The Landscape of Virtual Reality Use in Mobility Rehabilitation from 2010–2023: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
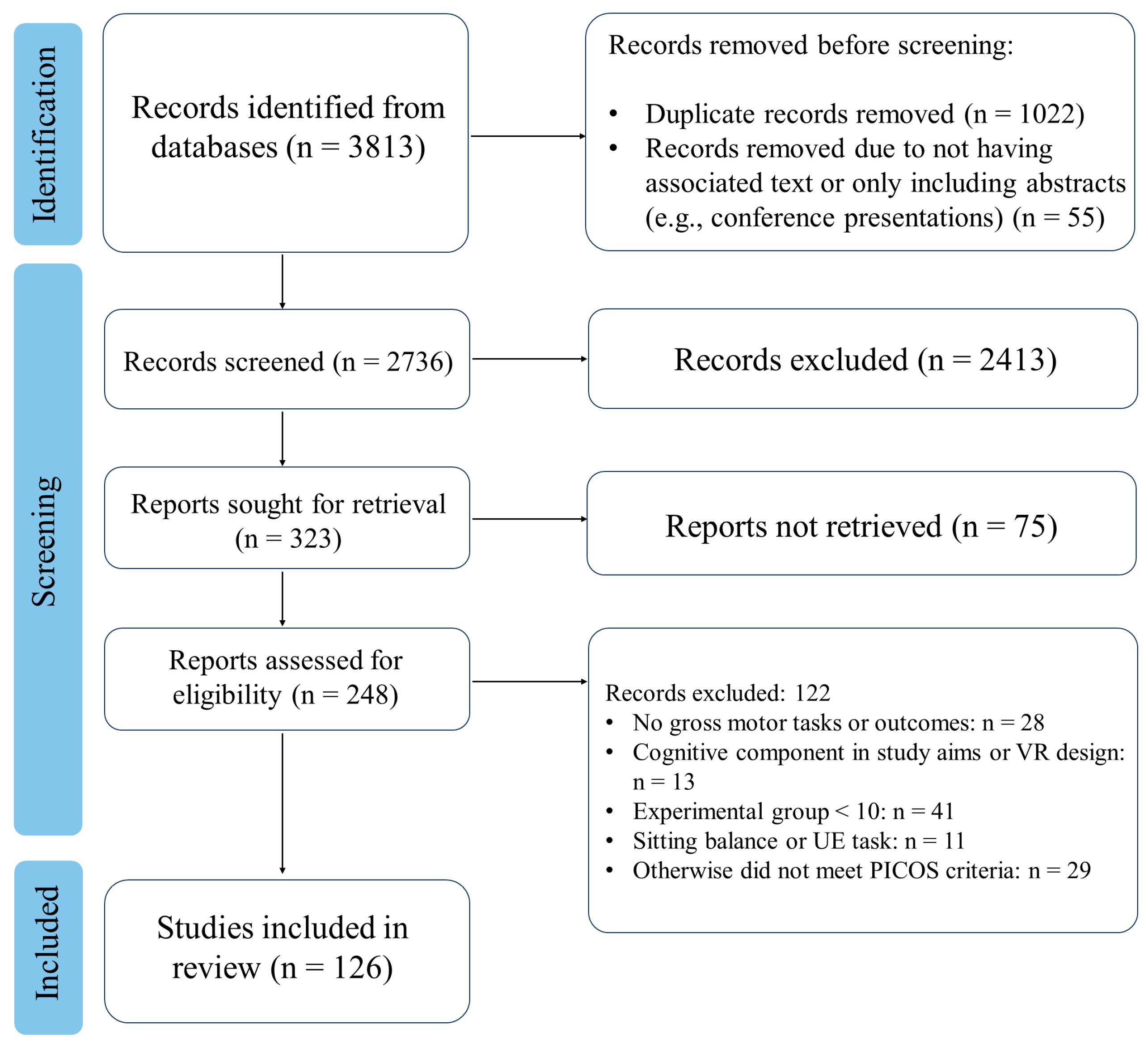
3.1. Study Selection
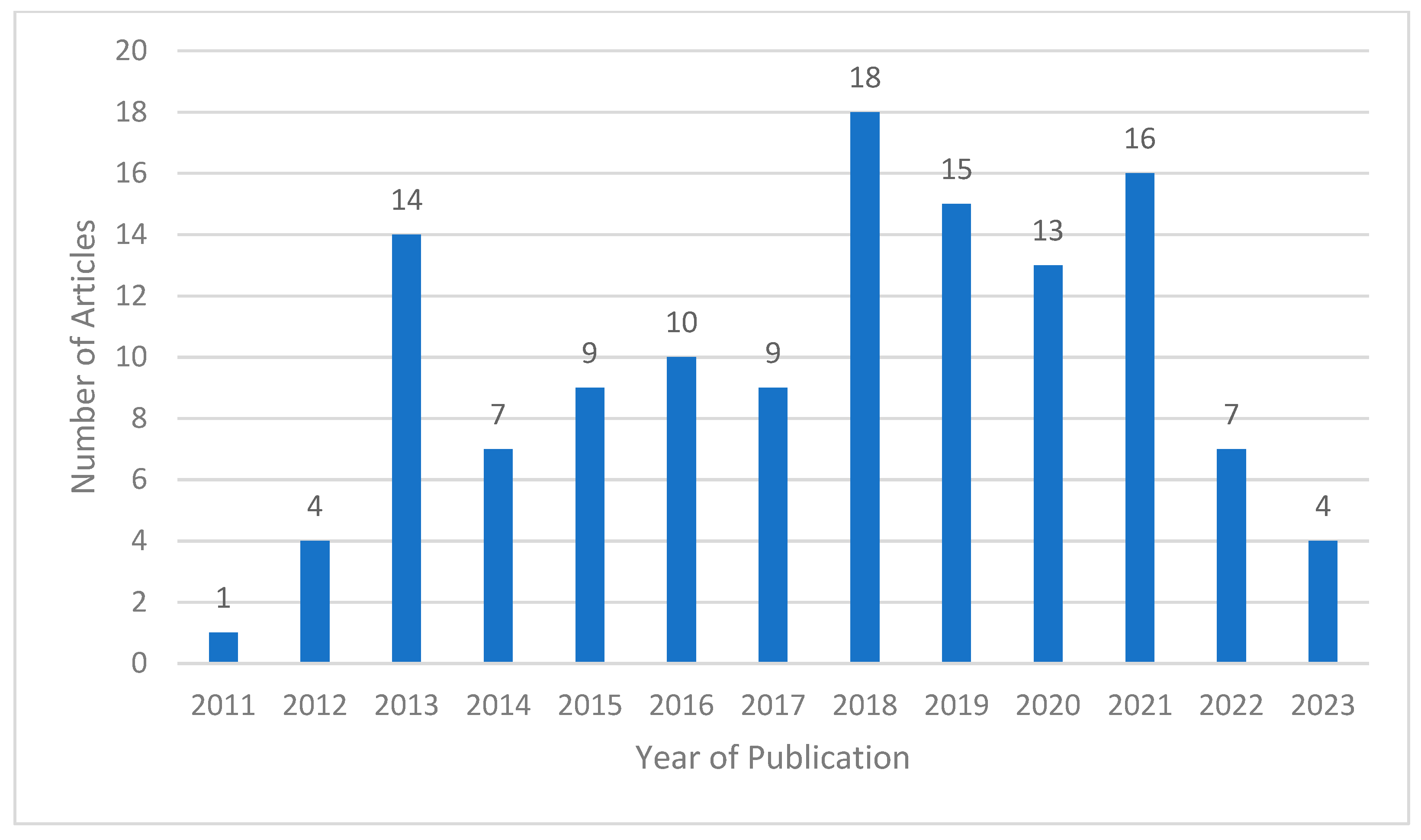
3.2. Publication Year
3.3. Population Studied
3.4. Location and Setting
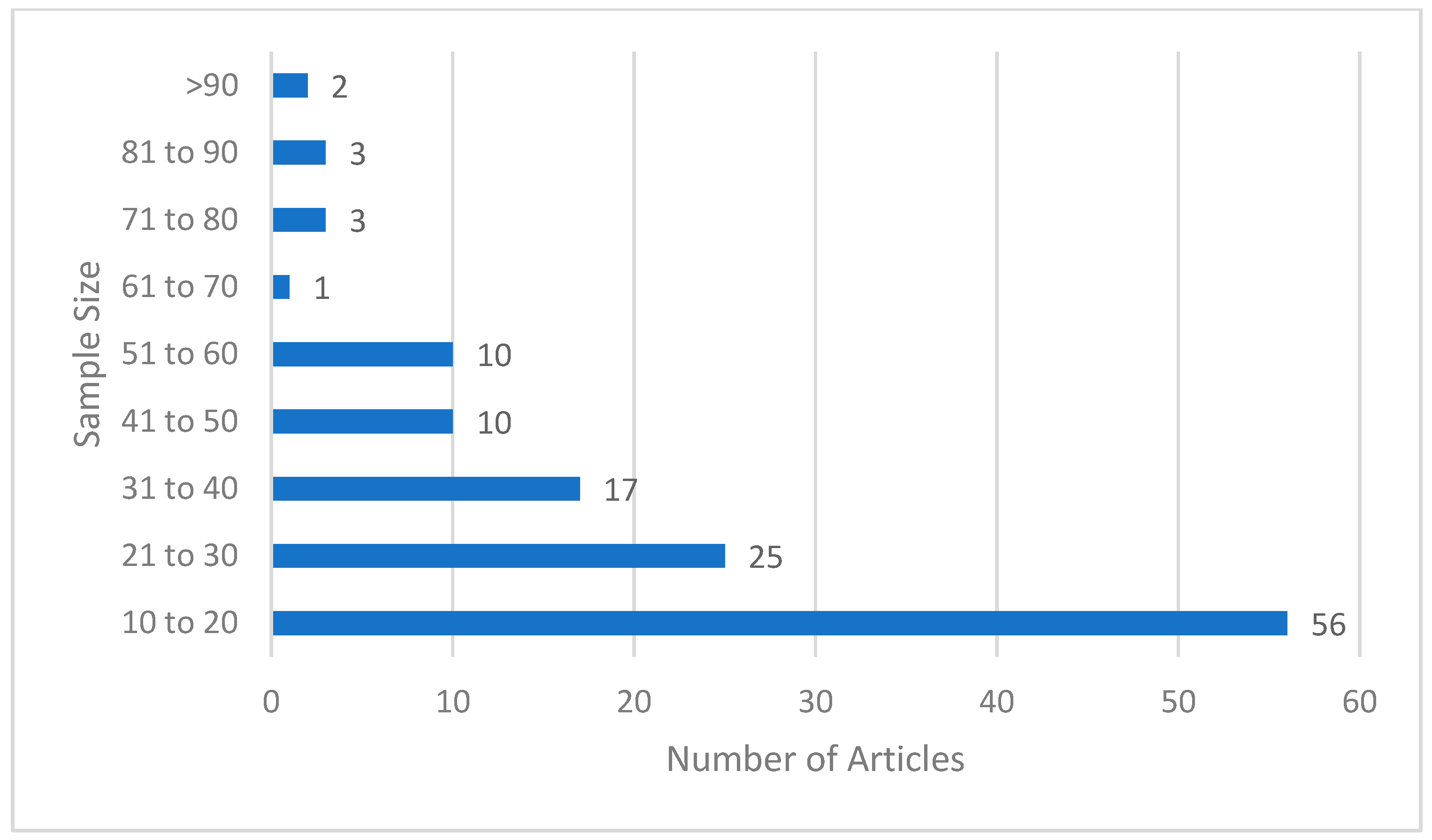
3.5. Study Protocols
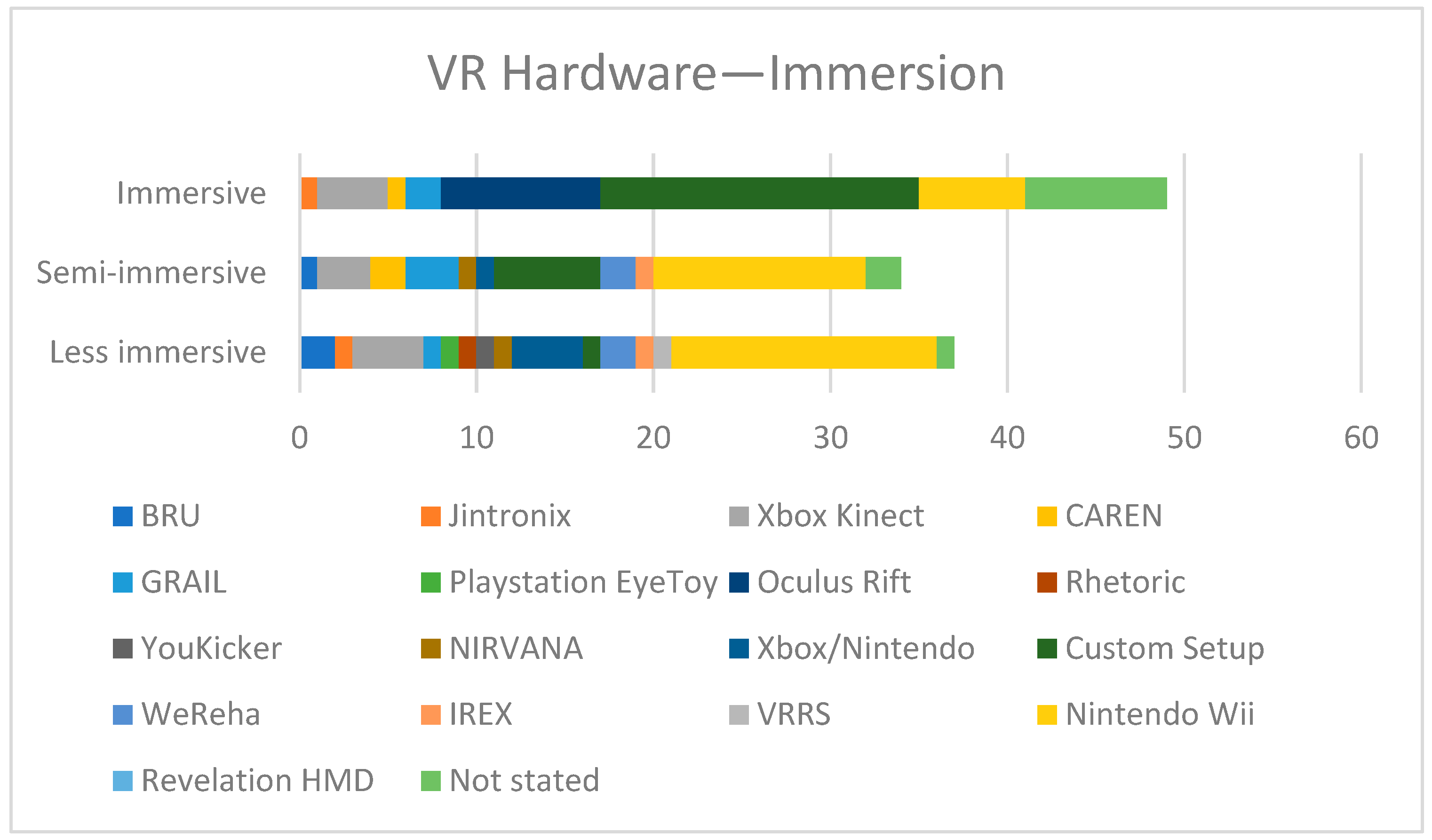
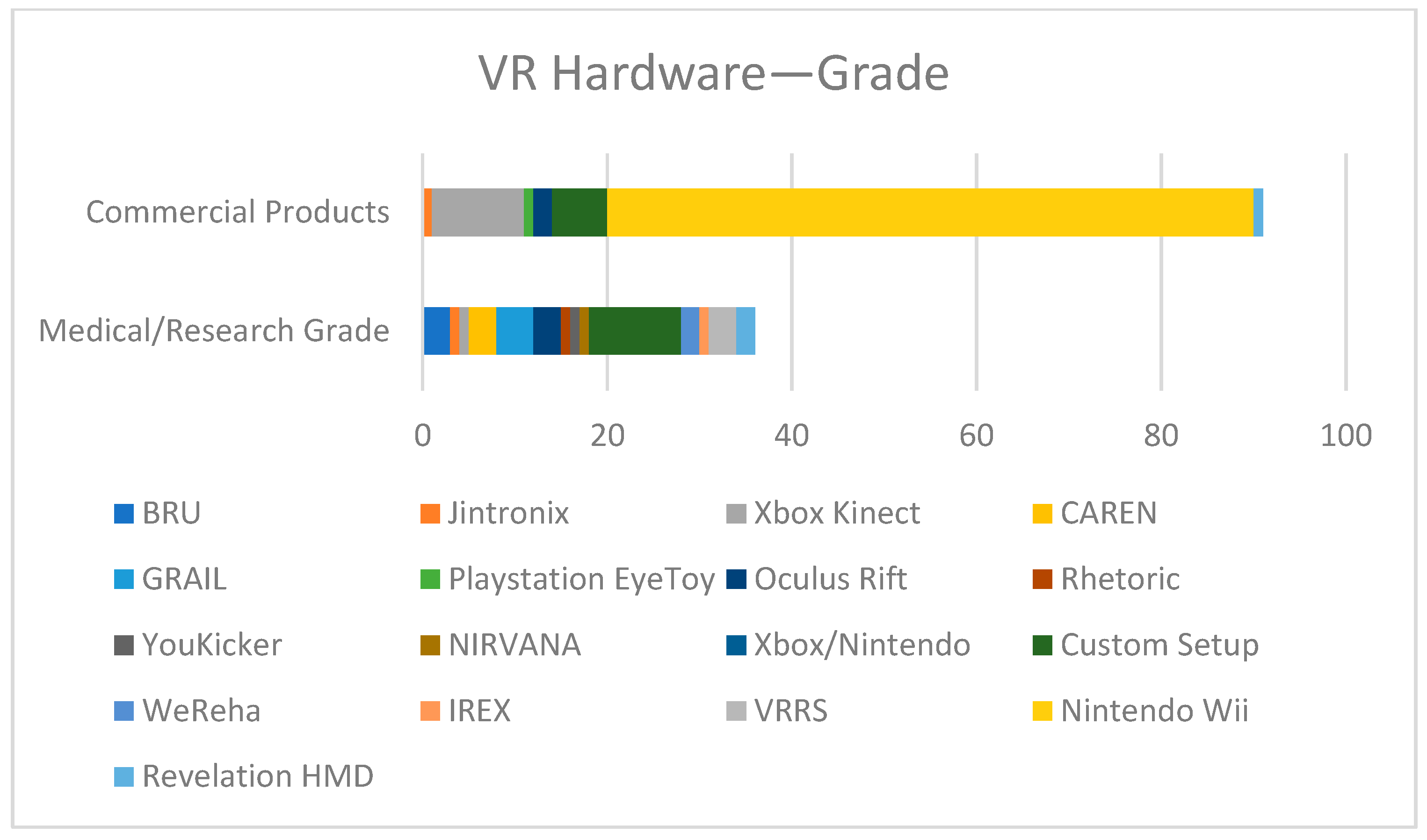
3.6. Virtual Reality Hardware and Software
3.7. Intervention Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bechtold, U.; Stauder, N.; Fieder, M. Let’s walk it: Mobility and the perceived quality of life in older adults. Int. J. Environ. Res. Public Health 2021, 18, 11515. [Google Scholar] [CrossRef]
- Despoti, A.; Karatzanos, E.; Patsaki, I.; Tzoumi, D.; Roussou, G.; Leventakis, N.; Papathanasiou, A.; Nanas, S.; Dimitriadi, N. Immersive virtual reality in cognitive rehabilitation: A systematic review. Health Res. J. 2022, 8, 225–241. [Google Scholar] [CrossRef]
- Patsaki, I.; Avgeri, V.; Rigoulia, T.; Zekis, T.; Koumantakis, G.A.; Grammatopoulou, E. Benefits from incorporating virtual reality in pulmonary rehabilitation of COPD patients: A systematic review and meta-analysis. Adv. Respir. Med. 2023, 91, 324–336. [Google Scholar] [CrossRef] [PubMed]
- Goudman, L.; Jansen, J.; Billot, M.; Vets, N.; Smedt, A.D.; Rouland, M.; Rigoard, P.; Moens, M. Virtual reality applications in chronic pain management: Systematic review and meta-analysis. JMIR Serious Games 2022, 10, e34402. [Google Scholar] [CrossRef]
- Kanschik, D.; Bruno, R.R.; Wolff, G.; Kelm, M.; Jung, C. Virtual and augmented reality in intensive care medicine: A systematic review. Ann. Intensive Care 2023, 13, 81. [Google Scholar] [CrossRef] [PubMed]
- Felsberg, D.T.; Maher, J.P.; Rhea, C.K. The state of behavior change techniques in virtual reality rehabilitation of neurologic populations. Front. Psychol. 2019, 10, 979. [Google Scholar] [CrossRef] [PubMed]
- Howard, M.C. A meta-analysis and systematic literature review of virtual reality rehabilitation programs. Comput. Hum. Behav. 2017, 70, 317–327. [Google Scholar] [CrossRef]
- Cano Porras, D.; Siemonsma, P.; Inzelberg, R.; Zeilig, G.; Plotnik, M. Advantages of virtual reality in the rehabilitation of balance and gait: Systematic review. Neurology 2018, 90, 1017–1025. [Google Scholar] [CrossRef]
- Campo-Prieto, P.; Cancela, J.M.; Rodríguez-Fuentes, G. Immersive virtual reality as physical therapy in older adults: Present or future (systematic review). Virtual Real. 2021, 25, 801–817. [Google Scholar] [CrossRef]
- Jerald, J. The VR Book: Human-Centered Design for Virtual Reality, 1st ed.; ACM Books: New York, NY, USA, 2016. [Google Scholar]
- Rizzo, A.; Koenig, S.T. Is clinical virtual reality ready for primetime? Neuropsychology 2017, 31, 877–899. [Google Scholar] [CrossRef]
- Steinicke, F.; Visell, Y.; Campos, J.; Lécuyer, A. Human Walking in Virtual Environments, 1st ed.; Springer: New York, NY, USA, 2013. [Google Scholar]
- Adamovich, S.V.; Fluet, G.G.; Tunik, E.; Merians, A.S. Sensorimotor training in virtual reality: A review. NeuroRehabilitation 2009, 25, 29–44. [Google Scholar] [CrossRef]
- Levin, M.F. Can virtual reality offer enriched environments for rehabilitation? Expert Rev. Neurother. 2011, 11, 153–155. [Google Scholar] [CrossRef] [PubMed]
- Levac, D.; Sveistrup, H. Motor learning and virtual reality. In Virtual Reality for Physical and Motor Rehabilitation; Weiss, P.L., Keshner, E.A., Levin, M.F., Eds.; Springer: New York, NY, USA, 2014; pp. 25–46. [Google Scholar]
- Zimmerli, L.; Jacky, M.; Lunenburger, L.; Riener, R.; Bolliger, M. Increasing patient engagement during virtual reality-based motor rehabilitation. Arch. Phys. Med. Rehabil. 2013, 94, 1737–1746. [Google Scholar] [CrossRef]
- Góra, T.; Tsos, A.; Indyka, S. Bibliometric analysis of the application of digital technology in physical rehabilitation. Sport Tour. Cent. Eur. J. 2024, 7, 133–146. [Google Scholar] [CrossRef]
- Bateni, H.; Carruthers, J.; Mohan, R.; Pishva, S. Use of virtual reality in physical therapy as an intervention and diagnostic tool. Rehabil. Res. Pract. 2024, 2024, 1122286. [Google Scholar] [CrossRef] [PubMed]
- Cieślik, B.; Mazurek, J.; Wrzeciono, A.; Maistrello, L.; Szczepańska-Gieracha, J.; Conte, P.; Kiper, P. Examining technology-assisted rehabilitation for older adults’ functional mobility: A network meta-analysis on efficacy and acceptability. npj Digit. Med. 2023, 6, 159. [Google Scholar] [CrossRef] [PubMed]
- Pang, W.Y.J.; Cheng, L. Acceptance of gamified virtual reality environments by older adults. Educ. Gerontol. 2023, 49, 830–841. [Google Scholar] [CrossRef]
- Peters, M.D.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 154, 339. [Google Scholar] [CrossRef]
- Afridi, A.; Malik, A.N.; Ali, S.; Amjad, I. Effect of balance training in older adults using Wii Fit Plus. J. Pak. Med. Assoc. 2018, 68, 480–483. [Google Scholar]
- Aharoni, M.M.H.; Lubetzky, A.V.; Arie, L.; Krasovsky, T. Factors associated with dynamic balance in people with Persistent Postural Perceptual Dizziness (PPPD): A cross-sectional study using a virtual-reality Four Square Step Test. J. Neuroeng. Rehabil. 2021, 18, 55. [Google Scholar] [CrossRef] [PubMed]
- Alahmari, K.A.; Sparto, P.J.; Marchetti, G.F.; Redfern, M.S.; Furman, J.M.; Whitney, S.L. Comparison of virtual reality-based therapy with customized vestibular physical therapy for the treatment of vestibular disorders. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 22, 389–399. [Google Scholar] [CrossRef] [PubMed]
