae, Rubiaceae, and Zingiberaceae were the majority of the cited families. Oryza sativa L. and Zingiber montanum (J. Koenig) Link ex A.Dietr. were the most preferred plants combined in the prescriptions, which had the highest use value (UV = 0.83). The highest relative frequency of citation was represented by Curcuma longa L., Eurycoma longifolia Jack, Knema globularia (Lamk.) Warb, and Senna siamea (Lam.) Irwin & Barneby. (0.55 each). This research suggests the importance of traditional healers in the healing of skin diseases with herbal remedies. A variety of medicinal plants are used in the prescriptions for the treatment of skin disorders in the Songkhla province, in the south of Thailand. Pharmacological and toxicological activities as well as phytochemical constituents of polyherbal remedies should be further investigated to scientifically verify further applications of widely practiced herbal medicines.
1. Introduction
Skin disease is a global public health problem that often has physiological, psychological, and social impacts [1]. The occurrence of skin diseases usually affects human health, from newborns to elderly people. Common skin diseases impact global distribution both in resource-poor areas and advanced economic settings. Scabies and pyoderma are examples of skin diseases in resource-poor settings. Skin disorders such as atopic eczema, psoriasis, skin ulcers, and pruritus are commonly distributed in both resource-poor areas and advanced economic settings [2]. Infectious skin diseases include a variety of conditions ranging in severity. The clinical presentation and the pattern of infectious skin diseases depend on the type of causative pathogen, the layers and structures of the skin, and the underlying medical condition of the patient [3]. Although the prescribed accessible drugs have been applied for the medication of skin diseases, many adverse effects of the drugs, for example skin irritation, erythema, pruritus, staining, and skin cancers can possibly occur [4].
Natural products and traditional medicines are valuable for the treatment and prevention of various diseases [5]. They are gaining popularity as alternative treatments for common skin conditions [6]. Natural medicines from plants have been continuously prominent due to many advantages, including fewer side effects, being inexpensive, and acceptable use for a long time. Moreover, medicinal plants are also applicable raw materials for the synthesis of novel therapeutic agents. Several plants, such as Aloe vera (L.) Burm.f., Azadirachta indica A.Juss., Calendula officinalis L., Cannabis sativa L., Portulaca amilis Speg., and others, have been investigated for the treatment of skin diseases ranging from itching to skin cancer and have been reported to be effective in various skin diseases [7]. One hundred and six plant species are utilized in the local communities of Northern Pakistan to treat skin problems such as wound healing, skin burns, boils, pimples, inflammatory abscesses, etc. [8].
Phytochemical substances are found in plants that are utilized to treat skin problems. Plant constituents, or phytoconstituents, are divided into primary and secondary metabolites depending on their activity in a basic metabolic process. Secondary metabolites have been demonstrated to have a variety of biological effects, providing a scientific foundation for the use of herbs in traditional medicine in many ancient cultures. Secondary metabolite classes include phenolics, lipids, saponins, carbohydrates, alkaloids, and terpenes according to their chemical structures [9]. Some phytochemical compounds used to treat skin diseases, including mangiferin, lutein, curcumin, resveratrol, embelin, naringenin, quercetin, lycopene, gingerol, and apigenin, as well as their mechanism of action against skin disorders such as inflammation reduction, reduction of skin infection, wound healing, treating skin cancer, and reducing skin aging have been reviewed [10].
Traditional healers are significant for public health in Thai communities, and many individuals have confidence in the healing attributes of herbal medicine [11]. The folk healer is one of the important sources for determining the use of herbal medicine for treating people in the local area, and it will be the initiation process for searching for the prominent plants. This study focused on the Songkhla province due to its large area in the south of Thailand. Although elderly folk healers in Songkhla actively cooperated, their wisdom has been transferred in a limited manner [12]. The ethnomedicinal surveys on plants used for disease treatment in Songkhla were documented [12,13,14,15]. However, there is no systematic ethnomedicinal study attended to polyherbal prescriptions used by traditional healers for the remedy of skin disorders in this area. This study aimed to determine the traditional knowledge and examine the utilization of medicinal plants for skin disease treatment by traditional healers in the Songkhla province, in the south of Thailand.
2. Results and Discussion
2.1. Socio-Demographic Characteristics of Informants
Traditional medicines as well as herbal medicines have been used for health care in Southeast Asia and other global regions. They have been established and have developed empirical experience. This wisdom and knowledge are part of the social and cultural heritage of people and countries and can be passed from one generation to another [16]. In this study, six traditional healers participated. All professional folk healers were males. The informants were divided into three age groups, including 50–59 (16.7%), 60–69 (33.3%), and over 70 (50%) (Table 1). This finding is similar to a previous study that reported the majority of experienced healers were males aged 69–79 years old [8]. Based on education, fifty percent of the participants had graduated from primary school, while 16.7% in each group were secondary school, vocational diploma, and bachelor’s degree holders. The majority of the informants were Buddhists. In the past, Thai men had more opportunities to be educated than women. Additionally, Buddhist males had a chance to enter the monkhood. They could be the causes of men’s ability to write and read. Moreover, men take their duty of obtaining plant materials for their family’s living, leading to intensive experience in plant utilization [17].

Table 1.
Demographical characteristics of experienced traditional healers in the Songkhla province, Thailand.
2.2. Prescriptions of Polyherbal Remedies Applied for the Treatment of Skin Diseases
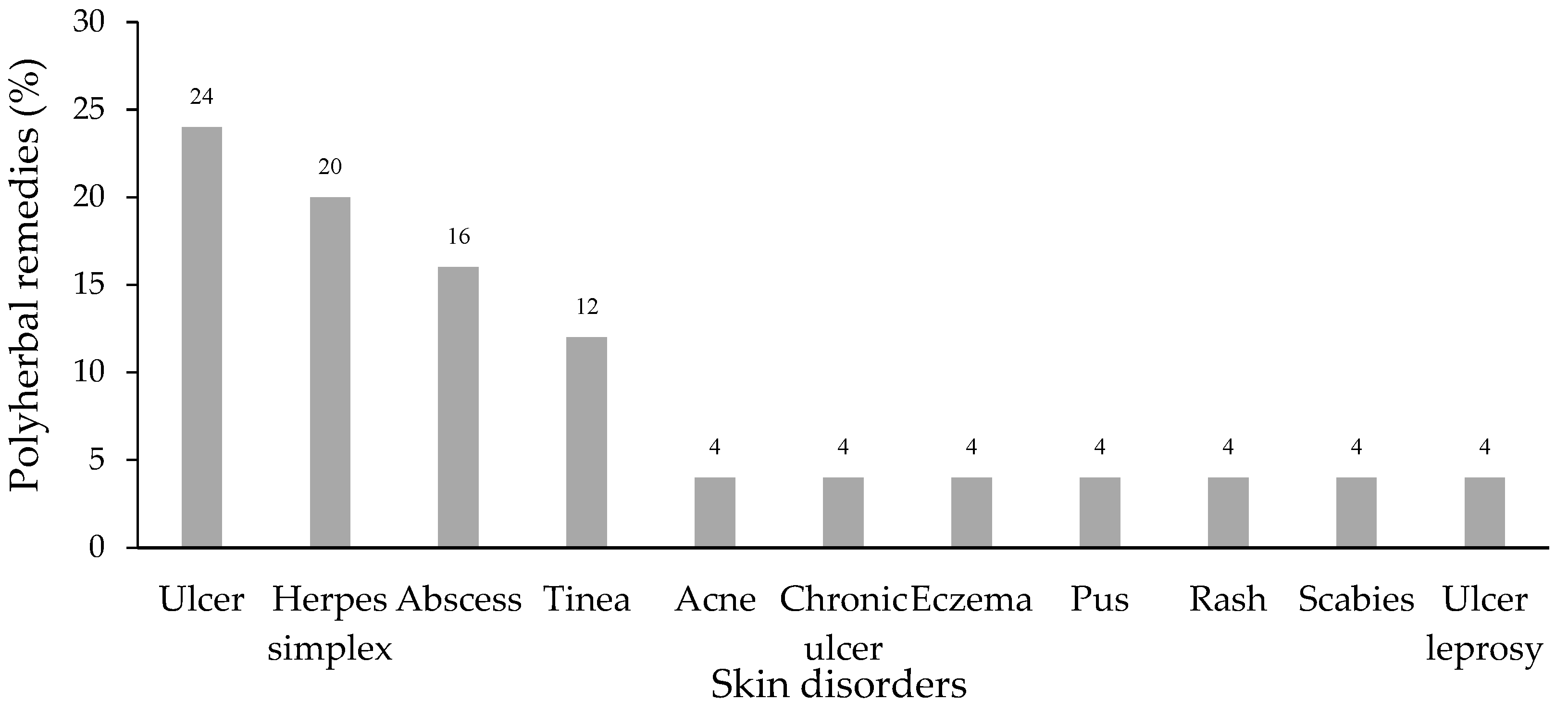
Twenty-five polyherbal remedies obtained from the folk healers were used to treat skin disorders including ulcers (24%), herpes simplex (20%), abscesses (16%), and tinea (12%). The rest of the treated skin diseases are presented in Figure 1.
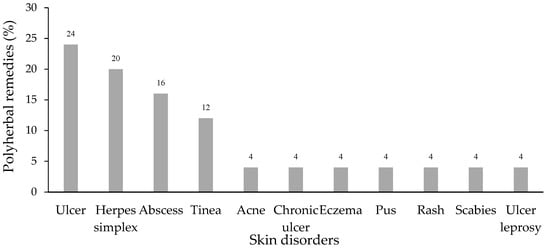
Figure 1.
Skin disorders treated by polyherbal remedies.