- Alhirsan, S.M.; Capó-Lugo, C.E.; Brown, D.A. Effects of different types of augmented feedback on intrinsic motivation and walking speed performance in post-stroke: A study protocol. Contemp. Clin. Trials Commun. 2021, 24, 100863. [Google Scholar] [CrossRef]
- An, C.M.; Park, Y.H. The effects of semi-immersive virtual reality therapy on standing balance and upright mobility function in individuals with chronic incomplete spinal cord injury: A preliminary study. J. Spinal Cord Med. 2018, 41, 223–229. [Google Scholar] [CrossRef]
- Anson, E.; Ma, L.; Meetam, T.; Thompson, E.; Rathore, R.; Dean, V.; Jeka, J. Trunk motion visual feedback during walking improves dynamic balance in older adults: Assessor-blinded randomized controlled trial. Gait Posture 2018, 62, 342–348. [Google Scholar]
- Anwar, N.; Karimi, H.; Ahmad, A.; Mumtaz, N.; Saqulain, G.; Gilani, S.A. A novel virtual reality training strategy for post-stroke patients: A randomized clinical trial. J. Healthc. Eng. 2021, 6598726. [Google Scholar]
- Bang, Y.S.; Son, K.H.; Kim, H.J. Effects of virtual reality training using Nintendo Wii and treadmill walking exercise on balance and walking for stroke patients. J. Phys. Ther. Sci. 2016, 28, 3112–3115. [Google Scholar] [CrossRef]
- Bellomo, R.G.; Paolucci, T.; Saggino, A.; Pezzi, L.; Bramanti, A.; Cimino, V.; Tommasi, M.; Saggini, R. The WeReha project for an innovative home-based exercise training in chronic stroke patients: A clinical study. J. Cent. Nerv. Syst. Dis. 2020, 12, 117957352097986. [Google Scholar] [CrossRef]
- Brachman, A.; Marszałek, W.; Kamieniarz, A.; Michalska, J.; Pawłowski, M.; Juras, G. Biomechanical measures of balance after balance-based exergaming training dedicated for patients with Parkinson’s disease. Gait Posture 2021, 87, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Brachman, A.; Marszałek, W.; Kamieniarz, A.; Michalska, J.; Pawłowski, M.; Akbaş, A.; Juras, G. The effects of exergaming training on balance in healthy elderly women—A pilot study. Int. J. Environ. Res. Public Health 2021, 18, 1412. [Google Scholar] [CrossRef]
- Pazzaglia, C.; Imbimbo, I.; Tranchita, E.; Minganti, C.; Ricciardi, D.; Lo Monaco, R.; Parisi, A.; Padua, L. Comparison of virtual reality rehabilitation and conventional rehabilitation in Parkinson’s disease: A randomized controlled trial. Physiotherapy 2020, 106, 36–42. [Google Scholar] [CrossRef]
- Cacau, L.D.A.P.; Oliveira, G.U.; Maynard, L.G.; Araújo Filho, A.A.; Silva Jr, W.M.; Cerqueria Neto, M.L.; Antoniolli, A.R.; Santana-Filho, V.J. The use of virtual reality as an intervention tool in the postoperative period of cardiac surgery. Rev. Bras. Cir. Cardiovasc. 2013, 28, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Calabrò, R.S.; Naro, A.; Cimino, V.; Buda, A.; Paladina, G.; Di Lorenzo, G.; Manuli, A.; Milardi, D.; Bramanti, P.; Bramanti, A. Improving motor performance in Parkinson’s disease: A preliminary study on the promising use of the computer-assisted virtual reality environment (CAREN). Neurol. Sci. 2020, 41, 933–941. [Google Scholar] [CrossRef]
- Campo-Prieto, P.; Cancela-Carral, J.M.; Rodríguez-Fuentes, G. Feasibility and effects of an immersive virtual reality exergame program on physical functions in institutionalized older adults: A randomized clinical trial. Sensors 2022, 22, 6742. [Google Scholar] [CrossRef] [PubMed]
- Cannell, J.; Jovic, E.; Rathjen, A.; Lane, K.; Tyson, A.M.; Callisaya, M.L.; Smith, S.T.; Ahuja, K.D.K.; Bird, M.-L. The efficacy of interactive, motion capture-based rehabilitation on functional outcomes in an inpatient stroke population: A randomized controlled trial. Clin. Rehabil. 2018, 32, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Cano Porras, D.; Sharon, H.; Inzelberg, R.; Ziv-Ner, Y.; Zeilig, G.; Plotnik, M. Advanced virtual reality-based rehabilitation of balance and gait in clinical practice. Ther. Adv. Chronic Dis. 2019, 10, 2040622319868379. [Google Scholar] [CrossRef]
- Chen, P.J.; Penn, I.W.; Wei, S.H.; Chuang, L.R.; Sung, W.H. Augmented reality-assisted training with selected Tai-Chi movements improves balance control and increases lower limb muscle strength in older adults: A prospective randomized trial. J. Exerc. Sci. Fit. 2020, 18, 142–147. [Google Scholar] [CrossRef]
- Cho, G.H.; Hwangbo, G.; Shin, H.S. The effects of virtual reality-based balance training on balance of the elderly. J. Phys. Ther. Sci. 2014, 26, 615–617. [Google Scholar] [CrossRef]
- Cho, K.H.; Lee, K.J.; Song, C.H. Virtual-reality balance training with a video-game system improves dynamic balance in chronic stroke patients. Tohoku J. Exp. Med. 2012, 228, 69–74. [Google Scholar] [CrossRef]
- Cikajlo, I.; Rudolf, M.; Mainetti, R.; Borghese, N.A. Multi-exergames to set targets and supplement the intensified conventional balance training in patients with stroke: A randomized pilot trial. Front. Psychol. 2020, 11, 572. [Google Scholar] [CrossRef]
- Collado-Mateo, D.; Dominguez-Muñoz, F.J.; Adsuar, J.C.; Merellano-Navarro, E.; Gusi, N. Exergames for women with fibromyalgia: A randomized controlled trial to evaluate the effects on mobility skills, balance, and fear of falling. PeerJ 2017, 5, e3211. [Google Scholar] [CrossRef]
- de Melo, G.E.L.; Kleiner, A.F.R.; Lopes, J.B.P.; Dumont, A.J.L.; Lazzari, R.D.; Galli, M.; Oliveira, C.S. Effect of virtual reality training on walking distance and physical fitness in individuals with Parkinson’s disease. NeuroRehabilitation 2018, 42, 473–480. [Google Scholar] [CrossRef] [PubMed]
- de Rooij, I.J.M.; van de Port, I.G.L.; Punt, M.; Abbink-van Moorsel, P.J.M.; Kortsmit, M.; van Eijk, R.P.A.; Visser-Meily, J.M.A.; Meijer, J.-W.G. Effect of virtual reality gait training on participation in survivors of subacute stroke: A randomized controlled trial. Phys. Ther. 2021, 101, pzab051. [Google Scholar] [CrossRef] [PubMed]
- de Vries, A.W.; Faber, G.; Jonkers, I.; Van Dieen, J.H.; Verschueren, S.M.P. Virtual reality balance training for elderly: Similar skiing games elicit different challenges in balance training. Gait Posture 2018, 59, 111–116. [Google Scholar] [CrossRef]
- Feng, H.; Li, C.; Liu, J.; Wang, L.; Ma, J.; Li, G.; Gan, L.; Shang, X.; Wu, Z. Virtual reality rehabilitation versus conventional physical therapy for improving balance and gait in Parkinson’s disease patients: A randomized controlled trial. Med. Sci. Monit. 2019, 25, 4186–4192. [Google Scholar] [CrossRef] [PubMed]
- Ferraz, D.D.; Trippo, K.V.; Duarte, G.P.; Neto, M.G.; Bernardes Santos, K.O.; Filho, J.O. The effects of functional training, bicycle exercise, and exergaming on walking capacity of elderly patients with Parkinson’s disease: A pilot randomized controlled single-blinded trial. Arch. Phys. Med. Rehabil. 2018, 99, 826–833. [Google Scholar] [CrossRef]
- Finley, J.M.; Gotsis, M.; Lympouridis, V.; Jain, S.; Kim, A.; Fisher, B.E. Design and development of a virtual reality-based mobility training game for people with Parkinson’s disease. Front. Neurol. 2020, 11, 577713. [Google Scholar] [CrossRef]
- Fransson, P.A.; Patel, M.; Jensen, H.; Lundberg, M.; Tjernström, F.; Magnusson, M.; Ekvall Hansson, E. Postural instability in an immersive virtual reality adapts with repetition and includes directional and gender-specific effects. Sci. Rep. 2019, 9, 3168. [Google Scholar] [CrossRef]
- Gagliardi, C.; Turconi, A.C.; Biffi, E.; Maghini, C.; Marelli, A.; Cesareo, A.; Diella, E.; Panzeri, D. Immersive virtual reality to improve walking abilities in cerebral palsy: A pilot study. Ann. Biomed. Eng. 2018, 46, 1376–1384. [Google Scholar] [CrossRef]
- Gandolfi, M.; Geroin, C.; Dimitrova, E.; Boldrini, P.; Waldner, A.; Bonadiman, S.; Picelli, A.; Regazzo, S.; Stirbu, E.; Primon, D.; et al. Virtual reality telerehabilitation for postural instability in Parkinson’s disease: A multicenter, single-blind, randomized, controlled trial. BioMed Res. Int. 2017, 2017, 7962826. [Google Scholar] [CrossRef]
- Garcia, A.P.; Ganança, M.M.; Cusin, F.S.; Tomaz, A.; Ganança, F.F.; Caovilla, H.H. Vestibular rehabilitation with virtual reality in Ménière’s disease. Braz. J. Otorhinolaryngol. 2013, 79, 366–374. [Google Scholar] [CrossRef]
- Gatica-Rojas, V.; Cartes-Velásquez, R.; Guzmán-Muñoz, E.; Méndez-Rebolledo, G.; Soto-Poblete, A.; Pacheco-Espinoza, A.C.; Amigo-Mendoza, C.; Albornoz-Verdugo, M.E.; Elgueta-Cancino, E. Effectiveness of a Nintendo Wii balance board exercise programme on standing balance of children with cerebral palsy: A randomised clinical trial protocol. Contemp. Clin. Trials Commun. 2017, 6, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Gianola, S.; Stucovitz, E.; Castellini, G.; Mascali, M.; Vanni, F.; Tramacere, I.; Banfi, G.; Tornese, D. Effects of early virtual reality-based rehabilitation in patients with total knee arthroplasty: A randomized controlled trial. Medicine 2020, 99, e19136. [Google Scholar] [CrossRef] [PubMed]
- Goffredo, M.; Pournajaf, S.; D’Elia, T.S.; Pellicciari, L.; Bertone, M.; Criscuolo, S.; Damiani, C.; Franceschini, M. Does virtual reality rehabilitation influence postural control after total knee replacement? Gait Posture 2019, 74, 19–20. [Google Scholar] [CrossRef]
- Gómez Álvarez, N.; Venegas Mortecinos, A.; Zapata Rodríguez, V.; López Fontanilla, M.; Maudier Vásquez, M.; Pavez-Adasme, G.; Hemández-Mosqueira, C. Effect of an intervention based on virtual reality on motor development and postural control in children with Down syndrome. Rev. Chil. Pediatr. 2018, 89, 747–752. [Google Scholar] [PubMed]
- Gonçalves, G.B.; Leite, M.A.A.; Orsini, M.; Pereira, J.S. Effects of using the Nintendo Wii Fit Plus platform in the sensorimotor training of gait disorders in Parkinson’s disease. Neurol. Int. 2014, 6, 5048. [Google Scholar] [CrossRef]
- Gulcan, K.; Guclu-Gunduz, A.; Yasar, E.; Ar, U.; Sucullu Karadag, Y.; Saygili, F. The effects of augmented and virtual reality gait training on balance and gait in patients with Parkinson’s disease. Acta Neurol. Belg. 2023, 123, 1917–1925. [Google Scholar] [CrossRef]
- Gutiérrez, R.O.; Galán del Río, F.; Cano de la Cuerda, R.; Alguacil Diego, I.M.; González, R.A.; Page, J.C.M. A telerehabilitation program by virtual reality-video games improves balance and postural control in multiple sclerosis patients. NeuroRehabilitation 2013, 33, 545–554. [Google Scholar] [CrossRef]
- Hadamus, A.; Białoszewski, D.; Błażkiewicz, M.; Kowalska, A.J.; Urbaniak, E.; Wydra, K.T.; Wiaderna, K.; Boratyński, R.; Kobza, A.; Marczyński, W. Assessment of the effectiveness of rehabilitation after total knee replacement surgery using sample entropy and classical measures of body balance. Entropy 2021, 23, 164. [Google Scholar] [CrossRef]
- Hadamus, A.; Błażkiewicz, M.; Wydra, K.T.; Kowalska, A.J.; Łukowicz, M.; Białoszewski, D.; Marczyński, W. Effectiveness of early rehabilitation with exergaming in virtual reality on gait in patients after total knee replacement. J. Clin. Med. 2022, 11, 4950. [Google Scholar] [CrossRef]
- Holmes, J.D.; Gu, M.L.; Johnson, A.M.; Jenkins, M.E. The effects of a home-based virtual reality rehabilitation program on balance among individuals with Parkinson’s disease. Phys. Occup. Ther. Geriatr. 2013, 31, 241–253. [Google Scholar] [CrossRef]