The information from the prescriptions in Table 2 showed that twenty-two formulations (81.8%) were applied for microbial skin infectious diseases, including bacterial infections such as ulcers, abscesses, acne, and pus, viral infections (herpes simplex), and fungal infections (tinea). The traditional healers possessed the medical expertise to formulate the herbal medicine for the treatment of each patient. The polyherbal prescription was defined by the combination of each plant at equal weight. Many diseases can be healed using one or a combination of plants as a synergistic effect. In addition, the plant’s scientific name, local name, family, and plant part used are also shown in Table 2.

Table 2.
Polyherbal remedies used by traditional healers for the treatment of skin diseases in the Songkhla province, Thailand.
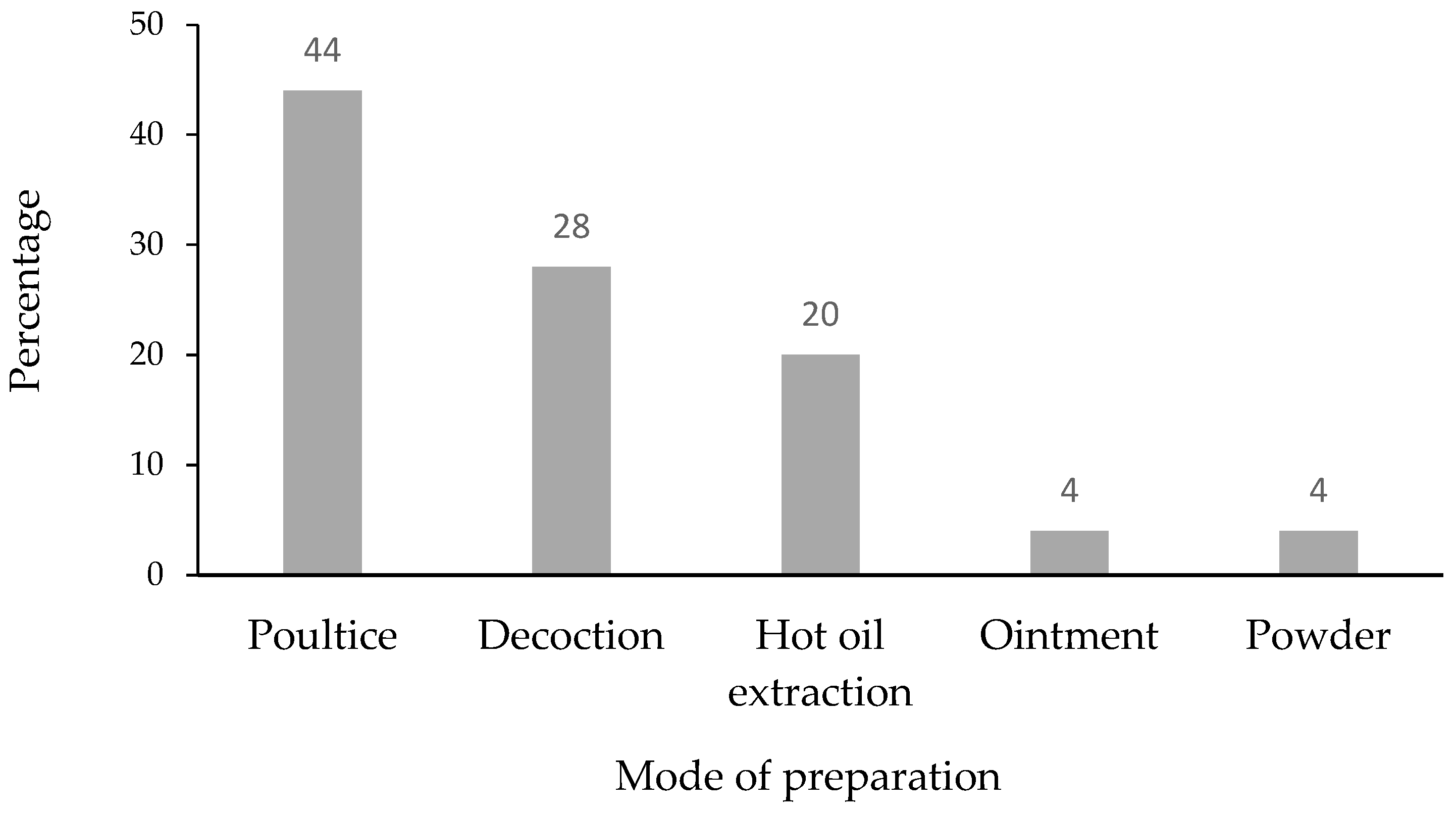
The traditional preparations of the remedies were made by poultice (44%), decoction (28%), hot oil extraction (20%), ointment (4%) and powder (4%) as shown in Figure 2. A variety of medicinal plant preparation methods for skin disorder treatment, such as powder, paste, oil, infusion, decoction, and concoction, have been documented in many ethnobotanical surveys [8,18,19]. The poultice was the most famous preparation method applied to the patients in this study. It might be due to the convenient preparation used for topical skin disease treatment.
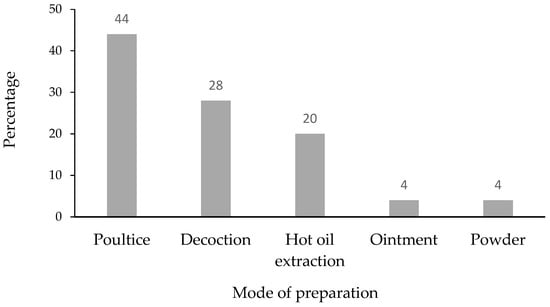
Figure 2.
Mode of preparation of polyherbal prescriptions used by traditional healers.
2.3. The Habits of Medicinal Plants and the Plant Part Used
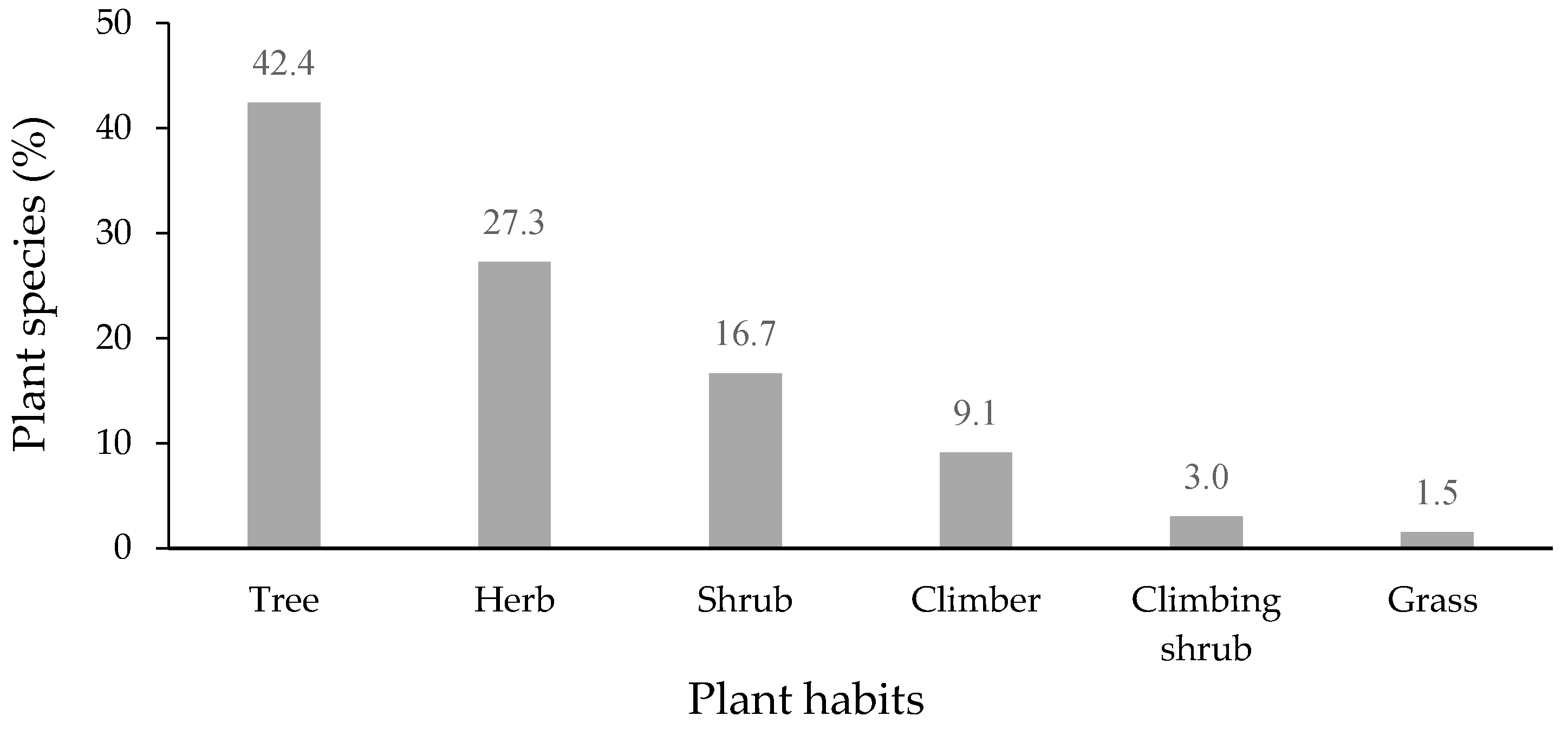
All plant species in the 25 polyherbal remedies were classified into six habits (Figure 3). Trees (42.4%) were found to be the most commonly used plant habit included in herbal remedies, followed by herbs (27.3%), shrubs (16.7%), and climbers (9.1%). Trees were the most preferable plant habit used in polyherbal prescriptions, which was consistent with the habits of medicinal plants from a previous study in the Songkhla province [12].
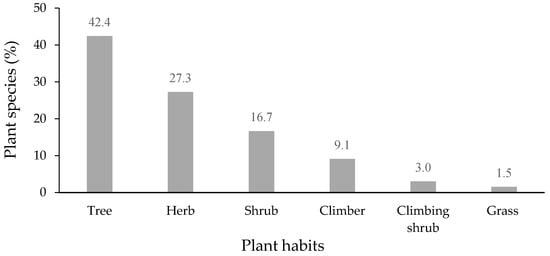
Figure 3.