- Ibrahim, M.S.; Mattar, A.G.; Elhafez, S.M. Efficacy of virtual reality-based balance training versus the Biodex balance system training on the body balance of adults. J. Phys. Ther. Sci. 2016, 28, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Imaizumi, L.F.I.; Polastri, P.F.; Penedo, T.; Vieira, L.H.P.; Simieli, L.; Navega, F.R.F.; Monteiro, C.B.M.; Rodrigues, S.T.; Barbieri, F.A. Virtual reality head-mounted goggles increase the body sway of young adults during standing posture. Neurosci. Lett. 2020, 737, 135333. [Google Scholar] [CrossRef]
- Janeh, O.; Fründt, O.; Schönwald, B.; Gulberti, A.; Buhmann, C.; Gerloff, C.; Steinicke, F.; Pötter-Nerger, M. Gait training in virtual reality: Short-term effects of different virtual manipulation techniques in Parkinson’s disease. Cells 2019, 8, 419. [Google Scholar] [CrossRef] [PubMed]
- Jelsma, J.; Pronk, M.; Ferguson, G.; Jelsma-Smit, D. The effect of the Nintendo Wii Fit on balance control and gross motor function of children with spastic hemiplegic cerebral palsy. Dev. Neurorehabil. 2013, 16, 27–37. [Google Scholar] [CrossRef]
- Junior, V.A.D.S.; Santos, M.D.S.; Ribeiro, N.M.D.S.; Maldonado, I.L. Combining proprioceptive neuromuscular facilitation and virtual reality for improving sensorimotor function in stroke survivors: A randomized clinical trial. J. Cent. Nerv. Syst. Dis. 2019, 11, 1179573519863826. [Google Scholar] [CrossRef] [PubMed]
- Kafri, M.; Weiss, P.L.; Zeilig, G.; Bondi, M.; Baum-Cohen, I.; Kizony, R. Performance in complex life situations: Effects of age, cognition, and walking speed in virtual versus real-life environments. J. Neuroeng. Rehabil. 2021, 18, 30. [Google Scholar] [CrossRef]
- Kalron, A.; Fonkatz, I.; Frid, L.; Baransi, H.; Achiron, A. The effect of balance training on postural control in people with multiple sclerosis using the CAREN virtual reality system: A pilot randomized controlled trial. J. Neuroeng. Rehabil. 2016, 13, 13. [Google Scholar] [CrossRef]
- Kamińska, M.S.; Miller, A.; Rotter, I.; Szylińska, A.; Grochans, E. The effectiveness of virtual reality training in reducing the risk of falls among elderly people. Clin. Interv. Aging 2018, 13, 2329–2338. [Google Scholar] [CrossRef]
- Kantha, P.; Hsu, W.L.; Chen, P.J.; Tsai, Y.C.; Lin, J.J. A novel balance training approach: Biomechanical study of virtual reality-based skateboarding. Front. Bioeng. Biotechnol. 2023, 11, 1136368. [Google Scholar] [CrossRef]
- Kanyılmaz, T.; Topuz, O.; Ardıç, F.N.; Alkan, H.; Öztekin, S.N.S.; Topuz, B.; Ardıç, F. Effectiveness of conventional versus virtual reality-based vestibular rehabilitation exercises in elderly patients with dizziness: A randomized controlled study with 6-month follow-up. Braz. J. Otorhinolaryngol. 2022, 88 (Suppl. S3), S41–S49. [Google Scholar] [CrossRef]
- Karasu, A.U.; Batur, E.B.; Karataş, G.K. Effectiveness of Wii-based rehabilitation in stroke: A randomized controlled study. J. Rehabil. Med. 2018, 50, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Khalil, H.; Al-Sharman, A.; El-Salem, K.; Alghwiri, A.A.; Al-Shorafat, D.; Khazaaleh, S.; Abu Foul, L. The development and pilot evaluation of virtual reality balance scenarios in people with multiple sclerosis (MS): A feasibility study. NeuroRehabilitation 2018, 43, 473–482. [Google Scholar] [CrossRef]
- Kim, J.; Son, J.; Ko, N.; Yoon, B. Unsupervised virtual reality-based exercise program improves hip muscle strength and balance control in older adults: A pilot study. Arch. Phys. Med. Rehabil. 2013, 94, 937–943. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.J.; Heo, M. Comparison of virtual reality exercise versus conventional exercise on balance in patients with functional ankle instability: A randomized controlled trial. J. Back Musculoskelet. Rehabil. 2019, 32, 905–911. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.J.; Heo, M. Effects of virtual reality programs on balance in functional ankle instability. J. Phys. Ther. Sci. 2015, 27, 3097–3101. [Google Scholar] [CrossRef]
- Kim, N.; Park, Y.; Lee, B.H. Effects of community-based virtual reality treadmill training on balance ability in patients with chronic stroke. J. Phys. Ther. Sci. 2015, 27, 655–658. [Google Scholar] [CrossRef]
- Kiper, P.; Luque-Moreno, C.; Pernice, S.; Maistrello, L.; Agostini, M.; Turolla, A. Functional changes in the lower extremity after non-immersive virtual reality and physiotherapy following stroke. J. Rehabil. Med. 2020, 52, jrm00122. [Google Scholar] [CrossRef]
- Kumar, D.; Sinha, N.; Dutta, A.; Lahiri, U. Virtual reality-based balance training system augmented with operant conditioning paradigm. Biomed. Eng. Online 2019, 18, 90. [Google Scholar] [CrossRef]
- Kwon, J.A.; Shin, Y.K.; Kim, D.J.; Cho, S.R. Effects of balance training using a virtual reality program in hemiplegic patients. Int. J. Environ. Res. Public Health 2022, 19, 2805. [Google Scholar] [CrossRef]
- Lee, H.Y.; Kim, Y.L.; Lee, S.M. Effects of virtual reality-based training and task-oriented training on balance performance in stroke patients. J. Phys. Ther. Sci. 2015, 27, 1883–1888. [Google Scholar] [CrossRef]
- Lee, K. Speed-interactive pedaling training using smartphone virtual reality application for stroke patients: Single-blinded, randomized clinical trial. Brain Sci. 2019, 9, 295. [Google Scholar] [CrossRef] [PubMed]
- Lee, K. Virtual reality gait training to promote balance and gait among older people: A randomized clinical trial. Geriatrics 2020, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.M.; Shin, D.C.; Song, C.H. Canoe game-based virtual reality training to improve trunk postural stability, balance, and upper limb motor function in subacute stroke patients: A randomized controlled pilot study. J. Phys. Ther. Sci. 2016, 28, 2019–2024. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.Y.; Lee, D.K.; Song, H.S. Effect of virtual reality dance exercise on the balance, activities of daily living, and depressive disorder status of Parkinson’s disease patients. J. Phys. Ther. Sci. 2015, 27, 145–147. [Google Scholar] [CrossRef]