Habit of plants in polyherbal remedies used for the treatment of skin diseases (n = 66).
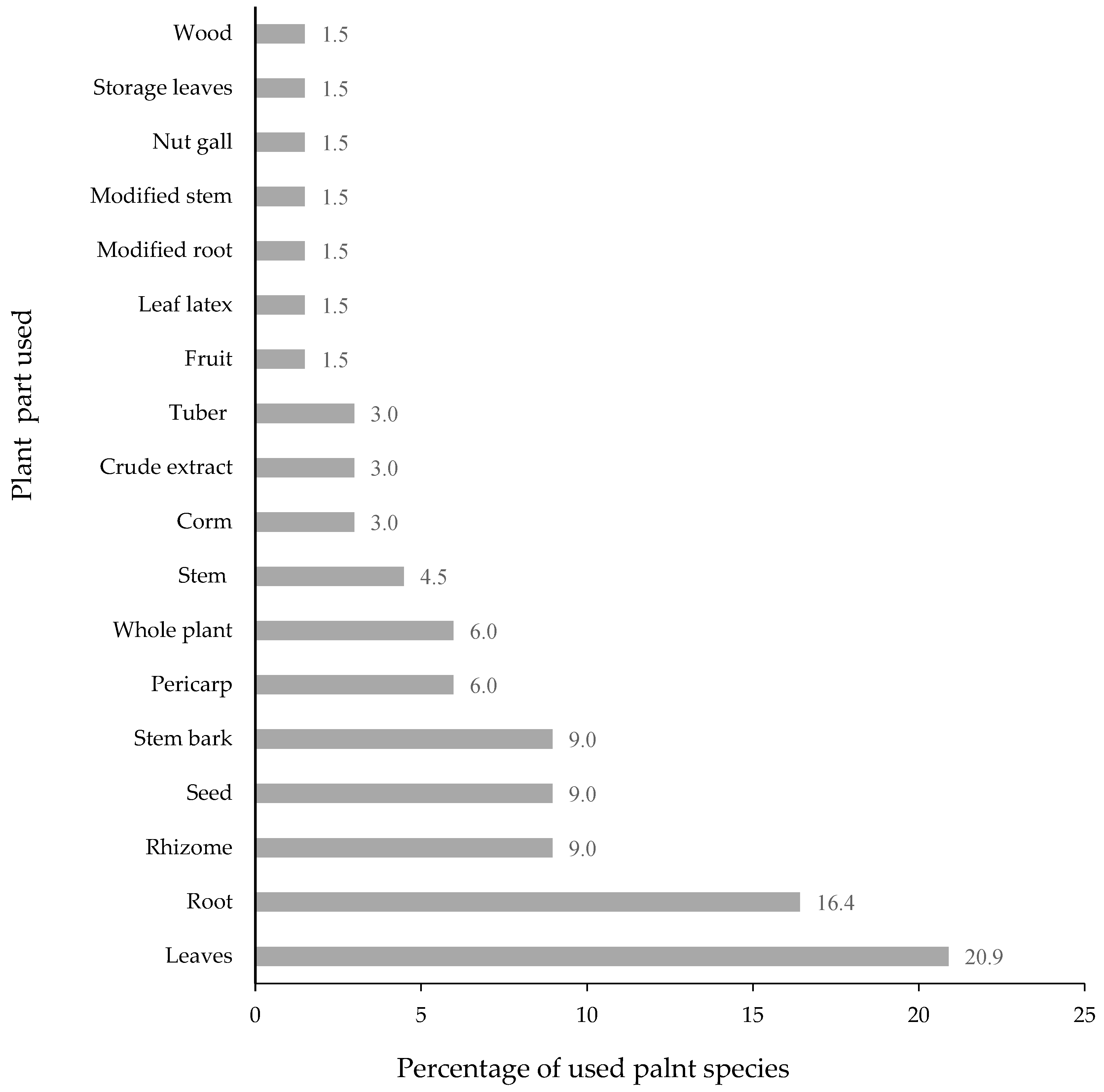
Sixteen different plant parts were used in the polyherbal formulations for skin infection. Leaves were the most frequently used part (20.9%), followed by roots (16.4%), rhizomes (9.0%), seeds (9.0%), and stem bark (9%). The rest of the parts used of the plants are shown in Figure 4. In many reports [8,20], as well as in this study, leaves were the major plant part used for skin disease treatment. It could be due to the fact that the collection of leaves is easier than that of other parts, such as roots, seeds, bark, and rhizomes, and they are harvested every season. Another reason might be that leaves are soft and the chemical contents might be readily extracted [12].
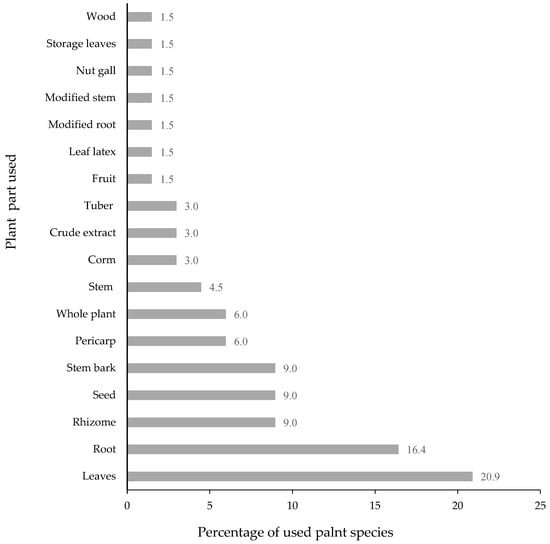
Figure 4.
Plant part used in herbal remedies for skin diseases (n = 66).
2.4. A Variety of Plant Materials Used in Polyherbal Remedies for Skin Disorders
Totally, 66 plant species and one animal material (Sepia spp. cuttlebone) were included in the 25 prescriptions of herbal remedies. The plants were classified into 61 genera and 38 families (Table 2). In regard to the numbers of plant species used in the families, Fabaceae, Rubiaceae, and Zingiberaceae (7.6%) were the most notable families, followed by Acanthaceae (6.1%), as shown in Table 3. The plants in the Fabaceae family included Acacia catechu (L.f.) Willd., Entada rheedii Spreng., Pterocarpus indicus Willd., Senna alata (L.) Roxb., and Senna siamea (Lam.) Irwin & Barneby. Mitragyna speciosa (Roxb.) Korth., Uncaria gambir (Hunter) Roxb., Prismatomeris tetrandra (Roxb.) K. Schum, Hydnophytum formicarium Jack, and Ceriscoides turgida (Roxb.) Tirveng. were in Rubiaceae, while those in the Zingiberaceae consisted of Zingiber montanum (J.Koenig) Link ex A.Dietr., Curcuma zedoaria (L.) Roscoeex Sm., Curcuma longa L., Zingiber zerumbet (L.) Roscoeex Sm., and Curcuma aromatica Salisb. Fabaceae and Zingiberaceae are well known among plants used in traditional medicine. The study of medicinal plants used in Thai traditional medicine in modern healthcare services reported 89 medicinal plant species. The plants belonged to 37 families, with the highest numbers of medicinal plant species being Zingiberaceae (11 species) and Fabaceae (10 species) [21]. Similarly, Zingiberaceae, Fabaceae, and Rubiaceae were the major families of plant species used and cited by traditional healers in the Patthalung province, in the south of Thailand [11]. In addition, five plant species in the Fabaceae family and three species in the Rubiaceae family were used in herbal remedies for skin diseases treated by a folk healer in the Songkhla province [22].

Table 3.
Percentage of plant species in 38 families in polyherbal remedies used for skin diseases.