- Lee, S.; Shin, S. Effectiveness of virtual reality using video gaming technology in elderly adults with diabetes mellitus. Diabetes Technol. Ther. 2013, 15, 489–496. [Google Scholar] [CrossRef]
- Lheureux, A.; Lebleu, J.; Frisque, C.; Sion, C.; Stoquart, G.; Warlop, T.; Detrembleur, C.; Lejeune, T. Immersive virtual reality to restore natural long-range autocorrelations in Parkinson’s disease patients’ gait during treadmill walking. Front. Physiol. 2020, 11, 572063. [Google Scholar] [CrossRef]
- Liao, Y.Y.; Yang, Y.R.; Cheng, S.J.; Wu, Y.R.; Fuh, J.L.; Wang, R.Y. Virtual reality–based training to improve obstacle-crossing performance and dynamic balance in patients with Parkinson’s disease. Neurorehabil. Neural Repair 2015, 29, 658–667. [Google Scholar] [CrossRef]
- Lima Rebêlo, F.; de Souza Silva, L.F.; Doná, F.; Sales Barreto, A.; de Souza Siqueira Quintans, J. Immersive virtual reality is effective in the rehabilitation of older adults with balance disorders: A randomized clinical trial. Exp. Gerontol. 2021, 149, 111308. [Google Scholar] [CrossRef]
- Lloréns, R.; Colomer-Font, C.; Alcañiz, M.; Noé-Sebastián, E. BioTrak: Análisis de efectividad y satisfacción de un sistema de realidad virtual para la rehabilitación del equilibrio en pacientes con daño cerebral. Neurología 2013, 28, 268–275. [Google Scholar] [CrossRef]
- Lloréns, R.; Gil-Gómez, J.A.; Alcañiz, M.; Colomer, C.; Noé, E. Improvement in balance using a virtual reality-based stepping exercise: A randomized controlled trial involving individuals with chronic stroke. Clin. Rehabil. 2015, 29, 261–268. [Google Scholar] [CrossRef]
- Malik, A.N.; Masood, T. Effects of virtual reality training on mobility and physical function in stroke. JPMA J. Pak. Med. Assoc. 2017, 67, 1618–1620. [Google Scholar]
- Martelli, D.; Xia, B.; Prado, A.; Agrawal, S.K. Gait adaptations during overground walking and multidirectional oscillations of the visual field in a virtual reality headset. Gait Posture 2019, 67, 251–256. [Google Scholar] [CrossRef] [PubMed]
- McEwen, D.; Taillon-Hobson, A.; Bilodeau, M.; Sveistrup, H.; Finestone, H. Virtual reality exercise improves mobility after stroke: An inpatient randomized controlled trial. Stroke 2014, 45, 1853–1855. [Google Scholar] [CrossRef]
- Meldrum, D.; Herdman, S.; Moloney, R.; Murray, D.; Duffy, D.; Malone, K.; French, H.; Hone, S.; Conroy, R.; McConn-Walsh, R. Effectiveness of conventional versus virtual reality-based vestibular rehabilitation in the treatment of dizziness, gait, and balance impairment in adults with unilateral peripheral vestibular loss: A randomised controlled trial. BMC Ear Nose Throat Disord. 2012, 12, 3. [Google Scholar] [CrossRef] [PubMed]
- Micarelli, A.; Viziano, A.; Micarelli, B.; Augimeri, I.; Alessandrini, M. Vestibular rehabilitation in older adults with and without mild cognitive impairment: Effects of virtual reality using a head-mounted display. Arch. Gerontol. Geriatr. 2019, 83, 246–256. [Google Scholar] [CrossRef]
- Miclaus, R.S.; Roman, N.; Henter, R.; Caloian, S. Lower extremity rehabilitation in patients with post-stroke sequelae through virtual reality associated with mirror therapy. Int. J. Environ. Res. Public Health 2021, 18, 2654. [Google Scholar] [CrossRef] [PubMed]
- Mirelman, A.; Maidan, I.; Herman, T.; Deutsch, J.E.; Giladi, N.; Hausdorff, J.M. Virtual reality for gait training: Can it induce motor learning to enhance complex walking and reduce fall risk in patients with Parkinson’s disease? J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011, 66, 234–240. [Google Scholar] [CrossRef]
- Mohammadi, N.; Hadian, M.R.; Olyaei, G.R. Compare the effect of traditional and virtual reality training on subjective-sense of instability and balance in basketball players with functional ankle instability: Matched randomized clinical trial. J. Biomed. Phys. Eng. 2023, 13, 269–280. [Google Scholar] [CrossRef]
- Morone, G.; Paolucci, T.; Luziatelli, S.; Iosa, M.; Piermattei, C.; Zangrando, F.; Paolucci, S.; Vulpiani, M.C.; Saraceni, V.M.; Baldari, C.; et al. Wii Fit is effective in women with bone loss condition associated with balance disorders: A randomized controlled trial. Aging Clin. Exp. Res. 2016, 28, 1187–1193. [Google Scholar] [CrossRef]
- Nuic, D.; Vinti, M.; Karachi, C.; Foulon, P.; Van Hamme, A.; Welter, M.-L. The feasibility and positive effects of a customised videogame rehabilitation programme for freezing of gait and falls in Parkinson’s disease patients: A pilot study. J. NeuroEng. Rehabil. 2018, 15, 31. [Google Scholar] [CrossRef]
- Oh, K.; Stanley, C.J.; Damiano, D.L.; Kim, J.; Yoon, J.; Park, H.S. Biomechanical evaluation of virtual reality-based turning on a self-paced linear treadmill. Gait Posture 2018, 65, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Gutiérrez, R.; Cano-de-la-Cuerda, R.; Galán-del-Río, F.; Alguacil-Diego, I.M.; Palacios-Ceña, D.; Miangolarra-Page, J.C. A telerehabilitation program improves postural control in multiple sclerosis patients: A Spanish preliminary study. Int. J. Environ. Res. Public Health 2013, 10, 5697–5710. [Google Scholar] [CrossRef]
- Park, E.C.; Kim, S.G.; Lee, C.W. The effects of virtual reality game exercise on balance and gait of the elderly. J. Phys. Ther. Sci. 2015, 27, 1157–1159. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.H.; Lee, C.H.; Lee, B.H. Clinical usefulness of the virtual reality-based postural control training on the gait ability in patients with stroke. J. Exerc. Rehabil. 2013, 9, 489–494. [Google Scholar] [CrossRef]