2.5. Preferred Plants Used in Polyherbal Recipes for Skin Disorder Treatment
The preferred medicinal plants used in polyherbal remedies for skin diseases and their pharmacological activities are presented in Table 4. According to the quantitative analysis, Oryza sativa L. and Zingiber montanum (Koenig) Link ex Dietr. show the highest use value with 0.83, followed by Nicotiana tabacum L. with a use value of 0.67. Oryza sativa L. was applied for herpes simplex and abscess treatment, while Zingiber montanum (Koenig) Link ex Dietr. was used for treating tinea, acne, and ulcer leprosy, which is similar to Nicotiana tabacum L. Other important plants were Curcuma longa L., Eurycoma longifolia Jack, Knema globularia (Lamk.) Warb, and Senna siamea (Lam.) Irwin & Barneby. with a use value of 0.50. The species with a use value of 0.33 are listed in Table 4. Other plants (50 species) exhibited the UV of 0.17. In previous reports, the seed of Oryza sativa L. was frequently used in skin treatment. Oryza sativa L. contained high levels of anthocyanin polyphenols, which presented beneficial effects on health owing to their antioxidant properties. Anthocyanin from Oryza sativa L. exhibited anti-inflammatory properties and anti-aging activity by modulating type I collagen gene expression and suppressing H2O2-induced NF-κB activation in skin fibroblasts [23]. The crude extract, alkaloids, flavonoids, and saponins from Oryza sativa L. showed antibacterial effects against multidrug resistant Staphylococcus aureus [24]. In addition, the antimicrobial activity of Oryza sativa L. against fungi [25] and viruses [26] has been revealed. Cream containing niosomes loaded with purple glutinous rice (Oryza sativa L.) extract possessed anti-aging activity on human skin [27]. The antioxidative and immunomodulatory properties of Oryza sativa L. crude extract reduced the severity of psoriasis [28]. Zingiber montanum (Koenig) Link ex Dietr., another one of the most frequently used plants in this study, has been previously investigated for its phytochemicals and pharmacological activity. Numerous bioactive phytochemicals were discovered in the rhizomes of Zingiber montanum (Koenig) Link ex Dietr. including alkaloids, saponins, tannins, flavonoids, terpenoids, phenolic compounds, phlobatannins, steroids, and glycosides [29,30]. The essential oil of Zingiber montanum (Koenig) Link ex Dietr. rhizome exhibited antifungal activity against Candida albicans [31]. (E)-8(17),12-labdadiene-15,16-dial, zerumbol, zerumbone, buddledone A, furanodienone, germacrone, borneol, and camphor were isolated from the rhizomes of Zingiber montanum. Among these terpenes, (E)-8(17),12-labdadiene-15,16-dial and zerumbol exhibited antibacterial activity against a number of clinical isolates of multi-drug-resistant (MDR) and methicillin- resistant Staphylococcus aureus (MRSA) [32]. Zerumbone, a sesquiterpenoid, is one of the major compounds in the essential oils and rhizomes of Zingiber montanum. Furthermore, zerumbone-treated wound sections showed greater tissue regeneration and more fibroblasts, possibly through the enhanced expression of VEGF, TGF-β1 and collagen IV [33]. Cysteine protease glycoprotein, purified from Zingiber montanum rhizome, showed antioxidant activity in biochemical systems and THP-1 cells [34], and anti-inflammatory activity [35]. The leaf of Nicotiana tabacum L. was the preferred component in the formulations, and it possessed many biological activities. The different extracts of Nicotiana tabacum L. leaves contain the phytochemical constituents of alkaloids, phenolic compounds, tannins, flavonoids, steroids, terpenoids, cardiac glycosides, essential oils, resins, saponins, quinones, and polypeptides [36]. Antimicrobial activity was observed in the ethyl acetate extract of Nicotiana tabacum L. against Staphylococcus aureus, Pseudomonas aeruginosa, Klebsiella pneumoniae, and biofilm-forming Escherichia coli and Klebsiella species. The most common phytochemical components found in the ethyl acetate extract were 3, 4, 5,6-tetrahydro-1, 3-dimethyl-2(1h)-pyrimidinone, pyridine, 3-(1-methyl-2-pyrrolidinyl)-, (S)-, isododecane, n-pentadecane, and tetradecylaldehyde. The antibacterial property demonstrated could be due to pyridine, 3-(1-methyl-2-pyrrolidinyl)-(S), the major compound detected, with a broad spectrum of activity [37]. Six sesquiterpenes, including tabasesquiterpenes A−C, balsamiferine B, samboginone, and ent-4(15)-eudesmen-1α,11-diol were isolated from the leaves of Nicotiana tabacum L. Tabasesquiterpenes B exhibited high antiviral activity with an inhibition rate of 35.2%. The other compounds also demonstrated antiviral activity with inhibition rates ranging from 20.5–28.6% [38]. Nicotiana tabacum L. leaf cow urine extract was found to have potential anti-dandruff activity against a causative agent, Malassezia furfur [39].

Table 4.
Preferred plants used in polyherbal remedies for skin diseases and their pharmacological activities.
The plants that were commonly used by traditional healers for the treatment of skin diseases were illustrated by relative frequency citation (RFC) (Table 4). The RFC values ranged from 0.17–0.50. The highest RFC value (0.50) was reported for Curcuma longa L., Eurycoma longifolia Jack, Knema globularia (Lamk.) Warb, and Senna siamea (Lam.) Irwin & Barneby. Other high RFC species included Curcuma zedoaria (L.) Roscoeex Sm., Datura metel L., Garcinia mangostana L., Nicotiana tabacum L., Oryza sativa L., Punica granatum L., Quercus infectoria Oliv., and Tiliacora triandra (Colebr.) Diels. The RFC value of 0.17 belonged to the rest of the plants (53 species). Curcumin and derivatives from Curcuma longa L. exhibited biological activities. Curcumin showed anti-bacteria, anti-HIV, antioxidant, anti-inflammatory, and anti-tumor activity. Demethoxy curcumin and bisdemethoxy curcumin had antioxidant activity, while sodium curcuminate showed anti-inflammation [40]. The presence of high levels of curcuminoids and other compounds in MeOH extracts from Curcuma longa L. reflected the potency of antioxidant activity [41]. Curcumin and its derivatives, gallium-curcumin and Cu-curcumin, exhibited remarkable antiviral effects on herpes simplex virus type 1 (HSV-1) in cell culture [42]. Ethanolic extract of Curcuma longa L. rhizomes was found to have better and faster wound healing activity than the standard drug povidone iodine ointment on the excision wound model [43]. The hydroalcoholic extract of Eurycoma longifolia Jack showed significant antioxidant and anti-inflammatory activity [44]. Phenolic compounds, flavonoids, terpenoids, alkaloids, protein, and cardiac glycosides were presented in the extracts from the stem and root of Eurycoma longifolia Jack. The extracts showed antimicrobial activity against Bacillus cereus, Staphylococcus aureus, and Aspergillus niger [45]. Two quassinoid compounds including 14,15 β-dihydroxyklaineanone and eurycomanone had strong antiproliferative activities against all tested cancer cell lines including KATO III (stomach cancer), HCT-15 (colon cancer), Colo205 (colon cancer), HepG2 (hepatoma), PC-3 (prostate cancer), HL-60 (promyelocytic leukemia), and Jurkat (acute T cell leukemia) [46]. Knecorticosanone B and malabaricone D from the fruits of Knema globularia (Lamk.) Warb, exhibited a moderate cytotoxic effect against Hep-G2, MCF-7 and SK-LU-1 cell lines [47]. Giffithane, a compound isolated and characterized from the roots of Knema globularia (Lamk.) Warb, showed strong cytotoxicity against the NCI-H187 and MCF-7 cell lines with IC50 values of 3.08 and 6.68 mg/mL, respectively [48]. Six compounds, knecorticosanones C–H were isolated from the fruits of Knema globularia (Lamk.) Warb. Knecorticosanones C exhibited the most cytotoxicity against HepG2 and KKU-M156 cell lines [49]. Chloroform and 95% ethanolic extracts of Senna siamea (Lam.) Irwin & Barneby leaves had good antifungal activity against Candida albicans and Aspergillus niger. Petroleum ether extracts of leaves were found to be very active against S. aureus [50]. Senna siamea (Lam.) Irwin & Barneby extract contained alkaloid, anthraquinone, saponin, tannin, phenol, steroid, flavonoid, terpenoid, and glycosides, according to phytochemical screening. Senna siamea (Lam.) Irwin & Barneby leaf extracts are effective against Klebsiella pneumoneae, Salmonella typhi, Shigella spp., Escherichia coli, and Pseudomonas aeruginosa. The antibacterial activities of the extracts were expected due to the presence of bioactive compounds, which were dissolved in the solvents [51]. An aqueous extract of Senna siamea (Lam.) Irwin & Barneby leaves showed interesting activity against inflammation. Alkaloids, polyphenols, terpenoids, steroids, anthraquinones, cardiotonic glycosides, and anthocyanins have been identified in this plant [52]. All the other preferable plants combined in the herbal formulations exhibited antimicrobial, anti-oxidant, and anti-inflammatory activities as shown in Table 4. Interestingly, wound healing activity was reported in notable plants including Curcuma longa L [43], Curcuma zedoaria (L.) Roscoeex Sm. [53], Aloe vera (L.) Burm.f. [54], Garcinia mangostana L. [55], Punica granatum L. [56], gall of Quercus infectoria Oliv. [57], and Tinospora crispa (L.) Miers ex Hook.f. [58]. A variety of plants indicated in this study exhibited dermatological healing properties.
3. Methods
3.1. Study Area
The Songkhla province is located in the eastern part of the south of Thailand between latitude 6°17′–7°56′ N and longitude 100°01′–101°06′ E. The province is on the Malay Peninsula, on the coast of the Gulf of Thailand. The height above mean sea level is 4 m. It is approximately 950 km from Bangkok, the capital city. It covers 7393.889 km2. The north is connected to Nakhon Si Thammarat and Phatthalung provinces, while the east borders on the Gulf of Thailand. The neighboring provinces in the south are Yala and Pattani in Thailand and Kadah and Perlis in Malaysia. Phatthalung and Satun provinces are the neighbors in the west. It had a total population of 1,432,628 in 2018 with 63.71% being Buddhists, 33.16% being Muslims, and 3.19% being Christians and Hindus. The weather conditions in Songkhla are influenced by the southwest and northeast monsoons. The average annual temperature is 27.76 °C. The annual rainfall is about 3,434.9 mm, with a relative average humidity of 79.93% [114]. The study was conducted in five districts in Songkhla province, including Muang Songkhla, Chana, Rattaphum, Khuan Niang, and Singhanakhon.
3.2. Informants
In the present study, all traditional healers were selected from their extensive experience and actively practiced patient treatment. All the informants had experience of at least 10 years. According to the intensive criteria, six traditional healers were chosen. All the professional folk healers were males, 54–74 years old. Based on education, three of the healers had graduated from primary school, while one in each group was a secondary school, vocational diploma, and bachelor’s degree holder. Five of the informants were Buddhist, and one of them was Muslim (Table 1).
3.3. Ethnobotanical Data Collection
Ethnobotanical information about skin diseases was obtained from local herbal healers. Before interviewing, the purposes of the study were distinctly explained to the traditional healers and their family members, and verbal informed consent was obtained.
The informants were interviewed using questionnaires and conversations. The interview was performed to investigate the prescriptions for skin disease treatment. Data on the plant’s local names, plant parts used, skin diseases treated with herbal remedies, mode of use, and administration were gathered. Field trips to the sites where the traditional herbal healers normally go to harvest the plants were carried out. Plant materials were collected and processed according to the standard taxonomic method [115]. The scientific names of the plants in the polyherbal formulations were identified according to the principle of plant taxonomy using the Flora of Thailand and the related literature from neighboring areas. The accepted names were verified against The Plant List (2013) [116]. Voucher specimens were deposited at the Faculty of Thai Traditional Medicine, Prince of Songkla University, Songkhla, Thailand. However, some medicinal plants were not obtained from nature because they were exotic or not distributed in the study location. Therefore, they were purchased from the drug stores following the healers’ suggestion, and for their scientific names, we referred to authentic books in traditional Thai pharmacy.
3.4. Data Analysis
The plants were analyzed regarding their habits of plants, and plant parts used in polyherbal remedies for treatment of skin diseases, frequency in families, and quantitative ethnobotany analysis including use value (UV) and relative frequency of citation (RFC).
3.5. Use Value (UV)
Use value was calculated based on the number of uses and the number of people citing a given plant. It indicated the most significant plant species, recognized by a given population [117].
where u is the total number of use reports stated by participants for a given species, and N is the whole number of participants. UV is normally “1” if there are more usages, and “0” if there are fewer usages reported for plant species.
UV = u/N
3.6. Relative Frequency of Citation (RFC)
RFC was analyzed to intricate the knowledge of traditional flora about usage of therapeutic flora in the study site.
where RFC is denoted by relative frequency citation, FC (frequency of citation) is the number of participants mentioning the plant species and N is total number of participants [118].
RFC = FC/N (0 < RFC < 1)
4. Conclusions
Currently, the Thai government has a policy to promote and develop the use of traditional medicines. Thai traditional medicines as well as drugs developed from medicinal plants are included in the national list of essential medicines. The traditional healer is one of the most essential sources for determining the usage of herbal medicine for treating individuals in the community. The results from this study represent the polyherbal remedies used by experienced folk healers for the treatment of skin disorders in the Songkhla province, in the south of Thailand. Ethnopharmacological expertise is abundant among traditional healers. They have significant knowledge of many plant species used for a variety of skin disorder treatment. The utilization of medicinal plants was widespread in the prescriptions, with 66 species in 38 families. The poultice was the most frequent method of administration. The most prominent plant families were Fabaceae, Rubiaceae, and Zingiberaceae. The highest use values were reported for Oryza sativa L. and Zingiber montanum (Koenig) Link ex Dietr. Based on RFC, the highest was found for Curcuma longa L., Eurycoma longifolia Jack, Knema globularia (Lamk.) Warb, and Senna siamea (Lam.) Irwin & Barneby. Although local treatment of herbal prescriptions and ethnobotanical surveys are underway, more research on phytochemicals and their pharmacological activities is needed to ensure the application of polyherbal prescriptions used by traditional healers, as well as product development in herbal medicine for the treatment of skin diseases, in order to promote the sustainable and safe use of natural resources.
Author Contributions
Conceptualization: J.S., K.M. and S.P.V.; methodology: K.M., J.S., O.S. and S.L.; data collection: K.M., O.S. and S.L.; data analysis: J.S. and K.M.; writing-original draft: J.S.; writing—review & editing: J.S., K.M., F.G. and S.P.V.; supervision, project administration, and funding acquisition: S.P.V. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by Prince of Songkla University and the Ministry of Higher Education, Science, Research and Innovation, Thailand, under the Reinventing University Project (Grant Number REV64051) and National Research Council of Thailand (Grant Number N41A640071).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Verbal informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
The Article Processing Charge of this work was financially supported by Mae Fah Luang University. We are grateful to all traditional healers in the Songkhla province for sharing their valuable knowledge and their families for the hospitality during the fieldwork. We appreciate our staff for the assistance in plant collection.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Zhang, X.J.; Wang, A.P.; Shi, T.Y.; Zhang, J.; Xu, H.; Wang, D.Q.; Feng, L. The psychosocial adaptation of patients with skin disease: A scoping review. BMC Public Health 2019, 19, 1404. [Google Scholar] [CrossRef] [PubMed]
- Hay, R.J.; Augustin, M.; Griffiths, C.E.M.; Sterry, W. The global challenge for skin health. Br. J. Dermatol. 2015, 172, 1469–1472. [Google Scholar] [CrossRef] [PubMed]
- Dawson, A.L.; Dellavalle, R.P.; Elston, D.M. Infectious skin diseases: A review and needs assessment. Dermatol. Clin. 2012, 30, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Li, V.C.; Chowdhury, M.M. Dermatological pharmacology: Topical agents. Medicine 2017, 45, 359–362. [Google Scholar] [CrossRef]
- Yuan, H.; Ma, Q.; Ye, L.; Piao, G. The Traditional medicine and modern medicine from natural products. Molecules 2016, 21, 559. [Google Scholar] [CrossRef] [PubMed]
- Jones, V.A.; Patel, P.M.; Wilson, C.; Wang, H.; Ashack, K.A. Complementary and alternative medicine treatments for common skin diseases: A systematic review and meta-analysis. JAAD Int. 2021, 2, 76–93. [Google Scholar] [CrossRef]
- Tabassum, N.; Hamdani, M. Plants used to treat skin diseases. Pharmacogn. Rev. 2014, 8, 52–60. [Google Scholar] [CrossRef]
- Malik, K.; Ahmad, M.; Zafar, M.; Ullah, R.; Mahmood, H.M.; Parveen, B.; Rashid, N.; Sultana, S.; Shah, S.N. An ethnobotanical study of medicinal plants used to treat skin diseases in northern Pakistan. BMC Complement. Altern. Med. 2019, 19, 210. [Google Scholar] [CrossRef]
- Hussein, R.A.; El-Anssary, A.A. Plants secondary metabolites: The key drivers of the pharmacological actions of medicinal plants. In Herbal Medicine; Builders, P.F., Ed.; IntechOpen: London, UK, 2019; pp. 11–30. [Google Scholar] [CrossRef]
- Zaid, N.A.M.; Sekar, M.; Bonam, S.R.; Gan, S.H.; Lum, P.T.; Begum, M.Y.; Rani, N.N.I.M.; Vaijanathappa, J.; Wu, Y.S.; Subramaniyan, V.; et al. Promising natural products in new drug design, development, and therapy for skin disorders: An overview of scientific evidence and understanding their mechanism of action. Drug Des. Dev. Ther. 2020, 16, 23–66. [Google Scholar] [CrossRef]
- Maneenoon, K.; Khuniad, C.; Teanuan, Y.; Saedan, N.; Prom-In, S.; Rukleng, N.; Kongpool, W.; Pinsook, P.; Wongwiwat, W. Ethnomedicinal plants used by traditional healers in Phatthalung Province, Peninsular Thailand. J. Ethnobiol. Ethnomed. 2015, 11, 43. [Google Scholar] [CrossRef]
- Neamsuvan, O.; Komonhiran, P.; Boonming, K. Medicinal plants used for hypertension treatment by folk healers in Songkhla province, Thailand. J. Ethnopharmacol. 2018, 214, 58–70. [Google Scholar] [CrossRef] [PubMed]
- Neamsuvan, O.; Madeebing, N.; Mah, L.; Lateh, W. A survey of medicinal plants for diabetes treating from Chana and Nathawee district, Songkhla province, Thailand. J. Ethnopharmacol. 2015, 174, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Neamsuvan, O.; Sengnona, N.; Seemaphrika, N.; Chouychooa, M.; Rungrata, R.; Sujittra, B. Survey of medicinal plants around upper Songkhla lake, Thailand. Afr. J. Tradit. Complement. Altern. Med. 2015, 12, 133–143. [Google Scholar] [CrossRef]
- Neamsuvan, O.; Bunmee, P. A survey of herbal weeds for treating skin disorders from southern Thailand: Songkhla and Krabi province. J. Ethnopharmacol. 2016, 193, 574–585. [Google Scholar] [CrossRef]
- World Health Organization. Regional Office for South-East Asia. Traditional Herbal Remedies for Primary Health Care; WHO Regional Office for South-East Asia: New Delhi, India, 2010; pp. 1–167. ISBN 978-92-9022-382-5. [Google Scholar]
- Neamsuvan, O.; Phumchareon, T.; Bunphan, W.; Kaosaeng, W. Plant materials for gastrointestinal diseases used in Chawang district, Nakhon Si Thammarat province, Thailand. J. Ethnopharmacol. 2016, 194, 179–187. [Google Scholar] [CrossRef]
- Asong, J.; Ndhlovu, P.; Khosana, N.; Aremu, A.; Otang-Mbeng, W. Medicinal plants used for skin-related diseases among the Batswanas in Ngaka Modiri Molema District Municipality, South Africa. S. Afr. J. Bot. 2019, 126, 11–20. [Google Scholar] [CrossRef]
- Salhi, N.; Bouyahya, A.; Fettach, S.; Zellou, A.; Cherrah, Y. Ethnopharmacological study of medicinal plants used in the treatment of skin burns in occidental Morocco (area of Rabat). S. Afr. J. Bot. 2019, 121, 128–142. [Google Scholar] [CrossRef]