- Pedreira Da Fonseca, E.; Ribeiro Da Silva, N.M.; Pinto, E.B. Therapeutic effect of virtual reality on post-stroke patients: Randomized clinical trial. J. Stroke Cerebrovasc. Dis. 2017, 26, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Peri, E.; Panzeri, D.; Beretta, E.; Reni, G.; Strazzer, S.; Biffi, E. Motor improvement in adolescents affected by ataxia secondary to acquired brain injury: A pilot study. BioMed Res. Int. 2019, 2019, 8967138. [Google Scholar] [CrossRef]
- Phu, S.; Vogrin, S.; Al Saedi, A.; Duque, G. Balance training using virtual reality improves balance and physical performance in older adults at high risk of falls. Clin. Interv. Aging 2019, 14, 1567–1577. [Google Scholar] [CrossRef]
- Punt, I.M.; Armand, S.; Ziltener, J.L.; Allet, L. Effect of Wii Fit™ exercise therapy on gait parameters in ankle sprain patients: A randomized controlled trial. Gait Posture 2017, 58, 52–58. [Google Scholar] [CrossRef]
- Raffegeau, T.E.; Clark, M.; Fawver, B.; Engel, B.T.; Young, W.R.; Williams, A.M.; Lohse, K.R.; Fino, P.C. The effect of mobility-related anxiety on walking across the lifespan: A virtual reality simulation study. Exp. Brain Res. 2023, 241, 1757–1768. [Google Scholar] [CrossRef]
- Rajaratnam, B.S.; Gui, K.J.; Lee, J.K.; Kwek, S.; Sim, F.; Lee, E.; Ang, Y.; Ng, K.; Su, Y.; Woo, W.; et al. Does the inclusion of virtual reality games within conventional rehabilitation enhance balance retraining after a recent episode of stroke? Rehabil. Res. Pract. 2013, 2013, 649561. [Google Scholar] [CrossRef]
- Rendon, A.A.; Lohman, E.B.; Thorpe, D.; Johnson, E.G.; Medina, E.; Bradley, B. The effect of virtual reality gaming on dynamic balance in older adults. Age Ageing 2012, 41, 549–552. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, E.V.; Gallo, L.H.; Guimarães, A.T.B.; Melo Filho, J.; Luna, B.C.; Gomes, A.R.S. Effects of dance exergaming on depressive symptoms, fear of falling, and musculoskeletal function in fallers and nonfallers community-dwelling older women. Rejuvenation Res. 2018, 21, 518–526. [Google Scholar] [CrossRef]
- Rosiak, O.; Krajewski, K.; Woszczak, M.; Jozefowicz-Korczynska, M. Evaluation of the effectiveness of a virtual reality-based exercise program for unilateral peripheral vestibular deficit. J. Vestib. Res. Equilib. Orientat. 2018, 28, 409–415. [Google Scholar] [CrossRef]
- Shema, S.R.; Brozgol, M.; Dorfman, M.; Maidan, I.; Sharaby-Yeshayahu, L.; Malik-Kozuch, H.; Wachsler Yannai, O.; Giladi, N.; Hausdorff, J.M.; Mirelman, A. Clinical experience using a 5-week treadmill training program with virtual reality to enhance gait in an ambulatory physical therapy service. Phys. Ther. 2014, 94, 1319–1326. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, H.; Jehu, D.A.; Daneshjoo, A.; Shakoor, E.; Razeghi, M.; Amani, A.; Hakim, M.N.; Yusof, A. Effects of 8 weeks of balance training, virtual reality training, and combined exercise on lower limb muscle strength, balance, and functional mobility among older men: A randomized controlled trial. Sports Health 2021, 13, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Salem, Y.; Gropack, S.J.; Coffin, D.; Godwin, E.M. Effectiveness of a low-cost virtual reality system for children with developmental delay: A preliminary randomized single-blind controlled trial. Physiotherapy 2012, 98, 189–195. [Google Scholar] [CrossRef]
- Sana, V.; Ghous, M.; Kashif, M.; Albalwi, A.; Muneer, R.; Zia, M. Effects of vestibular rehabilitation therapy versus virtual reality on balance, dizziness, and gait in patients with subacute stroke: A randomized controlled trial. Medicine 2023, 102, e33203. [Google Scholar] [CrossRef]
- Santos, P.; Machado, T.; Santos, L.; Ribeiro, N.; Melo, A. Efficacy of the Nintendo Wii combination with conventional exercises in the rehabilitation of individuals with Parkinson’s disease: A randomized clinical trial. NeuroRehabilitation 2019, 45, 255–263. [Google Scholar] [CrossRef]
- Sengupta, M.; Gupta, A.; Khanna, M.; Rashmi Krishnan, U.K.; Chakrabarti, D. Role of virtual reality in balance training in patients with spinal cord injury: A prospective comparative pre-post study. Asian Spine J. 2020, 14, 51–58, Erratum in Asian Spine J. 2020, 14, 268. https://doi.org/10.31616/asj.2019.0013.e1. [Google Scholar] [CrossRef]
- Severiano, M.I.R.; Zeigelboim, B.S.; Teive, H.A.G.; Santos, G.J.B.; Fonseca, V.R. Effect of virtual reality in Parkinson’s disease: A prospective observational study. Arq. Neuropsiquiatr. 2018, 76, 78–84. [Google Scholar] [CrossRef]
- Sheehy, L.; Taillon-Hobson, A.; Sveistrup, H.; Bilodeau, M.; Fergusson, D.; Levac, D.; Finestone, H. Does the addition of virtual reality training to a standard program of inpatient rehabilitation improve sitting balance ability and function after stroke? Protocol for a single-blind randomized controlled trial. BMC Neurol. 2016, 16, 42. [Google Scholar] [CrossRef] [PubMed]
- Shema, S.R.; Bezalel, P.; Sberlo, Z.; Yannai, O.W.; Giladi, N.; Hausdorff, J.M.; Mirelman, A. Improved mobility and reduced fall risk in older adults after five weeks of virtual reality training. J. Altern. Med. Res. 2017, 9, 171–175. [Google Scholar]
- Shideler, B.L.; Martelli, D.; Prado, A.; Agrawal, S.K. Overground gait training using virtual reality aimed at gait symmetry. Hum. Mov. Sci. 2021, 76, 102770. [Google Scholar] [CrossRef]
- Singh, D.K.A.; Rajaratnam, B.S.; Palaniswamy, V.; Raman, V.P.; Bong, P.S.; Pearson, H. Effects of balance-focused interactive games compared to therapeutic balance classes for older women. Climacteric J. Int. Menopause Soc. 2013, 16, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.K.A.; Nordin, N.A.M.; Abd Aziz, N.A.; Beng Kooi, L.; Li Ching, S. Effects of substituting a portion of standard physiotherapy time with virtual reality games among community-dwelling stroke survivors. BMC Neurol. 2013, 13, 199. [Google Scholar] [CrossRef] [PubMed]
- Song, G.B.; Park, E.C. Effect of virtual reality games on stroke patients’ balance, gait, depression, and interpersonal relationships. J. Phys. Ther. Sci. 2015, 27, 2057–2060. [Google Scholar] [CrossRef]
- Takami, A.; Watanabe, K.; Makino, M. Immediate effect of video viewing with an illusion of walking at a faster speed using virtual reality on actual walking of stroke patients. J. Phys. Ther. Sci. 2021, 33, 560–564. [Google Scholar] [CrossRef]
- Tarakci, D.; Ersoz Huseyinsinoglu, B.; Tarakci, E.; Razak Ozdincler, A. Effects of Nintendo Wii-Fit® video games on balance in children with mild cerebral palsy. Pediatr. Int. 2016, 58, 1042–1050. [Google Scholar] [CrossRef]
- Tefertiller, C.; Hays, K.; Natale, A.; O’Dell, D.; Ketchum, J.; Sevigny, M.; Eagye, C.B.; Philippus, A.; Harrison-Felix, C. Results from a randomized controlled trial to address balance deficits after traumatic brain injury. Arch. Phys. Med. Rehabil. 2019, 100, 1409–1416. [Google Scholar] [CrossRef]
- Tsang, W.W.N.; Fu, A.S.N. Virtual reality exercise to improve balance control in older adults at risk of falling. Hong Kong Med. J. 2016, 22 (Suppl. S2), S19–S22. [Google Scholar] [CrossRef]
- Valiani, V.; Lauzé, M.; Martel, D.; Pahor, M.; Manini, T.M.; Anton, S.; Aubertin-Leheudre, M. A new adaptive home-based exercise technology among older adults living in nursing homes: A pilot study on feasibility, acceptability, and physical performance. J. Nutr. Health Aging 2017, 21, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Van Dijsseldonk, R.B.; De Jong, L.A.F.; Groen, B.E.; Vos-van Der Hulst, M.; Geurts, A.C.H.; Keijsers, N.L.W. Gait stability training in a virtual environment improves gait and dynamic balance capacity in incomplete spinal cord injury patients. Front. Neurol. 2018, 9, 963. [Google Scholar] [CrossRef] [PubMed]
- Villiger, M.; Liviero, J.; Awai, L.; Stoop, R.; Pyk, P.; Clijsen, R.; Curt, A.; Eng, K.; Bolliger, M. Home-based virtual reality-augmented training improves lower limb muscle strength, balance, and functional mobility following chronic incomplete spinal cord injury. Front. Neurol. 2017, 8, 635. [Google Scholar] [CrossRef]
- Villiger, M.; Bohli, D.; Kiper, D.; Pyk, P.; Spillmann, J.; Meilick, B.; Curt, A.; Hepp-Reymond, M.C.; Hotz-Boendermaker, S.; Eng, K. Virtual reality–augmented neurorehabilitation improves motor function and reduces neuropathic pain in patients with incomplete spinal cord injury. Neurorehabil. Neural Repair 2013, 27, 675–683. [Google Scholar] [CrossRef]
- Wiskerke, E.; Kool, J.; Hilfiker, R.; Sattelmayer, K.M.; Verheyden, G. Determining the optimal virtual reality exergame approach for balance therapy in persons with neurological disorders using a Rasch analysis: Longitudinal observational study. JMIR Serious Games 2022, 10, e30366. [Google Scholar] [CrossRef]
- Wüest, S.; Borghese, N.A.; Pirovano, M.; Mainetti, R.; van de Langenberg, R.; de Bruin, E.D. Usability and effects of an exergame-based balance training program. Games Health J. 2014, 3, 106–114. [Google Scholar] [CrossRef]
- Yaman, F.; Leblebicier, M.A.; Okur, İ.; Kızılkaya, M.İ.; Kavuncu, V. Is virtual reality training superior to conventional treatment in improving lower extremity motor function in chronic hemiplegic patients? Turk. J. Phys. Med. Rehabil. 2022, 68, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.C.; Wang, H.K.; Wu, R.M.; Lo, C.S.; Lin, K.H. Home-based virtual reality balance training and conventional balance training in Parkinson’s disease: A randomized controlled trial. J. Formos. Med. Assoc. 2016, 115, 734–743. [Google Scholar] [CrossRef]
- Xu, Y.; Tong, M.; Ming, W.K.; Lin, Y.; Mai, W.; Huang, W.; Chen, Z. A depth camera–based, task-specific virtual reality rehabilitation game for patients with stroke: Pilot usability study. JMIR Serious Games 2021, 9, e20916. [Google Scholar] [CrossRef]
- Yeh, S.C.; Chen, S.; Wang, P.C.; Su, M.C.; Chang, C.H.; Tsai, P.Y. Interactive 3-dimensional virtual reality rehabilitation for patients with chronic imbalance and vestibular dysfunction. Technol. Health Care 2014, 22, 915–921. [Google Scholar] [CrossRef]
- Yin, C.; Hsueh, Y.H.; Yeh, C.Y.; Lo, H.C.; Lan, Y.T. A virtual reality-cycling training system for lower limb balance improvement. BioMed Res. Int. 2016, 2016, 9276508. [Google Scholar] [CrossRef]
- Yom, C.; Cho, H.Y.; Lee, B. Effects of virtual reality-based ankle exercise on the dynamic balance, muscle tone, and gait of stroke patients. J. Phys. Ther. Sci. 2015, 27, 845–849. [Google Scholar] [CrossRef]
- Yousefi Babadi, S.; Daneshmandi, H. Effects of virtual reality versus conventional balance training on balance of the elderly. Exp. Gerontol. 2021, 153, 111498. [Google Scholar] [CrossRef]
- Zahedian-Nasab, N.; Jaberi, A.; Shirazi, F.; Kavousipor, S. Effect of virtual reality exercises on balance and fall in elderly people with fall risk: A randomized controlled trial. BMC Geriatr. 2021, 21, 509. [Google Scholar] [CrossRef]
- Greenwald, A.G. Consequences of prejudice against the null hypothesis. Psychol. Bull. 1975, 82, 1–20. [Google Scholar] [CrossRef]
- Lohse, K.; Buchanan, T.; Miller, M. Underpowered and overworked: Problems with data analysis in motor learning studies. J. Mot. Learn. Dev. 2016, 4, 37–58. [Google Scholar] [CrossRef]