- Alamgeer; Sharif, A.; Asif, H.; Younis, W.; Riaz, H.; Bukhari, I.A.; Assiri, A.M. Indigenous medicinal plants of Pakistan used to treat skin diseases: A review. Chin. Med. 2018, 13, 52. [Google Scholar] [CrossRef]
- Chotchoungchatchai, S.; Saralamp, P.; Jenjittikul, T.; Pornsiripongse, S.; Prathanturarug, S. Medicinal plants used with Thai traditional medicine in modern healthcare services: A case study in Kabchoeng Hospital, Surin Province, Thailand. J. Ethnopharmacol. 2012, 141, 193–205. [Google Scholar] [CrossRef]
- Kesornmas, S.; Nakthaworn, K.; Musikapong, K.; Viriyabubpa, C. A Study on the treatment with herbal remedies in seven groups of diseases: A case study of Mr. Prawit Kaewthong, Songkhla Province. J. Tradit. Thai Altern. Med. 2019, 17, 263–279. [Google Scholar]
- Palungwachira, P.; Tancharoen, S.; Phruksaniyom, C.; Klungsaeng, S.; Srichan, R.; Kikuchi, K.; Nararatwanchai, T. Antioxidant and anti-inflammatory properties of anthocyanins extracted from Oryza sativa L. in primary dermal fibroblasts. Oxid. Med. Cell Longev. 2019, 2019, 2089817. [Google Scholar] [CrossRef] [PubMed]
- Amber, R.; Adnan, M.; Tariq, A.; Khan, S.N.; Mussarat, S.; Hashem, A.; Al-Huqail, A.A.; Al-Arjani, A.F.; Abd Allah, E.F. Anti-bacterial activity of selected medicinal plants of northwest Pakistan traditionally used against mastitis in livestock. Saudi J. Biol. Sci. 2018, 25, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Gu, C.Z.; Xia, X.M.; Lv, J.; Tan, J.W.; Baerson, S.R.; Pan, Z.Q.; Song, Y.Y.; Zeng, R.S. Diterpenoids with herbicidal and antifungal activities from hulls of rice (Oryza sativa). Fitoterapia 2019, 136, 104183. [Google Scholar] [CrossRef] [PubMed]
- Aoki, H.; Akaike, T.; Abe, K.; Kuroda, M.; Arai, S.; Okamura, R.; Negi, A.; Maeda, H. Antiviral effect of oryzacystatin, a proteinase inhibitor in rice, against herpes simplex virus type 1 in vitro and in vivo. Antimicrob. Agents Chemother. 1995, 39, 846–849. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Manosroi, J.; Chankhampan, C.; Kitdamrongtham, W.; Zhang, J.; Abe, M.; Akihisa, T.; Manosroi, W.; Manosroi, A. In vivo anti-ageing activity of cream containing niosomes loaded with purple glutinous rice (Oryza sativa Linn.) extract. Int. J. Cosmet. Sci. 2020, 42, 622–631. [Google Scholar] [CrossRef] [PubMed]
- Ampawong, S.; Kengkoom, K.; Sukphopetch, P.; Aramwit, P.; Muangkaew, W.; Kanjanapruthipong, T.; Buaban, T. Evaluating the effect of rice (Oryza sativa L.: SRNC05053-6-2) crude extract on psoriasis using in vitro and in vivo models. Sci. Rep. 2020, 10, 17618. [Google Scholar] [CrossRef]
- Majaw, S.; Moirangthem, J. Qualitative and Quantitative Analysis of Clerodendron colebrookianum Walp. Leaves and Zingiber cassumunar Roxb. Rhizomes. Ethnobot. Leafl. 2009, 13, 578–589. [Google Scholar]
- Joram, A.; Das, A.K.; Mahanta, D. Evaluation of antioxidant and phenolic contents of Zingiber montanum (J. Koenig) Link ex Dietr.: A potential ethomedicinal plant of Arunachal Pradesh, India. Pleione 2018, 12, 255–264. [Google Scholar] [CrossRef]
- Verma, R.S.; Joshi, N.; Padalia, R.C.; Singh, V.R.; Goswami, P.; Verma, S.K.; Iqbal, H.; Chanda, D.; Verma, R.K.; Darokar, M.P.; et al. Chemical composition and antibacterial, antifungal, allelopathic and acetylcholinesterase inhibitory activities of cassumunar-ginger. J. Sci. Food Agric. 2018, 98, 321–327. [Google Scholar] [CrossRef]
- Siddique, H.; Pendry, B.; Rahman, M.M. Terpenes from Zingiber montanum and their screening against multi-drug resistant and methicillin resistant Staphylococcus aureus. Molecules 2019, 24, 385. [Google Scholar] [CrossRef]
- Liu, W.Y.; Tzeng, T.-F.; Liu, I.-M. Healing potential of zerumbone ointment on experimental full-thickness excision cutaneous wounds in rat. J. Tissue Viability 2017, 26, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Jamir, K.; Seshagirirao, K. Purification, biochemical characterization and antioxidant property of ZCPG, a cysteine protease from Zingiber montanum rhizome. Int. J. Biol. Macromol. 2018, 106, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Jamir, K.; Ganguly, R.; Seshagirirao, K. ZCPG, a cysteine protease from Zingiber montanum rhizome exhibits enhanced anti-inflammatory and acetylcholinesterase inhibition potential. Int. J. Biol. Macromol. 2020, 163, 2429–2438. [Google Scholar] [CrossRef] [PubMed]
- Oeung, S.; Nov, V.; Ung, H.; Roum, K.; Yin, V.; Keo, S.; Chea, S. Phytochemical analysis of different extracts of leaves of Nicotiana tabacum L. of Cambodia. Asian J. Pharmacogn. 2017, 1, 18–26. [Google Scholar]
- Ameya, G.; Manilal, A.; Merdekios, B. In vitro antibacterial activity and phytochemical analysis of Nicotiana tabacum L. extracted in different organic solvents. Open Microbiol. J. 2017, 11, 352–359. [Google Scholar] [CrossRef]
- Shang, S.Z.; Zhao, W.; Tang, J.G.; Xu, X.M.; Sun, H.D.; Pu, J.X.; Liu, Z.H.; Miao, M.M.; Chen, Y.K.; Yang, G.Y. Antiviral sesquiterpenes from leaves of Nicotiana tabacum. Fitoterapia 2016, 108, 1–4. [Google Scholar] [CrossRef]
- Itankar, P.; Murkute, A.V. Evaluation of in vitro antidandruff activity of biotransformed material (extract) of Nicotiana tabacum leaves. J. Nat. Remedies 2015, 15, 65–70. [Google Scholar] [CrossRef]
- Araújo, C.A.C.; Leon, L.L. Biological activities of Curcuma longa L. Mem. Inst. Oswaldo. Cruz. 2001, 96, 723–728. [Google Scholar] [CrossRef]
- Kasai, H.; Yamane, Y.; Ikegami-Kawai, M.; Sudo, H. Analysis of compounds of Curcuma rhizome using mass spectrometry and investigation of the antioxidant activity of rhizome extracts. Med. Aromat. Plants 2019, 8, 336. [Google Scholar]
- Zandia, K.; Ramedania, E.; Mohammadi, K.; Tajbakhsh, S.; Deilami, I.; Rastian, Z.; Fouladvand, M.; Yousefi, F.; Farshadpour, F. Evaluation of antiviral activities of curcumin derivatives against HSV-1 in Vero cell line. Nat. Prod. Commun. 2010, 5, 1935–1938. [Google Scholar] [CrossRef]
- Purohit, S.K.; Solanki, R.; Mathur, V.; Mathur, M. Evaluation of wound healing activity of ethanolic extract of Curcuma longa rhizomes in male albino rats. Asian J. Pharm. Res. 2013, 3, 79–81. [Google Scholar]
- Varghese, C.P.; Ambrose, C.; Jin, S.C.; Lim, Y.J.; Keisaban, T. Antioxidant and anti-inflammatory activity of Eurycoma longifolia Jack, a traditional medicinal plant in Malaysia. Int. J. Pharm. Sci. Nanotechnol. 2013, 5, 1875–1878. [Google Scholar] [CrossRef]
- Khanam, Z.; Wen, C.S.; Bhat, I.U.H. Phytochemical screening and antimicrobial activity of root and stem extracts of wild Eurycoma longifolia Jack (Tongkat Ali). J. King Saud Univ. Sci. 2015, 27, 23–30. [Google Scholar] [CrossRef]
- Tung, N.H.; Uto, T.; Hai, N.T.; Li, G.; Shoyama, Y. Quassinoids from the root of Eurycoma longifolia and their antiproliferative activity on human cancer cell lines. Pharmacogn. Mag. 2017, 13, 459–462. [Google Scholar] [PubMed]
- Pham, T.V.; Bach, H.K.T.; Ho, D.V.; Nguyen, B.C. Chemical constituents from the Knema globularia fruits and their in vitro cytotoxicity. Nat. Prod. Res. 2020, 36, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Sriphana, U.; Yenjai, C.; Suthiwong, J.; Poopasit, K. A new diarylhexane and two new diarylpropanols from the roots of Knema globularia. Nat. Prod. Res. 2020. [Google Scholar] [CrossRef]
- Chuenban, C.; Sombatsri, A.; Sribuhom, T.; Pornchoo, C.; Prawan, A.; Tontapha, S.; Amornkitbamrung, V.; Yenjai, C. Knecorticosanones C–H from the fruits of Knema globularia (Lam.) warb. RSC Adv. 2021, 11, 4097–4103. [Google Scholar] [CrossRef]
- Mehta, J.P.; Parmar, P.H.; Kukadiya, N.B.; Godhani, D.R. Antimicrobial assay of extracts of Cassia Siamea (Lam.) and Cassia Javanica (Linn.). J. Pharm. Chem. Biol. Sci. 2018, 5, 386–395. [Google Scholar]
- Nas, F.; Oyeyi, T.; Ali, M. Antibacterial efficacy and phytochemical screening of Senna siamea leaves extracts on some pathogenic bacteria. J. Microbiol. Exp. 2018, 6, 159–163. [Google Scholar]
- Nsonde Ntandou, G.F.; Etou Ossibi, A.W.; Elion Itou, R.D.G.; Boumba, S.L.; Ouamba, J.M.; Abena, A.A. Laxative, antiinflammatory and analgesic effects of Cassia Siamea Lam (Fabaceae) leaves aqueous extract. IOSR J. Pharm. Biol. Sci. 2018, 13, 6–15. [Google Scholar]
- Tungcharoen, P.; Sudsai, T.; Leejae, S.; Wattanapiromsakul, C.; Tansakul, P.; Tewtrakul, S. Wound healing activity of Curcuma zedoaroides. Songklanakarin J. Sci. Technol. 2016, 38, 621–630. [Google Scholar]
- Fox, L.T.; Mazumder, A.; Dwivedi, A.; Gerber, M.; du Plessis, J.; Hamman, J.H. In vitro wound healing and cytotoxic activity of the gel and whole-leaf materials from selected aloe species. J. Ethnopharmacol. 2017, 200, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Siriwattanasatorn, M.; Itharat, A.; Thongdeeying, P.; Ooraikul, B. In Vitro Wound healing activities of three most commonly used Thai medicinal plants and their three markers. Evid. Based Complement. Altern. Med. 2020, 2020, 6795383. [Google Scholar] [CrossRef] [PubMed]
- Amal, B.; Veena, B.; Jayachandran, V.P.; Shilpa, J. Preparation and characterization of Punica granatum pericarp aqueous extract loaded chitosan-collagen-starch membrane: Role in wound healing process. J. Mater. Sci. Mater. Med. 2015, 26, 181. [Google Scholar] [CrossRef]
- Chokpaisarn, J.; Chusri, S.; Voravuthikunchai, S. Clinical randomized trial of topical Quercus infectoria ethanolic extract for the treatment of chronic diabetic ulcers. J. Herb. Med. 2020, 21, 100301. [Google Scholar] [CrossRef]
- Arcueno, R.O.; Retumban, J.L.B.; Echano, J.E.; Guerrero, J.J.G. Wound healing potential of Tinospora Crispa (Willd.) Miers [Menispermaceae] stem on diabetic mice. J. Med. Plants Stud. 2015, 3, 106–109. [Google Scholar]
- Rahman, H.; Eswaraiah, M.C.; Dutta, M. In-vitro Anti-inflammatory and anti-arthritic activity of Oryza sativa Var. Joha rice (An aromatic indigenous rice of Assam). Am. Eurasian J. Agric. Environ. Sci. 2015, 15, 115–121. [Google Scholar]
- Al-Amin, M.; Sultana, G.N.; Hossain, C.F. Antiulcer principle from Zingiber montanum. J. Ethnopharmacol. 2012, 141, 57–60. [Google Scholar] [CrossRef]
- Al-Amin, M.; Eltayeb, N.M.; Hossain, C.F.; Khairuddean, M.; Fazalul Rahiman, S.S.; Salhimi, S.M. Inhibitory activity of extract, fractions, and compounds from Zingiber montanum rhizomes on the migration of breast cancer cells. Planta Med. 2020, 86, 387–394. [Google Scholar] [CrossRef]
- Anumudu, C.; Nwachukwu, M.; Obasi, C.; Nwachukwu, I.; Ihenetu, F. Antimicrobial activities of extracts of tobacco leaf (Nicotiana tabacum) and its grounded snuff (Utaba) on Candida albicans and Streptococcus pyogenes. J. Trop. Dis. 2019, 7, 300. [Google Scholar]
- Ru, Q.M.; Wang, L.J.; Li, W.M.; Wang, J.L.; Ding, Y.T. In vitro antioxidant properties of flavonoids and polysaccharides extract from tobacco (Nicotiana tabacum L.) leaves. Molecules 2012, 17, 11281–11291. [Google Scholar] [CrossRef] [PubMed]
- Vaziri, S.; Mojarrab, M.; Farzaei, M.H.; Najafi, F.; Ghobadi, A. Evaluation of anti-aphthous activity of decoction of Nicotiana tabacum leaves as a mouthwash: A placebo-controlled clinical study. J. Tradit. Chin. Med. 2016, 36, 160–164. [Google Scholar] [CrossRef]
- Gupta, A.; Mahajan, S.; Sharma, R. Evaluation of antimicrobial activity of Curcuma longa rhizome extract against Staphylococcus aureus. Biotechnol. Rep. 2015, 6, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Long, L.; Zhang, F.; Chen, Q.; Yu, X.; Liu, Q.; Bao, J.; Long, Z. Antifungal activity, main active components and mechanism of Curcuma longa extract against Fusarium graminearum. PLoS ONE 2018, 13, e0194284. [Google Scholar] [CrossRef] [PubMed]
- Ichsyani, M.; Ridhanya, A.; Risanti, M.; Desti, H.; Ceria, R.; Putri, D.; Sudiro, T.; Dewi, B. Antiviral effects of Curcuma longa L. against dengue virus in vitro and in vivo. IOP Conf. Ser. Earth Environ. Sci. 2017, 101, 012005. [Google Scholar] [CrossRef]
- Savaringal, J.P.; Lally, M.S. Anti-inflammatory effect of rhizome of Curcuma longa Linn, in albino rats by the method of carrageenin induced paw oedema. Int. J. Basic Clin. Pharmacol. 2018, 7, 229–233. [Google Scholar] [CrossRef]
- Stasiłowicz, A.; Tykarska, E.; Lewandowska, K.; Kozak, M.; Miklaszewski, A.; Kobus-Cisowska, J.; Szymanowska, D.; Plech, T.; Jenczyk, J.; Cielecka-Piontek, J. Hydroxypropyl-β-cyclodextrin as an effective carrier of curcumin-piperine nutraceutical system with improved enzyme inhibition properties. J. Enzyme Inhib. Med. Chem. 2020, 35, 1811–1821. [Google Scholar] [CrossRef]
- Alloha, I.B.; Aziz, N.A.L.B.; Faisal, G.G.; Abllah, Z.; Arzmi, M.H. Effects of Eurycoma Longifolia Jack (Tongkat Ali) alcoholic root extract against oral pathogens. Pharmacog. J. 2019, 11, 1299–1302. [Google Scholar] [CrossRef]
- Wan Hassan, W.N.A.; Zulkifli, R.M.; Ahmad, F.; Yunus, M.A.C. Antioxidant and tyrosinase inhibition activities of Eurycoma longifolia and Swietenia macrophylla. J. Appl. Pharm. Sci. 2015, 5, 6–10. [Google Scholar] [CrossRef]
- Phaiphan, A.; Baharin, B.S.; Tan, C.P.; Rahman, R.A.; Ganesan, P. Antioxidant and antibacterial activities of different solvent extractions from Cassia siamea (Lamk.) leaves. J. Chem. Pharm. 2014, 6, 655–662. [Google Scholar]
- Islam, M.; Hoshen, A.; Ayshasiddeka; Islam, F.; Yeasmin, T. Antimicrobial, membrane stabilizing and thrombolytic activities of ethanolic extract of Curcuma zedoaria Rosc. rhizome. J. Pharmacogn. Phytochem. 2017, 6, 38–41. [Google Scholar]
- Chachad, D.P.; Talpade, M.B.; Jagdale, S.P. Antimicrobial activity of rhizomes of Curcuma zedoaria Rosc. Int. J. Sci. Res. 2016, 5, 938–940. [Google Scholar]
- Huang, S.J.; Chyau, C.C.; Tsai, C.H.; Chen, C.C.; Mau, J.L.; Tsai, S.Y. Antioxidant properties of extracts from Curcuma zedoaria rhizome. Adv. Mat. Res. 2015, 1120, 920–925. [Google Scholar] [CrossRef]
- Lakshmi, S.; Padmaja, G.; Remani, P. Antitumour effects of isocurcumenol isolated from Curcuma zedoaria rhizomes on human and murine cancer cells. Int. J. Med. Chem. 2011, 2011, 253962. [Google Scholar] [CrossRef] [PubMed]
- Bachheti, R.K.; Rai, I.; Mishra, V.K.; Joshi, A. Antioxidant and antimicrobial properties of seed oil of Datura metel. J. Environ. Biol. 2018, 39, 182–188. [Google Scholar] [CrossRef]
- Fakai, I.M.; Bagudo, A.I.; Aminu, H.; Isaac, M. Physico-chemical analysis and antifungal activity of Datura metel seed oil. Int. J. Pharm. Biosci. 2016, 3, 61–68. [Google Scholar]
- Roy, S.; Mukherjee, S.; Pawar, S.; Chowdhary, A. Evaluation of in vitro antiviral activity of Datura metel Linn. against rabies virus. Pharmacogn. Res. 2016, 8, 265–269. [Google Scholar] [CrossRef]
- Bhardwaj, K.; Kumar, S.; Ojha, S. Antioxidant activity and FT-IR analysis of Datura innoxia and Datura metel and seed methanolic extract. Afr. J. Tradit. Complement. Altern. Med. 2016, 13, 7–16. [Google Scholar]
- Tatiya-Aphiradee, N.; Chatuphonprasert, W.; Jarukamjorn, K. Anti-inflammatory effect of Garcinia mangostana Linn. pericarp extract in methicillin-resistant Staphylococcus aureus-induced superficial skin infection in mice. Biomed. Pharmacother. 2019, 111, 705–713. [Google Scholar] [CrossRef]
- Rahmayanti, F.; Sastradipura, D.F.S.; Masúd, Z.A.; Bachtiar, B.M.; Wimardhani, Y.S.; Permana, G. Ethyl acetate fraction of Garcinia mangostana Linn pericarp extract: Anti—Candida albicans and epithelial cytotoxicity. Asian J. Pharm. Clin. Res. 2016, 9, 357–360. [Google Scholar]
- Tarasuk, M.; Songprakhon, P.; Chimma, P.; Sratongno, P.; Na-Bangchang, K.; Yenchitsomanus, P.T. Alpha-mangostin inhibits both dengue virus production and cytokine/chemokine expression. Virus Res. 2017, 240, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, G.; Ibrahim, S. New benzophenones and a dihydroflavanonol from Garcinia mangostana pericarps and their antioxidant and cytotoxic activities. Phytochem. Lett. 2020, 39, 43–48. [Google Scholar] [CrossRef]
- Wang, J.; Shi, Q.; Zhang, W.; Sanderson, B. Anti-skin cancer properties of phenolic-rich extract from the pericarp of mangosteen (Garcinia mangostana Linn.). Food Chem. Toxicol. 2012, 50, 3004–3013. [Google Scholar] [CrossRef] [PubMed]