- Cheng, L.; Sunzi, K.; Dai, F.; Liu, X.; Wang, Y.; Zhang, B.; He, L.; Ju, M. Effects of virtual reality rehabilitation training on gait and balance in patients with Parkinson’s disease: A systematic review. PLoS ONE 2019, 14, e0224819. [Google Scholar]
- Charness, G.; Gneezy, U.; Kuhn, M.A. Experimental methods: Between-subject and within-subject design. J. Econ. Behav. Organ. 2012, 81, 1–8. [Google Scholar] [CrossRef]
- Schwartz, C.E.; Chesney, M.A.; Irvine, M.J.; Keefe, F.J. The control group dilemma in clinical research: Applications for psychosocial and behavioral medicine trials. Psychosom. Med. 1997, 59, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Ortman, J.; Velkoff, V.; Hogan, H. An Aging Nation: The Older Population in the United States; U.S. Census Bureau: Washington, DC, USA, 2014. [Google Scholar]
- Basford, J.R.; Chou, L.S.; Kaufman, K.R.; Brey, R.H.; Walker, A.; Malec, J.F.; Moessner, A.M.; Brown, A.W. An assessment of gait and balance deficits after traumatic brain injury. Arch. Phys. Med. Rehabil. 2003, 84, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Murray, R.F.; Asghari, A.; Egorov, D.D.; Rutkowski, S.B.; Siddall, P.J.; Soden, R.J.; Ruff, R. Impact of spinal cord injury on self-perceived pre- and postmorbid cognitive, emotional, and physical functioning. Spinal Cord 2007, 45, 429–436. [Google Scholar] [CrossRef]
- Chen, C.H.; Jeng, M.C.; Fung, C.P.; Doong, J.L.; Chuang, T.Y. Psychological benefits of virtual reality for patients in rehabilitation therapy. J. Sport Rehabil. 2009, 18, 258–268. [Google Scholar] [CrossRef]
- Qian, J.; McDonough, D.J.; Gao, Z. The effectiveness of virtual reality exercise on individuals’ physiological, psychological, and rehabilitative outcomes: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 4133. [Google Scholar] [CrossRef]
- Ambrose, A.F.; Paul, G.; Hausdorff, J.M. Risk factors for falls among older adults: A review of the literature. Maturitas 2013, 75, 51–61. [Google Scholar] [CrossRef]
- Alexander, N.B. Postural control in older adults. J. Am. Geriatr. Soc. 1994, 42, 93–108. [Google Scholar] [CrossRef]
- Dermody, G.; Whitehead, L.; Wilson, G.; Glass, C. The role of virtual reality in improving health outcomes for community-dwelling older adults: Systematic review. J. Med. Internet Res. 2020, 22, e17331. [Google Scholar] [CrossRef]
- Molina, K.I.; Ricci, N.A.; de Moraes, S.A.; Perracini, M.R. Virtual reality using games for improving physical functioning in older adults: A systematic review. J. Neuroeng. Rehabil. 2014, 11, 156. [Google Scholar] [CrossRef]
- Neri, S.G.; Cardoso, J.R.; Cruz, L.; Lima, R.M.; de Oliveira, R.J.; Iversen, M.D.; Carregaro, R.L. Do virtual reality games improve mobility skills and balance measurements in community-dwelling older adults? Systematic review and meta-analysis. Clin. Rehabil. 2017, 31, 1292–1304. [Google Scholar] [CrossRef]
- Darekar, A.; McFadyen, B.J.; Lamontagne, A.; Fung, J. Efficacy of virtual reality-based intervention on balance and mobility disorders post-stroke: A scoping review. J. Neuroeng. Rehabil. 2015, 12, 46. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]




| Participants | Studies were included if they included human (healthy or clinical) populations. Modeling and animal model studies were excluded. |
| Interventions | Studies were included if they covered treatment interventions using VR that aimed to improve gait, standing balance, and/or upright mobility. Studies were excluded if they used adjunct therapeutic modalities simultaneously with the VR intervention (robot-assisted gait training, transcranial magnetic stimulation, etc.). |
| Comparisons | Studies were included if they included pre- and post-treatment assessments and/or comparisons between VR and conventional treatment (i.e., balance training, etc.). Studies were excluded if they did not include these comparisons. |
| Outcomes | Studies were included if they reported functional or clinical outcome measurements of gross motor abilities, or biomechanical measurements related to gait, balance, or upright mobility. Studies with outcomes outside of this description were excluded. |
| Study Design | Study designs that employed baseline and post-treatment assessments were included. Studies were excluded if they were case studies or had <10 participants in the experimental group. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Felsberg, D.T.; Pousti, R.; Howard, C.K.; Ross, S.E.; Raisbeck, L.D.; McGuirt, J.T.; Rhea, C.K. The Landscape of Virtual Reality Use in Mobility Rehabilitation from 2010–2023: A Scoping Review. Technologies 2025, 13, 167. https://doi.org/10.3390/technologies13050167
Felsberg DT, Pousti R, Howard CK, Ross SE, Raisbeck LD, McGuirt JT, Rhea CK. The Landscape of Virtual Reality Use in Mobility Rehabilitation from 2010–2023: A Scoping Review. Technologies. 2025; 13(5):167. https://doi.org/10.3390/technologies13050167
Chicago/Turabian StyleFelsberg, Danielle T., Reza Pousti, Charlend K. Howard, Scott E. Ross, Louisa D. Raisbeck, Jared T. McGuirt, and Christopher K. Rhea. 2025. "The Landscape of Virtual Reality Use in Mobility Rehabilitation from 2010–2023: A Scoping Review" Technologies 13, no. 5: 167. https://doi.org/10.3390/technologies13050167
APA StyleFelsberg, D. T., Pousti, R., Howard, C. K., Ross, S. E., Raisbeck, L. D., McGuirt, J. T., & Rhea, C. K. (2025). The Landscape of Virtual Reality Use in Mobility Rehabilitation from 2010–2023: A Scoping Review. Technologies, 13(5), 167. https://doi.org/10.3390/technologies13050167