- Ohno, R.; Moroishi, N.; Sugawa, H.; Maejima, K.; Saigusa, M.; Yamanaka, M.; Nagai, M.; Yoshimura, M.; Amakura, Y.; Nagai, R. Mangosteen pericarp extract inhibits the formation of pentosidine and ameliorates skin elasticity. J Clin. Biochem. Nutr. 2015, 57, 27–32. [Google Scholar] [CrossRef]
- Fitri, E.W.; Anwar, A.I.; Djawad, K.; Seweng, A.; Changara, H.; Alam, G. The effectiveness of topical mangosteen pericarp extract on the collagen of mice skin exposed to ultraviolet B. Am. J. Clin. Exp. Med. 2016, 4, 88–93. [Google Scholar] [CrossRef][Green Version]
- Moorthy, K.; Punitha, T.; Vinodhini, R.; Sureshkumar, B.T.; Vijayalakshmi, P.; Thajuddin, N. Antimicrobial activity and qualtative phytochemical analysis of Punica granatum Linn. (Pericarp). J. Med. Plants Res. 2013, 7, 474–479. [Google Scholar]
- Anibal, P.C.; Peixoto, I.T.; Foglio, M.A.; Höfling, J.F. Antifungal activity of the ethanolic extracts of Punica granatum L. and evaluation of the morphological and structural modifications of its compounds upon the cells of Candida spp. Braz. J. Microbiol. 2013, 44, 839–848. [Google Scholar] [CrossRef]
- Houston, D.M.J.; Bugert, J.J.; Denyer, S.P.; Heard, C.M. Potentiated virucidal activity of pomegranate rind extract (PRE) and punicalagin against herpes simplex virus (HSV) when co-administered with zinc (II) ions, and antiviral activity of PRE against HSV and aciclovir-resistant HSV. PLoS ONE 2017, 12, e0179291. [Google Scholar]
- Jacob, J.; Lakshmanapermalsamy, P.; Illuri, R.; Bhosle, D.; Sangli, G.K.; Mundkinajeddu, D. In vitro evaluation of antioxidant potential of isolated compounds and various extracts of peel of Punica granatum L. Pharmacogn. Res. 2018, 10, 44–48. [Google Scholar]
- Houston, D.; Bugert, J.; Denyer, S.; Heard, C. Anti-inflammatory activity of Punica granatum L. (Pomegranate) rind extracts applied topically to ex vivo skin. Eur. J. Pharm. Biopharm. 2017, 112, 30–37. [Google Scholar] [CrossRef]
- Seifabadi, S.; Vaseghi, G.; Ghannadian, M.; Javanmard, S. Standardized Punica granatum pericarp extract, suppresses tumor proliferation and angiogenesis in a mouse model of melanoma: Possible involvement of PPAR alpha and PPAR gamma pathways. Iran. J. Pharm. Sci. 2019, 18, 348–357. [Google Scholar]
- Wan Nor Amilah, W.A.; Masrah, M.; Hasmah, A.; Noor Izani, N.J. In vitro antibacterial activity of Quercus infectoria gall extracts against multidrug resistant bacteria. Trop. Biomed. 2014, 31, 680–688. [Google Scholar] [PubMed]
- Vanga, S.; Pingili, M.; Tharigoppula, S. Phytochemical screening and evaluation of antifungal activity of gall extracts of Quercus infectoria. Int. J. Pharm. Sci. Res. 2017, 8, 3010–3013. [Google Scholar]
- Ghafarzadeh, M.; Eatemadi, A. Clinical efficacy of liposome-encapsulated Aloe vera on melasma treatment during pregnancy. J. Cosmet. Laser Ther. 2017, 19, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Chokpaisarn, J.; Chusri, S.; Amnuaikit, T.; Udomuksorn, W.; Voravuthikunchai, S. Potential wound healing activity of Quercus infectoria formulation in diabetic rats. PeerJ 2017, 5, e3608. [Google Scholar] [CrossRef]
- Chokpaisarn, J.; Urao, N.; Voravuthikunchai, S.; Koh, T. Quercus infectoria inhibits Set7/NF-kappa B inflammatory pathway in macrophages exposed to a diabetic environment. Cytokine 2017, 94, 29–36. [Google Scholar] [CrossRef]
- Rahman, M.M.; Shamsuzzaman, M.; Khatun, M.; Rahman, M.M.; Hossain, A.S.M.S.; Alam, A.H.M.K.; Mosaddik, A.; Wahed, M.I.I. Phytochemical and antimicrobial properties of Tiliacora triandra stem bark. Br. J. Pharm. Res. 2017, 17, 1–9. [Google Scholar] [CrossRef]
- Añibarro-Ortega, M.; Pinela, J.; Barros, L.; Ćirić, A.; Silva, S.P.; Coelho, E.; Mocan, A.; Calhelha, R.C.; Soković, M.; Coimbra, M.A.; et al. Compositional features and bioactive properties of Aloe vera leaf (fillet, mucilage, and rind) and flower. Antioxidants 2019, 8, 444. [Google Scholar] [CrossRef]
- Dziewulska, D.; Stenzel, T.; Smialek, M.; Tykalowski, B.; Koncicki, A. An evaluation of the impact of aloe vera and licorice extracts on the course of experimental pigeon paramyxovirus type 1 infection in pigeons. Poult. Sci. 2018, 97, 470–476. [Google Scholar] [CrossRef]
- Vijayalakshmi, D.; Dhandapani, R.; Jayaveni, S.; Jithendra, P.S.; Rose, C.; Mandal, A.B. In vitro anti-inflammatory activity of Aloe vera by down regulation of MMP-9 in peripheral blood mononuclear cells. J. Ethnopharmacol. 2012, 141, 542–546. [Google Scholar] [CrossRef]
- Fox, L.T.; du Plessis, J.; Gerber, M.; van Zyl, S.; Boneschans, B.; Hamman, J.H. In Vivo skin hydration and anti-erythema effects of Aloe vera, Aloe ferox and Aloe marlothii gel materials after single and multiple applications. Pharmacogn. Mag. 2014, 10, S392–S403. [Google Scholar] [PubMed]
- Fox, L.T.; Gerber, M.; du Preez, J.L.; du Plessis, J.; Hamman, J.H. Skin permeation enhancement effects of the gel and whole-leaf materials of Aloe vera, Aloe marlothii and Aloe ferox. J. Pharm. Pharmacol. 2015, 67, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Dhanabal, S.P.; Priyanka Dwarampudi, L.; Muruganantham, N.; Vadivelan, R. Evaluation of the antipsoriatic activity of Aloe vera leaf extract using a mouse tail model of psoriasis. Phytother. Res. 2012, 26, 617–619. [Google Scholar] [CrossRef] [PubMed]
- Prakash, A.; Vadivel, V.; Banu, S.F.; Nithyanand, P.; Lalitha, C.; Brindhad, P. Evaluation of antioxidant and antimicrobial properties of solvent extracts of agro-food by-products (cashew nut shell, coconut shell and groundnut hull). Agric. Nat. Resour. 2018, 52, 451–459. [Google Scholar] [CrossRef]
- Sudjaroen, Y.; Thongkao, K.; Suwannahong, K. Antioxidant, antibacterial, and cytotoxicity activities of cashew (Anacardium occidentale) Nut Shell Waste. Int. J. Green Pharm. 2018, 12, S229–S234. [Google Scholar]
- Mahata, D.; Mandal, S.M.; Bharti, R.; Gupta, V.K.; Mandal, M.; Nag, A.; Nando, G.B. Self-assembled cardanol azo derivatives as antifungal agent with chitin-binding ability. Int. J. Biol. Macromol. 2014, 69, 5–11. [Google Scholar] [CrossRef] [PubMed]
- de Souza, M.Q.; Teotônio, I.M.S.N.; de Almeida, F.C.; Heyn, G.S.; Alves, P.S.; Romeiro, L.A.S.; Pratesi, R.; de Medeiros Nóbrega, Y.K.; Pratesi, C.B. Molecular evaluation of anti-inflammatory activity of phenolic lipid extracted from cashew nut shell liquid (CNSL). BMC. Complement. Altern. Med. 2018, 18, 181. [Google Scholar] [CrossRef]
- Faruk, M.O.; Sardar, R.; Haque, S.T.; Haque, M.E. Antimicrobial, cytotoxic and antioxidant activities of Barringtonia acutangula (L). Bioresearch Commun. 2016, 2, 205–209. [Google Scholar]
- Inampudi, V.K.; Jay Kumar, S.; Koshy, R.K.; Patel, Y.; Sujitha, P.J. Anti-oxidant and anti-inflammatory activities of Barringtonia acutangula linn. bark extracts on rats. Int. J. Curr. Res. 2014, 6, 9785–9790. [Google Scholar]
- Haque, A.; Islam, A.; Shahriar, M. Antimicrobial, cytotoxicity and antioxidant activity of Tinospora crispa. J. Pharm. Biomed. Sci. 2011, 13, 1–4. [Google Scholar]
- Hipol, R.L.B.; Cariaga, M.F.N.M.; Hipol, R.M. Inflammatory activities of the aqueous extract of the stem of Tinospora Crispa (Family Menispermaceae). J. Nat. Stud. 2012, 11, 88–95. [Google Scholar]
- Songkhla Provincial Public Health Office, Ministry of Public Health, Thailand. 2019, pp. 13–14. Available online: https://www.skho.moph.go.th/strategy/inspec/2562/2/index.html#p=15 (accessed on 6 February 2022).
- Bridson, D.; Forman, L. The Herbarium Handbook; Royal Botanic Gardens: Kew, UK, 1992. [Google Scholar]
- The Plant List. Version 1.1. 2013. Available online: http://www.theplantlist.org/ (accessed on 13 January 2021).
- Umair, M.; Altaf, M.; Abbasi, A.M. An ethnobotanical survey of indigenous medicinal plants in Hafizabad district, Punjab-Pakistan. PLoS ONE 2017, 12, e0177912. [Google Scholar] [CrossRef] [PubMed]
- Kayani, S.; Ahmad, M.; Zafar, M.; Sultana, S.; Khan, M.P.Z.; Ashraf, M.A.; Hussain, J.; Yaseen, G. Ethnobotanical uses of medicinal plants for respiratory disorders among the inhabitants of Gallies–Abbottabad, northern Pakistan. J. Ethnopharmacol. 2014, 156, 47–60. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).